- 1McGill Centre for Integrative Neuroscience, Montreal Neurological Institute, McGill University, Montreal, QC, Canada
- 2Division of Social & Transcultural Psychiatry, McGill University, Montreal, QC, Canada
- 3Culture and Mental Health Research Unit, Lady Davis Institute, Jewish General Hospital, Montreal, QC, Canada
- 4Technoculture, Arts and Game Centre, Milieux Institute for Art, Culture and Technology, Concordia University, Montreal, QC, Canada
- 5Patient Partner, Montreal, QC, Canada
- 6Department of Psychology, McGill University, Montreal, QC, Canada
- 7Department of Computer Science, Concordia University, Montreal, QC, Canada
- 8PERFORM Centre, Concordia University, Montreal, QC, Canada
- 9Department of Creative Art Therapies, Concordia University, Montreal, QC, Canada
- 10Department of Anesthesiology, Leiden University Medical Centre, Leiden University, Leiden, Netherlands
- 11Faculty of Dentistry, McGill University, Montreal, QC, Canada
- 12Department of Sociology, Concordia University, Montreal, QC, Canada
The value of understanding patients' illness experience and social contexts for advancing medicine and clinical care is widely acknowledged. However, methodologies for rigorous and inclusive data gathering and integrative analysis of biomedical, cultural, and social factors are limited. In this paper, we propose a digital strategy for large-scale qualitative health research, using play (as a state of being, a communication mode or context, and a set of imaginative, expressive, and game-like activities) as a research method for recursive learning and action planning. Our proposal builds on Gregory Bateson's cybernetic approach to knowledge production. Using chronic pain as an example, we show how pragmatic, structural and cultural constraints that define the relationship of patients to the healthcare system can give rise to conflicted messaging that impedes inclusive health research. We then review existing literature to illustrate how different types of play including games, chatbots, virtual worlds, and creative art making can contribute to research in chronic pain. Inspired by Frederick Steier's application of Bateson's theory to designing a science museum, we propose DiSPORA (Digital Strategy for Play-Oriented Research and Action), a virtual citizen science laboratory which provides a framework for delivering health information, tools for play-based experimentation, and data collection capacity, but is flexible in allowing participants to choose the mode and the extent of their interaction. Combined with other data management platforms used in epidemiological studies of neuropsychiatric illness, DiSPORA offers a tool for large-scale qualitative research, digital phenotyping, and advancing personalized medicine.
Introduction
Chronic Pain: The Limits of Biomedical Models
Chronic persistent pain (CP) is a leading cause of disability worldwide (1–5). Medical science has had limited success in treating many forms of CP and there is increasing recognition that responding to CP requires more than purely biomedical models (6, 7). Contemporary approaches recognize that the sensory processes of pain are modulated by top-down influences including expectations, emotions, and cultural mediated meanings (8). Melzack's neuromatrix pain theory, for example, considers that variations in nociceptive sensitivity may arise from genetic predispositions (9), as well as from a cascade of emotional and cognitive factors that modulate the sensory neural signaling resulting in different experiences among individuals even when they experience similar injury, and for the same individual in different contexts (6). Psychological stress affects pain perception (6, 10, 11). Sociopolitical, economic and cultural stressors do too (12–14). As Craig's Social Communication Model of Pain emphasizes, because humans must adapt to complex social environments, social contexts impact on how pain is experienced, and thus cognitive and social processes and contexts must be considered in understanding patients' own perceptions and behaviors in presence of pain (15). The neuromatrix and communication models can be integrated and extended by recognizing that bodily experiences and social contexts provide metaphors for thinking about and expressing pain experience—and can reshape that experience (16). Pain experience is mediated, elaborated and communicated through cultural models which need to be studied with qualitative methods (17–19).
Pain is inherently a subjective experience and the quality of communication between patient and clinician is crucial for assessment and treatment. Communicating effectively about one's pain in clinical settings is challenging (20). Social factors, including power imbalances inherent in healthcare systems (in which both patient and physician may assume that doctors know better and their time is too valuable to waste), can distort effective communication and silence the patient (21–27). Miscommunication can lead to inaccurate or incomplete assessment, limit patients' access to resources for pain control, coping, and prevention and impede community support and medical care (28). The failure to adequately assess and track patients' experience of pain contributes to disparities in care and may impede progress in the development of innovative interventions.
Partnerships between people with lived experience of pain and researchers are recognized as vital for advancing knowledge and practice in CP care (29–33). However, the experience of CP remains extremely challenging to communicate, quantify, and explain to others (34, 35). Unlike many chronic health conditions (such as hypertension), there are no reliable objective measures or biomarkers for pain, hence patients' self-reports are crucial. Even standardized psychometric instruments may miss patients with clinically important pain (36). The framework we describe in this paper aims to provide an innovative approach to pain experience in research and clinical settings by using digital technology to facilitate playful exploration and reflection.
Integrating Context and Experience in Pain Research
Given the diverse cultural contexts, constructs, and belief systems that shape how individuals communicate distress and seek care, it is difficult to quantify individual differences in pain experience (17, 20, 37). By extension, it is difficult to offer personalized care without an understanding of the social-cultural contexts or ecologies in which individual experience is embedded and from which it draws meaning and consequence. These contexts have physical, geographical, ideological, linguistic, political, and historical dimensions that need to be studied qualitatively. Qualitative analysis can inform the development of quantitative measures that more accurately capture the lived experience and consequences of pain and that can be used in large-scale studies. However, qualitative research is labor intensive even with small samples and hence cannot insure representativeness or generalizability of results. Large samples are needed to canvas the range of experiences, establish generalizability, and better understand the interaction of multiple variables.
Large-scale qualitative research poses methodological challenges related to: gathering data rigorously (38); creating a space for research partners to communicate and actively collaborate (39); ensuring inclusivity and equitable opportunities for shared learning through mutual respect; and disseminating knowledge through effective action (40). Faced with these challenges, biomedical research (which aims to produce “hard evidence” through rigorous hypothesis testing) may limit engagement with modes of knowledge creation and practice that do not fit easily with its epistemic culture (21, 22) and opt for methods that elide patient experience (41).
The Promise of Information and Communication Technologies (ICT) for Integrative Pain Research
ICTs are becoming widely used tools for research and clinical data collection (42). They allow incorporating social media, biosensing, and artificial intelligence in the collection and analysis of health data (43), thus increasing efficiency in the accumulation and analysis of large datasets for digital phenotyping (44) in fields as diverse as behavioral neuroscience and computational sociology. Given the global penetration of smart mobile technologies (78% in 2020), ICTs make it possible to collect ecological data, disseminate information, and offer digital interventions remotely (45). For example, a recent systemic meta-review by Finucane et al. found that interventions such as videoconferencing, interactive social media and weblogs, educational websites, and high-fidelity simulators targeting professionals for retraining were feasible and potentially impactful tools for reducing costs, improving patient care, facilitating communication and information sharing, as well as for data collection and decision-making support in palliative care (46).
Although often used to collect quantitative data, ICTs can readily be adapted to obtain rich qualitative data and configured in ways that allow the interaction essential for more participatory health research. Several approaches to deploying ICTs in health research are currently being tested. Initiatives such as “Saskatchewan, let's move and map our activity” used citizen science to study active living, with a mobile app incorporating various tools from location monitoring to questionnaires in order to identify factors that motivate individuals to be physically active in different seasons (26). Initiatives such as PatientsLikeMe serve as virtual science laboratories where, while conducting N = 1 self-trials (47), participants also provide support to each other and exchange knowledge by sharing personal experiences as well as biological samples (48). Further, recent advances in data science demonstrate that social media can be important platforms for data collection and community knowledge creation (49). For example, the impact of Twitter interactions on public health was extensively studied during the COVID-19 pandemic (50–52). Massive multiplayer online games (MMOG), or role playing games (RPG) are other examples of ICTs that have been used for interactive research data collection (53).
Shortcomings of Current ICTs for Qualitative Research
Large-scale qualitative research among culturally, geographically, and linguistically heterogenous populations is challenging (38, 39). ICTs are readily deployed to accumulate large datasets and one simple application of ICTs in mixed-methods research is to facilitate survey studies that lead to the creation and validation of reliable instruments for quantitative research (45). Alternatively, passive data generation (through surveillance and monitoring), and data-mining algorithms can try to uncover patterns (and predict outcomes). However, passive data collection methods often overlook the specific contexts or circumstances that define an individual's agency, subjectivity, and ability to express their priorities and concerns (54, 55). Neither surveys nor surveillance systems (through biosensors or trackers) solicit participants' opinions or knowledge; they therefore invite criticism on the grounds of ecological validity as well as research ethics (56–58).
For these and other reasons, if data mining is to advance healthcare, there is a need to integrate the ethical principles and processes of participatory health research (PHR), which involves the systematic engagement of patients and other stakeholders in the process of initiating, designing and interpreting research to develop actionable solutions (59, 60). To achieve this, ICTs must go beyond passive data mobilization to create the conditions for patient-oriented and person-centered research that is informed and guided by individuals' experiences (26, 61, 62).
Research Approach
In the past 20 years, researchers have created numerous cohorts with neuropsychological epidemiological data to discover the causes and correlates of various brain-related disorders (63–66). Vast resources have been dedicated to data mining from biological specimens, extensive arrays of psychometric and physiological measures, and various types of radiological data (67, 68). However, active engagement of stakeholders and research participants at every stage of project development from its earliest conception, through design, data collection and interpretation, to translation into policy and practice can improve the relevance, quality and impact of health research (40, 69–80).
Given this context, we aimed to explore how ICTs could be used to add capacity to integrate qualitative data with standard quantitative research methods used in epidemiological studies of brain-related disorders. Our approach was inspired by emerging research that has shown that play with digital media is a promising strategy for conducting integrative neuropsychological research (81–84).
Our long-term goal is to use technology to diversify and democratize experimentation and participatory knowledge creation in health research. Chronic pain is an important focus for this work for several reasons: Pain is a debilitating physical condition that is universally experienced (so much so that there are now machine learning algorithms to detect pain experience from facial expressions or postural patterns) (85); but the causes of the chronicity of pain remain poorly understood and clinical assessment and care do not adequately incorporate patients' experience and life contexts.
We brought together an interdisciplinary team of clinicians, social scientists, bioethicists, designers, and computer scientists, with support from an intersectoral funding opportunity in the Province of Quebec (Canada), to develop an innovative ICT framework for play-oriented pain research. We held a 2-day public workshop in October 2019, bringing together research team members, clinicians, and individuals with lived experience of chronic pain (86, 87). The workshop was held at Concordia University's 4TH SPACE, an open gallery designed to showcase research and seek engagement from the public who were invited with the following message: “We are scientists, artists, therapists. We work to advance medicine through communication, community, creativity. Can we study pain by shedding on it the light of play?” Discussions were stimulated by playful activities that were facilitated by creative arts therapists, as well as by presentations from neuropsychology students on non-pharmacological pain research (music, movement, yoga), and performances by artists (theater, poetry). Two questions were the focus of these discussions:
• What strategies can capture the psychosocial and cultural mediators of chronic pain?
• What strategies can increase the opportunities of co-learning and co-creation among medical professionals, researchers, and patients who deal with chronic pain?
To answer these questions, we built on the workshop findings by reviewing the relevant literatures and iteratively developing a framework through discussions among team members. The approach presented in this paper is based on our identification of pragmatic, structural and cultural conflicts that need to be addressed in designing health-related ICTs. In this paper, we propose a theory-based approach that can guide the design of such applications.
The theoretical perspectives we draw from include neuromatrix pain theory (9), pain communication theory (15), cultural somatization theory (88), and person-centered research (23, 32, 37). We apply Gregory Bateson's cybernetic theory of self to illustrate how play (as a state of mind, as a mode of creation and communication, and as a structured, yet flexible framework for individual and group exploration) can provide a critical tool to advance mind-body research. The framework we propose aims to use digital media and game-like activities to engage people in exploring the quality, parameters, and modulators of their pain experience. Using modes of play can afford people some distance from the suffering associated with their health problem, while mobilizing both coping strategies and social connection to others. This theoretical framework has evolved in tandem with development of a limited prototype in the form of a bilingual mobile phone application, PlayThePain (86).
The paper is structured in three parts: First, we outline a theoretical framework for play as a tool for pain research; we then present a working definition of play, illustrated with examples of different types of play-oriented activities that can be implemented in a digital framework for pain research; finally, we provide a critical overview of how digital playgrounds can be implemented to be maximally inclusive and adaptable.
Theory: A Cybernetic Approach to Studying Pain By Playing
Gregory Bateson's Steps to an Ecology of Mind
Gregory Bateson was an anthropologist and interdisciplinary biological epistemologist whose work focused on the comparative analysis of relationships and interactions in human systems, extended to the relationship between ideas and the circumstances that determined the survival or extinction of cultural or natural subsystems. The systemic, interactional, ecosocial view that Bateson championed provides an integrative framework for advancing transdisciplinary research (89, 90).
In his collected papers, Steps to An Ecology of Mind (1972), Bateson laid the foundation of his cybernetic methodology—a recursive, simulation-based, experimental process that examines the emergence of meaning by observing variations in relationships, interactions, and feedback mechanisms between existing and emerging factors in a given system (91). His basic model of mind-body research distinguished three categories of knowledge, which can be applied to the study of chronic pain (Figure 1):
1. Observable phenomena (e.g., the manifest behaviors of an organism, such as avoiding painful stimuli or inability to move due to pain);
2. Explanatory constructs (e.g., self, motivation, anxiety, coping strategy, resilience); and
3. Underlying mechanisms, which either describe the processes involved in specific situations (e.g., prevalence of post-surgical pain) or common across varied contexts (e.g., the nociceptive pathways or circuits of the nervous system).
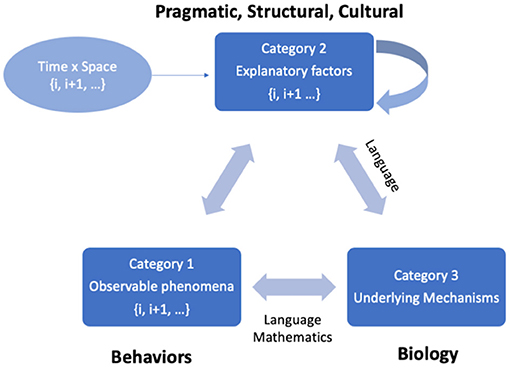
Figure 1. Bateson's cybernetic model of knowledge production. In neuropsychological research, the primary aim is to understand underlying mechanisms that give rise to an observable phenomenon. The relation between underlying mechanisms and the observable phenomena is mediated over time by various explanatory variables that may be interpreted flexibly within given contexts. Explanatory variables are influenced by various pragmatic, structural and cultural constraints and are prone to conflicts (including double binds) which involve recursive looping processes that must be studied over time and across contexts. The knowledge that emerges in this cybernetic model is often language dependent; however, if concepts are operationalized in measurable ways and sufficient data are collected, certain aspects can be represented by formal mathematical models.
Our understanding of the relationship between observations and underlying mechanisms is mediated by a complex set of explanatory factors (Category 2) which have different degrees of pragmatic, structural, behavioral, and social-cultural constraints.
Because explanatory constructs are communicated through language (using personal and local cultural models and metaphors) and are employed in self-understanding and social presentations, they are susceptible to becoming entangled in what Bateson termed double binds (92, 93). Double binds arise in conditions where:
1. Two or more individuals are involved in an intense relationship with a high (physical or psychological) survival value for at least one of them (e.g., mother and child; physician and patient);
2. In this relationship, messages are regularly given that, at one level of communication, assert something, but at another level negate or conflict with this assertion (e.g., the mother yells at the child that yelling is bad; a physician who prescribed the narcotics to a patient stops providing the prescription because he fears the patient will become an addict);
3. The messaging implies a form of punishment or cost (e.g., the mother yells at the child that if they yell, they will be punished; the physician responds negatively to the patient who persists in requesting opioid medication);
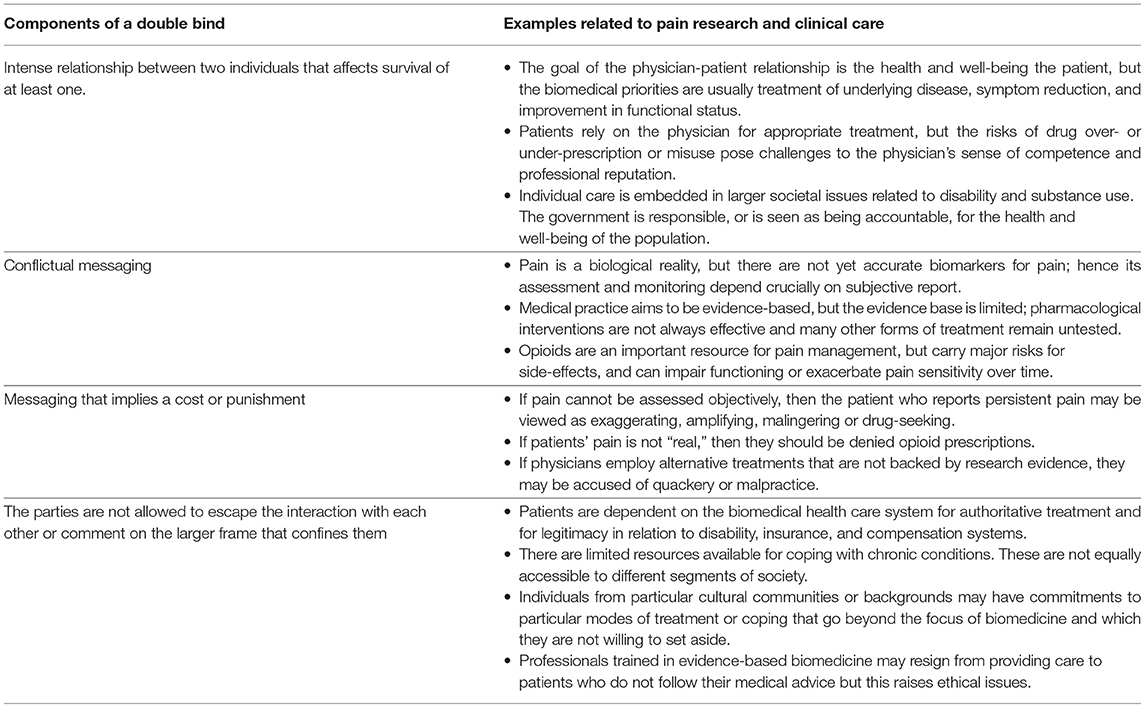
4. Those in the relationship cannot escape the relationship, nor are they allowed or able to comment on it (e.g., the authority of mother over child; the power imbalance between physician and patient). (Further examples are provided in Table 1).
Bateson suggested that such double binds could lead to serious mental health problems, particularly schizophrenia. Subsequent research has not borne this out—double binds are ubiquitous and not uniquely associated with psychosis, indeed they can also motivate creativity (94)—but there is no doubt that double-bind situations are stressful and can erode trust and collaboration in health care settings (27, 95–99). Bateson suggested two strategies for overcoming double binds: (i) meta-communication (i.e., talking about the difficulty of talking) (94, 100); and (ii) collecting large amounts of data to identify the regularities behind cultural variation and to reveal (and momentarily step outside) the taken-for-granted frameworks that create double-bind situations [(91), p. 161]. Bateson also suggested that play serves as a tool for meta-communication, making it possible to simulate double binds and re-negotiate relationships through fictive conflicts [(91), p. 170–193].
Play as Context and Method
In Western culture, “play” has been an object of theoretical reflection at least since Erasmus who argued that play is an existential necessity because it helps humans confront the inevitability of aging and death by becoming forgetful and carefree like children (101). Freud considered play a creative, adaptive, and therapeutic activity that generates pleasure by releasing tension (102, 103). According to Piaget, the pleasure of play is an important motivational asset, critical to behavioral and emotional development by promoting thinking, imagining, pretending, remembering, guessing, hoping, redoing, and working through problems (104). This developmental role is obvious in childhood but, in different forms, extends across the human lifespan. Huizinga argued that play is a precursor to the creation of culture, based on numerous examples showing that play is a uniquely human tendency to create imaginative aesthetics and rituals (religion, poetry, architecture, etc.), that give different meanings to the acts of satisfying biological needs (e.g., shelter, food, safety) (105).
Formal definitions of play have tried to operationalize it as a specific state of mind, mode of action, or form of communication. Play is “state of being active, operative, unimpeded in the logic of movement or the scope for action” (106). But play can also be defined by specific set of rules that structure actions in ways that may not have an obvious utilitarian function, such as in games or performances (on stage, in music, or sports). Play can engage with contradictory or ambiguous aspects of experience and explore new meanings and possibilities through performance. This can occur in solitary activities, small groups, or larger carnivalesque forms of play that allow individuals and communities to move beyond the dominant norms (frames) and interpretations of an experience (107).
For Bateson, all the characteristics of play (as state of mind, mode of action, and framework for communication) make play an experimental space for recursive learning in which participants learn by simulation and iterative interpretation and evaluation of outcomes without real-world costs or consequences. The paradoxical logic of play (for example, two people preparing to “fight” without intention to fight) allows simulating a double bind in which reality and fantasy co-exist, and relationships can be negotiated. By framing the meaning of actions as “just play,” the play situation then provides opportunities for meta-communication—reflecting on the rules and regulations that usually govern social interaction and experience [(91), p. 170–193]. Indeed, the anthropologist Sutton-Smith suggests the rhetorical uses and ambiguity of play (e.g., children's play, games and gambling, role playing, creative play, leisure and relaxation, or joking and foolishness) make it a useful tool for ethnographic research into how cultures construct meaning (108).
The message “this is play” creates opportunities for imaginative exploration in the safety of a context or situation defined as “as if” —that is, as outside the usual norms and structures of consequential action. Because the stakes in play are not consequential, the frame-flexibility can be modified. Rules of play, for example, can be negotiated to create new imaginative scenarios that provide opportunities for learning by observing causal links (through cycles of sensorimotor action) and by discovering tensions and possibilities in extended images, metaphors, and narratives. Through these experimental engagements with play, we can document how people with different pragmatic, structural and cultural resources, and constraints learn to adopt new behaviors and adapt to challenging experiences [(91), p. 170].
Applying the Cybernetic Model to Pain Research
Applying Bateson's cybernetic model (Figure 1) to the phenomenon of pain (9), a person's descriptions and expressions of pain (verbal, facial, bodily gestures, functional, or behavioral) are the observable phenomena, and the underlying mechanisms are the cognitive, physiological, and neural processing that subserve pain experience. Top-down processes of cognition, affect regulation, and expectation influence the activity of sensory pathways and central information processing (19, 109). These links are partly hardwired, partly learned, and also influenced by the ways that individuals interpret and narrate their experience. Communicative interactions between patients and others in the social world, including care providers, influence the way the observable phenomena and underlying mechanisms are linked (15). Social-cultural differences in embodied experience and metaphors for pain further mediate the relationship between the observed phenomena and mechanistic processes (17, 19, 37).
Consider the cybernetic model of chronic pain experience and treatment outlined in Figure 2. This diagram represents some of the complex relationships between an individual patient and the health and social care system. A patient in this system is an individual with unique personal experiences, knowledge, values and practices that shape their preferences and choices of treatment. Medical professionals provide care to individuals following current evidence-based practices for safe and efficacious treatment. But economic factors affect the availability of such services. Social and cultural factors such as family and community support systems, illness explanatory models, and expectations affect how an individual interacts with the health care system, which is itself governed by healthcare policy (110). Together this forms a complex system that does not lend itself to the general linear modeling that is common in scientific research.
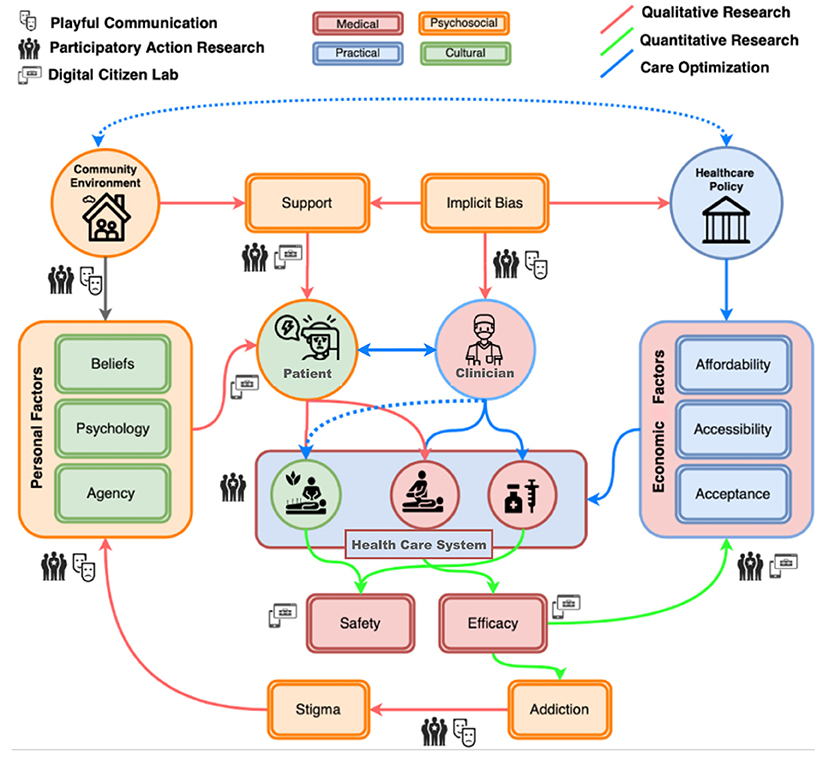
Figure 2. An extended cybernetic model for pain research. This diagram represents potential sites for data collection in the system of relationships between factors that govern the interaction of an individual patient and the health care system. Variables that relate to patients (indicated in green) include personal experiences and expressions of pain, as well as individual beliefs, psychological traits, and behaviors that express patients' agency, e.g., their treatment preferences and choices. Variables that relate to medical professionals (in pink) include the availability of evidence-based treatments with established safety and efficacy, and economic factors that affect the availability of services. Cultural contexts influence psychosocial factors (in orange) and reflect individuals' personal history and the community and wider social contexts in which they live. Social factors such as support systems, the implicit biases of healthcare institutions, and stigma (e.g., due to the perceived risk of addiction to opioid analgesics) influence individuals' pain experience and interactions with the health care system. Healthcare policy (in blue) influences the availability of care options (complementary and alternative, non-pharmacological, and biomedical) by determining their affordability, accessibility and acceptability. Different research methodologies can be deployed to investigate the interactions between these variables, including: quantitative data collection through a digital interface (indicated by a screen icon), e.g., analgesic efficacy and safety, cost, and availability of support; participatory action research (community icon), e.g., the study of stigma, community factors, implicit biases or economic factors; and play (theater masks icon) which can provide a flexible frame for studying interactions that are not captured by conventional research methodologies.
Bateson's approach suggests identifying pragmatic constraints (e.g., the extent of disability, costs, and accessibility of pharmacological or complementary resources, geographic distance from care systems, and language barriers that present obstacles to service access), and structural constraints (e.g., policies, commercial interests, and capital investment in research and technological innovation) and then examining how variations in cultural factors influence the meanings of individual experiences and behaviors in relation to the social frames and norms that surround an individual. In chronic pain, there are several common conflicts that affect the quality of care and, when these conflicts cannot be escaped because there are no feasible or accessible alternatives, they may constitute double binds. Examples of double-bind situations in relation to chronic pain are listed in Table 1. In the next section, we discuss three important conflicts and double binds that emerge from intersection of qualitative and quantitative approaches to studying and caring for people living with chronic pain.
Identifying Double Binds
Costs of Care vs. Cure
Modern medicine is heavily invested in discovering evidence-based cures. However, many CP conditions resist cure and instead require long-term care (111). Searching for a cure and providing care are both pragmatic responses to the predicament of persistent pain, but in the cultural context of modern medicine, individuals are expected to follow biomedical prescriptions. The imbalances in power arising from professional hierarchies then increase the risk of bias and stigmatization, resulting in blaming patients for lacking mental resolve to be cured, or blaming physicians for their inability to find a cure (112).
In ethnographic studies of chronic pain, anthropologists have shown that shame and stigma are multifaceted sociocultural constructs that are co-created by patients and caregivers (doctors, nurses, families) as well as the larger society (113–115). Providing long-term care is costly, and within societies in which productivity is a virtue, disability—even if socially accepted and accommodated—can be associated with self-reflective shame (116).
Double binds arising from confused messaging around care vs. cure can, in turn, create a pragmatic bias in what kind of treatment approach is acceptable (117). An instance of this conflicted messaging is that while the long-term efficacy of many pharmacological treatments for chronic pain remains uncertain (118–120), complementary, and alternative medicine (CAM) approaches are often dismissed outright by biomedicine as “quack science” (121). Even in a country like Germany—with its 200-year legacy of alternative medicine (122)—only half of physicians surveyed had a positive attitude toward CAMs (123). This is a concern because research has shown that doctors who are prone to dismissing CAMs based on a lack of clinical evidence are also more likely to be dismissive of their CP patients, creating a bias against the research and development required to test the efficacy of these treatments (24, 25). Lack of financial investment to scientifically evaluate what Vos and colleagues call “the orphaned fields of medicine” creates further disparity and inequities in access to care for those who cannot afford the “luxury” of paying for CAMs (124). Strategies to undertake inclusive research to identify cost-effective, efficient, and accessible interventions are needed to overcome persistent biases in knowledge creation and translation to practice. Cost-effective participatory methodologies may help insure inclusivity in research on more effective methods for care.
Underlying Mechanisms: Biomedical vs. Psychosocial
Double binds happen when two individuals are involved in an ongoing relationship they cannot exit because it has an important survival value for at least one of them. This can happen between patients and clinicians in health care settings. The poor correlation between extent of tissue damage and level of pain also undermines the credibility of patients' reports of pain. The persistent dualism of Western medical practice makes physicians uncomfortable treating patients who complain of pain with no visible or measurable physical substrate (125, 126). Pain experience is mediated and modulated by a host of psychological processes. However, viewing pain as a condition that is influenced by the mind runs the risk of implying that patients are causing their own problems, whether they are seen as malingering, drug seeking, or suffering from “somatoform disorders” (125, 127, 128). These negative appraisals and biases affect all patients with medically unexplained symptoms but are particularly severe for women and minorities. At the same time, evidence also suggests that the experience of discrimination is associated with increased pain, as found in studies with African Americans (12, 13) and Asian Americans (14). A review of epidemiological studies of pain among North American Indigenous Peoples found that patient-provider interactions generally were rated poorly by patients, who considered healthcare professionals to be uninterested or unsympathetic to their expressions of pain, potentially due to cultural differences in pain communication (129).
While there is a growing acceptance that “pain is whatever patient says it is,” what might be termed a forensic approach to diagnosis and clinical assessment aimed at determining the objective truth of “subjective” pain perpetuates implicit biases within the healthcare systems (130, 131). This has a gendered dimension, with women more likely to face dismissive attitudes based on “psychosomatic” attributions of pain (132), further blocking the channels for effective communication of their experiences (133, 134).
Semi-structured interviews with chronic pain patients have found that patients desire care providers who are open-minded, non-judgmental, attentive, and trusting of their expressed needs (135). Yaffe et al. found that trust fostered open communication with care-givers, which can lead to better outcomes (136). Understanding how people narrate (37), and interpret pain across variations in age, gender, culture, or ethnicity requires innovative approaches to data gathering and analysis (137). Beyond quantitative methods, we need to explore experiences more qualitatively and hermeneutically; that is, to learn how to interpret narratives of suffering as they are expressed in conversations, and to examine the ways in which the process of co-construction of meaning unfolds in the course of interactions between patients, clinicians and researchers (37).
Cultural Attitudes Toward Pain and Pleasure
Confused messaging can arise from the metaphoric language of “battling” illness which turns the inability to find a cure into failure or defeat, especially in cultural contexts in which competitiveness and winning are virtues (116). This competitiveness may make the notion of “winning” over pain a particular salient trope in Western, individualistic societies, but the determination to endure and contain one's suffering may be motivated by other cultural values that occur in different contexts. A 2018 study found that Indigenous participants in Alberta (Canada) framed their experience with arthritis in terms of “toughing it out”—an approach that allowed them to survive independently of Western medicine. This culturally and historically shaped attitude contributed to their hesitancy to seek timely medical care (138).
There is a substantial literature on ethnocultural differences in coping with pain which reflect differences in styles of emotional expression and communication as well as the meanings of pain and suffering (139–141). For example, a number of factors influence how people from Asian cultures may communicate their pain, such as stoicism (enduring pain or pleasure without expressing it), Buddhism (endurance of pain as a reality of being alive), Confucianism (emphasizing social harmony, and putting society's needs before one's own), social hierarchy status (the physician as holding a position of authority), and, in the case of migrants, language barriers within immigrant communities (142). These cultural variations affect the use of services, modes of clinical presentation and can lead to the false impression that certain populations experience less pain than others.
Cultural differences in the communication of pain and pleasure are based on sensory experiences that are influenced by metaphors that can reshape subsequent experiences (17). This cultural mediation of pain experience points to the importance of a multidisciplinary approach to pain assessment and intervention. Having asserted that access to pain management is a “fundamental human right,” The Declaration of Montreal ratified in 2010 by the International Association for the Study of Pain (IASP) (comprising IASP representatives from chapters in 64 countries plus members in 130 countries, as well as members of the community) emphasized the necessity of multidisciplinary pain clinics equipped to address the complex biopsychosocial aspects of CP (143). Yet, despite consensus among professionals and policy makers, the implementation of such programs has been limited because they are costly, and they have remained inaccessible to many in low-income and marginalized communities.
Given the limited availability of multimodal treatment programs and non-pharmacological methods of pain control (144), primary care physicians have focused on medications, including opioids as an expedient approach. This leads to ambiguities and conflicts in communication and treatment negotiation in primary care and other clinical settings (145–148). Miscommunication is also associated with disparities in over- or under-prescription of pain medications to racialized and ethnic minorities (149, 150) that are tied to a lack of attention to social context (151) and to implicit biases that are deeply rooted (152–154). Inconsistencies and lack of trust with regard to permissive or restrictive opiate prescription creates potential double binds in the relationship between healthcare providers and marginalized, racialized, or ethnic minority patients (155).
The double bind in the prescription of opiates arises from the confusing or contradictory messages that opiates have the power to alleviate pain (though inconsistently) (145, 146), but they are 'dangerous' and addictive (148). Moreover, they can also evoke pleasurable feelings and hence, their use may be viewed as a form of self-indulgence and expression of moral weakness (156). Patients who develop opioid dependency struggle when the healthcare system limits access to narcotics (157, 158). In the process, these patients also come to bear the stigma of being labeled as “drug seekers” (159, 160).
To understand the influence of culture and context on how individuals cope with pain and on the delivery of health care, it is important to devise a strategy that accommodates open discussion of both the stoic and hedonic aspects of taking care of one's pain. In what follows, we suggest that modes of exploratory play enabled by digital media can provide a useful component of such a strategy.
Implementing Play as a Tool for ICT-Based Citizen Science
Science Museums as Playgrounds for Research
Contemporary science museums, which are designed to provide opportunities for playful exploration of natural phenomena, offer a useful illustration of how we might incorporate play in participatory health research. These museums are set up to allow visitors to explore and interact with exhibits in a flexible way (161). In designing The Museum of Science and Industry in Tampa, Florida, Steier applied Bateson's notion of the flexibility of the frame of play to develop a mode of knowledge generation, by asking: “How do different families interact with the material of an exhibit and how do they interact with each other?” (162). In a science museum, the frame is created by the explicit objective of science communication, the physical location of the installation, the types of science on display, and the specific modes of interaction enabled by media and human docents or facilitators. However, this frame is flexible; it is defined by who chooses to participate, how involved they wish to become, what experiments they choose to explore, and how they engage with and reflect on the activities. Information from these interactions can also inform re-designing the museum to meet the needs of specific groups of users (163).
There are several modes of incorporating play in knowledge creation used in science museums that can be implemented in a digital health research “laboratory.” A virtual simulation of a “science museum” in digital media that simulates the dynamics of exploring exhibits can provide flexible ways for participants to engage and interact with various exhibits on “display.” These exhibits can provide specific modes of playful interaction that serve therapeutic, educational, creative, and experimental objectives. These exhibits can also invite critical reflection on specific issues or questions (e.g., How much does it cost to care for chronic pain? What psychosocial factors exacerbate the burden of pain? How do people from different cultures express and cope with pain? What implicit biases impact on the healthcare system?).
Play as a Tool for Multi-Modal Data Generation
Citizen Science labs require active participation. In the model of the science museum, this participation takes the form of individuals choosing whether and when to engage with the playful activities or information that are presented in that space. In a play mode, participants may try to challenge the rules to reconfigure the elements, and do so alone or in a group (101–108). Although people often expect to benefit from play as a pleasurable, challenging, or expressive and creative activity that may help them learn new skills, make connections with others, and build relationships, because play occurs within a digitally simulated context, it does not need to be tied to a real-world outcome. As such, play encourages imaginative exploration and provides an opportunity to generate data that can be captured passively (by tracing interactions of users in the digital space) and actively (by inviting users to explicitly record and reflect on their experience and to interact with the arrangement of the space itself to reconfigure and re-create it in ways that suit their own needs and interests).
Games
Games are the most widely recognized forms of play. In a bid to capture the motivational aspects of games in non-game contexts, gamification has emerged in the last decade as a popular means of incorporating game-like elements in non-game contexts (164). Even without being designed for specific benefits, playing video games can be helpful for those who cope with mental or behavioral health problems. In a 2018 qualitative study with 20 US Army veterans (165), Colder Carras et al. showed that the participants used video games to manage mood and stress, and as a path to recovery by adaptive coping (e.g., distraction, control, symptom substitution); increasing mastery (confidence, insight, role functioning); and socializing (participation, support, brotherhood). Participants drew meaning from game narratives and characters, and enjoyed exciting or calming gameplay, as well as opportunities to connect, talk, and lead others—benefits that outweighed the problems arising from excessive use of games.
Gamification is increasingly used in rehabilitation and self-care routines to increase adherence and engagement (166–168). The use of game elements in virtual citizen science can bring increased user activity, motivation, and engagement to large-scale scientific projects (169). For example, the video game Re-Mission (www.re-mission.net), designed for children and young adults diagnosed with certain types of cancer, aims to educate participants about their illness and ways to manage chemotherapy treatment side-effects. To play the game, players control a virtual nanobot to make strategically effective decisions regarding self-care for side effects of their treatment regimen. Players must complete a mission successfully before moving on to the next level.
There has been considerable research on the analgesic benefits of digital playing for cancer pain (170, 171), burn victims (172–174), pediatric patients (171, 175) and amputees (176), albeit mostly targeting younger players. In pain management, the focus of playing such games is typically on patient education, distraction, or self-management—for example, evoking analgesia through active engagement with VR or digital games (170, 171, 176, 177). When explicitly used for pain control, such interventions can be viewed as Serious Games—designed to benefit players by training them to improve specific outcome measures (changes in cognitive, physical, and educational variables) against predefined goals (178). Such games serve a double purpose: they can be used both as experimental tools to capture data about patients' learning and behavioral adaptation, and as modes of intervention (if the data suggests efficacy).
Storytelling, Art Making, and Interpretation
Creative self-expression activities, such as digital storytelling (179), art making (or performance) or interpretation (180), can provide a context and a vehicle to communicate pain more hermeneutically (37)—that is, to convey not simply the mere fact of pain as a biomedical sensation or index of pathology but also its meaning as an experience mediated by interpretations that emerge from dynamic interactions between patients, clinicians, and researchers. Compared to games, art making and other forms of self-expression may be more flexible media for participatory and qualitative data generation (181). Indeed, internet groups, blogs, and social media already provide flexible tools for self-expression and communication (182, 183).
The language and process of art making are important resources for therapeutic care (184, 185). Reflecting on 3 years of experience with art therapy in palliative care, Bras et al. (186) suggested that medical professionals and patients can adopt the language of art, not only as a means for providing patients therapeutic relief, but also as a means to raise public awareness, and facilitate communication among patients, medical professionals and others involved in decision making about pain. Creative arts therapies have long been offered to individuals with chronic pain (187) to help reduce the psychosocial and emotional burden of chronic illnesses (188).
Digital frameworks can be used for content creation, and dissemination, for example, writing poems and stories, making music, recording sound, and creating images, drawings, videos, and light shows. When shared, the conversations that emerge from encounters with art work can provide language to explore the ways that individuals make sense of experiences that challenge or exceed their usual sensory or cognitive norms (32).
Critical Play in Virtual Worlds
Critical play is an important tool for action research. Introduced by Mary Flanagan, critical play refers to a genre of interaction that harnesses the pleasure of play in order to communicate and raise awareness about difficult topics, such as social problems arising from implicit biases and stereotypes, and to create transformative models of institutions that overcome these issues in an imaginative space (189, 190). Critical play combines games and art making to provide a space for self-expression, as well as reformatting or re-skinning (changing the surface and the boundaries of a game be it in its aesthetics, dynamics, or mechanics), rewriting and subverting the rules of the play “shifting authority and power relations toward non-hierarchical, participatory exchange” [(189), p. 256]. Critical play also provides opportunities for meta-communication in which frames can be “toyed with” and the rules can be challenged, re-interpreted, and re-written by each person through an iterative process that evaluates their relation to other emerging themes [(189), p. 257].
Unlike goal-driven competitive games, the objectives in critical play are not winning, but rather the imagination, simulation, and communication of new, more suitable, or desirable modes of interaction with self, others, institutions, and the larger social order. For example, Bill of Health is a public-health board game in which players grapple with the dynamics of “accountable care” where fee-for-service is replaced by universal healthcare and the players must keep people healthier for an overall price whether they need an expensive surgery, or just smarter health coaching (https://tiltfactor.org/game/bill-of-health/). RePlay Health is another example of critical play in a role-playing game (for up to 25 participants) geared toward generating empathy in health policy makers. In this game, players assume the role of patients, care givers and policy makers to explore the healthcare costs through a range of “what if” scenarios (e.g., What if we paid healthcare providers differently? What if our hospitals ran more efficiently? What if everyone only went to the ER when they needed emergency care?) (https://tiltfactor.org/game/replay-health/) (191).
Virtual worlds such as Second Life (SL) or The Sims are examples of digital laboratories, where players construct an interactive environment with objects, avatars, and rules about how to socialize, trade, make and exhibit art, or disseminate knowledge. Because virtual worlds are highly customizable, participants can create imaginary institutions and places to be inhabited as anonymized or identifiable avatars, depending on the user's preferences. Virtual worlds such as SL provide an opportunity for critical play and simulated decision-making for example in nursing education, where resources or opportunities for creating physical encounters with diverse populations are not available (192–201).
Although digital play may be more limited than in-person play in terms of stimulating deeper conversations (202), the anonymity offered by the virtual world can increase participants' comfort and willingness to engage with research questions, with less concern about social desirability (203). For example, Nosek et al. deployed a pilot weight management intervention program in SL for women with mobility impairments, and demonstrated that while the intervention was feasible and effective it also created new research questions centered on the role of age, gender, and identity as barriers to access to weight loss programs, which could be better facilitated through anonymous avatar self-representations (204).
Conversations With Virtual Agents (Chatbots)
Chatbots can be operationalized across three axes: the illness (related to body-mind interactions or lifestyle); the psychology (behavioral monitoring and motivation, affective and cognitive decision-making); and community (connection, personalization, scalability) (205). There is important potential for playful communication with chatbots based on the development of pictorial media in recent years (emoticons, and more recently gif memes) which are creating a new, more universal language of communication (206–209). The usefulness of chatbots as a digital strategy for healthcare has been demonstrated in the detection of suicidal ideation (210), personalized patient education (211, 212), and for qualitative study of patient behaviors (213), or treatment outcomes (214).
Interacting with computerized agents has been found to be conducive to “opening up” (215). Bickmore and colleagues have shown that adding relational skills (empathy, dialogue, non-verbal intimacy, and maintenance of a social and collaborative relationship) to chatbots increased user engagement in a palliative care setting (216). Lucas et al. showed that among active-duty military service members (who were reluctant to disclose their post-deployment health conditions), the anonymity—and, importantly, the rapport—created with a virtual human communicating via online chat was associated with revealing more post-traumatic symptoms than in traditional in-person interviews (217).
An example of a playful clinical chatbot is Woebot, a humorous motivational and information delivery about depression. In a study testing Woebot with 34 users (who used Woebot to become mindful of their mood) compared to 36 matched controls (who used the handbook of the National Institutes for Mental Health), Fitzpatrick et al. found that depression symptom scores among Woebot users were significantly improved after 2 weeks of use (218).
Chatbots can be deployed for critical play as well. Rice et al. illustrated the value of SL in helping oncology nurses cope with grief in a virtual story-telling environment which did not exist in the personal and professional lives of the grieving nurses (219). Yu and colleagues compared the efficacy of real-time counseling in SL to synchronous face-to-face communication and to asynchronous communication via emails and chatrooms. They found that SL and computerized asynchronous counseling were rated more positively than face-to-face communication for providing anonymity, privacy, diversity of choices for self-representation and environmental personalization, as well as for convenience of time and place of delivery (220).
Pitfalls of Play
All media—including playful ICTs—reproduce roles, norms and values derived from cultural contexts (221). Culture also drives who plays what and how (222). This means that any specific approach to play is unlikely to be equally successful in capturing the attention of (and therefore interactions with) diverse individuals. For example, the emphasis on the developmental role of play as an exploratory activity essential for children, can make adults less open to engaging with play unless it is tied to a quantifiable benefit (223, 224). For some, the frame of play may convey a lack of seriousness that undermines the urgency of health problems. In the present instance, the notion of “playing the pain” may itself be construed as a dismissive attitude toward the reality of someone's suffering and undermine efforts to obtain adequate medical care. Thus, working definitions of play (what, how, and why) that respect the priorities and concerns of participants are critical in developing frameworks that engage adults with chronic pain or other health problems.
Competitive games can be engaging for adults both individually and in groups. In Reality Is Broken: Why Games Make us Better and How they Can Change the World, Jane McGonigal argues that when we create a simulated environment where players can experiment with various no-cost approaches to solving a problem, we stimulate cooperation among members of the same side to resolve conflicts with opponents (225). In such an approach, activities and interactions are often re-contextualized to include game elements such as points, scores, and rewards that quantify a win.
However, Rey and Bogost criticize the use of play to create virtual commodities and subjects who desire them, because it risks perpetuating a system of social control in which the virtual tokens of reward or achievement metrics replace the real-world resources needed by players (226, 227). The objective of “winning over” rather than “living-with” pain valorizes mastery rather than adaptation (228, 229). As Rilla Khaled has noted, “differentiation and social recognition make sense in mastery-and achievement-focused cultures. […] But in egalitarianism and harmony-oriented cultures […] successful individuals are expected to downplay and de-emphasize their achievements” (p. 308). Even when gamification encourages a community of participants to support and motivate one another, the emphasis on achievement will create hierarchies of success and popularity that can jeopardize community cohesion (230).
A major risk with digitization of play is that it can distort reality without the fully informed awareness and participation of the player. Computational algorithms can offer a narrow space of interactivity to make decisions and take action. This risks turning the play space into a system that forces conformity (231). This goes against the ethics of participatory research. Sicart posits that “the ethical game is not that which evaluates the players' actions according to predetermined moral systems embedded in the game, but that in which the ethics of the game experience and all its elements are reflected on and visible in the game design, in the game experience, and in the game community” (232).
If play is not properly framed, it can also create unintended conflicts—especially if it challenges dominant social norms or moral rules (233, 234). Among the risks of digital media and play that have been identified are stigmatization through social media (235), cyberbullying in massive multiplayer online games (236), and compulsive behavior in Internet gaming disorders (236–238). The challenge in implementing a playground for health research then is developing a mode of interaction that is flexible enough to maximize inclusive participation and leaves room for potential conflicts that arise from divergent views, but provides a frame in which the limits of play are explained and maintained through a shared commitment to creating a safe space for exchange (239).
Dispora: A Digital Strategy for Play-Oriented Research and Action
What Is DiSPORA?
DiSPORA is a framework to enable large-scale qualitative research through a digital playground that can be used as a platform for citizen science (specifically, to explore psychosocial and cultural determinants of pain). DiSPORA is grounded in Bateson's cybernetic model, which emphasizes the need to capture the interplay between observable phenomenon and explanatory constructs in order to understand underlying mechanisms that give rise to complex conditions like chronic pain (Figure 1). DiSPORA aims to use play as a way to step outside some of the double-binds that beset chronic pain care (e.g., hard to escape conflicts related to the cost of care vs. cure, the dualism in herent in biomedical vs. psychological explanations, and cultural attitudes toward pain or pleasure—most obviously manifested in the stigmatization of medications associated with addiction). Pain research needs innovative approaches to capture diverse perspectives on these issues. To respond to this need, DiSPORA is designed to serve as a citizen science laboratory for studying the psychosocial aspects of pain experience.
According to Thomas, Scheller and Schroder, a citizen laboratory for social research must offer: (1) a space for social encounters; (2) a frame for communicative practice; (3) a process to initiate social self-understanding; (4) and dynamics that allow participants to engage in and counter public discourse (71). However, pain is also a biomedical condition and, as such, collecting quantitative data is important to conduct analyses that establish the correlations between psychosocial determinants of pain experience and the outcome of interventions. DiSPORA therefore includes a database that can store different data types actively provided by participants (quantitative, narrative, and multimedia) as well as algorithms that passively capture interactions of participants within the playground through the user interface. Ethical data collection requires consent, and DiSPORA includes a procedure to obtain informed consent to participate in pain research that can be tailored to specific projects (see Table 2).
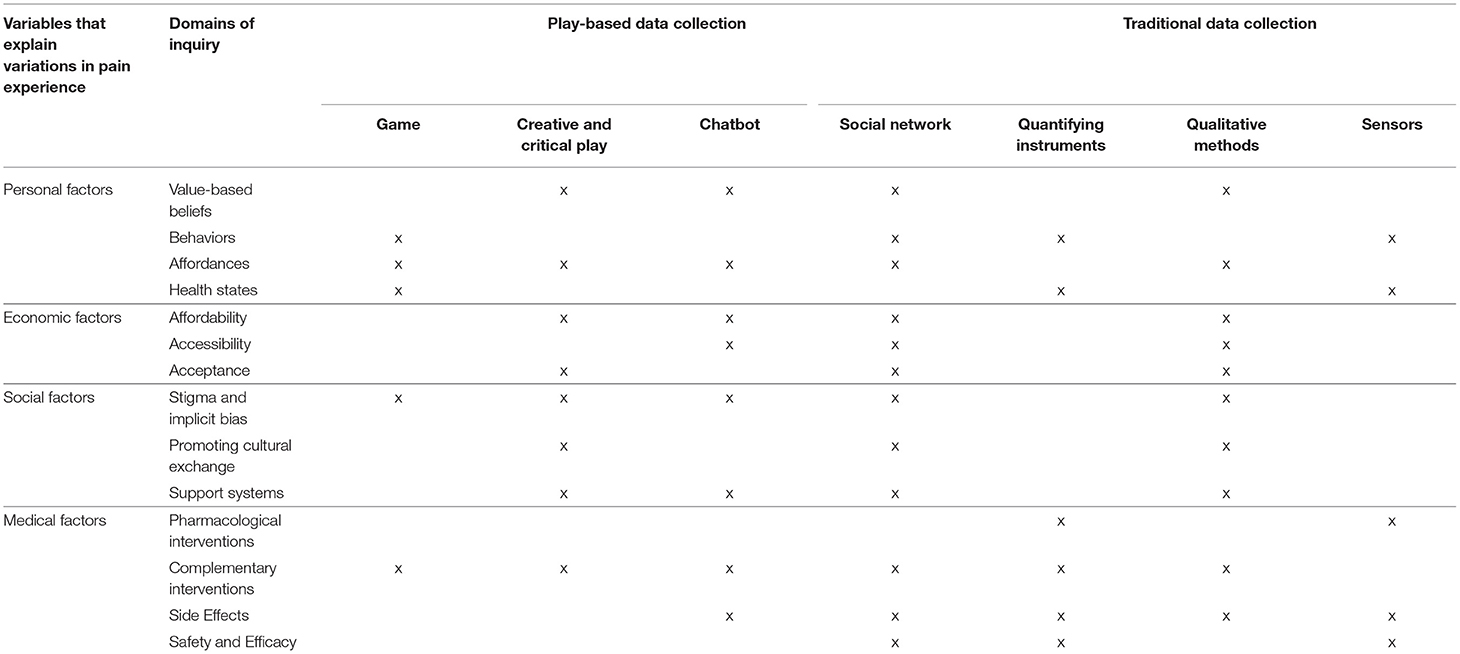
Table 2. Research questions, domains of inquiry and potential modes of data collection about factors that influence chronic pain experience and treatment.
To accommodate self-understanding in a personal and social context, DiSPORA incorporates features from pain diaries that have been used to self-track pain more ecologically, in order to refine the taxonomy of pain disorders, and optimize treatment, based on the psychological and temporal profile of pain experiences (240–242). It includes features such social networking and chatbots to enable collecting communicative data from conversations, narratives, or semi-structured interviews. More importantly, it includes different types of games that may be structured and goal driven (e.g., serious games designed for alleviating pain), or open-ended critical play that allows users to reconfigure and challenge dominant systems of knowledge creation or care in virtual worlds or through creative self-expression. In both cases, the users have the opportunity to critically engage with presumptive discourses (e.g., distraction by game A is analgesic, or care system B is efficient).
As a citizen laboratory, DiSPORA aims to: (1) increase participation of those who may be excluded from research because of geographic location, language skills, lack of recognition of diversity in knowledge and experience, or concern about stigma; (2) enable users to use digital tools (games, surveys, algorithms) to record data from the effects of non-pharmacological interventions that can be delivered or facilitated by digital media (e.g., self-expressive creative arts, serious games, or social networking); and (3) provide opportunities for critical play to reflect on and reconfigure the components and structures of care toward developing a collective action-plan. As such, DiSPORA can be deployed in N = 1 studies (e.g., an individual exploring the impact of different gamified therapeutic interventions on their own pain experience), focus-group studies (e.g., a group of researchers and patient partners collaborating through critical playing or storytelling), or hypothesis-driven experiments (e.g., comparing the effects of two interventions to alleviate pain in a large group, while gathering feedback and conducting interviews online).
Key Dimensions of DiSPORA
Framed and Flexible Experimentation Through Play
DiSPORA is framed as a digital playground that can include different tools, such as sensors, questionnaires, or algorithms for computational or statistical data generation and analysis. It can also have different implementations of play to generate different types of data. For example, games can be used for tracing behaviors of users, while interacting with the information and training modules in the game. Virtual worlds can foster creative self-expression or critical play around specific questions (for example by role playing, or construction of new spaces).
In the interpretation of these types of data, the impacts of both frame and flexibility need to be considered. In Play Matters (243), Miguel Sicart notes the flexibility of digital forms of play which reflects the ways that they: facilitate the storage and processing of large amounts of data in real-time; have a modular organization that can incorporate diverse modes of data capture such as video, audio, text, sensors (which also can be used to overcome barriers of language); and allow multiple agents to interact with the system in different ways (e.g., in multiplayer games or social networks). Digital forms of play can be deployed on both small and large scales, and personalized to varying extents (e.g., through choice of characters, levels of interaction, and modes of engagement, language, aesthetics). Of course, all digitized spaces are constrained by a more or less rigid frame imposed by computational logic. This makes it possible to do observational research by capturing variations in the ways the people interact with the digital playground and to conduct experiments by introducing small modifications (243, 244). Allowing participants to modify the frame can introduce another level of knowledge generation through active exploration.
Figure 3 provides a schematic diagram of some of the ways that play can be deployed for data generation (What games do people select to play? With whom? How do they play it?) and a mindset (Why do people select specific games? Do they follow—or break—the rules?). Table 2 provides a summary of the dimensions of experience that can be explored with DiSPORA and multiple modes of data collection, that can be triangulated to improve reliability and find better answers to specific questions (245).
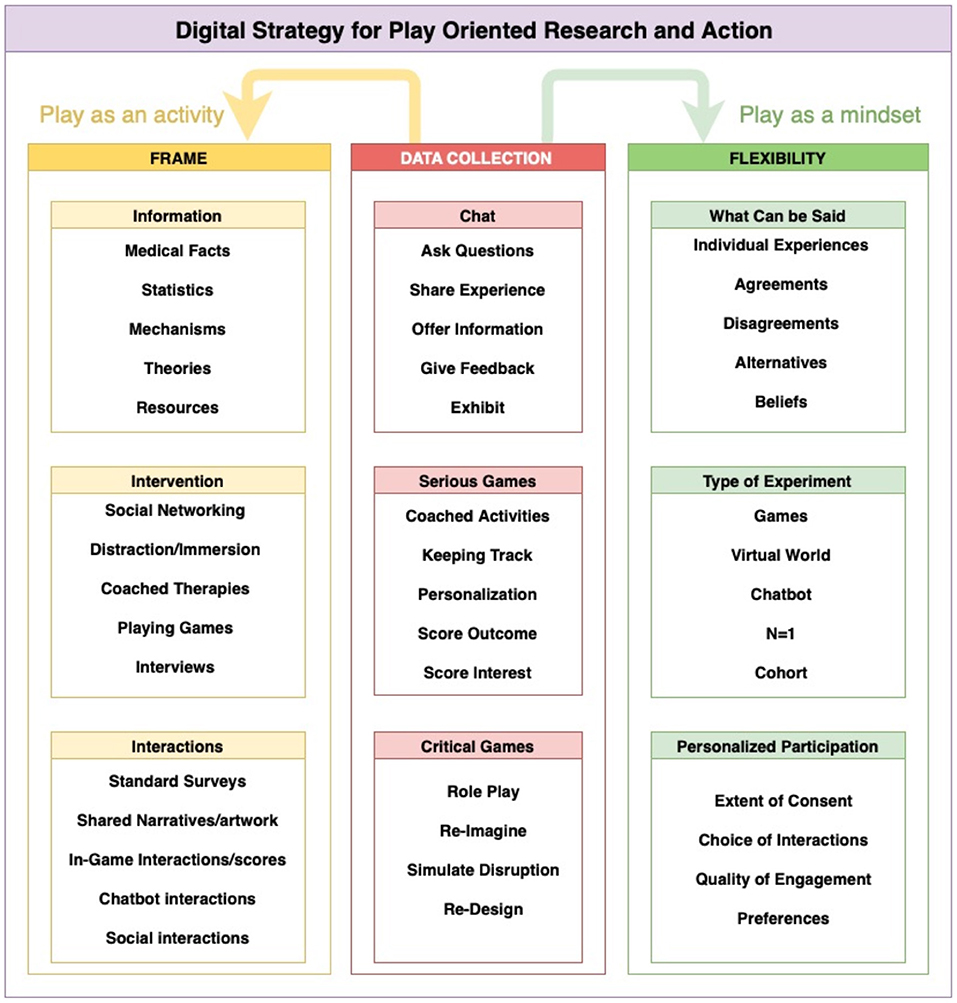
Figure 3. A schematic representation of DiSPORA. Set up similarly to a science museum, the DiSPORA research environment is framed by a set of digitally implemented modules that provide information, offer tools for experimenting with suggested interventions, and capture data from interactions. Play is implemented as a strategy for data collection, encouraging a playful mindset (playing with different ideas) and providing a framework for activities (chatbots, serious games, simulated worlds). The system is designed to be flexible, allowing participants to share ideas or beliefs, decide on the type of experimentation and knowledge generation, select activities, and choose the type and extent of data-sharing they prefer and for which they give explicit consent.
Person-Centered but Socially Oriented
An important requirement in the implementation of DiSPORA is to make it person-centered—i.e., to respect the validity of the subjective experiences and personal knowledge of each individual. In a meta-analysis of 29 qualitative studies investigating the experiences of patients in patient-centered care models, Winsor et al. found that patients' level of participation was linked to support systems that strengthened their skills for communication of their personal health beliefs, and that recognized their autonomy in self-management (246). In Coping With Illness Digitally (247), Stephan Rains reviews evidence to show that meaningful communication and social networking are the most important affordances of ICTs in healthcare. For patients, ICTs can increase visibility (making one's self known to others, and vice versa), availability (overcoming the barriers of distance, time, and cost), control (the ability to limit interactions and exposure), and reach (including the potential for selective outreach to relevant groups or individuals). In a playground model, each individual's experience is personalized through their decision to engage in certain activities, but the activities occur in a shared virtual space. This shared space offers opportunities to observe and interact with others, co-learn, offer feedback, or share narratives. The modular structure of DiSPORA makes it possible for participants to suggest changes that will improve the playground to better meet their needs.
Inclusive and Tolerant of Conflicting Views
A goal in designing DiSPORA is to contribute to equity in health research and practice by enabling participants from diverse cultural backgrounds to contribute knowledge based on their health experiences and perspectives. Structural inequities in society have led to systematic biases in research participation, design, sampling, and measurement. These include biases in what forms of knowledge production and authority are recognized, which can result in what Fricker has termed epistemic injustice (27, 97, 98). Therefore, it is expected that in a social and interactive space that invites feedback and personal narrative, conflicts will emerge. However, as Bergold and Thomas have argued, creating a situation that tolerates conflictual views also creates conditions for valuable self-reflexivity and negotiation to advance research (248).
Similarly to our proposal, Thomas et al. have argued that meta-communication provides a path forward in resolving conflicts in participatory citizen research projects (71). This requires that the users of DiSPORA are made aware of the risks of such conflicts, and consent to play to communicate (rather than to receive pain “therapy” or “find a winning solution”). Therefore, to ensure self-reflexive mediation of conflicts, DiSPORA needs to have professionally facilitated or moderated dialogues to ensure that stakeholders engage with one another without a vocal minority or the forceful majority silencing any participant's unique experiences and perspectives.
A Prototype of DiSPORA
In line with DiSPORA, as proof of principle, we have recently developed an app (PlaythePain.com) to examine the affordances of playful, creative and social activities in a digital citizen laboratory (86). The app is designed to serve as a participatory citizen science laboratory, and respect individual differences in focus, interests, modes of self-evaluation, self-expression, and self-care. As such, a range of customization features are available to allow users to select what to play, what data to share, and with whom. This prototype has been launched in both English and French (and, with the exception of the chatbot, it strives to communicate visually; see Figure 4). In this pilot project, we have included five features:
• Talk: An chatbot that encourages reflection and allows semi-structured qualitative data collection about various aspects of daily experiences;
• Track: A digital pain diary to record information about sleep, activities, feelings, and medication;
• Share: A restricted social network that allows users to create a gallery of their stories, artwork, and videos about various activities or experiences that they wish to share with other participants;
• Play: A library of different mHealth-mediated interventions (diet, exercise, brain training), as well as games. A default set is available initially, but users have the ability to add their own games and linked apps as well;
• Report: A comprehensive report of all data collected within the app, transparently available to the user which can be shared only if they grant access to a designated research-partner.
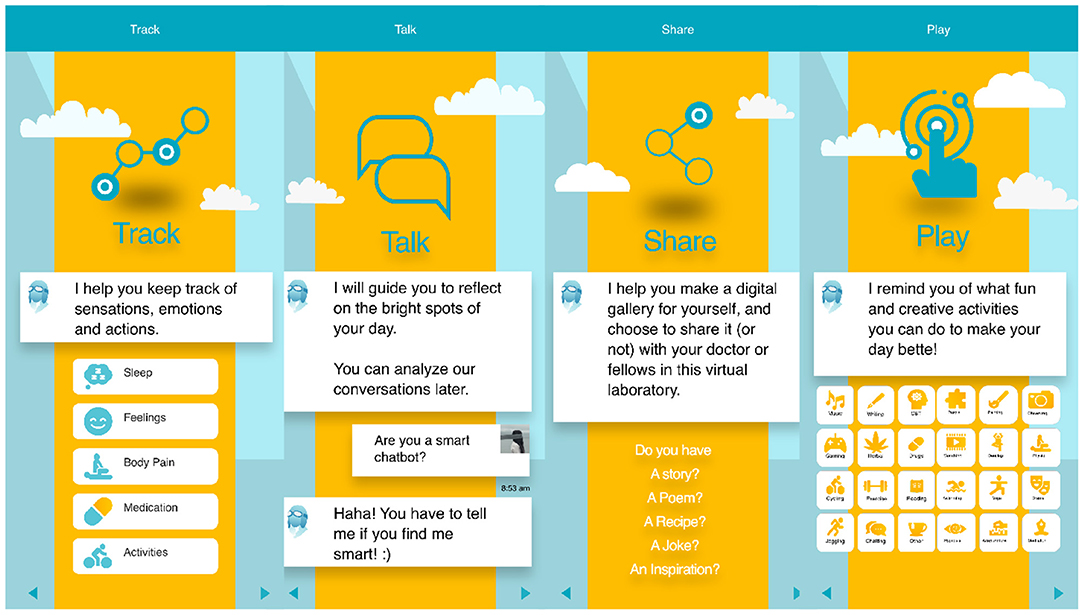
Figure 4. Features of PlaythePain App. The app allows uses to track their pain experience in ways similar to conventional pain diaries. Data-generation via play is supported by features including: Talk, where an interactive chatbot encourages conversations about various topics which the player selects; Share, a social-media like forum for sharing art and ideas; and Play, a catalog of various playful activities that are coached through third-party applications, either suggested by researchers or introduced to the forum by participants.
Individuals can join this platform anonymously (by registering via email) and after signing the terms and conditions that emphasize the need to adhere to social norms and behave courteously in socialization with other users. Users are unrestricted in the content of their conversation with chatbots, or in sharing private stories which can be mined in the future for the purpose of research. In future work, we plan to test and integrate this version of Play the Pain in our local neuroinformatics ecosystems (249).
How DiSPORA Could Serve as a Tool for Participatory Health Research
Medical care faces the challenge of understanding the complex interactions between brain, person, and environment that give rise to problems like chronic pain as well as the processes of healing and recovery (137, 250). Precision medicine and psychiatry aim to replace one-size-fits-all models in healthcare with more tailored, personalized approaches that consider biology, behavior and environmental context (251). A growing body of evidence demonstrates that environmental and psychosocial factors that affect brain plasticity also impact on physical health throughout the lifespan (252). This points to the need for a multilevel (bio-psycho-social) framework that encompasses the physiological, psychological, and social processes that are constitutive of experience in health and illness (29, 30). To date, however, precision medicine has focused primarily on biological factors which are assessed with laboratory measures.
Patients, patient-advocacy groups, nurses and social workers, and qualitative public health researchers have played an important role in shifting healthcare from a purely medical model to one that is person-centered (29, 30), involving patients in clinical decision-making, and self-management (135). Considering the patient as a person in a social context or life world can help address issues of diversity and representativeness in health research, including differences associated with gender, ethnicity, education, and social class and their intersections (78–80, 137).
One way to address the limitations of the narrow biological approach is to democratize knowledge-creation by empowering patients to take charge of their evaluation and the development and delivery of interventions informed by their lived experience (74–76). This can be achieved through cooperative participation of various stakeholders in a process that gives everyone, especially those who are marginalized, a voice to contribute to research and policy-making through knowledge-sharing and co-learning (40, 77). The value of such patient empowerment approaches has long been recognized in public health (77), particularly in efforts to address the social determinants of health (78, 79).
However, methodological challenges related to rigorous data gathering (38), communication (39), and inclusivity (40) limit the use of qualitative research practices in large-scale health research. In the section above on Integrating Context and Experience in Pain Research we suggested some ways in which ICTs can benefit such research, and in section The Promise of Information and Communication Technologies (ICT) for Integrative Pain Research, we listed the shortcomings of existing implementations of ICT in health research. DiSPORA proposes to overcome some of these limitations by creating a framework for capturing participants' perspectives through a scalable framework that takes advantage of the affordances of play as a meta-communication strategy (32, 205, 225, 243, 247) in a citizen science participatory research laboratory (47, 48, 53, 71, 169). Of course, in itself, the use of DiSPORA does not establish the conditions necessary for participatory research. Achieving true participation requires setting up and maintaining essential protocols and structures of governance for processes of partnership and collaboration that are well-described in the literature on participatory health research (69–73).
Conclusion
Main Arguments
Medical researchers are increasingly aware of the need for qualitative and participatory research to inform policy and clinical practice. To help address this need, our interdisciplinary team of clinicians, social scientists, bioethicists, designers, and computer scientists developed an innovative ICT framework for knowledge generation in chronic-pain research.
Examining chronic pain from the perspective of the Neuromatrix Pain Theory (9), Pain Communication Theory (15), Cultural Somatization Theory (87), and person-centered action-research in chronic pain (23, 32, 37), we asked whether and how ICTs can improve research that can integrate these theories. We adapted Bateson's cybernetic approach to studying mind-body processes in ecosocial context. In Bateson's cybernetic model, the links between the observable phenomena and underlying mechanisms are mediated by culturally contextualized explanatory factors. We also identified some double binds (inescapable tensions or conflicts) that need to be addressed in pain research involving issues that are structural (investing in care vs. cure), pragmatic (investing in biomedical vs. psychosocial), and cultural (moralizing attitudes toward pain and pleasure).
We adapted play (a mode of communication, simulated action or performance, and creative disruption) as a framed but flexible research tool for meta-communication and for recursive knowledge generation about pragmatic, structural, and cultural conflicts in pain research. To clarify the potential uses of play in research, we reviewed evidence suggesting that playing games, role-playing in virtual worlds, engaging in creative arts and self-expression (e.g., through talking to chatbots or social networking) offer opportunities for passive and active data generation.
Finally, we proposed a model for operationalizing play in citizen science research we call DiSPORA. Drawing inspiration from the design of science museums, DiSPORA provides a digital playground that includes interactive information delivery, games, social networks, virtual chatbots, and simulated virtual worlds. Participant interactions with DiSPORA are facilitated to ensure that data is captured in ways that are safe and inclusive. The key elements of DiSPORA are: a clear but flexibile frame; person-centered but enabling sociability; and tolerance for diversity and inclusivity. A simple prototype app has been constructed to illustrate how this citizen lab could be implemented.
Limitations and Next Steps
DiSPORA is a proposal for how to design an ICT framework to engage patients as active participants in studying diverse psychosocial questions that arise in relation to their healthcare needs. However, in itself, a framework does not ensure the social relationships, ethical commitments, or organizational structures and procedures that are necessary for participatory research and action.
Although we think that the modular design of DiSPORA can serve as a flexible frame for citizen research, the fact that DiSPORA is governed by its computational logic may limit its ability to capture important dimensions of experience not built into its algorithms. The social networking and collaboration that can be enabled by DiSPORA might allow stakeholders to tailor it to their own research questions and needs. However, recent global experiences with social media raise concerns about the risks of disseminating misinformation, or exacerbating bias and stigma through ingroup/outgroup dynamics. In addition, important ethical issues related to privacy, individual recognition, and data sovereignty remain to be addressed (253). These are important research questions that can be explored in the collaborative refinement of DiSPORA applications through an agile recursive design process (254).
Finally, reliance on digital media and play to engage people in exploring the quality, parameters, and modulators of their pain experience is based on the assumption that play can afford people some distance from the suffering associated with their health problem, while mobilizing both coping strategies and social connection to others. Whether these characteristics of play can be maintained through interaction with a digital citizen lab remains to be tested. However, our own recursive learning process in developing this concept and feedback from peer reviewers have provided encouragement and valuable lessons about reaching consensus on the basic requirements for research that respects individual and diverse ways of knowing and knowledge generation.
Author Contributions
NK-M, TG, and MR conceptualized the Play the Pain project. NK-M, EH, and SW conducted the research. NK-M, EH, SW, LK, RK, BS, ML, MN, and RH contributed to the analysis and co-wrote the paper. AD and JT-B provided expert advice on clinical and community practices of care, respectively. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by a grant from the Quebec Research Funds to NK-M (FRQSC-AUDACE), additionally supported by MCIN (McGill University), Milieux Institute for Art, Culture and Technology, PERFORM Center (Concordia University), and the Healthy Brains for Healthy Lives Program (CFREF, McGill University).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Drs. Lynn Hughes, Chris Salter, Linda Booij, Thien-Thanh Dang-Vu, Rosanna Maule, and Marie-Paule Grimaldi for their feedback during conceptualization of Play the Pain project (playthepain.com).
References
1. Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(18)32279-7
2. Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. (2020) 8:299. doi: 10.21037/atm.2020.02.175
3. Wright P, Walsh Z, Margolese S, Sanchez T, Arlt S, Belle-Isle L, et al. Canadian clinical practice guidelines for the use of plant-based cannabis and cannabinoid-based products in the management of chronic non-cancer pain and co-occurring conditions: protocol for a systematic literature review. BMJ Open. (2020) 10:e036114. doi: 10.1136/bmjopen-2019-036114
4. Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults — United States, 2016. MMWR Morbidity Mortal Weekly Rep. (2018) 67:1001–6. doi: 10.15585/mmwr.mm6736a2
5. Shupler MS, Kramer JK, Cragg JJ, Jutzeler CR, Whitehurst DGT. Pan-Canadian estimates of chronic pain prevalence from 2000 to 2014: a repeated cross-sectional survey analysis. J Pain. (2019) 20:557–65. doi: 10.1016/j.jpain.2018.10.010
6. Melzack R. Pain and theneuromatrix in the brain. J Dent Educ. (2001) 65:1378–82. doi: 10.1002/j.0022-0337.2001.65.12.tb03497.x
7. Naranjo-Hernández D, Reina-Tosina J, Roa LM. Sensor technologies to manage the physiological traits of chronic pain: a review. Sensors. (2020) 20:365. doi: 10.3390/s20020365
8. Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. (2013) 14:502–11. doi: 10.1038/nrn3516
9. Melzack R. Pain–an overview. Acta Anaesthesiol Scand. (1999) 43:880–4. doi: 10.1034/j.1399-6576.1999.430903.x
10. Ahn H, Weaver M, Lyon D, Choi E, Fillingim RB. Depression and pain in asian and white americans with knee osteoarthritis. J Pain. (2017) 18:1229–36. doi: 10.1016/j.jpain.2017.05.007
11. Olango WM, Finn DP. Neurobiology of stress-induced hyperalgesia. behavioral neurobiology of chronic pain. Curr Top Behav Neurosci. (2014) 20:251–80. doi: 10.1007/7854_2014_302
12. Haywood C, Diener-West M, Strouse J, Carroll CP, Bediako S, Lanzkron S, et al. Perceived discrimination in health care is associated with a greater burden of pain in sickle cell disease. J Pain Symptom Manage. (2014) 48:934–43. doi: 10.1016/j.jpainsymman.2014.02.002
13. Edwards RR. The association of perceived discrimination with low back pain. J Behav Med. (2008) 31:379–89. doi: 10.1007/s10865-008-9160-9
14. Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am J Public Health. (2007) 97:1275–82. doi: 10.2105/AJPH.2006.091827
15. Craig KD. The social communication model of pain. Canad Psychol/Psychol Canad. (2009) 50:22–32. doi: 10.1037/a0014772
16. Kirmayer LJ, Young A. Culture and somatization. Psychosom Med. (1998) 60:420–30. doi: 10.1097/00006842-199807000-00006
17. Kirmayer LJ. Culture and the metaphoric mediation of pain. Transcult Psychiatry. (2008) 45:318–38. doi: 10.1177/1363461508089769
18. Kirmayer LJ. Culture, affect and somatization. Transcult Psychiatric Res Rev. (2016) 21:159–88. doi: 10.1177/136346158402100301
19. Kirmayer LJ. Unpacking the placebo response: Insights from ethnographic studies of healing. In: Raz A, Harris CS, editors. Placebo Talks: Modern Perspectives on Placebos in Society. Oxford University Press (2016). p. 119–43. doi: 10.1093/acprof:oso/9780199680702.003.0008
20. Hadjistavropoulos T, Craig KD, Duck S, Cano A, Goubert L, Jackson PL, et al. A biopsychosocial formulation of pain communication. Psychol Bull. (2011) 137:910–39. doi: 10.1037/a0023876
21. Good MJ, Hannah SD. “Shattering culture”: perspectives on cultural competence and evidence-based practice in mental health services. Transcult Psychiatry. (2015) 52:198–221. doi: 10.1177/1363461514557348
22. Kirmayer LJ. Cultural competence and evidence-based practice in mental health: epistemic communities and the politics of pluralism. Soc Sci Med. (2012) 75:249–56. doi: 10.1016/j.socscimed.2012.03.018
24. Hadjistavropoulos H, Williams A, Craig K. Psychologicalinterventions: cognitive behavioral and stress management approaches. In: Lynch ME, Craig KD, Peng PWH, editors. Clinical Pain Management: A Practical Guide Chichester. Chichester: Wiley-Blackwell; John Wiley & Sons, Ltd (2011). p. 200–6. doi: 10.1002/9781444329711.ch24
25. Craig KD, Versloot J. PsychosocialPerspectives on Chronic Pain. Clinical Pain Management. Chichester: Wiley-Blackwell; John Wiley & Sons, Ltd. (2010). p. 24–31. doi: 10.1002/9781444329711.ch4
26. Katapally TR. The SMART framework: integration of citizen science, community-based participatory research,and systems science for population health science in the digital age. JMIR mHealth uHealth. (2019) 7:e14056. doi: 10.2196/14056
27. Williams G. Explainingepistemic injustice in medicine: tightrope walking, double binds, paths of least resistance and the invisibility of power positions to those who occupy them. Europ J Person Centered Healthcare. (2020) 8:323–35. doi: 10.5750/ejpch.v8i3.1861
28. Craig KD. Towardthe social communication model of pain. In: Vervoort T, Karos K, Trost Z, Prkachin K, editors. Social and Interpersonal Dynamics in Pain. Cham: Springer (2018). p. 23–41. doi: 10.1007/978-3-319-78340-6_2
29. Mintzberg H. Managing the Myths of Health Care : Bridging the Separations Between Care, Cure, Control, and Community. 1st ed. Oakland, CA: Berrett-Koehler Publishers, Inc. (2017) viii, 262 pages p. doi: 10.1007/978-3-319-53600-2_1
30. Darnall BD, Carr DB, Schatman ME. Pain psychology and the biopsychosocial model of pain treatment: ethical imperatives and social responsibility. Pain Med. (2016) 18:1413–5. doi: 10.1093/pm/pnw166
31. Sylliboy JR, Hovey RB. Humanizing Indigenous Peoples' engagement in health care. CMAJ. (2020) 192:E70–2. doi: 10.1503/cmaj.190754
32. Hovey RB, Khayat VC, Feig E. Listening to and letting pain speak: poetic reflections. Br J Pain. (2018) 12:95–103. doi: 10.1177/2049463717741146
33. Kerns RD, Brandt CA, Peduzzi P. NIH-DoD-VA pain management collaboratory. Pain Med. (2019) 20:2336–45. doi: 10.1093/pm/pnz186
34. Nugraha B, Gutenbrunner C, Barke A, Karst M, Schiller J, Schäfer P, et al. The IASP classification of chronic pain for ICD-11. Pain. (2019) 160:88–94. doi: 10.1097/j.pain.0000000000001433
35. van Velzen M, Dahan A, Niesters M. Neuropathic pain: challenges and opportunities. Front Pain Res. (2020) 1:1. doi: 10.3389/fpain.2020.00001
36. Krebs EE, Carey TS, Weinberger M. Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med. (2007) 22:1453–8. doi: 10.1007/s11606-007-0321-2
37. Hovey RB, Amir N. The hermeneuticsof suffering: researching trauma. Int J Person Centered Med. (2013) 3:160–9. doi: 10.5750/ijpcm.v3i2.395
38. Campbell J. A critical appraisal of participatory methods in development research. Int J Soc Res Methodol. (2002) 5:19–29. doi: 10.1080/13645570110098046
39. Cook T. Where participatoryapproaches meet pragmatism in funded (Health) research: the challenge of finding meaningful spaces. Forum Qualitative Sozialforschung / Forum. (2012) 13. doi: 10.17169/fqs-13.1.1783
40. Dedding C, Goedhart NS, Broerse JEW, Abma TA. Exploring the boundaries of ‘good' Participatory Action Research in times of increasing popularity: dealing with constraints in local policy for digital inclusion. Educ Action Res. (2020) 29:20–36. doi: 10.1080/09650792.2020.1743733
41. Sandman L, Munthe C. Shared decision making, paternalism and patient choice. Health Care Anal. (2009) 18:60–84. doi: 10.1007/s10728-008-0108-6
42. Jibb LA, Khan JS, Seth P, Lalloo C, Mulrooney L, Nicholson K, et al. Electronic data capture versus conventional data collection methods in clinical pain studies: systematic review and meta-analysis. J Med Internet Res. (2020) 22:e16480. doi: 10.2196/16480
43. Kelly JT, Campbell KL, Gong E, Scuffham P. The internet of things: impact and implications for health care delivery. J Med Internet Res. (2020) 22:e20135. doi: 10.2196/20135
44. Insel TR. Digital phenotyping: technology for a new science of behavior. JAMA. (2017) 318:1215–6. doi: 10.1001/jama.2017.11295
45. Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. (2018) 6:149. doi: 10.3389/fpubh.2018.00149
46. Finucane AM, O'Donnell H, Lugton J, Gibson-Watt T, Swenson C, Pagliari C. Digital health interventions in palliative care: a systematic meta-review. Npj Digital Med. (2021) 4: 64. doi: 10.1038/s41746-021-00430-7
48. Okun S, Wicks P. DigitalMe: a journey towards personalized health and thriving. Biomed Eng Online. (2018) 17:119. doi: 10.1186/s12938-018-0553-x
49. Arigo D, Pagoto S, Carter-Harris L, Lillie SE, Nebeker C. Using social media for healthresearch: methodological and ethical considerations for recruitment and intervention delivery. Digital Health. (2018) 4:1–15. doi: 10.1177/2055207618771757
50. Ainley E, Witwicki C, Tallett A, Graham C. UsingTwitter comments to understand people's experiences of UK healthcare during the Covid-19 pandemic. J Med Internet Res. (2021) 23:e31101. doi: 10.2196/preprints.31101
51. Hu T, Wang S, Luo W, Zhang M, Huang X, Yan Y, et al. Revealing public opinion towards COVID-19 vaccines with Twitter data in the United States: a spatiotemporal perspective. J Med Internet Res. (2021) 23:e30854. doi: 10.2196/preprints.30854
52. Sanders AC, White RC, Severson LS, Ma R, McQueen R, Alcantara Paulo HC, et al. Unmasking the conversation on masks: natural language processing for topical sentiment analysis of COVID-19 Twitter discourse. AMIA Annu Symp Proc. (2021) 2021:555–64. doi: 10.1101/2020.08.28.20183863
53. Ybarra ML, Boyd D. Can clans protect adolescent players of massively multiplayer online games from violent behaviors? Int J Public Health. (2015) 60:267–76. doi: 10.1007/s00038-014-0637-8
54. Ienca M, Ferretti A, Hurst S, Puhan M, Lovis C, Vayena E. Considerations for ethics review of big data health research: a scoping review. PLoS ONE. (2018) 13:e0204937. doi: 10.1371/journal.pone.0204937
55. Kennedy H, Moss G. Known or knowing publics? Social media data mining and the question of public agency. Big Data Soc. (2015) 2:1–11. doi: 10.1177/2053951715611145
56. Martinez-Martin N, Insel TR, Dagum P, Greely HT, Cho MK. Data mining for health: staking out the ethical territory of digital phenotyping. NPJ Digit Med. (2018) 1:68. doi: 10.1038/s41746-018-0075-8
57. Mittelstadt BD, Floridi L. The ethics of big data: current and foreseeable issues in biomedical contexts. Sci Eng Ethics. (2016) 22:303–41. doi: 10.1007/s11948-015-9652-2
58. Maher NA, Senders JT, Hulsbergen AFC, Lamba N, Parker M, Onnela J-P, et al. Passive data collection and use in healthcare: a systematic review of ethical issues. Int J Med Inform. (2019) 129:242–7. doi: 10.1016/j.ijmedinf.2019.06.015
59. Spears Johnson CR, Kraemer Diaz AE, Arcury TA. Participation levels in 25 community-based participatory research projects. Health Educ Res. (2016) 31:577–86. doi: 10.1093/her/cyw033
60. Wicks P, Massagli M, Frost J, Brownstein C, Okun S, Vaughan T, et al. Sharing health data for better outcomes on PatientsLikeMe. J Med Internet Res. (2010) 12:e19. doi: 10.2196/jmir.1549
61. Kirmayer LJ, Mezzich JE, Van Staden CW. Health experience and values in person-centered assessment and diagnosis. In: Mezzich JE, Botbol M, Christodoulou GN, Cloninger CR, Salloum IM, editor. Person Centered Psychiatry. Springer International Publishing AG (2016). p. 179–99. doi: 10.1007/978-3-319-39724-5_14
62. Dickinson JL, Zuckerberg B, Bonter DN. Citizen science as an ecological research tool: challenges and benefits. Annu Rev Ecol Evol Syst. (2010) 41:149–72. doi: 10.1146/annurev-ecolsys-102209-144636
63. Schmaal L, Pozzi E, T CH, van Velzen LS, Veer IM, Opel N, et al. ENIGMA MDD: seven years of global neuroimaging studies of major depression through worldwide data sharing. Transl Psychiatry. (2020) 10:172. doi: 10.1038/s41398-020-0842-6
64. Smith SM, Douaud G, Chen W, Hanayik T, Alfaro-Almagro F, Sharp K, et al. An expanded set of genome-wide association studies of brain imaging phenotypes in UK Biobank. Nat Neurosci. (2021) 24:737–45. doi: 10.1038/s41593-021-00826-4
65. Mertz L. Sharing data to solve the autism riddle: an interview with Adriana Di Martino and Michael Milham of ABIDE. IEEE Pulse. (2017) 8:6–9. doi: 10.1109/MPUL.2017.2750819
66. Jack CR Jr., Bernstein MA, Fox NC, Thompson P, Alexander G, et al. The Alzheimer's Disease Neuroimaging Initiative (ADNI): MRI methods. J Magn Reson Imaging. (2008) 27:685–91. doi: 10.1002/jmri.21049
67. Das S, Glatard T, MacIntyre LC, Madjar C, Rogers C, Rousseau ME, et al. The MNI data-sharing and processing ecosystem. Neuroimage. (2016) 124:1188–95. doi: 10.1016/j.neuroimage.2015.08.076
68. Herrick R, Horton W, Olsen T, McKay M, Archie KA, Marcus DS. XNAT Central: Open sourcing imaging research data. Neuroimage. (2016) 124:1093–6. doi: 10.1016/j.neuroimage.2015.06.076
69. Fortuna K, Barr P, Goldstein C, Walker R, Brewer L, Zagaria A, et al. Application of community-engaged research to inform the development and implementation of a peer-delivered mobile health intervention for adults with serious mental illness. J Particip Med. (2019) 11:e12380. doi: 10.2196/12380
70. Senabre Hidalgo E, Perelló J, Becker F, Bonhoure I, Legris M, Cigarini A. Participation and Co-creation in Citizen Science. In: Vohland K, Land-Zandstra A, Ceccaroni L, Lemmens R, Perelló J, Ponti M, et al., editors. The Science of Citizen Science. Cham: Springer International Publishing (2021). p. 199–218. doi: 10.1007/978-3-030-58278-4_11
71. Thomas S, Scheller D, Schröder S. Co-creation in citizen social science: the research forum as a methodological foundation for communication and participation. Human Soc Sci Commun. (2021) 8:244. doi: 10.1057/s41599-021-00902-x
72. Wallerstein N, Duran B, Oetzel JG, Minkler M. Community-Based Participatory Research for Health : Advancing Social and Health Equity. 3rd ed. San Francisco, CA: Jossey-Bass, A Wiley brand (2018) xxxviii, 439 p.
73. Tritter JQ, McCallum A. The snakes and ladders of user involvement: moving beyond Arnstein. Health Policy. (2006) 76:156–68. doi: 10.1016/j.healthpol.2005.05.008
74. Fals-Borda O, Rahman MA. Action and Knowledge : Breaking the Monopoly With Participatory Action Research. New York, NY, London: Apex Press: Intermediate Technology Publications (1991). viii, 182.p.
75. Warriner DS, Bigelow M. Critical Reflections on Research Methods : Power and Equity in Complex Multilingual Contexts. Bristol: Blue Ridge Summit: Multilingual Matters (2019) xi, 200 p. doi: 10.21832/9781788922562
76. Wright MT, Hartung S, Bach M, Brandes S, Gebhardt B, Jordan S, et al. Impact and lessons learned from a national consortium for participatory health research: PartKommPlus-German Research Consortium for Healthy Communities (2015-2018). Biomed Res Int. (2018) 2018:5184316. doi: 10.1155/2018/5184316
77. Baum F. Participatory action research. J Epidemiol Commun Health. (2006) 60:854–7. doi: 10.1136/jech.2004.028662
78. Minkler M, Wallerstein N. Community-Based Participatory Research for Health : From Process to Outcomes. 2nd ed. San Francisco, CA: Jossey-Bass (2008). xxxv, 508. p.
80. Regitz-Zagrosek V. Sex and gender differences in health. EMBO Rep. (2012) 13:596–603. doi: 10.1038/embor.2012.87
81. Mandryk RL, Birk MV. The potential of game-based digital biomarkers for modeling mental health. JMIR Ment Health. (2019) 6:e13485. doi: 10.2196/13485
82. Mandryk RL, Birk MV. Toward game-based digital mental health interventions: player habits and preferences. J Med Internet Res. (2017) 19:e128. doi: 10.2196/jmir.6906
83. Re L, Birkhoff JM, Sozzi M, Andrello L, Osculati AM. The choking game: a deadly game. analysis of two cases of “self-strangulation” in young boys and review of the literature. J Forensic Leg Med. (2015) 30:29–33. doi: 10.1016/j.jflm.2014.12.008
84. Haak SW, Burton S, Birka AM, Carlin MA, Davey SS, Hujcs M. Clinical judgment: an instructional game for nursing. Nurse Educ. (1990) 15:11:20, 8.
85. Cheng D, Liu D, Philpotts LL, Turner DP, Houle TT, Chen L, et al. Current state of science in machine learning methods for automatic infant pain evaluation using facial expression information: study protocol of a systematic review and meta-analysis. BMJ Open. (2019) 9:e030482. doi: 10.1136/bmjopen-2019-030482
86. Holowka EM, Woods S, Pahayahay A, Roy M, Khalili-Mahani N. Principles for designing an mhealth app for participatory research and management of chronic pain. In: Duffy VG, editor. Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management AI, Product and Service. Lecture Notes in Computer Science (2021). p. 50–67. doi: 10.1007/978-3-030-77820-0_5
87. Jones N, Atterbury K, Byrne L, Carras M, Brown M, Phalen P. Lived experience, research leadership, and the transformation of mental health services: building a researcher pipeline. Psychiatric Serv. (2021) 72:591–3. doi: 10.1176/appi.ps.202000468
89. Montuori A. Gregorybateson and the promise of transdisciplinarity. Cybern Hum Knowing. (2005) 12:147–58.
90. Harries-Jones P. A Recursive Vision : Ecological Understanding and Gregory Bateson. Toronto, ON, London: University of Toronto Press (1995) 358. p.
91. Bateson G. Steps to An Ecology of Mind. Chicago, IL: University of Chicago Press (2000) xxxii, 533. p.
92. Beels C. Family Process 1962-1969. Fam Process. (2011) 50:4–11. doi: 10.1111/j.1545-5300.2010.01342.x
93. Visser M. Gregory Bateson on deutero-learning and double bind: a brief conceptual history. J Hist Behav Sci. (2003) 39:269–78. doi: 10.1002/jhbs.10112
95. Sluzki CE, Veron E. The double bind as a universal pathogenic situation. Fam Process. (1971) 10:397–410. doi: 10.1111/j.1545-5300.1971.00397.x
96. Thorne S. Patient-provider communication in chronic illness: a health promotion window of opportunity. Fam Commun Health. (2006). 29(1 Suppl):4S−11S. doi: 10.1097/00003727-200601001-00003
97. Buchman DZ, Ho A, Goldberg DS. Investigating trust, expertise, and epistemic injustice in chronic pain. J Bioeth Inq. (2017) 14:31–42. doi: 10.1007/s11673-016-9761-x
98. Groot B, Haveman A, Abma T. Relational, ethically sound co-production in mental health care research: epistemic injustice and the need for an ethics of care. Critic Public Health. (2020) 1–11. doi: 10.1080/09581596.2020.1770694
99. Alexander L. The double-bind between dialysis patients and their health practitioners. In: Eisenberg L, Kleinman A, editors. The Relevance of Social Science for Medicine. Dordrecht: Springer (1981). p. 307–29. doi: 10.1007/978-94-009-8379-3_14
102. Holowchak MA. freud on play, games, and sports fanaticism. J Am Acad Psychoanal Dyn Psychiatry. (2011) 39:695–715. doi: 10.1521/jaap.2011.39.4.695
105. Huizinga J. Homo Ludens; A Study of the Play-Element in Culture. London: Routledge & K. Paul (1949). 220. p.
106. Definition of Play [Internet]. Available online at: https://www.merriam-webster.com/dictionary/play (accessed August 1, 2021).
108. Sutton-Smith B. The Ambiguity of Play. Cambridge, MA: Harvard University Press (1997) x, 276. p.
109. Urien L, Wang J. Top-down cortical control of acute and chronic pain. Psychosom Med. (2019) 81:851–8. doi: 10.1097/PSY.0000000000000744
110. Kirmayer LJ, Bhugra D editors. Culture and Mental Illness: Social Context and Explanatory Models. In: Salloum IM, Mezzich JE, editor. Psychiatric Diagnosis: Patterns and Prospects. New York, NY: Wiley (2009). p. 29–40.
111. Bates MS, Rankin-Hill L, Sanchez-Ayendez M. The effects of the cultural context of health care on treatment of and response to chronic pain and illness. Soc Sci Med. (1997) 45:1433–47. doi: 10.1016/S0277-9536(97)00068-3
112. Cohen M, Quintner J, Buchanan D, Nielsen M, Guy L. Stigmatization of patients with chronic pain: the extinction of empathy. Pain Med. (2011) 12:1637–43. doi: 10.1111/j.1526-4637.2011.01264.x
113. Kleinman A. The Illness Narratives: Suffering, Healing, and the Human Condition. Ann Arbor: The University of Michigan Press (1988).
114. Good M-JD. Pain as Human Experience : An Anthropological Perspective. Berkeley; London: University of California Press (1992) vii, 214. p.
115. Jackson JE. Stigma, liminality, and chronic pain: mind-body borderlands. Am Ethnol. (2005) 32:332–53. doi: 10.1525/ae.2005.32.3.332
116. Collier R. “Complainers, malingerers and drug-seekers” — the stigma of living with chronic pain. Canad Med Assoc J. (2018) 190:E204–5. doi: 10.1503/cmaj.109-5553
117. Whorton JC. Nature Cures : The History of Alternative Medicine in America. Oxford; New York, NY: Oxford University Press (2002) xv, 368. p.
118. Preuss CV, Kalava A, King KC. Prescription of Controlled Substances: Benefits and Risks. Treasure Island, FL: StatPearls (2020).
119. Fenton JJ. The cost of satisfaction. Arch Intern Med. (2012) 172:405–11. doi: 10.1001/archinternmed.2011.1662
120. Jones W, Kurdyak P, Fischer B. Examining correlations between opioid dispensing and opioid-related hospitalizations in Canada, 2007–2016. BMC Health Serv Res. (2020) 20:677. doi: 10.1186/s12913-020-05530-w
121. Wadman M. Row over alternative medicine's status at NIH. Nature. (1997) 389:652. doi: 10.1038/39409
122. Albrecht H. Alternative medicine in Germany. In: Willich SN, Elm S, editors. Medical Challenges for the New Millennium. Dordrecht: Springer Science+Business Media (2001). p. 39–46. doi: 10.1007/978-94-015-9708-1_4
123. Joos S, Musselmann B, Szecsenyi J. Integration of complementary and alternative medicine into family practices in germany: results of a national survey. Evidence-Based Complement Alternat Med. (2011) 2011:1–8. doi: 10.1093/ecam/nep019
124. Vos R, Willems D, Houtepen R. Coordinating the norms and values of medical research, medical practice and patient worlds-the ethics of evidence based medicine in orphaned fields of medicine. J Med Ethics. (2004) 30:166–70. doi: 10.1136/jme.2003.007153
125. Webster LR. The Painful Truth : What Chronic Pain is Really Like and Why it Matters to Each of Us. New York, NY: Oxford University Press (2016). doi: 10.1093/med/9780190659721.001.0001
126. Miresco MJ, Kirmayer LJ. The persistence of mind-brain dualism in psychiatric reasoning about clinical scenarios. Am J Psychiatry. (2006) 163:913–8. doi: 10.1176/ajp.2006.163.5.913
127. Kirmayer LJ, Gómez-Carrillo A. Agency, embodiment and enactment in psychosomatic theory and practice. Med Humanit. (2019) 45:169–82. doi: 10.1136/medhum-2018-011618
128. Kirmayer LJ, Sartorius N. Cultural models and somatic syndromes. Psychosom Med. (2007) 69:832–40. doi: 10.1097/PSY.0b013e31815b002c
129. Jimenez N, Garroutte E, Kundu A, Morales L, Buchwald D. A review of the experience, epidemiology, and management of pain among american indian, alaska native, and aboriginal canadian peoples. J Pain. (2011) 12:511–22. doi: 10.1016/j.jpain.2010.12.002
130. Goldberg DS. Pain, objectivity and history: understanding pain stigma. Med Humanit. (2017) 43:238–43. doi: 10.1136/medhum-2016-011133
131. Malmusi D, Artazcoz L, Benach J, Borrell C. Perception or real illness? How chronic conditions contribute to gender inequalities in self-rated health. Europ J Public Health. (2011) 22:781–6. doi: 10.1093/eurpub/ckr184
132. Dusenbery M. Doing Harm : The Truth About How Bad Medicine and Lazy Science Leave Women Dismissed, Misdiagnosed, And sick. 1st ed. New York, NY: HarperOne (2017) 390. p.
133. Werner A, Isaksen LW, Malterud K. ‘I am not the kind of woman who complains of everything': illness stories on self and shame in women with chronic pain. Soc Sci Med. (2004) 59:1035–45. doi: 10.1016/j.socscimed.2003.12.001
134. Werner A, Malterud K. It is hard work behaving as a credible patient: encounters between women with chronic pain and their doctors. Soc Sci Med. (2003) 57:1409–19. doi: 10.1016/S0277-9536(02)00520-8
135. Haverfield MC, Giannitrapani K, Timko C, Lorenz K. Patient-centered pain management communication from the patient perspective. J Gen Intern Med. (2018) 33:1374–80. doi: 10.1007/s11606-018-4490-y
136. Yaffe MJ, Hovey RB, Rodriguez C. Useof patients' unsolicited correspondence to a family doctor to describe and understand valued components of a doctor-patient relationship: a Hermeneutics approach. BMC Fam Pract. (2019) 20:1–8. doi: 10.1186/s12875-019-1024-6
137. Kirmayer LJ, Ban L. Cultural psychiatry: research strategies and future directions. Adv Psychosom Med. (2013) 33:97–114. doi: 10.1159/000348742
138. Julien N, Lacasse A, Labra O, Asselin H. Review of chronic non-cancer pain research among Aboriginal people in Canada. Int J Qual Health Care. (2018) 30:178–85. doi: 10.1093/intqhc/mzx195
139. Edwards RR, Doleys DM, Fillingim RB, Lowery D. Ethnic differences in pain tolerance: clinical implications in a chronic pain population. Psychosom Med. (2001) 63:316–23. doi: 10.1097/00006842-200103000-00018
140. Losin EAR, Woo CW, Medina NA, Andrews-Hanna JR, Eisenbarth H, Wager TD. Neural and sociocultural mediators of ethnic differences in pain. Nat Hum Behav. (2020) 4:517–30. doi: 10.1038/s41562-020-0819-8
141. Kim HJ, Yang GS, Greenspan JD, Downton KD, Griffith KA, Renn CL, et al. Racial and ethnic differences in experimental pain sensitivity: systematic review and meta-analysis. Pain. (2017) 158:194–211. doi: 10.1097/j.pain.0000000000000731
142. Tung W-C, Li Z. Pain beliefs and behaviors among chinese. Home Health Care Manag Pract. (2014) 27:95–7. doi: 10.1177/1084822314547962
143. Banerjee S, Argaez C. Multidisciplinary Treatment Programs for Patients with Chronic Non-Malignant Pain: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines. CADTH Rapid Response Reports. Ottawa, ON (2017).
144. Becker WC, Dorflinger L, Edmond SN, Islam L, Heapy AA, Fraenkel L. Barriers and facilitators to use of non-pharmacological treatments in chronic pain. BMC Fam Pract. (2017) 18:41. doi: 10.1186/s12875-017-0608-2
145. Chou R, Hartung D, Turner J, Blazina I, Chan B, Levander X, et al. Opioid treatments for chronic pain. In: AHRQ Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality (2020). doi: 10.23970/AHRQEPCCER229
146. Fields HL. The doctor's dilemma: opiate analgesics and chronic pain. Neuron. (2011) 69:591–4. doi: 10.1016/j.neuron.2011.02.001
147. Henry SG, Bell RA, Fenton JJ, Kravitz RL. Communication about chronic pain and opioids in primary care: impact on patient and physician visit experience. Pain. (2017) 159:371–9. doi: 10.1097/j.pain.0000000000001098
148. Chou R, Turner JA, Devine EB, Hansen RN, Sullivan SD, Blazina I, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. (2015) 162:276–86. doi: 10.7326/M14-2559
149. Seedat S, Singhal A, Tien Y-Y, Hsia RY. Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS One. (2016) 11:e0159224. doi: 10.1371/journal.pone.0159224
150. Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health. (2003) 93:2067–73. doi: 10.2105/AJPH.93.12.2067
151. Militello LG, Anders S, Downs SM, Diiulio J, Danielson EC, Hurley RW, et al. Understanding how primary care clinicians make sense of chronic pain. Cogn Technol Work. (2018) 20:575–84. doi: 10.1007/s10111-018-0491-1
152. Kerner J, McCoy B, Gilbo N, Colavita M, Kim M, Zaval L, et al. Racial disparity in the clinical risk assessment. Community Ment Health J. (2019) 56:586–91. doi: 10.1007/s10597-019-00516-3
153. Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S, et al. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med. (2017) 24:895–904. doi: 10.1111/acem.13214
154. Baugh RF. The evolution of social beliefs 1960-2016 in the United states and its influence on empathy and prosocial expression in medicine. Adv Med Educ Pract. (2020) 11:437–46. doi: 10.2147/AMEP.S246658
155. Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. (2007) 97:1283–9. doi: 10.2105/AJPH.2005.080762
156. McCradden MD, Vasileva D, Orchanian-Cheff A, Buchman DZ. Ambiguous identities of drugs and people: a scoping review of opioid-related stigma. Int J Drug Policy. (2019) 74:205–15. doi: 10.1016/j.drugpo.2019.10.005
157. Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. (2015) 36:559–74. doi: 10.1146/annurev-publhealth-031914-122957
158. Gaines TL, Wagner KD, Mittal ML, Bowles JM, Copulsky E, Faul M, et al. Transitioning from pharmaceutical opioids: a discrete-time survival analysis of heroin initiation in suburban/exurban communities. Drug Alcohol Depend. (2020) 213:108084. doi: 10.1016/j.drugalcdep.2020.108084
159. Hirsch R. The opioid epidemic: it's time to place blame where it belongs. Mo Med. (2017) 114:82–90.
160. Glod SA. The other victims of the opioid epidemic. N Engl J Med. (2017) 376:2101–2. doi: 10.1056/NEJMp1702188
161. Steier F, Ostrenko W. Taking cybernetics seriously at a science center: reflection-in-interaction and second order organizational learning. Cybern Hum Knowing. (2000) 7:47–69.
163. Thompson WT, Steier F, Ostrenko W. Designing communication process for the design of an idea zone at a science center. J Appl Commun Res. (2014) 42:208–26. doi: 10.1080/00909882.2013.874570
165. Colder Carras M, Kalbarczyk A, Wells K, Banks J, Kowert R, Gillespie C, et al. Connection, meaning, and distraction: a qualitative study of video game play and mental health recovery in veterans treated for mental and/or behavioral health problems. Soc Sci Med. (2018) 216:124–32. doi: 10.1016/j.socscimed.2018.08.044
166. González-González CS, Toledo-Delgado PA, Muñoz-Cruz V, Torres-Carrion PV. Serious games for rehabilitation: gestural interaction in personalized gamified exercises through a recommender system. J Biomed Inform. (2019) 97:103266. doi: 10.1016/j.jbi.2019.103266
167. Octavia JR, Coninx K. Adaptive personalized training games for individual and collaborative rehabilitation of people with multiple sclerosis. Biomed Res Int. (2014) 2014:1–22. doi: 10.1155/2014/345728
168. Bonnechère B, Jansen B, Omelina L, Van Sint Jan S. The use of commercial video games in rehabilitation: a systematic review. Int J Rehabil Res. (2016) 39:277–90. doi: 10.1097/MRR.0000000000000190
169. Simperl E, Reeves N, Phethean C, Lynes T, Tinati R. Is virtual citizen science a game? Trans Soc Comput. (2018) 1:6. doi: 10.1145/3209960
170. Ghazisaeidi M, Safdari R, Goodini A, Mirzaiee M, Farzi J. Digital games as an effective approach for cancer management: opportunities and challenges. J Educ Health Promot. (2017) 6:30. doi: 10.4103/jehp.jehp_146_14
171. Kato PM, Cole SW, Bradlyn AS, Pollock BH. A video game improves behavioral outcomes in adolescents and young adults with cancer: a randomized trial. Pediatrics. (2008) 122:e305–17. doi: 10.1542/peds.2007-3134
172. Soltani M, Drever SA, Hoffman HG, Sharar SR, Wiechman SA, Jensen MP, et al. Virtual reality analgesia for burn joint flexibility: a randomized controlled trial. Rehabil Psychol. (2018) 63:487–94. doi: 10.1037/rep0000239
173. Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. (2008) 24:299–304. doi: 10.1097/AJP.0b013e318164d2cc
174. Hoffman HG, Patterson DR, Soltani M, Teeley A, Miller W, Sharar SR. Virtual reality pain control during physical therapy range of motion exercises for a patient with multiple blunt force trauma injuries. Cyberpsychol Behav. (2009) 12:47–9. doi: 10.1089/cpb.2008.0056
175. Birnie KA, Campbell F, Nguyen C, Lalloo C, Tsimicalis A, Matava C, et al. iCanCope PostOp: user-centered design of a smartphone-based app for self-management of postoperative pain in children and adolescents. JMIR Form Res. (2019) 3:e12028. doi: 10.2196/12028
176. Ambron E, Miller A, Kuchenbecker KJ, Buxbaum LJ, Coslett HB. Immersive low-cost virtual reality treatment for phantom limb pain: evidence from two cases. Front Neurol. (2018) 9:67. doi: 10.3389/fneur.2018.00067
177. Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. (2014) 69:153–66. doi: 10.1037/a0035747
178. Deterding S, Dixon D, Khaled R, Nacke L. From game design elements to gamefulness. In: Proceedings of the 15th International Academic MindTrek Conference on Envisioning Future Media Environments - MindTrek. Tampere (2011).
179. de Jager A, Fogarty A, Tewson A, Lenette C, Boydell K. Digital storytelling in research: a systematic review. Qual Rep. (2017) 22:2548–82. doi: 10.46743/2160-3715/2017.2970
180. Larsen ME, Vaughan P, Bennett J, Boydell K. The ‘BIG Anxiety Project': using the arts to visually explore public experiences and attitudes to anxiety. J Appl ArtsHealth. (2018) 9:85–97. doi: 10.1386/jaah.9.1.85_1
181. Watfern C, Doran B, Dadich A, Triandafilidis Z, Habak S, Boydell KM. The HIVE: a co-created art installation about health. Public Health. (2021) 193:26–8. doi: 10.1016/j.puhe.2020.12.007
182. Ruehlman LS, Karoly P, Enders C. A randomized controlled evaluation of an online chronic pain self management program. Pain. (2012) 153:319–30. doi: 10.1016/j.pain.2011.10.025
183. Merolli M, Gray K, Martin-Sanchez F, Lopez-Campos G. Patient-reported outcomes and therapeutic affordances of social media: findings from a global online survey of people with chronic pain. J Med Internet Res. (2015) 17:e20. doi: 10.2196/jmir.3915
184. Ettun R, Schultz M, Bar-Sela G. Transforming pain into beauty: on art, healing, and care for the spirit. Evidence-Based Complement Alternat Med. (2014) 2014:1–7. doi: 10.1155/2014/789852
185. de Witte M, Orkibi H, Zarate R, Karkou V, Sajnani N, Malhotra B, et al. From Therapeutic Factors to Mechanisms of Change in the Creative Arts Therapies: A Scoping Review. Front Psychol. (2021) 12:678397. doi: 10.3389/fpsyg.2021.678397
186. Braš M, Dordević V, Janjanin M. Person-centered pain management – science and art. Croat Med J. (2013) 54:296–300. doi: 10.3325/cmj.2013.54.296
187. Angheluta A-M, Lee BK. Art therapy for chronic pain: applications and future directions. Canad J Counsell Psychother. (2011) 45:112–31. Retrieved from: https://cjc-rcc.ucalgary.ca/article/view/59289
189. Flanagan M. Critical Play : Radical Game Design. Cambridge, MA, London: MIT Press (2009) vii, 353. p. doi: 10.7551/mitpress/7678.001.0001
190. Flanagan M, Nissenbaum HF. Values at Play in Digital Games. Cambridge, MA: The MIT Press (2014) xiv, 207 p. doi: 10.7551/mitpress/9016.001.0001
191. Kaufman G, Flanagan M, Seidman M, Wien S. “RePlay Health”: an experiential role-playing sport for modeling healthcare decisions, policies, and outcomes. Games Health J. (2015) 4:295–304. doi: 10.1089/g4h.2014.0134
193. Schmidt B, Stewart S. Implementing the virtual reality learning environment: second life. Nurse Educ. (2009) 34:152–5. doi: 10.1097/NNE.0b013e3181aabbe8
194. Kidd LI, Knisley SJ, Morgan KI. Effectiveness of a second life((R)) simulation as a teaching strategy for undergraduate mental health nursing students. J Psychosoc Nurs Ment Health Serv. (2012) 50:28–37. doi: 10.3928/02793695-20120605-04
195. McCallum J, Ness V, Price T. Exploring nursing students' decision-making skills whilst in a Second Life clinical simulation laboratory. Nurse Educ Today. (2011) 31:699–704. doi: 10.1016/j.nedt.2010.03.010
196. Menzel N, Willson LH, Doolen J. Effectiveness of a poverty simulation in Second Life(R): changing nursing student attitudes toward poor people. Int J Nurs Educ Scholarsh. (2014) 11:39–45. doi: 10.1515/ijnes-2013-0076
197. Metcalfe S. Second life patient scenarios: enhancing the diversity of the nursing profession. Creat Nurs. (2016) 22:166–70. doi: 10.1891/1078-4535.22.3.166
198. Weiner E, McNew R, Trangenstein P, Gordon J. Using the virtual reality world of second life to teach nursing faculty simulation management. Stud Health Technol Inform. (2010) 160:615–9. doi: 10.3233/978-1-60750-588-4-615
199. Weiner E, Trangenstein P, McNew R, Gordon J. Using the virtual reality world of second life to promote patient engagement. Stud Health Technol Inform. (2016) 225:198–202. doi: 10.3233/978-1-61499-658-3-198
200. Schaffer MA, Tiffany JM, Kantack K, Anderson LJ. Second Life((R)) virtual learning in public health nursing. J Nurs Educ. (2016) 55:536–40. doi: 10.3928/01484834-20160816-09
201. Evans DA, Curtis AR. Animosity, antagonism, and avatars: teaching conflict management in second life. J Nurs Educ. (2011) 50:653–5. doi: 10.3928/01484834-20110729-03
202. Kaufman G, Flanagan M. Digital Divide: Comparing the Impact of Digital and Non-Digital Platforms on Player Behaviors and Game Impact. In: Dubbels B, editor. Transforming Gaming and Computer Simulation Technologies across Industries (2017). p. 94–101. doi: 10.4018/978-1-5225-1817-4.ch005
203. McElhinney E, Cheater FM, Kidd L. Undertaking qualitative health research in social virtual worlds. J Adv Nurs. (2014) 70:1267–75. doi: 10.1111/jan.12281
204. Nosek MA, Robinson-Whelen S, Ledoux TA, Hughes RB, O'Connor DP, Lee RE, et al. A pilot test of the GoWoman weight management intervention for women with mobility impairments in the online virtual world of Second Life((R)). Disabil Rehabil. (2019) 41:2718–29. doi: 10.1080/09638288.2018.1473511
205. Pereira J, Díaz Ó. Using health chatbots for behavior change: a mapping study. J Med Syst. (2019) 43:135. doi: 10.1007/s10916-019-1237-1
206. Aldunate N, Villena-Gonzalez M, Rojas-Thomas F, Lopez V, Bosman CA. Mood detection in ambiguous messages: the interaction between text and emoticons. Front Psychol. (2018) 9:423. doi: 10.3389/fpsyg.2018.00423
207. Feldman LB, Aragon CR, Chen NC, Kroll JF. Emoticons in text may function like gestures in spoken or signed communication. Behav Brain Sci. (2017) 40:e55. doi: 10.1017/S0140525X15002903
208. Lo SK. The nonverbal communication functions of emoticons in computer-mediated communication. Cyberpsychol Behav. (2008) 11:595–7. doi: 10.1089/cpb.2007.0132
209. Derks D, Bos AE, von Grumbkow J. Emoticons in computer-mediated communication: social motives and social context. Cyberpsychol Behav. (2008) 11:99–101. doi: 10.1089/cpb.2007.9926
210. Cook BL, Progovac AM, Chen P, Mullin B, Hou S, Baca-Garcia E. Novel Use of Natural Language Processing (NLP) to predict suicidal ideation and psychiatric symptoms in a text-based mental health intervention in madrid. Comput Math Methods Med. (2016) 2016:1–8. doi: 10.1155/2016/8708434
211. Wang Z, Huang H, Cui L, Chen J, An J, Duan H, et al. Using natural language processing techniques to provide personalized educational materials for chronic disease patients in china: development and assessment of a knowledge-based health recommender system. JMIR Med Inform. (2020) 8:e17642. doi: 10.2196/17642
212. Vaci N, Liu Q, Kormilitzin A, De Crescenzo F, Kurtulmus A, Harvey J, et al. Natural language processing for structuring clinical text data on depression using UK-CRIS. Evid Based Ment Health. (2020) 23:21–6. doi: 10.1136/ebmental-2019-300134
213. Shoenbill K, Song Y, Gress L, Johnson H, Smith M, Mendonca EA. Natural language processing of lifestyle modification documentation. Health Informatics J. (2020) 26:388–405. doi: 10.1177/1460458218824742
214. Funk B, Sadeh-Sharvit S, Fitzsimmons-Craft EE, Trockel MT, Monterubio GE, Goel NJ, et al. A framework for applying natural language processing in digital health interventions. J Med Internet Res. (2020) 22:e13855. doi: 10.2196/13855
215. Lucas GM, Gratch J, King A, Morency L-P. It's only a computer: virtual humans increase willingness to disclose. Comput Human Behav. (2014) 37:94–100. doi: 10.1016/j.chb.2014.04.043
216. Bickmore T, Gruber A, Picard R. Establishing the computer–patient working alliance in automated health behavior change interventions. Patient Educ Couns. (2005) 59:21–30. doi: 10.1016/j.pec.2004.09.008
217. Lucas GM, Rizzo A, Gratch J, Scherer S, Stratou G, Boberg J, et al. Reporting mental health symptoms: breaking down barriers to care with virtual human interviewers. Front Robotics AI. (2017) 4:51. doi: 10.3389/frobt.2017.00051
218. Fitzpatrick KK, Darcy A, Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health. (2017) 4:e19. doi: 10.2196/mental.7785
219. Rice KL, Bennett MJ, Billingsley L. Using second life to facilitate peer storytelling for grieving oncology nurses. Ochsner J. (2014) 14:551–62.
220. Yu FY, Hsieh HT, Chang B. The potential of Second Life for university counseling: a comparative approach examining media features and counseling problems. Res Pract Technol Enhanc Learn. (2017) 12:24. doi: 10.1186/s41039-017-0064-6
221. Simon B. Beyond cyberspatial flaneurie. Games Cult. (2006) 1:62–7. doi: 10.1177/1555412005281789
222. Wilhelm C. Gender role orientation and gaming behavior revisited: examining mediated and moderated effects. Informat Commun Soc. (2016) 21:224–40. doi: 10.1080/1369118X.2016.1271902
223. Khalili-Mahani N, De Schutter B, Mirgholami M, Holowka EM, Goodine R, DeJong S, et al. For whom the games toll: a qualitative and intergenerational evaluation of what is serious in games for older adults. Comput Game J. (2020) 9:221–44. doi: 10.1007/s40869-020-00103-7
224. van Leeuwen L, Westwood D. Adult play, psychology and design. Digital Creativ. (2008) 19:153–61. doi: 10.1080/14626260802312665
225. McGonigal J. Reality is Broken : Why Games Make us Better and How They Can Change The world. London: Vintage (2012) 396. p.
226. Rey P. Gamification and PostFordian Capitalisam. In: Walz SP, Detrerding S, editors. The Gameful World: Approaches, Issues, Applications. Cambridge, MA; London: The MIT Press (2015). p. 277.
227. Bogost I. Why gamification is bullshit. In: Walz SP, Detrerding S, editors. The Gameful World, Approaches, Issues and Applications. Cambridge, MA; London: The MIT Press (2015). p. 65–79.
228. Khalili-Mahani N, Schutter BD. Affective game planning for health applications: quantitative extension of gerontoludic design based on the appraisal theory of stress and coping. JMIR Serious Games. (2019) 7:e13303. doi: 10.2196/13303
229. Goodman-Vincent E, Roy M, Khalili-Mahani N. Affective game planning for playing the pain. extended abstracts of the 2020. In: Annual Symposium on Computer-Human Interaction in Play. Ottawa, ON (2020). p. 122–8. doi: 10.1145/3383668.3419933
230. Khaled R. Gamification and culture. In: Walz SP, Detrerding S, editors. The Gameful World, Approaches, Issues and Applications. Cambridge, MA; London: The MIT Press (2015). p. 301–21.
231. Simon B. The return of panopticism: supervision, subjection and the new surveillance. Surveill Soc. (2002) 3:1–20. doi: 10.24908/ss.v3i1.3317
232. Sicart M. The Ethics of Game Design. The Ethics of Computer Games. Cambridge, MA: MIT Press (2009). p. 207–22. doi: 10.7551/mitpress/9780262012652.003.0007
233. Laycock J. Dangerous Games : What the Moral Panic Over Role-Playing Games Says About Play, Religion, and Imagined Worlds. Oakland, CA: University of California Press (2015) xiv, 349 p. doi: 10.1525/9780520960565
234. Stavropoulos V, Vassallo J, Burleigh TL, Gomez R, Colder Carras M. The role of internet gaming in the association between anxiety and depression: a preliminary cross-sectional study. Asia-Pacific Psychiatry. (2021) e12474. doi: 10.1111/appy.12474
235. Robinson P, Turk D, Jilka S, Cella M. Measuring attitudes towards mental health using social media: investigating stigma and trivialisation. Soc Psychiatry Psychiatr Epidemiol. (2018) 54:51–8. doi: 10.1007/s00127-018-1571-5
236. Ballard ME, Welch KM. Virtual warfare. Games Culture. (2015) 12:466–91. doi: 10.1177/1555412015592473
237. Naudet F, Colder Carras M, Shi J, Hard G, Saldanha IJ. Evaluating the quality of evidence for gaming disorder: a summary of systematic reviews of associations between gaming disorder and depression or anxiety. PLoS One. (2020) 15:e0240032. doi: 10.1371/journal.pone.0240032
238. Kircaburun K, Pontes HM, Stavropoulos V, Griffiths MD. A brief psychological overview of disordered gaming. Curr Opin Psychol. (2020) 36:38–43. doi: 10.1016/j.copsyc.2020.03.004
239. Bergold J, Thomas S. Participatory research methods: a methodological approach in motion. Forum Qualit Sozialforschung/Forum. (2012) 13. doi: 10.17169/fqs-13.1.1801
240. Omaki E, Castillo R, Eden K, Davis S, McDonald E, Murtaza U, et al. Using m-health tools to reduce the misuse of opioid pain relievers. Inj Prev. (2017) 25:334–9. doi: 10.1136/injuryprev-2017-042319
241. Boschen KA, Robinson E, Campbell KA, Muir S, Oey E, Janes K, et al. Results from 10 years of a CBT pain self-management outpatient program for complex chronic conditions. Pain Res Manage. (2016) 2016:4678083. doi: 10.1155/2016/4678083
242. Harrison AM, McCracken LM, Jones K, Norton S, Moss-Morris R. Using mixed methods case-series evaluation in the development of a guided self-management hybrid CBT and ACT intervention for multiple sclerosis pain. Disabil Rehabil. (2016) 39:1785–98. doi: 10.1080/09638288.2016.1209580
243. Sicart M. Play Matters. Cambridge, MA: The MIT Press (2014) x, 158 p. doi: 10.7551/mitpress/10042.001.0001
244. Lopez C, Tucker C. Toward personalized adaptive gamification: a machine learning model for predicting performance. IEEE Trans Games. (2020) 12:155–68. doi: 10.1109/TG.2018.2883661
245. Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. (2014) 41:545–7. doi: 10.1188/14.ONF.545-547
246. Winsor S, Smith A, Vanstone M, Giacomini M, Brundisini FK, DeJean D. Experiences of patient-centredness with specialized community-based care: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. (2013) 13:1–33. Retrieved from: http://www.hqontario.ca/en/documents/eds/2013/full-report-OCDM-patient-centredness.pdf
247. Rains SA. Coping With Illness Digitally. Cambridge: MIT Press (2018). doi: 10.7551/mitpress/11219.001.0001
248. Batchelor JA, Briggs CM. Subject, project or self? Thoughts on ethical dilemmas for social and medical researchers. Soc Sci Med. (1994) 39:949–54. doi: 10.1016/0277-9536(94)90206-2
249. Das S, Glatard T, Rogers C, Saigle J, Paiva S, MacIntyre L, et al. Cyberinfrastructure for open science at the montreal neurological institute. Front Neuroinform. (2016) 10:53. doi: 10.3389/fninf.2016.00053
250. Kirmayer L, Worthman C, Kitayama S. Epilogue: Interdisciplinarity in the Study of Culture, Mind, and Brain. In: Kirmayer L, Worthman C, Kitayama S, Lemelson R, Cummings C, editors. Culture, Mind, and Brain: Emerging Concepts, Models, and Applications (Current Perspectives in Social and Behavioral Sciences). Cambridge: Cambridge University Press (2020). p. 494–512. doi: 10.1017/9781108695374.028
251. Fernandes BS, Williams LM, Steiner J, Leboyer M, Carvalho AF, Berk M. The new field of ‘precision psychiatry'. BMC Med. (2017) 15:80. doi: 10.1186/s12916-017-0849-x
252. Glasgow RE, Kwan BM, Matlock DD. Realizing the full potential of precision health: the need to include patient-reported health behavior, mental health, social determinants, and patient preferences data. J Clin Trans Sci. (2018) 2:183–5. doi: 10.1017/cts.2018.31
253. Rasmussen LM. Research Ethics in Citizen Science. In: Iltis AS, MacKay D, editors. The Oxford Handbook of Research Ethics. (2021). doi: 10.1093/oxfordhb/9780190947750.001.0001
Keywords: chronic pain, personalized medicine, citizen labs, stigma & discrimination, digital health, serious games (SGs), big-data, play
Citation: Khalili-Mahani N, Holowka E, Woods S, Khaled R, Roy M, Lashley M, Glatard T, Timm-Bottos J, Dahan A, Niesters M, Hovey RB, Simon B and Kirmayer LJ (2021) Play the Pain: A Digital Strategy for Play-Oriented Research and Action. Front. Psychiatry 12:746477. doi: 10.3389/fpsyt.2021.746477
Received: 23 July 2021; Accepted: 11 November 2021;
Published: 15 December 2021.
Edited by:
Max V. Birk, Eindhoven University of Technology, NetherlandsReviewed by:
Conor Linehan, University College Cork, IrelandMathijs Lucassen, The Open University, United Kingdom
Copyright © 2021 Khalili-Mahani, Holowka, Woods, Khaled, Roy, Lashley, Glatard, Timm-Bottos, Dahan, Niesters, Hovey, Simon and Kirmayer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Najmeh Khalili-Mahani, bmFqbWVoLmtoYWxpbGktbWFoYW5pQGNvbmNvcmRpYS5jYQ==
 Najmeh Khalili-Mahani
Najmeh Khalili-Mahani Eileen Holowka4
Eileen Holowka4 Sandra Woods
Sandra Woods Mathieu Roy
Mathieu Roy Tristan Glatard
Tristan Glatard Janis Timm-Bottos
Janis Timm-Bottos Albert Dahan
Albert Dahan Richard B. Hovey
Richard B. Hovey Laurence J. Kirmayer
Laurence J. Kirmayer