- 1Department of Psychiatry, University of Occupational and Environmental Health, Kitakyushu, Japan
- 2Department of Environmental Epidemiology, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Japan
- 3Department of Occupational Medicine, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Japan
- 4Department of Mental Health, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Japan
- 5Department of Environmental Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Japan
- 6Department of Work Systems and Health, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Japan
- 7Department of Occupational Health Practice and Management, Institute of Industrial Ecological Sciences, University of Occupational and Environmental Health, Kitakyushu, Japan
- 8Department of Preventive Medicine and Community Health, School of Medicine, University of Occupational and Environmental Health, Kitakyushu, Japan
Background: The current coronavirus (COVID-19) pandemic has had large impacts on society, including people practicing social distancing. This behavioral response has increased loneliness. Loneliness not only increases the risk of psychiatric disorders, but also affects occupational mental health. To avoid the negative effects of isolation, it is important to have social contact with other people, especially family members. Employment and economic instability caused by COVID-19 may have also affected family relationships. It is important to understand the association between family relationships and loneliness in workers under the pandemic.
Methods: We collected usable data from 27,036 Japanese workers who completed an online survey during the COVID-19 pandemic. Participants were asked how long they spend with members of their family during mealtimes or at home, and if they experienced loneliness; the latter was assessed by a single question. Other questions included whether participants lived with their spouse, or with someone in need of care. To estimate the odds ratios (ORs) of time with family associated with loneliness we used a multilevel logistic model nested in the prefecture of residence, with adjustments for age, sex, marital status, presence of a cohabitant requiring care, equivalent income, educational level, number of employees in the workplace, frequency of remote work, availability of someone for casual chat, smoking, drinking, time for leisure interests, and cumulative rates of COVID-19 in the prefecture.
Results: Ten percent (2,750) of the 27,036 participants reported loneliness. The survey showed a significant negative correlation between time spent with family and loneliness (p < ‘0.001): participants who spent more time with family were less likely to feel loneliness. In addition, not living with a spouse and living with someone in need of care were associated with loneliness (not living with a spouse: p < 0.001; living with someone in need of care: p < 0.001).
Conclusion: Loneliness under COVID-19 pandemic conditions was negatively associated with time spent with family members, with the converse result found for participants cohabiting with someone in need of care. These associations suggest the potential value of changes to working practices and interventions to combat loneliness.
Introduction
The coronavirus (COVID-19) outbreak caused by SARS-CoV-2 in December 2019 has resulted in a global pandemic that has led to multiple public health issues related to mental health (1). A wide-range of age groups, including adolescents and the elderly, have experienced mental health problems during the pandemic (2, 3). Similar findings have been reported for groups including pre-infected people and cancer survivors (4, 5). COVID-19 is highly infectious and can lead to serious illness, so efforts to prevent the spread of the disease have been implemented worldwide. The strongest effort was to lock down cities and restrict human movements and contacts. In addition, WHO recommended avoiding the “Three Cs,” namely closed spaces, crowded places and close-contact settings, to minimize transmission of the disease. Furthermore, to restrict people's movements, the Japanese government requested companies to implement remote work, which many companies urgently adopted. Remote work reduces opportunities to communicate with workmates and to receive support from the workplace (6). Although these infection control measures are considered effective in preventing the spread of disease, they also potentially increase the risk of loneliness and mental health problems, both of which have become new public health challenges (7). The increase in loneliness, in particular, has been attributed to the loss of contact with others and of usual routines due to the COVID-19 pandemic-related introduction of social distancing (8).
Loneliness is defined as “a distressing feeling that accompanies the perception that one's social needs are not being met by the quantity or especially the quality of one's social relationships” (9). Biologically, it has been linked to activity in the ventral striatum and parietal junction (10), while epidemiologically it has been linked to social status factors such as education, and income (11, 12). Loneliness is associated not only with psychological distress (13, 14), but also depression and anxiety (15, 16), sleep disorders (17), alcoholism (18), Alzheimer's disease (19), and other psychiatric disorders. Loneliness is also associated with increased mortality and suicidal ideation (20, 21). In Japan, suicides attributed to loneliness have increased rapidly since the pre-COVID-19 pandemic period (22). Loneliness may influence not only mental health in general, but also occupational mental health. For example, workers with loneliness are more likely to feel low job satisfaction and express frustration (23).
To avoid isolation, it is important to have contact with other people. It is generally considered that people have the highest frequency of contacts with family members (24). Family involvement is not only related to frequency of social contacts, but also to reported levels of happiness (25). People living alone reported more loneliness than those living with others (26). Another study showed that people without partners, such as divorcees and widows, were more likely to have loneliness (16). On the other hand, people living with family members in need of care are more susceptible to feeling stressed due to the burden of care (27). Therefore, it can be hypothesized that spending time with close family members may reduce loneliness, but this effect may vary depending on the family situation.
We hypothesized that workstyle changes resulting from the COVID-19 pandemic, such as remote work, have resulted in reduced opportunities to interact with others and have led to increased loneliness among workers. At the same time, as remote work continues to increase due to the COVID-19 pandemic, workers are released from commuting time and therefore have more time to spend with their families. In fact, before COVID-19, remote work was recommended in Japan from the perspective of work-life balance. However, employment and economic problems caused by COVID-19 may have also affected family relationships. Therefore, this study aimed for a better understanding of the association between family relationships and loneliness in workers during the COVID-19 pandemic.
Methods
Study Design and Participants
We conducted an online survey from December 22 to 26, 2020, under the Collaborative Online Research on the Novel-coronavirus and Work (CORoNaWork) Project. Information about the protocol for this cross-sectional study has already been published (28). The target population comprised workers with a full-time employment contract at that time. The survey was conducted by Cross Marketing Inc. (Tokyo, Japan), which has 4.7 million registered monitors. E-mail invitations to participate were sent to 605,381 monitors. Of these, 55,045 answered the initial screening questions, of whom 33,302 matched the survey's inclusion criteria (relating to worker status, region, sex, and age) and responded to the survey. A further 215 respondents were excluded because they were deemed to have provided false responses by Cross Marketing Inc, leaving a total of 33,087 participants eligible respondents who completed the survey. Of these, 6,051 completions identified as containing invalid responses or response errors were excluded. Exclusion criteria included extremely short response time (≤6 min), extremely low reported body weight (<30 kg), extremely short reported height (<140 cm), inconsistent answers to similar questions throughout the survey (e.g., about marital status and area of residence), and wrong answers to a question designed to identify fraudulent responses (“Choose the third largest number from the following five numbers.”). Protocols in peer-reviewed journals show that several characteristics of excluded groups differ from those of included groups (28). In total, 27,036 completed surveys were available for analysis. Participants were not compensated for participation. The study was approved by the ethics committee of the University of Occupational and Environmental Health, Japan. Participants provided informed consent by filling out a form on the survey website.
Assessment of Time Spent With Family During Mealtimes or at Home
The survey included questions designed to find out how much time participants spend with their family for meals or simply at home. To the question: ”How long do you spend with family having a meal or at home?” participants selected one of the following options: more than 2 h, more than 1 h, more than 30 min, <30 min, and almost never. The following questions were also included in the survey, and required “Yes” or “No” answers: “Do you live with your spouse?” and “Do you live with someone in need of care?”
Assessment of Loneliness
One question focused on whether the participants experienced loneliness or not. To the question: “During the last 30 days, how frequently have you felt loneliness?” participants selected one of the following options: never, a little, sometimes, usually, always. Answers “always,” “usually,” or “sometimes” were taken as indicating loneliness.
Other Covariates
The following demographic and socioeconomic factors were included as covariates: age, sex, marital status, presence of a cohabitant in need of care, equivalent income, educational level, number of employees in the workplace, frequency of remote work, presence of someone for casual chat, smoking, drinking, time for leisure interests and cumulative rates of COVID-19 in the prefecture of residence.
The cumulative incidence of COVID-19 in the prefecture of residence between the time of the survey and 1 month later was used as a community-level variable. The relevant information was obtained from public institution websites.
Statistical Analysis
We used a multilevel logistic model to estimate odds ratios (ORs) for time spent with family during mealtimes or at home and loneliness. Loneliness was identified only if participants answered always, usually, or sometimes to that question. The multivariate model was adjusted for the factors: age, sex, marital status, presence of a cohabitant in need of care, equivalent income, educational level, number of employees in the workplace, frequency of remote work, presence of someone for casual chat, smoking, drinking, time for leisure interests and cumulative incidence rate of COVID-19 in the prefecture.
P-values below 0.05 were considered statistically significant. All analyses were run on Stata Statistical Software Release 17. (StataCorp LLC, College Station, TX, USA.).
Results
Table 1 shows the basic characteristics of the participants. Ten percent (2,750) of the 27,036 participants experienced loneliness. When asked about time spent with family, the largest group (26.6%) answered “almost never;” however, among participants with loneliness, 46.1% answered “almost never” to this question. Of those who spent more than 2 h with family, 9.9% had loneliness. Notably, the incidence of loneliness decreased as the time spent with family increased. In addition, loneliness was reported less frequently by participants who lived with their spouse, but more frequently by those living with someone in need of care.
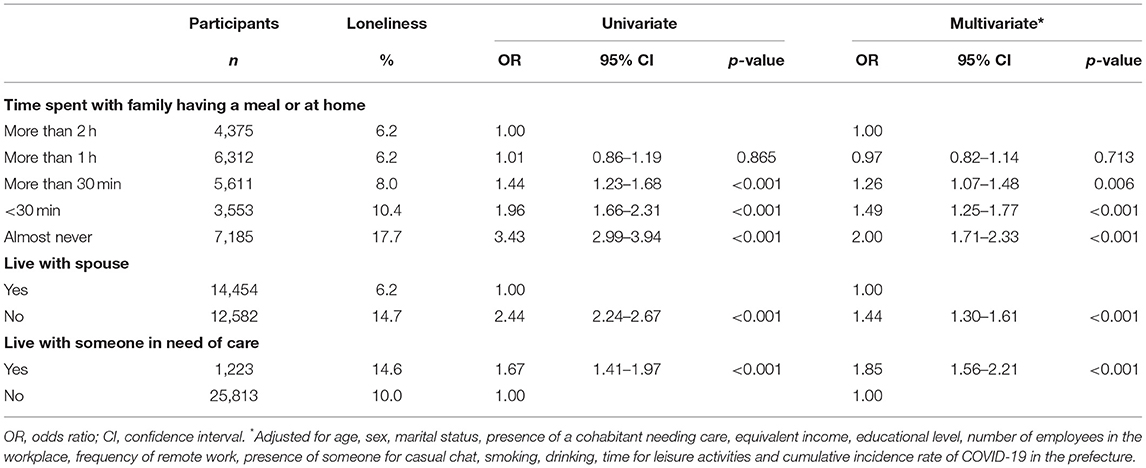
Table 2 shows the odds ratio (OR) of time spent with family and loneliness estimated by the logistic model. The age-sex adjusted OR of loneliness for those who reported spending little or no time with family indicated a significant association (OR = 3.43, 95% CI 2.99–3.94, p < 0.001). This result was similar with multivariate analysis (OR = 2.00, 95% CI 1.71–2.33, p < 0.001). In addition, not living with a spouse and living with someone in need of care were associated with loneliness (OR = 2.44, 95% CI 2.24–2.67, p < 0.001, and OR = 1.67, 95% CI 1.41–1.97, p < 0.001, respectively). Again, similar results were obtained with multivariate analysis (not living with a spouse: OR = 1.44, 95% CI 1.30–1.61, p < 0.001; living with someone in need of care: OR = 1.85, 95% CI 1.56–2.21, p < 0.001).
Discussion
This study showed that during the COVID-19 pandemic, workers in Japan who spent less time with their families were more likely to report loneliness. Those who did not live with their spouse were also more likely to feel lonely than those who did live with their spouse. Another study conducted during the COVID-19 pandemic similarly found that people who were not living with a partner felt lonely (29). However, time spent with family members in need of care and attention was associated with more loneliness.
The relationship between time spent with family and loneliness showed a dose-response function: the shorter the time spent with family, the greater the likelihood of feeling lonely. These results were robust even after adjusting for factors such as income, social status, and education, which have been reported to be associated with loneliness in previous studies. Time spent with family members is thought to contribute to well-being because of the social integration provided by the family, enhanced importance of the self, and the accessibility of social support (24). Low well-being is correlated with loneliness (30), possibly further illustrating the relationship between time spent with family and loneliness. Previous studies have also reported that living without a partner is a contributory factor in loneliness (31), while others have suggested that not only cohabitation but also the strength of the relationship between partners modulates the intensity of loneliness (32). Our results provide evidence in support of the importance of strong family relationships, as the less time spent with family, the more participants were likely to report loneliness.
Biological mechanisms have been proposed to explain the association between time spent with family and loneliness. Dopamine can be involved in loneliness. Dopaminergic nerves serve in regulating reward-processing behavior mediated by pleasure and enjoyment, and emotional behaviors such as romantic love. The ventral striatum is a neurotransmitter-related region centered on dopamine and may be involved in feelings of loneliness (10). This dopaminergic function may mediate loneliness (33). In a survey of female workers on how they spend their time in daily activities, most participants described time spent with their spouse and family as enjoyable, whereas time alone was not enjoyable (34). A similar association between loneliness and family time was found in this study. Because this study assessed loneliness using the subjective question “How frequently have you felt loneliness?,” the results seem likely to be influenced by subjective experiences such as pleasure and enjoyment. We presume that dopamine nerves of the reward system are implicated in the finding that the less time spent with family, the more loneliness participants experienced.
Interestingly, loneliness varied with factors other than simple time spent with family. In contrast to living with a spouse, living with a person in need of care was strongly positively correlated with loneliness. The burden of care on family members increases not only psychological stress but also economic burden (35). A previous study reported that caring for a family member was correlated with loneliness particularly when the family members lived together (36). Research has also suggested that emotional support from others, social connections and contact with friends are important for countering caregiver's feelings of loneliness (37, 38).
This study prompts two suggestions. First, time spent with family may be useful in reducing loneliness, as the mental health impact of the COVID-19 pandemic becomes a global public health issue. Second, recommended measures for preventing COVID-19 infection, such as maintaining social distance and refraining from going out, may lead to reduced opportunities for communication with others, which may in turn negatively affect mental health (7). However, increased time spent with family due to increased time spent at home, such as in the case of remote work, may compensate for the effects of reduced opportunities for socializing. Furthermore, home-alone and single workers are a high-risk group for loneliness, and may require careful support in terms of mental well-being.
Several limitations of the present study should be addressed. First, the results are based on an Internet survey, and so the generalizability of the results is open to question. However, we purposively aimed for a diverse target population in terms of gender, occupation, and region, based on COVID-19 incidence data. Second, although there are several ways to assess loneliness (39), we did so by using a single question, following previous studies on loneliness that used a single assessment item (40). Third, causal relationships are unclear due to the cross-sectional nature of the study and the existence of unmeasured confounding factors. Fourth, in this study the problem of common-method-bias was assumed, because many standardized question options are used in internet surveys. However, we consider any impact of the common-method-bias to be small because the variance explained by Harman's one-factor test on all of the self-reported outcome measures we used, namely, the Kessler 6 scale, WFun, and Job Content Questionnaire, was 25%, which is lower than 50%. Finally, the survey was conducted during the COVID-19 pandemic, but it remains unclear how the pandemic and resulting changes in daily and occupational environments might have affected the survey outcomes.
In this study, 10% of participants reported feelings of loneliness during the COVID-19 pandemic. The feeling of loneliness was associated with time spent with family members, with contrasting results depending on the status of the cohabitants. Greater consideration should be given to interventions such as support for caregivers, and encouragement regarding remote work and other potential changes, consistent with the worker's family and living conditions.
Data Availability Statement
Data is not available due to ethical restrictions. Requests to access the datasets should be directed to Rintaro Fujii, cmludGFyb3UxMzMxJiN4MDAwNDA7Z21haWwuY29t.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the University of Occupational and Environmental Health, Japan. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YF was the chairperson of the study group. RF conceived the research questions and drafted the initial manuscript. RF conducted the statistical analysis with YF. All authors designed the research protocol, developed the questionnaire, revised, and approved the final manuscript.
Funding
This study was supported and partly funded by research grants from the University of Occupational and Environmental Health, Japan. Japanese Ministry of Health, Labour and Welfare (H30-josei-ippan-002, H30-roudou-ippan-007, 19JA1004, 20JA1006, 210301-1, and 20HB1004). Anshin Zaidan, the Collabo-Health Study Group and Hitachi Systems, Ltd. and scholarship donations from Chugai Pharmaceutical Co., Ltd. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank other members of the CORoNaWork Project: Akira Ogami, Arisa Harada, Hajime Ando, Hisashi Eguchi, Kei Tokutsu, Kosuke Mafune, Kyoko Kitagawa, Ning Liu, Rie Tanaka, Ryutaro Matsugaki, Tomohiro Ishimaru, and Tomohisa Nagata.
References
1. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. (2020) 7:883–92. doi: 10.1016/S2215-0366(20)30308-4
2. Saleem M, Bakar A, Durrani AK, Manzoor Z. Impact of perceived severity of COVID-19 (SARS-COV-2) on mental health of university students of Pakistan: the mediating role of Muslim religiosity. Front Psychiatry. (2021) 12:1216. doi: 10.3389/fpsyt.2021.560059
3. Grolli RE, Mingoti MED, Bertollo AG, Luzardo AR, Quevedo J, Réus GZ, et al. Impact of COVID-19 in the mental health in elderly: psychological and biological updates. Mol Neurobiol. (2021) 58:1905–16. doi: 10.1007/s12035-020-02249-x
4. Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236,379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. (2021) 8:416–27. doi: 10.1016/S2215-0366(21)00084-5
5. Han J, Zhou F, Zhang L, Su Y, Mao L. Psychological symptoms of cancer survivors during the COVID-19 outbreak: a longitudinal study. Psychooncology. (2021) 30:378–84. doi: 10.1002/pon.5588
6. Tavares AI. Telework and health effects review. Int J Healthc Inf Syst Inform. (2017) 3:30. doi: 10.5430/ijh.v3n2p30
7. Wickens CM, McDonald AJ, Elton-Marshall T, Wells S, Nigatu YT, Jankowicz D, et al. Loneliness in the COVID-19 pandemic: associations with age, gender and their interaction. J Psychiatr Res. (2021) 136:103–8. doi: 10.1016/j.jpsychires.2021.01.047
8. Shah SGS, Nogueras D, van Woerden HC, Kiparoglou V. The COVID-19 pandemic: a pandemic of lockdown loneliness and the role of digital technology. J Med Internet Res. (2020) 22:e22287. doi: 10.2196/22287
9. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. (2010) 40:218–27. doi: 10.1007/s12160-010-9210-8
10. Cacioppo JT, Norris CJ, Decety J, Monteleone G, Nusbaum H. In the eye of the beholder: individual differences in perceived social isolation predict regional brain activation to social stimuli. J Cogn Neurosci. (2009) 21:83–92. doi: 10.1162/jocn.2009.21007
11. Bosma H, Jansen M, Schefman S, Hajema KJ, Feron F. Lonely at the bottom: a cross-sectional study on being ill, poor, and lonely. Public Health. (2015) 129:185–7. doi: 10.1016/j.puhe.2014.11.016
12. Cohen-Mansfield J, Hazan H, Lerman Y, Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr. (2016) 28:557–76. doi: 10.1017/S1041610215001532
13. Losada-Baltar A, Jiménez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro MDS, Fernandes-Pires J, Márquez-González M. “We are staying at home” association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J Gerontol B Psychol Sci Soc Sci. (2021) 76:e10–6. doi: 10.1093/geronb/gbaa048
14. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. (2020) 324:93–4. doi: 10.1001/jama.2020.9740
15. Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. (2006) 21:140–51. doi: 10.1037/0882-7974.21.1.140
16. Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:5–13. doi: 10.1007/s00127-012-0515-8
17. Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev. (2016) 25:21–30. doi: 10.1016/j.smrv.2015.01.003
18. Akerlind I, Hörnquist JO. Loneliness and alcohol abuse: a review of evidences of an interplay. Soc Sci Med. (1992) 34:405–14. doi: 10.1016/0277-9536(92)90300-F
19. Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. loneliness and risk of Alzheimer disease. Arch Gen Psychiatry. (2007) 64:234–40. doi: 10.1001/archpsyc.64.2.234
20. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
21. Stravynski A, Boyer R. Loneliness in relation to suicide ideation and parasuicide: a population-wide study. Suicide Life Threat Behav. (2001) 31:32–40. doi: 10.1521/suli.31.1.32.21312
22. Ministry of Health, Labour and Welfare, Japan. Suicide Statistics: Each Year. Available online at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/seikatsuhogo/jisatsu/jisatsu_year.html
23. Soler-Gonzalez J, San-Martín M, Delgado-Bolton R, Vivanco L. Human connections and their roles in the occupational well-being of healthcare professionals: a study on loneliness and empathy. Front Psychol. (2017) 8:1475. doi: 10.3389/fpsyg.2017.01475
24. Elliott S, Umberson D. Recent demographic trends in the US and implications for well-being. In: Scott J, Treas J, Richards M, editors. The Blackwell Companion to the Sociology Of Families. New York, NY: John Wiley & Sons Press; Blackwell (2004). p. 34–53.
25. Herrera M, Sani F, Bowe M. Perceived family continuity: implications for family identification and psychological well-being. Soc Psychol Educ. (2011) 26:387–99. doi: 10.1174/021347411797361275
26. Rania N, Coppola I. Psychological impact of the lockdown in Italy due to the COVID-19 outbreak: are there gender differences? Front Psychol. (2021) 12:567470. doi: 10.3389/fpsyg.2021.567470
27. Schulz R, Beach SR, Czaja SJ, Martire LM, Monin JK. Family caregiving for older adults. Annu Rev Psychol. (2020) 71:635–59. doi: 10.1146/annurev-psych-010419-050754
28. Fujino Y, Ishimaru T, Eguchi H, Tsuji M, Tateishi S, Ogami A, et al. Protocol for a nationwide internet-based health survey of workers during the COVID-19 pandemic in 2020. J UOEH. (2021) 43:217–25. doi: 10.7888/juoeh.43.217
29. Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. (2020) 291:113267. doi: 10.1016/j.psychres.2020.113267
30. Gubler DA, Makowski LM, Troche SJ, Schlegel K. Loneliness and well-being during the Covid-19 pandemic: associations with personality and emotion regulation. J Happiness Stud. (2021) 22:2323–42. doi: 10.1007/s10902-020-00326-5
31. Hawkley LC, Browne MW, Cacioppo JT. How can i connect with thee? let me count the ways. Psychol Sci. (2005) 16:798–804. doi: 10.1111/j.1467-9280.2005.01617.x
32. de Jong Gierveld J, Broese van Groenou M, Hoogendoorn AW, Smit JH. Quality of marriages in later life and emotional and social loneliness. J Gerontol B Psychol Sci Soc Sci. (2009) 64B:497–506. doi: 10.1093/geronb/gbn043
33. Matthews GA, Nieh EH, Vander Weele CM, Halbert SA, Pradhan RV, Yosafat AS, et al. Dorsal raphe dopamine neurons represent the experience of social isolation. Cell. (2016) 164:617–31. doi: 10.1016/j.cell.2015.12.040
34. Kahneman D, Krueger AB, Schkade DA, Schwarz N, Stone AA. A survey method for characterizing daily life experience: the day reconstruction method. Science. (2004) 306:1776–80. doi: 10.1126/science.1103572
35. Covinsky KE, Goldman L, Cook EF, Oye R, Desbiens N, Reding D, et al. The impact of serious illness on patients' families. SUPPORT investigators study to understand prognoses and preferences for outcomes and risks of treatment. JAMA. (1994) 272:1839–44. doi: 10.1001/jama.272.23.1839
36. Bramboeck V, Moeller K, Marksteiner J, Kaufmann L. Loneliness and burden perceived by family caregivers of patients with Alzheimer disease. Am J Alzheimers Dis Other Demen. (2020) 35:1533317520917788. doi: 10.1177/1533317520917788
37. Secinti E, Rand KL, Johns SA, O'Neil BH, Helft PR, Shahda S, et al. Social correlates of mental health in gastrointestinal cancer patients and their family caregivers: exploring the role of loneliness. Support Care Cancer. (2019) 27:2077–86. doi: 10.1007/s00520-018-4467-8
38. Pinquart M, Sorensen S. Influences on loneliness in older adults: a meta-analysis. Basic Appl Soc Psych. (2001) 23:245–66. doi: 10.1207/S15324834BASP2304_2
39. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. (2010) 7:e1000316. doi: 10.1371/journal.pmed.1000316
Keywords: COVID-19, loneliness, family, workers, Japan
Citation: Fujii R, Konno Y, Tateishi S, Hino A, Tsuji M, Ikegami K, Nagata M, Yoshimura R, Matsuda S and Fujino Y (2021) Association Between Time Spent With Family and Loneliness Among Japanese Workers During the COVID-19 Pandemic: A Cross-Sectional Study. Front. Psychiatry 12:786400. doi: 10.3389/fpsyt.2021.786400
Received: 30 September 2021; Accepted: 16 November 2021;
Published: 08 December 2021.
Edited by:
André Hajek, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Zixin Lambert Li, Stanford University, United StatesFatjona Kamberi, University of Vlorë, Albania
Copyright © 2021 Fujii, Konno, Tateishi, Hino, Tsuji, Ikegami, Nagata, Yoshimura, Matsuda and Fujino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yoshihisa Fujino, emVucSYjeDAwMDQwO21lZC51b2VoLXUuYWMuanA=
 Rintaro Fujii
Rintaro Fujii Yusuke Konno1,2
Yusuke Konno1,2 Ayako Hino
Ayako Hino Kazunori Ikegami
Kazunori Ikegami Reiji Yoshimura
Reiji Yoshimura Yoshihisa Fujino
Yoshihisa Fujino