
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 29 September 2021
Sec. Psychopharmacology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.728204
This article is part of the Research Topic Rising Stars in Psychopharmacology View all 5 articles
 Ling Zhang1*†
Ling Zhang1*† Han Qi2†
Han Qi2† Yun-Yi Xie1†
Yun-Yi Xie1† Wei Zheng3†
Wei Zheng3† Xiao-Hui Liu1†
Xiao-Hui Liu1† Dong-Bin Cai4†
Dong-Bin Cai4† Chee H. Ng5
Chee H. Ng5 Gabor S. Ungvari6,7
Gabor S. Ungvari6,7 Yu-Tao Xiang8,9,10*
Yu-Tao Xiang8,9,10*Aripiprazole, metformin, and paeoniae–glycyrrhiza decoction (PGD) have been widely used as adjunctive treatments to reduce antipsychotic (AP)-induced hyperprolactinemia in patients with schizophrenia. However, the comparative efficacy and safety of these medications have not been previously studied. A network meta-analysis of randomized controlled trials (RCTs) was conducted to compare the efficacy and safety between aripiprazole, metformin, and PGD as adjunctive medications in reducing AP-induced hyperprolactinemia in schizophrenia. Both international (PubMed, PsycINFO, EMBASE, and Cochrane Library databases) and Chinese (WanFang, Chinese Biomedical, and Chinese National Knowledge infrastructure) databases were searched from their inception until January 3, 2019. Data were analyzed using the Bayesian Markov Chain Monte Carlo simulations with the WinBUGS software. A total of 62 RCTs with 5,550 participants were included in the meta-analysis. Of the nine groups of treatments included, adjunctive aripiprazole (<5 mg/day) was associated with the most significant reduction in prolactin levels compared to placebo (posterior MD = −65.52, 95% CI = −104.91, −24.08) and the other eight treatment groups. Moreover, adjunctive PGD (>1:1) was associated with the lowest rate of all-cause discontinuation compared to placebo (posterior odds ratio = 0.45, 95% CI = 0.10, 3.13) and adjunctive aripiprazole (>10 mg/day) was associated with fewer total adverse drug events than placebo (posterior OR = 0.93, 95% CI = 0.65, 1.77) and other eight treatment groups. In addition, when risperidone, amisulpride, and olanzapine were the primary AP medications, adjunctive paeoniae/glycyrrhiza = 1:1, aripiprazole <5 mg/day, and aripiprazole >10 mg/day were the most effective treatments in reducing the prolactin levels, respectively. Adjunctive aripiprazole, metformin, and PGD showed beneficial effects in reducing AP-induced hyperprolactinemia in schizophrenia, with aripiprazole (<5 mg/day) being the most effective one.
Hyperprolactinemia (HPRL) is a common adverse effect of antipsychotics (APs), related to the blocking of dopamine receptors (1), which occurs in around 70% patients receiving AP medications (2). The normal plasma level of prolactin is below 25 ng/ml for women and below 20 ng/ml for men, and HPRL refers to sustained prolactin levels above normal (3). HPRL is usually asymptomatic and does not affect the quality of life of patients, but preclinical and clinical evidence indicate that persistent HPRL is associated with an increased risk of sexual dysfunction, weight gain, cardiovascular diseases, and certain mental health problems (e.g., depression) and even cancers (4–6).
Aripiprazole has been shown to effectively reduce the prolactin level due to its partial inhibition of D2 receptors (7). Recently, aripiprazole has been recommended in the guidelines for the treatment of AP-induced HPRL (8). However, aripiprazole is associated with side effects, such as sedation, insomnia, and headache, in some patients (9). Consequently, alternative treatments, such as adjunctive metformin and paeoniae–glycyrrhiza decoction (PGD), have been trialed for AP-induced HPRL.
As a first-line antidiabetic drug, previous studies have found that metformin may reduce weight, insulin resistance, and prolactin levels in patients receiving APs (10). Other studies have also found the benefit of PGD in reducing AP-induced HPRL (11). PGD is a traditional herbal medicine with active ingredients of paeoniae (“shaoyao” in Chinese) and glycyrrhiza (“Gancao” in Chinese), which could modulate D2 receptor expression, inhibit P450 enzymes, and is well-tolerated in schizophrenia patients (12).
The efficacy of aripiprazole, metformin, and PGD in reducing AP-induced HPRL has been separately examined in previous meta-analyses (13–15), but their comparative efficacy and safety have not yet been studied. Network meta-analysis (NMA) is a widely used method which integrates both direct and indirect comparisons based on frequentist model or Bayesian model (16). We thus conducted this NMA of randomized controlled trials (RCTs) to compare the efficacy and safety of aripiprazole, metformin, and PGD as adjunctive medications in reducing AP-induced HPRL in schizophrenia.
This NMA was conducted according to the Preferred Reporting Items of Systematic Review and Meta-analysis-NMA statement (17) and registered in the international prospective register of systematic reviews (PROSPERO: CRD42018088004).
Literature search was performed following the PICOS acronym: participants—adult patients with schizophrenia or schizophrenia spectrum disorders according to study-defined diagnostic criteria; interventions—primary AP plus adjunctive aripiprazole or metformin or PGD; comparators—primary AP plus placebo or AP monotherapy; outcomes—the primary outcome was the mean change of prolactin levels (ng/ml) between baseline and endpoint, while the secondary outcomes included the change in psychotic symptoms as measured by the Positive and Negative Syndrome Scale (PANSS) (18) or Brief Psychiatric Rating Scale (BPRS) (19), adverse drug reactions (e.g., akathisia, somnolence, drooling, fatigue, dizziness, dry mouth, insomnia, and nausea), and all-cause discontinuation; and study type—RCTs with available data on the efficacy and safety of adjunctive aripiprazole, metformin, and paeoniae–glycyrrhiza decoction for AP-induced hyperprolactinemia. Moreover, head-to-head trials that compared adjunctive aripiprazole, metformin, and PGD with each other were included, if any. RCTs that used aripiprazole, metformin, or PGD as the primary medications for schizophrenia were excluded.
Three researchers (YX, XL, and DC) independently searched both international (PubMed, PsycINFO, EMBASE, and Cochrane Library databases) and Chinese (WanFang, Chinese Biomedical, and Chinese National Knowledge infrastructure) databases from inception dates to January 3, 2019 using the combination of medical subject headings and free search terms (Supplementary Materials).
Subsequently, three researchers (YX, XL, and DC) independently screened the title and abstract and then read the full text of the relevant papers. The reference lists of relevant review articles were also checked for additional studies. The first or corresponding authors of related studies were contacted for additional information, if necessary. Any discrepancies in the study selection were resolved by a discussion with a fourth researcher (WZ).
Two researchers (YX and XL) independently extracted relevant data using a standardized Excel sheet, such as the first author, publication year, country, blinding assessment, use of primary APs and adjunctive medications, diagnosis criteria of schizophrenia, prolactin level, psychotic symptoms, and adverse drug events. Data in figures were extracted using GetData Graph Digitizer 2.2.6 (http://www.getdata-graph-digitizer.com).
The Cochrane risk of bias (20) and Jadad scale with three domains (randomization, double blinding, and description withdrawals and dropouts) (21) were used to evaluate the study quality. A Jadad total score of ≥3 was defined as “high quality” (21). The overall quality evidence was examined by the grading of recommendation assessment, development, and evaluation (GRADE) system (22).
The Bayesian Markov Chain Monte Carlo simulation was used to establish the NMA model with the WinBUGS software (MRC Biostatistics Unit, Cambridge, UK) (23). Each chain used 20,000 iterations using a burn-in number of 10,000, with a thin interval of 1. We modeled the mean changes of prolactin levels with standard deviations and reported posterior mean difference (MD) with 95% confidence intervals (CIs). The concentration unit of prolactin was unified into nanogram per milliliter using a relevant conversion formula. Standard mean difference (SMD) with 95% CI was calculated as the effect size when pooling the pair-wise results of prolactin level changes. For all-cause discontinuation and adverse drug events, we modeled the odds ratio (OR) with 95%CI.
Use of the random or fixed effects model was determined by the deviance information criteria (DIC), and the model with a smaller DIC was used to perform the NMA (24). In this NMA, the random effects model was used due to a smaller DIC of 1,212.77 (DIC for fixed effects model was 1,309.82). Node-split method was used to calculate the inconsistency between direct and indirect evidence (25). We compared the efficacy of adjunctive aripiprazole, metformin, and PGD using the surface under the cumulative ranking curve (SUCRA), with the higher area under the curve combined with the higher probability of the best rank indicating better efficacy (26). The final ranks were determined according to the results of Bayesian analyses and SUCRA. Heterogeneity was assessed using I2 (27), with I2 of >50% indicating great heterogeneity. Subgroup (for categorical variables), meta-regression (for continuous variables), and sensitivity analyses were preformed to examine the sources of heterogeneity. Funnel plot and Egger's test were used to assess the pulication bias (28). RCTs with multiple arms were split into several two-arms trials when inputting into Stata (29) (e.g., a RCT with three treatment arms was split into three two-arm studies); therefore, the total number of studies and the overall sample size in Stata (n = 87, sample size = 6,567) were more than in WinBUGS (n = 62, sample size = 5,550). P < 0.05 was considered statistically significant, with a two-sided test. If adjunctive aripiprazole, metformin, or PGD were used with the same primary AP, additional NMAs for these studies were performed to directly compare the efficacy of adjunctive aripiprazole, metformin, or PGD in reducing prolactin levels.
In total, 550 studies were initially identified and, finally, 62 studies with 5,550 participants were included for the analyses. Figure 1 shows the flow chart of the study selection. Fifty-three RCTs used adjunctive aripiprazole, five RCTs used adjunctive PGD, and four RCTs used adjunctive metformin (Table 1). According to the type of primary APs, NMAs were conducted to compare the efficacy and safety of adjunctive aripiprazole, PGD, and metformin in reducing proclatin levels as follows: any primary APs (62 RCTs), risperidone (22 RCTs), amisulpride (eight RCTs), and olanzapine (seven RCTs). For 25 RCTs with other primary APs (e.g., paliperidone, sulpiride, chlorpromazine, perphenazine, haloperidol, quetiapine, and multiple APs), NMA was not conducted due to the small number of studies and different types of control.
According to the doses of adjunctive aripiprazole, PGD, and metformin, nine groups of treatment were established: aripiprazole (<5 mg/day, n = 2; 5 mg/day, n = 29; 5–10 mg/day, n = 16; >10 mg/day, n = 14), metformin (<1,000 mg/day, n = 3; ≥1,000 mg/day, n = 2), PGD (paeoniae/glycyrrhizae = 1:1, n = 3; paeoniae/glycyrrhizae >1:1, n = 3), and placebo (n = 62) (Figures 2A,B). Following other NMAs (90), the doses are classified according to commonly clinically prescribed dose and the median doses used in the included studies. Eight RCTs had multiple treatment arms that compared different doses of adjunctive aripiprazole, PGD, and metformin (Table 1). The mean age of the participants was 35.2 years, and the median trial duration was 8 weeks. Twenty-three RCTs only included females, while seven RCTs included males. All 62 RCTs reported changes of prolactin levels from baseline to endpoint, while 41 RCTs reported a change in psychotic symptoms as measured by PANSS, 25 reported all-cause discontinuation, and 27 reported adverse drug events.
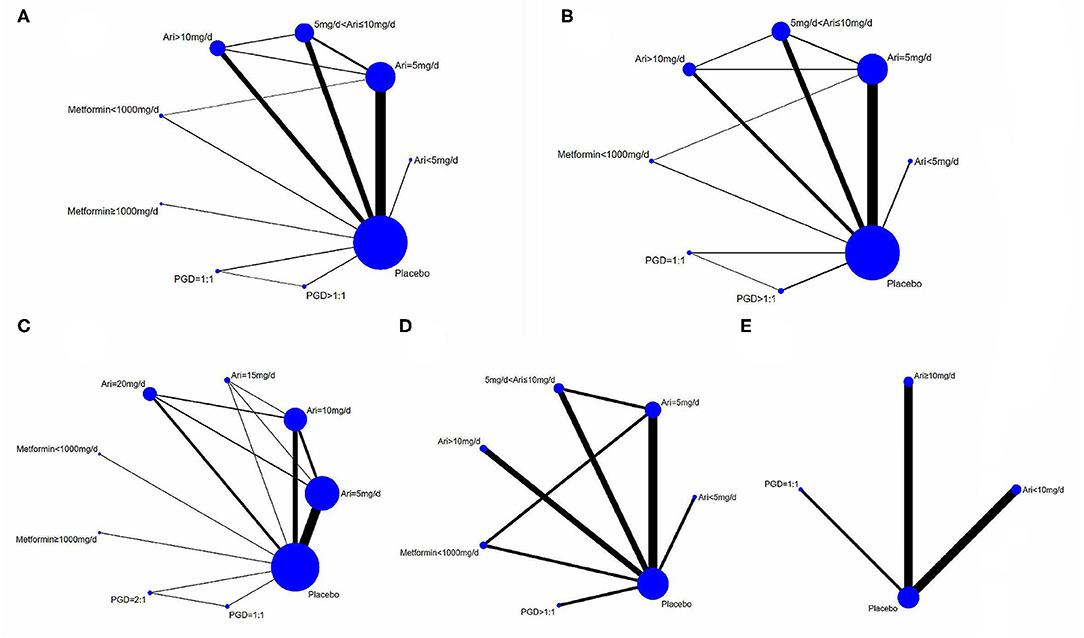
Figure 2. Direct comparison of adjunctive aripiprazole, metformin and PGD in the treatment of hyperprolactinemia for schizophrenic patients. (A) Direct comparisons of adjunctive aripiprazole, metformin and PGD for reducing prolactin levels with all primary antipsychotics. (B) Direct comparisons of adjunctive aripiprazole, metformin and PGD in PANSS score changes with all primary antipsychotics. (C–E) Direct comparisons of adjunctive aripiprazole, metformin and PGD for reducing prolactin levels when using risperidone, amisulpride and olanzapine respectively as primary antipsychotics, respectively.
In the assessment of Cochrane risk of bias, 59 of the 62 studies had a low risk in randomization, and three (48, 62, 68) had a high risk as the patients were randomized to different groups according to the sequence of treatments. The allocation concealment was clearly described in six RCTs but unclear in 45 RCTs and showed a high risk in 11 RCTs. Thirteen RCTs were double-blind, 11 were single-blind, 16 were open-label, and the others did not use blinding methods. Ten RCTs had an unclear risk of bias in incomplete outcome data as they did not report the reasons for the missing data (Supplementary Table 1 and Supplementary Figures 1, 2). The Jadad assessment showed that 41 RCTs (66.1%) were of high quality (Jadad total score ≥3).
The results of GRADE were performed according to direct, indirect, and NMA results separately. In the five node-split direct comparisons, three were considered moderate grade and two were low grade of evidence. Of the 36 indirect comparisons, three (8.3%) were “high” quality, three (8.3%) were “moderate,” four (11.1) were “low,” and others were “very low” (72.2%) grades of evidence. Similarly, of the 36 NMA comparisons, the evidence ranged from “very low” (69.4%), “low” (8.3%), “moderate” (8.3%) to “high” (11.1%) grade. The principal reasons for down-grading included indirectness, large 95%CI, and potential publication bias (Supplementary Table 2).
Across the 62 studies, the overall pooled prolactin level decreased from baseline to endpoint significantly when using adjunctive aripiprazole, metformin, or PGD (SMD = −1.29, 95% CI = −1.35, −1.23, P < 0.01, I2 = 96.5%). In NMA, adjunctive aripiprazole at <5 mg/day showed the most significant decrease in prolactin levels when compared to placebo (posterior MD = −65.52, 95% CI = −104.91, −24.08) and the other eight treatment groups (Table 2) (the best probability, PrBest = 56.3%) (Table 3), followed by aripiprazole at >10 mg/day (posterior MD = −45.85, 95% CI = −60.69, −31.55) and aripiprazole at 5 mg/day (posterior MD = −45.59, 95% CI = −55.89, −35.75).
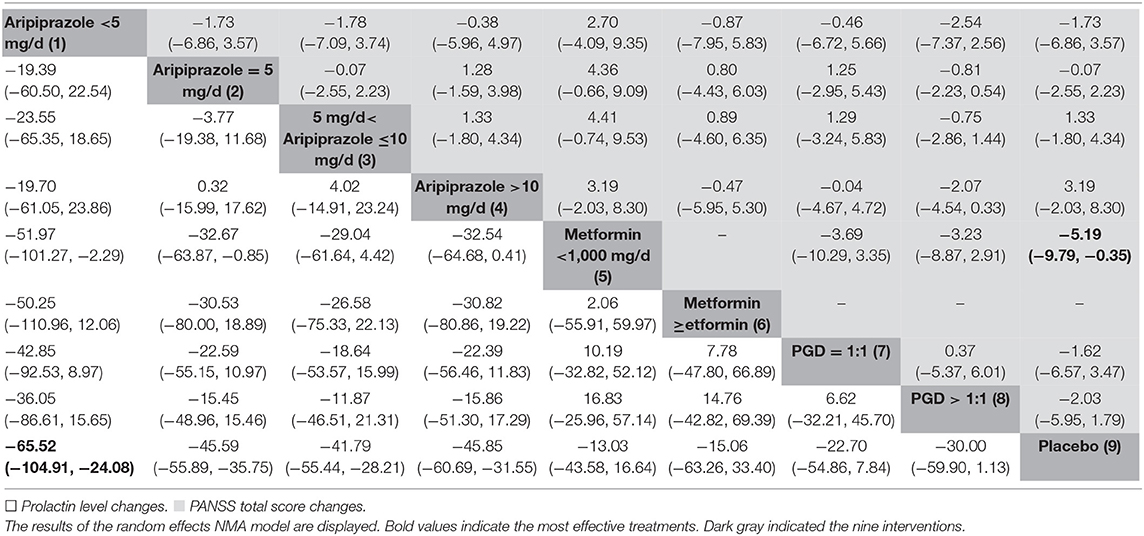
Table 2. Network meta-analysis of adjunctive aripiprazole, metformin, and PGD with regard to the mean changes of prolactin levels and PANSS total scores in schizophrenia [mean differences (95% CI)].
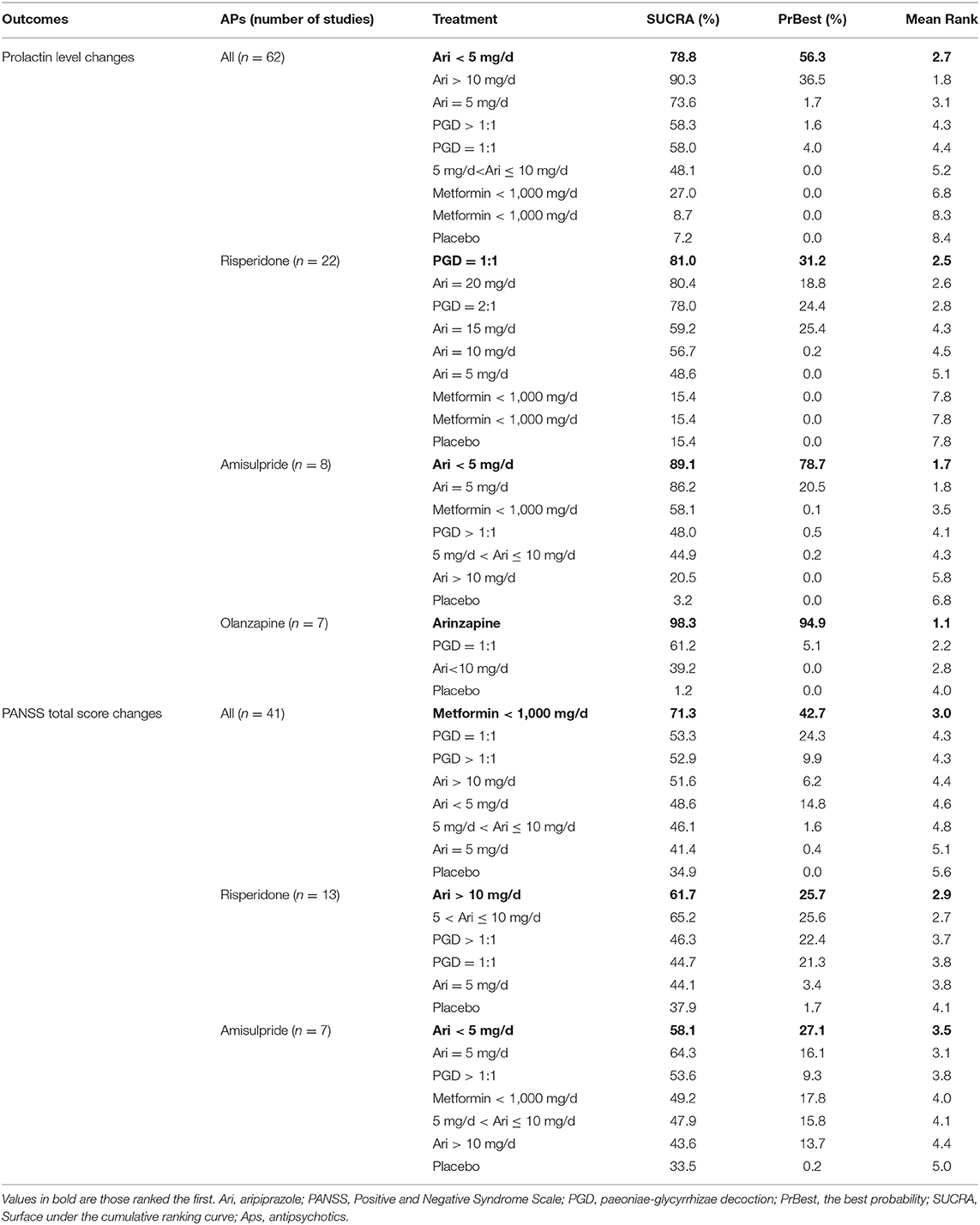
Table 3. Rankings of adjunctive aripiprazole, metformin and PGD in reducing prolactin levels in schizophrenia.
Similarly, a reduction of PANSS total scores was significantly associated with the use of adjunctive aripiprazole, metformin, and PGD (SMD = −0.12, 95% CI = −1.80, −0.06; P < 0.01, I2 = 60.7%). In NMA, metformin at <1,000 mg/day was most efficacious in reducing the total PANSS score compared to placebo (posterior MD = −5.19, 95% CI = −9.79, −0.35; PrBest = 42.7%) and the other seven treatment groups (Tables 2, 3), followed by PGD = 1:1 (posterior MD = −1.62, 95% CI = −6.57, 3.47). The analyses of BPRS total score were not performed due to an insufficient number of studies.
The NMA of all-cause discontinuation and adverse drug events was performed to evaluate the tolerability and safety of the three adjunctive medications separately. Of the nine treatment groups, PGD >1:1 had the lowest rate of all-cause discontinuation compared to placebo (posterior OR = 0.45, 95% CI = 0.10, 3.13) and the other eight treatment groups (Supplementary Table 3). Moreover, aripiprazole at >10 mg/day led to fewer total adverse drug events than placebo (posterior OR = 0.93, 95% CI = 0.65, 1.77) and other groups (Supplementary Table 3). For akathisia reported in 10 RCTs, aripiprazole at >10 mg/day showed a lower number of akathisia than placebo (posterior OR = 0.77, 95% CI = 0.25, 2.39), aripiprazole = 5 mg/day (posterior OR = 0.94, 95% CI = 0.18, 4.47), PGD = 1:1 (posterior OR = 0.39, 95% CI = 0.01, 4.91), and PGD >1:1 (posterior OR = 0.38, 95% CI = 0.05, 5.24). For somnolence, which was reported in 10 RCTs, aripiprazole at <5 mg/day had fewer somnolence than placebo (posterior OR <0.01, 95% CI = 0.00, 2.02) and the other five treatment groups. Aripiprazole at <5 mg/day had likewise the lower number of insomnia (19 RCTs) and nausea (six RCTs) than placebo (posterior OR = 0.81, 95% CI = 0.01, 50.15 for insomnia; posterior OR <0.01, 95% CI = 0.00, 0.65 for nausea) and the other groups. In 14 RCTs with data on headaches, PGD = 1:1 had a lower frequency of headache than placebo (posterior OR = 0.44, 95% CI = 0.00, 41.04) and the other groups.
Twenty-two RCTs used risperidone as primary AP, and the network plot is shown in Figure 2C. In total, nine treatment groups were examined. The pooled pair-wise SMD of adjunctive aripiprazole, metformin, and PGD regarding prolactin level change from baseline to endpoint was −1.28, 95% CI (−1.36, −1.20), P < 0.01, I2 = 94.8%. NMA showed that PGD = 1:1 had the most significant effect on prolactin reduction compared to placebo (posterior MD = −47.58, 95% CI = −114.5, −45.4) and other treatment groups (Supplementary Table 4).
When compared with placebo and other medications, aripiprazole at >10 mg/day had the most significant effect in reducing the PANSS total score from baseline to endpoint across 13 RCTs with the posterior MD of −4.09, 95%CI: −6.55, −1.12 (PrBest = 25.7%). The NMA of all-cause discontinuation and ADRs were not performed due to insufficient studies.
Eight studies reported a change in prolactin levels with amisulpride as the primary AP. The direct comparisons are shown in Figure 2D. The pooled SMD of adjunctive aripiprazole, metformin, and PGD for the change in prolactin levels was −1.24, 95% CI (−1.42, −1.06), P < 0.01, I2 = 98%. NMA revealed that aripiprazole at <5 mg/day had the most significant effect in reducing the prolactin levels compared to placebo (posterior MD = −74.30, 95% CI = −163.30, −73.88) and the other treatment groups (Table 3 and Supplementary Table 5), followed by aripiprazole at 5 mg/day (posterior MD = −74.30, 95% CI = −163.30, −73.88) and metformin <1,000 mg/day (posterior MD = −25.60, 95% CI = −37.47, −13.75) (Supplementary Table 5). In addition, aripiprazole at <5 mg/day showed the most significant decrease in PANSS total score compared to placebo (posterior MD = −6.76, 95% CI = −83.70, 74.23), followed by aripiprazole at 5 mg/day (posterior MD = −1.65, 95% CI = −42.78, 42.46).
Seven RCTs which used adjunctive aripiprazole, metformin, or PGD reported prolactin level reduction with olanzapine as the primary AP. The pooled pair-wise SMD was −2.51, 95% CI (−2.73, −2.28), P < 0.01, I2 = 96.5%. Aripiprazole at ≥10 mg/day showed a significant reduction of prolactin levels compared to placebo (posterior MD = −33.77, 95% CI = −51.34, −24.86), followed by aripiprazole at <10 mg/day (posterior MD = −27.64, 95% CI = −45.11, −9.18) and PGD = 1:1 (posterior MD = −17.56, 95% CI = −41.96, −18.23) (Supplementary Table 6). The NMA of PANSS total changes, all-cause discontinuation, and ADRs was not performed due to insufficient studies.
The node-split method was performed to explore the inconsistency of prolactin changes between direct and indirect comparisons within loops. Overall, no significant inconsistencies in aripiprazole at 5 mg/day vs. 5 mg/day < aripiprazole ≤ 10 mg/day (P = 0.25), aripiprazole = 5 mg/day vs. aripiprazole >10 mg/day (P = 0.19), aripiprazole = 5 mg/day vs. metformin <1,000 mg/day (P = 0.42), 5 mg/day < aripiprazole ≤ 10 mg/day vs. aripiprazole >10 mg/day (P = 0.83), PGD = 1:1 vs. PGD >1:1 (P = 0.83) were found in primary APs. The details are shown in the GRADE evaluation (Supplementary Table 2). Both Funnel plot and Egger's test found obvious publication bias (t = −9.91, P < 0.01) in the 62 RCTs. Moreover, “trim and fill” method was used, and the “correct” estimations of pooled SMD was −2.18, 95% CI (−2.50, −1.86).
Supplementary Table 7 shows the subgroup analyses of the efficacy of adjunctive aripiprazole, metformin, and PGD in reducing prolactin levels. RCTs which were of single blind design (SMD = −2.45, 95%CI: −2.63, −2.26), involving both male and female genders (SMD = −1.45, 95%CI: −1.54, −1.37), using the CCMD-III (SMD=-1.82, 95%CI: −1.92, −1.71), and having smaller sample size (SMD=-1.50, 95%CI: −1.60, −1.41) exhibited a more obvious reduction in prolactin levels. Meta-regression analyses revealed that mean age (P = 0.27), Jadad quality score (P = 0.11), trial duration (P = 0.46), and total sample size (P = 0.99) were not significantly associated with the heterogeneity of the pooled results. The blinding method was significantly associated with the great heterogeneity (P = 0.03) and explained 4.8% of the heterogeneity.
To the best of our knowledge, this was the first NMA to compare the efficacy and safety of adjunctive aripiprazole, metformin, and PGD in reducing AP-induced HPRL for schizophrenia. The results showed that aripiprazole (<5 mg/day) was associated with the most significant decrease in AP-induced prolactin levels when compared to placebo and other treatments. The NMA also found that adjunctive PGD (1:1) had the most significant effect in reducing risperidone-induced HPRL. Adjunctive aripiprazole (<5 mg/day) had the most significant effect in reducing amisulpride-induced HPRL, and aripiprazole (>10 mg/day) had the most significant effect in reducing olanzapine-related HPRL. Moreover, PGD (>1:1) was associated with the lowest rate of all-cause discontinuation, and aripiprazole (>10 mg/day) had fewer total ADRs.
The advantage of aripiprazole in reducing HPRL is consistent with previous reviews (13, 91). In addition, the advantage of aripiprazole at the dose of <5 mg/day compared to higher doses suggests that higher doses are unnecessary to reduce the AP-induced prolactin level for schizophrenia. This finding is similar to previous findings that aripiprazole at a low dose (3 mg/day) could reduce HPRL, but with increasing dose, the effect reaches a plateau at doses beyond 6 mg/day (92). This is probably because most D2 receptors are already occupied in the striatum at low-dose aripiprazole (93). Some studies did not find a significant association between prolactin levels and the dose of aripiprazole (94), while others (52) found that the effects of aripiprazole on prolactin reduction were significantly greater at higher doses (10 and 20 mg/day) than at 5 mg/day. In this meta-analysis, aripiprazole at both >10 and 5 mg/day had less effects than at <5 mg/day in reducing the prolactin levels. The dose–response effects of aripiprazole on AP-induced HPRL would require further research.
This NMA also found that the prolactin reduction effects of adjunctive aripiprazole, PGD, and metformin are variable across different primary APs—for example, adjunctive PGD = 1:1 was most effective in reducing risperidone-related HPRL, while adjunctive aripiprazole at doses of <5 and ≥10 mg/day are most effective in reducing amisulpride- and olanzapine-related HPRL, respectively. It is likely that the impact of various antipsychotic medications on prolactin levels is different (90). Due to the relatively slow dissociation rate with D2 receptors and weak blood–brain barrier penetrating ability, risperidone is more likely to elevate prolactin compared to other APs (95). The powerful effect of PGD on risperidone-induced HPRL may be associated with its modulation of D2 receptor and transporters and normalization of sex hormone dysfunction through the hypothalamic–pituitary–gonadal axis (96). Of the three adjunctive medications in this NMA, PGD >1:1 was associated with the least all-cause discontinuation rate, which supports the high tolerability in schizophrenia patients. However, the quality standardization of PGD preparation is still lacking, and efficacy studies of PGD on HPRL need to be replicated in countries other than China.
The effect of metformin on the reproductive axis was first found in women with polycystic ovary syndrome (97). Some studies later found that metformin could act on pituitary function and reduce the levels of luteinizing hormone, gonadotropin, and prolactin (98). However, this NMA did not find any significant effect of adjunctive metformin in suppressing the prolactin level, which is probably because metformin may only be effective in reducing AP-induced HPRL at high doses (2.55–3 g/day) and after prolonged treatment courses (99). In this NMA, the doses of adjunctive metformin ranged from 0.5 to 1.5 g/day in five studies, which could explain the non-significant effects. Furthermore, the baseline prolactin level and the different stages of reproductive life could also influence the effectiveness of treatments on HPRL (100). Therefore, long-term metformin treatment at a higher dose may be more clinically useful to treat AP-induced HPRL in those with obesity or diabetes. It should be noted that the long-term use of metformin could decrease the serum levels of folic acid and vitamin B12 and increase serum homocysteine (101). Therefore, the concentration of folic acid, B12, and homocysteine needs to be regularly monitored if long-term metformin treatment for AP-related HPRL and/or metabolic syndrome is given.
Subgroup analyses found that male patients had a greater reduction in prolactin levels when compared to female patients after receiving adjunctive aripiprazole, metformin, or PGD, which is similar to previous findings that aripiprazole had a significantly lower risk of HPRL in men but not in women (102). The sex difference in prolactin reduction may be associated with endogenous cholinergic neuronal activity, concentration of estrogen, and genetic variations of D2 receptors (103). Due to the lower response to pharmacotherapy in females, the gender differences in terms of doses, type, and treatment duration of adjunctive medication for AP-related HPRL should be considered.
The strengths of this study include the use of NMA to compare the efficacy and safety of adjunctive aripiprazole, metformin, and PGD for AP-induced HPRL. In addition, the effects of adjunctive aripiprazole, metformin, and PGD are compared with respect to different AP medications (e.g., risperidone, amisulpride, and olanzapine). However, several limitations should be noted. First, the positive and negative symptoms as measured by the PANSS and Brief Psychiatric Rating Scale and data on sexual dysfunction were not analyzed due to insufficient original data. Most studies did not present data by gender; therefore, the influence of gender on outcomes could not be examined. Second, we manually searched the gray literature, but a significant publication bias remained in the analyses, which is probably associated with unpublished non-significant findings. Third, despite conducting subgroup and meta-regression analyses, there were obvious heterogeneity between studies due to inconsistent samples, methodology, and study quality. Lastly, dose–response relationships were not examined due to insufficient data.
Adjunctive aripiprazole, PGD, and metformin could be effective in reducing AP-induced HPRL in schizophrenia. However, in clinical practice, the selection of an appropriate adjunctive medication for AP-induced HPRL should be individualized according to the needs of the patient.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
LZ, WZ, and Y-TX participated in the study design. HQ, Y-YX, X-HL, and D-BC participated in the collection, analysis, and interpretation of data. LZ, HQ, and Y-TX drafted the manuscript. CN and GU contributed to the critical revision of the manuscript. All the authors approved the final version for publication.
This work was supported by The National Key Research and Development Program of China grant number (no. 2016YFC0900600/2016YFC0900603 and no. 2016YFC1307200), the University of Macau (no. MYRG2015-00230-FHS and no. MYRG2016-00005-FHS), the Beijing Municipal Administration of Hospitals Incubating Program (no. PX2016028), and the Beijing Municipal Administration of Hospitals' Ascent Plan (no. DFL20151801).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.728204/full#supplementary-material
1. Petty RG. Prolactin and antipsychotic medications: mechanism of action. Schizophr Res. (1999) 35:S67–73. doi: 10.1016/S0920-9964(98)00158-3
2. Inder WJ, Castle D. Antipsychotic-induced hyperprolactinaemia. Aust N Z J Psychiatry. (2011) 45:830–7. doi: 10.3109/00048674.2011.589044
3. Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:273–88. doi: 10.1210/jc.2010-1692
4. Froes Brandao D, Strasser-Weippl K, Goss PE. Prolactin and breast cancer: the need to avoid undertreatment of serious psychiatric illnesses in breast cancer patients: a review. Cancer. (2016) 122:184–8. doi: 10.1002/cncr.29714
5. Johnston AN, Bu W, Hein S, Garcia S, Camacho L, Xue L, et al. Hyperprolactinemia-inducing antipsychotics increase breast cancer risk by activating JAK-STAT5 in precancerous lesions. Breast Cancer Res. (2018) 20:42. doi: 10.1186/s13058-018-0969-z
6. Milano W, D'Acunto CW, De Rosa M, Festa M, Milano L, Petrella C, et al. Recent clinical aspects of hyperprolactinemia induced by antipsychotics. Rev Recent Clin Trials. (2011) 6:52–63. doi: 10.2174/157488711793980138
7. Shapiro DA, Renock S, Arrington E, Chiodo LA, Liu LX, Sibley DR, et al. Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology. (2003) 28:1400–11. doi: 10.1038/sj.npp.1300203
8. Halperin Rabinovich I, Camara Gomez R, Garcia Mouriz M, Ollero Garcia-Agullo D. [Clinical guidelines for diagnosis and treatment of prolactinoma and hyperprolactinemia]. Endocrinol Nutr. (2013) 60:308–19. doi: 10.1016/j.endonu.2012.11.005
9. Marder SR, McQuade RD, Stock E, Kaplita S, Marcus R, Safferman AZ, et al. Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. (2003) 61:123–36. doi: 10.1016/S0920-9964(03)00050-1
10. Wu RR, Jin H, Gao K, Twamley EW, Ou JJ, Shao P, et al. Metformin for treatment of antipsychotic-induced amenorrhea and weight gain in women with first-episode schizophrenia: a double-blind, randomized, placebo-controlled study. Am J Psychiatry. (2012) 169:813–21. doi: 10.1176/appi.ajp.2012.11091432
11. Yamada K, Kanba S, Yagi G, Asai M. Herbal medicine (Shakuyaku-kanzo-to) in the treatment of risperidone-induced amenorrhea. J Clin Psychopharmacol. (1999) 19:380–1. doi: 10.1097/00004714-199908000-00018
12. Hasani-Ranjbar S, Vahidi H, Taslimi S, Karimi N, Larijani B, Abdollahi M. A systematic review on the efficacy of herbal medicines in the management of human drug-induced hyperprolactinemia; potential sources for the development of novel drugs. Int J Pharmacol. (2010) 6:691–5. doi: 10.3923/ijp.2010.691.695
13. Li X, Tang Y, Wang C. Adjunctive aripiprazole versus placebo for antipsychotic-induced hyperprolactinemia: meta-analysis of randomized controlled trials. PLoS ONE. (2013) 8:e70179. doi: 10.1371/journal.pone.0070179
14. Zheng W, Cai DB, Li HY, Wu YJ, Ng CH, Ungvari GS, et al. Adjunctive Peony-Glycyrrhiza decoction for antipsychotic-induced hyperprolactinaemia: a meta-analysis of randomised controlled trials. Gen Psychiatr. (2018) 31:e100003. doi: 10.1136/gpsych-2018-100003
15. Zheng W, Yang XH, Cai DB, Ungvari GS, Ng CH, Wang N, et al. Adjunctive metformin for antipsychotic-related hyperprolactinemia: a meta-analysis of randomized controlled trials. J Psychopharmacol. (2017) 31:625–31. doi: 10.1177/0269881117699630
16. Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. (2005) 331:897–900. doi: 10.1136/bmj.331.7521.897
17. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint–preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. (2009) 89:873–80. doi: 10.1093/ptj/89.9.873
18. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
19. Overall JE GD. The brief psychiatric rating scale. Psychol Rep. (1962) 10:799–812. doi: 10.2466/pr0.1962.10.3.799
20. Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons (2011).
21. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17:1–12. doi: 10.1016/0197-2456(95)00134-4
22. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. (2004) 328:1490. doi: 10.1136/bmj.328.7454.1490
23. Ades AE, Sculpher M, Sutton A, Abrams K, Cooper N, Welton N, et al. Bayesian methods for evidence synthesis in cost-effectiveness analysis. Pharmacoeconomics. (2006) 24:1–19. doi: 10.2165/00019053-200624010-00001
24. Dias S, Sutton AJ, Ades AE, Welton NJ. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Mak. (2013) 33:607–17. doi: 10.1177/0272989X12458724
25. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. (2010) 29:932–44. doi: 10.1002/sim.3767
26. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
27. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
28. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
29. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS ONE. (2013) 8:e76654. doi: 10.1371/journal.pone.0076654
30. Wang XL, Xie J. Aripiprazole combined with amisulpride in the treatment of schizophrenia with negative symptoms (in Chinese). J Qiqihar Med Univ. (2013) 34:1734–5. doi: 10.3969/j.issn.1002-1256.2013.12.010
31. Li M, Zhang SF, Shao YC, Fu HP, Qiu SW. Effect of different dosage aripiprazole on proiactin in female schizophrenia with amisulpride treated (in Chinese). China J Health Psychol. (2016) 24:175–8. doi: 10.13342/j.cnki.cjhp.2016.02.004
32. Li JG. Efficacy of amisulpride combined with aripiprazole in female patients with schizophrenia (in Chinese). Med Equip. (2016) 29:120–1. doi: 10.3969/j.issn.1002-2376.2016.20.094
33. Yang Y, Xia Y, Zhu CJ, Chen YB. Effect of aripiprazole on hyperprolactinemia induced by amisulpride (in Chinese). Chin J Clin Pharmacol Ther. (2016) 21:693–6.
34. Lin YC. Aripiprazole combined w ith amisulpride in the treatment of male schizophrenia patients with hyperprolaetinemia in 30 cases (in Chinese). China Health Stand Manage. (2017) 8:55–7. doi: 10.3969/j.issn.1674-9316.2017.17.029
35. Yang P, Li L, Yang D, Wang C, Peng H, Huang H, et al. Effect of peony-glycyrrhiza decoction on amisulpride-induced hyperprolactinemia in women with schizophrenia: a preliminary study. Evid Based Complement Alternat Med. (2017) 2017:7901670. doi: 10.1155/2017/7901670
36. Sha JM, Zhang W, Ding JJ, Chen GD. Effect of low-dose aripiprazole combined with amisulpride on sexual function and prolactin in male patients with schizophrenia (in Chinese). Chin Rural Health Serv Administr. (2017) 37:356–8. doi: 10.13479/j.cnki.jip.2018.04.009
37. Jin JF, Chao YQ, Xu LP, Song ZX, Shao YQ. Clinical study of combined low-dose aripiprazole to improve hyperprolactinemia induced by chlorpromazine (in Chinese). J Psychiatry. (2008) 21:455–6. doi: 10.3969/j.issn.1009-7201.2008.06.022
38. Liu L, Deng SG, Dong XH, Jiang DZ, Cui FW, Pan QH. A placebo-controlled trial of adjunctive treatment with aripiprazole for risperidone-induced hyperprolactinemia (in Chinese). China J Health Psychol. (2011) 19:1288–90. doi: 10.13342/j.cnki.cjhp.2011.11.046
39. Xia JX, Wang YB, Gan JG, Cao SL, Duan D, Qian PH, et al. Efficacy of metformin combined behavior intervention in the treatment of metabolic disorders caused by risperidone (in Chinese). Chinese J Clin Pharmacol. (2011) 27:417–9. doi: 10.13699/j.cnki.1001-6821.2011.06.010
40. Sun XG. Clinical study of low-dose aripiprazole in the treatment of hyperprolactinemia in women with risperidone (in Chinese). Medical J Chin People's Health. (2012) 24:1343–4. doi: 10.3969/j.issn.1672-0369.2012.11.026
41. Xue L, Zhou LJ, Tan WZ, Zou YF, Hu JW, Huang ZM. Aripiprazole in the treatment of 68 cases of male hyperprolactinemia caused by risperidone (in Chinese). Jilin Yi Xue. (2012) 33:107–8. doi: 10.3969/j.issn.1004-0412.2012.01.063
42. Zhu JX, Yin JB. A clinical controlled study of aripiprazole in the treatment of hyperprolactinemia in women with risperidone (in Chinese). Chin Commun Doct. (2012) 14:124–5. doi: 10.3969/j.issn.1007-614x.2012.01.115
43. Zhou HS, Li B, Liu J, Wang HL. The efficacy and safety of aripiprzole in the treatment of female hyperprolact inemia caused by risperidone (in Chinese). China J Health Psychol. (2012) 20:1129–30. doi: 10.13342/j.cnki.cjhp.2012.08.061
44. Lee BJ, Lee SJ, Kim MK, Lee JG, Park SW, Kim GM, et al. Effect of aripiprazole on cognitive function and hyperprolactinemia in patients with schizophrenia treated with risperidone. Clin Psychopharmacol Neurosci. (2013) 11:60–6. doi: 10.9758/cpn.2013.11.2.60
45. Chen SH. Clinical observation of aripiprazole in the treatment of drug-induced amenorrhea caused by risperidone (in Chinese). Med J Chin People's Health. (2013) 25:56–8. doi: 10.3969/j.issn.1672-0369.2013.03.019
46. Zhang HF, Chai YL. Controlled clinical study of adjunctive treatment with aripiprazole for risperidone induced hyperprolactinemia (in Chinese). Chin J Modern Drug Appl. (2013) 7:18–19. doi: 10.14164/j.cnki.cn11-5581/r.2013.19.195
47. Zhou P, Liu LQ, Hao JF, Zhang HX, Yu J, Li YY, et al. The Study of Aripiprazole on preventing the hyperprolactinemia induced by antipsychotics on female schizophrenic patients (in Chinese). China J Health Psychol. (2013) 23:263–64. doi: 10.13479/j.cnki.jip.2014.02.021
48. Zhou JQ, Dong ZW, Zhou X. Metformin treatment of risperidone starting schizophrenia patients with the influence of bai metabolic control study (in Chinese). Chin J Drug Abuse Prev Treat. (2014) 20144–7+154. doi: 10.3969/j.issn.1006-902X.2014.03.005
49. Shen ZT. Effect of aripiprazol on increased prolactin caused by risperidone (in Chinese). Pract Pharm Clin Remed. (2014) 17:871–4. doi: 10.14053/j.cnki.ppcr.2014.07.023
50. Wang W, Wang J, Luo X, Ye ZC, Lin YY. Controlled clinical research on treatment of schizophrenia by risperidone combined with low-dose aripiprazole (in Chinese). China J Health Psychol. (2014) 22:964–6. doi: 10.13342/j.cnki.cjhp.2014.07.002
51. Chen Q, Qian ZP, Lu FR, Fei P. Effect of aripiprazole on the hyperprolactinmia induced by risperidone in quinquagenarian female schizophrenia patients (in Chinese). Sichuan Mental Health. (2015) 28:420–3. doi: 10.11886/j.issn.1007-3256.2015.05.011
52. Chen JX, Su YA, Bian QT, Wei LH, Zhang RZ, Liu YH, et al. Adjunctive aripiprazole in the treatment of risperidone-induced hyperprolactinemia: a randomized, double-blind, placebo-controlled, dose-response study. Psychoneuroendocrinology. (2015) 58:130–40. doi: 10.1016/j.psyneuen.2015.04.011
53. Xie SS, Ding L, Chen YQ. Effects of peony licorice bolus of risperidone with different proportions on female schizophrenia patients suffered hyperprolactinemia (in Chinese). Med Res Educ. (2015) 32:35–8. doi: 10.3969/j.issn.1674-490X.2015.05.009
54. Wen N, Tang W, Pan JS, Zhang JL. Aripiprazole ameliorated the increase of prolactin in female patients with schizophrenia caused by risperidone (in Chinese). Zhejiang Clin Med Jo. (2016) 18:1606–8. Available online at: https://d-wanfangdata-com-cns.vpn.ccmu.edu.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwODE4Eg96amxjeXgyMDE2MDkwMTQaCHI2OG9rYXds
55. Pan XO, Ju ML, Wu J, Qian ZS. Therapeutic effects of aripiprazole and metformin on hyperprolactinemia caused by amisulpride medication (in Chinese). Hebei Med J. (2018) 40:2984–6. doi: 10.3969/j.issn.1002-7386.2018.19.026
56. Zhang LG, Li YL, Liu Y, Chen JX, Liu YH. Dose-effect relationship of aripiprazole on hyperprolactinemia induced by risperidone in m ale patients (in Chinese). Chinese J New Drugs. (2018) 27:334–8. doi: 10.3969/j.issn.1003-3734.2018.03.015
57. Chen JH, Wu YF, Liao XZ. Efficacy analysis of olanzapine combined with aripiprazole in the treatment of first-episode schizophrenia in women (in Chinese). Guide Chin. Med. (2012) 10:145–6. doi: 10.15912/j.cnki.gocm.2012.22.274
58. Gu P, Jin X, Li X, Wu YQ. Treatment of olanzapine-induced hyperprolactinemia by shaoyao gancao decoction (in Chinese). Chinese J Integr Trad Western Med. (2016) 36:1456–9. doi: 10.7661/CJIM.2016.12.1456
59. Lai ZC. Clinical effect of aripiprazole and olanzapine in the treatment of schizophrenia (in Chinese). Chin Foreign Med Res. (2018) 16:36–8. doi: 10.14033/j.cnki.cfmr.2018.25.017
60. Ping JJ, Deng SS, Wan J, Xue SX. Effect of combination of aripiprazole with olanzapine on sex hormone of patients with schizophrenia (in Chinese). Med Innov China. (2018) 15:135–7. doi: 10.3969/j.issn.1674-4985.2018.12.039
61. Chang JS, Ahn YM, Park HJ, Lee KY, Kim SH, Kang UG, et al. Aripiprazole augmentation in clozapine-treated patients with refractory schizophrenia: an 8-week, randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. (2008) 69:720–31. doi: 10.4088/jcp.v69n0505
62. Xu D, Zhu JJ, Wan HY, Li M. Effect of low-dose aripiprazole on prolactin elevation in patients with schizophrenia induced by amisulpride (in Chinese). Chin J Pract Nerv Dis. (2015) 18:28–9.
63. Ren LZ, Hu M. Preventive effect of aripiprazole on sulpiride-induced hyperprolactinemia (in Chinese). Med Inform. (2011) 24:2455. doi: 10.3969/j.issn.1006-1959.2011.06.259
64. Sun W, Zhang JL, Kang MX. Aripiprazole improves the weight gain and prolactin levels in women with schizophrenia induced by olanzapine (in Chinese). Sichuan Mental Health. (2011) 24:98–100. doi: 10.3969/j.issn.1007-3256.2011.02.013
65. Liang J, Yan J, Zhang XY. Aripirazole reduces paliperidone-induced increase of prolactin in patients with schizophrenia: a randomized, double blind and placebo-controlled study (in Chinese). Chin J New Drugs. (2014) 23:1300–3+1310.
66. Huang SN, Yang SZ, Liu XX. Clinical study of paliperidone combined with aripiprazole in the treatment of schizophrenia (in Chinese). Med Inform. (2014) 23:471–2. doi: 10.3969/j.issn.1006-1959.2014.18.573
67. Wu HL, Lin DD, Li Y, Xu YJ. Influence of aripiprazole on hyperprolactinemia caused by antipsychotics in elderly patients with schizophrenia (in Chinese). J Clin Psychiatry. (2013) 23:263–4.
68. Sun W, Ma SF, Gao TF. Efect of aripiprazole on hyperprolactinemia in patients with senile schiz0phr nia induced by antipsychotic drugs (in Chinese). China Foreign Med Treat. (2015) 34:109–10. doi: 10.16662/j.cnki.1674-0742.2015.17.080
69. Song ZX, Chen Q, Xu LP, Cai ZK, Ji JY, Wang WH, et al. Aripiprazole in the treatment of 70 cases of hyperprolactinemia caused by sulpiride (in Chinese). Herald Med. (2009) 28:479–81. doi: 10.3870/yydb.2009.04.030
70. Zhang WH, Chen XY, Wang XJ, Zhou HX. Clinical effect of aripiprazole on olanzapine in the treatment of post-schizophrenia patients with increased body weight (in Chinese). Chin J Biochem Pharmaceut. (2017) 37:201–6. doi: 10.3969/j.issn.1005-1678.2017.03.061
71. Zhang B, Wang L, Xu LP, Shi JA, Sun J. Clinical study of aripiprazole in the treatment of hyperprolactinemia caused by perphenazine (in Chinese). J Neurosis Mental Health. (2008) 8:375–6. doi: 10.3969/j.issn.1009-6574.2008.05.015
72. Li YJ, Gao H. Effect of aripiprazole combined with risperidone for lowering serum prolactin in scltlzophrenic patients (in Chinese). China Pharmaceut. (2014) 23:88–90. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2014&filename=YYGZ201413050&v=lK7z3XfJhtwN3J0CgygjqMpXCemBexaommDpuVTVpts9EQaCCv3j4PJAV6fCsa7N
73. Wang HL. Clinical study of aripiprazole and olanzapine in the treatment of female schizophrenia (in Chinese). Modern Diagn Treat. (2016) 27:234–5.
74. Wang YF, Lv BJ, He EB. The effect of combined with aripiprazole to improve hyperprolactinemia caused by antipsychotic drugs (in Chinese). Chin J Prim Med Pharm. (2015) 1187–9. doi: 10.3760/cma.j.issn.1008-6706.2015.08.023
75. Sheng JH, Lu GH, Qiao Y, Qiao Y. Effect of small dose aripiprazole in the treatment of hyperprolactinemia induced by second generation antipsychotics (in Chinese). J Psychiatry. (2016) 29:245–8. doi: 10.3969/j.issn.2095-9346.2016.04.002
76. Wang L, Zhang B, Xu LP, Shi JA, Shao YQ. A ciinical study on aripiprzole in the treatment of female hyperprolactinemia by haloperidol (in Chinese). China J Health Psychol. (2009) 17:194–5. doi: 10.13342/j.cnki.cjhp.2009.02.023
77. Tang P, Feng J, Xia N. Observation on effect of aripiprazole in treatment of hyperprolactinemia caused by risperidone in schizophrenic patients in 75 cases (in Chinese). China Pharmaceut. (2015) 24:19–20.
78. Guo JH, Cao CA, Liao CP, Xu YM, Liu YY. A control study on aripiprazole in the treatment of hyperprol actinaemaia by antipsychotics (in Chinese). China J Health Psychol. (2013) 21:487–9. doi: 10.13342/j.cnki.cjhp.2013.04.063
79. Chen LJ, Zhuo ZM, Zhuang H. A study of aripiprazole in sulpiride induced male hyperprolactinemia (in Chinese). J Clin Psychiatry. (2010) 20:304–5.
80. Chen JX, Zhang RZ, Li W. Adjunctive treatment of risperidone-induced hyperprolactinemia with aripiprazole: a randomized, double blind, placebo-controlled study (in Chinese). Chin J New Drugs. (2014) 23:811–4.
81. Chen HZ, Yu BR, Yang SG, Shen ZX, Mi Q, Jiang YH. Effect of aripiprazoleonthe hyperprolactinernia caused by sulpiride in the treatment of patients with schizophrenia—a clinical observation (in Chinese). Herald Med. (2007) 26:1145–6. doi: 10.3870/j.issn.1004-0781.2007.10.012
82. Wang XF, Guo HL, Sun KF. Effect of aripiprazole on higher plasma prolactin level caused antipsychotic drugs in female schizophrenic patients (in Chinese). J Clin Psychiatry. (2018) 28:125–7. doi: 10.3969/j.issn.1005-3220.2018.02.017
83. Wang YG, Huang LG. Research on treatment of glucose and lipid metabolism disorder in patients with Quetiapine-induced schizophrenia with Metformin (in Chinese). China Modern Med. (2016) 23:156–9.
84. Yue LF. The effection of Jiawei Shaoyao Gancao decoction in treating hyperprolactinemia caused by antipsychotics and cognitive function (Thesis in Chinese). Henan: Xinxiang Medical University (2016).
85. Man SC, Li XB, Wang HH, Yuan HN, Wang HN, Zhang RG, et al. Peony-glycyrrhiza decoction for antipsychotic-related hyperprolactinemia in women with schizophrenia: a randomized controlled trial. J Clin Psychopharmacol. (2016) 36:572–9. doi: 10.1097/JCP.0000000000000607
86. Wang ZH, Gan B, Zhou H. Efects of aripiprazole on the antipsychotic-induced hyperprolactinemia (in Chinese). Acta Acad Med Wannan. (2017) 36:143–5. doi: 10.3969/j.issn.1002-0217.2017.02.013
87. Xu LP, Ji JY, Shi H, Zhai FL, Zhang B, Shao YQ, et al. A control study of aripiprazole in the treatment of hyperprolactinemia by antipsychotics origin (in Chinese). Chin J Behav Med Brain Sci. (2006) 15:718–20. doi: 10.3760/cma.j.issn.1674-6554.2006.08.019
88. Shim JC, Shin JG, Kelly DL, Jung DU, Seo YS, Liu KH, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. (2007) 164:1404–10. doi: 10.1176/appi.ajp.2007.06071075
89. Kane JM, Correll CU, Goff DC, Kirkpatrick B, Marder SR, Vester-Blokland E, et al. A multicenter, randomized, double-blind, placebo-controlled, 16-week study of adjunctive aripiprazole for schizophrenia or schizoaffective disorder inadequately treated with quetiapine or risperidone monotherapy. J Clin Psychiatry. (2009) 70:1348–57. doi: 10.4088/JCP.09m05154yel
90. Balijepalli C, Druyts E, Zoratti MJ, Wu P, Kanji S, Rabheru K, et al. Change in prolactin levels in pediatric patients given antipsychotics for schizophrenia and schizophrenia spectrum disorders: a network meta-analysis. Schizophr Res Treat. (2018) 2018:1543034. doi: 10.1155/2018/1543034
91. Meng M, Li W, Zhang S, Wang H, Sheng J, Wang J, et al. Using aripiprazole to reduce antipsychotic-induced hyperprolactinemia: meta-analysis of currently available randomized controlled trials. Shanghai Arch Psychiatry. (2015) 27:4–17. doi: 10.11919/j.issn.1002-0829.215014
92. Yasui-Furukori N, Furukori H, Sugawara N, Fujii A, Kaneko S. Dose-dependent effects of adjunctive treatment with aripiprazole on hyperprolactinemia induced by risperidone in female patients with schizophrenia. J Clin Psychopharmacol. (2010) 30:596–9. doi: 10.1097/JCP.0b013e3181ee832d
93. Grunder G, Fellows C, Janouschek H, Veselinovic T, Boy C, Brocheler A, et al. Brain and plasma pharmacokinetics of aripiprazole in patients with schizophrenia: an [18F]fallypride PET study. Am J Psychiatry. (2008) 165:988–95. doi: 10.1176/appi.ajp.2008.07101574
94. Sogawa R, Shimomura Y, Minami C, Maruo J, Kunitake Y, Mizoguchi Y, et al. Aripiprazole-associated hypoprolactinemia in the clinical setting. J Clin Psychopharmacol. (2016) 36:385–7. doi: 10.1097/JCP.0000000000000527
95. Peuskens J, Pani L, Detraux J, De Hert M. The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs. (2014) 28:421–53. doi: 10.1007/s40263-014-0157-3
96. Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features and management. Drugs. (2004) 64:2291–314. doi: 10.2165/00003495-200464200-00003
97. Genazzani AD, Battaglia C, Malavasi B, Strucchi C, Tortolani F, Gamba O. Metformin administration modulates and restores luteinizing hormone spontaneous episodic secretion and ovarian function in nonobese patients with polycystic ovary syndrome. Fertil Steril. (2004) 81:114–9. doi: 10.1016/j.fertnstert.2003.05.020
98. Billa E, Kapolla N, Nicopoulou SC, Koukkou E, Venaki E, Milingos S, et al. Metformin administration was associated with a modification of LH, prolactin and insulin secretion dynamics in women with polycystic ovarian syndrome. Gynecol Endocrinol. (2009) 25:427–34. doi: 10.1080/09513590902770172
99. Krysiak R, Kowalcze K, Szkrobka W, Okopien B. The effect of metformin on prolactin levels in patients with drug-induced hyperprolactinemia. Eur J Intern Med. (2016) 30:94–98. doi: 10.1016/j.ejim.2016.01.015
100. Mann WA. Treatment for prolactinomas and hyperprolactinaemia: a lifetime approach. Eur J Clin Invest. (2011) 41:334–42. doi: 10.1111/j.1365-2362.2010.02399.x
101. Sahin M, Tutuncu NB, Ertugrul D, Tanaci N, Guvener ND. Effects of metformin or rosiglitazone on serum concentrations of homocysteine, folate, and vitamin B12 in patients with type 2 diabetes mellitus. J Diabetes Complicat. (2007) 21:118–23. doi: 10.1016/j.jdiacomp.2005.10.005
102. Crespo-Facorro B, Ortiz-Garcia de la Foz V, Suarez-Pinilla P, Valdizan EM, Perez-Iglesias R, Amado-Senaris JA, et al. Effects of aripiprazole, quetiapine and ziprasidone on plasma prolactin levels in individuals with first episode nonaffective psychosis: analysis of a randomized open-label 1 year study. Schizophr Res. (2017) 189:134–141. doi: 10.1016/j.schres.2017.01.046
Keywords: aripiprazole, metformin, paeoniae–glycyrrhiza decoction, hyperprolactinemia, network meta-analysis
Citation: Zhang L, Qi H, Xie Y-Y, Zheng W, Liu X-H, Cai D-B, Ng CH, Ungvari GS and Xiang Y-T (2021) Efficacy and Safety of Adjunctive Aripiprazole, Metformin, and Paeoniae–Glycyrrhiza Decoction for Antipsychotic-Induced Hyperprolactinemia: A Network Meta-Analysis of Randomized Controlled Trials. Front. Psychiatry 12:728204. doi: 10.3389/fpsyt.2021.728204
Received: 22 June 2021; Accepted: 12 August 2021;
Published: 29 September 2021.
Edited by:
Mary V. Seeman, University of Toronto, CanadaReviewed by:
John Davis, University of Illinois at Chicago, United StatesCopyright © 2021 Zhang, Qi, Xie, Zheng, Liu, Cai, Ng, Ungvari and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Zhang, emxpbHllcGlAY2NtdS5lZHUuY24=; Yu-Tao Xiang, eHl1dGx5QGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.