- 1Department of Psychosomatic Medicine and Psychotherapy, University Hospital Tübingen, Tübingen, Germany
- 2Health Department Freudenstadt, Freudenstadt, Germany
- 3Charité Center for Internal Medicine and Dermatology, Department for Psychosomatic Medicine, Charité-Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
Objective: The SARS-CoV-2 pandemic has led to pronounced health changes, especially for those infected and psychologically burdened. This cross-sectional study examined the stress experience and coping strategies during home isolation of SARS-CoV-2 infected individuals and analyzed differences regarding psychological burden.
Methods: SARS-CoV-2 infected respondents were recruited by telephone and completed an online survey during their home isolation. This questionnaire assessed sociodemographic aspects, somatic factors, psychological burden (depressive symptoms, anxiety, and somatic symptom disorder), perceived stress and coping behavior during the home isolation.
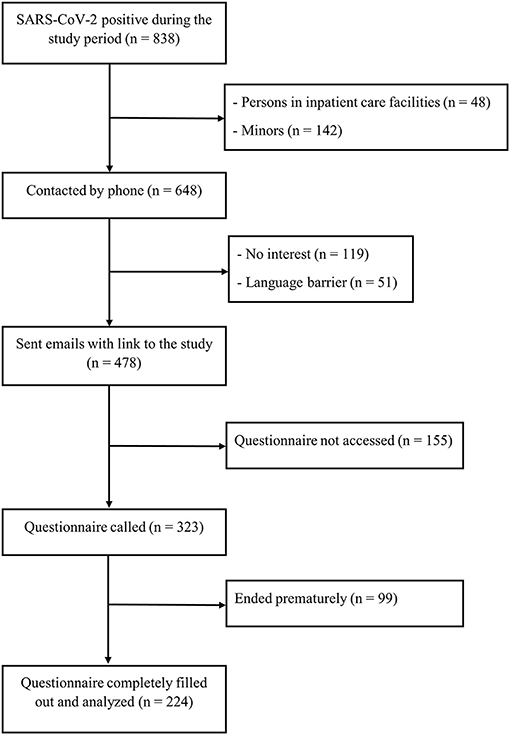
Results: Out of 838 SARS-CoV-2 infected individuals during the study period, 648 were contacted and 224 home-isolated respondents were included in the study. Disgrace, social restrictions, job fear, health concerns, and infectiousness could be explored as stressors during the home isolation. Fifty-four percent experienced psychological burden. SARS-CoV-2 infected and home-isolated individuals with psychological burden perceived significant stressors more strongly (p < 0.001, r = 0.5) and coped significantly less (p < 0.001, r = 0.3) with their infection and home isolation compared to SARS-CoV-2 infected individuals without psychological burden.
Conclusion: SARS-CoV-2 infected individuals with psychological burden experienced higher stressors and were unable to cope adaptively with home isolation. Therefore, a general and standardized screening procedure for psychological burden should be established. SARS-CoV-2 infected individuals with psychological burden should receive targeted support with professional help in the areas of stress experience and coping skills during their home isolation and beyond to avoid long-term consequences.
Introduction
Since the World Health Organization (WHO) declared the impact of the SARS-CoV-2 virus on humanity a pandemic of international scope on March 11th 2020 (1), major health-related changes have occurred worldwide. Media reports and policy decisions have concentrated on the daily case numbers of SARS-CoV-2-confirmed cases (over 230 million) and SARS-CoV-2 deceased (over 4.8 million) (2). SARS-CoV-2 infection is now a common disease. In a German study on patients (n = 301,290) with SARS-CoV-2 associated symptoms in general practices, the prevalence of SARS-CoV-2 infection was 13.8% (3).
The infected are those who, on the one hand, experience the health threat most acutely and, on the other hand, are most urgently exposed to the harshest countermeasures in the fight against the pandemic. The key element of global pandemic response is to break chains of infection (“flatten the curve”). In Germany, the public health institute (Robert Koch Institute) develops the national guidelines for the work of the individual health authorities. Infected persons must be isolated for at least 14 days from the onset of symptoms or from the date of testing positive. Isolation is the separation of confirmed infected persons. This definition differs from the concept of quarantine, which is the separation of contact persons who are suspected of being infected because they had contact with confirmed infected persons. The situations between quarantine and isolation differ significantly (4). For example, infected persons are exposed to different stressors (such as the great concern of having infected others) than their contacts, who are confronted with the uncertainty of whether they will still become ill. However, infected individuals and their contacts are not allowed to leave their homes during separation except for SARS-CoV-2 swabs and in emergencies. It is also recommended that they separate themselves from their own household members. In Germany, this containment strategy is coordinated by the local district health offices.
Meanwhile, many studies have dealt with the psychological burden due to SARS-CoV-2 infection. In a meta-analysis of 22 studies (n = 4,318), 38% of SARS-CoV-2 infected persons had depression and an equal number had anxiety (by reaching an appropriate cut-off value of screening questionnaires) (5). Pre-existing mental illness is associated with increased psychological burden due to SARS-CoV-2 infection (6). A cross-sectional study on hospitalized patients (n = 281) showed that patients with psychiatric disorder were vulnerable to the development of anxiety symptoms during their SARS-CoV-2 infection (6). Further, a small study (n = 30) on hospitalized SARS-CoV-2 infected patients suggested that increased anxiety and depression are associated with worse, or even more lethal outcomes (7).
Not only the SARS-CoV-2 infection itself, but also the isolation procedure triggers psychological burden. A current study from Bangladesh (n = 5,792) found a very high prevalence of depression (85.9%) among SARS-CoV-2 infected persons in isolation (8). Since now, the focus of the SARS-CoV-2 isolation studies has been on prevalence assessment of psychological burden among persons with a SARS-CoV-2 infection. However, to adequately support infected people in isolation, a deep understanding of the stressors and coping mechanism during the isolation is very important and still missing. Only few studies have evaluated stressors during separation measures of previous epidemics. They showed stressors like boredom and lack of self-control (9–13). There is only one study (n = 64) that has assessed the stressors of separation measures through SARS-CoV-2 isolation or quarantine in the setting at home (14). Qualitative interviews explored various stigmatization processes that led to impaired quality of life. Coping as the ability to manage stressful situations is a very important skill to overcome challenging situations as pandemics. Only three studies (n = 66, 84, and 100) have addressed the coping strategies of SARS-CoV-2 infected and hospitalized patients (15–17). The patients coped for example with positive reframing, emotional support, and communication with their families (15–17).
Essential points for understanding the isolation of SARS-CoV-2 infected persons are still unexplored. This particularly concerns the isolation at home. Most studies that have addressed stress and coping in SARS-CoV-2 isolation have looked at the situation of hospitalized patients (15–17). However, most SARS-CoV-2 infected persons spend their isolation at home. At home, the overall situation is very different compared to the hospitalized isolation. There is no around-the-clock medical care at home, no predefined daily structure, no symptom management etc. that might support adaptive coping in infected patients. Instead, SARS-CoV-2 infected individuals in isolation live in constant fear of infecting their household members due to inadequate isolation options and are left to cope with isolation on their own. Furthermore, isolation of infected individuals differs from quarantine of contact persons in many ways. The previous study on isolation at home did not consider this separately (14), although stress experience and coping strategies certainly differ significantly between isolation and quarantine. In summary, there is no data yet that examines the impact of isolation at home on mental health in people infected with SARS-CoV-2. However, this is important to develop care concepts with the aim to enhance coping strategies despite their home isolation and managing a SARS-CoV-2 infection. This is the first cross-sectional study of SARS-CoV-2 infected individuals that evaluates [1] the experienced psychological burden and stressors in home isolation, [2] the coping strategies during home isolation, and [3] the differences in stress experience and coping behavior regarding psychological burden. We tested the hypothesis that psychological burden is high during home isolation and that psychologically burdened individuals experience increased stress associated with lower coping strategies.
Materials and Methods
Study Design and Recruitment
The study population consists of SARS-CoV-2 infected and home isolated persons within the jurisdiction of the Freudenstadt Health Department (Germany). All infected persons had at least one positive SARS-CoV-2 PCR result at the time of the survey. The survey was conducted between January 29th and April 12th 2021. During this period, all infected persons whose positive PCR result was received by the Freudenstadt Health Department by March 31th 2021 at the latest were contacted by telephone during their first days of home isolation (n = 838).
During the phone call, patients were screened if they were cognitively able to participate in the study. The screening procedure was conducted with general questions regarding to the situation and person. If people expressed interest in the anonymous investigation, an email was sent directly after the phone call (n = 478) with further information about the study and with an invitation link to the online survey (EFS Survey) (18).
Patients completed the survey while still being in their home isolation. To prevent multiple completion, repeated access via the same IP address was blocked. All participants who did not finish the questionnaire were excluded (n = 99, from which 80.8% quit at the very beginning). Two hundred and twenty-four SARS-CoV-2 infected and home isolated respondents could be included in the study (see Figure 1). Upon completion of the online survey, all participants received information for further psychological support during the isolation at home.
Procedures/Ethics Statement
At the beginning of the online survey, consent forms were obtained for data protection, data processing and data analysis. Study participation was voluntary and anonymous, took about 40 min, and the questionnaire could be discontinued at any time without negative consequences for the participants. The local ethics committee approved the study (073/2021BO2).
Measures
Demographics, Somatic Parameters, and Subjective Support During Home Isolation
Age, gender, marital status, number of children, number of household members, size of residence, nationality, and highest level of education were assessed. Self-reported SARS-CoV-2 associated symptoms, risk factors for a more severe SARS-CoV-2 course according to the Robert Koch Institute (German public health institute) and the subjective assessment of the current and worst physical condition (0 = not ill at all to 100 = very severely ill) were assessed. Four self-generated items were used to assess subjective support (“How much do you feel supported by your social environment/employer/family doctor/health office during your isolation?”; 0 = no support at all to 100 = full support). Total support score was formed which has an acceptable reliability in the current sample (Cronbach's α = 0.684).
Patient Health Questionnaire
The Patient Health Questionnaire 8 (PHQ-8) originates from the Patient Health Questionnaire (19) and captures the module of depressiveness (20). Depressive symptomatology and depression severity are measured by a retrospective self-assessment of the past 2 weeks using a 4-point Likert scale (0 = not at all to 3 = nearly every day) (21). Clinically significant depressive symptoms can be assumed from a sum score of 10 (range = 0–24) (21). The PHQ-8 showed very good reliability in the current sample (Cronbach's α = 0.858).
Generalized Anxiety Disorder Scale
The Generalized Anxiety Disorder Scale 7 (GAD-7) is also taken from the Patient Health Questionnaire (19) and contains seven items assessing generalized anxiety disorder and general anxiety in a valid and standardized way (22, 23). A 4-point Likert scale screens for frequency of anxiety in the past 2 weeks (24). A sum score of 10 or greater indicates at least moderate anxiety (range = 0–21) (24). The GAD-7 showed very good reliability in the current sample (Cronbach's α = 0.882).
Somatic Symptom Disorder-B Criteria Scale
The Somatic Symptom Disorder-B Criteria Scale questionnaire is used to detect somatic symptom disorders based on DSM in a valid way (25–31). The 12-item questionnaire is divided into cognitive, affective, and behavioral aspects (32). A 5-point Likert scale (0 = never to 5 = very often) is used to assess somatoform disorders. Depending on age and gender, the sum score (range = 0–48) is recategorized into at least medium (80% quantile) psychological distress using a quantile regression based on norm values (32). The SSD-12 exhibited very good reliability in the current sample (Cronbach's α = 0.927).
Perceived Stress Questionnaire
The Perceived Stress Questionnaire (PSQ-20) is a short form of the PSQ-30 and measures the subjective perception, evaluation, and processing of stressors over the last 4 weeks using a 4-point Likert scale (1 = almost never to 4 = most of the time) (33). The items are divided into four scales: worries, tension, joy, and demands (34). The four scales are recoded to a scale rank from 0 to 100 (low to high expression) and after inverting the joy category, a total score was formed. The total score showed very good reliability in the current sample (Cronbach's α = 0.903).
Stress and Coping Inventory
The Stress and Coping Inventory records stress symptoms and various coping strategies (35). In this study, only the independent coping modules positive thinking (e.g., “I tell myself that stress and pressure also have their good sides”), active coping (e.g., “I do everything I can to prevent stress in the first place”), and social support (e.g., “When I get under pressure, I have people to help me”) were recorded (35). The remaining 12 items were recorded using a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree) (35, 36). The SCI showed good to very good reliability regarding all scales in the current sample (range of Cronbach's α: 0.717–0.827).
Specific Stressors Arising From Isolation and SARS-CoV-2 Infection
Sixteen items were created as home isolation- and SARS-CoV-2 infection-specific stressors based on the authors' extensive practical expertise witnessing the experiences of over 5,000 SARS-CoV-2 infected individuals. The items could be intuitively rated using a slider (0 = strongly disagree to 100 = strongly agree). A principal factor analysis with 16 items was performed with the help of an oblique rotation. Sampling adequacy was confirmed with Kaiser–Meyer–Olkin criterion (KMO = 0.773, range of KMO-values for individual items: 0.596–0.911) (37). According to Kaiser's criterion (eigenvalues > 1) (38, 39) and the scree plot, five factors were drawn, covering a total explained variance of 55.3%: disgrace, social restrictions, job fear, health concerns and infectiousness (e.g., “I am worried that the disease will take a severe course in me,” “I feel guilty because I might have infected those around me”). The absolute values of factor loadings were between 0.318 and 0.896 according to oblique rotation. All subscales had good to very good reliabilities in the current sample (range of Cronbach's α: 0.729–0.804). Total score and subscores were formed.
Coping of Isolated SARS-CoV-2 Infected Individuals
Twenty-four items were created by the expert team to assess how isolated SARS-CoV-2 infected people cope with this specific situation (e.g., “with my isolation I do something for society,” “I maintain social contacts”). The questions could be answered intuitively with a slider (0 = do not agree at all to 100 = agree completely). To create suitable subscales/constructs, various methods of exploratory factor analysis were applied. No constellation of factors could be found that appeared to be satisfactorily coherent both statistically and in terms of content. Consequently, a total score of 14 items was formed, which has a very good reliability in the current sample (Cronbach's α = 0.857). The discriminatory power of the individual items was good (range of corrected item-total correlation: 0.385–0.645).
Statistical Analyses
Data were analyzed using SPSS (Version 27). Descriptive statistics, means, standard deviations, frequencies and percentages were examined. 20.1% respondents had at least one missing value. The Little's MCAR test (40) (p = 0.463) and logistic regression estimation (41) with binary coded missing variables as dependent variables (0.063 ≥ p < 1.000) showed that the missing data were subject to a missing completely at random mechanism. The Fully Conditional Specification Method of Multiple Imputation was used to impute the missing values (20 imputations were performed) (42). Normal distribution was tested, and the dataset was found to be not normally distributed, so the Mann–Whitney U-test was used for the significance tests (2-sided, p < 0.05). All respondents who had a somatic symptom disorder or/and depressive symptoms or/and anxiety were grouped together as the category psychological burden. Thus, psychological burden was defined as reaching at least one of the cut-off scores of PHQ-8, GAD-7, or SSD-12. In the significance tests, respondents with psychological burden were always compared to respondents without psychological burden.
Results
Sample Description
Sociodemographic
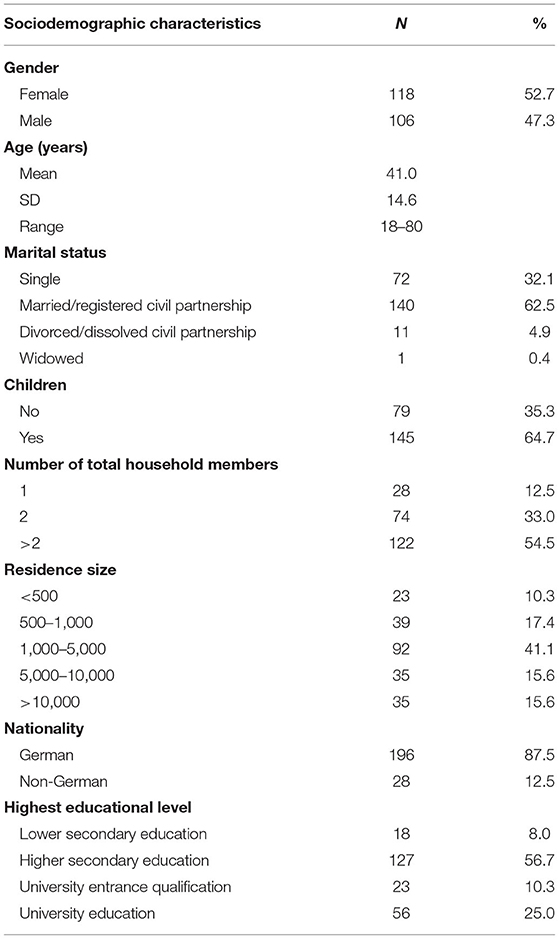
Of the 224 respondents, 52.7% were female and 43.3% were male. The mean age was 41 years (SD = 14.6). Further sociodemographic characteristics are listed in Table 1.
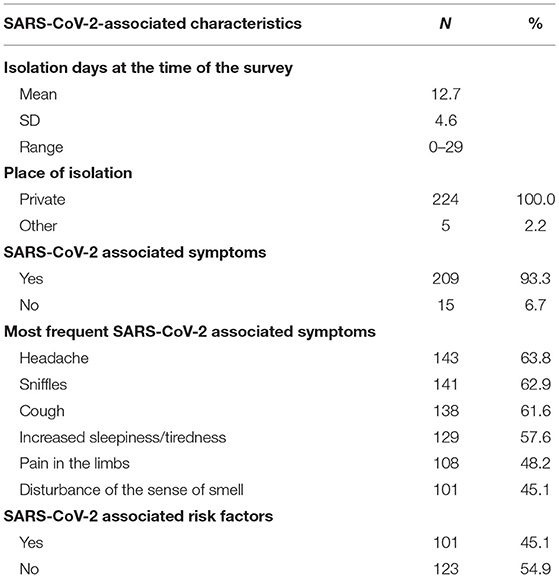
SARS-CoV-2 Associated Characteristics
On average, the survey was completed on the 12th day of isolation. One-hundred percent of the study participants spent their isolation at home (=private isolation). 93.3% of respondents had SARS-CoV-2 symptoms, with a mean of 6.1 symptoms (SD = 3.8, Range = 0–16). 45.1% had at least one SARS-CoV-2 associated risk factor. Additional SARS-CoV-2 associated characteristics can be found in Table 2.
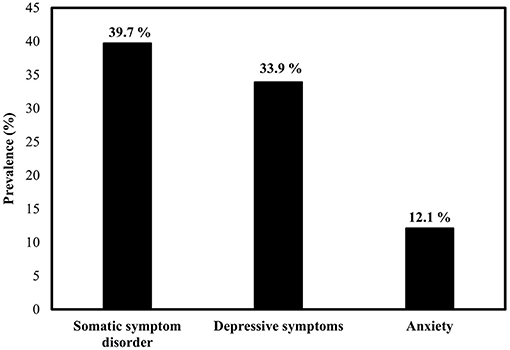
Prevalence of Psychological Burden
Ninety-eight respondents reached the cut-off value for somatic symptom disorder (M = 11.3, SD = 9.2, and Range = 0–41), 76 reached the cut-off value for clinically significant depressive symptoms (M = 7.5, SD = 5.2, and Range = 0–21), and 27 reached the cut-off value for clinically significant anxiety (M = 4.4, SD = 4.4, and Range = 0–21). Thus, 121 respondents were categorized as psychological burden (= respondents with somatic symptom disorder or/and depressive symptoms or/and anxiety, Figure 2).
Differences in Stress Experience Due to Psychological Burden
Different facets of stress experience regarding psychological burden that occurred in the context of home isolation during SARS-CoV-2 infection were investigated (Figure 3).
(1) Perceived stress: SARS-CoV-2 infected individuals with psychological burden (Mdn = 41.7) experienced significantly more perceived stress (higher PSQ-20 score) than respondents without psychological burden (Mdn = 26.7, U = 2,928.0, z = −6.8, p < 0.001, and r = 0.5). Respondents with psychological burden (Mdn = 60.0) experienced significantly higher levels of subjective psychological distress due the SARS-CoV-2 infection than the non-burdened group (Mdn = 24.0, U = 3,131.0, z = −6.4, p < 0.001, and r = 0.4).
(2) Stress due to somatic factors: Respondents with psychological burden reported significantly more SARS-CoV-2 symptoms (Mdn = 7.0) compared to respondents without psychological burden (Mdn = 5.0, U = 4,053.5, z = −4.5, p < 0.001, and r = 0.3). SARS-CoV-2 associated risk factors were significantly more frequent in the psychologically burdened group (Mdn = 1.0) than in the unburdened group (Mdn = 0.0, U = 5,034.0, z = −2.8, p = 0.006, and r = 0.2). The subjective physical health at the time of the survey was significantly worse among participants with psychological burden (Mdn = 26.0) compared to those without psychological burden (Mdn = 10.0, U = 3,514.0, z = −5.6, p < 0.001, and r = 0.4). The severity of disease on the worst day of illness was significantly worse among respondents with psychological burden (Mdn = 61.0) compared to those without psychological burden (Mdn = 40.0, U = 4,161.0, z = −4.3, p < 0.001, and r = 0.3).
(3) Specific stressors arising from SARS-CoV-2 infection and isolation: Respondents with psychological burden (Mdn = 37.3) perceived stressors arising from SARS-CoV-2 infection and isolation significantly more strongly than respondents without psychological burden (Mdn = 17.0, U = 4,362.5, z = −7.4, p < 0.001, and r = 0.5). These differences are reflected in all stressors (disgrace, social restrictions, job fear, health concerns, and infectiousness).
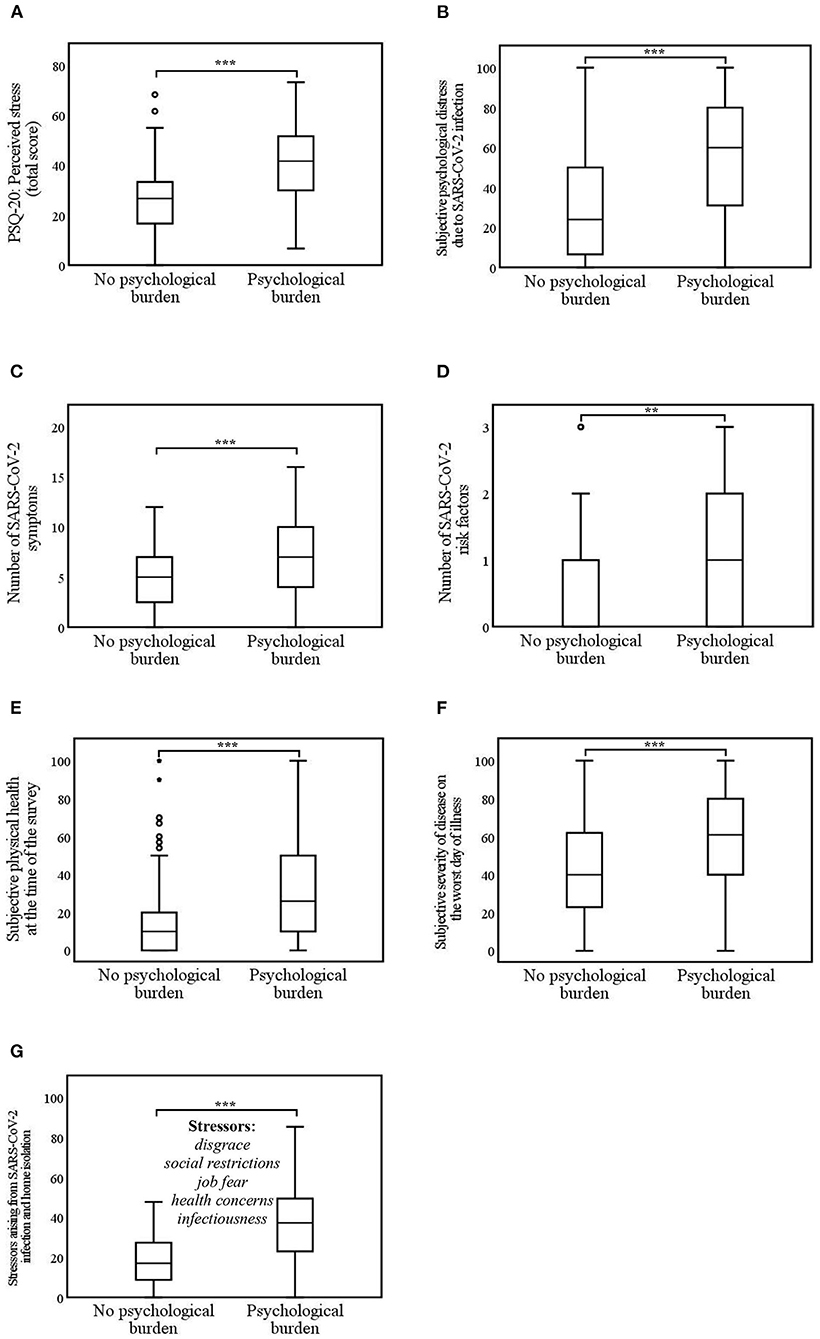
Figure 3. (A–G) Differences in stress experience due to psychological burden during SARS-CoV-2 infection and home isolation. Psychological burden = home-isolated SARS-CoV-2 infected individuals with somatic symptom disorder and/or depressive symptoms and/or anxiety. **p < 0.01; ***p < 0.001. (A) 0 = low perceived stress to 80 = high perceived stress; (B) 0 = very low stress level to 100 = very high stress level; (E,F) 0 = not ill at all to 100 = very severely ill; (G) 0 = not stressed at all to 100 = extremely stressed.
Differences in Coping Strategies Due to Psychological Burden
The differences in coping strategies depending on psychological burden used in the context of home isolation during SARS-CoV-2 infection were investigated next (Figure 4).
(1) Coping strategies in general (SCI): Respondents with psychological burden (Mdn = 10.0) used positive thinking significantly less as coping strategy than respondents without burden (Mdn = 11.0, U = 4,740.5, z = −3.1, p = 0.002, and r = 0.2). The coping strategy social support was used significantly less by the psychologically burdened participants (Mdn = 13.0) compared to the non-burdened participants (Mdn = 15.0, U = 5,038.5, z = −2.5, p = 0.01, and r = 0.2). However, active coping did not differ between the burdened (Mdn = 11.0) and unburdened groups (Mdn = 12.0, U = 5,316.0, z = −1.9, p = 0.06, and r = 0.1).
(2) Subjective support during SARS-CoV-2 infection and isolation: Infected respondents with psychological burden (Mdn = 69.3) felt significantly less supported by social environment, employer, family doctor, and health office (= support total score) than infected persons without psychological burden (Mdn = 82.0, U = 5,000.0, z = −2.5, p = 0.01, and r = 0.2).
(3) Specific strategies for coping with SARS-CoV-2 infection and isolation: Respondents with psychological burden (Mdn = 62.0) used significantly fewer specific coping strategies to overcome the SARS-CoV-2 infection and isolation than the unburdened (Mdn = 71.4, U = 4,362.0, z = −3.9, p < 0.001, and r = 0.3).
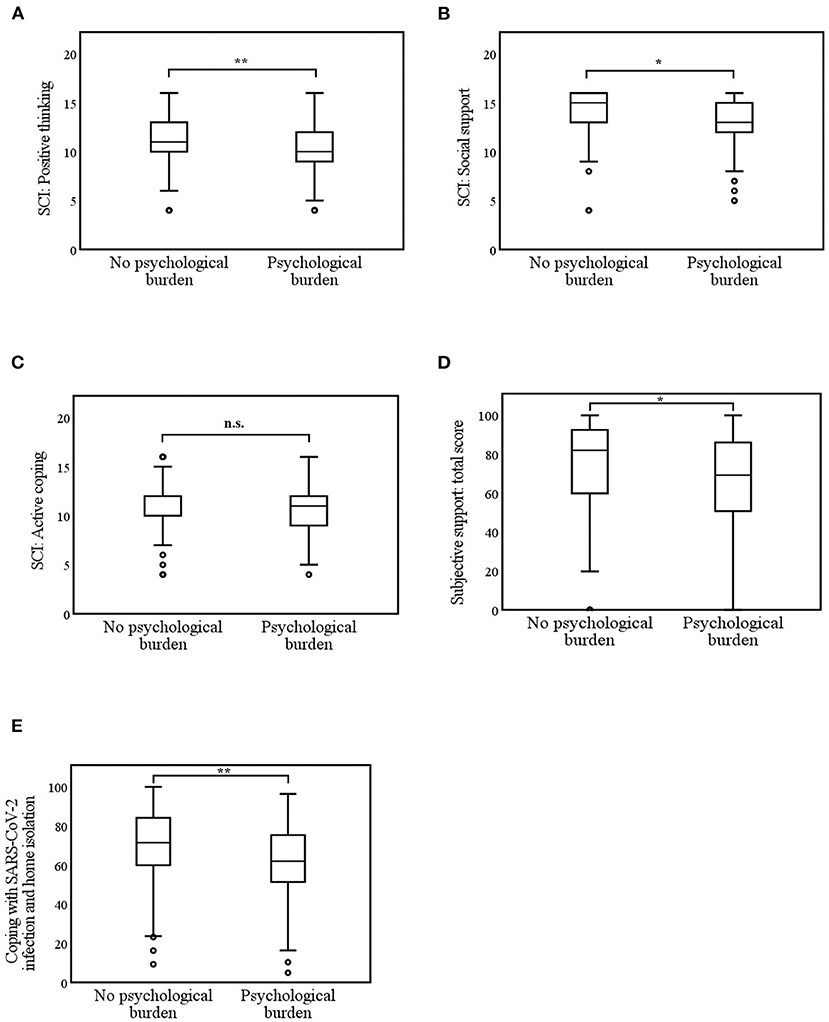
Figure 4. (A–E) Differences in coping strategies due to psychological burden during SARS-CoV-2 infection and home isolation. n.s. (not significant) p > 0.5; *p < 0.05; **p < 0.01; ***p < 0.001. (A–C) 0 = low coping skills to 20 = high coping skills. (D) Subjective support by social environment, employer, family doctor, health office; 0 = no support at all to 100 = full support; (E) 0 = low coping skills to 100 = high coping skills.
Discussion
This is the first cross-sectional study evaluating the stress experience and the coping strategies of SARS-CoV-2 infected individuals during their home isolation and evaluating the differences regarding psychological burden. Disgrace, social restrictions, job fear, health concerns, and infectiousness were identified as stressors in the context of SARS-CoV-2 infection during home isolation. Fifty-four percent of the 224 home isolated SARS-CoV-2 infected respondents showed psychological burden. For the first time it was shown that home isolated and SARS-CoV-2 infected individuals with psychological burden perceived stressors more strongly and coped less with their infection in home isolation.
To capture these differences, screening questionnaires were initially used to screen for psychological burden. 33.9% of home-isolated SARS-CoV-2 infected individuals had a clinically significant depressiveness score, which is close to the pooled prevalence of 38% of a large meta-analysis (n = 4,318) on patients with SARS-CoV-2 (5). 12.1% achieved a high score for anxiety compared with 38% in the meta-analysis, in which anxiety was diagnosed at significantly lower cut-off values (5) likely explaining this difference. 39.7% of the SARS-CoV-2 infected individuals achieved a high somatic symptom disorder score, which is significantly higher than the 5.4% individuals with somatic symptom disorder of the general German population according to a cross-sectional study (n = 2,531) (43). Both SARS-CoV-2 infection and the prolonged pandemic could be risk factors for the development of somatic symptom disorder (44) and could explain the significantly increased prevalence. Thus, more than half (54%) of SARS-CoV-2 infected and home-isolated study participants experienced psychological burden, and overall, this is likely to persist beyond the infection and isolation phase (45, 46).
Our study shows that home isolation in the setting of SARS-CoV-2 infection is associated with the following massive stressors: disgrace, social restrictions, job fear, health concerns, and infectiousness. A qualitative-retrospective study (n = 64) from Finland also reported stigmatization during SARS-CoV-2 domestic isolation, along with boredom as another stressor (14). In the Finish study, boredom was likely reported by potentially non-infected quarantined contacts and did not play a role as a stressor in our study because only infected individuals were included here. During home isolation, separation of family members is often not possible. Thus, feelings of guilt regarding possible infection are pervasive at home compared with the hospital setting. Those isolated at home continue to be very concerned that the disease could take a severe course (14). The great concern about a severe course is triggered by both media reports and the lack of medical care compared to hospitalized isolation. Fear of negative consequences at work was also captured in the present study, highlighting the far-reaching effects of isolation and infection.
Among psychologically burdened individuals, the experience of stress during home isolation differed significantly and with a large effect. All stressors were perceived as more severe. This also applies to the perception of physical symptoms as stressors. Psychologically burdened individuals reported significantly more SARS-CoV-2 associated symptoms and poorer physical health. A similar relationship has already been shown in patients with a mild SARS-CoV-2 course (n = 895) (47). The situation of being infected with SARS-CoV-2 and isolated at home carries a threatening mix of stress that particularly affects those with psychological burden.
We also showed that SARS-CoV-2 infected individuals with psychological burden use significantly fewer coping strategies to overcome their infection and home isolation. Furthermore, they feel significantly less supported by their social environment. However, social support acts as a protective factor against psychological burden from the pandemic in non-infected individuals with preexisting depression, according to a prospective cohort study (n = 1,928) (48). This patient group benefits particularly from external support in the context of the SARS-CoV-2 pandemic (48). In contrast, our study identified that psychologically burdened infected respondents failed to use sufficient adaptive coping strategies, such as maintaining social contacts, adhering to a daily structure, and getting adequate sleep. Adaptive coping strategies also work as a resilience factor (49). Our study reinforces this hypothesis, as patients without psychological burden used significantly more adaptive coping strategies. The use of adaptive coping strategies as a resilience factor could explain why, in the same threatening situation, some people feel psychologically burdened and others do not.
Previous studies on coping strategies of SARS-CoV-2 infected patients have only dealt with hospitalized patients (15–17). Thus, SARS-CoV-2 infected patients (n = 66) showed fewer depressive symptoms when they sought the help of medical staff during mandatory hospital isolation (17). In a qualitative study (n = 100), it was shown that during hospitalized isolation, direct communication with other patients is an important coping strategy (16). However, these are both coping strategies that were not available in the home isolation. Psychologically burdened patients did not manage this sufficiently in the home isolation and thus bear the risk of developing even long-term psychological burden and/or (neuro)psychiatric diseases.
At the time of the study, the neuropsychiatric aspects of SARS-CoV-2 infection had not yet been discussed in the present depth. The questionnaire was based on the symptom list of the Robert Koch Institute at that time (German public health institute). In our study population, neuropsychiatric symptoms (such as headache, increased sleepiness/tiredness, disturbance in the sense of smell) were among the most common symptoms of SARS-CoV-2 infection. A meta-analysis showed that cognitive deficits, sleep disturbances, and fatigue persist beyond acute SARS-CoV-2 infection (50). Post-traumatic stress symptoms are common (45) and originate from the acute infection. Risk factors are the severity of the acute infection, but also psychosomatic aspects, such as anxiety and depression (50). The neuropsychiatric and psychiatric symptoms could in turn lead to an increased stress experience and reduced coping abilities, making it even more difficult to overcome the acute situation. Longitudinal studies are needed to further investigate this relationship.
It may be helpful to consider the SARS-CoV-2 infection in a biopsychosocial context. Biological aspects directly influence psychosocial (long-term) outcome, such as anxiety, depression, and insomnia (51). In our study, this was manifested by the SARS-CoV-2-associated risk factors. These were significantly more frequent in the psychologically burdened group. Other biological elements, such as genetics and the immune system, may also cause a corresponding vulnerability to mental illness (51). Psychoneuroimmune and psychoneuroendocrine components are suspected to negatively affect mental health acutely and as long-term consequences (52). If these associations are further explored by additional studies, they could become key elements in preventing SARS-CoV-2-related mental illness through targeted therapy.
Psychotherapy should play a central role in the treatment of psychologically burdened patients with SARS-CoV-2 as well and may help alleviate psychiatric symptoms (53, 54). The major challenge is social distancing, which is obligatory in acute SARS-CoV-2 infection. Here, online mental health services, telepsychotherapy, and telepsychiatry can overcome this situation (55). In the acute situation, they may not be as helpful and preferred as regular psychotherapy (56), so aftercare programs and psychosocial support programs are essential to cope with the consequences of the SARS-CoV-2 infection.
Psychopharmacology may be indicated to overcome the acute situation and to avoid (neuropsychiatric) long-term consequences (57). However, because SARS-CoV-2 infection is a multiorgan disease with altered pharmacokinetics, psychopharmacologic treatment is complex (58). Furthermore, the drugs used to treat SARS-CoV-2 infection, such as remdesivir, chloroquine, or interferon, are suspected to have psychotropic effects (58). Further studies are needed to responsibly use the opportunities of psychopharmacology in SARS-CoV-2 infection.
This is the only study so far focusing on stress experience and coping behaviors during home isolation and eliciting differences in terms of psychological burden. Nevertheless, there are a few limitations in the sample selection and generalization. Persons in inpatient care facilities were excluded from the study because in the pandemic setting, completion of the online questionnaire by this group would have been hardly possible. As in previous studies, validated questionnaires were used for the diagnosis of psychological burden (5, 8). However, these were self-completed by the infected individuals and therefore prone to reporting bias. Moreover, symptoms were assessed but no clinical diagnoses were made. Here, clinical interviews would have been necessary. The self-generated questionnaires on stress experience and coping behavior during home isolation have proven to be reliable, but they have not undergone a validation process.
To confirm and better generalize these study results, further, supra-regional, prospective, and follow-up studies including people in inpatient care facilities, demented patients, patients with mild cognitive impairment, and minors, are needed.
For the first time, this study provides insights into the distinct stress experience and coping strategies of SARS-CoV-2 infected individuals with a focus on home isolation. Psychologically burdened subjects experience this situation as significantly more stressful and use fewer coping strategies to manage their infection during home isolation. Accordingly, a structured support service for SARS-CoV-2 infected individuals should be established that considers the special circumstances of home isolation. Initially, all home-isolated infected individuals could benefit from low threshold coping skills interventions, such as eHealth interventions (59–62). Since the prevalence of psychological burden is 54%, a general and standardized screening procedure for psychological burden among people with SARS-CoV-2 should be established. SARS-CoV-2 infected individuals with psychological burden should receive targeted support with professional help (63) in the areas of stress experience and coping skills during their home isolation to avoid long-term mental health consequences. It is very important that psychosocial care for patients with SARS-CoV-2 is based on guidelines and protocols (64, 65). Immediate assessment of individual concerns and stressors, resource-based psychosocial support and strengthening of coping skills should be employed to prevent negative long-term effects.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the University Hospital Tuebingen. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
EK, JG, AnS, SZ, and AxS: study design. EK: data collecting and analyzing and manuscript. JG, AnS, SZ, AxS, and EK: revising manuscript. All authors contributed to the article and approved the submitted version.
Funding
We acknowledge support by Deutsche Forschungsgemeinschaft and the Open Access Publishing Fund of the University of Tübingen.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We sincerely thank all study participants who took the time to complete the survey during their isolation. Further, we would like to thank the Freudenstadt Health Office and the Baden-Württemberg State Health Office (in particular the Head of the Health Protection and Epidemiology Unit Stefan Brockmann) for structural support during the recruitment phase.
References
1. Director-General W. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–11-march-2020 (accessed Ocotber 05, 2021).
2. WHO. W.H.O. COVID-19 Case Numbers. Available online at: https://who.sprinklr.com/ (accessed Ocotber 05, 2021).
3. Jacob L, Koyanagi A, Smith L, Haro JM, Rohe AM, Kostev K. Prevalence of and factors associated with COVID-19 diagnosis in symptomatic patients followed in general practices in Germany between March 2020 and March 2021. Int J Infect Dis. (2021) 111:37–42. doi: 10.1016/j.ijid.2021.08.010
4. Sánchez-Villena AR, de La Fuente-Figuerola V. COVID-19: quarantine, isolation, social distancing and lockdown: are they the same? An Pediatr (Engl Ed). (2020) 93:73–4. doi: 10.1016/j.anpedi.2020.05.001
5. Liu C, Pan W, Li L, Li B, Ren Y, Ma X. Prevalence of depression, anxiety, and insomnia symptoms among patients with COVID-19: a meta-analysis of quality effects model. J Psychosom Res. (2021) 147:110516. doi: 10.1016/j.jpsychores.2021.110516
6. Sahan E, Unal SM, Kirpinar I. Can we predict who will be more anxious and depressed in the COVID-19 ward? J Psychosom Res. (2021) 140:110302. doi: 10.1016/j.jpsychores.2020.110302
7. Ramezani M, Simani L, Karimialavijeh E, Rezaei O, Hajiesmaeili M, Pakdaman H. The role of anxiety and cortisol in outcomes of patients with Covid-19. Basic Clin Neurosci. (2020) 11:179–84. doi: 10.32598/bcn.11.covid19.1168.2
8. Ripon RK, Mim SS, Puente AE, Hossain S, Babor MMH, Sohan SA, et al. COVID-19: psychological effects on a COVID-19 quarantined population in Bangladesh. Heliyon. (2020) 6:e05481. doi: 10.1016/j.heliyon.2020.e05481
9. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
10. Cavicchioli M, Ferrucci R, Guidetti M, Canevini MP, Pravettoni G, Galli F. What will be the impact of the Covid-19 quarantine on psychological distress? Considerations based on a systematic review of pandemic outbreaks. Healthcare (Basel). (2021) 9:101. doi: 10.3390/healthcare9010101
11. Henssler J, Stock F, van Bohemen J, Walter H, Heinz A, Brandt L. Mental health effects of infection containment strategies: quarantine and isolation-a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. (2021) 271:223–34. doi: 10.1007/s00406-020-01196-x
12. Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. (2020) 42:e2020038. doi: 10.4178/epih.e2020038
13. Purssell E, Gould D, Chudleigh J. Impact of isolation on hospitalised patients who are infectious: systematic review with meta-analysis. BMJ Open. (2020) 10:e030371. doi: 10.1136/bmjopen-2019-030371
14. Lohiniva AL, Dub T, Hagberg L, Nohynek H. Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS One. (2021) 16:e0247962. doi: 10.1371/journal.pone.0247962
15. Kandeger A, Aydin M, Altinbas K, Cansiz A, Tan O, Tomar Bozkurt H, et al. Evaluation of the relationship between perceived social support, coping strategies, anxiety, and depression symptoms among hospitalized COVID-19 patients. Int J Psychiatry Med. (2021) 56:240–54. doi: 10.1177/0091217420982085
16. Datar M, Patil S, Shetty J, Naphade N. Psychological consequences and coping strategies of patients undergoing treatment for COVID-19 at a tertiary care hospital: a qualitative study. Asian J Soc Health Behav. (2021) 4:62–8. doi: 10.4103/shb.shb_5_21
17. Samrah SM, Al-Mistarehi AH, Aleshawi AJ, Khasawneh AG, Momany SM, Momany BS, et al. Depression and coping among COVID-19-infected individuals after 10 days of mandatory in-hospital quarantine, Irbid, Jordan. Psychol Res Behav Manag. (2020) 13:823–30. doi: 10.2147/PRBM.S267459
18. GmbH Q. EFS Survey, Version EFS Fall 2020. Cologne: Questback GmbH (2020). Available online at: https://www.questback.com/ (accessed Ocotber 05, 2021).
19. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
20. Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
21. Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114:163–73. doi: 10.1016/j.jad.2008.06.026
22. Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
23. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
24. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
25. Barsky AJ. Assessing the new DSM-5 diagnosis of somatic symptom disorder. Psychosom Med. (2016) 78:2–4. doi: 10.1097/PSY.0000000000000287
26. Husing P, Bassler M, Lowe B, Koch S, Toussaint A. Validity and sensitivity to change of the Somatic Symptom Disorder-B Criteria Scale (SSD-12) in a clinical population. Gen Hosp Psychiatry. (2018) 55:20–6. doi: 10.1016/j.genhosppsych.2018.08.006
27. Husing P, Lowe B, Toussaint A. Comparing the diagnostic concepts of ICD-10 somatoform disorders and DSM-5 somatic symptom disorders in patients from a psychosomatic outpatient clinic. J Psychosom Res. (2018) 113:74–80. doi: 10.1016/j.jpsychores.2018.08.001
28. Kop WJ, Toussaint A, Mols F, Lowe B. Somatic symptom disorder in the general population: associations with medical status and health care utilization using the SSD-12. Gen Hosp Psychiatry. (2019) 56:36–41. doi: 10.1016/j.genhosppsych.2018.10.004
29. Toussaint A, Husing P, Kohlmann S, Lowe B. Detecting DSM-5 somatic symptom disorder: criterion validity of the Patient Health Questionnaire-15 (PHQ-15) and the Somatic Symptom Scale-8 (SSS-8) in combination with the Somatic Symptom Disorder - B Criteria Scale (SSD-12). Psychol Med. (2020) 50:324–33. doi: 10.1017/S003329171900014X
30. Toussaint A, Riedl B, Kehrer S, Schneider A, Lowe B, Linde K. Validity of the Somatic Symptom Disorder-B Criteria Scale (SSD-12) in primary care. Fam Pract. (2018) 35:342–7. doi: 10.1093/fampra/cmx116
31. Toussaint A, Murray AM, Voigt K, Herzog A, Gierk B, Kroenke K, et al. Development and validation of the Somatic Symptom Disorder-B Criteria Scale (SSD-12). Psychosom Med. (2016) 78:5–12. doi: 10.1097/PSY.0000000000000240
32. Toussaint A, Lowe B, Brahler E, Jordan P. The Somatic Symptom Disorder – B Criteria Scale (SSD-12): factorial structure, validity and population-based norms. J Psychosom Res. (2017) 97:9–17. doi: 10.1016/j.jpsychores.2017.03.017
33. Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C, et al. Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychosom Res. (1993) 37:19–32. doi: 10.1016/0022-3999(93)90120-5
34. Fliege H, Rose M, Arck P, Walter OB, Kocalevent RD, Weber C, et al. The Perceived Stress Questionnaire (PSQ) reconsidered: validation and reference values from different clinical and healthy adult samples. Psychosom Med. (2005) 67:78–88. doi: 10.1097/01.psy.0000151491.80178.78
35. Satow L. Stress- und Coping-Inventar (SCI): Test- und Skalendokumentation. (2012). Available online at: http://www.drsatow.de (accessed on 05 Ocotber 2021).
36. Satow L. Stress- und Coping-Inventar (SCI): Testmanual und Normen. (2012). Available online at: http://www.drsatow.de (accessed on 05 Ocotber 2021).
37. Kaiser HF, Rice J. Little Jiffy, Mark Iv. Educ Psychol Meas. (2016) 34:111–7. doi: 10.1177/001316447403400115
38. Kaiser HF, Dickman KW editors. Analytic Determination of Common Factors. Washington, DC: American Psychological Association.
39. Guttman L. Some necessary conditions for common-factor analysis. Psychometrika. (1954) 19:149–61. doi: 10.1007/BF02289162
40. Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. (1988) 83:1198–202. doi: 10.1080/01621459.1988.10478722
41. Urban D, Mayerl J. Angewandte Regressionsanalyse: Theorie, Technik und Praxis. Studienskripten zur Soziologie. Wiesbaden: Springer (2018).
42. Urban D, Mayerl J, Wahl A. Regressionsanalyse bei fehlenden Variablenwerten (missing values):Imputation oder Nicht-Imputation? Eine Anleitung für die Regressionspraxis mit SPSS. Schriftenreihedes Instituts für Sozialwissenschaften der Universität Stuttgart—SISS (2016).
43. Hauser W, Hausteiner-Wiehle C, Henningsen P, Brahler E, Schmalbach B, Wolfe F. Prevalence and overlap of somatic symptom disorder, bodily distress syndrome and fibromyalgia syndrome in the German general population: a cross sectional study. J Psychosom Res. (2020) 133:110111. doi: 10.1016/j.jpsychores.2020.110111
44. Willis C, Chalder T. Concern for Covid-19 cough, fever and impact on mental health. What about risk of Somatic Symptom Disorder? J Ment Health. (2021) 30:551–5. doi: 10.1080/09638237.2021.1875418
45. Matalon N, Dorman-Ilan S, Hasson-Ohayon I, Hertz-Palmor N, Shani S, Basel D, et al. Trajectories of post-traumatic stress symptoms, anxiety, and depression in hospitalized COVID-19 patients: a one-month follow-up. J Psychosom Res. (2021) 143:110399. doi: 10.1016/j.jpsychores.2021.110399
46. Vincent A, Beck K, Becker C, Zumbrunn S, Ramin-Wright M, Urben T, et al. Psychological burden in patients with COVID-19 and their relatives 90 days after hospitalization: a prospective observational cohort study. J Psychosom Res. (2021) 147:110526. doi: 10.1016/j.jpsychores.2021.110526
47. Ismael F, Bizario JCS, Battagin T, Zaramella B, Leal FE, Torales J, et al. Post-infection depressive, anxiety and post-traumatic stress symptoms: a prospective cohort study in patients with mild COVID-19. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 111:110341. doi: 10.1016/j.pnpbp.2021.110341
48. Jung SJ, Jeon YJ, Yang JS, Park M, Kim K, Chibnik LB, et al. Impact of COVID-19 on mental health according to prior depression status: a mental health survey of community prospective cohort data. J Psychosom Res. (2021) 148:110552. doi: 10.1016/j.jpsychores.2021.110552
49. Pearman A, Hughes ML, Smith EL, Neupert SD. Age differences in risk and resilience factors in COVID-19-related stress. J Gerontol B Psychol Sci Soc Sci. (2021) 76:e38–e44. doi: 10.1093/geronb/gbaa120
50. Schou TM, Joca S, Wegener G, Bay-Richter C. Psychiatric and neuropsychiatric sequelae of COVID-19 - a systematic review. Brain Behav Immunity. (2021) 97:328–48. doi: 10.1016/j.bbi.2021.07.018
51. Kop WJ. Biopsychosocial processes of health and disease during the COVID-19 pandemic. Psychosom Med. (2021) 83:304–8. doi: 10.1097/PSY.0000000000000954
52. Menon V, Padhy SK. Mental health among COVID-19 survivors: are we overlooking the biological links? Asian J Psychiatry. (2020) 53:102217. doi: 10.1016/j.ajp.2020.102217
53. Shatri H, Prabu OG, Tetrasiwi EN, Faisal E, Putranto R, Ismail RI. The role of online psychotherapy in COVID-19: an evidence based clinical review. Acta Med Indones. (2021) 53:352–9. Available online at: http://www.actamedindones.org/index.php/ijim/article/view/1701/pdf (accessed October 22, 2021).
54. Holly A. Swartz MD. The role of psychotherapy during the COVID-19 pandemic. Am J Psychotherapy. (2020) 73:41–2. doi: 10.1176/appi.psychotherapy.20200015
55. Al-Alawi M, McCall RK, Sultan A, Al Balushi N, Al-Mahrouqi T, Al Ghailani A, et al. Efficacy of a six-week-long therapist-guided online therapy versus self-help internet-based therapy for COVID-19-induced anxiety and depression: open-label, pragmatic, randomized controlled trial. JMIR Ment Health. (2021) 8:e26683. doi: 10.2196/26683
56. Venville A, O'Connor S, Roeschlein H, Ennals P, McLoughlan G, Thomas N. Mental health service user and worker experiences of psychosocial support via telehealth through the COVID-19 pandemic: qualitative study. JMIR Ment Health. (2021) 8:e29671. doi: 10.2196/29671
57. Javelot H, Straczek C, Meyer G, Gitahy Falcao Faria C, Weiner L, Drapier D, et al. Psychotropics and COVID-19: an analysis of safety and prophylaxis. Encephale. (2021). doi: 10.1016/j.encep.2021.08.002. [Epub ahead of print].
58. Bilbul M, Paparone P, Kim AM, Mutalik S, Ernst CL. Psychopharmacology of COVID-19. Psychosomatics. (2020) 61:411–27. doi: 10.1016/j.psym.2020.05.006
59. Bauerle A, Graf J, Jansen C, Musche V, Schweda A, Hetkamp M, et al. E-mental health mindfulness-based and skills-based 'CoPE It' intervention to reduce psychological distress in times of COVID-19: study protocol for a bicentre longitudinal study. BMJ Open. (2020) 10:e039646. doi: 10.1136/bmjopen-2020-039646
60. Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. (2020) 39:101132. doi: 10.1016/j.ctcp.2020.101132
61. Wei N, Huang BC, Lu SJ, Hu JB, Zhou XY, Hu CC, et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J Zhejiang Univ Sci B. (2020) 21:400–4. doi: 10.1631/jzus.B2010013
62. Xiao CX, Lin YJ, Lin RQ, Liu AN, Zhong GQ, Lan CF. Effects of progressive muscle relaxation training on negative emotions and sleep quality in COVID-19 patients: a clinical observational study. Medicine (Baltimore). (2020) 99:e23185. doi: 10.1097/MD.0000000000023185
63. Kong X, Kong F, Zheng K, Tang M, Chen Y, Zhou J, et al. Effect of psychological-behavioral intervention on the depression and anxiety of COVID-19 patients. Front Psychiatry. (2020) 11:586355. doi: 10.3389/fpsyt.2020.586355
64. World Health Organization. Clinical management of COVID-19: Interim Guidance 2020. Report No.: Contract No.: WHO/2019-nCoV/clinical/2020.5. Geneva: World Health Organization (2020). Available online at: https://apps.who.int/iris/handle/10665/332196 (accessed October 05, 2021).
65. Committee I-AS. Operational Considerations for Multisectoral Mental Health and Psychosocial Support Programmes During the COVID-19 Pandemic. (2020). Available online at: https://interagencystandingcommittee.org/system/files/2020-06/IASC%20Guidance%20on%20Operational%20considerations%20for%20Multisectoral%20MHPSS%20Programmes%20during%20the%20COVID-19%20Pandemic.pdf (accessed October 05, 2021).
Keywords: cross-sectional study, COVID-19, mental health, patient, psychological, quarantine
Citation: Kowalski E, Schneider A, Zipfel S, Stengel A and Graf J (2021) SARS-CoV-2 Positive and Isolated at Home: Stress and Coping Depending on Psychological Burden. Front. Psychiatry 12:748244. doi: 10.3389/fpsyt.2021.748244
Received: 27 July 2021; Accepted: 01 November 2021;
Published: 22 November 2021.
Edited by:
Michael Noll-Hussong, Saarland University Hospital, Homburg (Saar), GermanyReviewed by:
Reiji Yoshimura, University of Occupational and Environmental Health Japan, JapanDarpan Kaur, Mahatma Gandhi Missions Medical College and Hospital, India
Copyright © 2021 Kowalski, Schneider, Zipfel, Stengel and Graf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johanna Graf, am9oYW5uYS5ncmFmQG1lZC51bmktdHVlYmluZ2VuLmRl
 Elias Kowalski
Elias Kowalski Axel Schneider2
Axel Schneider2 Stephan Zipfel
Stephan Zipfel Andreas Stengel
Andreas Stengel Johanna Graf
Johanna Graf