- Division of Psychiatry I, Department of Psychiatry, Psychotherapy and Psychosomatics, Medical University Innsbruck, Innsbruck, Austria
Background: The current study assesses the prevalence of burnout and psychological distress among general practitioners and physicians of various specialities, who are not working in a hospital, during the COVID-19 pandemic. Additionally in this context, contributing factors are registered.
Materials and Methods: Burnout and psychological distress were assessed with the Copenhagen Burnout Inventory (CBI) and the Brief Symptom Inventory (BSI-18). A newly developed self-reporting questionnaire was used to evaluate demographic data and pandemic-associated stress factors.
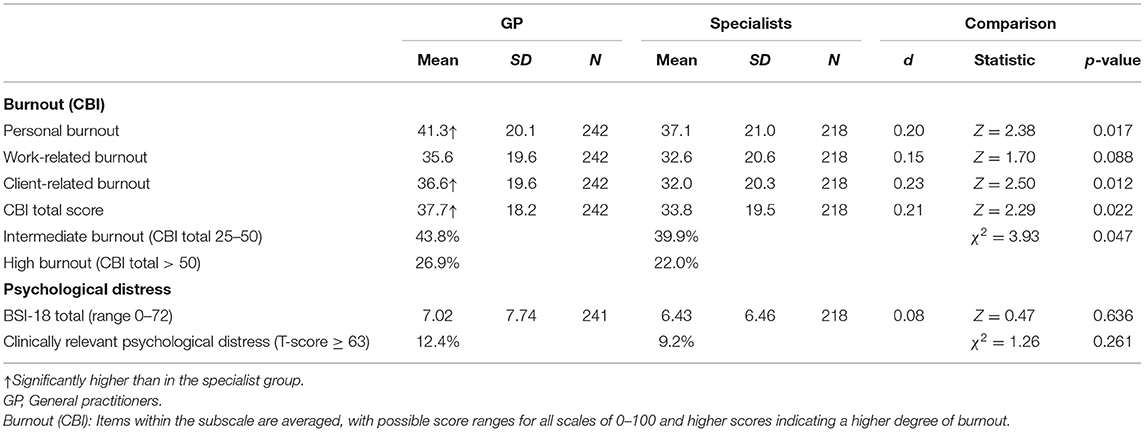
Results: 252 general practitioners and 229 private practice physicians provided sufficient responses to the outcome variables for analysis. The prevalence of clinically relevant psychological distress was comparable between groups (12.4 vs. 9.2%). A larger proportion of general practitioners than specialists had intermediate (43.8 vs. 39.9%) or high burnout (26.9 vs. 22.0%) without reaching statistical significance for either category. When combining study participants with intermediate and high levels of burnout, the group difference attained significance (70.7 % vs. 61.9%).
Conclusion: Our findings provide evidence that practicing physicians are at high risk of burnout in the context of the pandemic. Being single (standardized beta = 0.134), financial problems (beta = 0.136), and facing violence in patient care (beta = 0.135) were identified as significant predictors for psychological distress. Burnout was predicted by being single (beta = 0.112), financial problems (beta= 0.136), facing violence in patient care (beta = 0.093), stigmatization because of treatment of SARS-CoV-2-positive patients (beta = 0.150), and longer working hours during the pandemic (beta = 0.098).
Introduction
Even before the COVID-19 pandemic, physician burnout was a topic that was increasingly attracting scientific attention. Numerous studies have reported a greater prevalence of burnout amongst physicians in comparison to individuals in other careers (1), with a reported burnout rate ranging between 30 and 65% across medical specialities, with particular reference to those working on the front line of clinical care, in general internal medicine, and in emergency medicine (2).
Burnout is a psychological syndrome characterized by exhaustion, depersonalization (e.g., cynicism or negativity), and reduced professional efficacy (3). Overall, physician burnout is socio-politically important because it is associated with negative consequences on patient care, the physician workforce, healthcare system costs as well as physicians' own care and safety (4). Additionally, the literature provides indications of a correlation between burnout and an increased use of alcohol and drugs, physical exhaustion, family problems, depression, and suicide, and thus underlines the relevance of the burnout syndrome (5).
In Austria, Mayrhofer reported in 2011 (6) that 54% of the 6,249 Austrian physicians questioned showed burnout symptoms at various levels of severity. Out of those, 14% suffered from symptoms of high intensity. In 2017, Kurzthaler et al. (7) found similar results in our study about the prevalence and the severity of burnout symptoms in a sample of clinical physicians from various disciplines. These results illustrate the extent of burnout among physicians in Austria and emphasize the fact that the presence of burnout in the healthcare profession was already a serious issue before the novel coronavirus disease (COVID-19) was initially identified.
On March 11, 2020, the World Health Organization (8) officially declared the COVID-19 infection a pandemic. Studies carried out on previous outbreaks [severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), influenza, and Ebola epidemics] already describe signs of severe emotional distress in medical practitioners during outbreaks and face posttraumatic stress disorder (PTSD), depression, anxiety, and burnout after the threat of the outbreak has safely passed (9). However, the COVID-19 pandemic has intensified stressors in healthcare systems worldwide. Along with its high infection and fatality rates, it has generated a universal psychosocial impact by causing economic burden and financial losses (10). Healthcare workers in particular, such as physicians, are being affected during the COVID-19 pandemic by factors such as long working hours, enormous pressure to guard against the extreme danger of infection, shortages of protective equipment, frustration, discrimination, loneliness, and exhaustion (11). Recent literature already confirms that this wide range of occupational and personal stressors results in anxiety and depression and, simultaneously, that stress and anxiety are risk factors for the development of burnout at varying degrees (12). Noticing these scientific findings, one can argue that there will be an increase in the risk of burnout among physicians not only during but also after the COVID-19 pandemic, an escalation that is obviously dangerous especially because it arises from a pre-existing high baseline rate of burnout from before the COVID-19 pandemic.
To our knowledge, there are only a few current pieces of research that give any information about the impact of the COVID-19 pandemic on physician burnout. Wu et al. (13) first explored the prevalence of burnout amongst medical staff in China, when China was the epicenter of the virus. They reported that almost 23% of physicians had felt more burnout compared to the situation before the COVID-19 crisis. A further Italian study conducted by Giusti et al. (14) showed that more than two thirds of participants had reported moderate to severe levels of emotional exhaustion and reduced professional efficacy, and more than a quarter of the sample reported moderate to severe levels of depersonalization. At the same time, this same level of physician burnout (on average, 76%) was reported in a Romanian study by Dimitriu et al. (15). Here, the authors noted that this level of burnout was ‘superior to [that found in] studies conducted in normal periods'. The main reported predictors of burnout during the current pandemic consist of occupational factors such as place of work and increased working hours as well as the factor of female gender (5).
The aim of the current study was to evaluate the extent of burnout among general practitioners and physicians of various specialities who are not working in a hospital (referred as specialists in the rest of the manuscript) during the COVID-19 pandemic in Austria with respect to psychological distress and its underlining variable stress factors. Additionally, we focussed on the consideration of potential contributing factors and their role in physician burnout.
Materials and Methods
Study Population and Study Design
Together with the Austrian Medical Association, we conducted a cross-sectional, anonymous, self-administered, web-based study to investigate the prevalence of burnout among general practitioners and specialists during the COVID-19 pandemic. All based in Austria, practicing physicians received an email from their local medical association giving them prior notice and a study invitation together with the link and quick response (QR) code to access the electronic questionnaire. The questionnaire as well as the responses were received anonymously. The study was online from August 17th to November 22nd, 2020. Overall, 481 participants' responses were analyzed. The Ethics Committee of the Medical University Innsbruck, Austria approved the study protocol and procedures of informed consent. Participants had to answer a yes/no question to confirm their willingness to participate voluntarily. Only after confirmation of that question was the participant able to complete the self-reporting questionnaire.
Sociodemographic and COVID-19 Related Variables
In the first part of the survey, sociodemographic data were collected, including age, gender, partnership status, etc. as well as the duration of professional experience, and the location of surgery. In addition, some COVID-19 related data were collected, e.g., whether participants or their relatives had been tested positive for SARS-CoV-2, whether they had treated SARS-CoV-2-positive patients, and whether they had therefore experienced stigmatization. In addition, study participants were asked whether they felt exposed to more violence in patient care during the pandemic. An additional pool of data collected regarded the perception and acceptance of COVID-19-related measures and whether study participants had sufficient protective equipment to implement them.
Instruments
Questionnaire to Evaluate Demographic Data and Pandemic-Associated Stress Factors
We used a newly developed self-reporting questionnaire to record personal characteristics and COVID-19-related stress. The questionnaire assessed both individual and work-related strains, socioeconomic impacts (both before and during the pandemic), influence of workplace location (e.g., urban, rural, in a quarantine zone), rational understanding for preventive measures, and satisfaction with provided protective equipment as well as the information from public authorities. Additionally, physicians' fear of or concern about becoming infected with COVID-19, or transmitting it to their relatives, and affliction regarding stigma were evaluated. Most of the items had a simple binary response format (yes/no). Only a few items were open questions requiring free-text answers.
Copenhagen Burnout Inventory
The first and most commonly used instrument to evaluate burnout in different demographic and professional populations was the Maslach Burnout Inventory (MBI) (16). It became the gold standard metric of burnout. However, in recent years, authors began to criticize the unbalance and dubiety between the three dimensions of burnout evaluated by the MBI (17, 18). To cope with these shortcomings we used the newly created psychometrically valid Copenhagen Burnout Inventory (CBI) (16), which consists of three scales measuring personal burnout, work-related burnout, and client-related burnout through a 19-item survey. It allows clinicians and researchers to obtain one simple global burnout index to facilitate a clear and easy evaluation of the extent of professional burnout (19).
In the CBI, the core of burnout is fatigue and exhaustion. This is analogous with a more recent definition of burnout, which specifies this syndrome as a state of physical, emotional, and mental exhaustion that results from long-term involvement in work situations that are emotionally demanding (20). Personal burnout is the extent of physical and psychological fatigue and exhaustion experienced by the person. The work-related subscale measures the degree of physical and psychological fatigue and exhaustion that a person recognizes as work-related. Finally, the patient-related subscale shows the dimension of physical and psychological fatigue and exhaustion that a person classifies as being attributed to the work done with patients. Items within the subscales are averaged, with possible score ranges for all scales of 0–100 and higher scores indicating a higher degree of burnout. In the literature, scores of 25 or lower, 25 to 50, and higher than 50 categorize low, intermediate, and high burnout, respectively (19). Internal consistency (Cronbach's α) was excellently high with α = 0.93.
Brief Symptom Inventory
The BSI-18 (21) is a short form consisting of 18 items taken from the Symptom Checklist (SCL)-90-R. The BSI-18 assesses three six-item symptom scales—somatization, depression, and anxiety—and includes the global scale Global Severity Index (GSI). BSI-18 scores are calculated by sum scores. The total score therefore ranges from 0 to 72. The translation from raw scores into T-scores is based on gender-specific normative data from the general healthy population. As recommended by the authors of the instrument, GSI T-scores ≥ 63 were considered as clinically relevant psychological distress. Normative data for the BSI-18 derive from a sample of community-dwelling adults all employed by a single corporation in the United States, and its psychometric properties have been confirmed in a representative sample from Germany (22). The BSI-18 case-standard is identical to the standard used with the SCL-90-R. Internal consistency of BSI-18 scales as quantified by Cronbach's α ranged from 0.71 to 0.84, which is similar to the internal consistency reliabilities reported in a large sample of survivors (23), where α ranged from 0.75 to 0.88. For our sample we report a high internal consistency with α = 0.90.
Statistical Methods
IBM SPSS 26 was used for statistical analysis. For comparisons between the two physician groups regarding sociodemographic and COVID-19-related variables, Fisher's exact test, the Chi-squared test, and the Mann-Whitney U test were applied, depending on the variable type (dichotomous, categorical, or metric variables, respectively, where the majority of the metric variables had non-normal distribution). For comparisons between the situations before and during the COVID-19 pandemic, the McNemar test was used for dichotomous and Wilcoxon's matched-pairs test for metric variables with non-normal distribution. Spearman rank correlations were determined to analyze the relationship between sociodemographic and COVID-19-related variables on the one hand and burnout (CBI) as well as psychological distress (BSI-18) on the other. The size of the correlation coefficient can be interpreted as follows: r < 0.10 no correlation; r = 0.10–0.29 low correlation; r = 0.30–0.49 moderate correlation; and r ≥ 0.50 high correlation (24).
Multiple linear regression analyses were performed to investigate possible effects of demographic and COVID-19-related variables on the BSI and CBI scores of physicians. Only those COVID-19-related variables that had attained significance in the correlation analysis were considered in the regression analyses. Sociodemographic variables were entered first to adjust for potentially confounding effects. The other independent variables were entered by stepwise forward selection at a 0.05 level of significance. R squared was reported as an overall measure of goodness of fit.
Results
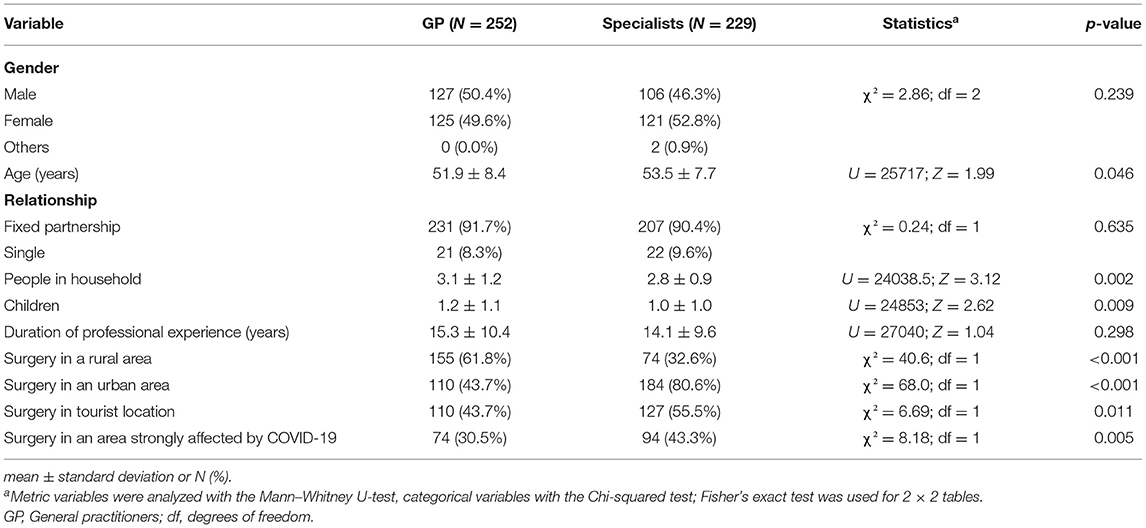
Sociodemographic Variables
In this nationwide online study, we obtained useable responses from 252 general practitioners and 229 physicians of various specialities. This accounts for ~5% of all Austrian general practitioners and 3.5% of all private practice specialists (25). The mean age of the specialist sample was higher than that of the practitioner sample. Concerning the private household members and the number of children, values were significantly higher in the group of general practitioners than in the group of specialists. The specialists' surgeries were located in urban areas, in a tourist location, or in an area strongly affected by COVID-19 more often than the general practitioners' surgeries were. Details are shown in Table 1.
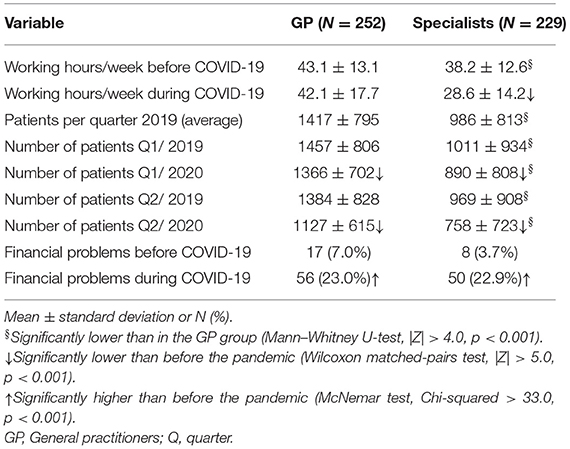
Work-Related Aspects
Details of work-related aspects before and during the COVID-19 pandemic are shown in Table 2. In the group of general practitioners, the weekly working time remained stable, whereas in the specialist group the working hours declined by ~10 h per week from 2019 to 2020 (before vs. during the pandemic). The number of patients seen per quarter decreased significantly in both groups, both in the first and second quarter of the respective years (2019 vs. 2020). In each of the groups, the percentage of respondents reporting financial problems increased considerably, from below 10% to about 23%.
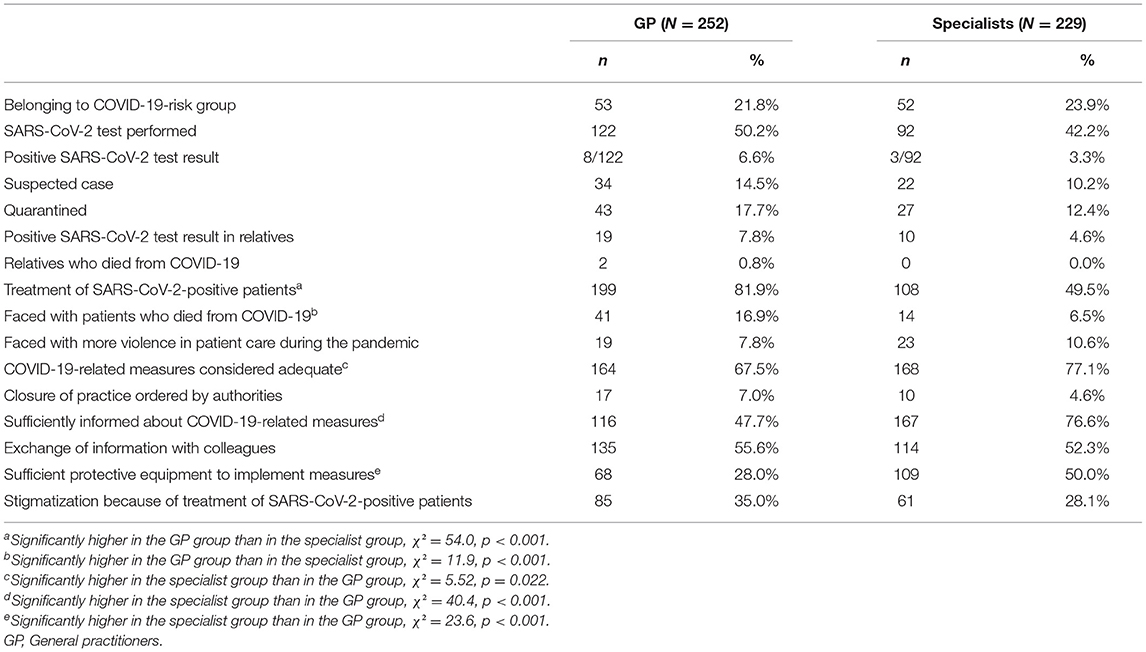
Further COVID-19-Related Variables
Table 3 shows a comparison of various other COVID-19-related variables, general practitioners were confronted with a significantly higher percentage of SARS-CoV-2-positive patients and were faced with significantly more deaths due to COVID-19 than the specialists were. Moreover, a significantly larger proportion of general practitioners had insufficient supplies of equipment to implement prescribed protective measures as compared to specialists. The COVID-19-related measures were considered to be justified by a higher percentage of specialists than general practitioners. Moreover, specialists generally felt better informed about the COVID-19-related measures than general practitioners did.
Psychological Distress and Burnout
As Table 4 shows, the two physician groups did not show significant differences in psychological distress, neither in the BSI-18 total scores nor in the prevalence of clinically relevant psychological distress (GSI T), showing values near 10% in both groups. Regarding burnout, however, general practitioners exhibited significantly higher scores in personal and client-related burnout as well as in the CBI total score. In line with the classification of burnout defined above, a larger proportion of general practitioners than specialists presented intermediate burnout (44 vs. 40%), and the same was true for high burnout (27 vs. 22%), without reaching statistical significance for either category. However, when combining intermediate and high levels of burnout, the difference attained significance (70.7 vs. 61.9%, p = 0.047).
Correlation Analyses
Findings of the correlation analyses are shown in the Appendix Table A1. Regarding sociodemographic, a younger age and the female gender were associated with higher levels of personal and work-related burnout. Single people, in contrast to those with a fixed partner, tended to have higher levels of personal burnout and psychological distress. Among work-related and COVID-19-related variables, the number of working hours in 2019 and an increase in working time from 2019 to 2020 were associated with higher levels of burnout. The latter variable also correlated with higher scores of psychological distress. Financial problems before and during the pandemic correlated with increased levels of both burnout and psychological distress. Further details can be found in Appendix Table A1. Separate correlation analyses for the two physician groups generally yielded similar findings.
Findings of Regression Analyses
Results of regression analyses for burnout are shown in Table 5A. As the findings for the individual burnout subscales were very similar, we confined this analysis to the CBI total score. The following variables were identified as significant predictors of burnout: being single, financial problems experienced during COVID-19 as well as those already experienced before, stigmatization because of treatment of SARS-CoV-2-positive patients, facing violence in patient care, and longer working hours during the pandemic. Separate regression analyses for the two groups yielded generally similar findings.
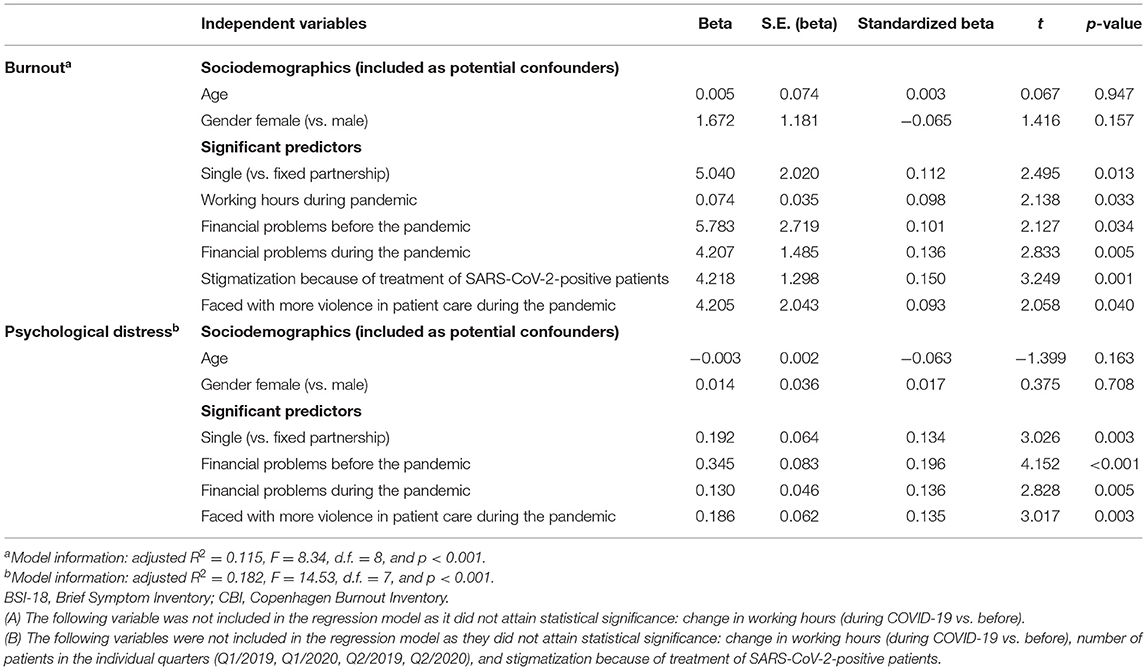
Table 5. Linear Regression—Burnout (CBI total score) (A) and psychological distress (BSI-18 total score) (B).
Findings of the regression analysis for psychological distress are summarized in Table 5B. The following variables emerged as significant predictors of psychological distress: being single, financial problems during COVID-19 as well as those already experienced before, and facing violence in patient care. Separate regression analyses for the two physician groups gave rise to similar findings.
Discussion
There is a consensus in all the relevant literature that healthcare professionals are at an increased risk of high levels of stress and burnout (26), which could have long-term psychological implications. In this national online survey, we found large proportions of physicians experiencing symptoms of burnout (general practitioners: 70%; specialists: 62%) and psychological distress (general practitioners: 12%; specialists: 9%) during the COVID-19 pandemic. Although psychological well-being was the main question, our research additionally identified factors contributing to these outcomes. We identified sociodemographic as well as work-related and specific COVID-19-related variables as risk factors that can result in physicians' impaired mental health.
Altogether, our results show a substantial increase in burnout rates compared to about 30% described for Austrian physicians in earlier studies before the COVID-19 outbreak (6, 7). Combining intermediate and high levels of burnout, the rate among general practitioners and specialists participating in this study amounted to 70.7 and 61.9%, respectively. This is an alarmingly high number and points to a particular burden in general practitioners. Compared to specialists, their workload remained unchanged during the pandemic despite a lower patient turnover. In addition, they reported significantly more frequently to be involved in the treatment of SARS-CoV-2-positive patients and/or faced with patients who died from COVID-19, to be not well informed about COVID-19-related measures, and to lack sufficient protective equipment. Among other factors, physician burnout has previously been shown to be related to lack of autonomy/control of work schedule, long work hours, financial issues, and inefficient and/or hostile work environments (27, 28). Accordingly, our finding of higher burnout rates in the general practitioner sample is not surprising.
Clinically relevant psychological distress as assessed by the BSI-18 showed comparable values of nearly 10% in both groups. Compared to the high proportion of physicians with burnout this percentage seems relatively low at first sight. One has to consider, however, that although psychological distress does not indicate mental disease but the presence of clinically relevant subjective impairment, burnout and the symptoms captured by the BSI-18 (somatization, depression, and anxiety) can be comorbid. While the society recognizes health care workers' tremendous stressors, the potential for more serious mental health crises among that profession has not received enough attention (29). Offering programs for preventive health maintenance making physicians aware of their affective response to external events like the current pandemic and appropriate mental health care is necessary to counteract psychological distress and burnout in this group. Our findings may indicate that study participants had a notable burnout symptomatology in the form of fatigue and exhaustion in the occupational context, but in a large part, they may have been able to cope, meaning that they protected themselves from developing clinically relevant psychological distress. This hypothesis cannot be tested by our data since we did not investigate coping mechanisms, however, the presence of burnout symptoms has been suggested be a risk factor for the development of clinically relevant psychological distress/mental illness (30) and accordingly, further longitudinal studies are needed to clarify this issue.
In line with previous investigations (26, 31), we detected several associations between burnout and sociodemographic, health- and work-related as well as COVID-19-related factors, even if the findings of correlation analyses were weak. However, the subsequently passed regression analyses showed single life, existing financial problems, stigmatization because of treatment of SARS-CoV-2-positive patients, and facing increased violence in patient care as predictors of both burnout and psychological distress. These findings largely corroborate those of earlier studies from other countries (32). On the other hand and contrary to previous reports, younger age and female sex were neither predictor variables for burnout nor for psychological distress among our sample. However, with regards to age one has to consider that study participants' mean age was above 50 and that the mean duration of self-employed professional experience amounted to ~15 years, whereas poor psychological outcomes have mainly been reported in young physicians at more junior career stages (32). Accordingly, our sample is not entirely comparable with others. Similarly, people with a higher burden or conversely, those with a lower burden may have been more likely to participate in the study and accordingly, a sample bias has to be taken into account. One can hypothesize that this and the fact that we exclusively investigated private practice physicians but not employed physicians may have concealed possible gender differences. However, this issue cannot be addressed by our data.
Remarkably, among both physician groups a decline in the number of patients with a medical condition showed a negative association with burnout and psychological distress. Quite to the contrary, one could assume that fewer patients to medicate would lead to a smaller workload with a reduction of psychological distress and burnout symptomatology. However, physicians probably connect a lower patient turnover with a fall in income that may initiate financial problems. Milch et al. (33), for instance, reported increased financial difficulties and financial loss in a breast imaging community during the COVID-19 pandemic and described them per se as linked with higher levels of psychological distress. This corroborates our finding of a positive association between financial problems both before and during the pandemic and psychological distress/burnout. Importantly, in comparison with the previous year's period, the percentage of physicians reporting financial problems during the pandemic tripled among general practitioners and increased six-fold in specialists. It remains to be seen whether this percentage normalizes in the course of the pandemic and whether this may subsequently be associated with a reduction in psychological distress and burnout
To add to the many challenges connected to the COVID-19 pandemic, we are seeing a worrying increase in violence against healthcare workers globally. Those attacks from patients or their relatives have been reported to often originate from the health workers' efforts to implement essential—but unpopular—COVID-19 prevention and control measures (e.g., placing a family member in a quarantine or isolation facility, or not allowing the family to attend to an infected loved one) (34, 35). This response is likely to exacerbate the already extraordinary COVID-19-related stress and burnout that healthcare workers and their families are experiencing in this pandemic. It is therefore not surprising that in the current study more violence in patient care was positively correlated with psychological distress and burnout among the general practitioners as well as among the specialists. Although generally weak, the lowest correlation was detected between the exposition to more violence in patient care and personal burnout, which is intuitively plausible
To the best of our knowledge, this is the first nationwide study conducted in Austria that investigated psychological distress and burnout among general practitioners and specialists during the COVID-19 pandemic. Notwithstanding the implications of our findings, there are a number of limitations, including the small sample size that should be considered. As mentioned above, our findings refer to a minority of Austrian general practitioners and specialists and accordingly, a sample bias has to be taken into account, which limits the generalizability of the obtained results. Those who did not respond may very well-represent those who are experiencing the most psychological distress/burnout. Secondly, the information obtained was obviously self-reported, which can result in social desirability bias. Thirdly, our participant population focused solely on general practitioners and private practice specialists and it remains to be seen if our findings can be repeated in employed physicians. Lastly, it is important to emphasize that during most time of our survey, general recommendations like the mandatory use of protective mouth/nose masks, distance keeping, and vigilant hand washing applied, whereas stricter measures were imposed by the Austrian government at the beginning of November, 2020. They were associated with a number of confinements, e.g., travel restrictions, school and University closure, closure of non-essential retail and commercial establishments, etc. Longitudinal studies are clearly needed to determine whether psychological distress/burnout in physicians changes as the pandemic continues. Notwithstanding these limitations, our study shows that during the first months of the pandemic practicing physicians were at high risk of burnout.
Conclusion
Our findings provide evidence that practicing physicians are at high risk of burnout in the context of the pandemic. Being single, financial problems, and facing violence in patient care were identified as significant predictors of burnout and psychological distress. Furthermore, burnout was predicted by stigmatization because of treatment of SARS-CoV-2-positive patients and by longer working hours during the pandemic.
Recommendations
As physician burnout impairs performance and quality of professional services with consequences for physicians, healthcare organizations, and patient outcomes, health systems are prompted to prioritize physicians' health and well-being both during and after the COVID-19 pandemic.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethikkommission Innsbruck. The patients/participants provided their online informed consent to participate in this study.
Author Contributions
IK and AH were responsible for draft writing and came up with the idea of producing this study, and also wrote the final manuscript. GK and BH took part in data collection, gave suggestion for data analysis, and assisted in transferring raw data into statistical software. All authors contributed to and approved the final report.
Funding
This work was supported by the Austrian Medical Association. The funder had no role in the design or conduct of the study; the data collection, management, analysis, or data interpretation; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.784131/full#supplementary-material
References
1. Shanafelt T, Boone S, Tan L, Dyrbye L, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. (2012) 172:1377. doi: 10.1001/archinternmed.2012.3199
2. Schrijver I. Review pathology in the medical profession?: Taking the pulse of physician wellness and burnout. Arch Pathol Lab Med. (2016) 140:976–82. doi: 10.5858/arpa.2015-0524-RA
3. World Health Organization. (2018). International Classification of Diseases for Mortality and Morbidity Statistics, 11th Revision. Available online at: https://icd.who.int/browse11/l-m/en (accessed May, 2021).
4. Dinibutun SR. Factors associated with burnout among physicians: an evaluation during a period of COVID-19 pandemic. J Healthc Leadersh. (2020) 12:85–94. doi: 10.2147/JHL.S270440
5. Shabbir A, Rashmi RS. The impact of COVID-19 on physician burnout globally: a review. Healthcare. (2020) 8:421. doi: 10.3390/healthcare8040421
7. Kurzthaler I, Kemmler G, Fleischhacker WW. Burnout in physicians. Neuropsychiatry. (2017) 31:56–62. doi: 10.1007/s40211-017-0225-2
8. World Health Organization. (2020). Coronavirus Disease 2019 Pandemic. Available online at: https://www.who.int/emergencies/disease/novel-coronavirus-2019 (accessed March 27, 2020).
9. Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. (2018) 87:123–27. doi: 10.1016/j.comppsych.2018.10.003
10. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. (2020) 14:779–88. doi: 10.1016/j.dsx.2020.05.035
11. Kang L, Li L, Hu S, Chen M, Yang C, Xiang Yang B, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
12. Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med. (2020) 21:1059–66. doi: 10.5811/westjem.2020.7.48684
13. Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson A. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manag. (2020) 60:e60–e5. doi: 10.1016/j.jpainsymman.2020.04.008
14. Giusti E, Pedroli E, D'Aniello G, Stramba Badiale C, Pietrabissa G, Manna C. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. (2020) 11:1684. doi: 10.3389/fpsyg.2020.01684
15. Dimitriu M, Pantea-Stoian A, Smaranda A, Nica A, Carap A, Constantin V, et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. (2020) 144:109972. doi: 10.1016/j.mehy.2020.109972
16. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. In: Zalaquett CP, Wood RJ, editors. Evaluating Stress: A Book of Resources. Lanham: The Scarecrow Press. Inc. (1997). p. 191–218.
17. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. (2005) 19:192–207. doi: 10.1080/02678370500297720
18. Borritz M, Rugulies R, Bjorner JB, Villadsen E, Mikkelsen OA, Kristensen TS. Burnout among employees in human service work: design and baseline findings of the PUMA study. Scand J Public Health. (2006) 34:49–58. doi: 10.1080/14034940510032275
19. Lapa T, Carvalho S, Viana J, Ferreira PL, Pinto-Gouvei J, Cabete AB. Development and evaluation of a global burnout index derived from the use of the Copenhagen Burnout Inventory in Portuguese Physicians. Acta Med Port. (2018) 31:534–41. doi: 10.20344/amp.10407
20. Schaufeli WB, Greenglass ER. Introduction to special issue on Burnout and health. Psychol Health. (2001) 16:501–10. doi: 10.1080/08870440108405523
21. Derogatis L. SI 18: Brief Symptom Inventory 18: Administration, Scoring, and Procedure Manual. Minneapolis, MN: NCS Pearson, Inc. (2001).
22. Franke GH, Jaeger S, Glaesmer H, Barkmann C, Petrowski K, Braehler E. Psychometric analysis of the Brief Symptom Inventory 18 (BSI-18) in a representative German sample. BMC Med Res Methodol. (2017) 17:14. doi: 10.1186/s12874-016-0283-3
23. Recklitis CJ, Parsons SK, Shih MC, Mertens A, Robison LL, Zeltzer L. Factor structure of the brief symptom inventory-18 in adult survivors of childhood cancer: results from the childhood cancer survivor study. Psychol Assess. (2006) 18:22–32. doi: 10.1037/1040-3590.18.1.22
24. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic (1988).
25. Österreichische Ärztekammer. Ärztestatistik für Österreich Zum. (2021). Available online at: https://www.aerztekammer.at/daten-fakten (accessed December 31, 2020).
26. Wang S, Wen X, Dong Y, Liu B, Cui M. Psychological influence of coronovirus disease 2019 (COVID-19) pandemic on the general public, medical workers, and patients with mental disorders and its countermeasures. Psychosomatics. (2020) 61:616–24. doi: 10.1016/j.psym.2020.05.005
27. Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. (2009) 144:371–6. doi: 10.1001/archsurg.2008.575
28. Kachadourian LK, Feder A, Murrough JW, Feingold JH, Kauderer HK, Charney D, et al. Transdiagnostic psychiatric symptoms, burnout, and functioning in frontline health care workers responding to the COVID-19 pandemic: a symptomics analysis. J Clin Psychiatry. (2021) 82:20m13766. doi: 10.4088/JCP.20m13766
29. Reger MA, Piccirillo ML, Buchmann-Schmitt JM. COVID-19, mental health, and suicide risk among health care workers: looking beyond the crisis. J Clin Psychiatry. (2020) 81:20com13381. doi: 10.4088/JCP.20com13381
30. Nuallaong W. Burnout symptoms and cycles of burnout: the comparison with psychiatric disorders and aspects of approaches. In: Bährer-Kohler S, editor. Burnout for Experts. Boston, MA: Springer (2013). p. 47–72.
31. Amoafo E, Hanbali N, Patel A, Singh P. What are the significant factors associated with burnout in doctors? Occup Med (Lond). (2015) 65:117–21. doi: 10.1093/occmed/kqu144
32. Fiest KM, Parsons Leigh J, Krewulak KD, Plotnikoff KM, Kemp LG, Ng-Kamstra J, et al. Experiences and management of physician psychological symptoms during infectious disease outbreaks: a rapid review. BMC Psychiatry. (2021) 21:91. doi: 10.1186/s12888-021-03090-9
33. Milch HS, Grimm LJ, Plimpton SR, Tran K, Markovic D, Dontchos BN, et al. COVID-19 and breast radiologist wellness: impact of gender, financial loss, and childcare need. J Am Coll Radiol. (2021) 1:1017–26. doi: 10.1016/j.jacr.2021.02.022
34. Forgione P. New Patterns of Violence Against Healthcare in the Covid-19 Pandemic. (2020). Available online at: https://blogs.bmj.com/bmj/2020/05/15/new-patterns-of-violence-against-healthcare-in-the-covid-19-pandemic/ (accessed May 15, 2020).
Keywords: COVID-19 pandemic, burnout, psychological distress, physicians, general practitioners
Citation: Kurzthaler I, Kemmler G, Holzner B and Hofer A (2021) Physician's Burnout and the COVID-19 Pandemic—A Nationwide Cross-Sectional Study in Austria. Front. Psychiatry 12:784131. doi: 10.3389/fpsyt.2021.784131
Received: 27 September 2021; Accepted: 12 November 2021;
Published: 07 December 2021.
Edited by:
Adriana Mihai, George Emil Palade University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureş, RomaniaReviewed by:
Liaqat Ali Khan, Ministry of Health, Saudi ArabiaMassimo Tusconi, University of Cagliari, Italy
Copyright © 2021 Kurzthaler, Kemmler, Holzner and Hofer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ilsemarie Kurzthaler, aWxzZW1hcmllLmt1cnp0aGFsZXJAaS1tZWQuYWMuYXQ=
 Ilsemarie Kurzthaler
Ilsemarie Kurzthaler Georg Kemmler
Georg Kemmler Bernhard Holzner
Bernhard Holzner Alex Hofer
Alex Hofer