
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 14 December 2021
Sec. Addictive Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.786664
This article is part of the Research TopicDual Disorders (Addictive and Concomitant Psychiatric Disorders): Mechanisms and TreatmentView all 13 articles
The frequent co-occurrence of post-traumatic stress disorder (PTSD) and substance use disorders (SUDs) leads to manifestations of both conditions that are more severe and more resistance to treatment than single disorders. One hypothesis to explain this synergy is the impact of intrusive memories on craving which, in turn, increases the risk of relapse among patients with substance use disorders. The aim of this systematic review is to examine this possibility by assessing the impact of PTSD and its symptoms on craving among dual disorder patients. Using PRISMA criteria, four databases were comprehensively searched up to June, 2021, in order to identify all candidate studies based on broad key words. Resulting studies were then selected if they examined the impact of PTSD or PTSD symptoms on craving, and if they used standardized assessments of PTSD, SUD, and craving. Twenty-seven articles matched the selection criteria and were included in this review. PTSD was found to be significantly associated with increased craving levels among patients with alcohol, cannabis, cocaine, tobacco, and other substance use disorders. Exposition to traumatic cues among dual disorder patients was also shown to trigger craving, with an additive effect on craving intensity when exposure to substance-related cues occurred. In addition, certain studies observed a correlation between PTSD symptom severity and craving intensity. Concerning mechanisms underlying these associations, some findings suggest that negative emotional states or emotion dysregulation may play a role in eliciting craving after traumatic exposure. Moreover, these studies suggest that PTSD symptoms may, independently of emotions, act as powerful cues that trigger craving. These findings argue for the need of dual disorder treatment programs that integrate PTSD-focused approaches and emotion regulation strategies, in addition to more traditional interventions for craving management.
The diagnosis of Post-Traumatic Stress Disorder (PTSD) first appeared in the 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders in 1980 (1), based largely on clinical descriptions of soldiers returning from the Vietnam war (2). Its definition has evolved considerably over recent decades, including its removal from the anxiety disorders in DSM 5 as well as the creation of a distinct diagnostic category for this disorder (3). PTSD is characterized by a variety of symptoms that persist over the months or years following a traumatic event and that notably include intrusive memories, avoidance of cues associated with the event, alterations of cognition and mood, and a state of hyperarousal. Although diverse mental disorders are frequently associated with PTSD, substance use disorders (SUDs) are particularly prevalent (4–6). The principal hypotheses that have been formulated to explain these associations include self-medication (implying that PTSD is the primary condition and that substance use disorders occur later), the notion that addiction to substances may constitute a risk factor for the occurrence of traumatic events (whereby PTSD is a secondary condition), and finally the possibility that both disorders share common vulnerability factors (7). Regardless of which mechanism best explains these forms of dual disorder, the combination of PTSD and addiction leads to poorer prognosis, increases in suicide attempts, greater social disability, poorer treatment adherence, and reduced medication efficacy when compared to patients without comorbidity (8–10). In line with these results, a recent review of clinical investigations also documented a strong relationship between the diagnosis of PTSD and increased substance use and relapse in dual disorder individuals (11), but again the exact mechanisms underlying this association remain unclear.
Craving has been studied extensively over the years and particularly over the past two decades due to acknowledgment of its crucial role in addiction (12, 13). Craving refers to the intense, urgent, and unwanted desire to consume a substance (14) and it is now considered to be a core component of addiction with important diagnostic implications following its inclusion in DSM-5. Based on findings that demonstrate a prospective link between craving episodes and substance use, craving is increasingly viewed as a central construct in the etiology and course of different forms of addiction, and it is a strong predictor of treatment outcome (15–19). Among the diverse factors that may affect craving, a large body of research has highlighted the major role of substance-related cues and stress (20–29). These investigations have shown the ability of substance-related cues and stress exposure to elicit craving among individuals with alcohol, opiate, cocaine, tobacco, and cannabis dependence. Moreover, laboratory studies have also shown that exposure to stress-related events among individuals with alcohol use disorder (AUD) reliably elicits craving in a manner that is as powerful as alcohol-related cues (30, 31). Although similar patterns of reactivity have been shown among individuals with PTSD and alcohol use disorder after exposures to personalized trauma cues via “trauma scripts,” such scripts were found to provoke greater craving that non-trauma scripts and to be more salient in eliciting alcohol craving (31, 32). These results could suggest that the intrusive memories experienced by persons with PTSD and the significant stress they induce may therefore constitute major triggers of craving as well as explain reductions in treatment efficacy in this population. This pattern of findings is consistent with the findings that patients in SUD treatment who report higher PTSD scores also report higher scores on craving, depression, anxiety and stress (33), with a potential relationship between PTSD severity, SUD severity and craving levels.
One hypothesis to explain the synergy of PTSD and SUDs as a dual disorder is therefore the impact of intrusive memories or trauma-related cues on craving which, in turn, increases the risk of relapse among patients with substance use disorders. Examining this relationship across different forms of substance addiction should help elucidate the mechanisms underlying the general increase in clinical severity in this population, and the literature on this topic is now of sufficient size to permit a reliable summary that should more fully respond to the goals of precision psychiatry and personalized medicine (34). The aim of this systematic review is to address this issue by assessing all published investigations of the impact of PTSD and its symptoms on craving, among dual disorder patients.
The study involved a systematic review of the literature based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines (35).
This review was based on the following databases: PUBMED/MEDLINE, Psychinfo, Cochrane, and Wiley Online Library. The search was performed for all years up to June, 2021.
The following search terms were used:
[(≪ Addiction ≫ or ≪ Substance Use Disorder ≫ or ≪ Substance-related Disorder ≫) and (≪ Post Traumatic Stress Disorder ≫ or ≪ PTSD ≫) and (≪ Craving ≫ or ≪ Urge ≫)].
The following criteria were used to select investigations for this review:
1. Studies Published in English-Language peer-reviewed journals.
2. Studies concerning patients, with no restrictive criteria regarding age, sex, ethnic origin, or place of residence. Studies had to include participants with PTSD and SUD comorbidity, defined, or explored according to standardized questionnaires.
3. Studies including measures of craving, and assessing the impact of PTSD or PTSD symptoms on craving occurrence or severity. It was not necessary that craving was designated as the primary outcome of the study in order for it to be included in this review.
Studies were excluded if they were based on animal models, or if they were limited to conference abstracts, dissertations, book chapters, or incomplete articles.
Two authors independently examined all titles and abstracts. Relevant articles were obtained in full-text and assessed for inclusion criteria separately by the two reviewers based on the inclusion and exclusion criteria previously mentioned. Disagreements were resolved via discussion of each article for which conformity to inclusion and exclusion criteria were uncertain and a consensus was reached. The reference lists of major papers were also manually screened in order to ensure comprehensiveness of the review. All selected studies were read in full to confirm inclusion criteria, study type, and study population.
Two reviewers (LJ and MF) assessed the quality of data in the included studies using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (S2C) from National Institutes of Health (36). This tool is comprised of 14 questions with responses to each being “yes,” “no,” or “other” (not applicable, NA or nor reported, NR). We rated the overall quality of each included study as “good,” “fair,” or “poor.”
Sample characteristics (including socio-demographic data, comorbidity, and treatment status), and information on study design and methods of assessment of PTSD, SUD, and craving were extracted. Table 1 presents these data extracted from the selected studies.
A total of 247 articles were identified through the search of the databases. After review of titles and abstracts, 52 articles were selected for further examination. After reading the full text, 27 met inclusion criteria for this review. This process is described in the PRISMA flowchart (Figure 1). The selected articles were published between 2002 and 2021.
A summary of risk of bias is presented in Table 2. Eleven studies were considered to be of “good” quality, six were “fair” quality and nine of “poor” quality.
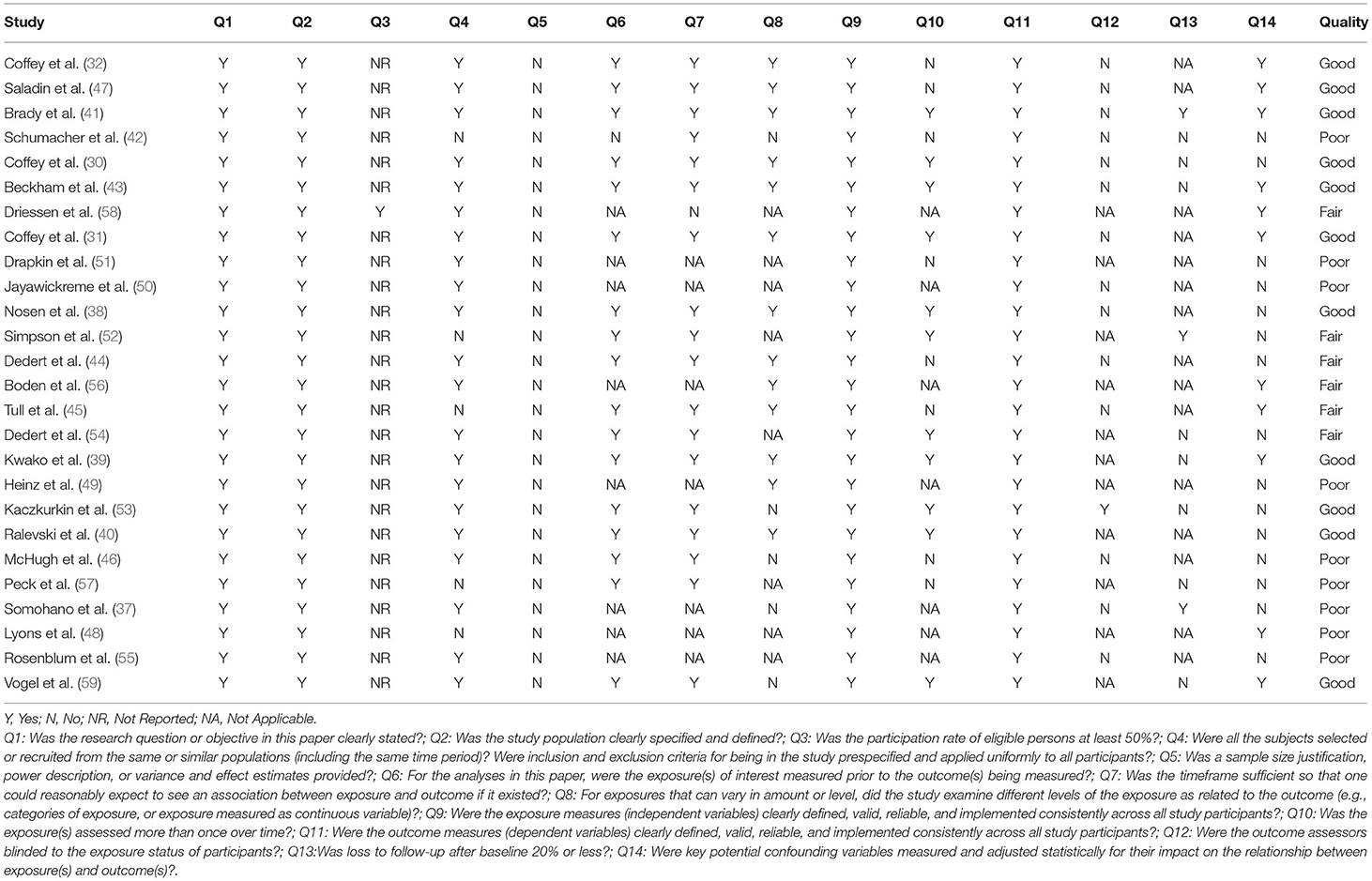
Table 2. Overall quality rating of the included studies using the The National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies.
Twenty-seven studies fulfilled criteria for inclusion in this review, of which 12 focused on alcohol, 4 on tobacco, 1 on cannabis, 1 on cocaine, and 9 on various substance use disorders (three studies on AUD and/or Cocaine Use Disorder and six studies on different types of SUD). Among the 27 included studies, 13 were experimental studies, 13 were observational studies and 1 was a randomized controlled trial.
In total, 3580 subjects were enrolled, of which 1960 (54.7%) met criteria for PTSD and SUD, 1206 (33.7%) for SUD only, and 105 for PTSD only. One study (37) did not indicate the prevalence of low vs. high PTSD scores. Participants were most often males (65.6%), with a mean age of 41.3 years. Most participants (n = 3,337; 93.2%) were recruited in care facilities including outpatient (n = 1804; 54%), inpatient (n = 497; 15%), residential (n = 497; 15%) or either inpatient/outpatient (n = 539, 16%) treatment programs. Among the included participants, 61.8% (n = 2212) met criteria for AUD, 10.9% (n = 390) were current smokers, 10.7% (n = 383) met criteria for Cocaine Use Disorder, 9.6% (n = 343) for Cannabis Use Disorder, 6.7% (n = 241) for Opiate Use Disorder, 3.3% (n = 118) for Stimulant Use Disorder, 2.4% (n = 85) for Anxiolytic or Hypnotic Use Disorder, 2.2% (n = 79) for comorbid Cocaine and Alcohol Use Disorder, and 1.2% (n = 45) for Polysubstance Use Disorder.
A detailed description of all studies included and their main results can be found in Tables 3, 4.
The 13 experimental studies selected for this review consisted, for most part, of exposing participants with comorbid SUD and PTSD to traumatic memories, non-specific stressors, and substance-related cues, and then evaluating their responses across SUD subgroups. Seven experimental studies involved AUD, two involved tobacco use disorder, one involved cocaine use disorder, and three studies included patients suffering from AUD and Cocaine Use Disorder.
The primary finding was that exposure to a traumatic memory (in the form of a script recounting a traumatic life event) generated a significantly greater increase in craving than neutral exposure and similarly to exposure to an alcohol-related cue (31, 38–40). The studies by Coffey et al. (31) and Nosen et al.'s (38) went further, showing that the combination of exposure to a traumatic script followed by an alcohol-related cue generated greater craving than each type of exposure when considered separately. Two studies showed that exposure to a traumatic memory increased craving more than a non-specific stressor (39, 40).
Only one study compared subjects with the comorbidity AUD and PTSD to subjects with AUD alone (41). This study found no significant difference between the two groups in terms of craving intensity after exposure to a non-specific stressor. Ralevski et al. (40) found no correlation between the intensity of craving provoked by the different scripts (traumatic, non-specific stress, and neutral) and the severity of PTSD symptoms, measured by the Clinician Administered PTSD Scale (CAPS). Finally, Schumacher et al. (42) showed that subjects who had suffered early childhood trauma (<13 years of age) presented a more severe AUD, traumatic intrusion symptoms, and post-exposure craving (traumatic script and alcohol-related cues), than subjects who suffered their first trauma later in adolescence (13–18 years of age).
Two experimental studies addressed tobacco use disorder. Beckham et al. (43) showed that the increase in craving, negative affect and traumatic symptoms were stronger after being exposed to traumatic scripts than stressful event scripts and neutral scripts. Subjects with PTSD experienced a more significant increase in craving and negative affect compared to the other group. Cigarette use was associated with a reduction in craving (which was greater in magnitude after a traumatic script), as well as reduction in negative affect, and traumatic symptoms, independently of group type. Dedert et al. (44) found that subjects with PTSD presented more severe withdrawal symptoms and a higher craving level for two dimensions (anticipation of reinforcing effect, anticipation of withdrawal symptoms and negative affect release) during acute withdrawal. Participants with PTSD reported lower craving reductions after smoking.
One experimental study by Tull et al. (45) assessed the effect of exposure to a personalized trauma cue on cocaine craving in patients with cocaine use disorder with or without PTSD. Subjects with PTSD had significantly higher craving for cocaine than other participants after the traumatic script.
Three experimental studies exposed subjects with alcohol and/or cocaine addiction and a history of traumatic events to combinations of traumatic or neutral scripts and substance-related or neutral cues (32, 46, 47). All studies showed that exposure to traumatic memories and substance-related cues increased craving and negative affect significantly more than neutral exposures. The studies of Saladin et al. (47) and McHugh et al. (46) showed a positive correlation between the severity of PTSD symptoms and the intensity of craving after traumatic exposure. Finally, McHugh et al. (46) observed a positive correlation between the level of anxiety sensitivity (tendency to react with fear to signs and symptoms of anxiety) and the severity of traumatic symptoms and negative affect, but not craving after the exposures.
A total of 14 studies investigated the association between PTSD symptoms and craving across SUD subgroups: 12 were observational studies (five for AUD, two for Tobacco Use Disorder, one for Cannabis Use Disorder, and four for different types of Substance Use Disorders), one was an experimental study and one was a Randomized Controlled Trial among AUD individuals.
Five cross-sectional observational studies examined correlations between different variables related to PTSD and AUD. The studies by Lyons et al. (48) and Heinz et al. (49) found a correlation between the intensity of craving for alcohol on the one hand and the severity of PTSD symptoms and consumption on the other, in comorbid subjects. For Lyons et al. (48), traumatic cognitions (self-deprecation, dangerousness of the world) generated negative affect, which in turn triggered craving. Jayawickreme et al. (50) also found a positive correlation between traumatic cognitions about oneself (self-depreciation and tendency to blame oneself), negative beliefs about the world and the intensity of craving, but this relationship was only significant in men. Finally, Drapkin et al. (51) compared the psychosocial functioning of subjects with comorbid PSTD and AUD with those with SUD or PTSD alone. The authors found that social functioning was more impaired (less education, lower income, more unemployment), as well as more severe depressive symptoms and cravings, in the comorbid subjects.
In a 28-day study using a daily monitoring with an Interactive Voice Response (IVR), Simpson et al. (52) found that PTSD severity was positively correlated with craving level on the same day but not the following day. In a more specific way, some traumatic symptoms (startle, irritability), were positively correlated with craving levels on the same day, whereas other symptoms (nightmares, emotional blunt, hypervigilance), predicted craving increases on the following day. On the other hand, craving intensity on a given day was not correlated with PTSD symptom severity on the following day.
Two studies assessed the impact of changes of PTSD symptoms overtime on craving after specific treatment approaches. In a randomized clinical trial conducted by Kaczkurkin et al. (53), 165 comorbid subjects were randomly assigned to four different treatment groups: Naltrexone + exposure therapy, Naltrexone alone, exposure therapy + placebo, and placebo alone. At baseline, participants with greater levels of PTSD symptom severity endorsed a significantly greater percentage of days drinking and alcohol craving. The percentage of days drinking was positively correlated with alcohol craving. Participants in the Naltrexone + exposure therapy group had a greater decrease in craving than in the Naltrexone alone group. Subjects with higher initial PTSD severity had a more rapid decrease in craving intensity over time. Finally, the percentage of drinking days and the severity of traumatic symptoms at time t predicted the intensity of craving at time t + 1, with alcohol craving being dependent on the amount of PTSD symptoms and alcohol use reported at the previous time point. Coffey et al. (30) compared the effectiveness of exposure therapy and relaxation-based therapy in 43 subjects with comorbid AUD and PTSD using a laboratory-based experiment. A first session conducted before the beginning of treatment showed an increase in craving and emotional distress of the participants after exposure to a traumatic script and alcohol-related cues. Follow-up analyses after six sessions of group exposure therapy found a reduction of both PTSD symptoms and alcohol craving overtime.
In 2014, Dedert et al. (54) used Ecological Momentary Assessment (EMA) to follow smokers with PTSD in daily life over 14 days. Participants were allowed to smoke freely during the first week, then had to begin withdrawal without any substitute or pharmacological treatment in the second week. Compared with the pre-withdrawal phase, abstinence was associated with reductions in PTSD symptoms and craving, but not negative affect. During withdrawal period, an increase in traumatic symptom intensity predicted an increase in craving at next EMA evaluation, but the reverse association was not observed.
Rosenblum et al. (55) compared three groups composed by 162 US Army veteran daily smokers: a PTSD group (52 subjects with PTSD alone or with a comorbid depressive episode); a depressive episode group (52 subjects with depressive episode without comorbidity); and a control group (58 subjects with no psychiatric disorder). The PTSD group (with or without depression) described higher craving than the control group without any psychiatric disorder.
Boden et al. (56) explored the links between PTSD and different characteristics associated with cannabis use (motivation, relational problems, withdrawal symptoms, and craving) in veterans with cannabis use disorder with and without PTSD. Patients with PTSD used cannabis more frequently as a coping strategy and reported a significatively higher level of craving in several components (compulsive, anticipating release of emotional distress, and use planification). Traumatic symptom severity was positively correlated with the emotional component of craving (release of emotional distress).
Two studies assessed the course of craving during SUD treatment according to PTSD symptoms severity at baseline. Wieferink et al. (33) assessed outcomes of standard, non-integrated SUD treatment among 297 SUD outpatients (AUD, or Cannabis or Cocaine Use Disorder) with higher (≥48) or lower (<48) PTSD symptom severity based on the Self-Reported Inventory for PTSD (SRIP). At baseline, there was no difference in the number of days of use between subjects, however, subjects with more severe PTSD symptoms had significantly higher levels of craving and anxiety-depressive symptoms. After 3 and 6 months of treatment, there was a decrease in the number of days of use for all subjects, a significantly greater decrease in craving for subjects with more severe traumatic symptoms, and a significant decrease in anxiety-depressive symptoms for subjects with severe traumatic symptoms only. However, patients with higher levels of PTSD symptoms still reported significantly higher scores on depression, anxiety and stress after 6 months of SUD treatment. Peck et al. (57) assessed the impact of a 6 weeks therapeutical program including cognitive processing therapy, Alcoholics Anonymous (AA) meetings, and group discussion with 72 American veterans suffering from PTSD and a substance use disorder (AUD, Cannabis Use Disorder, Cocaine Use Disorder, Opiate Use Disorder, Amphetamine Use Disorder, or Anxiolytic Use Disorder). Baseline dysfunctional cognitions associated with the trauma were positively correlated with PTSD and craving severity. However, PTSD severity was not correlated with craving levels. Cognitive processing therapy was associated with significant improvements in erroneous cognitions, trauma-cued substance craving, and depressive or trauma-related symptoms. Reduction in depressive or trauma-related symptoms was partly explained by the therapy's impact on erroneous cognitions, contrary to craving.
In a cross-sectional study, Driessen et al. (58) focused on the relationship between the type of addiction (alcohol or drug addiction or both), the severity of the addiction and of craving, and the presence or not of comorbid PTSD. Participants with PTSD had a higher addiction severity score, were more often hospitalized, had a shorter abstinence time between relapses and experienced craving more frequently than other participants. Somohano et al. (37) assessed the correlation between severity of different symptoms of PTSD and craving according to four classes of substances: alcohol, psycho-stimulants (cocaine, amphetamines), opiates and cannabis. Concerning subjects with alcohol use disorder (n = 131), global PTSD severity and hypervigilance levels were associated with craving intensity. For participants with psychostimulant use disorder (n = 66), craving levels were correlated with global PTSD severity and more precisely with avoidance syndrome intensity. Among subjects with opiate use disorder (n = 36), global PTSD severity was correlated with craving levels, but with no association to specific symptoms. Finally, for subjects with cannabis use disorder, no variable was associated with craving. An observational study led by Vogel et al. (59), highlighted a positive correlation between craving levels and PTSD symptoms over 6 days following admission for detoxification among comorbid patients (PTSD with alcohol, cannabis, sedatives or mixed use disorder). However, no correlation was found concerning PTSD symptoms at Day 1 and craving the following day.
Several studies focused on the role played by negative affect during different forms of exposures (31, 38, 40). The results were similar to those obtained for craving and showed that exposure to a traumatic script and an alcohol-related cue generated a more intense level of negative affect than during a neutral exposure. Nosen et al. (38) reported that in a traumatic context (exposure to a traumatic script), the intensity of craving was correlated with the severity of negative affect. The study of Coffey et al. (30), through a laboratory-based experiment, found a decrease of both craving and emotional distress after trauma-focused imaginal exposure, suggesting that negative emotions should constitute a mechanism of alcohol craving induced by trauma exposure. Lyons et al. (48) examined more specifically the mediation role of negative affect on the association between PTSD cognitions and craving among 136 treatment-seeking veterans with PTSD and AUD. Mediation models demonstrated that negative affect mediated the association between specific posttraumatic cognitions related to the self, the world, the self-blame, and craving controlling for PTSD/AUD symptom severity and gender. Posttraumatic cognitions were associated with increased negative affect, which in turn was related to increased craving. Finally, one observational study (50) examined sex differences in trauma cognitions and their relationship to symptoms of AUD including craving. Specifically, negative cognitions about the self were associated with increased craving in men, but not in women, a finding that could be related to greater subjective negative emotions related to traumatic experiences in men. In this perspective, higher craving levels could be explained as a result of maladaptive coping of trauma-related negative emotions.
The study of Dedert et al. (54) investigated whether craving for cigarettes was driven by PTSD symptoms and negative affect among smokers with PTSD attending to quit, using an EMA procedure. Negative emotions were identified as predictors of craving during the withdrawal period (54). Increased PTSD symptoms and negative affect predicted an increase in craving at the next EMA evaluation, even on days with low levels of craving, but the reverse association was not observed.
In the experimental study of Tull et al. (45), in male subjects only, the experience of negative emotions (shame, guilt) in response to the traumatic script mediated the relationship between traumatic symptoms and craving for cocaine. The experience of self-conscious negative affect in response to the trauma script accounted for the relation between PTSD diagnosis and cocaine craving following trauma script exposure.
Twenty-seven studies fulfilled criteria for inclusion in this review, of which 12 focused on alcohol, 4 on tobacco, 1 on cannabis, 1 on cocaine and 9 on various substance use disorders. The results showed that regardless of substance type, PTSD and SUD dual disorder was associated with more intense craving levels and was characterized by a prospective link between PTSD symptom severity and craving episodes. Exposure to traumatic memories in experimental studies was associated with emotional distress whose severity was correlated with craving intensity (31, 38).
Whatever for alcohol (31, 38), tobacco (43), or cocaine (47), experimental results showed that exposure to traumatic cues among subjects with PTSD and substance use disorder comorbidity triggered craving in the same way as exposition to substance cues. There also was an additive effect of the association of both forms of exposure on craving, a finding that is consistent with literature showing an association between exposure to stress and craving among patients with substance use disorder (26, 60). However, beyond stress exposure, there appears to be a specific effect of traumatic memories on craving. According to the study by Beckham et al. (43), exposition to traumatic cues triggered significatively greater craving compared with exposure to non-traumatic stress cues. This result could explain the lack of difference in craving levels between subjects with and without PTSD, after exposition to a cold pressor task (neutral stress) in the investigation by Brady et al. (41). In this way, persons with these comorbidities are repeatedly exposed to traumatic memories and therefore to more intense craving, which could increase the risk of relapse. Moreover, the study by Boden et al. (56) lends support to this interpretation by highlighting the correlation between traumatic symptom severity and craving intensity. Finally, studies using EMA observed a prospective link in the association between PTSD symptoms and craving, showing notably that craving daily variation was a reaction to traumatic symptoms intensity. Such results are generally supportive of self-medication theory, as aggravation of PTSD symptoms would then trigger greater craving and lead to substance use as a means of assuaging traumatic symptoms.
In line with this interpretation, some studies in this review also highlighted the role of negative affect associated with traumatic exposure in the risk of relapse and thereby indicating that substance use may constitute a coping strategy to deal with negative affect. Experimental studies among subjects with alcohol and tobacco use disorder (31, 38, 43) showed a correlation in evolution of negative affect and craving after exposition to a traumatic factor. Moreover, negative emotions were identified as predictors of craving after exposition to traumatic cues as well as in daily follow-ups during withdrawal (54). This literature has also demonstrated a salient association between PTSD, addiction and negative emotions, and points specifically to the mediation role of negative emotions and the relationship between traumatic symptoms and alcohol use (61). According to Zvolensky et al. (62), smokers experience greater negative affect if they have comorbid PTSD. Individuals with comorbidity would also use emotions to assuage emotional distress, in accordance with the principle of negative reinforcement. This dysphoric state could be explained by a decrease in dopaminergic D2 receptor density in the reward network (ventral striatum) among persons with substance use disorders (63) and a higher number of DAT dopamine transporters in persons with PTSD (64) that are correlated with craving intensity. Perturbations of the stress axis could also be implicated in these dual disorders, as anomalies of the stress response among subjects with substance use disorders is associated with the activation of extra hypothalamic corticotropin-releasing factor (CRF) synthesis, excessively activating the amygdala (the brain structure implicated in emotional reactions such as fear) (65, 66). Such hyperactivity has also been observed among individuals with PTSD (67) and it is associated with the presence of enduring negative emotional states (anxiety, irritability, dysthymia). While the prefrontal cortex has a major impact on emotional regulation by the inhibition of the amygdala (68), SUD and PTSD are both associated with a hypoactivation of this area (69, 70) that could explain the major emotional dysregulation among these cases of dual disorder (71, 72). Thus, a negative emotional state or emotional dysregulation characterized by significant fluctuations in daily life could constitute a clinical feature of these dual disorders leading to greater craving frequency and/or intensity, although this hypothesis requires further investigation.
Another important observation of this review that could further understanding for mechanisms underlying PTSD and craving is the impact of early trauma. Schumacher and colleagues (42) demonstrated that patients with dual disorders and early trauma (<13 y.o.) experienced more severe PTSD symptoms, more craving after exposure, and more severe AUD. This is consistent with previous studies highlighting a link between age that the trauma was experienced and PTSD severity (73). The link with craving intensity could be partly explained by the fact that early trauma leads to deficit in inhibitory control during stress exposure, which might facilitate the use of substances as coping strategy (74). Indeed, deficits in inhibition capacities during adolescence is known to be associated with a greater risk of both substance experimentation and the development of substance use disorders (75).
Several limitations of this systematic review should be considered in interpreting its findings. A first concern is the heterogenous nature of the selected studies. Based on the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (S2C), most studies included in this review could be qualified as being of “Good” or “Fair” quality (n = 17 or 65%). However, nine studies (35%) were classified as “Poor” quality, and this may partly explain the considerable variation observed in study methods. The majority of investigations classified as “Poor” quality were observational studies while most of the “Good” quality studies were cross-sectional in nature. Moreover, the studies used a large variety of questionnaires to assess SUD, PTSD, and craving. Substance use was mainly reported using self-report questionnaires and only six studies used objective methods of assessment (urine or breath tests). Nevertheless, the majority of experimental studies on cue-reactivity administered single-item instruments, mainly visual analog scale which are considered as an acceptable and valid tool in experimental paradigms, while observational studies used different multi-items questionnaires. The heterogeneity of self-report measures of craving and research design in observational studies could explain some variability in the findings. Finally, few studies addressed sex differences in the analysis, although some results indicated specific relationships between trauma-related cognitions and emotions (self-depreciation and self-blame) and craving among males. More comprehensive analyses are needed to examine the impact of sex (and gender) on the underlying relationship between PTSD and SUD across different SUD subgroups. Despite these limitations, the results strongly underscore the strong relationship between PTSD and substance craving and the necessity to concomitantly treat SUD and PTSD as dual disorder.
Concerning treatment approaches, recent studies assessed several classes of pharmacological agents in the treatment of this dual disorder based on neurobiological mechanisms implicated in both disorders when considered individually (76). Moreover, the positive effect on alcohol use and traumatic symptoms was demonstrated with the association of Disulfiram and Naltrexone in a randomized trial (77), and the use of Desipramine led to an improvement of alcohol use and PTSD symptoms (78). Promising results have also been found with treatments using noradrenergic (Prazosine, Propranolol), GABA and glutamatergic system (Memantine, N-Acetyl-Cysteine, and Topiramate). The results of this review also suggest the importance of improving regulation of negative emotions associated with traumatic memories, and treatments of erroneous or dysfunctional cognitions linked with the traumatism. Furthermore, the potential mediation role of post-traumatic cognitions on negative affect and craving raises the issue to consider posttraumatic cognitions and negative emotions as a salient target for craving reduction. On this issue, several therapies targeting emotion regulation and dysfunctional cognitions linked with traumatism such as Prolonged Exposure and Cognitive Processing Therapy were found to be efficacious for substance use, craving and PTSD symptoms (53, 57, 79). The study of Coffey et al. (30) using trauma-focused exposure therapy led to reductions in negative affect and craving, although the potential link between negative post-traumatic cognitions, negative affect and craving was not specifically assessed. Integrated treatment combining prolonged exposure and naltrexone among individuals with comorbid PTSD and AUD demonstrated better outcomes in terms of alcohol craving compared to exposure alone or naltrexone alone. The necessity of global treatment approaches for comorbid patients, including pharmacological treatment, psychotherapies, and psycho-social treatment has also emphasized (80), but further studies are needed in other SUD populations to generalize these findings and examine the temporal changes of emotion dysregulation, trauma-related emotions such as guilt and shame, on subsequent craving and substance use.
Findings from the current study further inform our understanding of the synergetic relationship between PTSD and SUDs that lead to craving that is greater than that observed with either disorder alone. PTSD symptoms can act as powerful craving cues with an additive effect when combined with exposure to substance-related cues, thereby constituting a salient risk factor for relapse. The craving elicited by PTSD may differ according to specific PTSD symptoms and the effects of specific forms of substance use, although this possibility requires further investigation. Daily life studies using Ecological Momentary Assessment appear to be particularly adapted to investigating the temporal relationship between different PTSD symptoms, emotional states and the clinical expression of addiction, and hold considerable promise for the development of more personalized interventions in dually-diagnosed individuals. Since the majority of the studies included in our review concern alcohol and tobacco, it would be also interesting to expand this research to other substances as well as to behavioral addictions. Specifically, no studies examined the association between craving and MDMA or psychedelic drugs, that is a major issue in view of novel treatment approaches of PTSD.
Our data therefore challenge our current clinical practice in the treatment of patients suffering from dual diagnosis, and argue for the integration of an additional trauma-focused strategies into addiction facilities, notably including cognitive-behavioral therapies based on prolonged exposure. While all individuals suffering from SUD should be systematically assessed for trauma history and PTSD, the present data suggest that PTSD treatment should not be delayed until abstinence has been achieved. The direct relationship between PTSD symptoms and craving argues for the need of these integrated therapies in the goal of providing the most comprehensive and efficacious treatment possible.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
FR, LJ, JS, and MF designed the review, wrote, and reviewed the manuscript. FR and LJ reviewed the abstracts and the papers. FR, LJ, and MF obtained the data from the selected articles. All authors approved the final version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Psychiatric Association, Task Task Force on Nomenclature Statistics, Pichot P, Guelfi JD. Manuel Diagnostique et Statistique des Troubles Mentaux. Paris: Masson (1983).
2. Crocq M-A, Crocq L. From shell shock and war neurosis to posttraumatic stress disorder: a history of psychotraumatology. Dialogues Clin Neurosci. (2000) 2:47–55. doi: 10.31887/DCNS.2000.2.1/macrocq
3. American Psychiatric Association, eds. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th Edn. Washington, DC: American Psychiatric Association (2013).
4. Longo MSC, Vilete LMP, Figueira I, Quintana MI, Mello MF, Bressan RA et al. Comorbidity in post-traumatic stress disorder: a population-based study from the two largest cities in Brazil. J Affect Disord. (2020) 263:715–21. doi: 10.1016/j.jad.2019.11.051
5. Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry. (2005) 62:617–27. doi: 10.1001/archpsyc.62.6.617
6. Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. (2011) 25:456–65. doi: 10.1016/j.janxdis.2010.11.010
7. Haller M, Chassin L. Risk Pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychol Addict Behav. (2014) 28:841–51. doi: 10.1037/a0035878
8. Ouimette P, Goodwin E, Brown PJ. Health and well being of substance use disorder patients with and without posttraumatic stress disorder. Addict Behav. (2006) 31:1415–23. doi: 10.1016/j.addbeh.2005.11.010
9. Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without post-traumatic stress disorder: a comparison of substance use, trauma history and psychiatric comorbidity. Am J Addict. (2000) 9:51–62. doi: 10.1080/10550490050172227
10. Tarrier N, Gregg L. Suicide risk in civilian PTSD patients–predictors of suicidal ideation, planning and attempts. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:655–61. doi: 10.1007/s00127-004-0799-4
11. Lane AR, Waters AJ, Black AC. Ecological momentary assessment studies of comorbid PTSD and alcohol use: a narrative review. Addict Behav Rep. (2019) 10:100205. doi: 10.1016/j.abrep.2019.100205
12. THE CRAVING for alcohol; a symposium by members of the WHO expert committee on mental health and on alcohol. Q J Stud Alcohol. (1955) 16:34–66. doi: 10.15288/qjsa.1955.16.034
13. Lowman C, Hunt WA, Litten RZ, Drummond DC. Research perspectives on alcohol craving: an overview. Addiction. (2000) 95(Suppl. 2):S45–S54. doi: 10.1046/j.1360-0443.95.8s2.14.x
14. Auriacombe M, Serre F, Fatséas M. Le Craving: Marqueur Diagnostique et Pronostique Des Addictions? Traité d'addictologie 2° version (2016).
15. Sayette MA. The role of craving in substance use disorders: theoretical and methodological issues. Annu Rev Clin Psychol. (2016) 12:407–33. doi: 10.1146/annurev-clinpsy-021815-093351
16. Serre F, Fatseas M, Swendsen J, Auriacombe M. Ecological momentary assessment in the investigation of craving and substance use in daily life: a systematic review. Drug Alcohol Depend. (2015) 148:1–20. doi: 10.1016/j.drugalcdep.2014.12.024
17. Fatseas M, Denis C, Massida Z, Verger M, Franques-Rénéric P, Auriacombe M. Cue-induced reactivity, cortisol response and substance use outcome in treated heroin dependent individuals. Biol Psychiatry. (2011) 70:720–7. doi: 10.1016/j.biopsych.2011.05.015
18. Fatseas M, Serre F, Alexandre J, Debrabant R, Auriacombe M, Swendsen J. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: a comparison of substance- and person-specific cues. Addiction. (2015) 110:1035–42. doi: 10.1111/add.12882
19. Sinha R, Fox HC, Hong KA, Hansen J, Tuit K, Kreek MJ. Effects of adrenal sensitivity, stress- and cue-induced craving, and anxiety on subsequent alcohol relapse and treatment outcomes. Arch Gen Psychiatry. (2011) 68:942–52. doi: 10.1001/archgenpsychiatry.2011.49
20. Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl). (2001) 158:343–59. doi: 10.1007/s002130100917
21. Junghanns K, Backhaus J, Tietz U, Lange W, Bernzen J, Wetterling T, et al. Impaired serum cortisol stress response is a predictor of early relapse. Alcohol Alcohol. (2003) 38:189–93. doi: 10.1093/alcalc/agg052
22. Sinha R, Catapano D, O'Malley S. Stress-induced craving and stress response in cocaine dependent individuals. Psychopharmacology (Berl). (1999) 142:343–51. doi: 10.1007/s002130050898
23. Fox HC, Bergquist KL, Hong K-I, Sinha R. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol-dependent individuals. Alcohol Clin Exp Res. (2007) 31:395–403. doi: 10.1111/j.1530-0277.2006.00320.x
24. Hyman SM, Fox H, Hong K-IA, Doebrick C, Sinha R. Stress and drug-cue-induced craving in opioid-dependent individuals in naltrexone treatment. Exp Clin Psychopharmacol. (2007) 15:134–43. doi: 10.1037/1064-1297.15.2.134
25. Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology. (2009) 34:1198–208. doi: 10.1038/npp.2008.78
26. Back SE, Gros DF, Price M, LaRowe S, Flanagan J, Brady KT et al. Laboratory-induced stress and craving among individuals with prescription opioid dependence. Drug Alcohol Depend. (2015) 155:60–7. doi: 10.1016/j.drugalcdep.2015.08.019
27. Sinha R. Modeling stress and drug craving in the laboratory: implications for addiction treatment development. Addict Biol. (2009) 14:84–98. doi: 10.1111/j.1369-1600.2008.00134.x
28. Ferguson SG, Shiffman S. The relevance and treatment of cue-induced cravings in tobacco dependence. J Subst Abuse Treat. (2009) 36:235–43. doi: 10.1016/j.jsat.2008.06.005
29. Yu J, Zhang S, Epstein DH, Fang Y, Shi J, Qin H, et al. Gender and stimulus difference in cue-induced responses in abstinent heroin users. Pharmacol Biochem Behav. (2007) 86:485–92. doi: 10.1016/j.pbb.2007.01.008
30. Coffey SF, Stasiewicz PR, Hughes PM, Brimo ML. Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychol Addict Behav. (2006) 20:425–35. doi: 10.1037/0893-164X.20.4.425
31. Coffey SF, Schumacher JA, Stasiewicz PR, Henslee AM, Baillie LE, Landy N. Craving and physiological reactivity to trauma and alcohol cues in PTSD and alcohol dependence. Exp Clin Psychopharmacol. (2010) 18:340–9. doi: 10.1037/a0019790
32. Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug Alcohol Depend. (2002) 65:115–27. doi: 10.1016/S0376-8716(01)00157-0
33. Wieferink CEM, de Haan HA, Dijkstra BAG, Fledderus M, Kok T. Treatment of substance use disorders: effects on patients with higher or lower levels of PTSD symptoms. Addict Behav. (2017) 74:122–6. doi: 10.1016/j.addbeh.2017.06.005
34. Szerman N, Peris L. Precision psychiatry and dual disorders. J Dual Diagn. (2018) 14:237–46. doi: 10.1080/15504263.2018.1512727
35. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
36. Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. (2020) 7:7. doi: 10.1186/s40779-020-00238-8
37. Somohano VC, Rehder KL, Dingle T, Shank T, Bowen S. PTSD symptom clusters and craving differs by primary drug of choice. J Dual Diagn. (2019) 15:233–42. doi: 10.1080/15504263.2019.1637039
38. Nosen E, Nillni YI, Berenz EC, Schumacher JA, Stasiewicz PR, Coffey SF. Cue-elicited affect and craving: advancement of the conceptualization of craving in co-occurring posttraumatic stress disorder and alcohol dependence. Behav Modif. (2012) 36:808–33. doi: 10.1177/0145445512446741
39. Kwako LE, Schwandt ML, Sells JR, Ramchandani VA, Hommer DW, George DT et al. Methods for inducing alcohol craving in individuals with co-morbid alcohol dependence and posttraumatic stress disorder: behavioral and physiological outcomes. Addict Biol. (2015) 20:733–46. doi: 10.1111/adb.12150
40. Ralevski E, Southwick S, Jackson E, Jane JS, Russo M, Petrakis I. Trauma- and stress-induced response in veterans with alcohol dependence and comorbid post-traumatic stress disorder. Alcohol Clin Exp Res. (2016) 40:1752–60. doi: 10.1111/acer.13120
41. Brady KT, Back SE, Waldrop AE, McRae AL, Anton RF, Upadhyaya HP et al. Cold pressor task reactivity: predictors of alcohol use among alcohol-dependent individuals with and without comorbid posttraumatic stress disorder. Alcohol Clin Exp Res. (2006) 30:938–46. doi: 10.1111/j.1530-0277.2006.00097.x
42. Schumacher JA, Coffey SF, Stasiewicz PR. Symptom severity, alcohol craving, and age of trauma onset in childhood and adolescent trauma survivors with comorbid alcohol dependence and posttraumatic stress disorder. Am J Addict. (2006) 15:422–5. doi: 10.1080/10550490600996355
43. Beckham JC, Dennis MF, Joseph McClernon F, Mozley SL, Collie CF, Vrana SR. The effects of cigarette smoking on script-driven imagery in smokers with and without posttraumatic stress disorder. Addict Behav. (2007) 32:2900–15. doi: 10.1016/j.addbeh.2007.04.026
44. Dedert EA, Calhoun PS, Harper LA, Dutton CE, McClernon FJ, Beckham JC. Smoking withdrawal in smokers with and without posttraumatic stress disorder. Nicotine Tob Res. (2012) 14:372–6. doi: 10.1093/ntr/ntr142
45. Tull MT, Kiel EJ, McDermott MJ, Gratz KL. The effect of trauma cue exposure on cocaine cravings among cocaine dependent inpatients with and without posttraumatic stress disorder: exploring the mediating role of negative affect and discrete negative emotional states. J Exp Psychopathol. (2013) 4:485–501. doi: 10.5127/jep.028812
46. McHugh RK, Gratz KL, Tull MT. The role of anxiety sensitivity in reactivity to trauma cues in treatment-seeking adults with substance use disorders. Compr Psychiatry. (2017) 78:107–14. doi: 10.1016/j.comppsych.2017.07.011
47. Saladin ME, Drobes DJ, Coffey SF, Dansky BS, Brady KT, Kilpatrick DG. PTSD symptom severity as a predictor of cue-elicited drug craving in victims of violent crime. Addict Behav. (2003) 28:1611–29. doi: 10.1016/j.addbeh.2003.08.037
48. Lyons R, Haller M, Rivera G, Norman S. Negative affect mediates the association between posttraumatic cognitions and craving in veterans with posttraumatic stress disorder and alcohol use disorder. J Dual Diagn. (2020) 16:292–8. doi: 10.1080/15504263.2020.1741754
49. Heinz AJ, Pennington DL, Cohen N, Schmeling B, Lasher BA, Schrodek E, et al. Relations between cognitive functioning and alcohol use, craving, and post-traumatic stress: an examination among trauma-exposed military veterans with alcohol use disorder. Mil Med. (2016) 181:663–71. doi: 10.7205/MILMED-D-15-00228
50. Jayawickreme N, Yasinski C, Williams M, Foa EB. Gender-specific associations between trauma cognitions, alcohol cravings and alcohol-related consequences in individuals with comorbid PTSD and alcohol dependence. Psychol Addict Behav. (2012) 26:13–9. doi: 10.1037/a0023363
51. Drapkin ML, Yusko D, Yasinski C, Oslin D, Hembree EA, Foa EB. Baseline functioning among individuals with posttraumatic stress disorder and alcohol dependence. J Subst Abuse Treat. (2011) 41:186–92. doi: 10.1016/j.jsat.2011.02.012
52. Simpson TL, Stappenbeck CA, Varra AA, Moore SA, Kaysen D. Symptoms of posttraumatic stress predict craving among alcohol treatment seekers: results of a daily monitoring study. Psychol Addict Behav. (2012) 26:724–33. doi: 10.1037/a0027169
53. Kaczkurkin AN, Asnaani A, Alpert E, Foa EB. The impact of treatment condition and the lagged effects of PTSD symptom severity and alcohol use on changes in alcohol craving. Behav Res Ther. (2016) 79:7–14. doi: 10.1016/j.brat.2016.02.001
54. Dedert EA, Dennis PA, Swinkels CM, Calhoun PS, Dennis MF, Beckham JC. Ecological momentary assessment of posttraumatic stress disorder symptoms during a smoking quit attempt. Nicotine Tob Res. (2014) 16:430–6. doi: 10.1093/ntr/ntt167
55. Rosenblum MS, Engle JL, Piper ME, Kaye JT, Cook JW. Motives for smoking in those with PTSD, depression, and no psychiatric disorder. J Dual Diagn. (2020) 16:285–91. doi: 10.1080/15504263.2020.1759846
56. Boden MT, Babson KA, Vujanovic AA, Short NA, Bonn-Miller MO. Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. Am J Addict. (2013) 22:277–84. doi: 10.1111/j.1521-0391.2012.12018.x
57. Peck KR, Coffey SF, McGuire AP, Voluse AC, Connolly KM. A cognitive processing therapy-based treatment program for veterans diagnosed with co-occurring posttraumatic stress disorder and substance use disorder: the relationship between trauma-related cognitions and outcomes of a 6-week treatment program. J Anxiety Disord. (2018) 59:34–41. doi: 10.1016/j.janxdis.2018.09.001
58. Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M et al. Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol Clin Exp Res. (2008) 32:481–8. doi: 10.1111/j.1530-0277.2007.00591.x
59. Vogel L, Koller G, Ehring T. The relationship between posttraumatic stress symptoms and craving in patients with substance use disorder attending detoxification. Drug Alcohol Depend. (2021) 223:108709. doi: 10.1016/j.drugalcdep.2021.108709
60. McRae-Clark AL, Carter RE, Price KL, Baker NL, Thomas S, Saladin ME et al. Stress and cue-elicited craving and reactivity in marijuana-dependent individuals. Psychopharmacology (Berl). (2011) 218:49–58. doi: 10.1007/s00213-011-2376-3
61. Cohn A, Hagman BT, Moore K, Mitchell J, Ehlke S. Does negative affect mediate the relationship between daily PTSD symptoms and daily alcohol involvement in female rape victims? Evidence from 14 days of interactive voice response assessment. Psychol Addict Behav. (2014) 28:114–26. doi: 10.1037/a0035725
62. Zvolensky M, Gibson L, Vujanovic A, Gregor K, Bernstein A, Kahler C et al. Impact of Posttraumatic Stress Disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine Tobacco Res. (2008) 10:1415–27. doi: 10.1080/14622200802238951
63. Heinz A, Siessmeier T, Wrase J, Hermann D, Klein S, Grüsser SM, et al. Correlation between dopamine D(2) receptors in the ventral striatum and central processing of alcohol cues and craving. Am J Psychiatry. (2004) 161:1783–9. doi: 10.1176/ajp.161.10.1783
64. Hoexter MQ, Fadel G, Felício AC, Calzavara MB, Batista IR, Reis MA, et al. Higher striatal dopamine transporter density in PTSD: an in vivo SPECT study with [(99m)Tc]TRODAT-1. Psychopharmacology (Berl). (2012) 224:337–45. doi: 10.1007/s00213-012-2755-4
65. Koob GF. Dynamics of neuronal circuits in addiction: reward, antireward, and emotional memory. Pharmacopsychiatry. (2009) 42:S32–S41. doi: 10.1055/s-0029-1216356
66. Ruisoto P, Contador I. The role of stress in drug addiction. An integrative review. Physiol Behav. (2019) 202:62–8. doi: 10.1016/j.physbeh.2019.01.022
67. Liberzon I, Taylor SF, Amdur R, Jung TD, Chamberlain KR, Minoshima S, et al. Brain activation in PTSD in response to trauma-related stimuli. Biol Psychiatry. (1999) 45:817–26. doi: 10.1016/S0006-3223(98)00246-7
68. Ochsner KN, Ray RD, Cooper JC, Robertson ER, Chopra S, Gabrieli JDE, et al. For better or for worse: neural systems supporting the cognitive down- and up-regulation of negative emotion. Neuroimage. (2004) 23:483–99. doi: 10.1016/j.neuroimage.2004.06.030
69. Seo D, Lacadie CM, Tuit K, Hong K-I, Constable RT, Sinha R. Disrupted ventromedial prefrontal function, alcohol craving, and subsequent relapse risk. JAMA Psychiatry. (2013) 70:727–39. doi: 10.1001/jamapsychiatry.2013.762
70. Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. (2007) 164:1476–88. doi: 10.1176/appi.ajp.2007.07030504
71. Weiss NH, Tull MT, Anestis MD, Gratz KL. The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug Alcohol Depend. (2013) 128:45–51. doi: 10.1016/j.drugalcdep.2012.07.017
72. Weiss NH, Tull MT, Viana AG, Anestis MD, Gratz KL. Impulsive behaviors as an emotion regulation strategy: examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. J Anxiety Disord. (2012) 26:453–8. doi: 10.1016/j.janxdis.2012.01.007
73. Hembree EA, Street GP, Riggs DS, Foa EB. Do assault-related variables predict response to cognitive behavioral treatment for PTSD? J Consult Clin Psychol. (2004) 72:531–4. doi: 10.1037/0022-006X.72.3.531
74. Zhai ZW, Yip SW, Lacadie CM, Sinha R, Mayes LC, Potenza MN. Childhood trauma moderates inhibitory control and anterior cingulate cortex activation during stress. Neuroimage. (2019) 185:111–8. doi: 10.1016/j.neuroimage.2018.10.049
75. Smith JL, Mattick RP, Jamadar SD, Iredale JM. Deficits in behavioural inhibition in substance abuse and addiction: a meta-analysis. Drug Alcohol Depend. (2014) 145:1–33. doi: 10.1016/j.drugalcdep.2014.08.009
76. Sofuoglu M, Rosenheck R, Petrakis I. Pharmacological treatment of comorbid PTSD and substance use disorder: recent progress. Addict Behav. (2014) 39:428–33. doi: 10.1016/j.addbeh.2013.08.014
77. Petrakis IL, Poling J, Levinson C, Nich C, Carroll K, Ralevski E, et al. Naltrexone and disulfiram in patients with alcohol dependence and comorbid post-traumatic stress disorder. Biol Psychiatry. (2006) 60:777–83. doi: 10.1016/j.biopsych.2006.03.074
78. Petrakis IL, Ralevski E, Desai N, Trevisan L, Gueorguieva R, Rounsaville B, et al. Noradrenergic vs serotonergic antidepressant with or without naltrexone for veterans with PTSD and comorbid alcohol dependence. Neuropsychopharmacology. (2012) 37:996–1004. doi: 10.1038/npp.2011.283
79. Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav. (2012) 37:11–24. doi: 10.1016/j.addbeh.2011.09.010
Keywords: post-traumatic stress disorder (PSTD), substance use disorder, dual disorder (DD), craving, integrated treatment, systematic (literature) review
Citation: Renaud F, Jakubiec L, Swendsen J and Fatseas M (2021) The Impact of Co-occurring Post-traumatic Stress Disorder and Substance Use Disorders on Craving: A Systematic Review of the Literature. Front. Psychiatry 12:786664. doi: 10.3389/fpsyt.2021.786664
Received: 30 September 2021; Accepted: 16 November 2021;
Published: 14 December 2021.
Edited by:
Georges Brousse, Université Clermont Auvergne, FranceReviewed by:
Xi Zhu, Columbia University, United StatesCopyright © 2021 Renaud, Jakubiec, Swendsen and Fatseas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melina Fatseas, bWVsaW5hLmZhdHNlYXNAdS1ib3JkZWF1eC5mcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.