- 1Department of Psychiatry, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States
- 2School Psychology Program, University of North Carolina at Chapel Hill School of Education, Chapel Hill, NC, United States
- 3Darjeeling Ladenla Road Prerna, Darjeeling, India
- 4Department of Global Health and Development, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 5Broadleaf Health & Education Alliance, Stroudsburg, PA, United States
- 6Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 7Center for Global Health, Colorado School of Public Health, Aurora, CO, United States
- 8Department of Obstetrics and Gynecology, University of Colorado Anschutz Medical Campus, Aurora, CO, United States
- 9Department of Epidemiology, Colorado School of Public Health, Aurora, CO, United States
Objective: We assessed task-shifting children's mental health care to teachers as a potential approach to improving access to child mental health care.
Methods: In Darjeeling, India, we conducted a single-arm, mixed-methods feasibility study with 19 teachers and 36 children in five rural primary schools to determine whether teachers can deliver transdiagnostic mental health care to select children-in-need with fidelity to protocol, to assess which therapeutic options teachers chose to use within the protocol, and to evaluate for a potential signal of efficacy.
Results: Participation rates for intervention activities were >80%. A majority of teachers met or exceeded quality benchmarks for all intervention activities. Teachers chose to deliver teacher-centric techniques, i.e., techniques that only teachers could deliver given their role in the child's life, 80% of the time. Children improved in mental health score percentiles on the Achenbach Teacher Report Form. Key facilitators included the flexibility to adapt intervention activities to their needs, while identified barriers included limited time for care delivery.
Conclusion: Findings support the feasibility of task-shifting children's mental health care to classroom teachers in resource-limited schools. Fidelity to protocol appeared feasible, though the freedom to choose and adapt therapeutic techniques may also have enhanced feasibility. Surprisingly, teachers consistently chose to deliver teacher-centric therapeutic techniques that resulted in a potential signal of efficacy. This finding supports the potential emergence of “education as mental health therapy” (Ed-MH) as a new therapy modality. Continued investigation is required to test and refine strategies for involving teachers in the delivery of transdiagnostic mental health care.
Introduction
Most of the 20% of children with mental health needs will remain unrecognized, unsupported, and affected throughout their lives (1, 2). Access to quality mental health care remains poor for most, particularly in low and middle income countries (LMICs) such as in India where <1% of affected children receive care (3). Innovative care models are urgently required to overcome this care gap (4, 5).
Task-shifting mental health care, in which professionals train and support non-accredited lay counselors to deliver therapy, is one widely used approach to close mental health care gaps in LMICs for adults and adolescents (6). Task-shifting indicated child mental health care, however, has yielded mixed results, in part as its provision requires knowledge of and experience with children's developing cognitive and emotion-regulation abilities (7).
With relevant experience in child development, teachers in LMICs are uniquely positioned to deliver indicated task-shifted children's mental health care given their consistent access to children (8, 9). However, few publications in LMICs study interventions that shift to teachers the task of delivering mental health care to select children-in-need (6, 7, 9), perhaps due to teachers expressing lack of (1) training to do so and (2) time and energy to take on counseling tasks above their primary duties (4, 8).
Yet, relevant literature studying teachers delivering other forms of mental health care, specifically mental health prevention and promotion for children and indicated care for adolescents, indicate that teachers in LMICs can feasibly deliver this care with fidelity (7, 10–15). Notably, these interventions are structured as whole-school or whole-class interventions with elements that fit into teacher workflows, folding an alternative structure in with more typical one-on-one sessions lay counselors conduct (6, 7, 10, 14, 15). Further, as implementation fidelity is considered imperative in any task-shifting model, studying teacher fidelity to any protocol is crucial in determining whether teachers can deliver indicated, task-shifted mental health care (16, 17). No published studies have assessed the feasibility of teachers delivering with fidelity indicated, task-shifted, alternatively structured mental health care. Such an evaluation may have important implications for the viability of teachers delivering care to children with mental health needs.
The purpose of this study was to determine the feasibility of teachers delivering “Tealeaf” with fidelity, where “Tealeaf” (Teachers Leading the Frontlines - Mansik Swastha; Tealeaf – Mental Health; “Tealeaf”) is a novel intervention our team developed in which teachers deliver evidence-based, indicated psychological care to their students in need in rural primary schools of Darjeeling, India. Departing from traditional lay counseling models where care is solely delivered in one-on-one, office-based sessions, Tealeaf is unique in that teachers use a transdiagnostic, non-manualized, evidence-based approach that they can customize, including using both one-on-one sessions and care tasks fitted into their primary teaching duties. To evaluate the feasibility of Tealeaf, in 2018, we used a convergent parallel mixed methods design. We hypothesized that, with training, support, and supervision, classroom teachers could deliver indicated mental health care, Tealeaf, with fidelity, and that such fidelity was feasible for teachers. We further hypothesized that teachers would primarily choose therapeutic techniques traditionally used by lay counselors in one-on-one sessions and then choose supplementary classroom-based techniques to reinforce the therapeutic work completed in one-on-one sessions. Secondary aims were (1) to explore potential impact on student mental health statuses and (2) to assess whether fidelity of intervention delivery was associated with changes in children's mental health status.
Materials and Methods
Setting
Darjeeling is a district in the State of West Bengal in the Himalayas of Northeast India. Within India, Darjeeling is considered a multi-ethnic, geographically-distinct space with several minority communities existing within and side-by-side with Nepali residents (18). Economic conditions in the predominant tea plantation and small-scale agricultural communities are poor, with daily wages for tea labor at 202 INR ($2.75 USD) (18).
Due to a perception of higher quality education and preference for English education, many families in rural Darjeeling send their children to low-cost private (LCP) schools (19). While Darjeeling estimates of LCP enrollment are not available, LCP enrollment is estimated at 30–50% of primary school students across India (18). LCP schools are primarily established by community members charging modest tuition to cater to a low-income population (19). As a result, LCP school teachers get paid minimally, 1,500–3,000 INR ($23–45 USD) monthly (18). No study has published the demographics of teachers in Darjeeling; one study that aggregates LCP and government teacher demographics across India shows that, compared to government school teachers, LCP teachers were more likely to be younger (29.61 vs. 40.28 years) and be college graduates (49 vs. 39%), and less likely to complete a teaching certificate (28 vs. 80%) (20).
Participants
Seventeen LCP schools were approached; five were pragmatically selected. Inclusion criteria were set with the goal of reaching children in Darjeeling with poor access to care (19). Eligible schools could not be receiving government aid, could charge annual fees of 11,500 INR ($180 USD) or less, and were located in rural Darjeeling. Also, schools had to have four full-time teachers on faculty and enroll at least 50 students to increase the likelihood of accurate approximation of child mental health prevalence rates globally.
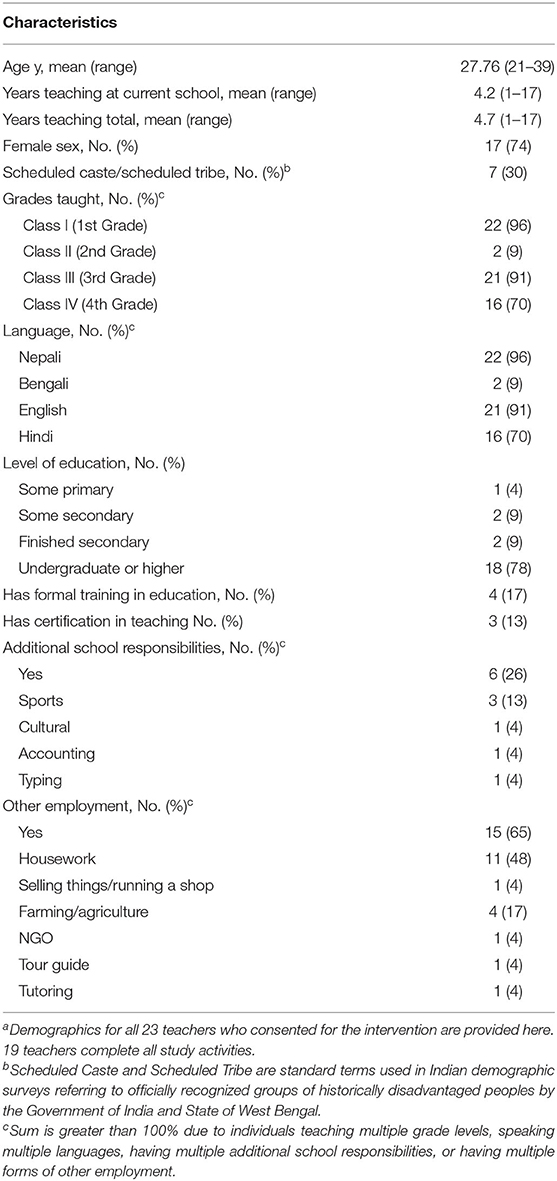
From these schools, 23 teachers were consented, 21 attended the Tealeaf 10-day training, and 19 teachers completed all study activities. Teachers were eligible if they had primary teaching responsibility for a primary grade level class (1–4) in an enrolled school, were 18 years or older, and were not suspected or convicted of child-related misconduct. Teachers were required to have >1 year of teaching experience to avoid confounding the feasibility of care delivery with learning how to teach. Teachers were not compensated for their participation in the study.
After teachers completed training, they used a study specific tool, the Behavior Type and Severity Tool (BTST; Supplementary Figure 1), to systematically capture their clinical impressions of each student in their class (ranging from 5 to 25 students). Tealeaf-trained teachers then each nominated two of their students in need of mental health care for their mental health services. The subject of a separate publication, teachers nominated children in need in this study with moderate accuracy, using their judgment and as aided by their impressions captured by the BTST (21, 22). The BTST as a stand-alone tool is weakly accurate in identifying students in need of mental health care as it was designed as a tool to aid teachers in their decision rather than as a definitive diagnostic tool; the moderate accuracy of teacher nomination largely stemmed instead from teacher judgment after completing training (21). Teachers were pragmatically limited to nominating two students each as, in earlier pilot testing, teachers voiced managing up to 2 students each feasibly given their education duties (21, 22).
The sole inclusion criteria for children (6–12 years old) was that they were in the class of an enrolled teacher. This inclusion criteria was set to be minimal to (1) to test teacher accuracy in nominating their students for mental health care and (2) allow children with any category of mental health difficulty and with any level of severity to be in the trial and receive care, as is the aim of Tealeaf. Tealeaf is designed to be resource-minimal given its LMIC setting and correspondingly leverages teachers for many care tasks, including selection of children for care. Thus, part of what was tested in this trial was teacher accuracy of nomination, as discussed above and the subject of a separate publication (21). Further, teachers are taught to deliver indicated care to students in need of that level of care. As a result, all levels of severity of symptoms were included; per study protocol and under the guidance of the principal investigator (CMC), though, children whose mental health difficulties endanger the safety of themselves or others are acutely referred to the local health system as is local custom (23, 24). Moreover, Tealeaf is designed to be transdiagnostic, as later described, such that teachers can deliver care to any child with any mental health struggle. Accordingly, all diagnostic categories of mental health symptoms were included.
Intervention
Tealeaf is an intervention that task-shifts to teachers the delivery of evidence-based, indicated child mental health care. It is a non-manualized approach that teachers can customize, including fitting care tasks into their primary teaching duties. Further, Tealeaf is designed to be transdiagnostic as this approach to care applies “the same underlying principles across mental disorders, without tailoring the protocol to specific diagnoses,” allowing teachers to learn one set of therapeutic techniques and still provide care for any diagnosis (25). It was created in response to community needs identified through a lay field-worker-led school health program for primary schools in Darjeeling, India (19).
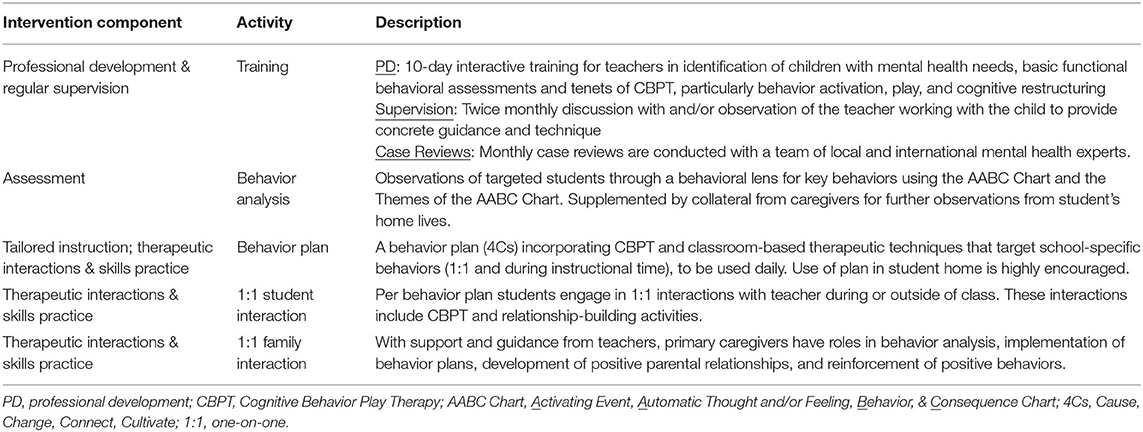
Tealeaf is implemented over a school year and involves six major components: training and supervision, nomination of students for care, behavior analysis, behavior plans, one-on-one interaction with students, and engaging caregivers. Basic functional behavioral assessments and Cognitive Behavior Play Therapy (CBPT) serve as core tenets of care. Teachers understand their students' mental health status and behavior through basic functional behavioral assessments. They then deliver care through the use of evidence-based therapy techniques, derived from CBPT, that are interwoven into a child's daily school schedule. CBPT was chosen as Tealeaf's core therapeutic modality as it provided teachers with practical and tangible therapeutic techniques based in Cognitive Behavior Therapy (CBT) that are cognitively accessible to primary-school-aged children using both talk and play forms of therapy (26). The efficacy of a play therapy medium for primary school students has been repeatedly validated while the efficacy of CBT has been extensively validated for older children, with evidence to support use in younger children (27). Table 1 breaks down Tealeaf into deliverable components.
A psychiatric social worker with expertise in youth mental health first delivers a 10-day training (see Supplementary Figure 2 for training outline). While the approach to care is transdiagnostic, a framework of behavior fitting into categories of anxiety, disruptive, or mood is taught to technically level for teachers the conceptualization of mental health behaviors and accompanying care, discussed further in a separate publication from this group of authors (21). Categories were named “nervous,” “disagreeable,” and “withdrawn,” respectively, after consulting with local experts and to refrain from further stigmatizing mental health.
Teachers then use a study specific tool, the BTST (Supplementary Figure 1), to systematically capture their clinical impressions of each student in their class. Using their judgment, aided by the BTST (as discussed above), they each choose two students to deliver care to, pragmatically limited, whom they believe have the highest mental health needs (21).
Thereafter, teachers analyze the behavior of each child they choose to deliver care to using 2 decision support tools, the Activating Event, Automatic Thought and/or Feeling, Behavior, & Consequence Chart (AABC Chart) and the Themes of the AABC Chart, that simplify and technically level behavior analysis (Supplementary Figures 3A,B). The AABC Chart is similar to an ABC Chart in CBT with the exception of the addition of “automatic thoughts and/or feelings.” This was added (1) to simplify the distinction between automatic thoughts and resulting feelings as teachers were considering them as one and the same in the pilot and (2) to set up their later work with students to identify the automatic thoughts and/or feelings associated with the observed behavior as part of cognitive restructuring. The Themes of the AABC chart was created as a decision support tool to further technically level the interpretation of the AABC Chart that teachers had expressed difficulty interpreting during pilot testing.
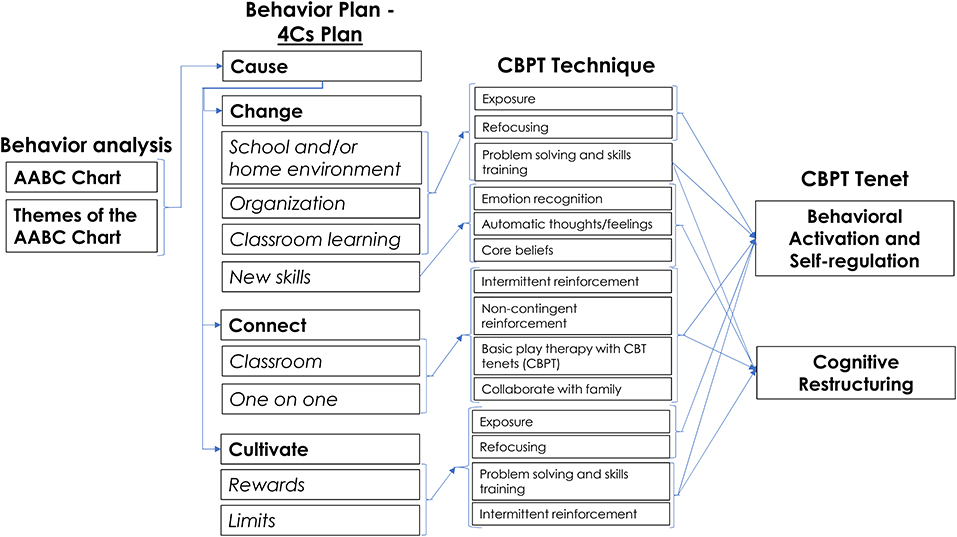
After behavior analysis, teachers then developed a targeted response using a behavior plan called the 4Cs Plan (Cause, Change, Connect, and Cultivate) (Supplementary Figure 3C). The 4Cs is akin to behavior plans teachers commonly use in high income countries (HICs) to manage a child's challenging behavior toward the goal of improved learning, but used in Tealeaf with the end goal of improving child mental health (28). An individualized behavior plan approach was chosen as the care implementation method (as opposed to manualized care) as it aligned with how teachers already adapted their teaching and interactions individually to students' needs (8). In the 4Cs, teachers select therapeutic techniques to deliver from (1) a menu of evidence-based therapeutic options to use for each category of behavior, (2) ones learned in training that were not listed on the menu of options, or (3) ones they adapted under the guidance of study staff (PG) (Supplementary Figure 4). In Tealeaf, the “dose” of care is each interaction between the teacher and student that is tweaked to be therapeutic and evidence-based, whether in the classroom or in one-on-one brief sessions. Such a dosing system deviates from traditional lay counselor task-shifted care where “doses” are measured as number and length of office-based, one-on-one therapy sessions.
CBPT techniques and tenets are infused throughout the 4Cs (Figure 1). As part of technically leveling CBPT, available techniques include ones that can fit within classroom activities or school schedules. To further technically level CBPT and increase potential feasibility, (1) behavioral activation and self-regulation and (2) cognitive restructuring are the chosen areas of therapeutic focus for teachers (Figure 1). Considered complementary in CBT and in neurocognitive systems, behavioral activation and self-regulation can be guided by teachers as it actually occurs, in contrast to an office-based therapist who is limited to planning and debriefing away from lived moments (8, 29, 30). Cognitive restructuring is incorporated through traditional means, such as the AABC Chart; it is also taught to be used in moments of struggle or success during which teachers are providing evidence to counter automatic thoughts/feelings and core beliefs in real time, similar to behavioral activation and self-regulation as above (8).
Following completion of the 4Cs, the remainder of the school year is dedicated to the development of therapeutic relationships and the delivery of therapeutic interactions and skills practice, with revisions to the 4Cs based on each child's progress. Teachers make changes to the school environment and engage with the child throughout the school day and in one-on-one (1:1) interactions. Real time interactions allow for immediate positive reinforcement of appropriate behaviors, as well as real time crisis management, processing of co-experienced behavioral struggles, and learning of social skills within the student's everyday setting. Rooted in each child's 4Cs Plan (and not manualized, as discussed above), teachers have the freedom to choose the content of their one-on-one interactions and sessions as well as how many, how long, and where their interactions and sessions will be. With the same level of freedom as the care-delivery, teachers also work with families to guide development of positive parental relationships and reinforcement of positive behaviors in the home. Throughout the year, teachers receive supervision through monthly site visits supplemented by as-needed telephone discussions by the psychiatric social worker with youth mental health expertise who also delivers their training to guide their care, leading to two supervision sessions monthly on average.
Outcomes and Procedures
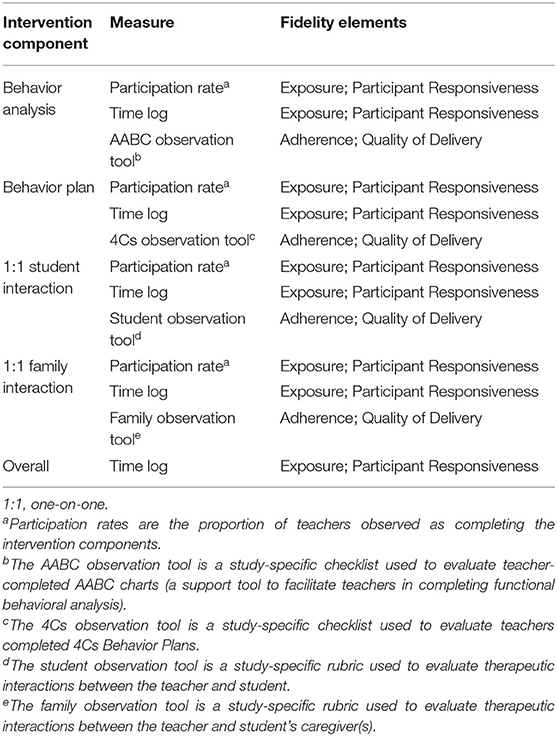
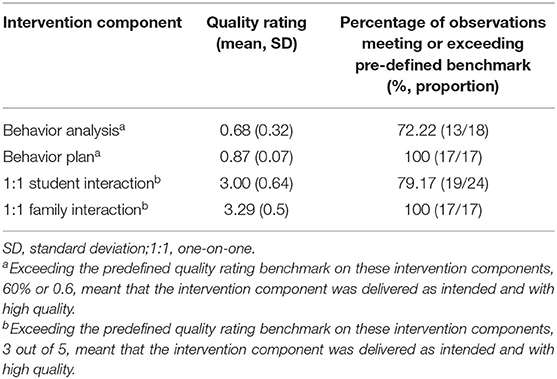
Fidelity was defined as the degree to which teachers implemented intervention activities as intended (16). Four elements of fidelity were assessed: (1) adherence, (2) exposure, (3) quality of delivery, and (4) participant responsiveness (31). To assess these elements of fidelity, we mapped quantitative indicators to the core components of the intervention (Table 2). Of note, evaluation of the training component is the subject of a separate manuscript (32).
Time logs and participation rates for intervention activities were used to assess exposure (the amount of the intervention delivered) and participant responsiveness (the extent to which teachers engaged in intervention activities). Teachers were requested to record the time spent and nature of interactions with the students (Supplementary Figure 5). A mean time investment of >30 min/week was chosen to indicate sufficient exposure and participant responsiveness, similar to other interventions in which lay counselors deliver task-shifted mental health care (6). Participation rates were defined as the proportion of teachers participating in core intervention activities, determined by direct observation by study personnel.
To assess adherence (whether teachers delivered the intervention as it was designed) and quality of delivery (the manner in which the teacher delivered the intervention), observation tools were developed for the four intervention activities (Supplementary Figure 6). These study-specific checklists and rubrics were developed by the research team, reviewed by a panel of experts, and field tested prior to finalization.
Teacher-completed AABC Charts and 4Cs Plans were rated using checklists that assessed understanding of theoretical concepts and application of key skills. Each item on the checklist was rated all (1), some (0.5), and none (0) and the results were averaged to yield a final score expressed as a percentage. Therapeutic interactions with the child and family were rated based on observations of counseling skills. Guided by rubrics, observers rated teachers from 1 to 5, 5 being of highest quality, at 0.5 intervals before determination of a final score.
We determined an a priori benchmark score of ≥60% for each observation tool to indicate that teachers delivered the intervention component as intended and with high quality. To set a high standard, 60% was chosen based on literature for rating fidelity when mental health professionals were demonstrating a new technique (33–35).
Observational assessments were conducted by the Research Administrator (PG). Multiple procedures were utilized to ensure reliability in ratings. The Research Administrator is a regional expert in child mental health with deep familiarity with the intervention. During 60 hours of training on the study-specific evaluation tools, she collaboratively scored a sub-sample of AABC Charts and 4Cs Plans with the PI (CMC) and reviewed observations of therapeutic interactions with the PI to norm scoring processes. She and the PI were blinded to the predetermined benchmarks.
Qualitative data were acquired in parallel to gain an in-depth understanding of feasibility. Semi-structured interviews (“interviews”) with 17 teachers were conducted in December 2018 (Supplementary Figure 7) and supplemented with intervention documentation (e.g., field notes and supervision notes). Interviews were recorded and conducted in Nepali; they were transcribed and translated into English by an outside agency. 4Cs Plans and field notes documenting changes to 4Cs Plans over time were also qualitatively evaluated to gain a descriptive understanding of the types of therapeutic measures teachers chose to implement.
To explore intervention impact on child mental health, students receiving care were assessed via the Achenbach Teacher Report Form (TRF) (36). Considered a gold standard, the TRF is standardized to capture teacher reports of child mental health challenges. Used globally in multicultural research, it has robust validity across LMICs, with evidence for partial support for factorial validity in the Indian context (37–39). Lower cutoffs for “clinical” and “borderline” designations than the TRF authors' published standards are thought to be more appropriate for the Indian context (37, 38). Still, no other teacher input form reviewed by a panel of experts was considered as locally applicable or as strongly validated for the local context as the TRF (37–39).
Based on teacher responses to 113 questions, several clinical scores are calculated on the TRF, with aggregate scores for Total Problem, Internalizing problems, Externalizing problems, Sluggish Cognitive Tempo, Obsessive Compulsive, and Stress Related, as well as subdomain scores for 8 empirically validated syndromes and 6 Diagnostic and Statistical Manual (DSM)—oriented scales. Raw scores are converted into T-scores, and a percentile score is obtained. Total problem, Externalizing, and Internalizing T-scores from 60 to 63 are considered “borderline” and ≥63 are “clinical.” The remaining aggregate scale scores and all subdomain T-scores from 65 to 69 are classified as “borderline” and ≥70 as “clinical.” Percentile scores <83 are considered “normal,” 83–90 “borderline,” and >90 “clinical” for Total Problem, Internalizing, and Externalizing scores. For the remaining aggregate scores and all subdomain scores, percentile scores <93 are considered “normal,” 93–97 “borderline,” and >97 “clinical.” For each child, TRFs were obtained pre-intervention (May), midpoint (September), and post-intervention (December). Each child was independently rated by two teachers: the primary observer was the teacher providing care and the secondary observer was another teacher not directly supporting the child but familiar with their behaviors and providing care to other students.
All participants provided written informed consent. For children, consent was obtained from a parent/guardian and children ≥7 years old provided verbal assent. The research protocol was approved by the University of North Carolina Institutional Review Board and a Darjeeling-based Ethics Committee. The study is registered with the Clinical Trials Registry-India (CTRI/2018/01/011471).
Analysis
To study fidelity outcomes, we conducted a series of descriptive analyses where appropriate proportions meeting predefined benchmarks were computed (a priori analysis). To explore impact, we calculated mean percentile scores at each time point for each observer category (a priori analysis). A linear regression analysis was conducted to compare TRF percentile scores across the time period of observation with β representing the slope for the best-fitting line fitted to the three TRF scores in order (baseline, midpoint, endpoint), adjusted for gender (a priori analysis). Pearson's correlation coefficients were calculated to assess whether there was a statistically significant relationship between each aspect of fidelity (time logs and observation ratings for core activities) and children's mental health outcomes (TRF total problem score percentiles) (post-hoc analysis). All P values were 2-tailed and significance was set at P < 0.05. Analysis was completed in SAS version 9.4 (40).
Qualitative analyses were pursued with two aims. First, interviews were analyzed with the aim of qualitative description of the feasibility of teacher-delivered mental health care (a priori analysis) (41). Second, we aimed to capture teachers' choices of therapeutic techniques through qualitative description of the 4Cs and the research administrator's accompanying field notes documenting changes to the 4Cs throughout the year (post-hoc analysis). Two independent analysts coded all 4Cs Plans, field notes, and interview transcripts and converged on codes for each document. Coding and analysis was an iterative process of reading, coding, summarizing, and rereading. One codebook was created for 4Cs Plans and field note analysis and a second codebook for interview analysis. Using content analysis, coding began through a deductive coding method using an unconstrained matrix, allowing emergent codes to be added (42).
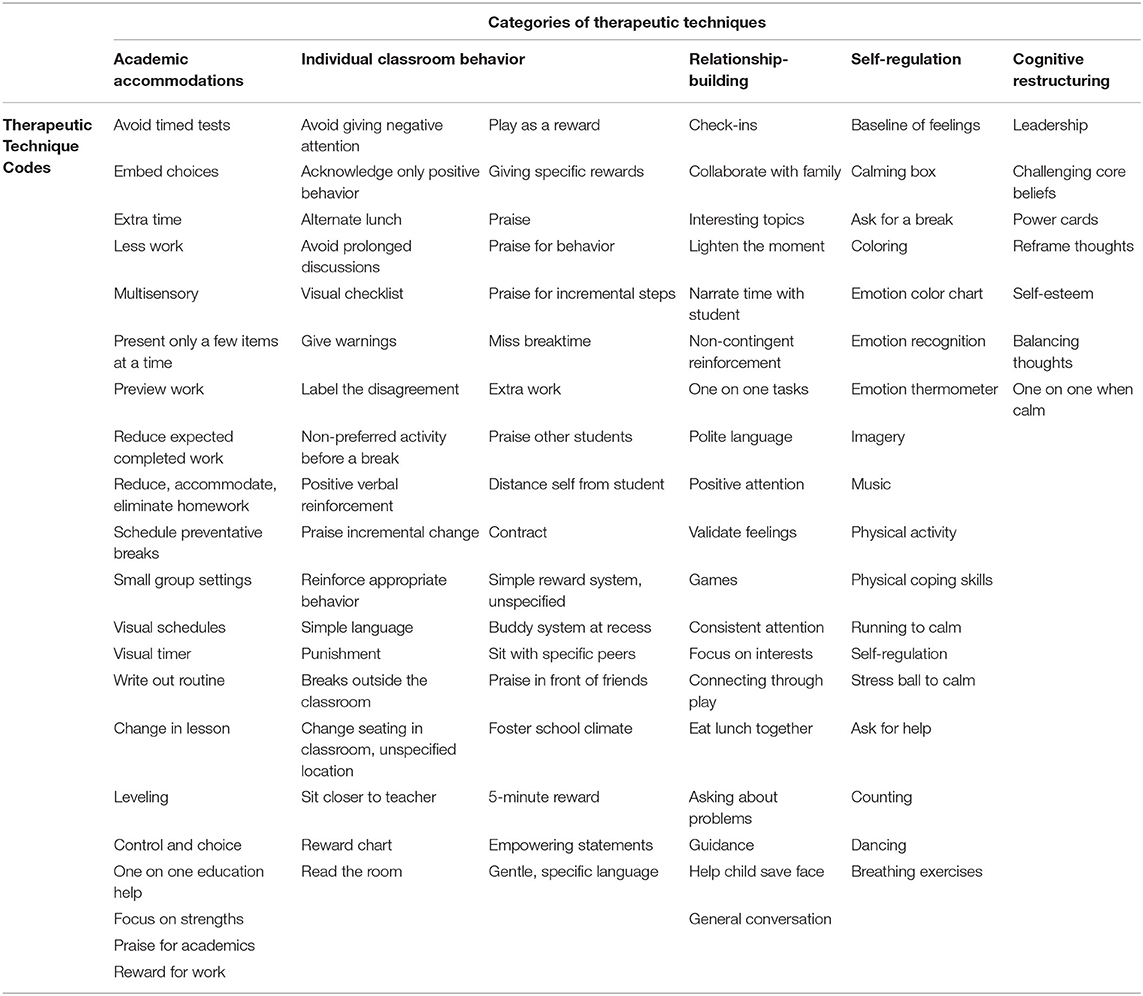
For interviews, codes were coalesced and a provisional set of themes and sub-themes were generated and reviewed, with important contrary opinions identified. Ultimately, a final set of common themes and sub-themes were identified alongside illustrative quotes. Results of the analysis were linked to common aspects of feasibility analyses (16). For 4Cs and field note analysis, each technique used was coded. Codes were then organized into a matrix of categories of therapeutic techniques that were based on a review of the literature and reviewed by a panel of experts in child mental health and education (Table 3). In line with a content analysis method, codes were tallied and tallies of codes within each category were summed to provide a descriptive picture of the types of techniques teachers chose for therapy delivery (42). ATLAS.ti was used for interview analysis and NVivo was used for 4Cs and field note analysis (43, 44).
Results
Demographics
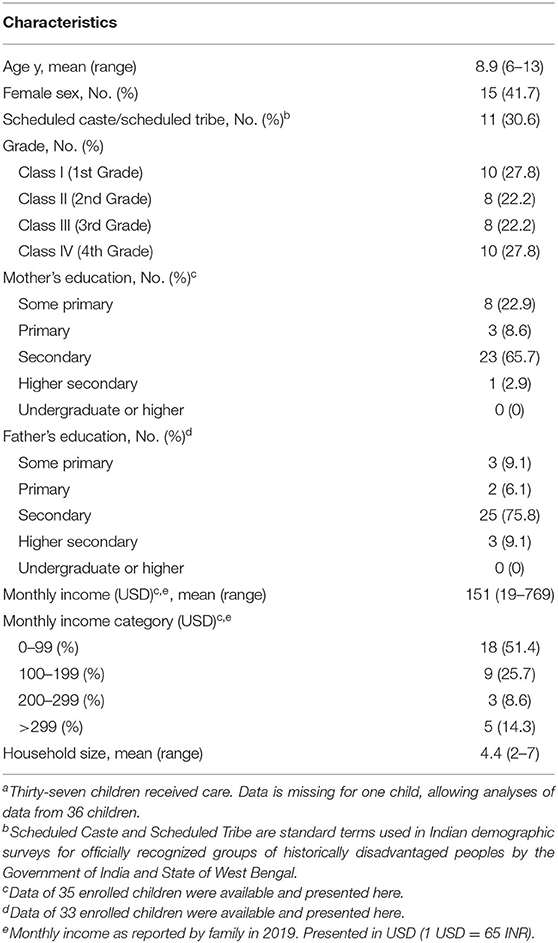
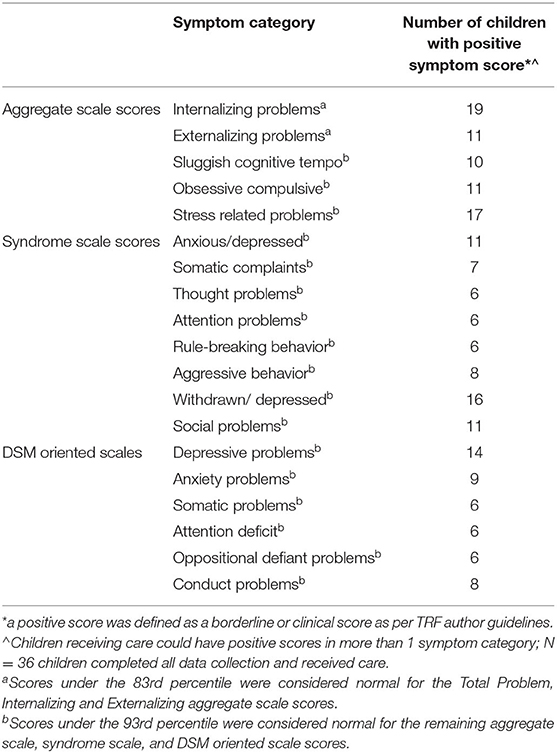
Of participating teachers (n = 19), the majority were female (74%) and 27.76 years old on average (range 21–39) (Table 4). Forty-two students were nominated and consented to the intervention; five students were withdrawn pre-intervention as their teachers determined that their behaviors normalized and they no longer required additional support (Table 5). The remaining 37 children received care from their teachers, and the 36 children who completed all data collection were included in data analyses. The average age of enrolled children was 8.9 years and 41.7% were female. Their diagnostic categories of struggles ranged across all aggregate and subdomains measured by the TRF, indicating a wide variety of symptoms experienced by enrolled children (Table 6). The most frequently experienced symptoms were internalizing in nature (n = 19). Correspondingly, the most frequent categories of symptoms children experienced were in depressive subdomains; 11 children were classified as anxious/depressed and 16 children as withdrawn/depressed on syndrome scale scores while 14 children were classified as having depressive problems on DSM-oriented scales.
Fidelity Outcomes
Participation rates for the assessed activities of behavior analysis and behavior plan were 85.7% and 81.0%, respectively. In time logs, teachers averaged 2.5 interactions/week and invested a mean of 19.0 min/week (standard deviation 27.5). The mean quality rating for each intervention activity met or exceeded the predefined benchmark: 60% for behavior analysis and behavior plan and 3 out of 5 for 1:1 student interaction and 1:1 family interaction (Table 7). Similarly, for individual observations, the percentage of teachers meeting or exceeding the benchmark ranged from 72 to 100%.
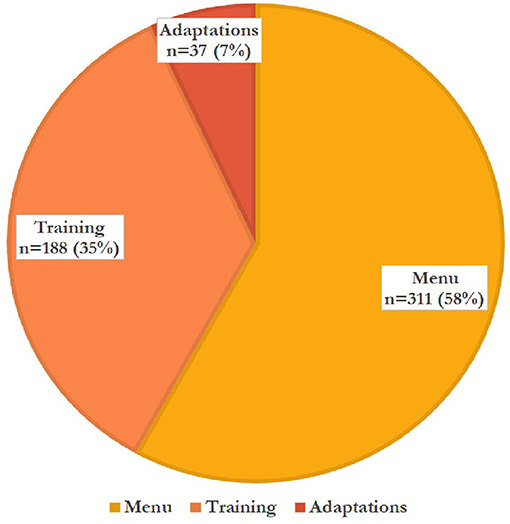
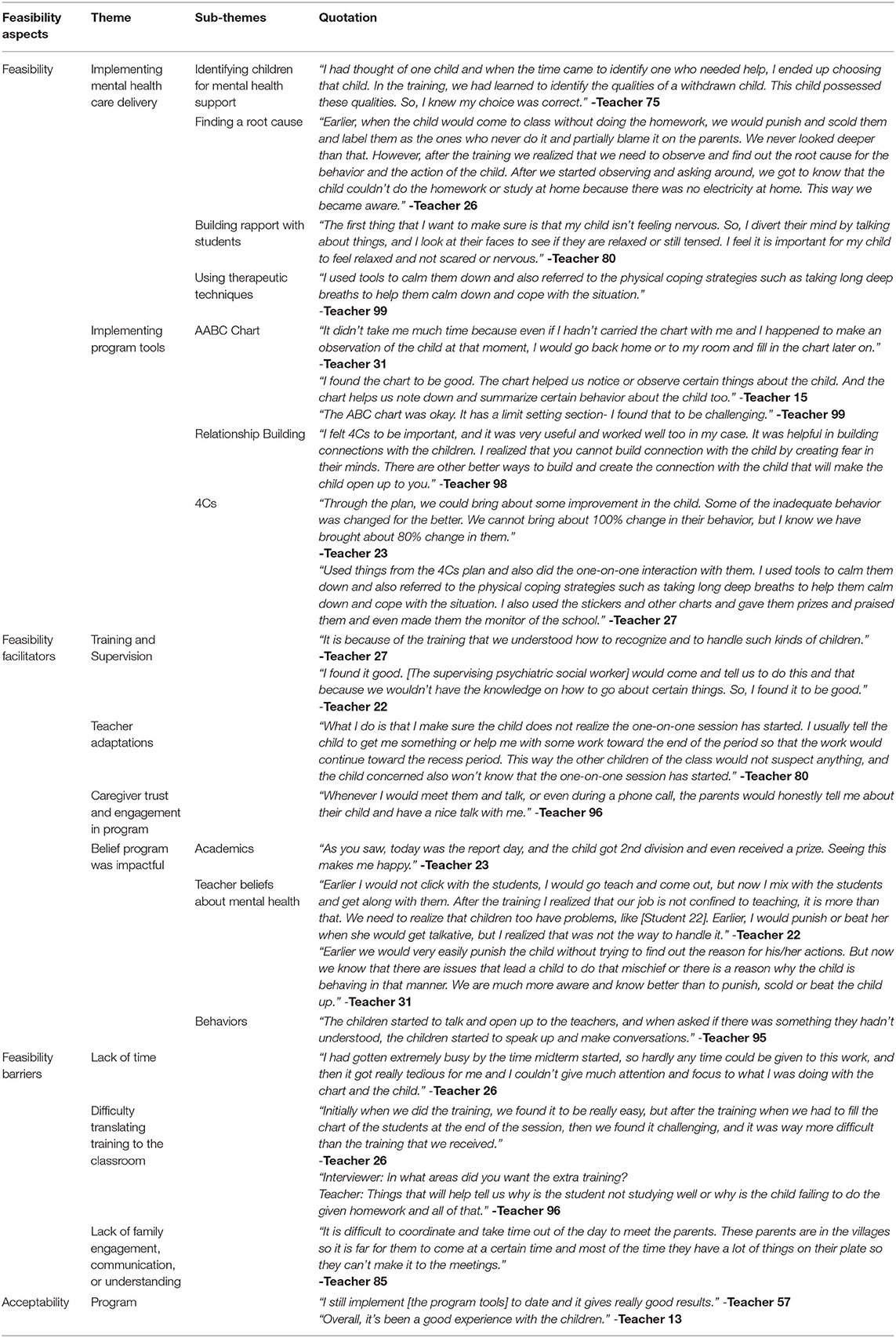
Figure 2 details the 536 therapeutic techniques teachers used per Tealeaf source (menu, training, or adaptation). Figures 3, 4 detail the 536 techniques per category (academic accommodations, individual classroom behavior, relationship building, self-regulation, or cognitive restructuring). Three-hundred-seventeen techniques (59%) were those only teachers (not office-based therapists) would be able to deliver, here termed “teacher-specific” care (Figure 3). These techniques had the purposes of improving both mental health and either knowledge transfer (“academic accommodations”) or classroom behavior (“individual classroom management”), tasks only teachers could dually accomplish and that office-based therapists could not, based on their job duties (8).
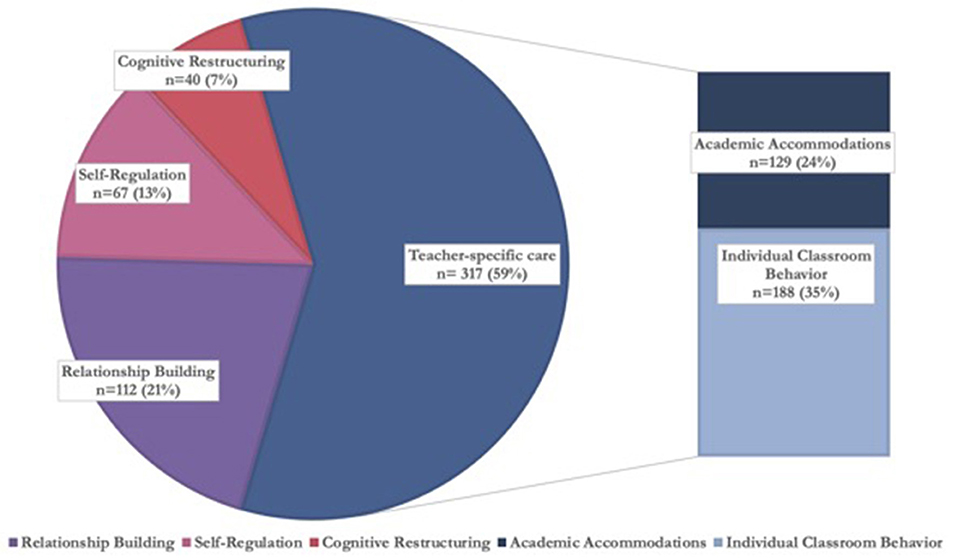
Figure 3. Categories of therapeutic techniques teachers used, grouped by teacher-specific care n = 536.
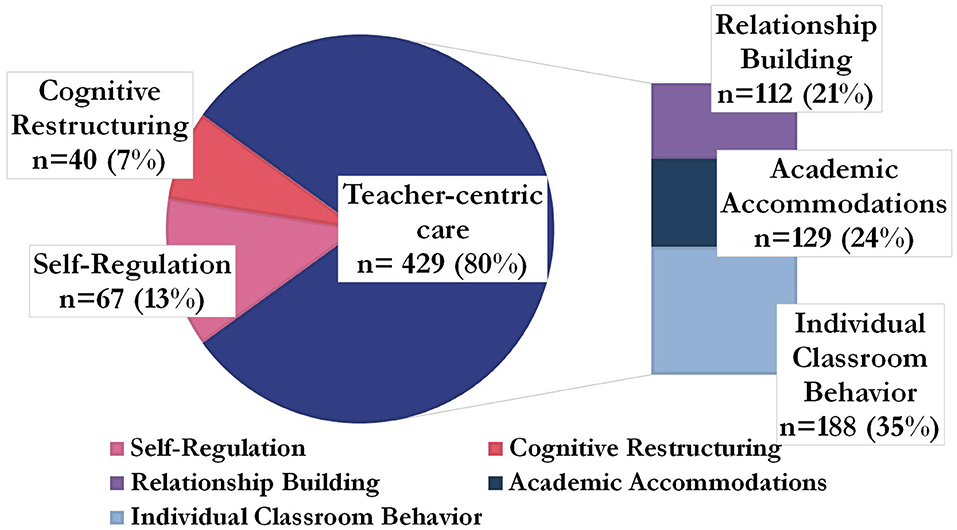
Figure 4. Categories of therapeutic techniques teachers used, grouped by teacher-centric care n = 536.
Academic accommodations (n = 129, 24%) were one category of techniques only teachers could use as only teachers would be able to use a student's academic work as a means of improving the student's mental health. A specific example of an academic accommodation technique follows. A student with anxiety who does not complete homework assignments is found to have counterproductive automatic thoughts underlying his homework difficulties, where he thinks he is incapable of completing homework assignments due to being overwhelmed by the quantity and needing to get all answers correct. To counter these automatic thoughts, his teacher can reduce the student's homework quantity for the purposes of behavioral activation, allowing the student to complete assignments successfully and counter the automatic thought that he is incapable. Over time, the teacher can increase the homework quantity as a form of exposure until the student can complete all of the originally assigned work. The second category of teacher-specific techniques centered on individual classroom behavior management (n = 188, 35%). For example, a teacher can separate the classroom and lunchroom seating of a student with depression and feelings of worthlessness from a student who is bullying the student and contributing to feelings of worthlessness, thereby reducing a precipitating factor of the student's experiencing of depression and making it easier for the student to practice self-regulation.
The relationship building techniques teachers used (n = 112, 21%) also consisted of measures only teachers would be able to take, such as giving consistent, non-contingent attention to the student receiving care throughout the school day. This was not counted in teacher-specific care, however, as office-based therapists also build relationships with clients as part of typical duties, though use different techniques (45). Still, when assessing the number of techniques teachers used that were ones only they could use, whether the purpose was unique to teachers (i.e., knowledge transfer or classroom behavior) or not (i.e., relationship building), here termed “teacher-centric,” 429 techniques (80%) used could be characterized as “teacher-centric” (Figure 4).
Feasibility Findings
Interviews provide evidence that teachers find delivering mental health care as structured in Tealeaf and using Tealeaf program tools to be feasible (Table 8). Feasibility was facilitated by training and supervision, teacher ability to adapt Tealeaf, caregiver trust and engagement, and a belief that the program was impactful. Barriers to feasibility included a lack of time to deliver Tealeaf, difficulty translating the training to the classroom, and a lack of family engagement. A theme of acceptability was indirectly expressed by many teachers (Table 8). They discussed their continuous delivery of care throughout the study, a desire to serve in the program and deliver care after the study's conclusion, and advocacy for the program to expand beyond this study, signs of acceptability (46).
Exploration of Impact; Correlation Between Fidelity and Impact
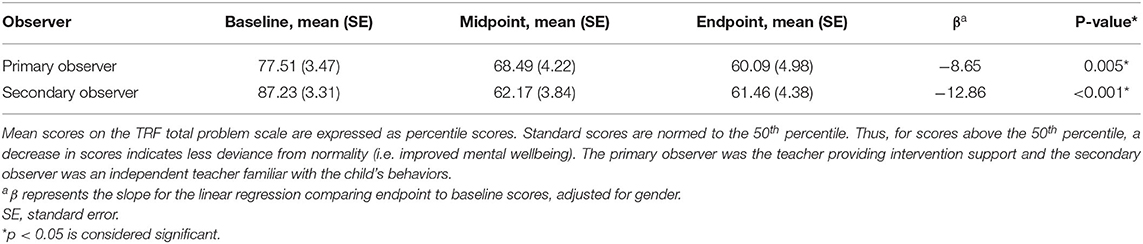
Improvement in mental health status is demonstrated by the decrease in mean TRF Total Problem score percentile across three time points (Table 9 and Supplementary Figure 8). Primary observers rated children on average as increasing in normalcy and secondary observers rated children on average as improving from borderline to normal. Only total time a teacher spent on intervention and their student's mental health outcomes were correlated (Pearson Correlation Coefficient 0.46, P = 0.009; Supplementary Table 1).
Discussion
Overall, the results of this mixed-methods feasibility study suggest that teachers in resource-limited primary schools in an LMIC setting are able to deliver indicated, transdiagnostic child mental health care with fidelity and feasibly but in a particular form, one with flexibility and that is incorporated into a teacher's primary duty of teaching.
Implementation fidelity underlies whether and how interventions achieve their intended outcomes, but may be at odds with feasibility (47). Teachers achieved quality implementation and were witnessed to adopt their chosen therapeutic techniques into their interactions with students and caregivers. Some teachers expressed difficulty with specific intervention tools. Overall, though, in interviews most teachers did not perceive Tealeaf to be beyond their capacity or abilities, and many further expressed acceptability of Tealeaf, indicators that teachers viewed delivering care with fidelity to be feasible.
The feasibility of delivering Tealeaf with fidelity may have been enhanced by teachers' ability to choose and adapt which therapeutic techniques to use. Fidelity is viewed as a marker of high quality implementation and is often in opposition to choice and adaptation (48). Here, with evidence of teacher choice considered a positive marker of fidelity, a balance of fidelity with choice and adaptation was intentionally sought. In unpublished pilot testing results, teachers expressed both that Tealeaf techniques were usable and that they valued the ability to choose and adapt techniques as seen fit. In this study, teachers then demonstrated that delivering Tealeaf care with fidelity was considered feasible while also using a wide variety of techniques. Further, in interviews, they voiced the usability of Tealeaf tools while also expressing that choice and adaptation were crucial to facilitating feasibility. Thus, it may be that a balance between fidelity to a structure (such as use of the 4Cs behavior plan) and choice and adaptation is needed to allow teachers to feasibly deliver care on top of and that fits with their typical duties.
The novel finding here is that, as a group, teachers organically overwhelmingly chose “teacher-centric” techniques (80%) to deliver child mental health care, that is, techniques that only teachers, and not office-based therapists, could implement. By contrast, we hypothesized that teacher-centric techniques would be a supplement to, but not more predominant than, one-on-one sessions. Such a consistent choice makes the care delivered in this study predominantly classroom-based and rooted in the knowledge transfer process, a sharp divergence from traditional office-like one-on-one sessions. An earlier publication from this group of authors found evidence for the potential emergence of “education as mental health therapy,” here abbreviated as “Ed-MH,” where, in interviews, teachers consistently reported choosing to use the mental health techniques that they could incorporate into the knowledge transfer process, their primary duty (32). In the present study, we believe we find evidence corroborating the emergence of Ed-MH as a potentially new therapy modality: teachers consistently chose to deliver care that was teacher-specific 59% of the time and teacher-centric 80% of the time, care only they could deliver.
The organic emergence of Ed-MH may speak to task-shifted care delivery by teachers having to be incorporated into their primary duties to be feasible. Time log results further support this consideration. The time logged in one-on-one sessions may not have included the total time teachers spent delivering care, as the time log did not account for the time teachers spent using teacher-centric techniques (Supplementary Figure 5) (6). Instead, the time logged may be the average available weekly time teachers could spend in one-on-one sessions, below our expectations. Further, a theme of a lack of time emerged in teacher interviews as a barrier to feasibility for some. Thus, for teachers to feasibly deliver indicated care on top of their regular duties, it may need to be incorporated into their workflow.
It is possible that teachers used one-on-one sessions less frequently than teacher-centric techniques not because of the additional time needed to conduct these sessions, but instead because they were less familiar with them. Accordingly, teachers may have chosen to use teacher-centric techniques for their familiarity. Moreover, in interviews, some teachers mentioned wanting more time in training while others stated wanting more frequent supervision (as under the theme “Difficulty translating training to the classroom” in Table 6). However, most teachers sought additional guidance on use of teacher-centric techniques that were nevertheless novel to them despite their overlap with methods of teaching. In the setting of time being a barrier to feasibility for some, then, it may be that teachers have additional time and capacity to learn therapeutic techniques that are closely related to their primary duties as these techniques can be relatively efficiently learned. By contrast, the knowledge and skills teachers need to conduct one-on-one sessions are conceptually further afield from their primary duties, potentially requiring further additional time to learn them that teachers do not have to spare. Teachers delivering care primarily through one-on-one sessions, thus, may be less feasible than an Ed-MH model given the additional time needed both to conduct the sessions and to learn the skills needed for these sessions, even if the latter are potentially attainable through additional training and supervision.
Notably, even when likely underestimated, time was the only fidelity factor correlated with improved child mental health outcomes. It may be that the extended time teachers can spend with children with mental health needs throughout the school day could be among the more effective structures through which to deliver task-shifted care. The literature correspondingly points to increased academic learning time in classrooms being associated with improved learning; a dose-response relationship between child psychotherapy sessions and mental health outcomes, though, has not been evidenced in the literature, perhaps speaking to the mixed efficacy of task-shifted child mental health care that has predominantly been structured as one-on-one sessions (49–51).
The teacher-centric techniques of Ed-MH, akin to an educational intervention, overlap with adaptations to pedagogy teachers make to individually target different learners, a standard in education (52). As above, teacher-centric techniques may have been predominantly chosen for their familiar overlap with pedagogy (52). Ed-MH differs from individualized pedagogy, however, in that its primary goal is to improve mental health, while individualized pedagogy solely aims to successfully transfer knowledge to the student (52). Evidence in the literature points to a potentially marked difference between Ed-MH and individualized pedagogy. Interventions enhancing teachers' ability to individualize pedagogy through additional training have demonstrated meaningful improvement in student academic, but not mental health, outcomes (53, 54). By contrast, in this study, Ed-MH showed a potential signal of efficacy with improved TRF Total Problem percentiles over the year.
This study expands on the current literature by demonstrating that teachers can deliver indicated mental health care to children in need when incorporating the care into their workflows as in Ed-MH within Tealeaf, in line with other studies reporting that teachers can deliver care with whole-school and whole-classroom-based aspects feasibly and with impact (11, 12). The Ed-MH structure is an alternative to the traditional and validated structure of task-shifted mental health care, modeled after office-based care (i.e., one-on-one sessions) in which lay counselors' main duty is to provide care. While such a model has been validated, it may not be sustainable as it requires employing additional human resources (4, 6, 11, 12, 46). Leveraging teachers to deliver care through interweaving it into their teaching duties, by contrast, may lead to the eventual sustainability of task-shifted child mental health care as it can feasibly and efficiently be delivered by an existing, experienced human resource within their existing workflows (28).
Limitations
Our findings should be considered within a number of limitations. First, due to the novel nature of the intervention, we were unable to identify suitable pre-existing validated fidelity measures and instead used study-specific instruments. Second, observational assessments were conducted by the same individual who trained and supervised the teachers. Resource limitations prevented the use of external raters. To mitigate potential biases we (1) utilized several strategies to promote ratings reliability and (2) purposely set quality benchmarks to be high, both discussed previously. Third, findings from a separate publication indicate that teachers identified more students in need of mental health care than they were able to nominate based on pragmatically set limitations (21, 22) and, based on resource limitation, we were unable to examine whether teachers could feasibly deliver care to more than two children. A future effectiveness and/or implementation study is warranted to examine whether teachers can feasibly deliver care to more than two children and whether mental health symptoms improve to the same extent for these children whose teachers are delivering care to more than two children. Such a study would further elucidate the potential reach of teachers as lay counselors. Fourth, our time analysis is limited by the quality of data captured by the teachers, previously discussed. Fifth, the TRF may not have accurately captured child mental health statuses in the Darjeeling context, as described earlier. A publication from this group of authors showed that a majority of children from Darjeeling nominated by teachers for mental health support had “normal” TRF Total Problem Scores, close to the borderline/normal cutoff; the selected students instead had “borderline” or “clinical” subscale scores reflecting teachers' concerns for their mental health needs to the point of categorizing most of them as “definitely needs support” on the BTST (21). Still, the TRF was chosen for its relative strength in local applicability and validation as judged by a panel of experts (37–39). Sixth, positive mental health outcomes are preliminary. Obtained in a small sample size, they were not compared to controls and the time interval between measurements raises the possibility of regression to the mean (55). Further, they were completed by teachers, subject to bias in wanting their students to improve, though mitigated some by a second teacher not working with the child additionally rating the students' mental health.
Findings may not be generalizable to different regions or types of schools (such as government). Specific aspects of the teacher population, such as having limited prior education training, may have made them more receptive to training than more established educators and may limit our findings' generalizability (56). Additionally, teachers were not randomly chosen and may have been more enthusiastic to deliver care than teachers more broadly.
Conclusion
Child mental health remains under-developed within the larger global mental health movement. The vast majority of children in LMICs lack access to high-quality mental health care. Findings from this study suggest that Ed-MH delivered within Tealeaf is potentially an efficient and sustainable path forward for bridging the care gap.
Continued innovation and research around teacher-delivered transdiagnostic mental health care may thus be warranted. Examining the feasibility and acceptability of teacher-delivered care to children and their families will crucially inform whether potential recipients of care are willing to receive it in a relatively public space (the classroom) from a community member of import culturally (57). Examining the acceptability to teachers of their delivery of care to their students merits evaluation as having a dual role may create conflict with their students and families and/or break trust between them. These concerns are the subject of a separate manuscript under peer review from this group of authors. Further, our group is conducting a cluster randomized controlled trial to definitively examine child mental health outcomes after receiving teacher-delivered Ed-MH mental health care in Tealeaf. Ultimately, such work has the potential to improve the life trajectories of children with a broad range of mental health challenges globally, wherever teachers teach.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available for ethical reasons. Requests to access the datasets should be directed to christina_cruz@med.unc.edu.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of North Carolina at Chapel Hill Institutional Review Board and a Darjeeling-based Ethics Committee. Written informed consent to participate in this study was provided by the participant or, for minors, their legal guardian/next of kin, as follows.
• Schools: PG called principals of area schools to gauge interest. Interested principals discussed with their teachers their interest in intervention delivery and study participation.
• Teachers: All eligible teachers in participating schools were invited to meet with study representatives to review study protocols. Those interested in participating voluntarily signed a written informed consent.
• Children: Parents or guardians of children nominated by their teacher for the intervention were invited to meet with study representatives to review study protocols. Those interested in their children participating in the study voluntarily signed a written informed consent on behalf of their children. Children greater than 7 years of age were verbally assented for participating in the study and were allowed to refuse to participate.
Author Contributions
CMC, KH, and MM designed the study. BNG was involved in study design. CMC, PG, and MM created the teacher training, intervention materials, and intervention protocol. PG delivered the teacher training, provided supervision to teachers, and collected data. SB provided supervision to teachers and collected data. CMC, AAG, and MM provided umbrella supervision for the supervision of teachers by PG and SB. MML performed quantitative data analysis while JLV and PF performed qualitative data analysis. CMC, MML, KH, PG, SB, JLV, PF, AAG, and MM were involved in data interpretation. CMC, PG, MML, JLV, and MM drafted the manuscript. All authors revised and approved the final version of the manuscript before submission.
Funding
This work was generously supported by the American Association of Child and Adolescent Psychiatry (AACAP) through the Pilot Research Award for Junior Faculty and Child and Adolescent Psychiatry Fellows, supported by AACAP, awarded to CMC; the manuscript's contents are the responsibility of the authors and do not necessarily reflect the official views of AACAP. The publication of findings is made possible by the Doris Duke Charitable Trust, Fund to Retain Clinical Scientists—Caregivers at Carolina Award, awarded to CMC.
Conflict of Interest
CMC, PG, and MM hold the copyright to the training materials, decision support tools, and intervention materials for the teacher-led task-shifted alternative system of children's mental health care at the center of this manuscript. They have disclosed this interest fully to Frontiers in Psychiatry.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We profusely thank Roshan Rai, Executive Director, and Ashesh Rai, Assistant Director, of Darjeeling Ladenla Road Prerna (DLRP); Nima Choden, Dhiraj Rai, Maryam Subba, and Satyam Tamang, community health workers of DLRP; Radha Khawas, former research assistant at DLRP; and Fatima Salman of the Atlantic Council for their support of the implementation of the teacher-led task-shifted children's mental health care studied in this manuscript. We thank Mary Paul, funded by the Doris Duke Charitable Trust, Fund to Retain Clinical Scientists - Caregivers at Carolina Award, for proofreading this manuscript. We humbly thank the Mariwala Health Initiative for their generous support of DLRP.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.790536/full#supplementary-material
References
1. Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, et al. Children's mental health service use across service sectors. Health Aff. (1995) 14:147–59. doi: 10.1377/hlthaff.14.3.147
2. Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. (2011) 378:1515–25. doi: 10.1016/S0140-6736(11)60827-1
3. Hossain MM, Purohit N. Improving child and adolescent mental health in India: Status, services, policies, and way forward. Indian J Psychiatry. (2019) 61:415. doi: 10.4103/psychiatry.IndianJPsychiatry_217_18
4. Patel V, Kieling C, Maulik PK, Divan G. Improving access to care for children with mental disorders: a global perspective. Arch Dis Child. (2013) 98:323–7. doi: 10.1136/archdischild-2012-302079
5. Belkin G, Wissow L, Lund C, Aber L, Bhutta Z, Black M, et al. Converging on child mental health–toward shared global action for child development. Glob Ment Health. (2017) 4:e20. doi: 10.1017/gmh.2017.13
6. Van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera S, Pian J, et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low-and middle-income countries. Cochrane Database Syst Rev. (2013) 11:CD009149. doi: 10.1002/14651858.CD009149.pub2
7. Fazel M, Patel V, Thomas S, Tol W. Mental health interventions in schools in low-income and middle-income countries. The Lancet Psychiatry. (2014) 1:388–98. doi: 10.1016/S2215-0366(14)70357-8
8. Reinke WM, Stormont M, Herman KC, Puri R, Goel N. Supporting children's mental health in schools: Teacher perceptions of needs, roles, and barriers. School Psychology Quarterly. (2011) 26:1. doi: 10.1037/a0022714
9. Dorsey S, Gray CL, Wasonga AI, Amanya C, Weiner BJ, Belden CM, et al. Advancing successful implementation of task-shifted mental health care in low-resource settings (BASIC): Protocol for a stepped wedge cluster randomized trial. BMC Psychiatry. (2020) 20:1–14. doi: 10.1186/s12888-019-2364-4
10. Das JK, Salam RA, Lassi ZS, Khan MN, Mahmood W, Patel V, et al. Interventions for adolescent mental health: an overview of systematic reviews. J Adolesc Health. (2016) 59:S49–60. doi: 10.1016/j.jadohealth.2016.06.020
11. Huang K-Y, Nakigudde J, Rhule D, Gumikiriza-Onoria JL, Abura G, Kolawole B, et al. Transportability of an evidence-based early childhood intervention in a low-income African country: results of a cluster randomized controlled study. Prevent Sci. (2017) 18:964–75. doi: 10.1007/s11121-017-0822-0
12. Adhikari RP, Upadhaya N, Satinsky EN, Burkey MD, Kohrt BA, Jordans MJ. Feasibility study of a family-and school-based intervention for child behavior problems in Nepal. Child Adolesc Psychiatry Ment Health. (2018) 12:20. doi: 10.1186/s13034-018-0226-3
13. Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, et al. Challenges and opportunities in global mental health: a research-to-practice perspective. Curr Psychiatry Rep. (2017) 19:28. doi: 10.1007/s11920-017-0780-z
14. Rivet-Duval E, Heriot S, Hunt C. Preventing adolescent depression in Mauritius: A universal school-based program. Child Adolesc Ment Health. (2011) 16:86–91. doi: 10.1111/j.1475-3588.2010.00584.x
15. Harnett PH, Dadds MR. Training school personnel to implement a universal school-based prevention of depression program under real-world conditions. J Sch Psychol. (2004) 42:343–57. doi: 10.1016/j.jsp.2004.06.004
16. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
17. Rojas-Andrade R, Bahamondes LL. Is implementation fidelity important? A systematic review on school-based mental health programs. Contemp Sch Psychol. (2019) 23:339–50. doi: 10.1007/s40688-018-0175-0
18. O'Brien E, Dukpa C, Vanderburg J. Teachers as Agents of Change: School-Based Mental Health Care in the Darjeeling Himalaya. Mumbai, India: ReFrame: The Mariwala Health Initiative Journal September. (2020).
19. Matergia M, Ferrarone P, Khan Y, Matergia DW, Giri P, Thapa S, et al. Lay Field-worker–led school health program for primary schools in low-and middle-income countries. Pediatrics. (2019) 143:e20180975. doi: 10.1542/peds.2018-0975
20. Muralidharan K, Kremer M. Public and private schools in rural India. Cambridge, MA: Harvard University, Department of Economics. (2006).
21. Cruz CM, Lamb MM, Hampanda K, Giri P, Campbell M, Chowdhury B, et al. Teacher nomination of school-aged children for mental health services in a low and middle income country. Glob Health Action. (2021) 14:1861921. doi: 10.1080/16549716.2020.1861921
22. Cruz CM, Matergia M, Lamb MM, Campbell MR, Hampanda K, Giri P, et al. 3. 56 teachers identifying children's mental illness in a task-shifting intervention in India. J Am Acad Child Adolesc Psychiatry. (2019) 58:S213. doi: 10.1016/j.jaac.2019.08.219
23. Das PP, Grover S, Avasthi A, Chakrabarti S, Malhotra S, Kumar S. Intentional self-harm seen in psychiatric referrals in a tertiary care hospital. Indian J Psychiatry. (2008) 50:187. doi: 10.4103/0019-5545.43633
24. Bharati S, Mallik S, Datta PP, Mukhopadhyay A, Datta D, Haq S. Socio-demographic profile and suicidal intent of attempted suicide cases: a hospital based study in West Bengal, India. Hindu. (2013) 135:86.5.
25. McEvoy PM, Nathan P, Norton PJ. Efficacy of transdiagnostic treatments: A review of published outcome studies and future research directions. J Cogn Psychother. (2009) 23:20–33. doi: 10.1891/0889-8391.23.1.20
26. Knell SM. Cognitive-Behavioral Play Therapy. Maryland, MD: Rowman and Littlefield Publishers (1993).
27. Fazio-Griffith LJ, Ballard MB. Cognitive behavioral play therapy techniques in school-based group counseling: Assisting students in the development of social skills. Vistas online. (2014) 18:1–14.
28. Han SS, Weiss B. Sustainability of teacher implementation of school-based mental health programs. J Abnorm Child Psychol. (2005) 33:665–79. doi: 10.1007/s10802-005-7646-2
29. Amodio DM, Master SL, Yee CM, Taylor SE. Neurocognitive components of the behavioral inhibition and activation systems: Implications for theories of self-regulation. Psychophysiology. (2008) 45:11–9.
30. McClelland MM, Cameron CE, Wanless SB, Murray A. Executive function, behavioral self-regulation, and social-emotional competence. Contemp Perspectives Social Learn Early Childhood Educ. (2007) 1:113–37.
31. Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control? Clin Psychol Rev. (1998) 18:23–45. doi: 10.1016/S0272-7358(97)00043-3
32. Cruz CM, Lamb MM, Giri P, Vanderburg J, Ferrarone P, Bhattarai S, et al. Perceptions, attitudes, and knowledge of teachers serving as mental health lay counselors in a low and middle income country: a mixed methods pragmatic pilot study. Int J Ment Health Syst. (2021) 15:1–16. doi: 10.1186/s13033-021-00453-3
33. Knutson N, Forgatch M, Rains L. Fidelity of Implementation Rating System (FIMP): The Training Manual for PMTO. Eugene: Oregon Social Learning Center. (2003).
34. Forgatch MS, Patterson GR, DeGarmo DS. Evaluating fidelity: Predictive validity for a measure of competent adherence to the Oregon model of parent management training. Behav Ther. (2005) 36:3–13. doi: 10.1016/S0005-7894(05)80049-8
35. de Vet R, Lako DA, Beijersbergen MD, van den Dries L, Conover S, van Hemert AM, et al. Critical time intervention for people leaving shelters in the Netherlands: assessing fidelity and exploring facilitators and barriers. Adm Policy Ment Health. (2017) 44:67–80. doi: 10.1007/s10488-015-0699-9
36. Achenbach TM. Manual for the Teacher's Report Form and 1991 Profile. Vermont, VT: University of Vermont (1991).
37. Shenoy J, Kapur M, Kaliaperumal V. Psychological disturbance among 5-to 8-year-old school children: a study from India. Soc Psychiatry Psychiatr Epidemiol. (1998) 33:66–73. doi: 10.1007/s001270050024
38. Leung PW, Wong MM. Measures of child and adolescent psychopathology in Asia. Psychol Assess. (2003) 15:268. doi: 10.1037/1040-3590.15.3.268
39. Rescorla L, Ivanova MY, Achenbach TM, Begovac I, Chahed M, Drugli MB, et al. International epidemiology of child and adolescent psychopathology II: integration and applications of dimensional findings from 44 societies. J Am Acad Child Adolesc Psychiatry. (2012) 51:1273–83. e8. doi: 10.1016/j.jaac.2012.09.012
41. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. (2000) 23. doi: 10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G
42. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. (2008) 62:107–15. doi: 10.1111/j.1365-2648.2007.04569.x
44. NVivo. Nvivo Qualitative Data Analysis Software. 8th ed. Melbourne, MB: QSR International Pty Ltd. (2008).
45. Del Mauro JM, Williams DJ. Children and adolescents' attitudes toward seeking help from professional mental health providers. Int J Adv Couns. (2013) 35:120–38. doi: 10.1007/s10447-012-9172-6
46. Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med. (2013) 97:82–6. doi: 10.1016/j.socscimed.2013.08.004
47. Moir T editor Why is implementation science important for intervention design and evaluation within educational settings? Front Educat. (2018). Frontiers. doi: 10.3389/feduc.2018.00061
48. Stirman SW, Miller CJ, Toder K, Calloway A. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implementation Science. (2013) 8:65. doi: 10.1186/1748-5908-8-65
49. Fisher CW, Berliner DC, Filby NN, Marliave R, Cahen LS, Dishaw MM. Teaching behaviors, academic learning time, and student achievement: An overview. J Classroom Interaction. (1981) 17:2–15.
50. Andrade AR, Lambert EW, Bickman L. Dose effect in child psychotherapy: Outcomes associated with negligible treatment. J Am Acad Child Adolesc Psychiatry. (2000) 39:161–8. doi: 10.1097/00004583-200002000-00014
51. Bickman L, Andrade AR, Lambert EW. Dose response in child and adolescent mental health services. Ment Health Serv Res. (2002) 4:57–70. doi: 10.1023/A:1015210332175
52. Landrum TJ, Tankersley M, Kauffman JM. What is special about special education for students with emotional or behavioral disorders? J Spec Educ. (2003) 37:148–56. doi: 10.1177/00224669030370030401
53. Özler B, Fernald LC, Kariger P, McConnell C, Neuman M, Fraga E. Combining pre-school teacher training with parenting education: a cluster-randomized controlled trial. J Dev Econ. (2018) 133:448–67.
54. Yoshikawa H, Leyva D, Snow CE, Treviño E, Barata M, Weiland C, et al. Experimental impacts of a teacher professional development program in Chile on preschool classroom quality and child outcomes. Dev Psychol. (2015) 51:309. doi: 10.1037/a0038785
55. Barnett AG, Van Der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. (2005) 34:215–20.
56. Richter D, Kunter M, Klusmann U, Lüdtke O, Baumert J. Professional development across the teaching career: Teachers' uptake of formal and informal learning opportunities. Teach Teach Educ. (2011) 27:116–26. doi: 10.1016/j.tate.2010.07.008
Keywords: teacher, task-shifting, child mental health, feasibility, fidelity, global mental health, school mental health, education as mental health therapy
Citation: Cruz CM, Giri P, Vanderburg JL, Ferrarone P, Bhattarai S, Giardina AA, Gaynes BN, Hampanda K, Lamb MM and Matergia M (2021) The Potential Emergence of “Education as Mental Health Therapy” as a Feasible Form of Teacher-Delivered Child Mental Health Care in a Low and Middle Income Country: A Mixed Methods Pragmatic Pilot Study. Front. Psychiatry 12:790536. doi: 10.3389/fpsyt.2021.790536
Received: 06 October 2021; Accepted: 15 November 2021;
Published: 16 December 2021.
Edited by:
Marinos Kyriakopoulos, King's College London, United KingdomReviewed by:
Sophie Bennett, University College London, United KingdomJean Lillian Paul, Medizinische Universität Innsbruck, Austria
Copyright © 2021 Cruz, Giri, Vanderburg, Ferrarone, Bhattarai, Giardina, Gaynes, Hampanda, Lamb and Matergia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christina M. Cruz, christina_cruz@med.unc.edu; Michael Matergia, michael.matergia@cuanschutz.edu
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
 Christina M. Cruz
Christina M. Cruz