
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 22 October 2021
Sec. Psychological Therapies
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.755744
This article is part of the Research TopicEfficacy of Psychological and Psychiatric Treatments and Potential Predictors in Social Anxiety Disorder and Obsessive-Compulsive DisorderView all 5 articles
 Vittoria Zaccari1,2*
Vittoria Zaccari1,2* Andrea Gragnani1
Andrea Gragnani1 Valerio Pellegrini3
Valerio Pellegrini3 Tecla Caiazzo1
Tecla Caiazzo1 Maria Chiara D'Arienzo1
Maria Chiara D'Arienzo1 Antonella Magno1
Antonella Magno1 Giuseppe Femia1
Giuseppe Femia1 Francesco Mancini1,2
Francesco Mancini1,2Background and Objectives: While the consequences of the COVID-19 pandemic for general mental health and the increase in anxiety and depression are clear, less is known about the potential effect of the pandemic on OCD. The purpose of this study is to collect new data to monitor the symptomatic status of patients with OCD during the period of emergency due to COVID-19 and to make a comparison between two psychodiagnostic evaluations.
Methods: Eleven OCD patients and their psychotherapists were recruited. All patients had a specific psychodiagnostic assessment for OCD (SCL-90; OCI-R; Y-BOCS self-report) performed between December 2019 and January 2020 (t0), and undertook cognitive behavioral therapy (CBT) and exposure and prevention of response protocol (ERP) before the lockdown. The psychodiagnostic assessment carried out at t0 was re-administered (t1) to all patients, together with a set of qualitative questions collected through an online survey. The respective therapists were asked to document the status of the therapy and the monitoring of symptoms through use of a semi-structured interview (Y-BOCS) and a qualitative interview. Non-parametric analyses were conducted.
Results: Patients reported a significant decrease in OCD symptoms. Data analysis showed a decrease in the scores across t0 and at t1 on the Y-BOCS (SR) total self-report, and on OCD symptoms' severity assessed by means of the OCI-r and SCL-90 r OC subscale, for 11 participants. Relating to the measures detected by psychotherapists, marginally significant improvements and lower scores were found in the Y-BOCS (I). An improvement in symptoms was noticed by 90.9% of the clinical sample; this was confirmed by 45.4% of the therapists, who claimed moderate progress in their patients.
Conclusions: The data collected through standardized measurements at two different times, albeit relative to a small sample, assume relevance from a clinical point of view. In the literature, some studies document the worsening of OCD. However, in many studies, the type of treatment, the detection time, and the intervention period are not well-specified. These results confirm the effectiveness of CBT/ERP as an elective treatment for OCD through a specific intervention procedure.
The COVID-19 pandemic had a significant impact on mental health in clinical and non-clinical populations (1–3). A wide range of studies has shown the impact on psychological distress in the adult clinical population (4, 5), in the general population (6–15), and in children and adolescents (16–20).
The pandemic has been associated with worsened mental health for those with pre-existing problems as well as new-onset mental health worries (21–23). The consequences for mental health and the increase of stress, depression, anxiety disorders, and suicide risk seem clear, as is well-documented in systematic reviews and metanalyses (10, 24–26).
The experience of long quarantine and isolation led to high levels of anger, stress, and confusion (27). Furthermore, during the pandemic, people were exposed to experience fear and fear linked to a greater likelihood of contamination, and were invited to implement protective behaviors. It is well-known that those who suffer from psychopathological anxiety engage in a series of safety-seeking, protective, and avoidance behaviors, or prudential reasoning, in order to avoid a threat, aspects that have a role in the maintenance of psychopathological symptoms (28, 29).
Although the consequences of the COVID-19 pandemic for general mental health and the increase in anxiety and depression are clear, less is known about the potential effect of the pandemic on obsessive-compulsive disorder [OCD; (30, 31)]. The increase in distress, concern, and fear has affected reactions to the present situation and exacerbated some existing psychiatric disorders (32, 33). In fact, some symptomatic domains have been triggered, typically anxiety or OCD (34, 35).
In this situation, the health impact of the COVID-19 pandemic on OCD cannot be overlooked. A growing body of research has shown how OCD is associated in some cases with a symptomatology that is highly sensitive to the fear and probability of contamination, with a perception of a greater possibility of becoming infected or infecting others, and with protective behaviors aimed at removing or neutralizing the possible risk of contamination (36–39), or preventing or neutralizing the fear of guilt related to irresponsibility (40–43, 48, 76) a specific mental state related to checking and cleaning compulsions (44). All these aspects were strongly conveyed in the period of emergency due to COVID-19.
The precautionary measures against COVID-19, such as hand washing, maintaining a high level of hygiene, and avoiding handshakes, may have triggered psychological distress in OCD patients, consequently increasing their symptoms. In this regard, it could be interesting to understand how the pandemic has triggered new or others fears, or if social isolation and restrictions have reinforced maintenance mechanisms such as avoidance behaviors, major doubt tendency, and major responsibility. Moreover, the constant condition of doubt, uncertainty, and fear of contagion may have caused an increase in prudential cognitive processes, mechanisms involved in the genesis and maintenance of the disorder (40, 41, 45–50). It is interesting to reflect on how this condition of uncertainty and alarm due to the pandemic has influenced OCD patients and so how the pandemic and the lockdown period may have affected OCD patients. However, two reviews have investigated the impact of the COVID-19 pandemic on OCD (30, 31) and the results are controversial.
A review by Sulaimani and Bagadood (30) analyzed all the empirical contributions on OCD, the most recent published in August 2020, and studies published from 2016 to 2020, and showed an increase in anxiety due to COVID-19, underlining that the associated prevention measures increase the severity of OCD symptoms. In their review, the authors highlight a worsening of OCD symptoms. However, it is impossible to generalize the results because the study refers only to the USA, China, India, and the UK. Another recent narrative review by Zaccari et al. (31) highlighted the presence of a small number of studies with controversial results. The authors underline that few studies have specified OCD subtypes and that samples cover a wide age range. Additionally, a large number of studies used different monitoring periods or quantitative measures, or did not use the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), considered the gold standard for OCD evaluation (45a). Also, in most studies, the typology of treatment was not clear. Due to these differences and lack of information, it was difficult to compare and rely on the results.
Even if patients in some studies showed an increase in the severity and in the number of obsessions (51–54), OCD patients in others have been only minimally impacted by the pandemic (23, 55) or shown a slight decrease in symptoms (56). Moreover, regarding the typology of treatment, Zaccari et al. (31) showed that OCD patients were given cognitive behavioral therapy (CBT) treatment with exposure and response prevention (ERP) during the monitoring period in only two studies (54, 57).
Storch et al. (54) reported on clinicians' perceptions of the impact of the COVID-19 pandemic on individuals with OCD receiving ERP prior to and during the pandemic. From this study emerges a general worsening of OCD symptoms in patients (over one-third of patients) during the initial period of the COVID-19 pandemic despite continuing active treatment. These findings show that the COVID-19 pandemic represented a significant stressor for most patients with OCD, exerting a negative effect on symptomatology.
The results of the study by Kuckertz et al. (57) are different. Their typical program was an intensive program, including 2–4 h of ERP daily; four groups daily based on CBT and acceptance and commitment therapy (ACT); and meetings with a behavior therapist (2–3x/week), a family therapist (1x/week), and a psychiatrist (1x/week). Compared to the general population, their patients varied in the ways they were impacted by COVID-19, yet the majority experienced improvements in OCD symptoms despite the context.
Although CBT and ERP represent the elective treatment for OCD according to the National Institute for Health and Clinical Excellence guidelines (58), Zaccari et al. (31) reported that only two studies used this protocol. Over the last 30 years, different studies have confirmed the beneficial effect of CBT with ERP for OCD patients (59–62, 100).
Moreover, there is a lack of use of quantitative measures as the Y-BOCS, considered the gold standard for OCD evaluation. In fact, symptom change before and after treatment according to Y-BOCS assessments is the primary outcome measure in pharmacological and psychotherapeutic intervention trials for OCD [see meta-analysis by (63)]. As a result, national and international guidelines for evidence-based interventions for OCD largely depend on the reliability and validity of the Y-BOCS.
This study aims to investigate the effects of the pandemic on OCD patients. In particular, the study aims to collect new data to monitor the symptomatic status of patients with OCD during the period of emergency due to COVID-19. At the same time, it aims to make a comparison between OCD subjects evaluated in the period December 2019–January 2020 and the current state. In accordance with the recent literature examined, we hypothesize that there is a general worsening of symptoms in OCD patients who presented a degree of impairment at the time of the initial evaluation through a difference in total scores in the different quantitative measures used for OCD symptoms. From the qualitative perspective, we expect that OCD patients and their respective psychotherapists will declare a worsening of their symptomatic status through a qualitative questionnaire. To achieve our purpose, we evaluated both patients' subjective perception of distress and the clinical judgment of psychotherapists through a self-report form and clinical interview.
For the purpose of this study, we recruited a sample of 11 adult Italian patients with OCD (male: 4; age: M = 34.55, SD = 7.88) who were undergoing treatment at the Center for Cognitive Psychotherapy in Rome but were not taking any medication, and their related psychotherapists. Diagnosis of OCD was made according to DSM-5 criteria (64) based on an extensive clinical examination and psychodiagnostic assessment.
Participants were recruited from the clinical assessment database belonged to the Center for Cognitive Psychotherapy in Rome. The selected patients were those undergoing CBT psychotherapy (with ERP) during the COVID-19 emergency period (March–December 2020). All patients had undergone previous treatment but had been evaluated at the symptom level in December 2019–January 2020.
Inclusion criteria for the study were as follows: being over 18 years of age; having a principal diagnosis of OCD, as diagnosed by an expert clinician using the Structured Clinical Interview for Diagnosis [SCID-5-CV; (65)]; having undergone a psychodiagnostic assessment with specific OCD quantitative measures and general symptomatology in the period December 2019–January 2020; having had CBT therapy with ERP during 2020; and reporting significant OCD symptoms at baseline [defined as a severe degree of impairment on the Y-BOCS ≥26 (66)]. Exclusion criteria included the following: significant physical or mental comorbid disorders (psychosis, schizotypy, borderline personality, mania, alcohol or drug abuse or dependence, impaired cognitive function); a current marked risk to self (self-harm or suicide); or dissociation symptoms (assessed on the basis of the first clinical evaluation with a clinical interview and psychodiagnostics assessment). Participant characteristics, gender, age, medications, and OCD subtypes for each subject are shown in Table 1.
Before recruitment to the study, we established the aims and the procedure, as well as the issues surrounding anonymity and privacy. Those who agreed to participate in the study were asked to complete a written informed consent and a battery of self-report questionnaires. No compensation was given for participation in the study. The procedure has been approved by the Ethical Committee of School of Cognitive Psychotherapy (Italy) and written informed consent from each participant were obtained before study initiation.
OCD patients who had undergone psychodiagnostic evaluations and clinical diagnosis between December 2019 and January 2020 (t0) were selected from the clinical center's database. The selected subjects had started a CBT intervention and treatment with ERP between January and February 2020. They were recruited between December 2020 and January 2021 again for a follow-up during the pandemic period (t1), undergoing the same psychodiagnostic assessment as at t0. Follow up data allow to monitor the symptomatic status of patients during the difficult period of COVID-19 pandemic.
Patients were assessed with respect to OC measures and symptomatology measures, and by qualitative questionnaires administered to their own psychotherapists and to the patients through an online survey prepared ad hoc. The assessment and scoring tests at t0 were rated by an expert psychodiagnostic clinician and at t1 by online survey, including a self-report measure and a qualitative report for patients and clinicians.
All subjects underwent a CBT intervention procedure according to international guidelines (67). The results obtained previously with this procedure were satisfactory: a clinically significant improvement was obtained in about 80% of all patients to whom this procedure was proposed. Furthermore, it is important to highlight that a very low rate of refusal of therapy and drop-out was found, at about 2% (67).
A crucial aspect of treatment is exposure with response prevention, consisting of a series of practical exercises for accepting consistently higher levels of threat. The underlying rationale is that if the patient increases the accepted level of risk, the effect is a lower investment in preventive activity and therefore less resistance to changing threat assumption (68–71). Alongside the exposure is a series of cognitive techniques and procedures aimed, in particular, at increasing motivation and collaboration in treatment and making the patient less vulnerable to the issues and mechanisms involved in maintenance of the disorder. The intervention procedure is divided into five phases.
The first phase starts after the preliminary assessment. It consists of reconstruction and sharing of the functioning scheme of the patient's disease. The purpose behind this phase is two-fold: to reconstruct the internal profile of the disorder (which allows rational planning of the therapeutic intervention), and to construct a good therapeutic alliance.
The second phase involves the possibility of modifying those beliefs that support the threat evaluation. The expected effect is the reduction of investment in threat prevention (72). Cognitive restructuring techniques—the probability pie technique and the cumulative probability technique—are used to reduce the probabilities of events (73), along with techniques to reduce responsibility (defense lawyer), and interventions for the normalization of forbidden thoughts (74), useful to reinforce an alternative to the beliefs that support valuations.
The purpose of the third phase is to promote factual acceptance, to help the patient enter the order of ideas that the threat, doubt and uncertainty can be accepted and should be accepted. This is achieved through modification of three different patient assumptions: the power to reduce risk, the advantage of investing in this direction, and the obligation to engage in risk reduction (75). This has a dual purpose. The first is to facilitate the acceptance of ERP exercises and increase the motivation to implement them. The second is justified by the fact that if a threat is accepted, the protective investment is reduced and, within this, the hyperprudent cognitive orientation, thus increasing the possibility that corrective information of the threat perception can really be taken into consideration by the patient (76, 77). At the same time ERP is introduced. The ERP is the most empirically effective CBT intervention (78). The procedure involves the combined application of two components: exposure and response prevention. It is appropriate to conceptualize the ERP as a series of practical exercises in accepting gradually increasing threat levels (79, 80).
The procedure used is the classic one in its different variants: gradual or prolonged exposure to the dreaded situations, with prevention of the responses frequently implemented by the patient (avoidance, and overt or covert rituals). The exposure predicts that the patient will be exposed to the feared stimuli, external or internal, for a time interval longer than he/she is normally willing to tolerate. Contact generally involves in vivo exposure with the anxiety-inducing stimulus according to a logic of progressive graduality; in some cases, due to precise therapeutic choices or depending on the specificity of the obsessive content, the exposure can also take place through an imaginative procedure. Prevention of the response, on the other hand, consists of interrupting the protective behaviors, also in this case for a longer time than usually elapses when the person postpones a ritual.
The fourth and fifth phases include action to reduce vulnerability to the OCD and are aimed to reduce the general disposition of OC patients to fear of guilt [(47, 81)]. This aim is pursued in two steps.
The first step (82) involves helping the patient to recognize the centrality that the fear of being guilty plays in their everyday life, focusing on situations in which this is activated and the quality of the internal dialogue, offering monitoring tasks to recognize the fear of being guilty, even at the body level. After this intervention the therapist helps the patient to decatastrophize the possibility of being guilty.
After that, the intervention is on the historical vulnerability working on elements of the patient's life history that have favored the onset of the disorder such as experiences, sensitizing episodes, factors predisposing to the specific disorder/problem. This phase's purpose is to make sensitizing experiences less relevant from an emotional point of view (83–86).
Finally, the last phase of treatment includes action to prevent relapses. At the end of the psychotherapeutic work, it is appropriate to discuss the possibility that the symptoms recur and define concrete interventions through which the patient can face them (75). Gragnani and Tenore (75) suggest sharing with the patient an alarm threshold beyond which it is convenient to contact the psychotherapist. Once the therapeutic objective has been achieved and an accurate phase of prevention of relapse finished it is possible to start the last part of the process: the conclusion of the therapy. It consists in retracing with the patient the phases of the work carried out and restructuring any dysfunctional beliefs on the end of the therapy.
Participants were given a battery of online tests through the QuestionPro platform, guaranteeing privacy and assigning each of them an identification code associated with an alphanumeric code assigned by their psychotherapist. Demographic information was collected using an initial questionnaire created by the authors of the study.
Several self-report questionnaires were administrated to investigate the severity of symptomatology, as follows.
The Obsessive-Compulsive Inventory-Revised [OCI-r; (87, 88), Italian version by (89)] is a brief, 18-item self-report questionnaire designed to measure the presence and distress caused by obsessive compulsive symptoms on a five-point Likert-type scale ranging from 0 (not at all) to 4 (extremely). The instrument assesses symptoms on six different dimensions including washing, checking, ordering, obsessing, hoarding, and mental neutralizing (three items each). The OCI-r Italian version (89) showed good internal consistency as well as convergent, divergent, and criterion validity [alpha = 0.85]. In the present study, only the total score is used.
The Yale-Brown Obsessive-Compulsive Scale [Y-BOCS; (90, 91); Italian version by (92)] was used to assess severity of OCD symptoms. It is a widely used clinician- administered interview to assess the presence and the severity of OCD symptoms in adults. The Y-BOCS includes two sections: the symptom checklist (Y-BOCS-SC) and the severity scale (Y-BOCS-SS). The symptom checklist is a clinician-rated checklist designed to guide a structured interview to determine the target symptoms for treatment. The severity scale consists of 10 items that assess the severity of obsessions (five items) and compulsions (five items) using a five-point Likert-type scale (from 0 to 4; the total score of the scale may range between 0 and 40). The final rating is based on the clinical judgment of the interviewer. In the present study, the Y-BOCS interview was administered by psychotherapists in parallel with online administration of the self-report form [Y-BOCS-SR; (93)]. Only the total score of Y-BOCS and the obsessions and compulsions subscales both in the self-report form to the patient and in the version by the clinicians (their psychotherapist) are used. The scales showed strong internal consistency for the total score and each subscale [α = 0.89–0.93; (94)].
The Symptom Checklist 90-Revised [SCL-90-R; (95); Italian version by (96)] is self-report questionnaire designed to measure general psychological symptoms and psychological distress. It contains nine subscales—somatization (SOM), obsessive-compulsive (O-C), interpersonal sensitivity (I-S), depression (DEP), anxiety (ANX), hostility (HOS), phobic anxiety (PHOB), paranoid ideation (PAR), and psychoticism (PSY)—and the nine frequently used subscales provide symptom profiles. It is a five-point Likert scale ranging from 1 to 5, where 1 = “not at all,” 2 = “a little bit,” 3 = “moderately,” 4 = “quite a bit,” and 5 = “extremely.” Thus, a higher score reflects a higher frequency or intensity of symptoms. The Global Severity Index (GSI) is equal to the average of all nine subscale scores. The internal consistency coefficients for the nine subscales were 0.76–0.90. In the present study, only the OC subscale is used.
In order to test our hypotheses, two questionnaires (one for psychotherapists and the other for patients) were created specifically for the purposes of the study and investigated a set of variables: (a) general information; (b) the frequency of psychotherapy during the pandemic and lockdown period; (c) possible suspension of psychotherapy; (d) evaluation of a worsening of symptoms; (e) evaluation of an improvement in symptoms; (f) appearance of new obsessions or compulsions; and (g) perception of how much the psychotherapy in progress has represented a protective factor against worsening or relapse.
Given the small number of participants, data were analyzed using a non-parametric test. Specifically, we implemented the Wilcoxon Signed Ranks Test for non-parametric comparison of the scores between the baseline (t0) and during treatment (t1) to show y participants on the following measures: total score of Y-BOCS-SS, obsessions and compulsions subscales, total score of OCI-r, and SCL-90 OC subscale. Analyses were conducted using the Statistical Package for Social Science (SPSS 25, Inc., Chicago, IL).
In a preliminary exploration of the data, we computed the descriptive statistics of the investigated variables at each measurement time (t0 and t1). Table 2 shows the resulting means and standard deviations. Because of the reduced size of the sample under examination, descriptive analyses were enriched by computing the median of participants' scores on each measure and the associated interquartile range. This latter was considered an indicator of data dispersion from the central tendency.
As previously mentioned, the small number of participants allows investigation of our hypotheses by means of non-parametric analyses. Thus, we implemented a Wilcoxon Signed Ranks Test for non-parametric comparison of the investigated OCD symptomatology between the t0 and t1 assessments (see Table 3).
As regards the primary outcome, the Wilcoxon tests showed a significant decrease in the scores across t0 and at t1 on the Y-BOCS (SR) total self-report form (p < 0.003), and of both the related sub-dimensions, obsessions (p < 0.003) and compulsions (p < 0.003). All patients reported lower scores at t1. The descriptive statistics data analysis shows a decrease in scores at t1 compared to t0 for the specific measures for OCD: Y-BOCS (SR) total (t1: M = 16; SD = 8.7 vs. t0: M = 30; SD = 5.9); Y-BOCS (SR) Obs. (t1: M = 8.5; SD = 4 vs. t0: M = 15.2; SD = 2.8); Y-BOCS (SR) Comp. (t1: M = 7.5; SD = 4.9 vs. t0: M = 14.8; SD = 3.4); OCI-r (t1: M = 16.4; SD = 14.3 vs. t0: M = 21.5; SD = 15.5); SCL-90 r OC (t1: M = 1.2; SD = 1 vs. t0: M = 1.8; SD = 0.9).
In terms of the secondary outcomes, the Wilcoxon tests also showed a significant decrease in scores for OCD symptoms' severity assessed by means of the OCI-r (p < 0.026) and SCL-90 r OC subscale (p < 0.24). Thus, participants' scores of 9 (for OCI-r) and 8 (for SCL-90) demonstrated decreases at follow-up, indicating a significant treatment effect. Specifically, the Wilcoxon tests showed a decrease in scores for Y-BOCS (SR), OCI-s, and SCL-90 r OC for 11 participants (see Table 3).
Relating to the measures detected by psychotherapists, marginally significant improvements, and lower scores were found only in the Y-BOCS (I) Obs. (p < 0.045; 8 out of 11 patients had scores lower than at t1). There were no statistically significant differences in the total score and the sub-dimension of compulsions for Y-BOCS (I) (see Table 3).
However, although no significant differences emerge, qualitatively it is found that nine patients reported scores lower than t1 in the total Y-BOCS (I) score, while only 7 of 11 reported scores lower than t1 in the compulsions sub-dimension (see Table 2).
From the qualitative data, collected from a questionnaire designed for this study, it is possible to observe good homogeneity of the sample. A total of 72.7% of participants were undergoing weekly treatment, the remainder being in treatment on a fortnightly basis (see Table 4). Only 1 of the 11 patients had suspended psychotherapy: 90.9% of the participants affirmed that their psychotherapy did not suffer suspensions.
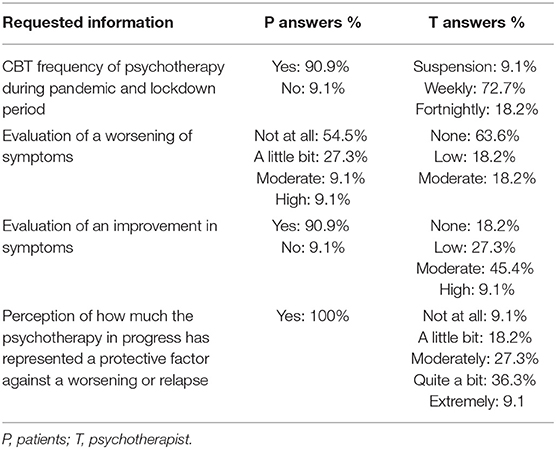
Table 4. Descriptive data: responses to the qualitative questionnaire administered to OCD patients and their psychotherapists.
However, as emerged from the therapists' questionnaire, some patients temporarily interrupted treatment, but it was just a summer interruption or was for work reasons.
More than half of patients (54.5%) did not observe a worsening of symptoms. Only in a single case did a therapist recognize the rise of a new obsession, probably falling into the checking subtype. This patient constantly checked if she was taking her birth-control pill correctly. In the other sample, therapists did not register the appearance of any new obsession or compulsion. In fact, 90.9% of the clinical sample noticed an improvement in their symptoms, and this was confirmed by 45.4% of the therapists, who claimed “moderate” progress in their patients.
All of the clinical sample affirmed that psychotherapy represented a protective factor against a worsening of their symptoms. According to these data, 45.4% of the therapists noticed a “quite a bit” or an “extreme” role of patients' psychotherapy during the pandemic.
This study aimed to investigate if the COVID-19 pandemic exacerbated the symptomatology of 11 OCD patients through an evaluation of the point of view of patients and psychotherapists. Indeed, this objective was pursued using psychodiagnostics evaluation carried out in two stages, with OCD patients and by recruiting their psychotherapists. This gave us the chance to consider evaluations regarding improvements/worsening of symptomatology and frequency of psychotherapy.
Although the sample was small, the results disconfirmed our hypothesis: patients did not have a worsening of symptomatology. We were still able to observe a significant decrease in the scores in the two specific OCD measures, Y-BOCS and OCI-r total scores, and in the SCL-90 OC subscale.
These statistical data were supported by the qualitative data wherein it was possible to observe a decrease in the follow-up scores compared to the baseline. Thus, despite this negative period, OCD patients' symptomatology was not adversely affected. The results also confirmed a decrease in symptomatology in self-report measures of the OCD re-test.
Thus, despite short periods of suspension of treatment, patients did not have worse symptomatology in the follow-up, as already highlighted by Kuckertz et al. (57).
For the qualitative data, as in many other studies (52, 53), we submitted questions to assess the subjective perception of the impact of the pandemic through the use of an ad hoc questionnaire. In line with others' results (56, 57, 97), we saw that most patients did not report a worsening of symptoms, and, in our study, the entire sample considered therapy a protective factor in the pandemic period.
Our observational study is one of the few studies (56) to assess symptom improvement in OCD patients during pandemic.
This result could be linked to the continued psychotherapy that the entire sample was receiving. The 11 patients were undergoing the same treatment procedure (67), an intervention procedure with CBT with ERP following international guidelines.
CBT with ERP treatment was used in two longitudinal studies (54, 57). In Kuckertz et al. (57), in response to COVID-19, part of the sample was more focused on the opportunity of engaging in new exposures and was interested in achieving new treatment goals. In contrast, in Storch et al. (54), clinicians observed a deterioration of symptoms in one-third of patients despite the continued therapy.
In our study, patients were followed for the same monitoring period and reported significant OCD symptoms at the baseline. Even though it is possible to observe lower scores in symptomatology in the follow-up from patients' results, in the psychotherapists' evaluations we detect only marginally significant improvements in obsession scores. Psychotherapists highlighted no statistically significant differences in the total score or in the compulsions sub-dimension of Y-BOCS. Despite this, even when not statistically significant, the global results of Y-BOCS were lower.
Thus, we observed a discrepancy between self-related and psychotherapist-related evaluations on the Y-BOCS, especially for the sub-dimension of compulsions. A similar result was highlighted by Hauschildt et al. (98). In that study, patients rated their own symptoms as less severe than their psychotherapists did, and the disagreement was stronger for obsessions and during the pre-assessment. These results could be linked to the inferior awareness that is typical in the early treatment stages, in which a patient does not really know the impact of the symptomatology.
These data have clinical relevance for OCD treatment. Despite the limited number of patients that did not allow us to conduct parametric statistical analyses, the results highlight how CBT procedure treatment (67) ensures a positive outcome. Although our results are not always statistically significant, the data that emerge are important from a clinical point of view and is in line with our clinical and research objectives, namely those of replicating the application of the OCD protocol and verifying the effectiveness of clinical practice.
In accordance with the naturalistic study of Mancini et al. (67) it is important to highlight in this study that patients undergoing CBT procedure treatment (67, 69) had some benefits despite the difficult period they were all enduring that could have contributed to worsening of the symptomatology, increase refusal of therapy or drop out.
It is important to point out that CBT associated with ERP is the gold standard of treatment for OCD (58). It has been proved that CBT with ERP is more functional than cognitive therapy and cognitive behavioral therapy, especially in the individual setting (60, 99, 100). As shown, patients undergoing CBT protocol treatment (67, 69) had some benefits despite the difficult period they were all enduring that could contribute to worsening of the symptomatology.
Despite our study bringing interesting results, our conclusions should be considered with caution, keeping in mind some important limitations. Firstly, our sample sizes for analyses were small; secondly, it was not possible to carry out parametric statistical analyses; and thirdly, no blinded heterodirect evaluation was conducted by other clinicians.
Moreover, we did not evaluate the presence of possible variables that could have moderated the symptomatology in positive terms. For example, being at home and had fewer opportunities to expose oneself to activating trigger.
Our modest purpose was to monitor the symptomatic status of patients with OCD during the COVID-19 pandemic. Such a stressful period could have led to an exacerbation of obsessions and compulsions, and this made it necessary to obtain clinical data to use to build effective treatments.
Despite the small sample and the low statistical power of analysis, it is important to observe that our study used clinical data in two different monitoring periods and a specific intervention procedure. Our observational results highlight a global improvement in the symptomatology. These results were obtained using classic self-report measures for OCD and Y-BOCS, considered the gold standard for OCD assessment. In conclusion, it seems to us that a protocol that combines procedures with proven efficacy with interventions that emphasize the theme of acceptance of specific emotional and cognitive states, compared to treatment with ERP alone, produces greater normalization of symptoms and an improvement. We argue that interventions that target specific cognitive structures, ERP used as an intervention that facilitates acceptance of the risk of being guilty of irresponsibility, and increasing collaboration in the treatment have an effect on reducing OCD vulnerability. This highlights the importance of the specific procedure intervention to replicate the results obtained from empirical research, and is useful for clinicians to give clear effective indications for the treatment of OCD.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval was not provided for this study on human participants because all the subjects who were recruited signed the informed consent for any follow-up, collection, and publication of data for scientific purposes before undertaking the treatment, through documentation provided by the cognitive psychotherapy center in Rome. The study in question is an observational study. The request for publication of the data was submitted to the ethics committee. The patients/participants provided their written informed consent to participate in this study.
VZ, AG, and GF devised the procedure and carried out data collection. VZ wrote the manuscript with support from TC, MD'A, AM, and VP who analyzed the data. GF contributed to sample preparation. FM conceived the original idea and supervised the project. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
This research was supported from School of Cognitive Psychotherapy, Rome, Italy. We thank the psychotherapists who contributed to the data collection: Katia Tenore, Barbara Basile, Stefania Fadda, Teresa Cosentino, Mauro Giacomantonio, and Silvia Timitilli. This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
1. Velotti P, Civilla C, Rogier G, Beomonte Zobel S. A fear of COVID-19 and PTSD symptoms in pathological personality: the mediating effect of dissociation and emotion dysregulation. Front Psychiatry. (2021) 12:590021. doi: 10.3389/fpsyt.2021.590021
2. Velotti P, Rogier G, Beomonte Zobel S, Castellano R, Tambelli R. Loneliness, emotion dysregulation and internalizing symptoms during Covid-19: a structural equation modeling approach. Front Psychiatry. (2021) 11:581494. doi: 10.3389/fpsyt.2020.581494
3. Rogier G, Beomonte Zobel S, Velotti P. Covid-19 and technological addiction: the role of loneliness. J Gambl Issues. (2021) (in press).
4. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
5. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
6. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM. (2020) 113:311–2. doi: 10.1093/qjmed/hcaa,110
7. Giallonardo V, Sampogna G, Del Vecchio V, Luciano M, Albert U, Carmassi C, et al. The impact of quarantine and physical distancing following COVID-19 on mental health: study protocol of a multicentric Italian population trial. Front Psychiatry. (2020) 11:533. doi: 10.3389/fpsyt.2020.00533
8. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
9. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
10. Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. (2020) 113:531–7. doi: 10.1093/qjmed/hcaa201
11. Sugaya N, Yamamoto T, Suzuki N, Uchiumi C. A real-time survey on the psychological impact of mild lockdown for COVID-19 in the Japanese population. Sci Data. (2020) 7:372. doi: 10.1038/s41597-020-00714-9
12. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
13. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
14. Yamamoto T, Uchiumi C, Suzuki N, Yoshimoto J, Murillo-Rodriguez E. The psychological impact of ‘mild lockdown' in Japan during the COVID-19 pandemic: a nationwide survey under a declared state of emergency. Int J Environ Res Public Health. (2020) 17:9382. doi: 10.3390/ijerph17249382
15. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
16. Clemens V, Deschamps P, Fegert JM, Anagnostopoulos D, Bailey S, Doyle M, et al. Potential effects of “social” distancing measures and school lockdown on child and adolescent mental health. Eur Child Adolesc Psychiatry. (2020) 29:739–42. doi: 10.1007/s00787-020-01549-w
17. Gindt M, Fernandez A, Richez A, Nachon O, Battista M, Askenazy F, et al. CoCo20 protocol: a pilot longitudinal follow-up study about the psychiatric outcomes in a paediatric population and their families during and after the stay-at-home related to coronavirus pandemic (COVID-19). BMJ. (2021) 11:e044667. doi: 10.1136/bmjopen-2020-044667
18. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. (2020) 174:819–20. doi: 10.1001/jamapediatrics.2020.1456
19. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adoles Health. (2020) 4:421. doi: 10.1016/S2352-4642(20)30109-7
20. Liu CH, Stevens C, Conrad RC, Hahm HC. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among US young adults with suspected and reported psychiatric diagnoses. Psychiatry Res. (2020) 292:113345. doi: 10.1016/j.psychres.2020.113345
21. Asmundson GJG, Paluszek MM, Landry CA, Rachor GS, McKay D, Taylor S. Do pre-existin anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J Anxiety Disord. (2020) 74:102271. doi: 10.1016/j.janxdis.2020.102271
22. Haider II, Tiwana F, Tahir SM. Impact of the COVID-19 pandemic on adult mental health. Pak J Med Sci. (2020) 36:S90–4. doi: 10.12669/pjms.36.COVID19-S4.2756
23. Plunkett R, Costello S, McGovern M, McDonald C, Hallahan B. Impact of the COVID-19 pandemic on patients with pre-existing anxiety disorders attending secondary care. Ir J Psychol Med. (2020) 8:1–9. doi: 10.1017/ipm.2021.32
24. Sergeant A, van Reekum EA, Sanger N, Dufort A, Rosic T, Sanger S, et al. Impact of COVID-19 and other pandemics and epidemics on people with pre-existing mental disorders: a systematic review protocol and suggestions for clinical care. BMJ Open. (2020) 10:e040229. doi: 10.1136/bmjopen-2020-040229
25. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. (2020) 16:57. doi: 10.1186/s12992-020-00589-w
26. Sher L. Psychiatric disorders and suicide in the COVID-19 era. QJM. (2020) 113:527–8. doi: 10.1093/qjmed/hcaa204
27. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
28. Helbig-Lang S, Peterman F. Tolerate or eliminate? A systematic review on the effects of safety behavior across anxiety disorders. Clin Psychol. (2010) 17:218–33. doi: 10.1111/j.1468-2850.2010.01213.x
29. Salkovskis PM, Clark DM, Hackmann A, Wells A, Gelder MG. An experimental investigation of the role of safety-seeking behaviors in the maintenance of panic disorder with agoraphobia. Behav Res Ther. (1999) 37:559–74. doi: 10.1016/S0005-7967(98)00153-3
30. Sulaimani MF, Bagadood NH. Implication of coronavirus pandemic on obsessive-compulsive-disorder symptoms. Rev Environ Health. (2021) 36:1–8. doi: 10.1515/reveh-2020-0054
31. Zaccari V, D'Arienzo MC, Caiazzo T, Magno A, Amico G, Mancini F. Narrative Review of COVID-19 impact on obsessive-compulsive disorder in child, adolescent, and adult clinical populations. Front Psychiatry. (2021) 12:575. doi: 10.3389/fpsyt.2021.673161
32. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. (2020) 52:102066. doi: 10.1016/j.ajp.2020.102066
33. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
34. Oosterhoff B, Palmer CA. Attitudes and psychological factors associated with news monitoring, social distancing, disinfecting, and hoarding behaviors among US adolescents during the coronavirus disease 2019 pandemic. JAMA Pediat. (2020) 174:1184–90. doi: 10.1001/jamapediatrics.2020.1876
35. Shojaei SF, Masoumi R. The importance of mental health training for psychologists in COVID-19 outbreak. Mid East J Rehabil Health Stud. (2020) 7:e102846. doi: 10.5812/mejrh.102846
36. Salkovskis PM, Forrester E. Responsibility. In: Frost RO, Steketee G, editors. Cognitive Approaches to Obsessions and Compulsions: Theory, Assessment, and Treatment. Pergamon: Elsevier Science Inc. (2002). p. 45–61. doi: 10.1016/B978-008043410-0/50005-2
37. Salkovskis PM, Wroe AL, Gledhill A, Morrison N, Forrester E, Richards C, et al. Responsibility attitudes and interpretations are characteristic of obsessive-compulsive disorder. Behav Res Ther. (2000) 38:347–72. doi: 10.1016/S0005-7967(99)00071-6
38. Shafran R. The manipulation of responsibility in obsessive-compulsive disorder. Br J Clin Psychol. (1997) 36:397–407. doi: 10.1111/j.2044-8260.1997.tb01247.x
39. Tallis F. Obsessions, responsibility and guilt: two case reports suggesting a common and specific aetiology. Behav Res Ther. (1994) 32:143–5. doi: 10.1016/0005-7967(94)90096-5
40. Johnson-Laird PN, Mancini F, Gangemi A. A hyper-emotion theory of psychological illnesses. Psychol Rev. (2006) 113:822. doi: 10.1037/0033-295X.113.4.822
41. Mancini F, D'Olimpio F, Cieri L. Manipulation of responsibility in non-clinical subjects: does expectation of failure exacerbate obsessive–compulsive behaviors? Behav Res Ther. (2004) 42:449–57. doi: 10.1016/S0005-7967(03)00153-0
42. Mancini F, Gangemi A, Johnson-Laird PN. Il ruolo del ragionamento nella psicopatologia secondo la Hyper Emotion Theory. Giornale Ital Psicol. (2007) 4:763–94. doi: 10.1421/25829
43. Mancini F, Rogier G, Gangemi A. The distinction between altruistic and deontological guilt feelings: Insights from psychopathology. In: Cardella PV, Gangemi A, editors. Psychopathology and Philosophy of Mind?: What Mental Disorders Can Tell Us About Our Minds. Routledge (2021). p. 75–95.
44. D'Olimpio F, Mancini F. Role of deontological guilt in obsessive-compulsive disorder–like checking and washing behaviors. Clin Psychol Sci. (2014) 2:727–39. doi: 10.1177/2167702614529549
45. De Jong PJ, Haenen M, Schmidt A, Mayer B. Hypochondriasis: the role of fear-confirming reasoning. Behav Res Ther. (1998) 36:65–74. doi: 10.1016/S0005-7967(97)10009-2
46. Gilbert P. The evolved basis and adaptive functions of cognitive distortions. Br J Med Psychol. (1998) 71:447–63. doi: 10.1111/j.2044-8341.1998.tb01002.x
47. Mancini F, Gangemi A. Fear of guilt from behaving irresponsibly in obsessive–compulsive disorder. J Behav Ther Exp Psychiatry. (2004) 35:109–20. doi: 10.1016/j.jbtep.2004.04.003
48. Mancini F, Gangemi A. Deontological guilt and obsessive-compulsive disorder. J Behav Ther Exp Psychiatry. (2015) 49:157–63. doi: 10.1016/j.jbtep.2015.05.003
50. Mancini F, Gragnani A. L'esposizione con prevenzione della risposta come pratica dell'accettazione. Cognitivismo Clinico. (2005) 2:38–58.
51. Benatti B, Albert U, Maina G, Fiorillo A, Celebre L, Girone N, et al. What happened to patients with obsessive compulsive disorder during the COVID-19 pandemic? A multicentre report from tertiary clinics in northern Italy. Front Psychiatry. (2020) 11:720. doi: 10.3389/fpsyt.2020.00720
52. Jelinek L, Moritz S, Miegel F, Voderholzer U. Obsessive-compulsive disorder during COVID-19: turning a problem into an opportunity? J Anxiety Disord. (2021) 77:102329. doi: 10.1016/j.janxdis.2020.102329
53. Prestia D, Pozza A, Olcese M, Escelsior A, Dettore D, Amore M. The impact of the COVID-19 pandemic on patients with OCD: effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatr Res. (2020) 291:113213. doi: 10.1016/j.psychres.2020.113213
54. Storch EA, Sheu JC, Guzick AG, Schneider SC, Cepeda SL, Rombado BR, et al. Impact of the COVID-19 pandemic on exposure and response prevention outcomes in adults and youth with obsessive-compulsive disorder. Psychiatr Res. (2021) 295:13597. doi: 10.1016/j.psychres.2020.113597
55. Chakraborty A, Karmakar S. Impact of COVID-19 on obsessive compulsive disorder (OCD). Ir J Psychiatry. (2020) 15:256. doi: 10.18502/ijps.v15i3.3820
56. Pan KY, Kok AA, Eikelenboom M, Horsfall M, Jörg F, Luteijn RA, et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. (2021) 8:121–9. doi: 10.1016/S2215-0366(20)30491-0
57. Kuckertz JM, Van Kirk N, Alperovitz D, Nota JA, Falkenstein MJ, Schreck M, et al. Ahead of the curve: responses from patients in treatment for obsessive-compulsive disorder to coronavirus disease 2019. Front Psychol. (2020) 11:572153. doi: 10.3389/fpsyg.2020.572153
58. National Institute for Health and Clinical Excellence: Obsessive Compulsive Disorder: Core Interventions in the Treatment of Obsessive-Compulsive Disorder and Body Dysmorphic Disorder [NICE Guideline]. Clinical guideline No. 31. London: National Institute for Health and Clinical Excellence (2005).
59. Hofmann SG, Asnaani A, Vonk IJJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. (2012) 36:427–40. doi: 10.1007/s10608-012-9476-1
60. Knopp J, Knowles S, Bee P, Lovell K, Bower P. A systematic review of predictors and moderators of response to psychological therapies in OCD: do we have enough empirical evidence to target treatment? Clin Psychol Rev. (2013) 33:1067–81. doi: 10.1016/j.cpr.2013.08.008
61. Öst LG, Havnen A, Hansen B, Kvale G. Cognitive behavioral treatments of obsessive-compulsive disorder: a systematic review and meta-analysis of studes published 1993-2014. Clin Psychol Rev. (2015) 40:156–69. doi: 10.1016/j.cpr.2015.06.003
62. Rosa-Alcázar AI, Sánchez-Meca J, Rosa-Alcázar Á, Iniesta-Sepúlveda M, Olivares-Rodríguez J, Parada-Navas JL. Psychological treatment of obsessive-compulsive disorder in children and adolescents: a meta-analysis. Span J Psychol. (2015) 18:E20. doi: 10.1017/sjp.2015.22
63. Lopez-Pina JA, Sánchez-Meca J, López-López JA, Marín-Martínez F, Núñez-Núñez RM, Rosa-Alcázar AI, et al. The Yale–Brown Obsessive Compulsive Scale: a reliability generalization meta-analysis. Assessment. (2015) 22:619–28. doi: 10.1177/1073191114551954
64. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
65. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5® Disorders - Clinician Version. Columbia, MD: APA Publishing (2015).
66. Storch EA, De Nadai AS, do Rosário MC, Shavitt RG, Torres AR, Ferrão YA, et al. Defining clinical severity in adults with obsessive– compulsive disorder. Compr. Psychiatry. (2015) 63:30–5. doi: 10.1016/j.comppsych.2015.08.007
67. Mancini F, Barcaccia B, Capo R, Gangemi A, Gragnani A, Perdighe C, et al. Trattamento cognitivo-comportamentale nel Disturbo Ossessivo-Compulsivo: risultati di uno studio di esito naturalistico in aperto con follow-up a 6, 12 e 24 mesi. Riv Psichiatr. (2006) 41:99–106. doi: 10.1708/129.1406
68. Mancini F. Il Disturbo Ossessivo-Compulsivo. Il manuale di terapia cognitiva. Torino: Bollati Boringhieri (2005).
69. Mancini F editor. The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder. New York: Routledge (2019). doi: 10.4324/9780429452956
70. Perdighe C, Gragnani A. editors. Psicoterapia cognitiva. Comprendere e curare i disturbi mentali. Milano: Raffaello Cortina Editore (2021).
71. Spera P, Mancini F editors. Affrontare il disturbo ossessivo compulsivo: quaderno di lavoro. Roma: Franco Angeli (2021).
72. Van Oppen P, Arntz A. Cognitive therapy for obsessive-compulsive disorder. Behav Res Ther. (1994) 32:79–87. doi: 10.1016/0005-7967(94)90086-8
73. Wells A. Cognitive Therapy of Anxiety Disorders. A Practice Manual and Conceptual Guide. Vol. 12. Hoboken NJ: John Wiley and Sons. (1997). p. 350–3. doi: 10.1891/0889-8391.12.4.350
74. Vos SPF, Huibers MJH, Arntz A. Experimental investigation of targeting responsibility versus danger in cognitive therapy of obsessive-compulsive disorder. Depress Anxiety. (2012) 29:629–37. doi: 10.1002/da.21915
75. Gragnani A, Buonanno C, Saettoni M. Techniques of cognitive restructuring. In: Mancini F, editor. The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder. New York: Routledge (2019). p. 180–200. doi: 10.4324/9780429452956-10
76. Gangemi A, Tenore K, Mancini F. Two reasoning strategies in patients with psychological illnesses. Front Psychol. (2019) 10:2335. doi: 10.3389/fpsyg.2019.02335
77. Perdighe C, Gragnani A, Rainone A. Accepting risk: cognitive techniques. In: Mancini F, editor. The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder. New York: Routledge (2019). p. 221–49. doi: 10.4324/9780429452956-12
78. Abramowitz JS. Understanding and Treating Obsessive-Compulsive Disorder: A Cognitive Behavioral Approach. New York: Lawrence Erlbaum Associates Inc. (2006). doi: 10.4324/9781410615718
79. Foa EB, Yadin E, Lichner TK. Exposure and Response (Ritual) Prevention for Obsessive-Compulsive Disorder. 2nd ed. New York: OUP (2012). doi: 10.1093/med:psych/9780195335286.001.0001
80. Luppino OI, Pontillo M. Exposure with response prevention as a practice of acceptance. In: Mancini F, editor. The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder. New York: Routledge (2019). p. 250–74. doi: 10.4324/9780429452956-13
81. Chiang B, Purdon C, Radomsky AS. Development and initial validation of the fear of guilt scale for obsessive-compulsive disorder (OCD). J Obsessive Compuls Relat Disord. (2016) 11:63–73. doi: 10.1016/j.jocrd.2016.08.006
82. Cosentino T, Saliani AM, Perdighe C, Romano G, Mancini F. Intervention to reduce current vulnerability to obessesive-compulsive disorder. In: Mancini F, editor. The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder. New York: Routledge (2019). p. 297–309. doi: 10.4324/9780429452956-15
83. Basile B, De Sanctis B, Fadda S, Luppino OI, Perdighe C, Saliani AM, et al. Early life experiences in ocd and other disorders: a retrospective observational study using imagery with re-scripting. Clin Neuropsychiatry. (2018) 15:299–05.
84. Luppino OI, Tenore K, Mancini F, Basile B. A theoretical integration of schema therapy and cognitive therapy in OCD treatment: goals and beliefs of the obsessive mind (part I). Psychology. (2018) 9:2261–77. doi: 10.4236/psych.2018.99129
85. Tenore K, Basile B, Cosentino T, De Sanctis B, Fadda S, Femia G, et al. Imagery rescripting on guilt-inducing memories in OCD: a single case series study. Front Psychiatry. (2020) 11:543806. doi: 10.3389/fpsyt.2020.543806
86. Tenore K, Gragnani A. Intervention on historical vulnerability. In: Mancini F, editor. The Obsessive Mind: Understanding and Treating Obsessive-Compulsive Disorder. New York: Routledge (2019). p. 310–22. doi: 10.4324/9780429452956-16
87. Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The obsessive-compulsive inventory: development and validation of a short version. Psychol Assess. (2002) 14:485–96. doi: 10.1037/1040-3590.14.4.485
88. Huppert JD, Walther MR, Hajcak G, Yadin E, Foa EB, Simpson HB, et al. The OCI-R: validation of the subscales in a clinical sample. J Anxiety Disord. (2007) 21:394–406. doi: 10.1016/j.janxdis.2006.05.006
89. Sica C, Ghisi M, Altoè G, Chiri LR, Franceschini S, Coradeschi D, et al. The Italian version of the Obsessive Compulsive Inventory: its psychometric properties on community and clinical samples. J Anxiety Disord. (2009) 23:204–11. doi: 10.1016/j.janxdis.2008.07.001
90. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL. The Yale–Brown Obsessive Compulsive Scale I. Development, use, and reliability. Arch Gen Psychiatry. (1989) 46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007
91. Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale–Brown Obsessive Compulsive Scale II: validity. Arch Gen Psychiatry. (1989) 46:1012–16. doi: 10.1001/archpsyc.1989.01810110054008
92. Hénin M. Yale-brown obsessive-compulsive scale. In: Sica C, editor. Disturbo Ossessivo- Compulsivo. Questionari e Interviste per la Valutazione Clinica. Trento: Erickson (2012).
94. Melli G, Avallone E, Moulding R, Pinto A, Micheli E, Carraresi C. Validation of the Italian version of the Yale–Brown Obsessive Compulsive Scale–Second Edition (Y-BOCS-II) in a clinical sample. Compr Psychiatry. (2015) 60:86–92. doi: 10.1016/j.comppsych.2015.03.005
95. Derogatis LR. SCL-90-R: Administration, Scoring, Procedures Manual II for the Revised Version and Other Instruments of the Psychopathology Rating Scale Series. Minneapolis, MN: National Computer Systems (1994).
96. Prunas A, Sarno I, Preti E, Madeddu F, Perugini M. Psychometric Properties of the Italian Version of the SCL-90-R: A Study on a Large Community Sample. Cambridge University Press (2011). doi: 10.1016/j.eurpsy.2010.12.006
97. Schwartz-Lifshitz M, Basel D, Lang C, Hertz-Palmor N, Dekel I, Zohar J, et al. Obsessive compulsive symptoms severity among children and adolescents during COVID-19 first wave in Israel? J Obsess Compuls Relat Disord. (2021) 28:100610. doi: 10.1016/j.jocrd.2020.100610
98. Hauschildt M, Dar R, Schröder J, Moritz S. Congruence and discrepancy between self-rated and clinician-rated symptom severity on the Yale–Brown Obsessive-Compulsive Scale (Y-BOCS) before and after a low-intensity intervention. Psychiatry Res. (2019) 273:595–602. doi: 10.1016/j.psychres.2019.01.092
99. Mancini F, Rogier G. Le linee guida per il trattamento psicologico del disturbo ossessivo compulsivo. Cognitivismo Clinico. (2020) 17:234–50.
Keywords: COVID-19, obsessive-compulsive disorder (OCD), obsessive-compulsive symptoms, cognitive behavioral therapy (CBT), Y-BOCS, adults
Citation: Zaccari V, Gragnani A, Pellegrini V, Caiazzo T, D'Arienzo MC, Magno A, Femia G and Mancini F (2021) An Observational Study of OCD Patients Treated With Cognitive Behavioral Therapy During the COVID-19 Pandemic. Front. Psychiatry 12:755744. doi: 10.3389/fpsyt.2021.755744
Received: 09 August 2021; Accepted: 23 September 2021;
Published: 22 October 2021.
Edited by:
Ana Isabel Rosa-Alcázar, University of Murcia, SpainReviewed by:
Mª Dolores García-Hernández, University of Murcia, SpainCopyright © 2021 Zaccari, Gragnani, Pellegrini, Caiazzo, D'Arienzo, Magno, Femia and Mancini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vittoria Zaccari, di56YWNjYXJpQHVuaW1hcmNvbmkuaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.