
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 11 November 2021
Sec. Child and Adolescent Psychiatry
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.759449
 Anyi Zhang1†
Anyi Zhang1† Le Shi1†
Le Shi1† Wei Yan1†
Wei Yan1† Han Xiao2†
Han Xiao2† Yanping Bao3
Yanping Bao3 Zhe Wang1
Zhe Wang1 Jiahui Deng1
Jiahui Deng1 Arun Ravindran4
Arun Ravindran4 Kai Yuan1
Kai Yuan1 Hong Mei2
Hong Mei2 Jie Shi3
Jie Shi3 Zhisheng Liu5*
Zhisheng Liu5* Jiajia Liu6*
Jiajia Liu6* Lin Lu1,7*
Lin Lu1,7*Introduction: To date, the mental health consequences of children hospitalized with COVID-19 remain unclear. We aimed to assess mental health status in children in the context of COVID-19, with a focus on discharged children.
Methods: We recruited discharged children who recovered from COVID-19 and healthy controls between July and September 2020 in Wuhan Children's Hospital. Post-traumatic stress disorder (PTSD), anxiety, depression, and sleep problems were assessed in these children using questionnaires. Univariable and multivariable logistic and linear regressions were conducted to identify risk factors.
Results: Totally, there were 152 children (61 discharged children and 91 healthy controls) aged 7–18 years old in our study. An increasing trend in the prevalence of PTSD, anxiety, and depression was observed in the discharged children compared with healthy controls (PTSD: 8.20 vs. 2.20%, anxiety: 22.95 vs. 13.19%; depression: 47.54 vs. 32.97%). Discharged children tended to report more depressive symptoms (β = 0.39) and less sleep problems (β = −0.37). Discharged children who lived in nuclear families and had longer hospital stays were more likely to report depression [odds ratio (OR) = 3.68 and 1.14, respectively]. Anxiety symptoms and the severity of sleep problems of discharged children were positively associated with caregivers' depression and PTSD symptoms (OR = 21.88 and 31.09, respectively).
Conclusion: In conclusion, PTSD, anxiety, and depression symptoms were common among recovered children 4 months after COVID-19 hospitalization. Children from nuclear family and those had longer hospital stays need special attention. In addition, parental mental health had a significant impact on their children's mental resilience and recovery.
By the end of May 2021, the coronavirus disease 2019 (COVID-19) pandemic afflicted more than 170 million people worldwide (1). The outbreak of COVID-19 has caused various mental health problems in the public and vulnerable populations, including healthcare workers, elderly, pregnant women, and children (2–8). Although children have a lower infection rate and relatively mild clinical symptoms, those with COVID-19 infection are considered more susceptible to mental health problems compared with unaffected children (9). Separation from caregivers and more mental health problems among caregivers that are caused by COVID-19 or close contact with confirmed cases can push affected children into a state of crisis and might increase their risk of psychiatric disorders (10). Additional stressors among children with COVID-19 may include hospital quarantine for prolonged periods of time, fear of the disease, being infected again, daily treatment, and the immunological response to infection (10).
Among the broader population, social distancing measures and school closures can also impact children's mental health. In a previous review, anxiety and depression were reported as the most prevalent psychological symptoms in children and adolescents during the COVID-19 pandemic (11). For example, a study in Wuhan, Hubei province, China, reported that depressive and anxiety symptoms affected 22.6 and 18.9% of primary students, respectively (12). In another study conducted in high school students during COVID-19 pandemic, 85.5% presented symptoms of post-traumatic stress disorder (PTSD), and post-pandemic PTSD in general population was 22.6% (13, 14). However, there were also positive impacts of the pandemic on children, as the school closure might protect children from school bullying or drug abuse (15). To date, most studies focused on the general population or healthy children, and evidence on children recovered from COVID-19 was scarce. Few studies evaluated the prevalence of psychological symptoms including anxiety, depression, and PTSD in children who were afflicted by COVID-19 and discharged from the hospital. Such studies are needed to determine appropriate support and resources. The present study (1) evaluated mental health status in children who had COVID-19 and were discharged from the hospital compared with healthy children who were quarantined at home and (2) explored risk factors that were associated with mental health problems in discharged children.
This study had a case control design. Participants were recruited from a cohort of discharged pediatric patients who were hospitalized and treated for COVID-19 in Wuhan Children's Hospital between January and March 2020, and family member being infected was not a part of selection criteria. The diagnosis of COVID-19 was based on guidelines from the National Health Commission of the People's Republic of China and Society of Pediatrics of China (16). The physical and mental health status of these children were assessed from July to September 2020 after the lockdown for COVID-19 (i.e., 4 months after hospital discharge). Given the different measurements that are applied for children of different ages, only data on ≥7-year-old children were analyzed in the present study. We divided the participants into two age groups: school-aged children (7–12 years old) who were mostly in primary school and adolescents (13–18 years old) who were mostly in junior and senior high school. During the COVID-19 pandemic in 2020 in Wuhan, there were 363 children with COVID-19 infection hospitalized and treated in the Wuhan Children's Hospital. We recruited those participants through telephone, and 243 children excluded as they were not approached, 55 children were excluded as they were younger than 7 years old, 4 were excluded because of the incomplete questionnaire. So, there were 61 children left in the patient group. All participants in the COVID-19 patient group were diagnosed with asymptomatic or mild COVID-19. None of the patients had hypoxemia, were admitted to an intensive care unit, or used mechanical ventilation. In our study, children with asymptomatic or mild COVID-19 were accompanied by an uninfected family member. Children in the healthy control group were recruited from a birth cohort in Wuhan Children's Hospital, and their physical and mental health assessment was conducted during the same period as the COVID-19 patient group. Because of China's lockdown strategy, children in the healthy control group were quarantined at home during the COVID-19 pandemic.
The present study was reviewed and approved by the Ethics Committee of Wuhan Children's Hospital and complied with the Declaration of Helsinki. All of the children and their caregivers provided written informed consent.
The children's socio-demographic characteristics were collected using the parent-reported questionnaire, including gender, age, ethnic, family structure, number of siblings, parents' age, household income, previous mental and physical health status, having family infected COVID-19 or not and family disease history.
PTSD symptoms were assessed using the Child PTSD Symptom Scale (CPSS), which comprised 17 questions that assessed three key symptoms of PTSD: re-experiencing, avoidance, and arousal. Each item was rated on a 4-point Likert-type scale (17). Individuals who met the following criteria were identified as having PTSD: (1) at least one severity score > 2 among the five re-experiencing symptoms, (2) at least three severity scores > 2 among the seven avoidance symptoms, and (3) at least two severity scores > 2 among the five arousal symptoms.
The Screen for Child Anxiety Related Emotional Disorders (SCARED) was used to evaluate anxiety symptoms in children, which is a self-report questionnaire that consists of 41 items (18). All items were answered on a 3-point Likert-type scale. A total score ≥ 23 indicated significant symptoms of anxiety.
We used the 10-item Children's Depression Inventory-Short version (CDI-S) to assess depression status. A total score ≥ 3 indicated the likely presence of depression (19).
Sleep problems were assessed using the 26-item Sleep Disturbance Scale for Children (SDSC). Scores > 39 indicated sleep problems (20).
This was assessed using 8 questions extracted from the 10-item Post-traumatic Growth Inventory–Short Form (PTGI-SF). Considering the different cultural backgrounds between China and Western countries, most Chinese people reported no religious beliefs (21), and this might lead to a lower score in the spiritual change subscale, so we deleted two items about spiritual change. In the present study, the Cronbach's α of the 8-item PTGI-SF was 0.91, which demonstrated a high internal consistency. Answers to the remaining 8-items were scored on a 4-point scale, ranging from 0 (not at all) to 3 (very much). A higher score indicated better PTG and greater positive change.
We used the revised Brief Trauma Questionnaire (BTQ) to assess the retrospective history of exposure to traumatic events in children (22). The BTQ contains 12 types of traumatic events that may have occurred to respondents or family members. Answers were dichotomous (yes or no). The total score ranged from 0 to 12. Higher scores indicated more exposure to traumatic events before the COVID-19 pandemic.
Resilience in children and adolescents was measured by the 10-item Connor–Davidson Resilience Scale (CD-RISC-10), extracted from the original 25-item CD-RISC (23). Higher scores indicated higher resilience capacity.
Perceived social support was assessed using the 12-item Multidimensional Scale of Perceived Social Support (MSPSS), which has been well-validated in many countries and widely used in children and adolescents (24, 25). Higher scores indicated a higher level of perceived social support.
We also evaluated the mental health status of caregivers, the details of which are presented in the Supplementary Material.
Descriptive statistics were used to present the demographic characteristics of the COVID-19 patients and healthy controls. Demographic characteristics were compared using the χ2 test for categorical variables and Kruskal-Wallis test for continuous variables. The prevalence of PTSD, anxiety, depression, and sleep problems in children, stratified by demographic factors, are presented, and compared using the χ2 test. The total scores of questionnaires that assessed psychological conditions in children and caregivers were non-normally distributed. Therefore, these scores are presented as medians and interquartile ranges (IQRs) and were compared using the Kruskal-Wallis test. We also explored the likely contributors to psychiatric symptoms in children using univariate and multivariate regression models. The potential factors were initially identified using univariate linear and logistic regression models, the details of which are presented in the Supplementary Material. Factors were then identified using multivariate logistic and linear regression analyses with forward stepwise variable selection based on the Wald statistic (variables with p < 0.1) for entry into the final adjusted models. Odds ratios (ORs) and 95% confidence intervals (CIs) were determined for the logistic regression analyses, and the beta-coefficient (β) and 95% CI are presented for the linear regression analyses. Because of the non-normal distribution of total scores of the questionnaires, square root transformations were conducted for the linear regression models. The estimation of collinearity among parameters was calculated by the variance inflation factor (VIF) for the linear regression models. Variables with VIF <5 were entered into the final model (26).
The same analysis strategy was used for children who had recovered from COVID-19. All analyses were performed using Statistical Package for the Social Sciences (SPSS) 23.0 software. The level of significance was set at p < 0.05 (two-tailed).
A total of 152 children and adolescents (61 discharged children and 91 healthy controls), 7–18 years old, were recruited in the present study. Among the discharged children, 13 (21.31%) were girls, which was lower than in healthy controls (45.06%; p = 0.010). There were 17 (27.87%) adolescents in the COVID-19 group, and 7 (7.69%) in the control group (p < 0.001). Among the discharged children, 75.41% (n = 46) reported having family with confirmed COVID-19. Among the healthy controls, 5.49% (n = 5) reported having family with confirmed COVID-19 (p < 0.001). The household income was significantly lower in discharged children compared with healthy controls (p < 0.01). Other demographic characteristics are shown in Table 1.
An increase trend in the prevalence of PTSD, anxiety, and depression was found in discharged children who recovered from COVID-19 compared with healthy controls (PTSD: 8.20 vs. 2.20%, p = 0.084; anxiety: 22.95 vs. 13.19%, p = 0.12; depression: 47.54 vs. 32.97%, p = 0.082). Among the total subjects, the prevalence of PTSD was higher in children whose caregivers reported PTSD (20.00 vs. 3.79%, p = 0.022) and poor sleep quality (10.53 vs. 1.15%, p = 0.016). In addition, the prevalence of anxiety in children was significantly higher in those whose caregivers reported depression (34.38 vs. 13.16%, p = 0.006). Depression severity was significantly higher in discharged children compared with healthy controls (median, IQR: 2.00, 6.00, and 2.00, 2.00, respectively; p = 0.023). In the whole participants, boys (median, IQR: 28.50, 11.00, and 31.00, 10.00, respectively; p = 0.044), the infected children (median, IQR: 27.00, 11.00, and 31.00, 10.00, respectively; p = 0.020), and nuclear family (median, IQR: 28.00, 9.00, and 31.00, 12.00, respectively; p = 0.045) were associated with fewer severe sleep problems. Children's sleep problems significantly increased in those whose caregivers reported PTSD (60.00 vs. 14.39%, p <0.001) and depression (40.63 vs. 11.40%, p <0.001). Additional data are presented in Table 2.
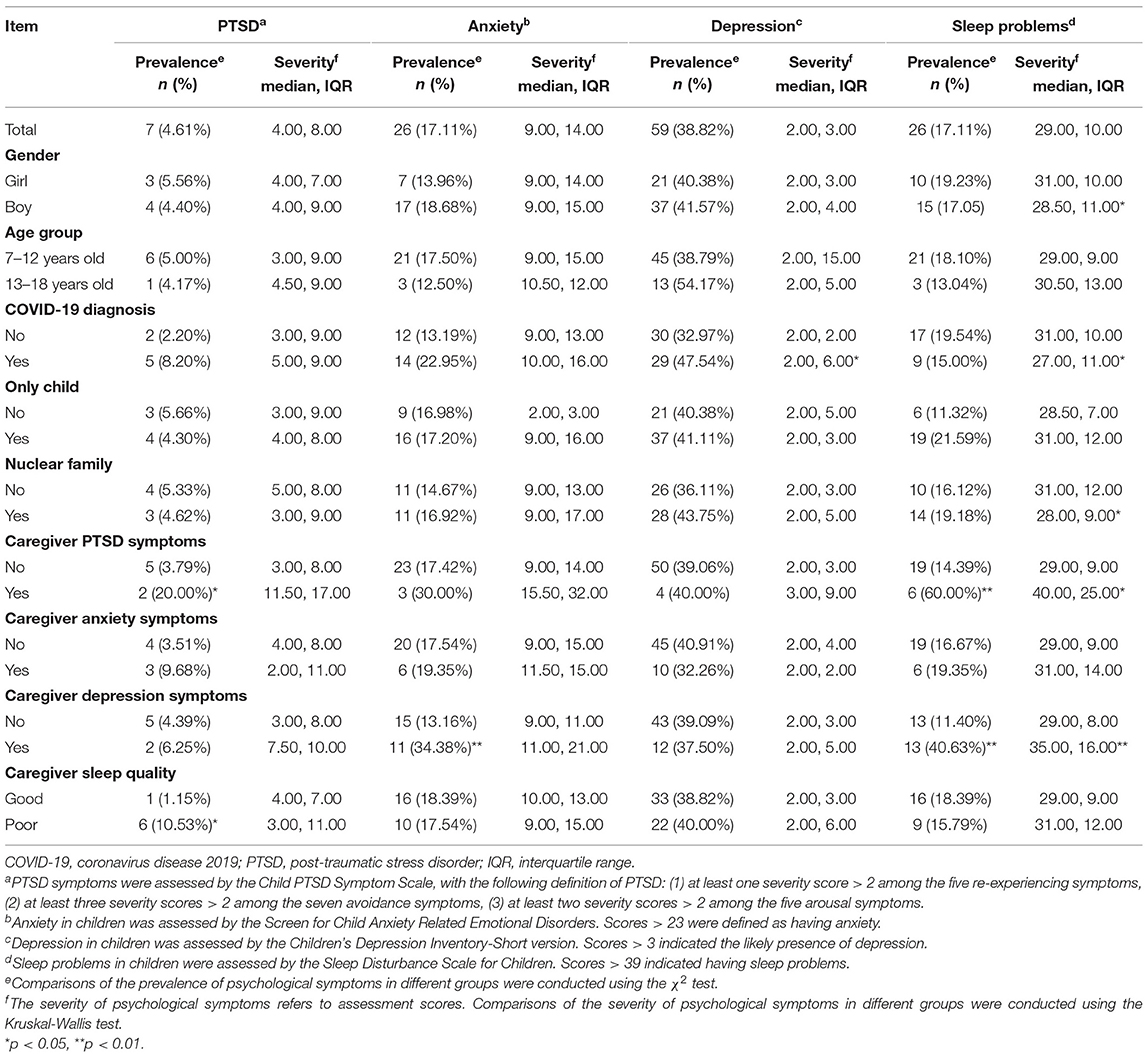
Table 2. Prevalence and severity of psychiatric symptoms in children stratified by epidemiological characteristics (n = 152).
As shown in Figure 1, children who experienced more stressful events before the pandemic (β = 0.30, p = 0.004 for PTSD, β = 0.35, p = 0.002 for anxiety), children who had COVID-19 (β = 0.39, p = 0.019) and children with fewer siblings (β = 0.37, p = 0.035) reported worse mental health status. While, male gender (β = −0.37, p = 0.043), resilience (β = −0.03, p = 0.009 for PTSD, β = −0.02, p = 0.003 for depression) and social support (β = −0.02, p = 0.043) would protect children from developing psychological symptoms. In addition, caregiver's mental health status was closely related to children's mental health. When caregivers showed depression symptoms (β = 0.07, p = 0.048 for children's PTSD, β = 0.09, p = 0.025 for children's anxiety symptoms) or post-traumatic stress symptoms (β = 0.04, p = 0.001), children might report an increased risk for psychological symptoms. PTG was higher in children from primary school (β = −0.37, p = 0.043) and children who perceived more resilience (β = 0.08, p < 0.001). Interestingly, children who had COVID-19 (β = −0.37, p = 0.049) tended to have fewer sleep problems.
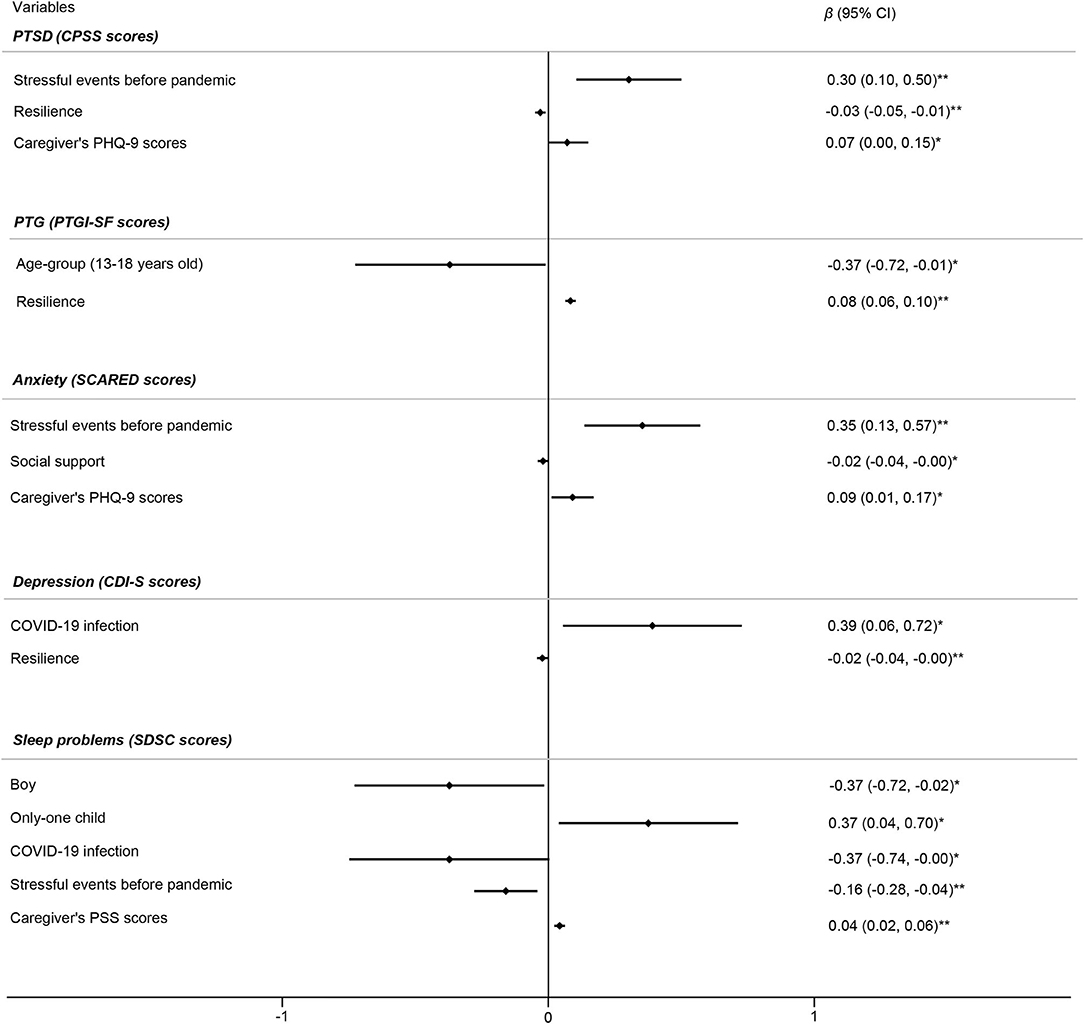
Figure 1. Factors associated with mental health symptoms in children (n = 152). Initial variables in the multivariate linear regression model for PTSD included gender, age group, COVID-19 diagnosis, stressful events before the pandemic, resilience, social support, and caregivers' PSS and PHQ-9 scores. Initial variables in the multivariate linear regression model for PTG included gender, age group, COVID-19 diagnosis, stressful events before the pandemic, resilience, social support, and caregivers' PSS and PHQ-9 scores. Initial variables in the multivariate linear regression model for anxiety included gender, age group, COVID-19 diagnosis, stressful events before the pandemic, resilience, social support, and caregivers' PHQ-9 scores. Initial variables in the multivariate linear regression model for depression included gender, age group, COVID-19 infection, nuclear family, stressful events before the pandemic, resilience, and social support. Initial variables in the multivariate linear regression model for sleep problems included gender, age group, COVID-19 diagnosis, being an only child, stressful events before the pandemic, and caregivers' PSS and PHQ-9 scores. Independent variables in the final model were determined using forward selection. *p < 0.05, **p < 0.01.
In the adjusted logistic regression model, the risk factors for mental health problems in the whole participants included stressful events before the pandemic (OR = 1.54, p = 0.025), elder age (OR = 1.17, p = 0.032), and the poor mental health status in caregivers. While, children's resilience (OR = 0.94, p = 0.003), perceived social support (OR = 0.97, p = 0.026), and higher household income (OR = 0.52, p = 0.008) might protect them against psychological symptoms. Moreover, children with COVID-19 infection had better sleep quality (OR = 0.24, p = 0.038). Details are presented in Table 3.
In the discharged children, mental health problems tended to be severe or prevalent in those experienced more stressful events before pandemic (β = 0.28, p = 0.015). Caregivers' poor mental health status (e.g., depression symptoms) might in turn worsen the psychological symptoms in children. In accordance with the relationship in the total subjects, higher level of resilience might decrease the severity of mental health problems in discharged children. Boys (β = −0.42, p = 0.050) had fewer sleep problems (Figure 2).
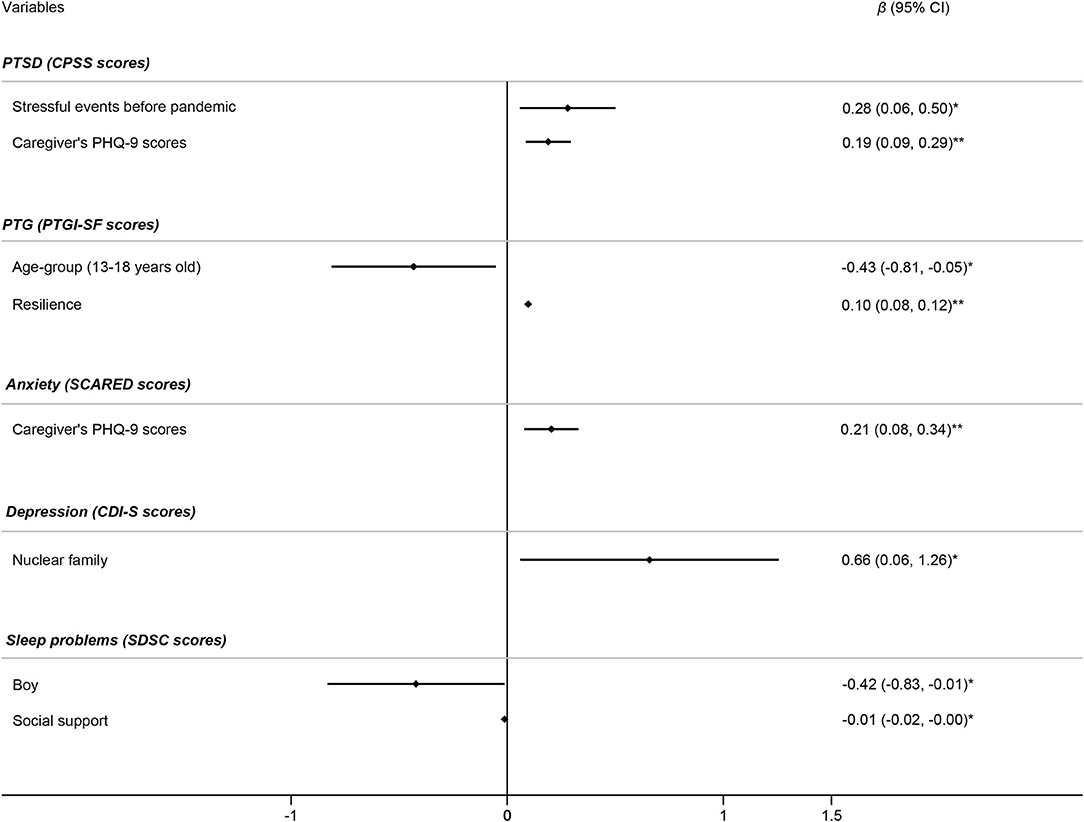
Figure 2. Factors associated with mental health symptoms in discharged children (n = 61). Initial variables in the multivariate linear regression model for PTSD included gender, age group, stressful events before the pandemic, and caregivers' GAD-7 and PHQ-9 scores. Initial variables in the multivariate linear regression model for PTG included gender, age group, resilience, social support, and caregivers' PHQ-9 and PSQI scores. Initial variables in the multivariate linear regression model for anxiety included gender, age group, and caregivers' PHQ-9 scores. Initial variables in the multivariate linear regression model for depression included gender, age group, being an only child, nuclear family, length of hospitalization, and social support. Initial variables in the multivariate linear regression model for sleep problems included gender, age group, being an only child, resilience, and social support. Independent variables in the final model were determined using forward selection. *p < 0.05, **p < 0.01.
In the logistic regression analysis, the risk factors for mental health problems in discharged children included caregivers' poor mental health, the nuclear family structure (OR = 3.68, p = 0.038) and the extended length of hospitalization (OR = 1.14, p = 0.045) (Table 4).
To our knowledge, this was the first study to analyze long-term mental health status in children who recovered from COVID-19 and discharged from hospital. We found a significantly higher level of depression compared with healthy controls who had not contracted COVID-19 and an increased trend in prevalence of PTSD and anxiety. We also found that COVID-19 infection was significantly associated with depression symptoms and sleep problems in children. Moreover, caregivers' poor mental health status was an important risk factor for mental health problems in children, especially in children who recovered from COVID-19.
The prevalence of PTSD in the present study was 4.61% among all participants (8.20% in discharged children and 2.20% in healthy controls). Individuals, especially children and adolescents, are known to have a higher risk of developing PTSD following exposure to traumatic events (14). A previous study reported that nearly two-thirds of children and adolescents might be exposed to traumatic events, such as violence, accidents, or witnessing trauma events, and 4.7–7.8% of them develop PTSD afterward (27). In the present study, the risk of developing PTSD was higher in children who previously experienced more stressful events, which was consistent with a previous study (27). As the previous exposure to the traumatic events might increase or worsen the physical or emotional reaction to the stressors or trauma, prior traumatic events exposure might increase the vulnerability of PTSD in children and adolescent (27). Additionally, children's PTSD symptoms were associated with their caregivers' PTSD symptoms. A previous cohort study found that caregivers' exposure to traumatic events was associated with a higher prevalence of PTSD, which would contribute to a harsh parenting style and consequently increase the prevalence of mental health problems in children (28). Similar results were found among children who were hospitalized because of COVID-19. Our results highlight the significance of properly addressing children's psychological needs in a timely fashion both during and after pandemics.
Children's and adolescents' responses to traumatic events vary. Some might have symptoms of PTSD, but others might experience positive changes, including hope for new possibilities, positive changes in relationships with others, the growth of personal strength, changes in spirit, and a greater appreciation of life, which are important characteristics of PTG (29). A previous systematic review identified factors that were associated with PTG, child factors (age and gender), trauma factors (type of trauma and level of trauma exposure), psychological factors (resilience and coping), and family factors (parental psychological characteristics) (30). In the present study, children who were younger and had greater resilience tended to have higher PTG, regardless of whether they had COVID-19, which was consistent with a previous study that found that older age was associated with lower PTG (30).
The overall prevalence of anxiety was 17.11% (22.95% in discharged children and 13.19% in healthy controls). It was comparable to previous studies reported that the prevalence of anxiety in children during the COVID-19 pandemic was about 20% (12). At the individual level, treatment and quarantine in a hospital bring sudden changes to children's daily routines, and some of them are separated from social network, which can worsen existing symptoms or lead to new symptoms (10). Children's mental health is related to the family environment. This was observed in the present study, in which children's anxiety was positively related to their caregivers' depression symptoms. During the COVID-19 pandemic, many parents lost their jobs and household income, which might worsen caregivers' depression symptoms and further affect the mental health status of their children (31). Another important finding in the present study was the negative correlation between children's perceived social support and anxiety symptoms. Social support is a type of psychological adjustment that helps individuals cope with difficult times, including traumatic events (32). The protective function of social support was not observed in children with COVID-19 in the present study, which might be because of the relatively limited resources of social support that were available during hospitalization.
In the present study, nearly half of the children who recovered from COVID-19 had depression symptoms. A previous study in Wuhan, China, reported that the prevalence of depression was 26.5% among children who were quarantined at home during the pandemic, which was much lower than in the present study (12). During the COVID-19 outbreak, school closures, restricted outdoor activities, and lack of social interactions might have led to more mental health problems in children who were restricted at home (33). For inpatients with COVID-19, physical inactivity, possible invasive surgeries, a higher risk of repeated infection, and separation from social network were all additional stressors (10). Interestingly, children from nuclear families were more likely to develop depression after recovering from COVID-19, suggesting that increased attention should be paid to children with emotional problems in the nuclear families. In the present study, nearly half of the families were extended families that included more than one generation. Grandparents provide important support for maintaining normal family function and are essential resources of social support, which may promote family and personal resilience (34). Additionally, the dramatic increase in the prevalence of depression indicated that increases in stress and poor mental health status exist for a prolonged time in children and adolescents even after the pandemic, highlighting the necessity of early and continuous prevention and intervention strategies to address potential mental health symptoms both during and after pandemics.
In the present study, the overall prevalence of sleep problems was 17.11% (15.00% in discharged children and 19.54% in healthy controls). Girls, being an only child, and not having COVID-19 but being quarantined at home were associated with more sleep problems. Caregivers' depression symptom was another important risk factor for sleep problems in children. This is consistent with Caldwell et al., who found that mothers' life stress was significantly and negatively related to their children's sleep quality (35). Evidence of the effects of COVID-19 on children's sleep quality is mixed, possibly because of the different ages of children in different studies. Moore et al. found that COVID-19 lockdowns did not affect sleep in children (36). Di Giorgio et al. and Lecuelle et al. reported an increase in the prevalence of sleep problems after the COVID-19 lockdown (37, 38). Both of these studies were conducted in preschool children. In contrast, we focused on school aged children and found that discharged children had fewer sleep problems than children who were quarantined at home. This might be related to a regular schedule for the hospitalized children. These findings imply that interventions for sleep problems in children and adolescents are essential, especially for children who are quarantined at home.
The present study investigated the prevalence of mental health consequences and risk factors among Chinese pediatric patients who had COVID-19, were hospitalized, and then were discharged. The present study has limitations. First, the total sample size was relatively small, which might decrease statistical power. Only one in three of the children who were hospitalized during the pandemic agreed to follow-up physical and mental health examinations. Such a lack of willingness to participate in the present study might be because that the children or caregivers feared being stigmatized. Further studies with larger and representative sample sizes are needed. Second, mental health status of children and adolescents was a cross-sectional assessment. We are planning to conduct follow-up studies to analyze trajectories of mental health symptoms in pediatric patients. Third, children and adolescents in the control group were mainly enrolled from a birth cohort in Wuhan Children's Hospital, which began in 2012. As a result, the oldest children in this cohort were 8 years old. The median age of the healthy controls was younger than discharged children. Future studies are needed with matched samples.
In conclusion, mental health problems were common among children who had COVID-19, even 4 months after hospital discharge. Children who experienced more stressful events before the pandemic and whose caregivers reported more depressive symptoms were more likely to develop PTSD and anxiety. Discharged children, especially children in nuclear families, were more likely to suffer from depressive symptoms compared with healthy controls. Caregivers' PTSD symptoms were another risk factor for children's poor sleep after COVID-19 recovery. Interventions and strategies that focus on children's mental health outcomes should be developed and provided to children continuously even after pandemics. For children who have had COVID-19, specific attention should be paid to those from nuclear families, girls, and students from junior and senior high school. Protecting and maintaining the mental health of caregivers should also be considered an essential strategy to improve children's mental health after COVID-19 and quarantine.
The datasets presented in this article are not readily available because this dataset is shared and managed by the authors in Peking University Sixth Hospital and Wuhan Children's Hospital. It might not be opened without the agreement of data managers in Peking University Sixth Hospital and Wuhan Children's Hospital. Requests to access the datasets should be directed to Jiajia Liu, bGl1amlhamlhX3NkdUBiam11LmVkdS5jbg==; Lin Lu, bGlubHVAYmptdS5lZHUuY24=; Han Xiao, dGp4aWFvaGFuMTk4MEAxNjMuY29t; and Zhisheng Liu, bGl1enNjQDEyNi5jb20=.
The studies involving human participants were reviewed and approved by the Ethics Committee of Wuhan Children's Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
AZ, LS, WY, and HX wrote the initial draft of manuscript with contributions from JL and YB. AZ and JL developed the study design and analysis plan. AZ, HX, ZW, JL, and HM collected the questionnaires. AZ and JL conducted the data analyses with help from YB. LS, YB, JL, JD, and LL critically revised the manuscript. JS, ZL, JL, and LL supported and led the data collection and data analysis. All authors approved the results and final version.
This study was supported by the Fundamental Research Funds of the Central Universities (no. 69004Y1230), National Natural Science Foundation of China (nos. 81761128036, 81821092, and 31900805), National Key Research and Development Program of China (no. 2019YFA0706200), PKU-Baidu Fund (2020BD011), and Peking University Medicine Fund of Fostering Young Scholars' Scientific and Technological Innovation and Fundamental Research Funds for Central Universities (no. BMU2020PYB013).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Authors would like to thank all the children and their parents that take part in our study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.759449/full#supplementary-material
1. World Health Organisation. WHO Coronavirus Disease (COVID-19) Dashboard. (2020). Available online at: https://covid19.who.int (accessed May 31, 2021).
2. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
3. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
4. Blix I, Birkeland MS, Thoresen S. Worry and mental health in the Covid-19 pandemic: vulnerability factors in the general Norwegian population. BMC Public Health. (2021) 21:928. doi: 10.1186/s12889-021-10927-1
5. Petersen MW, Dantoft TM, Jensen JS, Pedersen HF, Frostholm L, Benros ME, et al. The impact of the Covid-19 pandemic on mental and physical health in Denmark - a longitudinal population-based study before and during the first wave. BMC Public Health. (2021) 21:1418. doi: 10.1186/s12889-021-11472-7
6. Ranieri J, Guerra F, Perilli E, Passafiume D, Maccarone D, Ferri C, et al. Prolonged COVID 19 outbreak and psychological response of nurses in Italian Healthcare System: cross-sectional study. Front Psychol. (2021) 12:608413. doi: 10.3389/fpsyg.2021.608413
7. Shi L, Que JY, Lu ZA, Gong YM, Liu L, Wang YH, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry. (2021) 64:e18. doi: 10.1192/j.eurpsy.2021.5
8. Wang Y, Shi L, Que J, Lu Q, Liu L, Lu Z, et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry. (2021) 1–10. doi: 10.1038/s41380-021-01019-y
9. Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. (2020) 4:347–9. doi: 10.1016/S2352-4642(20)30096-1
10. Saurabh K, Ranjan S. Compliance and psychological impact of quarantine in children and qdolescents due to Covid-19 pandemic. Indian J Pediatr. (2020) 87:532–6. doi: 10.1007/s12098-020-03347-3
11. Chawla N, Tom A, Sen MS, Sagar R. Psychological impact of COVID-19 on children and adolescents: a systematic review. Indian J Psychol Med. (2021) 43:294–9. doi: 10.1177/02537176211021789
12. Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei province, China. JAMA Pediatr. (2020) 174:898–900. doi: 10.1001/jamapediatrics.2020.1619
13. Hou TY, Mao XF, Dong W, Cai WP, Deng GH. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J Psychiatr. (2020) 54:102305. doi: 10.1016/j.ajp.2020.102305
14. Yuan K, Gong YM, Liu L, Sun YK, Tian SS, Wang YJ, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry. (2021) 1–17. doi: 10.1038/s41380-021-01036-x
15. Chawla N, Sharma P, Sagar R. Psychological impact of COVID-19 on children and adolescents: is there a silver lining? Indian J Pediatr. (2021) 88:91. doi: 10.1007/s12098-020-03472-z
16. Society of Pediatrics Chinese Medical Association The Editorial Board Chinese Journal of Pediatrics. Recommendations for the diagnosis, prevention and control of the 2019 novel coronavirus infection in children (first interim edition). Chin J Pediatr. (2020) 58:E004. doi: 10.3760/cma.j.issn.0578-1310.2020.0004
17. Foa EB, Johnson KM, Feeny NC, Treadwell KR. The child PTSD symptom scale: a preliminary examination of its psychometric properties. J Clin Child Psychol. (2001) 30:376–84. doi: 10.1207/S15374424JCCP3003_9
18. Su L, Wang K, Fan F, Su Y, Gao X. Reliability and validity of the screen for child anxiety related emotional disorders (SCARED) in Chinese children. J Anxiety Disord. (2008) 22:612–21. doi: 10.1016/j.janxdis.2007.05.011
19. Allgaier AK, Frühe B, Pietsch K, Saravo B, Baethmann M, Schulte-Körne G. Is the children's depression inventory short version a valid screening tool in pediatric care? A comparison to its full-length version. J Psychosom Res. (2012) 73:369–74. doi: 10.1016/j.jpsychores.2012.08.016
20. Huang MM, Qian Z, Wang J, Vaughn MG, Lee YL, Dong GH. Validation of the sleep disturbance scale for children and prevalence of parent-reported sleep disorder symptoms in Chinese children. Sleep Med. (2014) 15:923–8. doi: 10.1016/j.sleep.2014.03.023
21. Liu JE, Wang HY, Hua L, Chen J, Wang ML, Li YY. Psychometric evaluation of the simplified Chinese version of the posttraumatic growth inventory for assessing breast cancer survivors. Eur J Oncol Nurs. (2015) 19:391–6. doi: 10.1016/j.ejon.2015.01.002
22. Taylor MK, Hernández LM, Sessoms PH, Kawamura C, Fraser JJ. Trauma exposure and functional movement characteristics of male tactical athletes. J Athl Train. (2020) 55:384–9. doi: 10.4085/1062-6050-111-19
23. Scali J, Gandubert C, Ritchie K, Soulier M, Ancelin ML, Chaudieu I. Measuring resilience in adult women using the 10-items Connor-Davidson Resilience Scale (CD-RISC). Role of trauma exposure and anxiety disorders. PLoS ONE. (2012) 7:e39879. doi: 10.1371/journal.pone.0039879
24. Grassi L, Rasconi G, Pedriali A, Corridoni A, Bevilacqua M. Social support and psychological distress in primary care attenders. Psychother Psychosom. (2000) 69:95–100. doi: 10.1159/000012372
25. Laksmita OD, Chung MH, Liao YM, Chang PC. Multidimensional scale of perceived social support in indonesian adolescent disaster survivors: a psychometric evaluation. PLoS ONE. (2020) 15:e0229958. doi: 10.1371/journal.pone.0229958
26. Gueugnon M, Stapley PJ, Gouteron A, Lecland C, Morisset C, Casillas JM, et al. Age-related adaptations of lower limb intersegmental coordination during walking. Front Bioeng Biotechnol. (2019) 7:173. doi: 10.3389/fbioe.2019.00173
27. McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, et al. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry. (2013) 52:815–30.e814. doi: 10.1016/j.jaac.2013.05.011
28. Bryant RA, Edwards B, Creamer M, O'Donnell M, Forbes D, Felmingham KL, et al. The effect of post-traumatic stress disorder on refugees' parenting and their children's mental health: a cohort study. Lancet Public Health. (2018) 3:e249–58. doi: 10.1016/S2468-2667(18)30051-3
29. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. (1996) 9:455–71. doi: 10.1002/jts.2490090305
30. Bernstein M, Pfefferbaum B. Posttraumatic growth as a response to natural disasters in children and adolescents. Curr Psychiatry Rep. (2018) 20:37. doi: 10.1007/s11920-018-0900-4
31. Shah K, Mann S, Singh R, Bangar R, Kulkarni R. Impact of COVID-19 on the mental health of children and adolescents. Cureus. (2020) 12:e10051. doi: 10.7759/cureus.10051
32. Scardera S, Perret LC, Ouellet-Morin I, Gariépy G, Juster RP, Boivin M, et al. Association of social support during adolescence with depression, anxiety, and suicidal ideation in young adults. JAMA Netw Open. (2020) 3:e2027491. doi: 10.1001/jamanetworkopen.2020.27491
33. Meng S, Dong P, Sun Y, Li Y, Chang X, Sun G, et al. Guidelines for prevention and treatment of internet addiction in adolescents during home quarantine for the COVID-19 pandemic. Heart Mind. (2020) 4:95–9. doi: 10.4103/hm.hm_36_20
34. Hwang HJ, St James-Roberts I. Emotional and behavioural problems in primary school children from nuclear and extended families in Korea. J Child Psychol Psychiatry. (1998) 39:973–9. doi: 10.1111/1469-7610.00400
35. Caldwell BA, Redeker NS. Maternal stress and psychological status and sleep in minority preschool children. Public Health Nurs. (2015) 32:101–11. doi: 10.1111/phn.12104
36. Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. (2020) 17:85. doi: 10.1186/s12966-020-00987-8
37. Di Giorgio E, Di Riso D, Mioni G, Cellini N. The interplay between mothers' and children behavioral and psychological factors during COVID-19: an Italian study. Eur Child Adolesc Psychiatry. (2020) 30:1401–12. doi: 10.1007/s00787-020-01631-3
Keywords: children, adolescent, mental health, COVID-19, PTSD
Citation: Zhang A, Shi L, Yan W, Xiao H, Bao Y, Wang Z, Deng J, Ravindran A, Yuan K, Mei H, Shi J, Liu Z, Liu J and Lu L (2021) Mental Health in Children in the Context of COVID-19: Focus on Discharged Children. Front. Psychiatry 12:759449. doi: 10.3389/fpsyt.2021.759449
Received: 16 August 2021; Accepted: 18 October 2021;
Published: 11 November 2021.
Edited by:
Veit Roessner, University Hospital Carl Gustav Carus, Dresden, GermanyReviewed by:
Nishtha Chawla, All India Institute of Medical Sciences, IndiaCopyright © 2021 Zhang, Shi, Yan, Xiao, Bao, Wang, Deng, Ravindran, Yuan, Mei, Shi, Liu, Liu and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Lu, bGlubHVAYmptdS5lZHUuY24=; Jiajia Liu, bGl1amlhamlhX3NkdUBiam11LmVkdS5jbg==; Zhisheng Liu, bGl1enNjQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.