- 1Department of Psychiatry and Psychotherapy, Carl Gustav Carus University Hospital, Technische Universität Dresden, Dresden, Germany
- 2Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA, United States
- 3Department of Addiction Medicine and Psychotherapy, kbo-Isar-Amper-Klinikum München-Ost, Haar, Germany
- 4Department of Psychiatry and Psychotherapy, Elblandklinikum Radebeul, Radebeul, Germany
Background: Methamphetamine use is a rapidly increasing cause of morbidity and mortality. Pregnant women and new parents who consume methamphetamine are at high risk since they seldom seek health services despite having multiple needs. We addressed this care gap by implementing an easily accessible program that pools resources from psychiatric, obstetric, and pediatric departments as well as community and government agencies.
Method: This real-life observational study evaluated an integrated care program in 27 expecting parents and 57 parents of minors. The outcome criteria were treatment retention, psychosocial functioning, and abstinence. We compared participant demographics according to outcome and applied ordinal logistic regression to predict treatment success.
Results: Patients received integrated care for almost 7 months on average. Nearly half achieved stable abstinence and functional recovery. Only one pregnant woman dropped out before a care plan could be implemented, and all women who gave birth during treatment completed it successfully. Three-fourths of patients had psychiatric comorbidities. Patients with depressive disorders were almost 5 times less likely to succeed with treatment. Attention-deficit hyperactivity disorder (ADHD) was diagnosed in nearly 30% of patients who dropped out of a care plan, which was about 4 times more often than in the successful outcome group.
Conclusion: Our program engaged pregnant women and parents in treatment and helped them recover from methamphetamine-related mental disorders. Management of comorbid ADHD and depression should be an integral part of care initiatives to counter the methamphetamine crisis that affects parents and children across the globe.
Introduction
Methamphetamine use continues to rise on a global scale (1), and methamphetamine-involved overdoses claim lives in staggering numbers (2). This humanitarian crisis is further fueled by maternal, fetal, and child deaths related to methamphetamine exposure (3–6). Moreover, ample evidence implicates methamphetamine in lasting health and psychosocial problems that severely affect parents and their children (3–5). Women who use methamphetamine are burdened by mental disorders in the perinatal period (5), and parents who use methamphetamine are overstrained by their caregiving roles in often adverse living conditions (7). Infants can experience serious damage, such as microcephaly, due to intrauterine methamphetamine exposure (5, 8). Child development is compromised as a result of these factors, as evidenced by lower IQ scores as well as internalizing (e.g., depression) and externalizing symptoms (e.g., aggression) (5, 7, 8). Despite the urgency for prevention and intervention, the uptake of antenatal, pediatric, and mental health services is low and too late in this population (5, 9, 10). Moreover, pregnant women who use methamphetamine leave substance use treatment against professional advice even more often than pregnant women who use other illicit drugs or alcohol (11).
The stark contrast between care needs and utilization highlights the importance of developing programs that are easily accessible and appealing to those impacted by methamphetamine. Pregnancy and parenthood can create a strong motivation for abstinence (7), but treatment may not be accessed due to fear of stigma and punitive measures (5, 12, 13). Thus, transparency and the commitment to keeping families together are paramount. To reach women of childbearing age, expecting parents, and parents of minors, different avenues within the healthcare system, social services, and the community should be used. Linking these avenues also promises to help families achieve lasting health benefits as continuity of care is instrumental in sustaining abstinence (14, 15).
We are aware of only one study that at least partly addressed this care gap. This study compared methamphetamine-specific psychoeducation with a program also covering relationship and parenting skills tailored to South-African pregnant women (12). Both group interventions reduced methamphetamine use and risky sexual behavior, and 92% of participants completed the 4-session comprising interventions (12). Only 14% had been in substance use treatment before, indicating that access to care can be improved substantially (12).
Acknowledging the unmet needs of families affected by substance use disorders, the concept “Mama denk an mich” (MAMADAM, “Mommy think of me”) was developed to deliver coordinated care across disciplines and settings. After having demonstrated the feasibility of MAMADAM (9, 16), we here present its potential to improve the mental health of pregnant women and parents who use methamphetamine. The findings on outcome prediction provide critical information for patient assessment and program optimization. With this report, we hope to encourage the implementation and study of similar initiatives to promote the well-being of parents and children impacted by methamphetamine.
Method
This is a real-life observational study of integrated care for expecting and new parents with methamphetamine-related psychiatric disorders, which was approved by the ethics committee at the Carl Gustav Carus Faculty of Medicine at the Technische Universität Dresden, Germany.
Care Model
MAMADAM is a family-centered concept that pools resources from psychiatric, obstetric, and pediatric departments as well as local drug counseling and child welfare services. The concept and its elements draw on the available evidence and best practice for the management of methamphetamine-related disorders (8). Services provided through MAMADAM are easily accessible and flexible, ranging from health information for women of childbearing age to comprehensive support for families across care sectors. Shared decision-making and the participation of patients in multidisciplinary meetings ensure that treatment is matched to their preferences and needs. Other engagement strategies are calling patients who missed appointments and offering provider continuity whenever feasible. The following outlines the parts that are directed to the mental health of expecting and new parents. The coordination and specifics of MAMADAM, including information on obstetric and pediatric services, are described elsewhere (9, 16).
All expecting and new parents who use methamphetamine and present to our psychiatric department are considered for enrollment in MAMADAM. Access is facilitated by referrals from healthcare providers and by psychiatric consultations at the obstetric and pediatric departments. Motivational interviewing is used to develop personalized care plans after assessing mental illness and methamphetamine-related medical sequelae. Patients are seen by psychiatrists and psychotherapists on an outpatient basis from several times a week to once a month as needed. Inpatient and day treatments are provided whenever necessary.
An individual session introduces a methamphetamine-specific relapse prevention program that combines aspects of psychoeducation, motivational interviewing, and cognitive behavior therapy (17, 18). Psychotherapists deliver this program in 15 sessions of 50 min to a maximum of 5 patients. Individual psychotherapy and other group therapies are also available (e.g., exercise classes, social skills training, psychoeducation for major depression).
Social workers and occupational therapists help patients enhance their functioning and well-being in areas such as work, housing, and childcare. They partner with local and government agencies to furnish services ranging from community connections to intensive home support. Home care includes random drug screening, but most patients are called into the clinic once in 6 days on average. Urine is collected under direct observation followed by temperature measurement to minimize manipulation.
Analytic Strategy
We studied a naturalistic sample of patients with methamphetamine-related disorders who received psychiatric care within MAMADAM since its start in 2016 and left or completed treatment before September 13, 2019. Outcome was classified as early dropout (before implementation of a care plan), partial completion of the program (late dropout), and successful completion. Successful completion was defined as a mutually agreed program discharge, which required continuous abstinence, stable housing, financial security, psychosocial functioning, and a support system. Psychosocial functioning required patients to perform daily activities in ways that were gratifying to them while meeting the demands of their dependents (e.g., safe environment, loving relationship) and the community (e.g., engagement in employment). Support usually involved primary care physicians, private psychiatrists, drug counseling centers, and child welfare services.
We used SPSS 27 (IBM, Armonk, NY, USA) and a significance level of 0.05 (two-tailed) for all analyses. Statistics were performed on complete data from all patients unless stated otherwise. We compared participant demographics and the duration of psychiatric care within MAMADAM according to outcome, using Pearson's chi-square-test, Fisher's exact-test, and Bonferroni-adjusted pairwise comparisons for categorical variables. Histograms, normal quantile-quantile plots, and normality tests (Kolmogorov-Smirnov, Shapiro-Wilk) determined the tests for continuous variables (one-way independent ANOVA, Kruskal-Wallis, Mann-Whitney). To identify predictors of outcome, we built a base model with all participant demographics that had complete data and met the assumptions of ordinal logistic regression. We then progressively removed non-significant variables to produce a parsimonious model. Variables that differed considerably between outcome groups and significant predictors were tested for associations, reporting the phi or Spearman's coefficient. These associations were not corrected for multiple comparisons.
Results
We studied 84 patients with methamphetamine-related mental disorders (1 × F15.0, 8 × F15.1, 74 × F15.2, 1 × F19.2; diagnosed according to the International Classification of Diseases, 10th revision). This sample comprised 27 expecting parents and 57 parents of minors (mean age of child ± SD, min-max: 19.02 ± 30.59, 1–144 months; newborns counted as 1 month). Sixteen patients (19.0%) dropped out before receiving a care plan, 27 (32.1%) completed part of the program, and 41 (48.8%) transitioned successfully to community care. Average program participation was over 6 months (mean ± SD, min-max: 202.49 ± 167.42, 0–793 days) and not statistically different between patients who partially and those who successfully completed treatment (n = 68, U = 655.00, z = 1.27, p = 0.203).
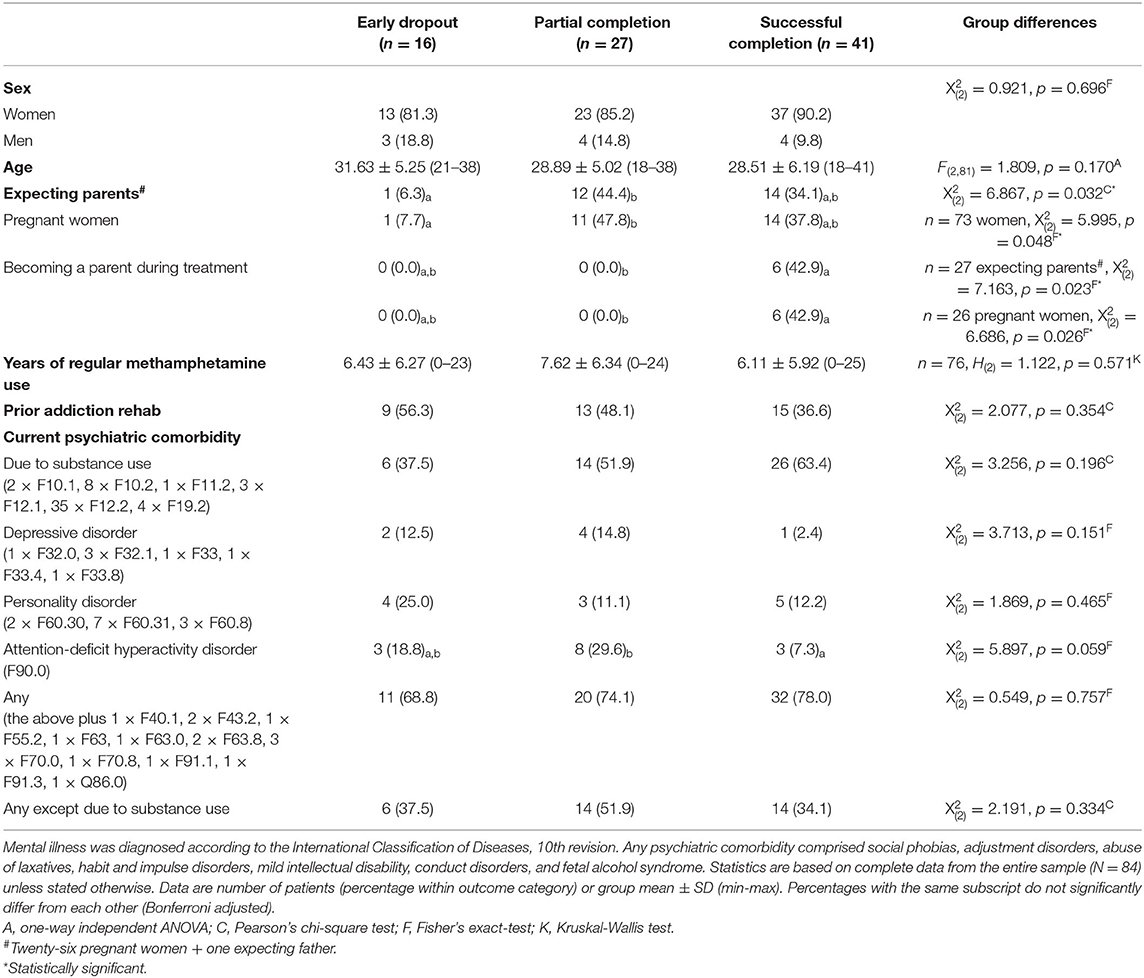
Table 1 displays demographics according to outcome, showing no statistical differences in sex, age, years of methamphetamine use, and prior addiction rehab. The proportion of pregnant women was significantly lower in the early than in the late dropout group, and all women who gave birth during treatment completed it successfully. Three-fourths of patients had psychiatric comorbidities. Groups were comparably affected except for attention-deficit hyperactivity disorder (ADHD). Although there was only a trend to an overall significant difference between groups, ADHD was significantly less common in patients successfully than in those partially completing the program.
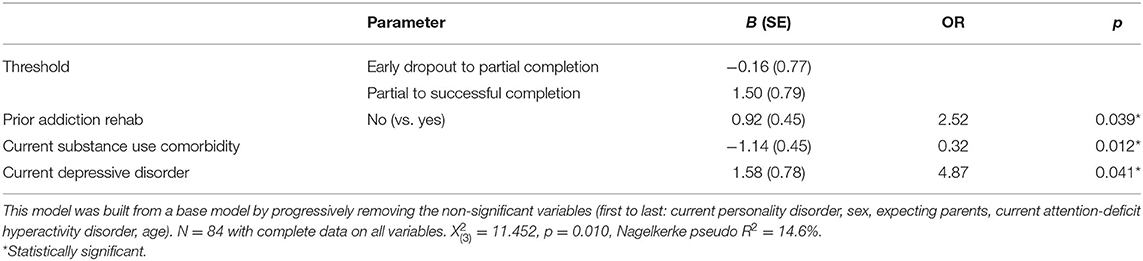
When accounting for the order of outcomes (worst to best: early dropout, partial completion, successful completion), depression, substance use comorbidity, and prior addiction rehab emerged as significant predictors. Patients with substance use comorbidities were more likely to have a better outcome, whereas the opposite applied to patients with depressive disorders and patients with prior addiction rehab. Table 2 lists the unique (net) contribution of each significant predictor to variations in outcomes (controlled for the other significant predictors).
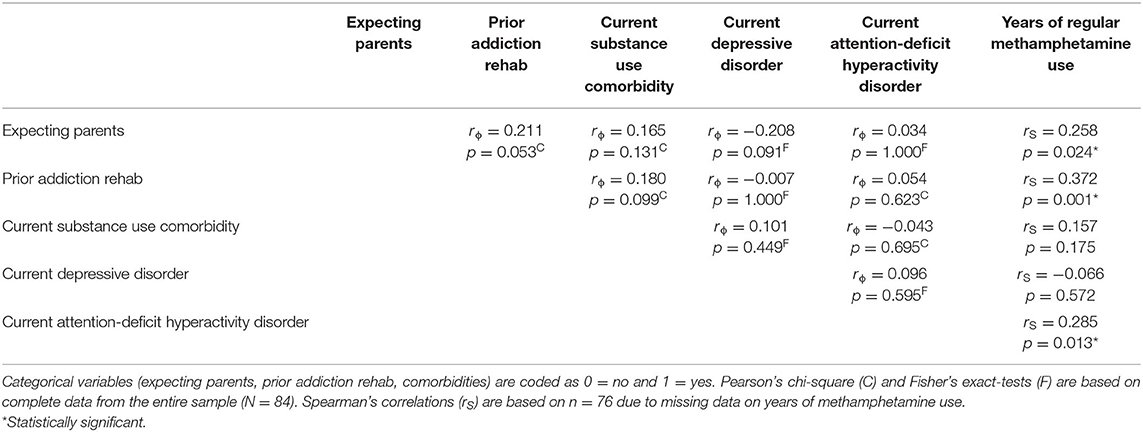
None of the outcome predictors or variables with considerable group differences were significantly related to one another (see Table 3). Yet, there was one trend-level significant association with 59.3% of expecting parents compared with 36.8% of parents having prior addiction rehab. Of note, expecting parents, patients with prior addiction rehab, and patients with ADHD featured a significantly longer use of methamphetamine. Regular methamphetamine use was also numerically longer for patients who dropped out compared with those who completed MAMADAM successfully.
Discussion
This study evaluated the real-world adherence to integrated care by pregnant women and parents with methamphetamine-related mental disorders. Despite being challenged by their roles and psychiatric comorbidities, nearly half of our patients completed treatment successfully, and only one pregnant woman dropped out before receiving a care plan. These data support the notion that pregnancy and parenthood can be motivators for abstinence (7, 8, 19). We are not aware of any study that evaluated a comparable concept for this population, but methamphetamine use is generally associated with high dropout rates (8, 19). Less than one-fourth of patients with methamphetamine as their primary drug completed 180 days of outpatient drug treatment, a duration previously identified as necessary for treatment success (20). Moreover, pregnant women using methamphetamine left substance use treatment against professional advice even more often than those using other illicit drugs or alcohol (11).
Three-fourths of our patients had at least one other mental disorder, which reflects the high psychiatric morbidity reported in association with methamphetamine use (8, 19). Patients with depressive disorders were almost 5 times more likely to have less treatment success than patients without such a diagnosis. This aligns with an outpatient treatment study for methamphetamine dependence in which higher baseline depression predicted methamphetamine use before discharge and poorer treatment attendance (21). Although not predicted by baseline depression scores, methamphetamine use 3 years post-treatment was associated with major depression at follow-up (21). Together, these findings emphasize the need for routine assessment and treatment of depression. Exercise and psychological interventions can reduce depressive symptoms, but methamphetamine-induced cognitive deficits complicate the latter (8, 19). Medications including antidepressants have largely failed and their potential for drug interaction effects has been highlighted (8, 19). Yet, recent research suggests that glutamatergic modulators with antidepressant and pro-cognitive properties may prove effective in treating methamphetamine use disorder and comorbid depression (22).
ADHD was diagnosed in almost one-third of patients who dropped out of an established care plan. This proportion was about 4 times as high as in the successful outcome group. Moreover, ADHD was associated with more years of regular methamphetamine use, which was also numerically longer for patients who dropped out. Routine assessment for ADHD seems therefore imperative, not least because some patients report using methamphetamine to treat ADHD symptoms (8). The risk of misuse and drug interactions warrants close monitoring of pharmacotherapy, with long-acting formulations recommended if stimulant medication is prescribed (19).
A diagnosis of substance use comorbidity predicted a better outcome, which indicates that the benefits of MAMADAM extend to other drugs. Experiencing a substance use comorbidity might increase readiness for change and treatment. Patients with prior addiction rehab were, in comparison, more likely to have a worse outcome. Similarly, previous drug treatment predicted treatment attrition in pregnant women using methamphetamine weekly or more (11). Prior treatment could indicate greater disease severity or longer disease duration, as patients with prior addiction rehab featured more years of regular methamphetamine use. Of note, more years of regular methamphetamine use predicted poor outcome in a study of the methamphetamine-specific group psychotherapy that we provide in MAMADAM (18). The data collectively highlight that patients with previous drug treatment require close monitoring and greater support. Recognizing the value of their treatment experiences may be a way to better meet their needs and expectations, which should improve retention in care and health outcomes.
Strengths and Limitations
To our knowledge, this is the first work evaluating the adherence to integrated care by pregnant women and parents with methamphetamine-related mental disorders. We did not include a control condition but the exploratory study of a naturalistic sample in the real world can provide outcome predictors of direct importance for patient care. Of note, we report significant predictors from a parsimonious regression model that did not control for non-significant variables and only considered variables with complete data. ADHD was not among the significant predictors in our regression model yet more prevalent in patients who dropped out, with the late dropout group statistically differing from the successful outcome group. We believe that ADHD and other comorbidities, such as depressive and personality disorders, are underreported for patients dropping out of MAMADAM early since these diagnoses require thorough assessments in drug-free intervals. Lastly, we did not collect follow-up data, but treatment success required stable abstinence and continuing care, which are critical factors for long-term recovery.
Conclusion
Integrated care is a promising strategy for pregnant women and parents with methamphetamine-related mental disorders. Pregnancy and parenthood provide opportunities to motivate change and engage a population that hardly accesses treatment despite the high psychiatric morbidity. Comorbid ADHD and depression warrant close monitoring as they jeopardize treatment engagement and success. Given the little information on the management of these conditions in the context of methamphetamine use, research is imperative to provide evidence-based interventions. Moreover, integrated care concepts should be disseminated to counter the increasing methamphetamine crisis that affects parents and children across the globe.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee at the Carl Gustav Carus Faculty of Medicine at the Technische Universität Dresden, Germany. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
UZ, MP, MS, and SH contributed to the development of the care concept. MS, SH, TK, UZ, and MP were members of the care team. MP, UZ, CS, and MK designed the study. MP and JP obtained funding. MK, CS, MS, MP, and TK collected the data. JP analyzed and interpreted the data and wrote the manuscript. All authors contributed to manuscript revision, as well as read and approved the final version.
Funding
This work was supported by the German Research Foundation [TRR 265 (23)]. The article processing charge was paid from the Publication Fund of the Technische Universität Dresden. The funders were not involved in the conceptualization of the study, the collection, analysis, interpretation of data, the preparation of the manuscript, or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the staff at the psychiatric outpatient department for assistance with data collection and Matthew Belanger for diligent proofreading.
Abbreviations
ADHD, attention-deficit hyperactivity disorder; MAMADAM, “Mama denk an mich”, “Mommy think of me”.
References
1. UNODC. World Drug Report 2020, Booklet 2 Drug Use and Health Consequences. United Nations publication, Vienna (2020).
2. Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential - United States, 2003-2017. Morb Mortal Wkly Rep. (2019) 68:388–95. doi: 10.15585/mmwr.mm6817a3
3. Admon LK, Bart G, Kozhimannil KB, Richardson CR, Dalton VK, Winkelman TNA. Amphetamine- and opioid-affected births: incidence, outcomes, and costs, United States, 2004-2015. Am J Public Health. (2019) 109:148–54. doi: 10.2105/AJPH.2018.304771
4. Dinger J, Hinner P, Reichert J, Rüdiger M. Methamphetamine consumption during pregnancy - effects on child health. Pharmacopsychiatry. (2017) 50:107–13. doi: 10.1055/s-0042-122711
5. Perez FA, Blythe S, Wouldes T, McNamara K, Black KI, Oei JL. Prenatal Methamphetamine- impact on the mother and child - a review. Addiction. (2021). doi: 10.1111/add.15509. [Epub ahead of print].
6. Tse R, Kesha K, Morrow P, Glenn C, Stables S. Commentary on: Kenneally M, Byard RW. Increasing methamphetamine detection in cases of early childhood fatalities. J Forensic Sci. (2020) 65:1384. doi: 10.1111/1556-4029.14459
7. Dyba J, Moesgen D, Klein M, Leyendecker B. Methamphetamine use in German families: parental substance use, parent-child interaction and risks for children involved. Subst Use Misuse. (2019) 54:583–91. doi: 10.1080/10826084.2018.1528459
8. Braunwarth W-D, Christ M, Dirks H, Dyba J, Härtel-Petri R, Harfst T, et al. S3 Practice Guideline Methamphetamine-Related Disorders. 1st ed. Berlin: Agency for Quality in Medicine (2016).
9. Dinger J, Näther N, Wimberger P, Zimmermann US, Schmitt J, Reichert J, et al. Increasing consumption of crystal meth in saxony and its risks for mother and child - experiences at a level I perinatal center from a pediatric viewpoint. Z Geburtshilfe Neonatol. (2017) 221:73–80. doi: 10.1055/s-0043-102953
10. Stevens S, Rogers J, Dansereau L, DellaGrotta S, Lester BM, Wouldes TA, et al. Prospective study of service use in the year after birth by women at high risk for antenatal substance use and mental health disorders. Int J Ment Health Addict. (2019) 19:1005–1018. doi: 10.1007/s11469-019-00207-w
11. Lindsay B, Albrecht J, Terplan M. Against professional advice: treatment attrition among pregnant methamphetamine users. Subst Abuse Rehabil. (2011) 2:189–95. doi: 10.2147/SAR.S25083
12. Jones HE, Myers B, O'Grady KE, Gebhardt S, Theron GB, Wechsberg WM. Initial feasibility and acceptability of a comprehensive intervention for methamphetamine-using pregnant women in South Africa. Psychiatry J. (2014) 2014:929767. doi: 10.1155/2014/929767
13. Lewis D. We were wrong about “crack babies”: are we repeating our mistake with “meth babies”? MedGenMed. (2005) 7:30.
14. Chi FW, Parthasarathy S, Mertens JR, Weisner CM. Continuing care and long-term substance use outcomes in managed care: early evidence for a primary care-based model. Psychiatr Serv. (2011) 62:1194–200. doi: 10.1176/ps.62.10.pss6210_1194
15. Manning V, Garfield JB, Best D, Berends L, Room R, Mugavin J, et al. Substance use outcomes following treatment: findings from the Australian Patient Pathways Study. Aust N Z J Psychiatry. (2017) 51:177–89. doi: 10.1177/0004867415625815
16. Groß C, Hahn S, Spreer M, Behrendt S, Dinger J, Reichert J, et al. “Mama denk' an mich” (MAMADAM) - ein multimodales Therapieprogramm für suchtkranke Schwangere, Mütter und Väter im Rahmen der psychiatrischen Institutsambulanz. SUCHT. (2018) 64:97–108. doi: 10.1024/0939-5911/a000533
17. Groß C, Schützwohl M, Mayer-Pelinski R, Hasler H, Kirchner T, Scheck A, et al. “CrystalClean” - a German-language manual for qualified detoxification and motivation treatment in cases of “crystal meth” dependency - feasibility and acceptance. Psychiatr Prax. (2020) 47:22–8. doi: 10.1055/a-1003-5148
18. Petzold J, Weber B, Bassett TR, Bauer M, Bernhardt N, Gross C, et al. Effectiveness of the first German-language group psychotherapy manual to accompany short-term treatment in methamphetamine dependence. Front Psychiatry. (2020) 11:130. doi: 10.3389/fpsyt.2020.00130
19. Grigg J, Manning V, Arunogiri S, Volpe I, Frei M, Phan V, et al. Methamphetamine Treatment Guidelines: Practice Guidelines for Health Professionals. 2nd ed. Richmond, VA, Victoria: Turning Point. (2018).
20. Maglione M, Chao B, Anglin MD. Correlates of outpatient drug treatment drop-out among methamphetamine users. J Psychoactive Drugs. (2000) 32:221–8. doi: 10.1080/02791072.2000.10400232
21. Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, Rawson R. Depression among methamphetamine users: association with outcomes from the methamphetamine treatment project at 3-year follow-up. J Nerv Ment Dis. (2009) 197:225–31. doi: 10.1097/NMD.0b013e31819db6fe
22. Petzold J, Szumlinski KK, London ED. Targeting mGlu(5) for methamphetamine use disorder. Pharmacol Ther. (2021) 224:107831. doi: 10.1016/j.pharmthera.2021.107831
Keywords: methamphetamine use disorder, drug dependence, addiction, ADHD, depression, pregnancy, multimodal therapy, outcome prediction
Citation: Petzold J, Spreer M, Krüger M, Sauer C, Kirchner T, Hahn S, Zimmermann US and Pilhatsch M (2021) Integrated Care for Pregnant Women and Parents With Methamphetamine-Related Mental Disorders. Front. Psychiatry 12:762041. doi: 10.3389/fpsyt.2021.762041
Received: 20 August 2021; Accepted: 27 September 2021;
Published: 25 October 2021.
Edited by:
Jean Lillian Paul, Medizinische Universität Innsbruck, AustriaReviewed by:
Michael Klein, Catholic University of Applied Sciences of North Rhine – Westphalia, GermanyIngrid Zechmeister-Koss, Austrian Institute for Health Technology Assessment GmbH, Austria
Rebecca Kate Allchin, Eastern Health, Australia
Copyright © 2021 Petzold, Spreer, Krüger, Sauer, Kirchner, Hahn, Zimmermann and Pilhatsch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johannes Petzold, am9oYW5uZXMucGV0em9sZEB1bmlrbGluaWt1bS1kcmVzZGVuLmRl
†ORCID: Johannes Petzold orcid.org/0000-0003-4163-9014
Maximilian Pilhatsch orcid.org/0000-0003-4323-3309
 Johannes Petzold
Johannes Petzold Maik Spreer
Maik Spreer Maria Krüger1
Maria Krüger1 Cathrin Sauer
Cathrin Sauer Ulrich S. Zimmermann
Ulrich S. Zimmermann Maximilian Pilhatsch
Maximilian Pilhatsch