- 1School of Nursing, The Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
- 2World Health Organization Collaborating Center for Community Health Services, The Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
Background: Previous studies address posttraumatic stress disorder (PTSD) following disasters as a public health issue. However, few studies investigate the long-term effect of disaster exposure on PTSD among hospital medical workers (HMWs).
Objectives: This study aimed to study the prevalence of ICD-11 PTSD and complex PTSD (CPTSD) among exposed and non-exposed HMWs 11 years after the Wenchuan earthquake in China, to identify the factors associated with PTSD and CPTSD scores, and to examine the factor structures of PTSD and CPTSD models.
Methods: A cross-sectional study was conducted using a self-administered online questionnaire. Two thousand fifty-nine valid samples were collected from four hospitals in 2019. Descriptive statistical analysis, multivariate regression models, and confirmatory factor analysis (CFA) were performed.
Results: The prevalence of PTSD and CPTSD was 0.58 and 0.34%, respectively. The unexposed group reported higher PTSD and CPTSD scores than the exposed group. The type of workplace and marital status were significantly associated with the PTSD and CPTSD scores of HMWs. The CFA results indicate that both the correlated first-order model and the correlated two-layer model were a good fit to explain the structure of PTSD and CPTSD.
Conclusion: These findings suggest that few HMWs who were exposed to the Wenchuan earthquake suffered from PTSD or CPTSD 11 years following the disaster. However, psychological support was still necessary for all HMWs, especially for unmarried HMWs who were Working in smaller hospitals. Further research is required to analyze mental health status using ICD-11 PTSD and CPTSD to provide ongoing evidence to help HWMs cope effectively with the challenges of future disasters.
Introduction
Posttraumatic stress disorder (PTSD) is one of the most common types of psychopathologies experienced after a mass traumatic incident caused by a disaster (1). The disorder involves substantial functional impairment and often coexists with other mental health conditions, such as depression, generalized anxiety disorder, and substance abuse. For these reasons, PTSD is the most frequently studied postdisaster mental health disorder (2–4). Moreover, disasters and disaster response can have long-term effects on individuals' mental health (5, 6). A cohort study of the link between hurricane experience and mental health found that adolescents at the time of the disaster had a reduced incidence of depression and PTSD up to 9 years postdisaster compared with those who were adults at the time of the disaster (7).
According to a report released by China's Ministry of Civil Affairs in 2008, the Wenchuan earthquake event of May 12, 2008, claimed 69,227 lives and injured 374,643 people, whereas 17,923 people were missing at the time of the report and 46,240,000 people were affected (8). The earthquake had a magnitude of 8.0 on the Richter scale, and its epicenter had a maximum intensity of 11.0 in Sichuan Province, southwest China. There were approximately 10,630 medical workers deployed to the affected areas to offer assistance with the rescue efforts, such as providing emergency response services, collaboration and cooperation, large-scale transportation, and the rehabilitation of those injured while responding to the earthquake (8). As the largest component of the medical care workforce, healthcare professionals often play a vital role in providing emergency medical relief when a disaster strikes (5, 9, 10). They are also vulnerable to developing PTSD (11) because they may witness mass causalities, deaths, and severe injuries, which may cause psychological shock or intense fear.
The prevalence of PTSD was relatively high directly following the Wenchuan earthquake, but its prevalence declined over time for the majority of people, according to a systematic review, which analyzed 58 original studies of PTSD prevalence in the 10 years after the earthquake among community populations (12). The prevalence of PTSD among medical rescue workers was 19.3% (13), 30.0% (11), 17.0% (14), and 1.7% (15) at 3, 6–12, and 14–17 months and 2 years after the earthquake, respectively. A longitudinal study examined adult survivors and found that the prevalence of PTSD was 58.2% at 2 months, 22.1% at 8 months, 19.8% at 14 months, 19.0% at 26 months, and 8.0% at ~44 months after the Wenchuan earthquake (16). However, studies of the long-term effects (e.g., more than 10 years) of disaster exposure on the mental health of medical rescue workers are lacking. In addition, most previous studies focusing on individuals' mental health after disasters do not include unexposed comparison groups to distinguish the effect of disaster exposure on PTSD (5).
The World Health Organization has published the 11th version of the International Classification of Diseases (ICD-11), which was approved by the World Health Assembly in 2017 (17). The initial criteria for PTSD can be traced back to 1980 in the third edition of the Diagnostic and Statistical Manual. The purpose of this updated version is to improve the utility of public health, disease-related, and clinical applications to maintain diagnostic and screening reliability and validity (18). Brewin et al. (17) further suggest that the value of ICD-11 is that it provides a brief set of systems to distinguish between two sibling disorders, PTSD and complex PTSD (CPTSD). Several studies examine the association of PTSD with disasters, such as studies of earthquake survivors in China (19, 20), Australian accident victims (21), and preadolescent children exposed to a hurricane in the United States (22). The findings of these studies indicate that the ICD-11 model has an acceptable fit for data collected from postdisaster settings.
Therefore, this study investigated ICD-11 PTSD and CPTSD among hospital medical workers (HMWs) 11 years after the Wenchuan earthquake. Specifically, the objectives were to examine (1) the prevalence of PTSD and CPTSD among earthquake-exposed and non-exposed HMWs, (2) the factors associated with their PTSD and CPTSD scores, and (3) the factor structure of PTSD and CPTSD models. The findings are significant as they demonstrate the long-term effects of PTSD and CPTSD. This helps us understand the effect of disasters on healthcare professionals' well-being and provides evidence to inform policies on the prevention of mental health disorders in the long term.
Materials and Methods
Design
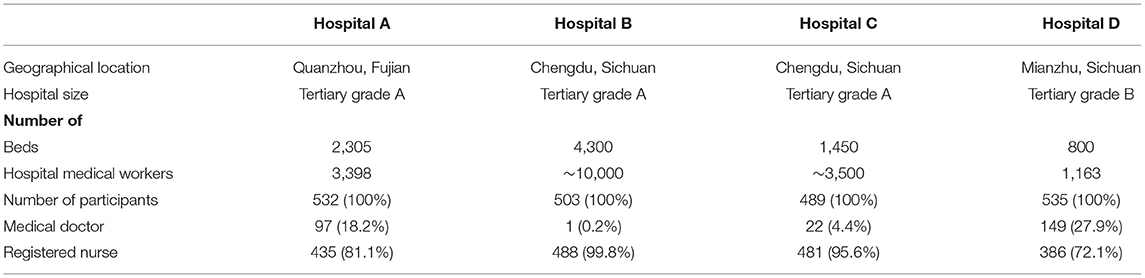
This was a cross-sectional study. Data were collected from four hospitals from June 2019 to October 2019. These four hospitals were selected based on the following criteria: (1) geographic location as they were located either at the epicenter of the Wenchuan earthquake (Hospital D in Mianzhu, Sichuan), near the epicenter (Hospitals B and C, Chengdu, Sichuan), or a great distance from the epicenter (Hospital A, Quanzhou, Fujian) and (2) the size of the hospital, including the total number of beds and HMWs and the number of potential participants. Hospital B was the largest hospital (4,300 beds and more than 10,000 healthcare workers), and Hospital D was the smallest hospital (800 beds and approximately 1,000 healthcare workers; Table 1).
Participants
HMWs were included in the study if they were (1) medical doctors or registered nurses working in one of the four selected hospitals and (2) willing to participate in the study and complete the online questionnaire. Those who were taking prolonged leave due to illness or maternity were excluded from the study. The sample size was large enough to ensure that parameter estimates were within the acceptable margin of error of 4% with a confidence level of 95%. Approximately 500 valid questionnaires were collected from each of the hospitals (Table 1). However, the numbers of participating medical doctors and registered nurses varied among these hospitals. The largest participation rate was from medical doctors from Hospital D (149 out of 535, 27.9%), whereas only one medical doctor (0.2%) from Hospital C completed the questionnaire.
Measurements
The International Trauma Questionnaire (ITQ) (23) was used as a self-reported measure of ICD-11 PTSD and CPTSD. CPTSD is a disorder comprising PTSD and disturbances in self-organization (DSO) symptoms.
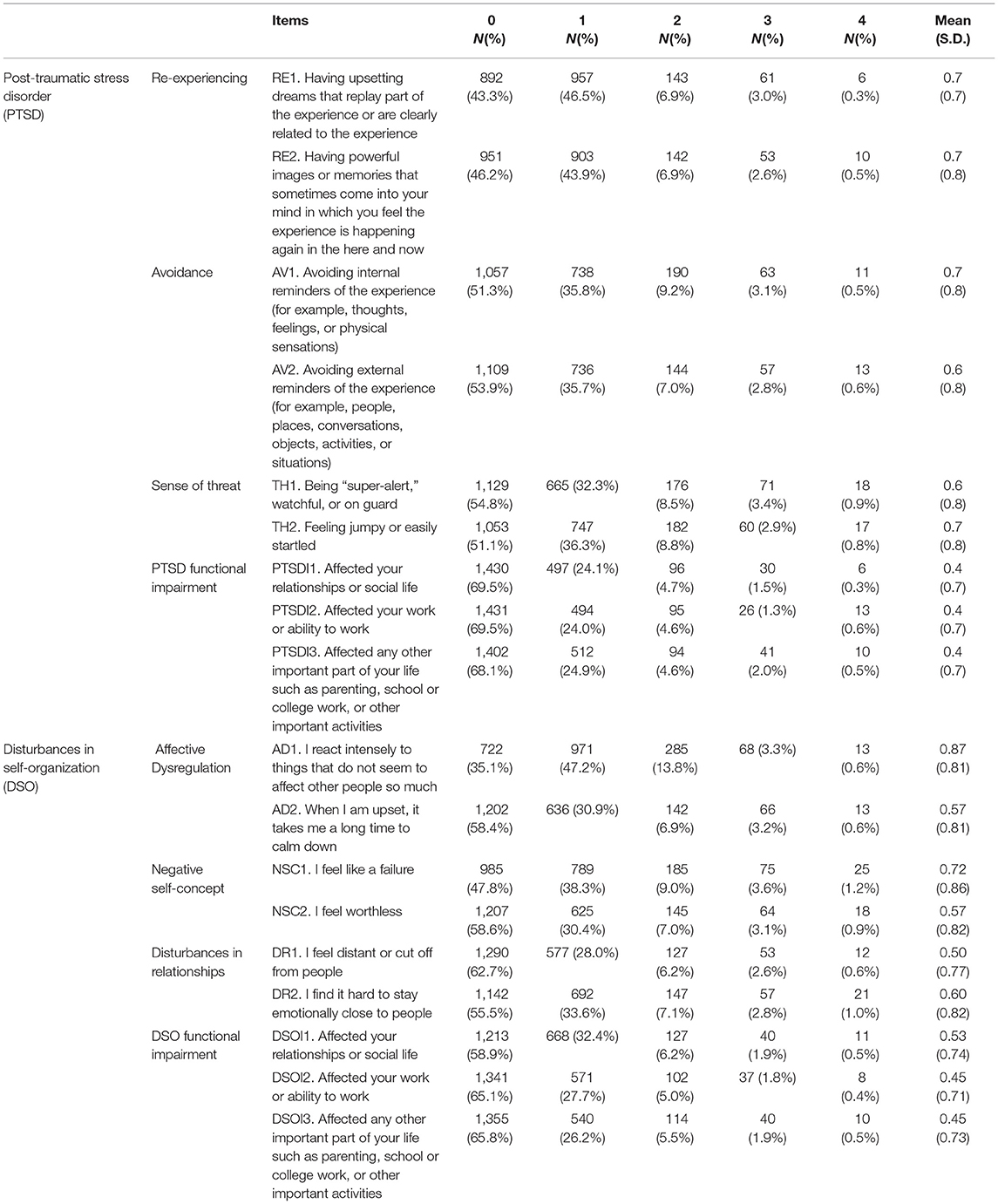
The ITQ measurement assesses six symptoms of PTSD distributed across the following three clusters: re-experiencing (RE with the symptoms of RE1, upsetting dreams, and RE2, reliving the events), avoidance (AV with the symptoms of AV1, internal avoidance, and AV2, external avoidance), and a sense of threat (TH with the symptoms of TH1, being on guard, and TH2, being easily startled). The six symptoms of DSO are distributed across the following three clusters: affective dysregulation (AD with the symptoms of AD1, intense reaction, and AD2, long time to calm down), negative self-concept (NSC with the symptoms of NSC1, feelings of failure, and NSC2, feelings of worthlessness), and disturbances in relationships (DR with the symptoms of DR1, feeling cut off from others, and DR2, difficulty staying close to others). All symptoms were assessed using a five-point Likert scale ranging from 0 = “not at all” to 4 = “extremely” (Table A1 in Appendix I).
PTSD and CPTSD prevalence: Three additional questions were used to evaluate PTSD-related functional impairment (PTSDI1, social life distress; PTSDI2, work affected; and PTSDI3, other aspects of life affected) and DSO-related functional impairment (DSOFI1, DSOFI2, and DSOFI3), also in the domains of social life, work life, and other important areas of life, respectively. Scores ≥ 2 (“moderately”) indicated the presence of a symptom. PTSD and DSO prevalence requires the presence of at least one symptom in each PTSD/DSO cluster plus the presence of functional impairment associated with these symptoms. CPTSD prevalence requires a PTSD prevalence, one symptom in each DSO cluster, and associated functional impairment. For example, if RE1 or RE2 > 2 (“moderately”), RE criteria were met; if AV1 or AV2 > 2, AV criteria were met; if TH1 or TH2 > 2, TH criteria were met; if PTSDI1, PTSDI2, or PTSDI3 > 2, PTSDI criteria were met; and if RE, AV, TH, and PTSDI criteria were all met, a diagnosis of PTSD was made. The same criteria were used for CPTSD prevalence. PTSD and CPTSD were assessed using a self-reported measure rather than a clinician-administered assessment. For this reason, the term “probable” is used when referring to estimating the prevalence of PTSD and CPTSD.
Wenchuan earthquake exposure: The participants were divided into the following three groups according to their level of exposure to the Wenchuan earthquake: unexposed HMWs, earthquake survivors (who were adolescents in 2008 and were exposed to the earthquake as survivors), and earthquake relief workers (who were adults in 2008 and were exposed to the earthquake as HMWs).
Workplaces: Four hospitals participated in the survey (Hospitals A, B, C, and D). They had different geographical locations and different numbers of HMWs and beds (Table 1).
Sociodemographic factors: The sociodemographic data that were collected included gender (male/female), educational level (college or below/university or above), marital status (unmarried/married), profession (medical doctor/registered nurse), age, and length of service in years.
Data Analysis
First, a descriptive analysis was performed to understand the characteristics of the sample and determine the prevalence of PTSD and CPTSD. Second, the PTSD and DSO scores were calculated for different groups of HMWs. Multivariate regression models were established to examine the effect of Wenchuan earthquake exposure, the type of workplace, and sociodemographic factors on the PTSD and DSO scores of the HMWs. All analyses were performed using SPSS software, version 25.0 (IBM, Armonk, NY, the United States) with the threshold for statistical significance at a two-tailed α value of 0.05. The beta coefficient (β), the associated two-tailed p-values (p), and 95% confidence intervals (CIs) were reported for each independent variable in the regression models. An analysis of variance test was performed, and p- and R2-values were reported to evaluate the performance of each regression model.
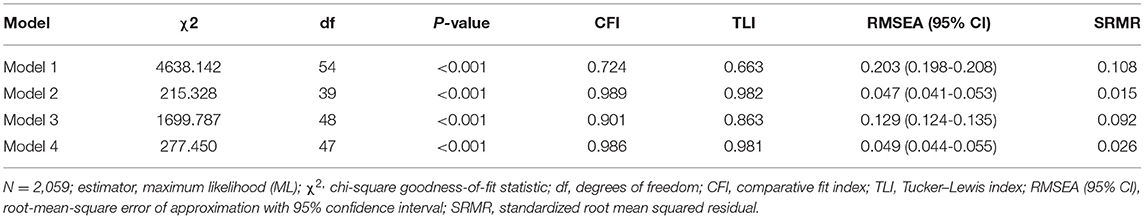
Third, confirmatory factor analysis (CFA) was performed using Mplus 7.11 (Muthén and Muthén, Los Angeles, CA, the United State) to examine the structure of PTSD and CPTSD in HMWs. Four different models were established for CFA based on data from multiple trials (24–26). Model 1 was a one-layer, one-factor model in which the latent factor of CPTSD was constructed by the 12 ITQ symptoms. Model 2 was a correlated six-factor model in which each of the clusters of PTSD (RE, AV, and TH) and DSO (AD, NSC, and DR) was a latent factor. The correlation between the six latent factors was tested in Model 2. Model 3 was a two-layer model in which CPTSD was constructed using the six latent factors in Model 2. Model 4 was a correlated two-layer model in which PTSD accounted for the covariation between the latent factors of RE, AV, and TH, whereas DSO accounted for the covariation between the latent factors of AD, NSC, and DR. The maximum likelihood estimation was used, and the STDYX standardization of estimate together with its standard errors (SE) were reported for each path in the CFA.
The comparative fit index (CFI), root mean square error of approximation (RMSEA) with 95% CI, and Tucker–Lewis index (TLI) were used to assess the fit of the hypothetical model. Cutoff values of 0.95 for CFI and TLI (a higher value is better) and 0.06 for RMSEA (a lower value is better) (27, 28) were used to determine the goodness of fit. To identify the model with the optimal fit, changes in the CFI (ΔCFI), TLI (ΔTLI), and RMSEA (ΔRMSEA) values were assessed. ΔCFI ≥ 0.01, ΔTLI ≥ 0.01, and ΔRMSEA ≥ 0.015 were considered to be evidence of a meaningful difference in the fit of the respective models (29).
Results
Demographic Characteristics and Prevalence of ICD-11 PTSD and CPTSD
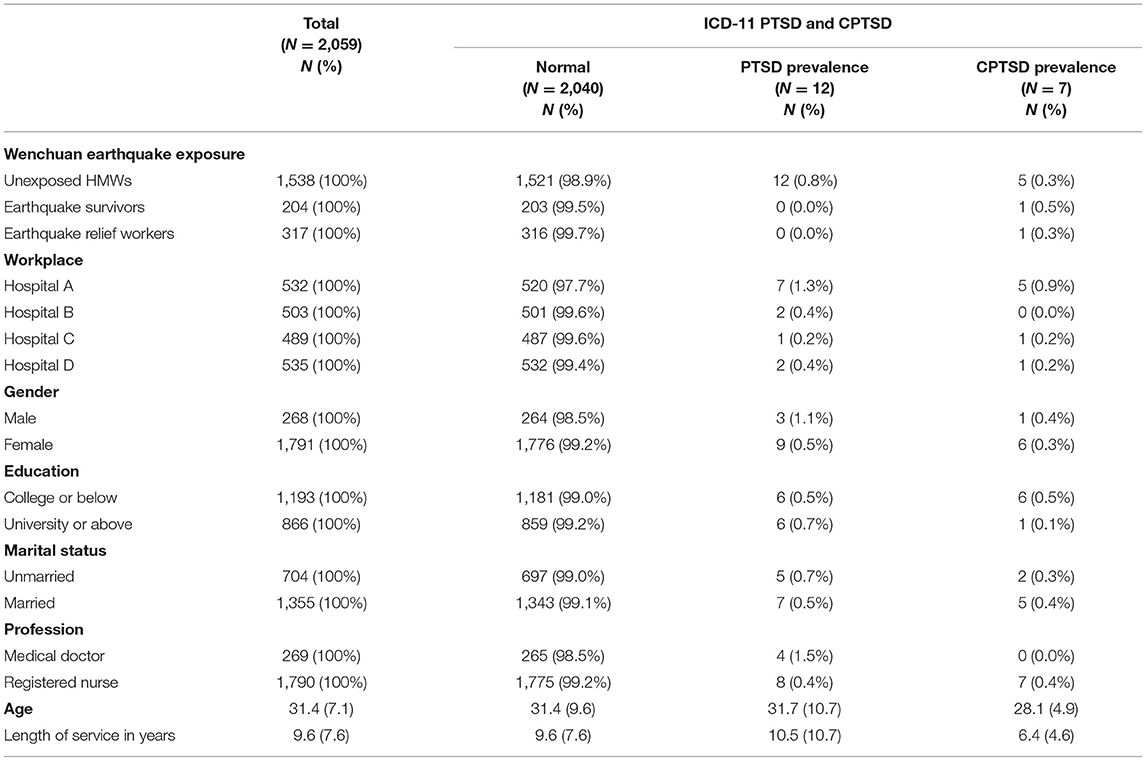
Of the 2,059 HMWs in the study, 9.9% experienced the Wenchuan earthquake as survivors (204 out of 2,059), 15.4% experienced the earthquake as disaster relief workers (317 out of 2,059), and 74.7% did not experience the earthquake (1,538 out of 2,059; Table 2). There were more female than male HMWs in the total sample (1,791 vs. 268). More participants had a college education level or below (including diploma and subdegree) than a university educational level or above (1,193 vs. 866). More of the participants were married than unmarried (1,355 vs. 704). More than 80% of the participants were registered nurses (1,790 of 2,059, 86.9%). The mean age of the participants was 31.4 with a standard deviation (SD) of 7.1, whereas the mean length of service as an HMW was 9.6 years with an SD of 7.6 years.
The prevalence of PTSD and CPTSD was 0.58% (12 of 2,059) and 0.34% (7 of 2,059), respectively. All participants with PTSD (100%, 12 of 12) and most of those with CPTSD (71.4%, 5 of 7) had not been exposed to the Wenchuan earthquake. Approximately equal numbers of participants were recruited from the four hospitals. However, Hospital A reported the highest prevalence of PTSD (1.3%, 7 of 521) and CPTSD (0.9%, 5 of 521). Moreover, male participants reported a higher prevalence of both PTSD (1.1 vs. 0.5%) and CPTSD (0.4 vs. 0.3%) than their female HMW counterparts. The participants with an education at the university level or above reported a higher prevalence of PTSD (0.7 vs. 0.5%) and a lower prevalence of CPTSD (0.1 vs. 0.5%) than their counterparts with lower educational levels. A higher prevalence of PTSD (0.7 vs. 0.5%) but a lower prevalence of CPTSD (0.3 vs. 0.4%), was reported by unmarried participants compared with married participants. Medical doctors reported a much higher prevalence of PTSD (1.5 vs. 0.4%) than registered nurses, whereas all cases of CPTSD were found in registered nurses. The mean age was lower and the length of service as an HMW was shorter in those with CPTSD than in those with PTSD and those without CPTSD or PTSD.
Dimensional Scores of PTSD and DSO and Their Determinants
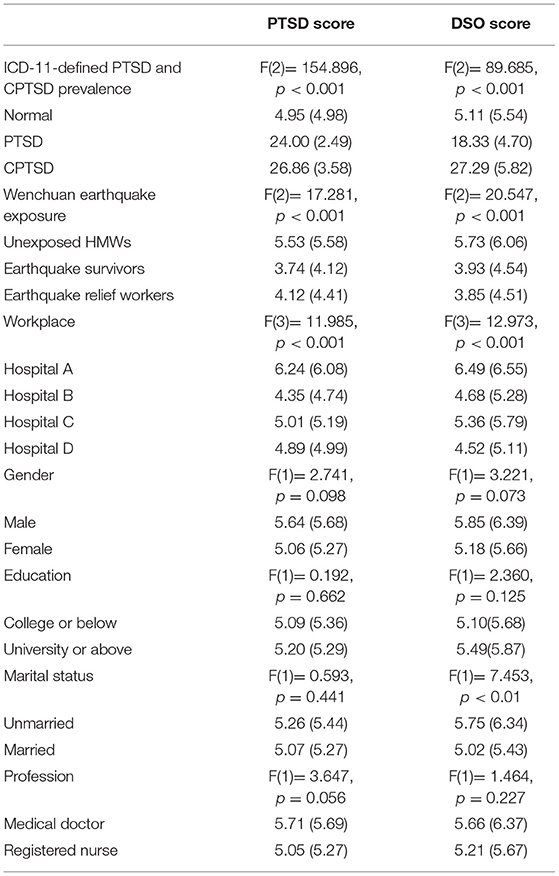
Participants, who were probable with CPTSD, reported the highest PTSD (mean = 26.86, SD = 3.58) and DSO (mean = 27.29, SD = 5.82) scores, followed by those with PTSD (Table 3). Participants with different types of Wenchuan earthquake exposure reported significantly different of PTSD [F(2) = 17.281, p < 0.001] and DSO [F(2) = 20.547, p < 0.001] scores. Unexposed HMWs reported the highest PTSD (mean = 5.53, SD = 5.58) and DSO (mean = 5.73, SD = 6.06) scores.
Participants from different hospitals showed significantly different PTSD [F(3) = 11.985, p < 0.001] and DSO [F(3) = 12.973, p < 0.001] scores. Participants from Hospital A reported the highest PTSD (mean = 6.24, SD = 6.08) and DSO (mean = 6.49, SD = 6.55) scores, followed by those from Hospital C (PTSD: mean = 5.01, SD = 5.19; DSO: mean = 5.36, SD = 5.79). Moreover, participants with different marital statuses had significantly different DSO scores [F(1) = 7.453, p < 0.01].
According to the multivariate regression models (Table 4), experiencing the Wenchuan earthquake as a survivor had a significant negative effect on PTSD (β = −1.326, 95% CI: −2.160, −0.493) and DSO (β = −1.153, 95% CI: −2.053, −0.253) scores. Being a relief worker after the earthquake also had a significant negative effect on PTSD (β = −1.188, 95% CI: −1.883, −0.492) and DSO (β = −1.481, 95% CI: −2.232, −0.729) scores.
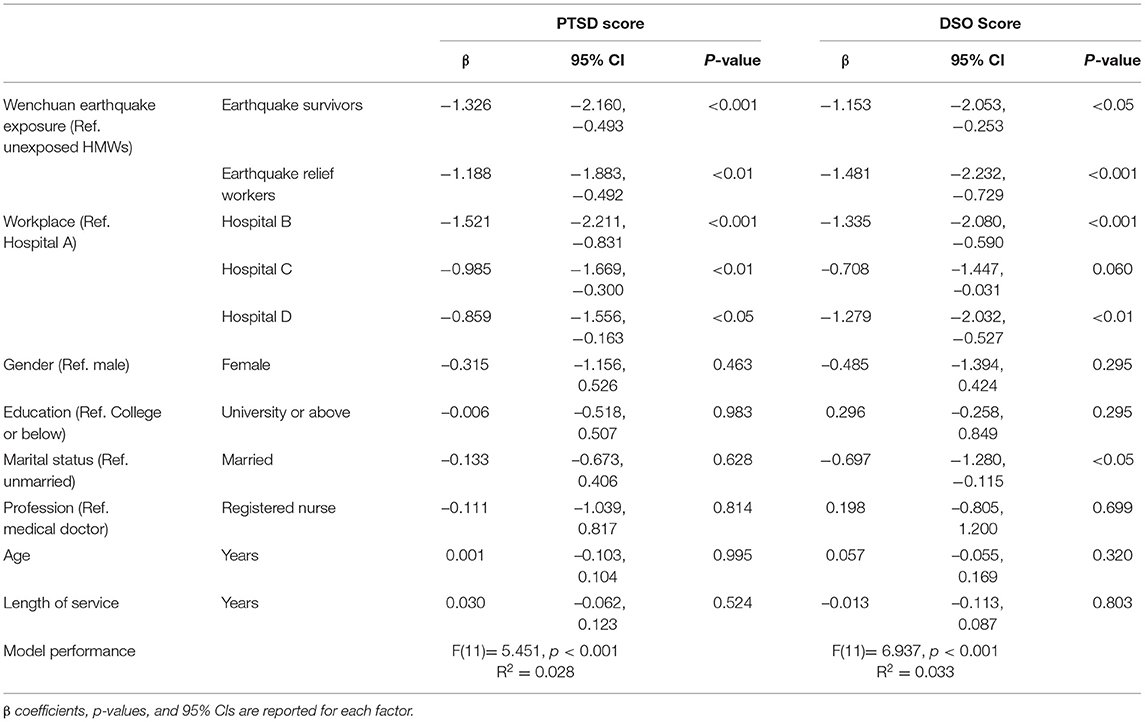
Table 4. Multivariate regression analysis of the effects of disaster exposure and sociodemographic factors on the dimensional scoring of PTSD and DSO.
The type of workplace also had a significant effect on the HMWs' PTSD and DSO scores. Specifically, working in Hospital D (located at the epicenter) was associated with a decrease in the PTSD score of 0.859 SDs (β = −0.859, 95% CI: −1.556, −0.163) and a decrease in the DSO score of 1.279 SDs (β = −1.279, 95% CI: −2.032, −0.527) while holding Wenchuan earthquake exposure and sociodemographic factors constant. Similarly, working in Hospital B (close to the epicenter) was associated with a decrease in the PTSD score of 1.521 SDs (β = −1.521, 95% CI: −2.211, −0.831) and a decrease in the DSO score of 1.335 SDs (β = −1.335, 95% CI: −2.080, −0.590) while holding Wenchuan earthquake exposure and sociodemographic factors constant.
In addition, being married was associated with a decrease in the DSO score of 0.697 SDs (β = −0.697, 95% CI: −1.280, −0.115) while holding Wenchuan earthquake exposure, type of workplace, and other sociodemographic factors constant. Finally, none of the associations of HMWs' PTSD or DSO scores with gender, educational level, profession, age, and length of service was statistically significant (Table 4).
The Structure of ICD-11 PTSD and CPTSD in HMWs
The CFA results are presented in Table 5; Figure 1. The chi-square statistics were significant for all four models. However, Models 1 and 3 were rejected because of their poor fit. Models 2 and 4 had acceptable fits based on the CFI, TLI, RMSEA, and standardized root mean squared residual (SRMR) values. Model 2 demonstrated the highest CFI and TLI values and the lowest RMSEA and SRMR values. However, the ΔCFI and ΔTLI values between Models 2 and 4 were lower than 0.01, and the ΔRMSEA value was lower than 0.015. Thus, the difference in fit between Models 2 and 4 was not significant. Therefore, both Models 2 and 4 had a good fit to examine the constructs of PTSD and CPTSD in HMWs.
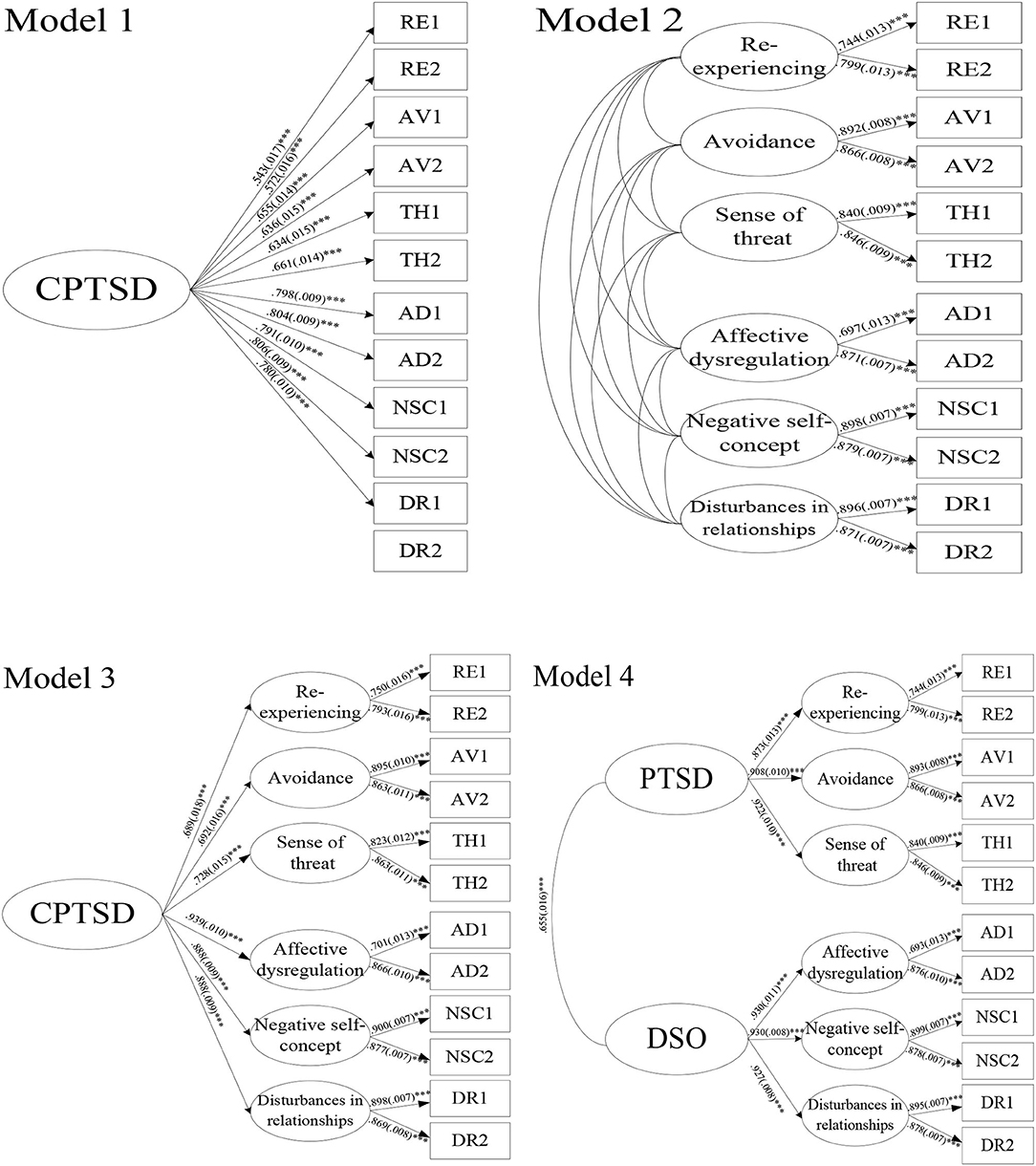
Figure 1. Factor models of ICD-11 PTSD and CPTSD tested using confirmatory factor analysis. The STDYX standardization of estimate and SE for Model 2: RE with AV, 0.802(0.007)***; RE with TH, 0.795(0.016)***; RE with AD, 0.596(0.022)***; RE with NSC, 0.505(0.022)***; RE with DR, 0.508(0.022)***; AV with TH, 0.837(0.012)***; AV with AD, 0.605(0.019)***; AV with NSC, 0.508(0.020)***; AV with DR, 0.525(0.019)***; TH with AD, 0.636(0.019)***; TH with NSC, 0.558(0.020)***; TH with DR, 0.525(0.019)***; AD with NSC, 0.861(0.012)***; AD with DR, 0.855(0.012)***; NSC with DR, 0.875(0.009)***.
All of the factors loaded in Models 2 and 4 were significant (p < 0.001) with coefficients ranging from 0.693 (SE = 0.013, AD1 loaded on affective dysregulation) in Model 4 to 0.930 (SE = 0.008, negative self-concept loaded on DSO; SE = 0.011, affective dysregulation loaded on DSO) in Model 4. All correlations between the six latent factors were significant with coefficients ranging from 0.508 (RE with DR, SE = 0.22; and AV with NSC, SE = 0.20) to 0.875 (NSC with DR, SE = 0.009) in Model 2. In Model 4, the latent factors of RE, AV, and TH constructed the second-layer latent factor of PTSD, while AD, NSC, and DR constructed DSO. PTSD was significantly correlated with DSO with a medium-sized effect (β = 0.655, SE = 0.016).
Discussion
PTSD and CPTSD in HMWs After the Wenchuan Earthquake
The prevalence rate of PTSD and CPTSD in HMWs was low (0.58 and 0.34%, respectively) 11 years after the Wenchuan earthquake. Moreover, none of the participants who reported Wenchuan earthquake exposure were probable for PTSD. After such a long time, many cases of PTSD may have been treated or spontaneously resolved. In some cases, the rescuers who may have had PTSD had left the HMW labor market and could not be recruited for this study. Moreover, in general, the prevalence of PTSD is lower after natural disasters than after manmade disasters (30). For example, the prevalence of PTSD ranged from 7 to 24% (mean 18%) in medical responders in the first 1 or 2 years following the 2004 tsunami in Asia (31), the 2010 Yushu earthquake (32), and the 2011 Great East Japan Earthquake (33). However, after manmade disasters, the prevalence of PTSD has a wide range from 1 to 90% (34–36). The low PTSD prevalence (1%) reported for nurses and doctors during violent events in Judea and Samaria (36) was mostly related to a highly restricted selection process and more comprehensive training. A high prevalence of PTSD was identified during violent wars in 2012 (35, 70%) and Israel-Gaza in 2014 (34, 90%). As these wars continued for a long duration, they may have caused daily traumatic events. Therefore, all HMWs are urged to be equipped with competency-driven, high-quality disaster education and training to enhance their knowledge and skills to meet the global challenge of disasters (9, 10, 37).
The Factors Associated With HMWs' PTSD and CPTSD Scores
The factors that had a significant and positive association with HMWs' PTSD and CPTSD scores were not being exposed to the earthquake and working in a hospital that was distant from the epicenter (i.e., Hospital A). These findings confirm that geographical location has a significant role in an individual's adaptation following a disaster as previously reported (38). Another possible explanation for these findings is that we only examined the effect of Wenchuan earthquake exposure on PTSD and did not evaluate the effects of other natural disasters (e.g., floods) on HMWs' mental health. Hospital A was distant from the epicenter of the Wenchuan earthquake but is located in a coastal area where typhoons, rainstorms, and high tides have become common in recent years (39). For example, in 2016, Typhoon Megi, which landed in Fujian, resulted in 91 deaths, 16 missing persons, and the collapse of 10,203 houses (40). HMWs who were working in Hospital A may have been deployed to the affected area of Fujian and exposed to traumatic incidents during flood relief work, which may have contributed to the development of PTSD in these HMWs (41).
In addition to earthquake exposure and the type of workplace, sociodemographic factors were also associated with HMWs' PTSD and CPTSD scores. An unmarried status was positively associated with PTSD and CPTSD scores, which is consistent with the findings of previous studies (41). This may be due to a lack of family and social support.
The Structure of ICD-11 PTSD and CPTSD in HMWs
The results from the CFA indicate that both the correlated first-order model (Model 2) and the correlated two-layer model (Model 4) had a good fit to explain the structure of PTSD and DSO. The correlated first-order model, which was constructed with three latent variables (RE, AV, and TH) representing PTSD and three latent variables (AD, NSC, and DR) representing DSO, was the model with the best fit. The correlated two-layer model included two second-order latent variables, PTSD and DSO, to explain the covariation among the six first-order factors. These results are consistent with previous studies showing that these two models are generally the best-fitting models (42–44).
Limitations and Further Research
First, this study was limited by its sampling methodology and the unbalanced ratio between medical doctors (18.2%) and registered nurses (81.1%) from the four selected hospitals. This may limit the generalizability of the finding that being a medical doctor predicted the development of PTSD and CPTSD. Second, this study only assessed HMWs' exposure to the Wenchuan earthquake, which occurred 11 years prior to the survey. There may have been other traumatic events during that period that caused PTSD or CPTSD. Therefore, a life event checklist for the past 11 years may be warranted to evaluate the effect of other traumatic events during this period. Third, we used an online self-reported survey, and we did not conduct interviews to make the diagnoses. Finally, this was a cross-sectional study with a non-random sampling strategy. With the recent increase in the number of disasters globally, a long-term longitudinal study is needed to serve as a guide to advocating for the protection of the mental health of healthcare professionals working in hospitals of different sizes.
Conclusions
The findings of this study suggest that HMWs who were exposed to the Wenchuan earthquake rarely reported PTSD or CPTSD 11 years following the disaster. However, psychological support is still necessary for all HMWs, especially for single HMWs working in smaller hospitals. Further research is required to evaluate the mental health status of HMWs using the ICD-11 criteria for PTSD and CPTSD to provide ongoing evidence to help HMWs cope effectively with the challenges of future disasters.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Human Subjects Ethics Sub-Committee in the Hong Kong Polytechnic University (Ref.HSEARS20190416035). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SL and SC designed and performed data collection. CG, SL, and SC analyzed the data. CG and SL drafted the manuscript. All authors contributed to the article and approved the article submission.
Funding
This study was supported by Dean's Reserve Grants (FHSS and FENG) from the Hong Kong Polytechnic University (Project ZZHH).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Thanos Karatzias and Dr. Grace Ho for providing us with valuable guidance on the research tools in both English and Chinese. We also thank Xianqiong Feng, Dr. Xin Jiang, Ms. Shaohua Chen, Ms. Xuemei Luo, and Ms. Rui Xia for their assistance with data collection. We also give special thanks to all of the participants in this study.
References
1. Neria Y, DiGrande L, Adams BG. Posttraumatic stress disorder following the September 11, 2001, terrorist attacks: a review of the literature among highly exposed populations. Am Psychol. (2011) 66:429–46. doi: 10.1037/a0024791
2. Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatr Interpers Biol Process. (2002) 65:207–39. doi: 10.1521/psyc.65.3.207.20173
3. Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: part I Summary I. and implications of the disaster mental health research. Psychiatr Interpers Biol Process. (2002) 65:240–60. doi: 10.1521/psyc.65.3.240.20169
4. Setti I, Argentero P. Traumatization PTSD in rescue workers: prevention, assessment, interventions. In: Martin C, Preedy V, Patel V, editors. Comprehensive Guide to Post-Traumatic Stress Disorders. Cham: Springer. (2016).
5. Guo C, Li S, Chan S. Long-term effects of disaster exposure on health care workers' resilience: A comparison of the Wenchuan earthquake-exposed and unexposed groups. Int J Dis Risk Reduct. (2022) 67:102658. doi: 10.1016/j.ijdrr.2021.102658
6. Mattei A, Fiasca F, Mazzei M, Necozione S, Bianchini V. Stress and burnout in health-care workers after the 2009 L'Aquila Earthquake: a cross-sectional observational study. Front Psychiatr. (2017) 8:98. doi: 10.3389/fpsyt.2017.00098
7. Jacobs M, Harville E. Long-term mental health among low-income, minority women following exposure to multiple natural disasters in early and late adolescence compared to adulthood. Child Youth Care Forum. (2015) 44:511–25. doi: 10.1007/s10566-015-9311-4
8. Zhang L, Liu X, Li Y, Liu Y, Liu Z, Lin J, et al. Emergency medical rescue efforts after a major earthquake: lessons from the 2008 Wenchuan earthquake. Lancet. (2012) 379:853–61. doi: 10.1016/S0140-6736(11)61876-X
9. Loke AY, Guo C, Molassiotis A. Development of disaster nursing education and training programs in the past 20 years 2000–2019: a systematic review. Nurse Educ Today. (2021) 99:104809. doi: 10.1016/j.nedt.2021.104809
10. Loke AY, Li S, Guo C. Mapping a postgraduate curriculum in disaster nursing with the International Council of Nursing's Core Competencies in Disaster Nursing V2.0: the extent of the program in addressing the core competencies. Nurse Educ Today. (2021) 106:105063. doi: 10.1016/j.nedt.2021.105063
11. Zhen Y, Huang ZQ, Jin J, Deng XY, Zhang LP, Wang JG. Posttraumatic stress disorder of Red Cross nurses in the aftermath of the 2008 Wenchuan China earthquake. Arch Psychiatr Nurs. (2012) 26:63–70. doi: 10.1016/j.apnu.2011.02.004
12. Liang Y, Cheng J, Ruzek JI, Liu Z. Posttraumatic stress disorder following the 2008 Wenchuan earthquake: A 10-year systematic review among highly exposed populations in China. J Affect Disord. (2019) 243:327–39. doi: 10.1016/j.jad.2018.09.047
13. Wang L, Zhang J, Zhou M, Shi Z, Liu P. Symptoms of posttraumatic stress disorder among health care workers in earthquake-affected areas in southwest China. Psychol Rep. (2010) 106:555–61. doi: 10.2466/pr0.106.2.555-561
14. Schenk EJ, Yuan J, Martel LD, Shi GQ, Han K, Gao X. Risk factors for long-term post-traumatic stress disorder among medical rescue workers appointed to the 2008 Wenchuan earthquake response in China. Disasters. (2017) 41:788–802. doi: 10.1111/disa.12222
15. Yin M, Li XL, Ma Y, Wu XH, Zhu SC. Post-traumatic stress disorder in nurses n hard-hit areas after Wenchuan earthquake 2 years later. Chin Mental Health J. (2013) 27:155–6. doi: 10.2147/NDT.S247527
16. Guo J, Wu P, Tian D, Wang X, Zhang W, Zhang X, et al. Post-traumatic stress disorder among adult survivors of the Wenchuan earthquake in China: a repeated cross-sectional study. J Anx Disord. (2014) 28:75–82. doi: 10.1016/j.janxdis.2013.12.001
17. Brewin CR, Cloitre M, Hyland P, Shevlin M, Maercker A, Bryant RA, et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin Psychol Rev. (2017) 58:1–15. doi: 10.1016/j.cpr.2017.09.001
18. First MB, Reed GM, Hyman SE, Saxena S. The development of the ICD-11 clinical descriptions and diagnostic guidelines for mental and behavioural disorders. World Psychiatr. (2015) 14:82–90. doi: 10.1002/wps.20189
19. McNally RJ, Robinaugh DJ, Wu GW, Wang L, Deserno MK, Borsboom D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clin Psychol Sci. (2015) 3:836–49. doi: 10.1177/2167702614553230
20. Li J, Wang W, Hu W, Yuan Z, Zhou R, Zhang W, et al. Validation of posttraumatic stress disorder (PTSD) and complex PTSD in Chinese children as per the ICD-11 proposals using the International trauma questionnaire. Eur J Psychotraumatol. (2021) 12:1888525. doi: 10.1080/20008198.2021.1888525
21. Bryant RA, Creamer M, O'Donnell M, Forbes D, McFarlane AC, Silove D, et al. Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: A network analysis. JAMA Psychiatry. (2017) 74:135–42. doi: 10.1001/jamapsychiatry.2016.3470
22. La Greca AM, Danzi BA, Chan SF. DSM-5 and ICD-11 as competing models of PTSD in preadolescent children exposed to a natural disaster: assessing validity and co-occurring symptomatology. Eur J Psychotraumatol. (2017) 8:1310591. doi: 10.1080/20008198.2017.1310591
23. Cloitre M, Shevlin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, et al. The International Trauma Questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Act Psychiatr Scand. (2018) 138:536–46. doi: 10.1111/acps.12956
24. Haselgrube A, Solva K, Lueger-Schuster B. Validation of ICD-11 PTSD and complex PTSD in foster children using the International Trauma Questionnaire. Act Psychiatr Scand. (2020) 141:60–73. doi: 10.1111/acps.13100
25. Ho GW, Hyland P, Shevlin M, Chien WT, Inoue S, Yang PJ, et al. The validity of ICD-11 PTSD and complex PTSD in East Asian cultures: findings with young adults from China, Hong Kong, Japan, and Taiwan. Eur J Psychotraumatol. (2020) 11:1717826. doi: 10.1080/20008198.2020.1717826
26. Kazlauskas E, Zelviene P, Daniunaite I, Hyland P, Kvedaraite M, Shevlin M, et al. The structure of ICD-11 PTSD and complex PTSD in adolescents exposed to potentially traumatic experiences. J Affect Disord. (2020) 265:169–74. doi: 10.1016/j.jad.2020.01.061
27. Buhi ER, Goodson P, Neilands TB. Structural equation modeling: a primer for health behavior researchers. Am J Health Behav. (2007) 31:74–85. doi: 10.5993/AJHB.31.1.8
28. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equat Model Multidiscipl J. (1999) 6:1–55. doi: 10.1080/10705519909540118
29. Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equat Model Multidiscipl J. (2007) 14:464–504. doi: 10.1080/10705510701301834
30. Naushad VA, Bierens JJ, Nishan KP, Firjeeth CP, Mohammad OH, Maliyakkal AM, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Dis Med. (2019) 34:632–43. doi: 10.1017/S1049023X19004874
31. Armagan E, Engindeniz Z, Devay AO, Eurdur B, Ozcakir A. Frequency of post-traumatic stress disorder among relief force workers after the tsunami in Asia: do rescuers become victims? Prehosp Dis Med. (2006) 21:168–72. doi: 10.1017/S1049023X00003630
32. Kang P, Lv Y, Hao L, Tang B, Liu Z, Liu X, et al. Psychological consequences and quality of life among medical rescuers who responded to the 2010 Yushu earthquake: a neglected problem. Psychiatry Res. (2015) 230:517–23. doi: 10.1016/j.psychres.2015.09.047
33. Sakuma A, Takahashi Y, Ueda I, Sato H, Katsura M, Abe M, et al. Post-traumatic stress disorder and depression prevalence and associated risk factors among local disaster relief and reconstruction workers fourteen months after the Great East Japan Earthquake: a cross-sectional study. BMC Psychiatry. (2015) 15:1–13. doi: 10.1186/s12888-015-0440-y
34. Abu-El-Noor NI, Aljeesh YI, Radwan AS, Abu-El-Noor MK, Qddura IAI, Khadoura KJ, et al. Post-traumatic stress disorder among health care providers following the Israeli attacks against Gaza Strip in 2014: A call for immediate policy actions. Arch Psychiatr Nurs. (2016) 30:185–91. doi: 10.1016/j.apnu.2015.08.010
35. Alhajjar B. Gaza nurses after war: are they traumatized? Proc Soc Behav Sci. (2014) 114:802–9. doi: 10.1016/j.sbspro.2013.12.789
36. Lubin G, Sids C, Vishne T, Shochat T, Ostfield Y, Shmushkevitz M. Acute stress disorder and post-traumatic stress disorder among medical personnel in Judea and Samaria areas in the years 2000–2003. Mil Med. (2007) 172:376–8. doi: 10.7205/MILMED.172.4.376
37. Molassiotis A, Guo C, Abu-Odah H, West C, Loke AY. Evolution of disaster nursing research in the past 30 years (1990–2019): a bibliometric and mapping analysis. Int J Dis Risk Reduct. (2021) 58:102230. doi: 10.1016/j.ijdrr.2021.102230
38. Guo C, Sim T, Su G. Individual disaster preparedness in drought-and-flood-prone villages in northwest china: impact of place, out-migration and community. Int J Environ Res Public Health. (2021) 18:1649. doi: 10.3390/ijerph18041649
39. Flood Control and Drought Relief in China. National flood disasters in 2017: a literature review. Flood Drought Dis. (2018) 28:60–6. (In Chinese).
40. Lin F. A brief discussion on typhoon flood disasters in Fuzhou, Fujian from 2013-2016. Flood Control Drought Relief China. (2018) 28:41–4. (In Chinese).
41. Lowell A, Suarez-Jimenez B, Helpman L, Zhu X, Durosky A, Hilburn A, et al. 9/11-related PTSD among highly exposed populations: a systematic review 15 years after the attack. Psychol Med. (2018) 48:537–53. doi: 10.1017/S0033291717002033
42. Ben-Ezra M, Karatzias T, Hyland P, Brewin CR, Cloitre M, Bisson JI, et al. Posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) as per ICD-11 proposals: a population study in Israel. Depress Anxiety. (2018) 35:264–74. doi: 10.1002/da.22723
43. Hyland P, Shevlin M, Brewin CR, Cloitre M, Downes AJ, Jumbe S, et al. Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International Trauma Questionnaire. Act Psychiatr Scand. (2017) 136:313–22. doi: 10.1111/acps.12771
44. Karatzias T, Shevlin M, Fyvie C, Hyland P, Efthymiadou E, Wilson D, et al. An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): evidence of construct validity. J Anxiety Disord. (2016) 44:73–9. doi: 10.1016/j.janxdis.2016.10.009
Appendix I
Keywords: posttraumatic stress disorder, complex PTSD, hospital medical workers, 2008 Wenchuan earthquake, cross-sectional study, Sichuan
Citation: Li S, Guo C and Chan SSS (2022) ICD-11 Posttraumatic Stress Disorder and Complex PTSD Among Hospital Medical Workers in China: Impacts of Wenchuan Earthquake Exposure, Workplaces, and Sociodemographic Factors. Front. Psychiatry 12:735861. doi: 10.3389/fpsyt.2021.735861
Received: 03 July 2021; Accepted: 09 December 2021;
Published: 17 January 2022.
Edited by:
Umberto Volpe, Marche Polytechnic University, ItalyReviewed by:
Cai-Lan Hou, Guangdong Mental Health Center, ChinaSimone Pompili, Marche Polytechnic University, Italy
Copyright © 2022 Li, Guo and Chan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunlan Guo, Y2h1bmxhbmd1b0BvdXRsb29rLmNvbQ==
 Sijian Li
Sijian Li Chunlan Guo1,2*
Chunlan Guo1,2*