
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 10 December 2021
Sec. Mood Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.765129
 Ji Hyun An1
Ji Hyun An1 Kyung-do Han2
Kyung-do Han2 Jin-Hyung Jung3
Jin-Hyung Jung3 Juhwan Yoo4
Juhwan Yoo4 Maurizio Fava5
Maurizio Fava5 David Mischoulon5
David Mischoulon5 Su-Min Jung6
Su-Min Jung6 Dong Wook Shin6
Dong Wook Shin6 Kyu Yeon Hur7
Kyu Yeon Hur7 Hong Jin Jeon1,8,9,10*
Hong Jin Jeon1,8,9,10*Objectives: Although obesity is associated with increased risk for depression in patients with type 2 diabetes mellitus (DM), the relationship between body weight variability (BWV) and depression remains poorly studied. This study was to investigate the incidence of depression in patients with type 2 DM according to their BWV.
Methods: Intraindividual variation in body weight were measured in the nationwide, population-based retrospective cohort of 540,293 patients with type 2 DM from the Korean national health insurance system between 2009 and 2010. The diagnoses of new-onset depression occurring until the end of 2017 were ascertained. Risk of new-onset depression was examined using multivariate-adjusted Cox proportional hazards regression analysis by BWV quartile.
Results: 93,149 (17.2%) patients developed new-onset depression for the follow up. BWV was significantly associated with an increased risk of depression after adjusting for confounding factors. The highest BWV quartile group had a hazard ratio (HR) of 1.17 (95% CI 1.15–1.19) compared to the lowest BWV quartile group as a reference. Obese patients in the highest BWV quartile group showed 12% increased risk of depression (HR 1.12, 95% CI 1.09–1.15) while non-obese patients in the highest BWV quartile group showed 20% increased risk of depression (HR: 1.20, 95% CI: 1.17–1.23) compared to their respective lowest BWV quartile groups.
Conclusion: A higher BWV was significantly associated with an increased risk of depression in patients with type 2 DM. Thus, BWV may serve as an indicator for early detection of depression in type 2 DM patients.
For patients with type 2 diabetes mellitus (DM), weight control through lifestyle intervention is important since obesity is associated with poor metabolic outcomes such as increased blood pressure, poor glycemic control, and worsening lipid parameters (1, 2). Furthermore, there is also growing evidence that body weight variability (BWV) is associated with an increased risk of cardiovascular events or mortality in patients with DM (3–5). About 20–30% of patients with type 2 DM suffer from depression (6, 7). The presence of comorbid depression in type 2 DM patients can increase the disease burden and worsen the prognosis (8–11). This has been hypothesized to be related to an increase in allostatic load (12). In addition, obesity has been suggested as a major etiological factor to developing depression in persons with type 2 DM (13, 14), through mechanisms such as autonomic/neuroendocrine dysregulation, pro-inflammatory state, or brain structural alterations (8, 15). This suggests that the metabolic pathway might be involved in the occurrence of depression in diabetic patients. Beside obesity, BWV also occurs more often in DM patients than in the general population due to lifestyle preference (exercise, dietary habit. etc.), therapeutic intervention (antidiabetic medication), or the course of the disease (weight loss due to insufficient insulin, weight gain as a premorbid status of DM, etc.). Thus, a relationship between BWV and poor metabolic outcomes can be easily inferred, this relationship affecting psychological outcomes and body weight of diabetic patients.
Several studies have reported the association between BWV and poor mental health outcome (16–18). However, whether BWV is associated with the development of incident depression in type 2 DM is unknown. Therefore, the objective of this nationwide population study was to examine the association between BWV and development of incident depression in type 2 DM patients. Investigating the impact of intra-individual BWV would give a better understanding of depression etiology than simply measuring body weight itself in diabetic patients. We hypothesized that a higher BWV would be associated with an increased risk of depression in type 2 DM.
This study was conducted using the dataset of the Korean national health insurance system (NHIS), the single insurer managed by the Korean government. The NHIS contains complete health information of about 50 million people (97% of Korean population), including sociodemographic data, clinical diagnosis with International Classification of Disease-10 Clinical modification (ICD-10-CM) codes, treatments, and health service utilization as described elsewhere (19). The NHIS also provides national health examination programs to Koreans aged over 40 years biennially or annually to workers regardless of age to examine individual health behaviors and obtain laboratory results and anthropometric measurements. We used NHIS health data and health examinations in the study.
Among 17,498,154 patients who underwent medical examinations during the index period (from January 1, 2009 to December 31, 2010), 8,393,409 patients who completed three or more medical examinations within 5 years prior to the index period were chosen. Type 2 DM patients were defined as those who had ICD-10-CM codes of E11–E14 with at least one prescription of antidiabetic medication or with a fasting glucose level ≥ 126 mg/dL in laboratory results. Finally, 540,590 patients aged 30 years or more with type 2 DM were identified after excluding those with missing data (n = 971,316) and those with a previous history of depression or new depression diagnosis within 2 years of the index year (n = 105,676) (Figure 1). All study patients were followed up until December 31, 2016. The mean duration of follow up was 5.42 ± 1.53 years. The entire study process was approved by the Institutional Review Board (IRB) of Samsung Medical Center in Seoul, Korea (IRB No: 2020-10-034). Informed consent was waived since this research did not involve any identifiable private information of study patients.
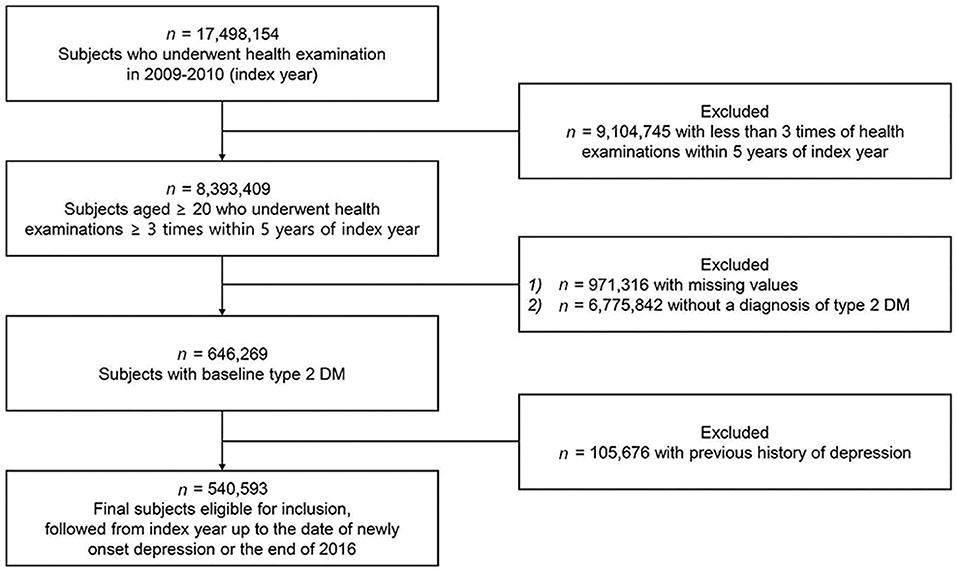
Figure 1. Flow chart showing the selection of study subjects. The target population 17,498,154 represents about one-fifth of the country's population. Type 2 DM patients were defined as those who had ICD-10-CM codes of E11-E14 with at least one prescription of antidiabetic medication or with a fasting glucose level ≥ 126 mg/dL.
The primary outcome of this study was new-onset depression defined as ICD-10-CM codes for depression (F32.0-32.9 for major depressive disorder with single episode and F 33.0-33.9 for major depressive disorder with recurrent episodes). Study patients were followed up for new-onset depression with a 2 year time lag after the index date until the diagnosis of new-onset depression, censoring by death or the end of the study (December 31, 2017).
Obesity was defined as BMI ≥ 25 kg/m2 based on the World Health Organization (WHO) recommendations for Asians (20). Three or more body weight measurements obtained within 5 years of the index period were used to calculate individual BWV. Four indices, including standard deviation (SD), coefficient of variation (CV), average successive variability (ASV) (21), and variability independent of the mean (VIM), were used to measure BWV. VIM was used as the primary measure of BWV, which was calculated as 100 × SD/meanβ, where β was the regression coefficient based on the natural logarithm of SD on the natural logarithm of the mean (22).
Baseline sociodemographic and lifestyle data included age, sex, income level (under 20% or above), current smoking status, alcohol consumption (≥ 30 g of alcohol per day indicating heavy drinking) (23), and regular exercise (vigorous physical activity three times or more per week or moderate physical activity five times or more per week) (24). A list of standardized health examination data such as height, weight, waist circumference, fasting glucose, blood pressure (systolic and diastolic), total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, and creatinine level was also included as covariates.
Baseline medical comorbidities were defined as a combination of laboratory measurement or ICD-10-CM diagnosis and prescribed medications (25, 26). Hypertension was defined as SBP/DBP ≥ 140/90 mmHg or ICD-10-CM code I10-13 or I15 with at least one prescription claim of antihypertensive medication per year. Dyslipidemia was defined as total cholesterol level ≥ 240 mg/dL or an ICD-10-CM code of E78 with at least one prescription claim of lipid lowering medication per year. Chronic kidney disease was defined as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m (27). Myocardial infarction (MI) was defined as ICD-10-CM code I12-22. Ischemic stroke was defined as ICD-10-CM I63-64 and evidence in brain CT or MRI. Atrial fibrillation was defined as ICD-10-CM I48. Malignancy was defined as ICD-10-CM C00-96 and exempted calculation code for severe disease (28). All covariates were assessed at the index date.
Baseline sociodemographic and lifestyle data, health examination data, and medical comorbidities were presented in relation to newly developed depression. We performed analysis of variance (ANOVA) for continuous variables and χ2 test for categorical variables. Patients were allocated into four groups according to BWV quartile of VIM. The risk of depression for each of the three higher quartiles of BWV (Q2, Q3, and Q4) relative to the lowest quartile (Q1) was calculated by Cox proportional hazards regression analysis after adjusting for age, sex, smoking status, drinking status, level of physical activity, low income, presence of medical comorbidities including hypertension, dyslipidemia, and variables related to severity of diabetes including insulin use, number of oral anti-diabetic medications, and duration of diabetes. Further analyses examined the relationship between BWV and risk of depression according to presence of baseline obesity to explore whether obese patients experiencing BWV were at higher risk for developing depression than non-obese patients. Kaplan-Meier estimates for incidence probability of depression were presented for BWV of each quartile group. Stratified analyses were performed for potential modification effects by age strata, sex, medical comorbidities, and variables related to the severity of diabetes. Hazard ratio (HR) of depression in stratified analyses was calculated for the highest quartile group (Q4) of BWV compared to lower quartile groups (Q1–Q3). All statistical analyses were conducted with Statistical Analysis System (SAS) version 9.4 (SAS Institute Inc., Cary, NC, USA). An alpha level of 0.05 indicated statistical significance.
Of 540,593 type 2 DM patients included in this cohort, 93,149 patients developed depression during the follow-up period (mean = 5.41 ± 1.53 years). Baseline sociodemographic and lifestyle differences between patients with and without new-onset depression are shown in Table 1. Type 2 DM patients with depression were older, more likely to be female, less likely to be smokers, and less likely to drink. They had a lower income but higher prevalence of medical comorbidities including hypertension, dyslipidemia, cardiovascular diseases, cancer, and chronic kidney disease. Type 2 DM patients with depression also had lower rate of obesity but higher BWV than those without depression.
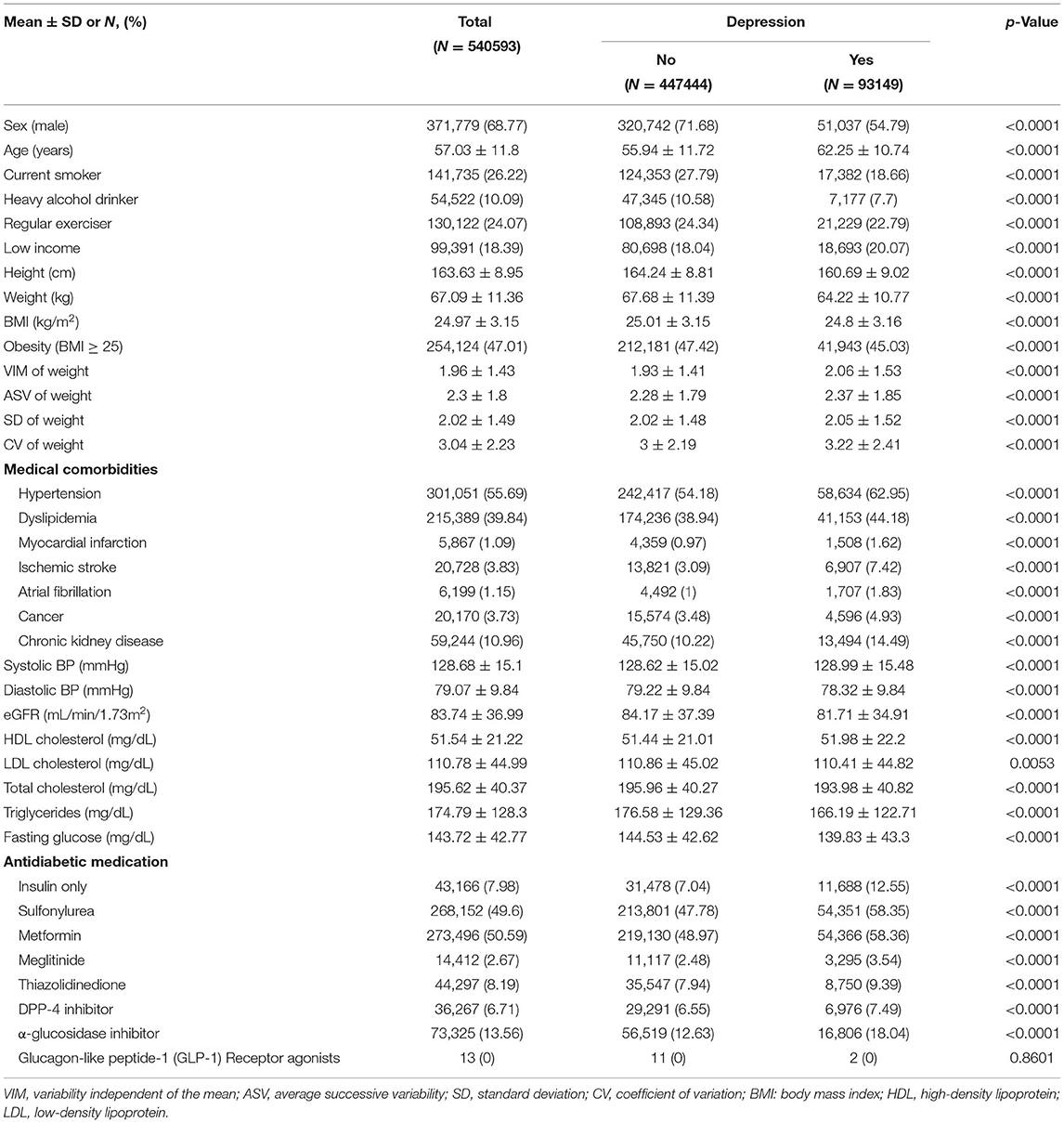
Table 1. Baseline characteristics of study patients according to the presence of new-onset depression.
Higher BWV was associated with a significantly higher rate of new-onset depression after multivariate adjustments (Table 2). Compared to the lowest BWV quartile group calculated by VIM, HR of depression for the highest quartile group was 1.17 (95% CI: 1.15–1.19). When analyzed by sex, males in the highest BWV quartile group showed a 22% greater risk of depression (HR: 1.22, 95% CI: 1.19–1.25) whereas females in the same quartile group showed a 12% greater risk of depression (HR: 1.12, 95% CI: 1.09–1.55) compared to the lowest quartile group.
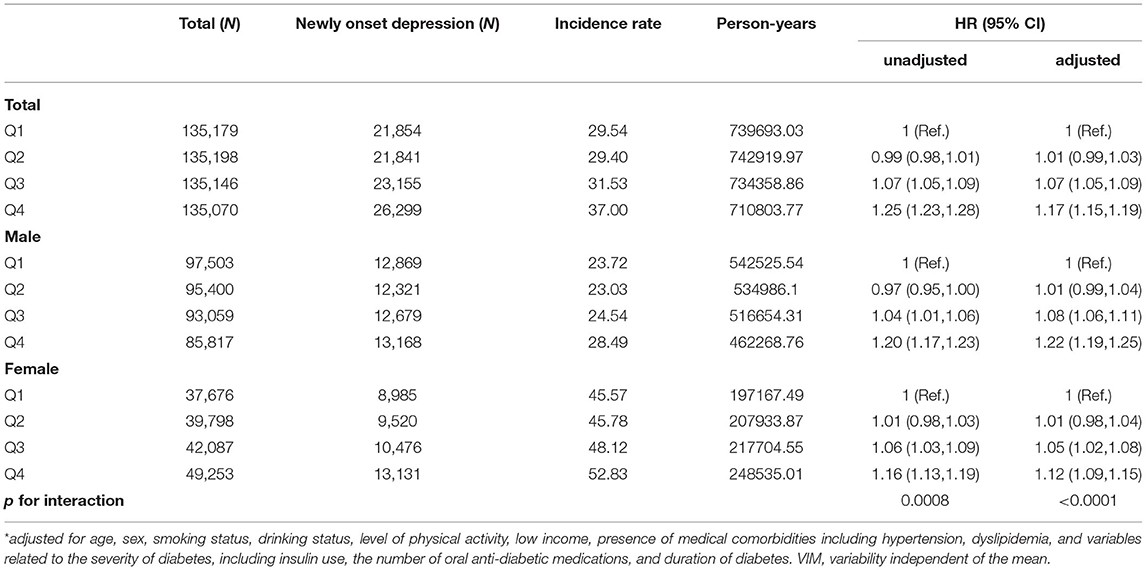
Table 2. Risk of incident depression by quartiles of VIM for body weight among patients with type 2 DM*.
In patients with baseline obesity, higher BWV numerically increased the risk of depression. Compared to the lowest quartile, obese patients in the highest BWV quartile group had a 12% greater risk of depression per the adjusted model (HR: 1.12, 95% CI: 1.09–1.15). The association was even stronger in non-obese patients, where the risk of depression increased by 20% in the highest BWV quartile group (HR: 1.20, 95% CI: 1.17–1.23) compared to the lowest quartile group (p < 0.001). A steep increase of depression risk was observed in the highest BWV quartile group compared to the lower three quartiles of non-obese type 2 DM patients (Figure 2).
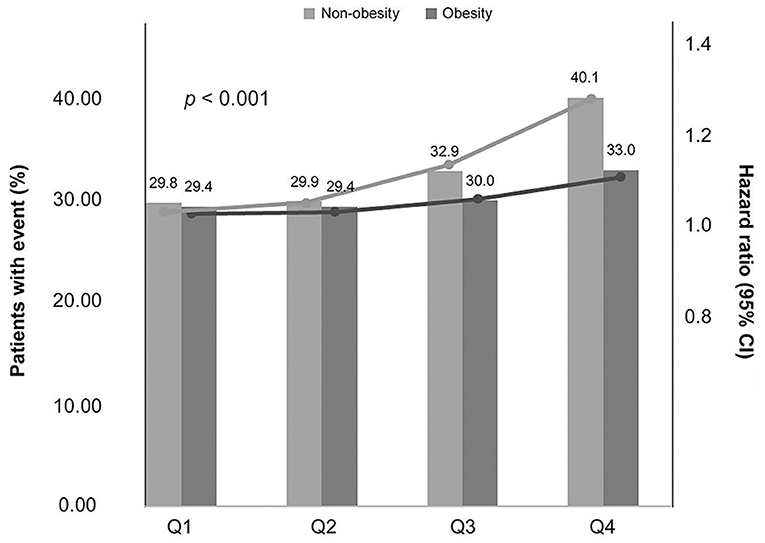
Figure 2. Association between the risk of depression and quartiles of BWV as a function of baseline obesity. The line represents depression incidence, and the bars represent HR. The P values indicate a significant difference between non-obesity and obesity in the respective BWV quartiles.
The probability of depression estimated by Kaplan-Meier curves according to each quartile of BWV was significantly increased in the highest quartile of both non-obese and obese patients with Type 2 DM, with the degree of increase being greater in the non-obese group (Supplementary Figure 1).
Figure 3 shows results of stratified analyses comparing the highest BWV quartile group to the lower three quartile groups. Higher BWV predicted increased risk of new-onset depression overall. The association was significantly stronger in males of older age, or with less severe diabetic status (i.e., use of less than two types of antidiabetic medications or shorter duration of DM) (all p < 0.05).
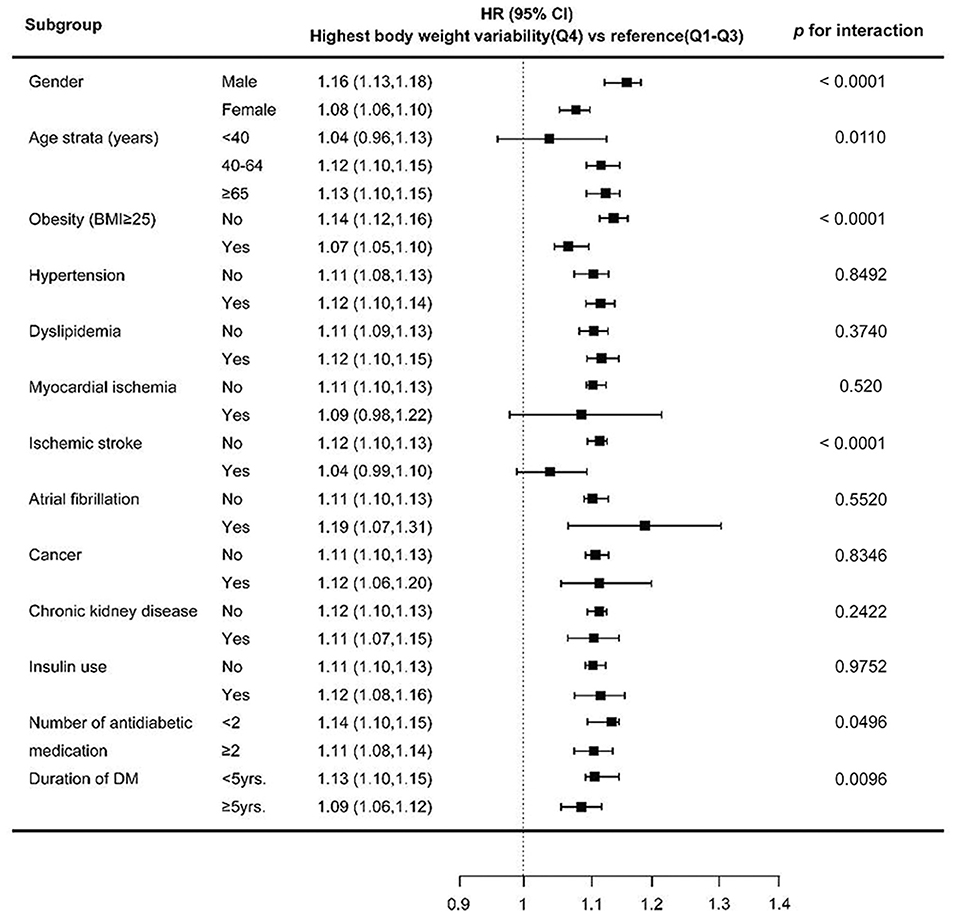
Figure 3. HR (95% CI) of depression in the highest quartile vs. lower three quartiles of BWV. Estimates were adjusted for age strata, gender, presence of obesity, medical comorbidities and severity of diabetes, except for the one stratified on. The horizontal lines represent 95 % CI. HR, hazard ratio; CI, confidence interval.
To the best of our knowledge, this is the first cohort study on the incidence of depression in type 2 DM patients with BWV. This study covered a large sample of a nationwide population (> 540,000 individuals) with a long follow up period of more than 7 years. We found that higher BWV was significantly associated with an increased risk of depression. This association was greater in non-obese patients than in obese patients independent of medical comorbidities. Stratified analysis also showed a consistent association between higher BWV and increased risk of depression. These findings may be considered to be less representative since the HR of depression in the highest BWV group are numerically small [i.e., 1.17 (95% CI 1.15–1.19) compared to the lowest BWV quartile group], but depression in diabetic patients is associated with increased mortality and worse prognosis so it should be interpreted in clinical significance.
The pathophysiological pathway underlying BWV and the development of depression has been poorly understood. Excessive weight fluctuation might cause alternation between a rapid shrinkage and a rapid expansion of adipose tissues. This mechanical cell stress to adipose tissues during weight fluctuation can result in accumulation of visceral fat mass and increased inflammatory responses of adipose cells, which could worsen vascular pathology and subsequently increase the risk of cardiovascular outcomes of patients with diabetes (15, 29). A recent study has demonstrated the association between body fat mass and depression (30), suggesting that inflammatory response during fat accumulation might also play an important role in the development of depression. Inflammatory cytokines such as tumor necrosis factor, C-reactive protein, interleukin (IL)-1b, and IL-6 are increased in depressed individuals (31). Several studies have also found that increased inflammation is associated with decreased connectivity of the dorsal/ventral striatum and ventromedial prefrontal cortex, brain regions involved in motivation and mood regulation (32, 33). Such deterioration of vascular pathology and decreased brain function caused by inflammation might have a synergistic effect on the development of depression in type 2 DM patients. Further molecular level research is needed to demonstrate the mechanisms involved in BWV-induced inflammation in depressed diabetic patients.
Another possible explanation is that endocrine factors (such as adipokines including leptin, adiponectin, and resistin, secreted by adipose tissues) might be involved in the effect of BWV on depression. Endocrine molecules, especially leptin and adiponectin, are known to be associated with depression by regulating the hypothalamic-pituitary-adrenal (HPA) axis and neuronal plasticity in the brain (34, 35). Adipose cell stress resulting from BWV could cause changes in blood levels of such adipokines, thus affecting mood regulation. Further research on such biological mechanisms is necessary.
The effect of high BWV on the development of depression in type 2 DM was greater in non-obese patients than in obese patients. Most studies examining BWV of DM patients showed a higher risk of medical complications including cardiovascular events and mortality in obese patients than in non-obese patients (3, 5, 36). Although comparative studies are lacking, psychosocial components could have more effects on the development of depression than other medical complications in type 2 DM patients. One explanation is that non-obese patients might react more sensitively to BWV than obese patients who frequently experience it because BWV is usually not a major problem for non-obese patients (whether the change is intentional or not) (37). It has been shown that body weight perception, not just actual weight itself, is associated with unhealthy weight control behaviors and depression (38). In addition, it has been increasingly reported that, besides obesity, underweight status is also associated with neuroticism, low life satisfaction, and depressed mood (39, 40). As such, BWV is not simply a metabolic consequence. Various psychological and behavioral factors might be involved in BWV. This supports our finding that the effect of BWV on depression is not limited to obese patients. Further study is needed the phenomenon of “obesity paradox” (41) is occurring psychologically as a flexible acceptance of body changes. Additionally, although the prescription rate was not high in our study cohort, glucagon-like peptide 1-receptor agonist or sodium glucose cotransporter 2-inhibitor can reduce weight during long-term use among diabetic agents, so it could be considered when interpretating higher depression risk in low BMI patients at baseline.
Also, BWV could be a consequence but not a cause of subclinical depression or other physical illness. That said, we performed several stratified analyses to minimize the effect of other causes of illness as much as possible.
Female gender is a demonstrated risk factor for developing depression. Several cross sectional studies have suggested an increased depression-obesity association in females (42). In our study as well, the prevalence of depression was higher in females. However, BWV–associated risk of depression was stronger in males.
Previous studies have mostly focused on the association between advanced stage of diabetes (more oral antidiabetic medication or longer duration of DM) and increased risk of depression in type 2 DM patients with obesity (43, 44). However, we found a reverse association between the severity of diabetes and depression in type 2 patients with BWV (i.e., the risk of depression was higher in less severe diabetic status). Although the mechanism is currently unclear, depression caused by BWV seems to have a different mechanism from depression caused by obesity in patients with type 2 DM. In addition, since men with less severe diabetes have a lower risk of depression compared to women with advanced diabetes, the relative risk of depression caused by BWV might be greater in these groups. Further research is warranted to confirm the background mechanisms and should more focus on several antidiabetic medications on the risk of depression [such as metformin, which is known to be associated with decreased rate of incident depression in recent study (45)] in time and dose dependent manner.
Several limitations should be considered when interpreting our results. First, the diagnosis of depression was based on claim data, and therefore some degree of misclassification is possible. Second, whether weight change was intended or naturally occurring was unknown. Third, restriction of the analysis to Koreans reduces generalizability. Fourth, as in any retrospective study, reverse causality might be overlooked. Therefore, we set a 2 year lag period and excluded previous depression diagnosis to avoid reverse causation as much as possible. Further study is needed to consider causality in prospective design. Fifth, variability independent of the mean (VIM) was used as the primary measure of BWV and as this is a mathematical estimation clinical relevance should be considered in interpretation.
This large cohort study confirmed that BWV was significantly associated with an increased risk of depression in patients with type 2 DM. The magnitude of depression risk was greater in those who were not obese at baseline. Thus, BWV may serve as an indicator for early detection of depression in type 2 DM patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of Samsung Medical Center in Seoul, Korea (IRB No: 2020-10-034). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
JHA participated in the study design, conception, data analysis, wrote the first manuscript drafting, and revised new drafts from co-authors. K-dH, J-HJ and JY participated in directed acquisition of the data and data analysis. MF, DM, S-MJ, DWS and KYH conceptualized the study and revised the manuscript. HJJ participated in whole study design and conception, and manuscript drafting. All authors read and approved the final manuscript.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HI21C0885), and by the Healthcare AI Convergence Research & Development Program (No. S1601-20-1041) through the National IT Industry Promotion Agency of Korea (NIPA) funded by the Ministry of Science and ICT.
DM has received research support from Nordic Naturals and Heckel Medizintechnik GmbH. He also works with the MGH Clinical Trials Network and Institute (CTNI), which has received research funding from multiple pharmaceutical companies and NIMH.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.765129/full#supplementary-material
1. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. (2003) 289:76–9. doi: 10.1001/jama.289.1.76
2. Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. (2001) 344:1343–50. doi: 10.1056/NEJM200105033441801
3. Bangalore S, Fayyad R, DeMicco DA, Colhoun HM, Waters DD. Body weight variability and cardiovascular outcomes in patients with type 2 diabetes mellitus. Circ Cardiovasc Qual Outcomes. (2018) 11:e004724. doi: 10.1161/circoutcomes.118.004724
4. Nam GE, Kim W, Han K, Lee CW, Kwon Y, Han B, et al. Body weight variability and the risk of cardiovascular outcomes and mortality in patients with type 2 diabetes: a nationwide cohort study. Diabetes Care. (2020) 43:2234–41. doi: 10.2337/dc19-2552
5. Yeboah P, Hsu FC, Bertoni AG, Yeboah J. Body mass index, change in weight, body weight variability and outcomes in type 2 diabetes mellitus (from the ACCORD trial). Am J Cardiol. (2019) 123:576–81. doi: 10.1016/j.amjcard.2018.11.016
6. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. (2001) 24:1069–78. doi: 10.2337/diacare.24.6.1069
7. Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. (2008) 31:2383–90. doi: 10.2337/dc08-0985
8. Champaneri S, Wand GS, Malhotra SS, Casagrande SS, Golden SH. Biological basis of depression in adults with diabetes. Curr Diab Rep. (2010) 10:396–405. doi: 10.1007/s11892-010-0148-9
9. Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. (2000) 160:3278–85. doi: 10.1001/archinte.160.21.3278
10. Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. (2010) 87:302–12. doi: 10.1016/j.diabres.2010.01.024
11. Sevilla-Gonzalez MDR, Quintana-Mendoza BM, Aguilar-Salinas CA. Interaction between depression, obesity, and type 2 diabetes: a complex picture. Arch Med Res. (2017) 48:582–91. doi: 10.1016/j.arcmed.2018.02.004
12. Guidi J, Lucente M, Sonino N, Fava GA. Allostatic load and its impact on health: a systematic review. Psychother Psychosom. (2021) 90:11–27. doi: 10.1159/000510696
13. de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. (2001) 63:619–30. doi: 10.1097/00006842-200107000-00015
14. Eckel RH, Kahn SE, Ferrannini E, Goldfine AB, Nathan DM, Schwartz MW, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? J Clin Endocrinol Metab. (2011) 96:1654–63. doi: 10.1210/jc.2011-0585
15. Stuart MJ, Baune BT. Depression and type 2 diabetes: inflammatory mechanisms of a psychoneuroendocrine co-morbidity. Neurosci Biobehav Rev. (2012) 36:658–76. doi: 10.1016/j.neubiorev.2011.10.001
16. Brumpton B, Langhammer A, Romundstad P, Chen Y, Mai XM. The associations of anxiety and depression symptoms with weight change and incident obesity: the HUNT study. Int J Obes. (2013) 37:1268–74. doi: 10.1038/ijo.2012.204
17. Foreyt JP, Brunner RL, Goodrick GK, Cutter G, Brownell KD, St Jeor ST. Psychological correlates of weight fluctuation. Int J Eat Disord. (1995) 17:263–75. doi: 10.1002/1098-108x(199504)17:3<263::aid-eat2260170307>3.0.co;2-n
18. Wyshak G. Weight change, obesity, mental health, and health perception: self-reports of college-educated women. Prim Care Companion J Clin Psychiatry. (2007) 9:48–54. doi: 10.4088/PCC.v09n0108
19. Seong SC, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol. (2017) 46:799–800. doi: 10.1093/ije/dyw253
20. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
21. Bangalore S, Fayyad R, Laskey R, DeMicco DA, Messerli FH, Waters DD. Body-weight fluctuations and outcomes in coronary disease. N Engl J Med. (2017) 376:1332–40. doi: 10.1056/NEJMoa1606148
22. Kim MK, Han K, Park YM, Kwon HS, Kang G, Yoon KH, et al. Associations of variability in blood pressure, glucose and cholesterol concentrations, and body mass index with mortality and cardiovascular outcomes in the general population. Circulation. (2018) 138:2627–37. doi: 10.1161/CIRCULATIONAHA.118.034978
23. Hyeon JH, Gwak JS, Hong SW, Kwon H, Oh SW, Lee CM. Relationship between bone mineral density and alcohol consumption in Korean men: the fourth Korea national health and nutrition examination survey (KNHANES), 2008-2009. Asia Pac J Clin Nutr. (2016) 25:308–15. doi: 10.6133/apjcn.2016.25.2.17
24. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
25. Lee H, Choi EK, Lee SH, Han KD, Rhee TM, Park CS, et al. Atrial fibrillation risk in metabolically healthy obesity: a nationwide population-based study. Int J Cardiol. (2017) 240:221–7. doi: 10.1016/j.ijcard.2017.03.103
26. Lee HJ, Choi EK, Han KD, Lee E, Moon I, Lee SR, et al. Bodyweight fluctuation is associated with increased risk of incident atrial fibrillation. Heart Rhythm. (2020) 17:365–71. doi: 10.1016/j.hrthm.2019.09.029
27. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National kidney foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. (2003) 139:137–47. doi: 10.7326/0003-4819-139-2-200307150-00013
28. Choi JB, Moon HW, Park YH, Bae WJ, Cho HJ, Hong SH, et al. The impact of diabetes on the risk of prostate cancer development according to body mass index: a 10-year nationwide cohort study. J Cancer. (2016) 7:2061–6. doi: 10.7150/jca.16110
29. van Baak MA, Mariman ECM. Mechanisms of weight regain after weight loss - the role of adipose tissue. Nat Rev Endocrinol. (2019) 15:274–87. doi: 10.1038/s41574-018-0148-4
30. Speed MS, Jefsen OH, Borglum AD, Speed D, Ostergaard SD. Investigating the association between body fat and depression via Mendelian randomization. Transl Psychiatry. (2019) 9:184. doi: 10.1038/s41398-019-0516-4
31. Miller AH. Beyond depression: the expanding role of inflammation in psychiatric disorders. World Psychiatry. (2020) 19:108–9. doi: 10.1002/wps.20723
32. Felger JC, Li Z, Haroon E, Woolwine BJ, Jung MY, Hu X, et al. Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry. (2016) 21:1358–65. doi: 10.1038/mp.2015.168
33. Yin L, Xu X, Chen G, Mehta ND, Haroon E, Miller AH, et al. Inflammation and decreased functional connectivity in a widely-distributed network in depression: centralized effects in the ventral medial prefrontal cortex. Brain Behav Immun. (2019) 80:657–66. doi: 10.1016/j.bbi.2019.05.011
34. Ge T, Fan J, Yang W, Cui R, Li B. Leptin in depression: a potential therapeutic target. Cell Death Dis. (2018) 9:1096. doi: 10.1038/s41419-018-1129-1
35. Taylor VH, Macqueen GM. The role of adipokines in understanding the associations between obesity and depression. J Obes. (2010) 2010:748048. doi: 10.1155/2010/748048
36. Nouwen A, Adriaanse MC, van Dam K, Iversen MM, Viechtbauer W, Peyrot M, et al. Longitudinal associations between depression and diabetes complications: a systematic review and meta-analysis. Diabet Med. (2019) 36:1562–72. doi: 10.1111/dme.14054
37. Miyawaki Y, Iwahashi H, Okauchi Y, Sudo Y, Fujiwara Y, Omote Y, et al. Differences in emotional distress among inpatients with type 1, obese type 2, and non-obese type 2 diabetes mellitus. Intern Med. (2015) 54:2561–7. doi: 10.2169/internalmedicine.54.3498
38. Tang J, Yu Y, Du Y, Ma Y, Zhu H, Liu Z. Association between actual weight status, perceived weight and depressive, anxious symptoms in Chinese adolescents: a cross-sectional study. BMC Public Health. (2010) 10:594. doi: 10.1186/1471-2458-10-594
39. Frederick DA, Sandhu G, Morse PJ. Swami V. Correlates of appearance and weight satisfaction in a US national sample: personality, attachment style, television viewing, self-esteem, and life satisfaction. Body Image. (2016) 17:191–203. doi: 10.1016/j.bodyim.2016.04.001
40. Kim H, Jeon HJ, Bae JN, Cho MJ, Cho SJ, Lee H, et al. Association of body mass index with suicide behaviors, perceived stress, and life dissatisfaction in the Korean general population. Psychiatry Investig. (2018) 15:272–8. doi: 10.30773/pi.2017.06.28
41. Lavie CJ, McAuley PA, Church TS, Milani RV, Blair SN. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol. (2014) 63:1345–54. doi: 10.1016/j.jacc.2014.01.022
42. Blazer DG, Moody-Ayers S, Craft-Morgan J, Burchett B. Depression in diabetes and obesity: racial/ethnic/gender issues in older adults. J Psychosom Res. (2002) 53:913–6. doi: 10.1016/S0022-3999(02)00314-8
43. de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res. (2010) 178:230–5. doi: 10.1016/j.psychres.2009.04.015
44. Snoek FJ, Bremmer MA, Hermanns N. Constructs of depression and distress in diabetes: time for an appraisal. Lancet Diabetes Endocrinol. (2015) 3:450–60. doi: 10.1016/S2213-8587(15)00135-7
Keywords: diabetes mellitus, depression, body weight variability, nationwide, body weight
Citation: An JH, Han K-d, Jung J-H, Yoo J, Fava M, Mischoulon D, Jung S-M, Shin DW, Hur KY and Jeon HJ (2021) High Bodyweight Variability Increases Depression Risk in Patients With Type 2 Diabetes Mellitus: A Nationwide Cohort Study in Korea. Front. Psychiatry 12:765129. doi: 10.3389/fpsyt.2021.765129
Received: 26 August 2021; Accepted: 15 November 2021;
Published: 10 December 2021.
Edited by:
Maj Vinberg, University Hospital of Copenhagen, DenmarkReviewed by:
Lars Vedel Kessing, University of Copenhagen, DenmarkCopyright © 2021 An, Han, Jung, Yoo, Fava, Mischoulon, Jung, Shin, Hur and Jeon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Jin Jeon, amVvbmhqQHNra3UuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.