
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 03 December 2021
Sec. Public Mental Health
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.769048
This article is part of the Research Topic Global Mental Health Among Marginalized Communities in Pandemic Emergencies View all 9 articles
 Kamrun Nahar Koly*
Kamrun Nahar Koly* Mosammat Ivylata Khanam
Mosammat Ivylata Khanam Md. Saiful Islam
Md. Saiful Islam Shehrin Shaila Mahmood
Shehrin Shaila Mahmood Syed Manzoor Ahmed Hanifi
Syed Manzoor Ahmed Hanifi Daniel D. Reidpath
Daniel D. Reidpath Fatema Khatun
Fatema Khatun Sabrina Rasheed
Sabrina RasheedBackground: Although mental health is an important part of health and wellbeing, very little is known about the impact of the COVID-19 pandemic on the mental health of marginalized communities like urban slum dwellers. Our study estimated the prevalence of generalized anxiety disorder and insomnia among the residents of the informal settlements of Dhaka, Bangladesh, during the COVID-19 pandemic.
Methods: A cross-sectional phone-based survey was conducted from October to November 2020 among adult residents of five informal settlements of Dhaka city randomly chosen from an existing Urban Health and Demographic Surveillance Systems (UHDSS) run by icddr,b. Data on Generalized Anxiety Disorder-7 (GAD-7) and Insomnia Severity Index (ISI) were collected. A multinomial logistic regression was performed to assess the associated factors of anxiety and insomnia.
Results: Of the total 586 participants, the prevalence of mild to severe anxiety and insomnia were 53% and 43%, respectively. As per the multinomial regression analysis, participants with mild anxiety were significantly more likely to be older (>50 years) and afraid of COVID-19 infection. Likewise, participants with moderate/severe anxiety were significantly more likely to share less household facilities (e.g., toilet, kitchen, water) (OR: 2.23; 95% CI: 1.31–3.79), to have difficulties in food availability (OR: 2.76; 95% CI: 1.10–6.93), to be afraid of self (OR: 5.27; 95% CI: 2.82–9.88), and to worry about the family members (OR: 2.26; 95% CI: 1.23–4.17) getting infected. Participants with mild insomnia were significantly more likely to share fewer household facilities and be afraid of being infected with COVID-19 infection. Moreover, participants with moderate/severe insomnia were significantly more likely to be female (OR: 1.90; 95% CI: 1.02–3.56), to receive food aid (OR: 0.50; 95% CI: 0.29–0.88), to be afraid of self (OR: 3.85; 95% CI: 1.81–8.19), and to worry about someone like friends or neighbors (OR: 2.45; 95% CI: 1.07–5.58) getting infected with COVID-19.
Conclusions: We found elevated prevalence of both anxiety and insomnia among the urban poor of Bangladesh in the context of COVID-19. This indicates the importance of integrating mental health in the mitigation and recovery efforts related to similar crises for the urban poor in the future.
Globally, the urban population has increased rapidly from 751 million in 1950 to 4.2 billion in 2018, and it is projected to increase by 68% within 2050 (1). Currently, worldwide more than 900 million people reside in the urban slums, and around 7 million live in ~3,394 slums of Dhaka, Bangladesh (2). Some of the challenges of living in urban slums include poor infrastructure, overcrowding, inadequate water supply, improper waste management, and less access to health services (3–7). The amenities available for daily living such as water and kitchen and toilet facilities are often shared by residents of the slums (8). The lives of urban working poor people were severely affected by the COVID-19 pandemic as they lost income and had to deal with the rising costs of living (8). During the COVID-19 pandemic, when movement restrictions, frequent hand washing, and maintaining social distance were promoted as preventive measures, compliance with these recommendations was particularly challenging for the residents of urban slums due to the environment they live in (9–11). In addition, several researchers have reported the poor mental health status of the slum residents due to their vulnerable socioeconomic status and the poor infrastructure of the slums in Bangladesh (12–14). The crowded living and inadequate infrastructure meant that this population was at higher risk of transmitting the disease both inside and outside their area of residence (8, 9, 15–17). The high risk of disease transmission among the residents of urban slums was likely to contribute to the high rates of COVID-19 infection among Dhaka city residents (18).
Researchers in many low- and middle-income countries (LMICs) have reported that disease outbreaks such as Ebola and influenza have led to a rise in unemployment, malnutrition, gender violence, and reduced access to healthcare services (8, 19, 20). During previous epidemics, researchers have also reported the increased of anxiety, stress, sleep, and appetite disorders (8, 21, 22). Similarly, during the current pandemic, researchers have reported rise in unemployment, food insecurity (rural and urban areas), violence, and reduction in healthcare seeking (8, 23, 24). Although the abovementioned stressors along with fear of contracting COVID-19 and stigma related to the pandemic are likely to manifest as stress and anxiety among the urban poor, very few studies have investigated the mental health implications of the pandemic for the residents of urban slums.
During the COVID-19 pandemic, there are a few studies that focused on the mental health of urban poor in Bangladesh (25–27). Most of these have investigated depression and stress and used convenient sampling procedures (25, 26). A previous study indicated the presence of anxiety and sleeping problems among slum dwellers during the pandemic (24). However, the study was conducted in a small sample and was exploratory in nature. Therefore, this study focused on the quantitative assessment of anxiety and insomnia using standardized tools among a representative sample of residents of urban slums in Dhaka city. It was hypothesized that the prevalence of anxiety and insomnia would be higher during the pandemic compared to the previous rates among the residents of urban slums in Dhaka city. The samples were drawn from an existing surveillance system of urban slum residents of Dhaka. Therefore, these study findings will help to inform future policies and programs related to the urban poor.
A cross-sectional survey was conducted among slum dwellers in Dhaka city, Bangladesh, under the Urban Health and Demographic Surveillance System (UHDSS) of icddr,b. It is a large surveillance system of icddr,b since 2015 covering 31,577 households and 121,912 individuals in five slums of the Korail, Mirpur, Shampur, Dholpur, and Gazipur areas of Dhaka North and South city corporations. Households were selected randomly with a probability proportional to size (PPS) so that the population represents the urban slums in general. From each household, one adult (≥ 18 years of age) with phone number registered with UHDSS was selected for the study interview ensuring that the male–female ratio remained similar. The residents who had migrated permanently out of the slum were excluded from the study.
As no similar studies among slum dwellers during the pandemic were available at the designing of the study, we assumed the prevalence of anxiety to be 50%. The minimum sample size (384) was estimated with an assumption of 50% poor mental health conditions with a 5% precision. Finally, a total of (384 × 1.5) 578 households were calculated with the design effect (1.5), and taking 20% non-response into consideration, ~695 households were estimated. Afterward, we determined the number of the respondents from each slum by using PPS methodology. Initially, a total of 1,519 adult slum residents (one from each household) were approached to take part in the survey. Finally, 586 participated and completed the survey, whereas 65 respondents refused to participate and 902 residents were unable to reach by phone, generating a non-response rate of 61.4%.
To avoid moving around and face-to-face contact during the government lockdown (movement and social restriction), a mobile phone-based survey was conducted. Trained research assistants who were already working within the selected communities and obtained data through phone calls after getting verbal consent by using a Bangla pretested questionnaire from the respondents. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of icddr,b.
A semi-structured questionnaire was used for data collection that included sections on socio-demographics including questions on age, sex, years of schooling, occupation, and income. Other sections included COVID-19 impact on household characteristics, food environment, and emotional wellbeing characteristics. Under the section household characteristics, we have assessed crowding index (number of people per room) and shared facilities (sharing of kitchen, toilet, and water supply). We collected questions about food availability, accessibility, and food aid under the section of food environment. Emotional wellbeing had some variables such as fear of contracting the COVID-19 infection for self, family members, and other close network; in addition, this section also measured anxiety and insomnia using two psychometric scales that have been used previously in the Bangladeshi population: the Generalized Anxiety Disorder-7 (GAD-7) scale and the Insomnia Severity Index (ISI) (28, 29).
The Generalized Anxiety Disorder (GAD-7) includes seven questions about symptoms of anxiety experienced over the last 2 weeks. Each question is scored on a four-point Likert scale (from “0 = not at all” to “3 = almost every day”). The total score ranges from 0 to 21 and is obtained by summing the raw scores of the seven items. A higher score is indicative of greater anxiety. In the present study, the following GAD-7 cutoffs were considered for assessing anxiety: > 15 for “severe anxiety”; 10–14 for “moderate anxiety”; 5–9 for “mild anxiety”; and < 5 considered was “minimal anxiety” (28). The Cronbach's alpha for GAD-7 in the present study was 0.94, indicating excellent reliability.
The Insomnia Severity Index (ISI) scale consists of seven items related to symptoms of insomnia over the past 2 weeks scored on a five-point Likert scale (e.g., “0 = Not at all” to “4 = Nearly every day”). The total score is obtained by summing the item scores. Individual scores range from 0 to 28, with higher scores reflecting more severe insomnia. The following ISI cutoffs were used for assessing insomnia; 22–28 for “severe insomnia”; 15–21 for “moderate insomnia”; and 8–14 for “mild” or “subthreshold insomnia”—and < 8 was considered as “minimal insomnia” (29). The Cronbach's alpha for the ISI in the present study was 0.80.
The descriptive statistics were computed for each variable. The bivariate analysis (i.e., Chi-square tests, Fisher's exact tests) were computed to assess the association between independent variables and outcome variables (i.e., anxiety and insomnia). Multinomial logistic regression analysis was performed involving all examined variables together to determine the associated factors of anxiety and insomnia categories (mild and moderate/severe). During regression analysis, “minimal” categories were kept as reference. Before performing the multinomial logistic regression models, multi-collinearity was checked. The multi-collinearity was absent as all values of the tolerance and variance inflation factor (VIF) were > 0.1 and < 2, respectively (30). All the studied variables were based on the previous literature which were included in the multinomial logistic regression models. Thus, it is expected that all the potential confounders have been adjusted. A p < 0.05 was considered as a statistically significant association. SPSS software (version 25) was used to analyze data.
Out of the 586 study participants, 50.9% were males; 48.6% were of 31–50 years old; 50.9% had 5–10 years of schooling; and 35.2% were housewives or students followed by 30.2% unemployed or daily wager. About 93.7% of respondents reported that COVID-19 had adversely affected their household income (Table 1).
Among the 586 study participants, 53.0% had mild to severe anxiety, and 43.0% had mild to severe insomnia (Figure 1). About a quarter of respondents had mild anxiety symptoms (25.4%), and a little under one-third had mild insomnia symptoms (30.2%). About 14.2% of respondents experienced moderate anxiety, and 10.1% had moderate insomnia. Severe anxiety was observed in about 13.3% of people and 2.6% experienced severe insomnia.
Figure 2 represents the participants' symptoms of anxiety and insomnia during the COVID-19 pandemic. About 61.3% of the slum residents experienced either anxiety or insomnia or both, 34.5% had both anxiety and insomnia symptoms, 18.4% experienced only anxiety, and 8.4% experienced only insomnia.
The distributions of minimal, mild, and moderate/severe anxiety and insomnia are presented in Tables 2, 3. During the Chi-square test, we found that anxiety was significantly associated with shared facilities, food availability, food purchasing ability, being afraid of being infected by COVID-19, and being worried about family members being infected (Table 2). On the other hand, insomnia was significantly associated with sex, shared facilities, food purchasing ability, being afraid of being infected by COVID-19, being worried about family members being infected, and having someone like friends or neighbors getting infected (Table 3).
A multinomial logistic regression evaluated the associated factors of anxiety and insomnia categories (mild and moderate/severe). The reference group was minimal anxiety and insomnia, respectively. Participants with mild anxiety were significantly more likely to be of older age (> 50 years) (OR: 2.11; 95% CI: 1.00–4.42, p < 0.05) and to be afraid of being infected by COVID-19 (OR: 2.65; 95% CI: 1.41–4.98, p < 0.01; Table 4). Likewise, participants with moderate/severe anxiety were significantly more likely to share fewer household facilities (OR: 2.23; 95% CI: 1.31–3.79, p < 0.01), to have difficulties in food availability (OR: 2.76; 95% CI: 1.10–6.93, p < 0.05), to be afraid of being infected by COVID-19 (OR: 5.27; 95% CI: 2.82–9.88, p < 0.001), and to be worried about family members to be infected (OR: 2.26; 95% CI: 1.23–4.17, p < 0.01).
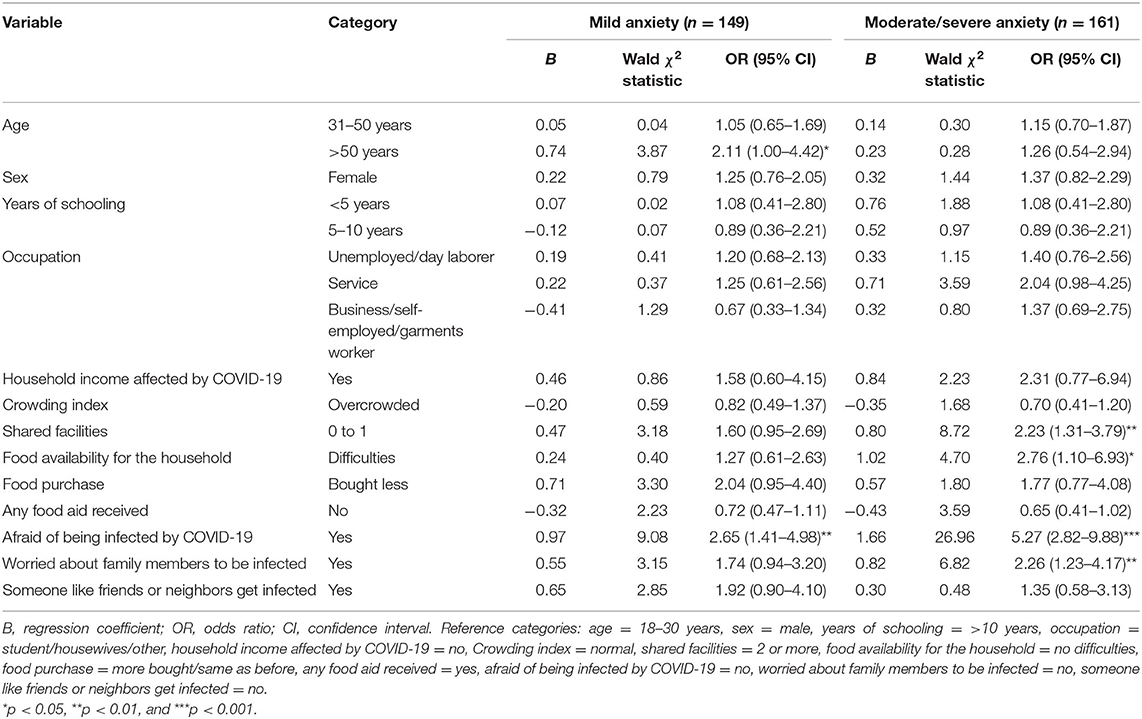
Table 4. Multinomial logistic regression differentiating minimal anxiety (n = 276) from mild and moderate/severe anxiety.
Participants with mild insomnia were significantly more likely to share fewer household facilities (OR: 2.32; 95% CI: 1.46–3.70, p < 0.01) and to be afraid of being infected by COVID-19 (OR: 3.47; 95% CI: 1.96–6.15, p < 0.01; Table 5). Likewise, participants with moderate/severe insomnia were significantly more likely to be female (OR: 1.90; 95% CI: 1.02–3.56, p < 0.05), to receive food aid (OR: 0.50; 95% CI: 0.29–0.88, p < 0.05), to be afraid of being infected by COVID-19 (OR: 3.85; 95% CI: 1.81–8.19, p < 0.01), and to be worried about someone like friends or neighbors getting infected (OR: 2.45; 95% CI: 1.07–5.58, p < 0.05).
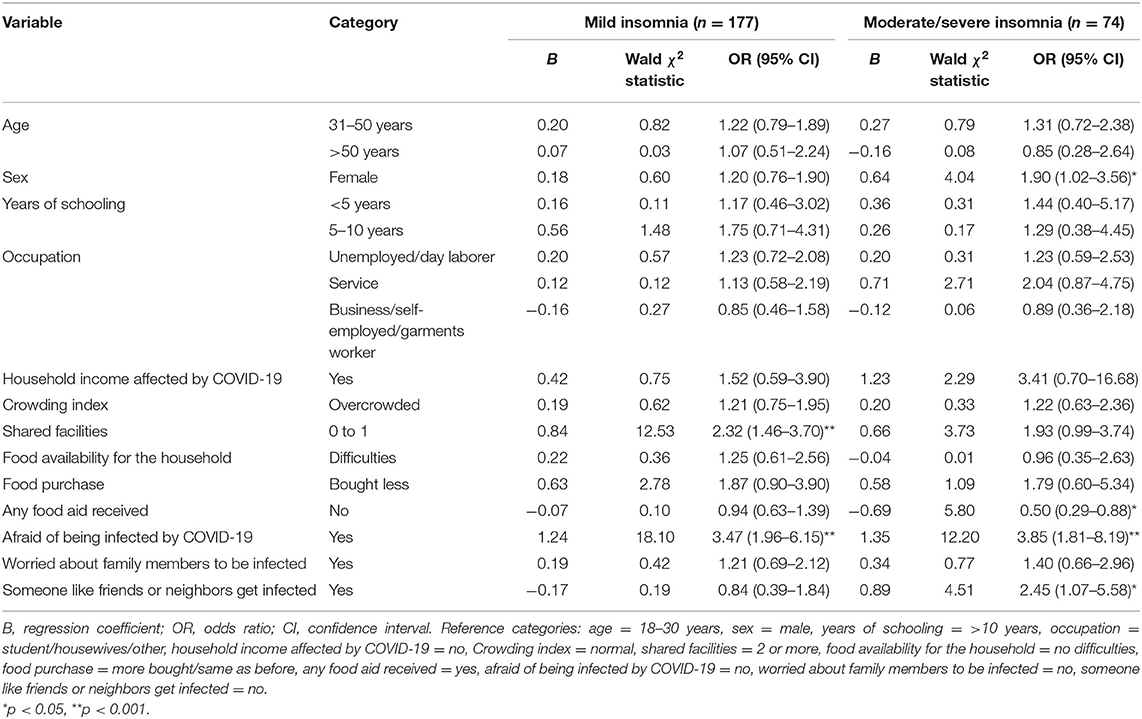
Table 5. Multinomial logistic regression differentiating minimal insomnia (n = 335) from mild and moderate/severe insomnia.
Mental health disorders contribute significantly to the global burden of diseases in LMICs including Bangladesh. Previously researchers found that the mental health of the urban poor was worse than that of the rural poor (31, 32). To date, the impact of the current pandemic on mental health has been studied among young adults and rural women, but the residents of urban slums have been understudied in Bangladesh (31). Our study was the first to examine the impact of the COVID-19 pandemic on mental health (anxiety and insomnia) among people living in urban slums of Bangladesh. The prevalence of mild to severe anxiety and insomnia was 53 and 43%, respectively. Being over 50 years of age and worrying about contracting COVID-19 was significantly associated with risk of mild anxiety. Having less shared facilities, difficulty in availing food, and worries related to COVID infection among self or family members were significantly associated with risk of moderate or severe anxiety. For insomnia, sharing of household facilities was negatively associated and worry about infection was positively associated with mild insomnia. Being female, receiving food aid, and worrying about infection were significantly associated with moderate or severe insomnia.
During this pandemic, there seem to have been a rise in the rates of general mental health conditions such as anxiety and insomnia among the residents of slums in Dhaka city. In studies prior to the COVID-19 pandemic, researchers reported rates of anxiety in urban slum dwellers in Bangladesh to be between 10 and 38% and insomnia to be 18% (33–39). However, in this current study, the rates of anxiety and insomnia were 53 and 43%, respectively, indicating a general decline in mental health status among the urban poor. A similar rise in anxiety disorders was reported among urban poor in India, China, and UK during the COVID 19 pandemic (40, 41). None of the studies described prevalence of insomnia. In addition to individual conditions, about 34.5% respondents presented with both conditions, which can be even more detrimental to the over wellbeing, making them vulnerable to their family members and societies (42). Also, it is important to note that researchers have reported the bidirectional relationship between insomnia and anxiety where anxiety could induce insomnia and vice versa (43, 44).
With regard to age, our study findings showed that people with higher age groups (≥50 years) have a significantly greater risk of anxiety than younger people. Prior to the pandemic, evidence from Bangladesh and India also documented that older people are disproportionately affected by mental illness due to the underlying long-term chronic illness, dependency on their family members, loneliness, etc. (45, 46). Several studies conducted during the COVID-19 pandemic reported that government-imposed isolation causes decrease in wellbeing, lack of social activities, and increase in loneliness leading to have severe impact on mental health particularly among older people (47–50).
In this current study, insomnia was found significantly higher among females compared to males during this pandemic. The global prevalence of mental illness is also found to be higher among women (24.5%) compared to men (16.3%) (51, 52). Several studies conducted during this pandemic also reported the increased rate of mental health symptoms such as anxiety and insomnia among women (53–55). A number of biological, hormonal, social, and cultural factors contribute to this gender disparity in terms of mental illness (56–58).
The significant association between increased number of shared facilities with decreased anxiety and insomnia is important to note. Although during the COVID-19 pandemic the public health officials have discouraged social interaction, our evidence suggests that sharing household facilities with other families, which is probably associated with interacting and socializing with neighbors, was beneficial for mental health as reported by researchers from India as well (59). This finding indicates that for a holistic approach to health, it is important that infection control consideration is coupled with mental wellbeing.
Among our respondents during the COVID-19 pandemic, stressors like difficulties with food availability were significantly associated with increased anxiety. Lack of availability and accessibility of food can lead to food insecurity which is a stressful experience that can result in frustration, feeling of hopelessness, alienation, and feelings of shame that may trigger new or amplify preexisting psychosocial stress (31). In previous studies, researchers have demonstrated that pandemics negatively affect food security of the poor in South Asian countries including Bangladesh (31). In the context of COVID-19, the feeling of psychosocial issues could have been compounded by the imposed social isolation and worries about new health risks (35, 60).
According to our study, participants who received food aid were significantly associated with insomnia. Over the past few years, different support programs are in place to support the residents of the informal settlements including food aids by different organizations (45, 61–64). During the initial outbreak of COVID-19, there were increased numbers of unemployment and lack of food availabilities causing most of the slum residents (31) to rely on food aids by different sources (45, 62, 63). Furthermore, in many instances during the pandemic there was an uneven, demeaning manner of food distribution, unfair political practices, and lack of proper management, documentation, and monitoring which may have rendered many residents to suffer from mental health issues such as insomnia (18, 60, 65–75).
Respondents who were afraid of contracting COVID-19 were more likely to suffer from anxiety and insomnia. Similarly, the respondents who were worried about someone with a close network getting infected had greater odds of insomnia. These findings were also in line with other Western and South Asian countries (24, 76–80). It can be assumed that fear of closed ones being infected, COVID-19-related myths, stigma, and distrust in healthcare bodies have given rise to fear and thus worsened the mental health status of the urban poor (81–83). It is important that we study how to communicate about risk management awareness measures without creating undue anxiety in the future.
Although unprecedented in scale, the experience of the COVID-19 pandemic has demonstrated the gaps in the existing social safety nets for the urban poor. In Dhaka city, 4 million of the urban population live in 5,000 slums and they are a very important part of different sectors such as RMG (readymade garments), transportation, construction, domestic workforce, and part of other local businesses (72, 73). They are a major contributor of the national economy of Bangladesh (84). In the longer term, it is crucial to plan to ensure how this population can be engaged in alternative productive employment opportunities so that they can themselves play a role in the recovery process of the consequences of the emergencies.
There were a few limitations of our study. The study was cross-sectional which means the findings presented were applicable to that point in time only and did not provide us with the insights over time. As the study relied on self-report, this might have resulted in some under- or overestimation due to recall bias or social desirability bias. Due to the restriction of the pandemic, the data were collected over phone which might cause some bias in the assessment of the mental health conditions of the respondents. Slum dwellers were not interviewed who did not have mobile phones or who could not be reached, which may lead to a kind of selection bias. Further, we do not have pre–post data of the same population to assess the additional contribution of COVID-19 pandemic in terms of mental health outcomes.
This study used the PPS methodology, which meant that the sample represents the residents of the five major informal settlements of Dhaka and Gazipur districts. We applied standard validated scales to assess the anxiety disorder and insomnia among the respondents. Furthermore, we have collected all the information just after the initial lockdown was over, which means that the findings represent the effect of the lockdown on mental health.
The findings indicate that anxiety and insomnia were prevalent and higher than previously observed. This study emphasizes the need to integrate the consideration of mental wellbeing in the infection control mechanism for the present pandemic as well as for similar situations in the future. Our study also recommends that during emergencies such as one presented by COVID-19, it is important that the health and wellbeing of the urban poor are safeguarded through a well-designed comprehensive social safety net program. Special effort could be made to educate communities about how to be safe while having social interactions. Primary care facilities could be equipped to deal with identification and referral of mental health conditions, and local opinion leaders could be engaged in talking about the importance of mental health. Finally, in the context of severe shortage of trained staff who are equipped to deal with mental health conditions, it is important that telemedicine and other online counseling facilities are made accessible and affordable for the urban poor so that their wellbeing can be ensured.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of icddr,b [PR-20075]. The participants provided their verbal consent through phone calls to participate in this study.
KK and SR: conceptualization. KK, SR, FK, SM, SH, and DR: methodology. MI, KK, MK, and SR: formal analysis and investigation. KK, MK, and MI: writing—original draft preparation. SM, SH, DR, FK, and SR: writing—review and editing. SR and DR: resources. SR: supervision. All authors have read and approved the final manuscript.
This study was funded by the Swedish International Development Cooperation Agency (SIDA), and the Grant Number was GR-01455. No other specific grant from any funding agency or from any other non-profit sectors was received for this research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank the respondents who participated in the interview and other research team members who contributed in implementing the study. icddr,b acknowledges with gratitude the commitment of (SIDA) to its research efforts. icddr,b was grateful to the Governments of Bangladesh, Canada, Sweden, and the UK for providing core/unrestricted support.
2. Friesen J, Taubenböck H, Wurm M, Pelz PF. Size distributions of slums across the globe using different data and classification methods. Eur J Remote Sens. (2019) 52:99–111. doi: 10.1080/22797254.2019.1579617
3. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. (2007) 370:859–77. doi: 10.1016/S0140-6736(07)61238-0
4. Arias-Granada Y, Haque SS, Joseph G, Yanez-Pagans M. Water and Sanitation in Dhaka Slums: Access, Quality, and Informality in Service Provision. The World Bank (2018).
5. Desa U. United Nations, Department of Economic Social Affairs, Population Division: World Urbanization Prospects, the 2009 Revision: Highlights. New York, NY: UN Publications (2010). Available online at: http://esa.un.org/unpd/wup/Documents/WUP2009 (accessed October 16, 2021).
6. Hossain KA, Roy S, Ullah MM, Kabir R, Arafat SY. COVID-19 and mental health challenges in Bangladesh. Adv Med Dent Health Sci. (2020) 3:31–3. doi: 10.5530/amdhs.2020.2.8
7. Anwar S, Nasrullah M, Hosen MJ. COVID-19 and Bangladesh: challenges and how to address them. Front Public Health. (2020) 8:154. doi: 10.3389/fpubh.2020.00154
8. Corburn J, Vlahov D, Mberu B, Riley L, Caiaffa WT, Rashid SF, et al. Slum health: arresting COVID-19 and improving well-being in urban informal settlements. J Urban Health. (2020) 97:348–57. doi: 10.1007/s11524-020-00438-6
9. Islam T, Kibria MG. Challenges to the prevention of COVID-19 spread in slums of Bangladesh. J Public Health (Oxf). (2020) 42:637–8. doi: 10.1093/pubmed/fdaa088
11. Hasan SM, Das S, Hanifi SMA, Shafique S, Rasheed S, Reidpath DD. A place-based analysis of COVID-19 risk factors in Bangladesh urban slums: a secondary analysis of World Bank microdata. BMC Public Health. (2021) 21:502. doi: 10.1186/s12889-021-10230-z
12. Gruebner O, Khan MMH, Lautenbach S, Müller D, Krämer A, Lakes T, et al. Mental health in the slums of Dhaka-a geoepidemiological study. BMC Public Health. (2012) 12:177. doi: 10.1186/1471-2458-12-177
13. Izutsu T, Tsutsumi A, Islam AM, Kato S, Wakai S, Kurita H. Mental health, quality of life, and nutritional status of adolescents in Dhaka, Bangladesh: comparison between an urban slum and a non-slum area. Soc Sci Med. (2006) 63:1477–88. doi: 10.1016/j.socscimed.2006.04.013
14. Mullick MSI, Goodman R. The prevalence of psychiatric disorders among 5-10 year olds in rural, urban and slum areas in Bangladesh. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:663–71. doi: 10.1007/s00127-005-0939-5
16. CDC. Overview and Infection Prevention and Control Priorities in Non-US Healthcare Settings. Centers for Disease Control and Prevention (2020).
17. Magalhães F. Slum Upgrading and Housing in Latin America. Washington, DC: Inter American Development Bank (2016).
18. von Seidlein L, Alabaster G, Deen J, Knudsen J. Crowding has consequences: prevention and management of COVID-19 in informal urban settlements. Build Environ. 2020:107472. doi: 10.1016/j.buildenv.2020.107472
19. Korkoyah DT Jr, Wreh FF. Ebola Impact Revealed: An Assessment of the Differing Impact of the Outbreak on the Women and Men in Liberia (2015).
20. de Francisco N, Donadel M, Jit M, Hutubessy R. A systematic review of the social and economic burden of influenza in low-and middle-income countries. Vaccine. (2015) 33:6537–44. doi: 10.1016/j.vaccine.2015.10.066
21. Lahariya C, Sharma A, Pradhan S. Avian flu and possible human pandemic. Indian Pediatr. (2006) 43:317–25.
22. Zürcher SJ, Kerksieck P, Adamus C, Burr CM, Lehmann AI, Huber FK, et al. Prevalence of mental health problems during virus epidemics in the general public, health care workers and survivors: a rapid review of the evidence. Front Public Heal. (2020) 8:560389. doi: 10.3389/fpubh.2020.560389
23. Hamadani JD, Hasan MI, Baldi AJ, Hossain SJ, Shiraji S, Bhuiyan MSA, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health. (2020) 8:e1380–e9. doi: 10.1016/S2214-109X(20)30366-1
24. Rashid SF, Aktar B, Farnaz N, Theobald S, Ali S, Alam W, et al. Fault-Lines in the Public Health Approach to Covid-19: Recognizing Inequities and Ground Realities of Poor Residents Lives in the Slums of Dhaka City, Bangladesh. (2020). doi: 10.2139/ssrn.3608577
25. Islam MS, Rahman ME, Banik R, Emran MGI, Saiara N, Hossain S, et al. Financial and mental health concerns of impoverished urban-dwelling Bangladeshi people during COVID-19. Front Psychol. (2021) 12:663687. doi: 10.3389/fpsyg.2021.663687
26. Ria AF, Raha SA, Rana S, Roy P, Aktar T, Al Mamun S, et al. Exploring the Impact of Covid-19 on Adolescents in Urban Slums in Dhaka, Bangladesh (2020).
27. Ahmed SAKS, Ajisola M, Azeem K, Bakibinga P, Chen Y-F, Choudhury NN, et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health. (2020) 5:e003042. doi: 10.1136/bmjgh-2020-003042
28. Spitzer R, Kroenke K, Williams J, Lowe B. Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. American Medical Association (2006).
29. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
30. Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. (2019) 72:558–69. doi: 10.4097/kja.19087
31. Chowdhury AI, Ghosh S, Hasan MF, Khandakar KAS, Azad F. Prevalence of insomnia among university students in South Asian Region: a systematic review of studies. J Prev Med Hyg. (2020) 61:E525–9. doi: 10.15167/2421-4248/jpmh2020.61.4.1634
32. Naveed S, Waqas A, Chaudhary AMD, Kumar S, Abbas N, Amin R, et al. Prevalence of common mental disorders in South Asia: a systematic review and meta-regression analysis. Front Psychiatry. (2020) 11:899. doi: 10.3389/fpsyt.2020.602062
33. Singh A, Arora M, Sharma V, Kotwal A. Stress: prevalence and correlates among residents of a suburban area. Ind Psychiatry J. (2019) 28:98. doi: 10.4103/ipj.ipj_33_18
34. Grover S, Sahoo S, Mehra A, Avasthi A, Tripathi A, Subramanyan A, et al. Psychological impact of COVID-19 lockdown: an online survey from India. Indian J Psychiatry. (2020) 62:354. doi: 10.4103/psychiatry.IndianJPsychiatry_427_20
35. Hombali A, Seow E, Yuan Q, Chang SHS, Satghare P, Kumar S, et al. Prevalence and correlates of sleep disorder symptoms in psychiatric disorders. Psychiatry Res. (2019) 279:116–22. doi: 10.1016/j.psychres.2018.07.009
36. Narayanan L, Pandit M, Basu S, Karmakar A, Bidhan V, Kumar H, et al. Impact of lockdown due to COVID-19 outbreak: lifestyle changes and public health concerns in India. Preprints. (2020). doi: 10.20944/preprints202006.0129.v1
37. Luo J, Zhu G, Zhao Q, Guo Q, Meng H, Hong Z, et al. Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: results from the Shanghai aging study. PLoS One. (2013) 8:e81261. doi: 10.1371/journal.pone.0081261
38. Simonelli G, Leanza Y, Boilard A, Hyland M, Augustinavicius JL, Cardinali DP, et al. Sleep and quality of life in urban poverty: the effect of a slum housing upgrading program. Sleep. (2013) 36:1669–76. doi: 10.5665/sleep.3124
39. Stranges S, Tigbe W, Gómez-Olivé FX, Thorogood M, Kandala N-B. Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep. (2012) 35:1173–81. doi: 10.5665/sleep.2012
40. Biel MG, Hamrah O. Learning from the pandemic: 'building back better' through research on risk and resilience with diverse populations. J Am Acad Child Adolesc Psychiatry. (2021) 60:445–7. doi: 10.1016/j.jaac.2021.02.001
41. Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. (2020) 6:e125. doi: 10.1192/bjo.2020.109
42. Rodríguez-Hidalgo AJ, Pantaleón Y, Dios I, Falla D. Fear of covid-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front Psychol. (2020) 11:591797. doi: 10.3389/fpsyg.2020.591797
43. Manzar MD, Noohu MM, Salahuddin M, Nureye D, Albougami A, Spence DW, et al. Insomnia symptoms and their association with anxiety and poor sleep hygiene practices among Ethiopian University Students. Nature Sci Sleep. (2020) 12:575. doi: 10.2147/NSS.S246994
44. Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
45. Farah S, Karim M, Khatun US. Health problems of the elderly population in some selected urban slums of Dhaka City. J Bangladesh Coll Physicians Surg. (2015) 33:202–6. doi: 10.3329/jbcps.v33i4.28140
46. Patel M, Bhardwaj P, Nebhinani N, Goel AD, Patel K. Prevalence of psychiatric disorders among older adults in Jodhpur and stakeholders perspective on responsive health system. J Fam Med Prim Care. (2020) 9:714. doi: 10.4103/jfmpc.jfmpc_1016_19
47. De Pue S, Gillebert C, Dierckx E, Vanderhasselt M-A, De Raedt R, Van den Bussche E. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Sci Rep. (2021) 11:1–11. doi: 10.1038/s41598-021-84127-7
48. Banerjee D. The impact of Covid-19 pandemic on elderly mental health. Int J Geriatr Psychiatry. (2020) 35:1466–7. doi: 10.1002/gps.5320
49. Brooke J, Jackson D. Older people and COVID-19 isolation, risk and ageism. J Clin Nurs. (2020) 29:2044–6. doi: 10.1111/jocn.15274
50. López J, Perez-Rojo G, Noriega C, Carretero I, Velasco C, Martinez-Huertas J, et al. Psychological well-being among older adults during the COVID-19 outbreak: a comparative study of the young-old and the old-old adults. Int Psychogeriatr. (2020) 32:1365–70. doi: 10.1017/S1041610220000964
51. Substance Abuse Mental Health Services Administration. (2017). Key Substance use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from: https://www.samhsa.gov/data/ (accessed October 16, 2021).
53. Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L. and Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. (2020) 287:112921. doi: 10.1016/j.psychres.2020.112921
54. Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. (2020) 291:113267. doi: 10.1016/j.psychres.2020.113267
55. van Nierop M, Lecei A, Myin-Germeys I, Collip D, Viechtbauer W, Jacobs N, et al. Stress reactivity links childhood trauma exposure to an admixture of depressive, anxiety, and psychosis symptoms. Psychiatry Res. (2018) 260:451–7. doi: 10.1016/j.psychres.2017.12.012
56. Melinda Smith MA, Robinson R, Jaffe J. Understanding Depression in Women. (2020). Available online at: https://www.helpguide.org/articles/depression/depression-in-women.htm (accessed October 16, 2021).
57. Islam SMS, Rawal LB, Niessen LW. Prevalence of depression and its associated factors in patients with type 2 diabetes: a cross-sectional study in Dhaka, Bangladesh. Asian J Psychiatry. (2015) 17:36–41. doi: 10.1016/j.ajp.2015.07.008
58. Bashar MI, Ahmed K, Uddin MS, Ahmed F, Emran A-A, Chakraborty A. Depression and quality of Life among postmenopausal women in Bangladesh: a cross-sectional study. J Menopausal Med. (2017) 23:172. doi: 10.6118/jmm.2017.23.3.172
59. Chauhan SK, Chauhan BG, Jungari S, Dhar M. Perceived quality of life of adolescents living in slums of Uttar Pradesh, India. Child Youth Serv Rev. (2020) 108:104646. doi: 10.1016/j.childyouth.2019.104646
60. Zhang H. The influence of the ongoing COVID-19 pandemic on family violence in China. J Fam Violence. (2020) 1–11. doi: 10.1007/s10896-020-00196-8. [Epub ahead of print].
61. Subbaraman R, Nolan L, Shitole T, Sawant K, Shitole S, Sood K, et al. The psychological toll of slum living in Mumbai, India: a mixed methods study. Soc Sci Med. (2014) 119:155–69. doi: 10.1016/j.socscimed.2014.08.021
62. Chauhan S, Aeri BT. Depression, anxiety, and stress among Indian urban affluent adults. Indian J Soc Psychiatry. (2020) 36:60. doi: 10.4103/ijsp.ijsp_115_18
63. Islam MM, Ali M, Ferroni P, Underwood P, Alam MF. Prevalence of psychiatric disorders in an urban community in Bangladesh. Gen Hosp Psychiatry. (2003) 25:353–7. doi: 10.1016/S0163-8343(03)00067-7
64. Ahmad A, Rahman I, Agarwal M. Early psychosocial predictors of mental health among Indians during coronavirus disease 2019 outbreak. J. Health Sci. (2020) 10:147–56. doi: 10.17532/jhsci.2020.950
65. Silva SA, Silva SU, Ronca DB, Gonçalves VSS, Dutra ES, Carvalho KMB. Common mental disorders prevalence in adolescents: a systematic review and meta-analyses. PLoS One. (2020) 15:e0232007. doi: 10.1371/journal.pone.0232007
66. Uphoff EP, Newbould L, Walker I, Ashraf N, Chaturvedi S, Kandasamy A, et al. A systematic review and meta-analysis of the prevalence of common mental disorders in people with non-communicable diseases in Bangladesh, India, and Pakistan. J Glob Health. (2019) 9:020417. doi: 10.7189/jogh.09.020417
67. Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. (2020) 75:12–20. doi: 10.1016/j.sleep.2020.05.011
68. Alasousi L, al Hammouri S, al Al-abdulhadi S. Anxiety and media exposure during COVID-19 outbreak in Kuwait. medRxiv [Preprint]. (2020). doi: 10.1101/2020.08.24.20180745
69. Shammi M, Bodrud-Doza M, Islam ARMT, Rahman MM. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon. (2020) 6:e04063. doi: 10.1016/j.heliyon.2020.e04063
70. Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. (2020) 17:4779. doi: 10.3390/ijerph17134779
72. Raihan S. Informal sector in Bangladesh: implications for growth and poverty. Indian J Labour Econ. (2010) 53:251–65.
74. Ahmad R. Public food distribution for poor decreases. Dhaka Tribune (2021). Available online at: https://www.dhakatribune.com/bangladesh/2021/06/22/public-food-distribution-for-poor-decreases (accessed October 16, 2021).
76. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
77. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health. (2020) 17:2032. doi: 10.3390/ijerph17062032
78. Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. (2020) 277:379–91. doi: 10.1016/j.jad.2020.08.043
79. Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. (2020) 274:1–7. doi: 10.1016/j.jad.2020.05.009
80. MacKinnon A, Madsen J, Dhillon A, Keys E, Giesbrecht G, Williamson T, et al. Sleeping for Two Structured Study Protocol (2021).
81. Rokanuzzaman M, Ali M, Hossain M, Miah M. Study on livelihood status of slum dwellers in the North Dhaka City corporation. J Environ Sci Nat Resour. (2013) 6:89–95. doi: 10.3329/jesnr.v6i2.22102
82. Alamgir M, Jabbar M, Islam M. Assessing the livelihood of slum dwellers in Dhaka city. J Bangladesh Agric Univ. (2009) 7:373–80. doi: 10.3329/jbau.v7i2.4749
83. Islam MS, Emran MGI, Rahman ME, Banik R, Sikder MT, Smith L, et al. Knowledge, attitudes and practices associated with the COVID-19 among slum dwellers resided in Dhaka City: a Bangladeshi interview-based survey. J Public Health (Oxf). (2020) 43:13–25. doi: 10.1101/2020.09.15.20195255
Keywords: public mental health, marginalized communities, slum dwellers, COVID-19, pandemic, emergency
Citation: Koly KN, Khanam MI, Islam MS, Mahmood SS, Hanifi SMA, Reidpath DD, Khatun F and Rasheed S (2021) Anxiety and Insomnia Among Urban Slum Dwellers in Bangladesh: The Role of COVID-19 and Its Associated Factors. Front. Psychiatry 12:769048. doi: 10.3389/fpsyt.2021.769048
Received: 01 September 2021; Accepted: 01 November 2021;
Published: 03 December 2021.
Edited by:
Peter Navario, New York University, United StatesReviewed by:
Sabrina Saba, University of Alberta, CanadaCopyright © 2021 Koly, Khanam, Islam, Mahmood, Hanifi, Reidpath, Khatun and Rasheed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kamrun Nahar Koly, a29seUBpY2RkcmIub3Jn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.