- 1Department of Medicine, Surgery and Dentistry “Scuola Medica Salernitana”, University of Salerno, Salerno, Italy
- 2Department of Neuroscience, Eating Disorders Center for Treatment and Research, University of Turin, Turin, Italy
- 3Unit of Psychiatry, DAME, University of Udine, Udine, Italy
- 4Department of Mental Health, ASST Santi Paolo e Carlo, Milan, Italy
- 5Section of Psychiatry, Department of Medical Sciences and Public Health, University of Cagliari, Cagliari, Italy
- 6Department of Mental Health, Asl Salerno, Salerno, Italy
- 7Department of Neuroscience, University of Padova, Padua, Italy
- 8Mental Health Department, Center for the Treatment and Research on Eating Disorders, ASL Lecce, Lecce, Italy
- 9Psychiatry Unit, Department of Neurological and Psychiatric Sciences, University of Florence, Florence, Italy
- 10Eating Disorders Centre Portogruaro, AULSS 4 Veneto Orientale, San Donà di Piave, Italy
- 11Department of Medical and Surgical Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy
- 12Eating Disorders Unit, Casa di Cura “Villa Margherita”, Arcugnano, Italy
- 13Section of Clinical Psychiatry, Department of Clinical Neurosciences/DIMSC, Università Politecnica delle Marche, Ancona, Italy
- 14Department of Translational Medicine, Psychiatry Institute, Università del Piemonte Orientale, Novara, Italy
- 15Department of Psychiatry, University of Campania L. Vanvitelli, Naples, Italy
The negative impact of COVID-19 pandemic on people with Eating Disorders (EDs) has been documented. The aim of this study was to evaluate whether a history of traumatic experiences during childhood or adolescence was associated with a higher degree of psychopathological worsening during COVID-19 related lockdown and in the following re-opening period in this group of people. People with EDs undergoing a specialist ED treatment in different Italian services before the spreading of COVID-19 pandemic (n = 312) filled in an online survey to retrospectively evaluate ED specific and general psychopathology changes after COVID-19 quarantine. Based on the presence of self-reported traumatic experiences, the participants were split into three groups: patients with EDs and no traumatic experiences, patients with EDs and childhood traumatic experiences, patients with EDs and adolescent traumatic experiences. Both people with or without early traumatic experiences reported retrospectively a worsening of general and ED-specific psychopathology during the COVID 19-induced lockdown and in the following re-opening period. Compared to ED participants without early traumatic experiences, those with a self-reported history of early traumatic experiences reported heightened anxious and post-traumatic stress symptoms, ineffectiveness, body dissatisfaction, and purging behaviors. These differences were seen before COVID-19 related restrictions as well as during the lockdown period and after the easing of COVID-19 related restrictions. In line with the “maltreated ecophenotype” theory, these results may suggest a clinical vulnerability of maltreated people with EDs leading to a greater severity in both general and ED-specific symptomatology experienced during the exposure to the COVID-19 pandemic.
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic was devastating and led countries around the world to adopt social and physical distancing to contain virus transmission (1). Closures and restrictions worldwide promoted social isolation and loneliness (2–7). Increased exposition to the Internet and social media messages contributed to the fear of being infected (8–12). As a result of such a stressful situation, a clear-cut increased prevalence of anxiety and depression occurred in the general population (13–25), while people with a pre-existing psychiatric condition showed a heightened vulnerability in terms of physical and mental distress (26–31) as well as a higher frequency of most severe outcomes of the infection (32, 33), emphasizing the need to involve psychiatrists in the management of the emergency (34–41).
Among vulnerable psychiatric patients, people with eating disorders (EDs) have been reported to experience a worsening of their specific psychopathology, although variability in the degree of worsening has been observed across the studies (42–53). Furthermore, a marked impairment in general psychopathological symptoms has been observed in these patients, which tended to persist after the easing of COVID-19 related restrictions (54, 55). Several factors, such as social isolation, family conflict, disruption in routine activities, and everyday life, heightened exposure to ED-specific media messages and fear of contagion, may have contributed to the vulnerability of people with EDs to the impact of COVID-19 pandemic (50, 56).
Traumatic experiences during development have been acknowledged as important risk factors for several psychiatric disorders (57), including EDs (58). Clinical features (for instance, in terms of age at onset of the disorder and psychiatric comorbidity) as well as the identification of specific biological markers in patients with childhood maltreatment led Teicher and Samson (57) to suggest the existence across individuals suffering from a psychiatric condition of a “maltreated ecophenotype” subgroup with possibly different clinical presentation, biological underpinning, and prognosis. This perspective offers a functional understanding of symptoms highlighting their developmental influences (59).
In accordance with this hypothesis, people with EDs and a history of childhood maltreatment have been reported to show an earlier age at symptom onset, a greater symptom severity and a more frequent concomitance of other psychiatric conditions (60), a poorer treatment response (61), as well as a heightened biological and emotional vulnerability to acute social stress exposure (62) and specific gray and white matter alterations (63), highlighting the need of a multidisciplinary approach to their management (64).
As the COVID-19 pandemic encompasses different types of stressors, ranging from family and social to health and economic adversities, it may provide the opportunity to explore in vivo the effects of an acute traumatic event in people with a potential vulnerability to acute stressors (65–68). According to the maltreated ecophenotype hypothesis, an increased vulnerability to the pandemic distress may be hypothesized in people with EDs and a history of early maltreatment. Thus, the aim of this study was to evaluate whether a history of traumatic experiences during childhood or adolescence was associated with a higher degree of psychopathological worsening during COVID-19 related lockdown and in the following re-opening period.
We conducted a secondary analysis of data obtained through an online survey filled in by Italian participants with EDs after the easing of lockdown measures (54). We hypothesized that people with EDs and history of early traumatic experiences would exhibit greater worsening of general and ED-related psychopathology during the COVID-19 lockdown and the following re-opening compared to people without early exposure to adverse experiences.
Materials and Methods
Participants
Patients previously admitted to specialist ED units located in different regions of Italy and diagnosed with anorexia nervosa (AN), atypical AN, bulimia nervosa (BN), binge-eating disorder (BED), and other specified feeding or eating disorders (OSFED) according to the DSM-5 criteria were asked to fill in an anonymous online survey. The diagnosis was made by expert psychiatrists through face-to-face clinical interviews at admission. Participants had to meet the following inclusion criteria: (a) no comorbid schizophrenia or bipolar disorder; (b) no intellectual disability; (c) absence of physical comorbidity not related to the ED. Participants were invited to participate in the survey during a 20-day period from 1st June 2020 up to and including 21st June 2020. The local ethical committee communicated us that, in line with local legislation and national guidelines, the completion of an anonymous online survey did not require their approval. The consent was to be considered implicit when participants accepted to fill in the survey.
Study Design and Measures
The online survey included a broad range of items aimed to assess the impact of the COVID-19 pandemic on the mental health of people with EDs.
Participants were asked to report their age, gender identity, geographic location (Italian Region), duration of illness, and undergoing treatments. Four different survey data collectors (one for each main ED diagnosis) were created. Each local investigator sent to the patients of her/his ED unit an email including a hyper-link to the survey from data collectors of the corresponding diagnosis and received completion feedback from patients.
The survey included a range of quantitative questions regarding both general and ED-specific psychopathology and it took ~20 min to be completed. Explored dimensions were anxiety, depression, post-traumatic stress symptoms (PTSS), obsessive-compulsive symptoms (OCS), panic symptoms, insomnia, suicide ideation. Questions related to these dimensions were adapted from the following questionnaires: Generalized Anxiety Disorder 7 (69), Patient Health Questionnaire 9 (70), PTSD Checklist for DSM-5 (71), and Obsessive-Compulsive Inventory (72). Items included were selected as the most consistent with the DSM-5 criteria for each psychiatric disorder. Questions specifically related to EDs psychopathology and behaviors included in the survey were adapted from the Eating Disorders Inventory [EDI-2; (73)]. The selected questions were representative of each EDI-2 subscale. Moreover, participants were asked to account for the use of laxatives and diuretics and the level of physical activity, which were reported as episode/week and hours/day, respectively.
Questions referred to three different time periods: 2 weeks before the spread of COVID-19 emergency; the lockdown period or “Phase 1” (that in Italy covered the months of March and April 2020); 2 weeks after the end of lockdown or “Phase 2” (that in Italy started on May 4, 2020). Each general psychopathology item was rated on a 10-point scale (0: not at all, 10: maximum), while ED specific items were rated on a 6-point scale, which was consistent with the original version of the EDI-2.
Participants were also asked if they had suffered any kind of traumatic experience such as sexual, physical, or emotional abuse or physical or emotional neglect (e.g., my family said hurtful things, I got hit badly enough to be noticed, I was sexually abused, I did not feel loved, I didn't have enough to eat), and if so if they had suffered it in childhood (up to the age of 10) or adolescence (age between 11 and 18 years). Based on the history of traumatic experiences, the participants were split into three groups: patients with EDs and no traumatic experiences, patients with EDs and childhood traumatic experiences, and patients with EDs and adolescent traumatic experiences.
Statistical Analysis
Statistical analyses were performed using JASP software (2020). Analysis of variance (ANOVA) was performed to test significant differences among groups in demographic and clinical variables. ANOVA with repeated measures and self-report traumatic experience as between-subject factors and post-hoc Tukey's test were performed. Greenhouse-Geisser sphericity correction was applied where appropriate. Demographic variables that differed among groups were added as covariates in the analyses. A statistical threshold of p < 0.05 was set as significant.
Results
Clinical and Demographic Characteristics
Clinical and demographic characteristics of the whole sample and changes in general psychopathological dimensions over the three explored time periods are reported in Monteleone et al. (54).
Based on the self-reported traumatic experience, 91 participants were included in the group without traumatic experience (noMal), 119 participants in the group with a self-reported traumatic experience during childhood (childMal), and 102 participants in the group with a self-reported traumatic experience during adolescence (adoMal). The diagnostic composition of the sample was the following: 179 participants (57.4%) had a current AN or atypical AN, 63 (20.2%) had a current BN, 48 (15.4%) had a current BED, 22 (7.05%) had a current OSFED. No statistically significant difference emerged in the diagnostic composition of the three groups (χ2 = 5.29, p = 0.51). The groups differed in age and self-reported illness duration [F(2,309) = 3.38, p = 0.03 and F(2,309) = 4.12, p = 0.02, respectively], but not in body mass index (BMI) and treatment duration [F(2,309) = 0.09, p = 0.91 and F(2,309) = 2.19, p = 0.11, respectively] (Table 1). Post-hoc Tukey's test revealed that noMal participants had an older age than adoMal participants (t = 2.58, p = 0.03) while childMal participants had a longer illness duration than adoMal participants (t = 2.85, p = 0.01). Therefore, age and treatment duration were entered as covariates in the ANOVA with repeated measures.
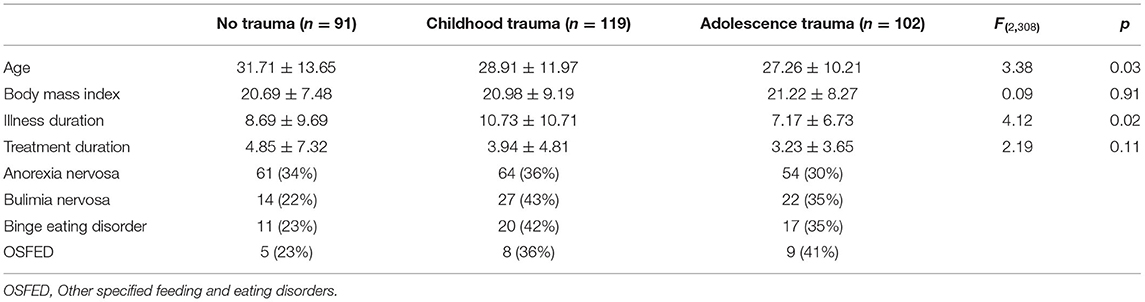
Table 1. Demographic characteristics of participants according to self-reported traumatic experiences.
General Psychopathology
Two way ANOVA with repeated measures showed a significant effect of time for symptoms of anxiety [F(2,614) = 12.27, p = 5.93 × 10−6], depression [F(2,614) = 4.19, p = 0.01], PTSS [F(1.95,599.16) = 6.16, p = 0.002], panic [F(2,614) = 3.41, p = 0.03], insomnia [F(2,614) = 3.72, p = 0.02], suicide ideation [F(1.87, 573.74) = 6.08, p = 0.003], but not for OCS [F(1.57,480.1) = 1.13, p = 0.31]. Indeed, compared to the pre-pandemic phase all but OCS scores were significantly higher after the start of COVID-19 related restrictions (Figure 1).
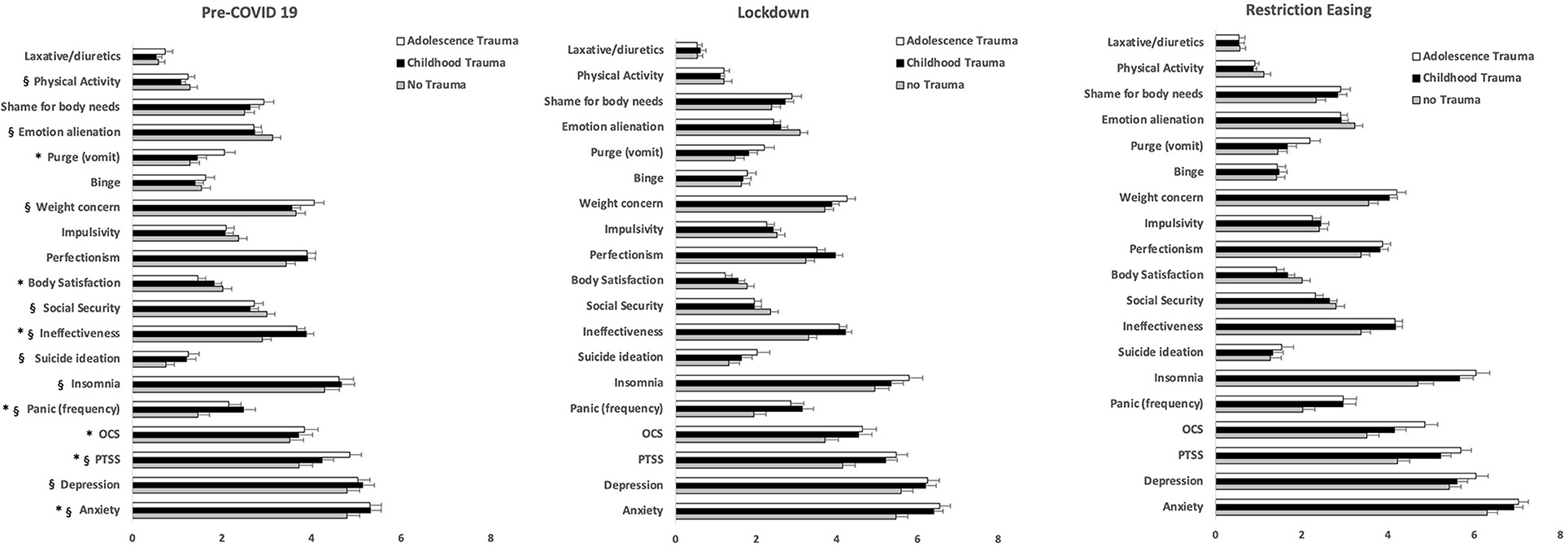
Figure 1. Scores of self-reported general and specific psychopathology and symptoms in participants with eating disorders according to self-reported history of early traumatic experiences. OCS, obsessive-compulsive symptoms; PTSS, post-traumatic stress symptoms. *Group effect: p < 0.05; §time effect: p < 0.05.
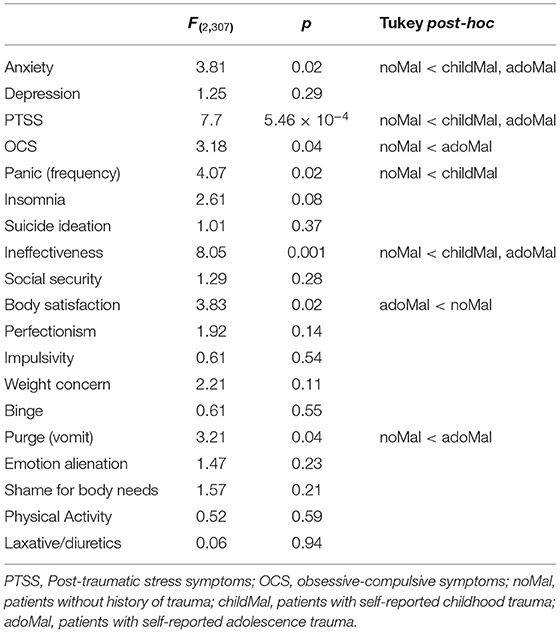
Between-group comparisons and post-hoc Tukey's test are summarized in Table 2.
Post-hoc Tukey's tests showed that anxiety and PTSS scores were significantly lower in noMal participants compared to both childMal (t = 2.54, p = 0.03 for anxiety and t = 2.44, p = 0.03 for PTSS) and adoMal groups (t = 2.29, p = 0.04 for anxiety and t = 3.91, p < 0.01 for PTSS), while OCS were significantly lower in noMal participants than in adoMal group (t = 2.52, p = 0.03) and panic was significantly lower in noMal participants than in childMal ones (t = 2.73, p = 0.02).
No significant time X group interaction emerged from the analyses. Participants' age and illness duration did not affect significantly these results with the exception for a marginal effect of age on OCS [F(1,307) = 4.51, p = 0.04].
ED-Related Psychopathology
Two way ANOVA with repeated measures showed a significant effect of time for ineffectiveness [F(2,614) = 7.33, p = 0.001], social security [F(2,614) = 9.57, p = 0.001], weight concern [F(1.8,569.15) = 5.55, p = 0.005], emotional alienation [F(2,614) = 8.35, p = 0.001], and physical activity [F(1.9,588.45) = 5.23, p = 0.006], but not for body satisfaction [F(1.76,541.93) = 1.12, p = 0.32], perfectionism [F(2,614) = 0.25, p = 0.77], impulsivity [F(2,614) = 1.26, p = 0.28], binge [F(2,614) = 2.70, p = 0.07], purge-vomit [F(2,614) = 2.19, p = 0.11], shame of body needs [F(1.89,580.5) = 0.71, p = 0.49], and laxative/diuretics abuse [F(1.7, 521.4) = 0.36, p = 0.66], demonstrating that, compared to the pre-pandemic period, these symptoms were significantly more severe after the beginning of COVID-19 related restrictions (Figure 1). Between-group comparisons and post-hoc Tukey's test are summarized in Table 2. Post-hoc Tukey's tests showed that ineffectiveness was lower in noMal participants compared to both childMal (t = 3.67, p < 0.01) and adoMal groups (t = 3.37, p < 0.01), while body satisfaction was lower in adoMal group than in noMal group (t = 2.69, p = 0.02) and purge-vomit was lower in noMal group than in adoMal group (t = 2.69, p = 0.04).
No significant time X group interaction emerged from the analyses. Participants' age and illness duration did not affect significantly these results except for the effects of age on binge [F(1,307) = 12.15, p = 0.001], emotional alienation [F(1,307) = 13.69, p = 0.001] and laxative/diuretics abuse [F(1,307) = 5.00, p = 0.02] and the effect of illness duration on emotional alienation [F(1,307) = 10.15, p = 0.002].
Discussion
The present study investigated changes in general and specific psychopathology during the COVID-19 related restrictions and in the following re-opening period in a large population of Italian patients with EDs with or without a history of early traumatic experiences.
Compared to the pre-pandemic phase, both people with or without exposure to early traumatic experiences reported a worsening of general and ED-specific psychopathology during the COVID 19-induced lockdown and in the following re-opening period. Perceived social isolation, forced cohabitation and heightened family conflict, disruption in routine activities and everyday life, heightened exposure to social media messages, and fear of contagion, may have contributed to the vulnerability of people with EDs to the impact of COVID-19 pandemic (50, 56). In line with our study hypothesis, participants with EDs and a history of early traumatic experiences showed higher scores in general and ED-related psychopathology in the pre-pandemic period, during the pandemic-induced lockdown and in the following re-opening period compared to participants with EDs without early traumatic experiences. To our knowledge, only one previous study (51) investigated the effect of childhood maltreatment on the psychopathology course during the COVID-19 related lockdown. The authors found that childhood trauma significantly predicted COVID-19-related post-traumatic symptomatology in patients with AN. In line with these data, we observed significantly higher PTS scores in our population of participants with mixed ED diagnoses and history of early traumatic experiences. Furthermore, compared to participants with EDs without trauma history, people with EDs and history of childhood or adolescent traumatic experiences reported higher levels of anxiety, panic, and OCS also in the pre-pandemic period. These data are in line with research findings demonstrating that a greater symptoms severity characterize people with EDs and history of early traumatic experiences (60) and support the existence of a “maltreated ecophenotype” clinically different from non-maltreated patients (57).
The present data were collected during a traumatic event which included many kinds of stressors such as social isolation, impairment in the family, and/or individual's economic condition and fear of being infected. Therefore, the increased severity of anxious symptoms observed in maltreated patients with EDs is also consistent with recent experimental research (62), which hypothesized a biological and emotional vulnerability to stressful events in this subgroup of people with EDs. Previous studies identified an altered emotion regulation and cognitive bias toward social negative stimuli in people with EDs and early adverse experiences (74, 75). Thus, heightened rejection sensitivity and emotion regulation difficulties promoted by early traumatic experiences may contribute to explain the association of these experiences with a more severe psychopathology. This is also in line with the research evidence supporting the central role of affect regulation for mental health (76).
Surprisingly, people with EDs and a history of early traumatic experiences did not differ in depression, insomnia, or suicidal ideation from those without childhood adverse experiences. This may point to an increased vulnerability of maltreated people with EDs to anxiety symptoms rather than to depressive ones and/or may indicate that the COVID-19 pandemic may exacerbate one type of symptoms more than others, although these hypotheses remain speculative. However, depressive symptoms have been found to be worsened during the lockdown in all people with EDs, suggesting the need for clinicians to address them with ad hoc interventions (77).
As for ED-specific psychopathology, participants with early traumatic experiences reported heightened levels of ineffectiveness, body dissatisfaction, and purging behavior (namely, self-induced vomiting). These results are in line with previous research data. Indeed, low self-esteem and ineffectiveness have been proposed as possible mediators between childhood maltreatment and ED-specific symptoms (78–82). In addition, some studies (83, 84) have reported that a more severe purging behavior may be promoted by the need to regulate trauma-induced negative emotions by engaging in rash actions and risky behaviors. Finally, an association between childhood maltreatment and body dissatisfaction in adulthood has been reported in both community samples (85) and people with EDs (66, 86).
Other ED specific psychopathological variables (social security, perfectionism, impulsivity, weight concern, binge eating, shame of body needs, physical activity, and laxative/diuretics abuse) did not differ between participants with and without history of early maltreatment. In a previous analysis (54), these psychopathological variables worsened during the COVID-19 lockdown but, differently from general psychopatholgical symptoms, they returned to pre-pandemic levels in the re-opening period. This could be related to the fact that the easing of COVID-19 related restrictions could not mean real changes in the everyday life conditions, even if the survey was taken during June 2020 when the daily number of COVID-19 cases has dropped significantly in Italy. In the light of the high pre-pandemic symptom levels in people with EDs, we suggest that the observed lack of differences in those ED-related psychopathological variables between maltreated and non-maltreated people with EDs may be explained by a sort of ceiling effect, which hides a higher vulnerability in maltreated people with ED. Since for patients with EDs and history of early adverse experiences social situations could be stressful (62), this hypothesis can also be aligned with the observed lack of difference in the reactivity (e.g., time × group effect) of maltreated people with EDs to the pandemic restrictions as well as to the easing of COVID-19 related restrictions: the higher pre-pandemic levels of psychopathology seen in maltreated people with EDs may persist, hiding a different reactivity.
Remarkably, the age at the trauma occurrence (e.g., childhood or adolescence) did not contribute to the psychopathological differences observed in maltreated people with EDs. Previous studies have suggested that the time of the trauma occurrence may promote different biological sequelae (57), although no data have confirmed this hypothesis from a clinical perspective in EDs. However, the retrospective nature of our assessment may affect this finding, suggesting that further research is needed to explore this issue.
From a clinical perspective, these findings confirm the need to systematically assess the presence of adverse traumatic experiences in patients with EDs and to therapeutically address the ability to adapt to and face adversities (87, 88), likely impaired in this subgroup of patients with EDs. This may promote more personalized psychotherapeutic approaches (89–93), possibly allowing to overcome treatment resistance (94, 95). The widespread implementation of Internet-delivered psychological treatments (96–99), associated with the relatively positive attitudes toward e-therapies in people with eating problems (100), may be a way to increase access to psychological treatment for people with EDs. Finally, the important role of general psychopathological symptoms in maltreated people with EDs may support the transdiagnostic perspective recently proposed (101, 102) for the treatment of various emotional disorders.
Some limitations of the present study need to be acknowledged. First, the retrospective design of our assessment does not allow to exclude recall biases. Indeed, early traumatic experiences were retrospective and self-reported: however, this is the most common methodology of early trauma data collection in EDs (103). Moreover, the survey was proposed and retrieved clinicians who were following the participants with EDs, which might lead to a bias on reporting traumatic experiences. Regarding psychopathology assessment, the short duration of time that elapsed between the beginning of COVID-19 outbreak and data collection partially reduced this bias. Second, in line with the transdiagnostic ED perspective (104, 105) and with experimentally shown lack of differences among different ED diagnoses in the symptom response to stress exposure (62), we did not account for possible differences between the main (AN, BN, BED and OSFED) ED diagnoses. This area needs to be addressed by future studies. Moreover, the methodology of data collection may have affected the study findings, and the use of a new online survey may also underpin aspects of subjectivity. However, since we built the survey by adopting questions from validated psychometric questionnaires, we are confident that this limitation had a slight impact on our findings, although we cannot completely rule out this bias. The relatively small sample size, in particular the low number of participants with ED diagnosis other than AN, and the self-reported illness duration may affect the generalizability of our results. Finally, the cross-sectional design does not allow to make causal interpretations.
Conclusions
People with EDs and history of early traumatic experiences reported heightened anxious and PTS symptoms, ineffectiveness, body dissatisfaction, and purging behaviors than those without early adverse experiences, regardless of the age when trauma occurred. These differences were seen before COVID-19 related restrictions as well as during the lockdown period and after the easing of COVID-19 related restrictions. In line with the “maltreated ecophenotype” theory, it is possible to hypothesize a vulnerability of maltreated people with EDs, leading to a greater severity in both general and ED-specific symptomatology experienced during the exposure to the stressful lockdown related to the COVID-19 pandemic. The persistence of this detrimental effect in the following re-opening period may suggest either a slower recover or a heightened sensitivity to the restoring social exposure in this patient subgroup.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
AM, FM, GCa, and PM designed the study, wrote the protocol, and wrote the manuscript. GA-D, MB, SB, BC, GCo, AF, CR, VR, PS, CS-G, PT, UV, and PZ collected data. GCa did statistical analyses. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Int Med. (2020) 180:817–8. doi: 10.1001/jamainternmed.2020.1562
3. Saltzman LY, Hansel CH, Bordnick PS. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol Trauma. (2020) 12:S55–7. doi: 10.1037/tra0000703
4. Shan Wong SY, Zhang D, Shan Sit RW, Kei Yip BH, Chung RYN, Man Wong CK, et al. Impact of COVID-19 on loneliness, mental health, and health service utilization: a prospective cohort study of older adults with multimorbidity in primary care. Br J Gen Pract. (2020) 70:E817–24. doi: 10.3399/bjgp20X713021
5. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. (2020) 5:E256. doi: 10.1016/S2468-2667(20)30061-X
6. Rooksby M, Furuhashi T, McLeod HJ. Hikikomori: a hidden mental health need following the COVID-19 pandemic. World Psychiatry. (2020) 19:399–400. doi: 10.1002/wps.20804
7. Creese B, Khan Z, Henley W, O'Dwyer S, Corbett A, Vasconcelos Da Silva M, et al. Loneliness, physical activity and mental health during Covid-19: a longitudinal analysis of depression and anxiety in adults over 50 between 2015 and 2020. Int Psychogeriatr. (2021) 33:505–14. doi: 10.1017/S1041610220004135
9. Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J Anxiety Disord. (2020) 74:102258. doi: 10.1016/j.janxdis.2020.102258
10. Rodríguez-Hidalgo AJ, Pantaleón Y, Dios I, Falla D. Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front Psychol. (2020) 11:591797. doi: 10.3389/fpsyg.2020.591797
11. Luo F, Ghanei Gheshlagh R, Dalvand S, Saedmoucheshi S, Li Q. Systematic review and meta-analysis of fear of COVID-19. Front Psychol. (2021) 12:661078. doi: 10.3389/fpsyg.2021.661078
12. Quadros S, Garg S, Ranjan R, Vijayasarathi G, Mamun MA. Fear of COVID 19 infection across different cohorts: a scoping review. Front Psychiatry. (2021) 12:708430. doi: 10.3389/fpsyt.2021.708430
13. Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. (2021) 296:567–76. doi: 10.1016/j.jad.2021.09.098
14. Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. (2020) 19:249–50. doi: 10.1002/wps.20758
15. Daly M, Sutin A, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. (2020) 1–10. doi: 10.1017/S0033291720004432. [Epub ahead of print].
16. van der Velden PG, Contino C, Das M, van Loon P, Bosmans MW. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J Affect Disord. (2020) 277:540–8. doi: 10.1016/j.jad.2020.08.026
17. Kwong ASF, Pearson RM, Adams MJ, Northstone K, Tilling K, Smith D, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br J Psychiatry. (2020) 1–10. doi: 10.1192/bjp.2020.242. [Epub ahead of print].
18. Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol Med. (2020) 1–10. doi: 10.1017/S003329172000241X
19. Giannopoulou I, Galinaki S, Kollintza E, Adamaki M, Kympouropoulos S, Alevyzakis E, et al. COVID-19 and post-traumatic stress disorder: The perfect 'storm' for mental health. Exp Ther Med. (2021) 22:1162. doi: 10.3892/etm.2021
20. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
21. Brown S. Perinatal mental health in the COVID-19 pandemic. World Psychiatry. (2020) 19:333–4. doi: 10.1002/wps.20779
22. Arora T, Grey I, Östlundh L, Lam KBH, Omar OM, Arnone D. The prevalence of psychological consequences of COVID-19: a systematic review and meta-analysis of observational studies. J Health Psychol. (2020) 1359105320966639. doi: 10.1177/1359105320966639. [Epub ahead of print].
23. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
24. Aknin L, De Neve J-E, Dunn E, Fancourt D, Goldberg E, Helliwell J, et al. Mental health during the first year of the COVID-19 pandemic: a review and recommendations for moving forward. Perspect Psychol Sci. (2021). doi: 10.31234/osf.io/zw93g
25. Tsamakis K, Tsiptsios D, Ouranidis A, Mueller C, Schizas D, Terniotis C, et al. COVID-19 and its consequences on mental health. Exp Ther Med. (2021) 21:244. doi: 10.3892/etm.2021.9675
26. Breaux R, Dvorsky M, Marsh N, Green C, Cash A, Shroff D. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD. J Child Psychol Psychiatry. (2021) 62:1132–9. doi: 10.1111/jcpp.13382
27. Hamm ME, Brown PJ, Karp JF, Lenard E, Cameron F, Dawdani A, et al. Experiences of American older adults with pre-existing depression during the beginnings of the COVID-19 pandemic: a multicity, mixed-methods study. Am J Geriatr Psychiatry. (2020) 28:924–32. doi: 10.1016/j.jagp.2020.06.013
28. Rutherford BR, Choi CJ, Chrisanthopolous M, Salzman C, Zhu C, Montes-Garcia C, et al. The COVID-19 pandemic as a traumatic stressor: mental health responses of older adults with chronic PTSD. Am J Geriatr Psychiatry. (2021) 29:105–14. doi: 10.1016/j.jagp.2020.10.010
29. Tanir Y, Karayagmurlu A, Kaya I, Kaynar TB, Türkmen G, Dambasan BN, et al. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. (2020) 293:113363. doi: 10.1016/j.psychres.2020.113363
30. Tsamakis K, Triantafyllis AS, Tsiptsios D, Spartalis E, Mueller C, Tsamakis C, et al. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment. Exp Ther Med. (2020) 20:159–62. doi: 10.3892/etm.2020.8671
31. Castellini G, Rossi E, Cassioli E, Sanfilippo G, Innocenti M, Gironi V, et al. A longitudinal observation of general psychopathology before the COVID-19 outbreak and during lockdown in Italy. J Psychosom Res. (2021) 141:110328. doi: 10.1016/j.jpsychores.2020.110328
32. Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. (2021) 20:124–30. doi: 10.1002/wps.20806
33. De Hert M, Mazereel V, Detraux J, Van Assche K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry. (2021) 20:54–5. doi: 10.1002/wps.20826
34. Adhanom Ghebreyesus T. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry. (2020) 19:129–30. doi: 10.1002/wps.20768
35. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMp2008017
36. Öngür D, Perlis R, Goff D. Psychiatry and COVID-19. JAMA. (2020) 324:1149–50. doi: 10.1001/jama.2020.14294
37. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. (2020) 63:e32. doi: 10.1192/j.eurpsy.2020.35
38. Marazziti D, Stahl SM. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry. (2020) 19:261. doi: 10.1002/wps.20764
39. Unützer J, Kimmel RJ, Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. (2020) 19:130–1. doi: 10.1002/wps.20766
40. Stewart DE, Appelbaum PS. COVID-19 and psychiatrists' responsibilities: a WPA position paper. World Psychiatry. (2020) 19:406–7. doi: 10.1002/wps.20803
41. Wasserman D, Iosue M, Wuestefeld A, Carli V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatry. (2020) 19:294–306. doi: 10.1002/wps.20801
42. Castellini G, Cassioli E, Rossi E, Innocenti M, Gironi V, Sanfilippo G, et al. The impact of COVID-19 epidemic on eating disorders: a longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int J Eat Disord. (2020) 53:1855–62. doi: 10.1002/eat.23368
43. Fernández-Aranda F, Munguía L, Mestre-Bach G, Steward T, Etxandi M, Baenas I, et al. COVID Isolation Eating Scale (CIES): analysis of the impact of confinement in eating disorders and obesity—a collaborative international study. Eur Eat Disord Rev. (2020) 28:871–83. doi: 10.1002/erv.2784
44. Baenas I, Caravaca-Sanz E, Granero R, Sánchéz I, Riesco N, Testa G, et al. COVID-19 and eating disorders during confinement: analysis of factors associated with resilience and aggravation of symptoms. Eur Eat Disord Rev. (2020) 28:855–63. doi: 10.1002/erv.2771
45. Branley-Bell D, Talbot C. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. J Eat Disord. (2020) 8:44. doi: 10.1186/s40337-020-00319-y
46. Giel KE, Schurr M, Zipfel S, Junne F, Schag K. Eating behaviour and symptom trajectories in patients with a history of binge eating disorder during COVID-19 pandemic. Eur Eat Disord Rev. (2021) 29:657–62. doi: 10.1002/erv.2837
47. Graell M, Morón-Nozaleda MG, Camarneiro R, Villaseñor A, Yáñez S, Muñoz R, et al. Children and adolescents with eating disorders during COVID-19 confinement: difficulties and future challenges. Eur Eat Disord Rev. (2020) 28:864–70. doi: 10.1002/erv.2763
48. Machado PPP, Pinto-Bastos A, Ramos R, Rodrigues TF, Louro E, Goncalves S, et al. Impact of COVID-19 lockdown measures on a cohort of eating disorders patients. J Eat Disord. (2020) 8:57. doi: 10.1186/s40337-020-00340-1
49. Phillipou A, Meyer D, Neill E, Tan E, Lin Toh W, Van Rheenen T, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord. (2020) 53:1158–65. doi: 10.1002/eat.23317
50. Rodgers RF, Lombardo C, Cerolini S, Franko DL, Omori M, Fuller-Tyszkiewicz M, et al. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. (2020) 53:1166–70. doi: 10.1002/eat.23318
51. Shah M, Sachdeva M, Johnston H. Eating disorders in the age of COVID-19. Psychiatry Res. (2020) 290:113122. doi: 10.1016/j.psychres.2020.113122
52. Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman TK, et al. Refuting the myth of a 'tsunami' of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol Med. (2021) 1–9. doi: 10.1017/S0033291721001665. [Epub ahead of print].
53. Sideli L, Lo Coco G, Bonfanti RC, Borsarini B, Fortunato L, Sechi C, et al. Effects of COVID-19 lockdown on eating disorders and obesity: a systematic review and meta-analysis. Eur Eat Disord Rev. (2021) 29:826–41. doi: 10.1002/erv.2861
54. Monteleone AM, Marciello F, Cascino G, Abbate-Daga G, Anselmetti S, Baiano M, et al. The impact of COVID-19 lockdown and of the following “re-opening” period on specific and general psychopathology in people with Eating Disorders: the emergent role of internalizing symptoms. J Affect Disord. (2021) 285:77–83. doi: 10.1016/j.jad.2021.02.037
55. Nisticò V, Bertelli S, Tedesco R, Anselmetti S, Priori A, Gambini O, et al. The psychological impact of COVID-19-related lockdown measures among a sample of Italian patients with eating disorders: a preliminary longitudinal study. Eat Weight Disord. (2021) 1:3. doi: 10.1007/s40519-021-01137-0
56. Monteleone AM, Cascino G, Marciello F, Abbate-Daga G, Baiano M, Balestrieri M, et al. Risk and resilience factors for specific and general psychopathology worsening in people with Eating Disorders during COVID-19 pandemic: a retrospective Italian multicentre study. Eat Weight Disord. (2021) 1:3. doi: 10.1007/s40519-020-01097-x
57. Teicher MH, Samson JA. Childhood maltreatment and psychopathology: a case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry. (2013) 170:1114–33. doi: 10.1176/appi.ajp.2013.12070957
58. Caslini M, Bartoli F, Crocamo C, Dakanalis A, Clerici M, Carrà G. Disentangling the association between child abuse and eating disorders. Psychosom Med. (2016) 78:79–90. doi: 10.1097/PSY.0000000000000233
59. Abed R, Brüne M, Wilson DR. The role of the evolutionary approach in psychiatry. World Psychiatry. (2019) 18:370–1. doi: 10.1002/wps.20688
60. Molendijk ML, Hoek HW, Brewerton TD, Elzinga BM. Childhood maltreatment and eating disorder pathology: a systematic review and dose-response meta-analysis. Psychol Med. (2017) 47:1402–16. doi: 10.1017/S0033291716003561
61. Castellini G, Lelli L, Cassioli E, Ciampi E, Zamponi F, Campone B, et al. Different outcomes, psy- chopathological features, and comorbidities in patients with eating disorders reporting childhood abuse: a 3-year follow-up study. Eur Eat Disord Rev. (2018) 26:217–29. doi: 10.1002/erv.2586
62. Monteleone AM, Cascino G, Ruzzi V, Pellegrino F, Patriciello G, Barone E, et al. Emotional traumatic experiences significantly contribute to identify a maltreated ecophenotype sub-group in eating disorders: experimental evidence. Eur Eat Disorders Rev. (2021) 29:269–80. doi: 10.1002/erv.2818
63. Monteleone AM, Monteleone P, Esposito F, Prinster A, Ruzzi V, Canna A, et al. The effects of childhood maltreatment on brain structure in adults with eating disorders. World J Biol Psychiatry. (2019) 20:301–9. doi: 10.1080/15622975.2017.1395071
64. Monteleone AM, Fernandez-Aranda F, Voderholzer U. Evidence and perspectives in eating disorders: a paradigm for a multidisciplinary approach. World Psychiatry. (2019) 18:369–70. doi: 10.1002/wps.20687
65. Monteleone AM. The impact of the COVID-19 pandemic on eating disorders: a paradigm for an emotional post-traumatic stress model of eating disorders. Eur Neuropsychopharmacol. (2021) 51:84–86. doi: 10.1016/j.euroneuro.2021.05.009
66. Feldman R. What is resilience: an affiliative neuroscience approach. World Psychiatry. (2020) 19:132–50. doi: 10.1002/wps.20729
67. Masten AS. Resilience from a developmental systems perspective. World Psychiatry. (2019) 18:101–2. doi: 10.1002/wps.20591
68. Bryant RA. Post-traumatic stress disorder: a state-of-the-art review of evidence and challenges. World Psychiatry. (2019) 18:259–69. doi: 10.1002/wps.20656
69. Spitzer RL, Kroenke K, Williams JBW, Lowe B A. brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
70. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
71. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) – Standard. Measurement Instrument. The National Center for PTSD (2013). Available online at: www.ptsd.va.gov (accesed October 1, 2021).
72. Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive-compulsive disorder scale: the obsessive-compulsive inventory. Psychol Assess. (1998) 10:206–14. doi: 10.1037/1040-3590.10.3.206
73. Rizzardi M, Trombini E, Trombini G. EDI-2: Manuale. Florence: Giunti Organizzazioni Speciali (1995).
74. Cardi V, Matteo RD, Corfield F, Treasure J. Social reward and rejection sensitivity in eating disorders: an investigation of attentional bias and early experiences. World J Biol Psychiatry. (2013) 14:622–33. doi: 10.3109/15622975.2012.665479
75. Moulton SJ, Newman E, Power K, Swanson V, Day K. Childhood trauma and eating psychopathology: a mediating role for dissociation and emotion dysregulation? Child Abuse Negl. (2015) 39:167–74. doi: 10.1016/j.chiabu.2014.07.003
76. Gross JJ, Uusberg H, Uusberg A. Mental illness and well-being: an affect regulation perspective. World Psychiatry. (2019) 18:130–9. doi: 10.1002/wps.20618
77. McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. (2020) 19:250–1. doi: 10.1002/wps.20767
78. Groleau P, Steiger H, Bruce K, Israel M, Sycz L, Ouellette AS, et al. Childhood emotional abuse and eating symptoms in bulimic disorders: An examination of possible mediating variables. Int J Eat Disord. (2012) 45:326–32. doi: 10.1002/eat.20939
79. Wolf NM, Elklit A. Child Maltreatment and Disordered Eating in Adulthood: a Mediating Role of PTSD and Self-Esteem? J Child Adolesc Trauma. (2018) 13:21–32. doi: 10.1007/s40653-018-0224-x
80. Stanghellini G. Embodiment and the Other's look in feeding and eating disorders. World Psychiatry. (2019) 18:364–5. doi: 10.1002/wps.20683
81. Monteleone AM, Cascino G, Pellegrino F, Ruzzi V, Patriciello G, Marone L, et al. The association between childhood maltreatment and eating disorder psychopathology: A mixed-model investigation. Eur Psychiatry. (2019) 61:111–8. doi: 10.1016/j.eurpsy.2019.08.002
82. Monteleone AM, Tzischinsky O, Cascino G, Alon S, Pellegrino F, Ruzzi V, et al. The connection between childhood maltreatment and eating disorder psychopathology: a network analysis study in people with bulimia nervosa and with binge eating disorder. Eat Weight Disord. (2021). doi: 10.1007/s40519-021-01169-6
83. Racine SE, VanHuysse JL, Keel PK, Burt SA, Neale MC, Boker S, et al. Eating disorder-specific risk factors moderate the relationship between negative urgency and binge eating: a behavioral genetic investigation. J Abnorm Psychol. (2017) 126:481–94. doi: 10.1037/abn0000204
84. Vanzhula IA, Calebs B, Fewell L, Levinson CA. Illness pathways between eating disorder and post-traumatic stress disorder symptoms: Understanding comorbidity with network analysis. Eur Eat Disord Rev. (2019) 27:147–60. doi: 10.1002/erv.2634
85. Brooke L, Mussap AJ. Brief report: maltreatment in childhood and body concerns in adulthood. J Health Psychol. (2013) 18:620–6. doi: 10.1177/1359105312454036
86. Dunkley DM, Masheb RM, Grilo CM. Childhood maltreatment, depressive symptoms, and body dissatisfaction in patients with binge eating disorder: the mediating role of self-criticism. Int J Eat Disord. (2010) 43:274–81. doi: 10.1002/eat.20796
87. Brewerton TD. Eating disorders, trauma, and comorbidity: focus on PTSD. Eat Disord. (2007) 15:285–304. doi: 10.1080/10640260701454311
88. Reynolds CF. Building resilience through psychotherapy. World Psychiatry. (2019) 18:289–91. doi: 10.1002/wps.20663
89. Lutz W, Saunders SM, Leon SC, Martinovich Z, Kosfelder J, Schulte D, et al. Empirically and clinically useful decision making in psychotherapy: Differential predictions with treatment response models. Psychol Assess. (2006) 18:133–41. doi: 10.1037/1040-3590.18.2.133
90. Vall E, Wade TD. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. (2015) 48:946–71. doi: 10.1002/eat.22411
91. Fairburn CG, Bailey-Straebler S, Basden S, Doll HA, Jones R, Murphy R, et al. A transdiagnostic comparison of enhanced cognitive behaviour therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating disorders. Behav Res Ther. (2015) 70:64–71. https://doi.org/10.1016/j.brat.2015.04.010
92. Cuijpers P. Targets and outcomes of psychotherapies for mental disorders: an overview. World Psychiatry. (2019) 18:276–85. doi: 10.1002/wps.20661
93. Barber JP, Solomonov N. Toward a personalized approach to psychotherapy outcome and the study of therapeutic change. World Psychiatry. (2019) 18:291–2. doi: 10.1002/wps.20666
94. Abbate-Daga G, Amianto F, Delsedime N, De-Bacco C, Fassino S. Resistance to treatment in eating disorders: a critical challenge. BMC Psychiatry. (2013) 13:294. doi: 10.1186/1471-244X-13-294
95. Demyttenaere K. What is treatment resistance in psychiatry? A “difficult to treat” concept. World Psychiatry. (2019) 18:354–5. doi: 10.1002/wps.20677
96. Loucas CE, Fairburn CG, Whittington C, Pennant ME, Stockton S, Kendall T. E-therapy in the treatment and prevention of eating disorders: a systematic review and meta-analysis. Behav Res Ther. (2014) 63:122–31. doi: 10.1016/j.brat.2014.09.011
97. Brothwood PL, Baudinet J, Stewart CS, Simic M. Moving online: young people and parents' experiences of adolescent eating disorder day programme treatment during the COVID-19 pandemic. J Eat Disord. (2021) 9:62. doi: 10.1186/s40337-021-00418-4
98. Lewis YD, Elran-Barak R, Grundman-Shev Tov R, Zubery E. The abrupt transition from face-to-face to online treatment for eating disorders: a pilot examination of patients' perspectives during the COVID-19 lockdown. J Eat Disord. (2021) 9:31. doi: 10.1186/s40337-021-00383-y
99. Andersson G, Titov N, Dear BF, Rozental A, Carlbring P. Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry. (2019) 18:20–8. doi: 10.1002/wps.20610
100. Linardon J, Shatte A, Tepper H, Fuller-Tyszkiewicz M. A survey study of attitudes toward, and preferences for, e-therapy interventions for eating disorder psychopathology. Int J Eat Disord. (2020) 53:907–16. doi: 10.1002/eat.23268
101. Thompson-Brenner H, Boswell JF, Espel-Huynh HM, Brooks GE, Lowe MR. Implementation of transdiagnostic treatment for emotional disorders in residential eating disorder programs: a preliminary pre-post evaluation. Corrected version. Psychother Res. (2018) 29:1045–61. doi: 10.1080/10503307.2018.1446563
102. Barlow DH, Harris BA, Eustis EH, Farchione TJ. The unified protocol for transdiagnostic treatment of emotional disorders. World Psychiatry. (2020) 19:245–6. doi: 10.1002/wps.20748
103. Trottier K, MacDonald DE. Update on psychological trauma, other severe adverse experiences and eating disorders: state of the research and future research directions. Curr Psychiatry Rep. (2017) 19:45. doi: 10.1007/s11920-017-0806-6
104. Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. (2003) 41:509–28. doi: 10.1016/s0005-7967(02)00088-8
Keywords: COVID-19, eating disorder, childhood maltreatment, stress, psychopathology
Citation: Cascino G, Marciello F, Abbate-Daga G, Balestrieri M, Bertelli S, Carpiniello B, Corrivetti G, Favaro A, Renna C, Ricca V, Salvo P, Segura-Garcia C, Todisco P, Volpe U, Zeppegno P, Monteleone P and Monteleone AM (2021) How Is the History of Early Traumatic Exposure Associated With the Psychopathological Outcomes of COVID-19 Related Lockdown and Subsequent Re-opening in People With Eating Disorders? Front. Psychiatry 12:789344. doi: 10.3389/fpsyt.2021.789344
Received: 04 October 2021; Accepted: 15 November 2021;
Published: 08 December 2021.
Edited by:
Tomasz M. Gondek, Self-employed, Wroclaw, PolandReviewed by:
Alfonso Tortorella, University of Perugia, ItalyEkin Sönmez Güngör, Istanbul Erenkoy Training and Research Hospital for Psychiatric and Neurological Diseases, Turkey
Copyright © 2021 Cascino, Marciello, Abbate-Daga, Balestrieri, Bertelli, Carpiniello, Corrivetti, Favaro, Renna, Ricca, Salvo, Segura-Garcia, Todisco, Volpe, Zeppegno, Monteleone and Monteleone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giammarco Cascino, Z2Nhc2Npbm8xNEBnbWFpbC5jb20=
 Giammarco Cascino
Giammarco Cascino Francesca Marciello
Francesca Marciello Giovanni Abbate-Daga
Giovanni Abbate-Daga Matteo Balestrieri3
Matteo Balestrieri3 Angela Favaro
Angela Favaro Valdo Ricca
Valdo Ricca Cristina Segura-Garcia
Cristina Segura-Garcia Patrizia Todisco
Patrizia Todisco Umberto Volpe
Umberto Volpe Patrizia Zeppegno
Patrizia Zeppegno Palmiero Monteleone
Palmiero Monteleone Alessio Maria Monteleone
Alessio Maria Monteleone