- 1Department of Family and Preventive Medicine, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 2Regenstrief Institute, Indiana University School of Medicine, Indianapolis, IN, United States
Generalist practitioners often find interacting with patients deeply satisfying and joyful; they also experience encounters that are challenging and complex. In both cases, they must be aware of the many issues that affect the processes and outcomes of patient care. Although using the BioPsychoSocial approach is an important, time-tested framework for cultivating one's awareness of patients' presenting concerns, recent developments suggest that additional frames of reference may enhance communication and relationships with patients. In this article, we describe several additions to the BioPsychoSocial approach, considerations we call “add-ons” and “add-ins”. We invite generalist practitioners and, indeed, all health care practitioners, to consider how they can improve their ongoing care of patients by personalizing these and other additions in their day-to-day work with patients.
Introduction
Based on systems theory and later complemented by patient- and relationship-centered care, the BioPsychoSocial (BPS) approach has become an important part of medical practice and medical education, especially among generalist practitioners (1–4). The approach is applicable as a way of conceptualizing, organizing, and addressing the physical, emotional, and social factors that influence how patients experience and describe their presenting concerns. Although not without its critics (5–7), and certainly not limited to generalist practice alone (8–10), the BPS approach has become one of the most important—some might suggest the most important—unifying model in generalist medicine over the last four decades (11).
Much has changed in generalist medicine since mention of the value of systems theory to patient care and publication of the seminal paper on the BPS approach (12, 13), which appeared in Science in 1977 (1). Significantly, scholars have established the overall importance of generalist principles and practices to highly functioning health care systems and improved population-based health care outcomes (14, 15). Much has changed in respect to the BPS approach, as well. From its origins as a theoretical approach to patients presenting principally with Somatic Disorders [now also referred as Medically Unexplained Symptoms (MUS) (16), Bodily Distress Syndrome (BDS) (17), or the patient-centered acronym PRESSS (Physical Reaction to Emotional Stress of Some Sort (18))], the BPS approach has sequentially emerged as a key element in both Patient-Centered Medicine and Relationship-Centered Care (19–21). The approach has also found adherents beyond generalist practice, and clinicians in a wide variety of specialties and sub-specialties (as well as many other health care professionals) have spoken to its utility in attending to patient concerns (8–10, 22, 23). Research into the BPS approach has evolved significantly over the years, and many evidence-based and evidence-informed studies have confirmed its benefits in clinical practice (24–26).
Nonetheless, much remains the same. Due to cultural and economic forces within medicine that prioritize site-specific technological interventions and highly-remunerative patterns of practice over holistic approaches to patient care (especially in countries that are highly dependent on for-profit models of health care, such as United States), generalism has struggled to find its place as a foundational element of medical education and practice (27). Additionally, theories that undergird such practice, including the BPS approach, continue to languish in the shadows of the dominant, strictly biomedical understanding of medicine. Even among generalist practitioners, the BPS approach remains undervalued relative to the more traditional linear methods of diagnosis and treatment (28). In many educational institutions, the BPS approach is manifestly far from being fully implemented; it is unmistakably given lip service, glanced over, or simply ignored in the face of a biomedically-focused pedagogical paradigm (26).
What can be done? Motivated by our (1) mutual misgivings regarding the traditional enculturation of medical students and residents away from thinking holistically and systemically, (2) recognition of the importance of the BPS approach to generalist practice, and (3) firm belief of the approach's positive influence on patients' health, we suggest it is time to reconsider how generalist practitioners understand and use the approach. We base our considerations on 70 years' combined direct clinical experience in and research observations of generalist practice—one of us is a seasoned family physician/medical anthropologist (WV) and the other a veteran medical sociologist/medical educator (RF)—plus a growing literature that speaks to the importance of the BPS approach and its successors on quality of care, (29) overall outcomes (24–26), and interpersonal satisfaction (30).
We frame our considerations in two opposing directions: first, as add-ons to the BPS approach—ways to expand our appreciation of patient-oriented concerns; and, second, as add-ins—ways to appreciate the approach as a means of influencing our own cognitive habits and practice behaviors. The purpose of this article, thus, is to help generalist practitioners personalize their use of the BPS approach so as to help nurture their therapeutic presence with patients and, ultimately, positively influence patients' health.
Adding-on to the BPS Approach
The traditional BPS approach refers to a natural system hierarchy in which patients are located somewhere on a continuum between subatomic particles and the biosphere (1, 2). The BPS approach suggests clinicians focus on the level of patients as people first, simultaneously appreciating how other system constituent themes influence patients' experience of disease and illness. From a thematic perspective, the traditional approach focuses, self-evidently, on the biological, psychological, and social dimensions of patients' lives.
Over the years, clinicians and scholars have added-on several other themes to the original approach. Some years ago, “spiritual” became a common appendage in generalist literature, giving recognition to the influence of religion and spirituality on the health and well-being of human beings (31, 32). As well, cultural and political-economical themes of care emerged as early generalist add-ons (5, 33). Much more recently, a number of other add-ons have come to the fore from outside of generalist circles—examples include such auxiliary themes as history, microhistory, and intersectionality (from psychiatry) (34, 35), social changeways and dynamic microsystems (from psychology) (36, 37), and institutional influences (from physiotherapy) (38).
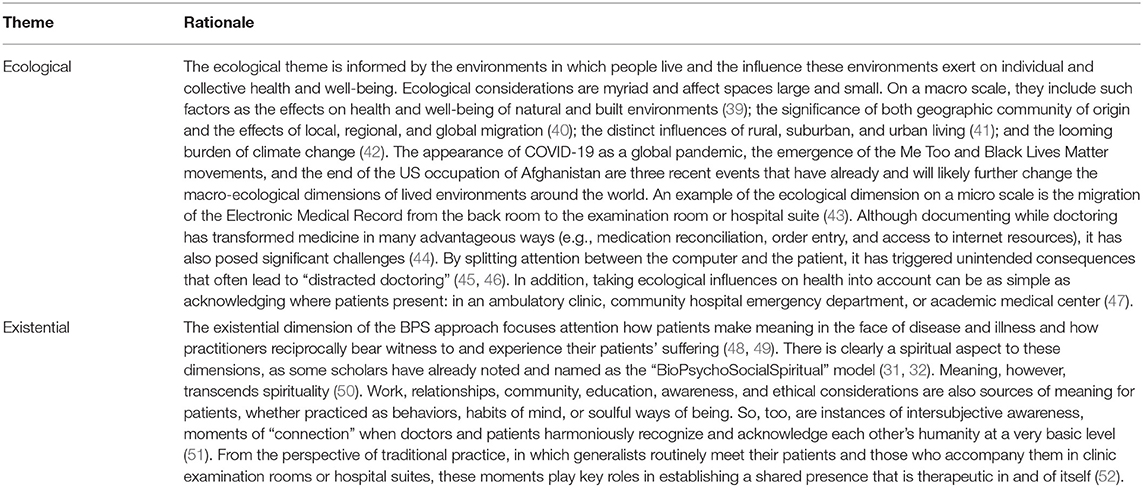
Our personal favorite thematic add-ons, broad in scope echoing our generalist backgrounds, are ecological and existential in nature. We do not, however, recommend anyone use the term “BioPsychoEcoSocialExistential.” It is a quite a mouthful and, simply, another artificial construct with extra perceptual boundaries to contend with. We prefer generalists keep things simple—BioPsychoSocial is perfectly suitable in this regard (Table 1).
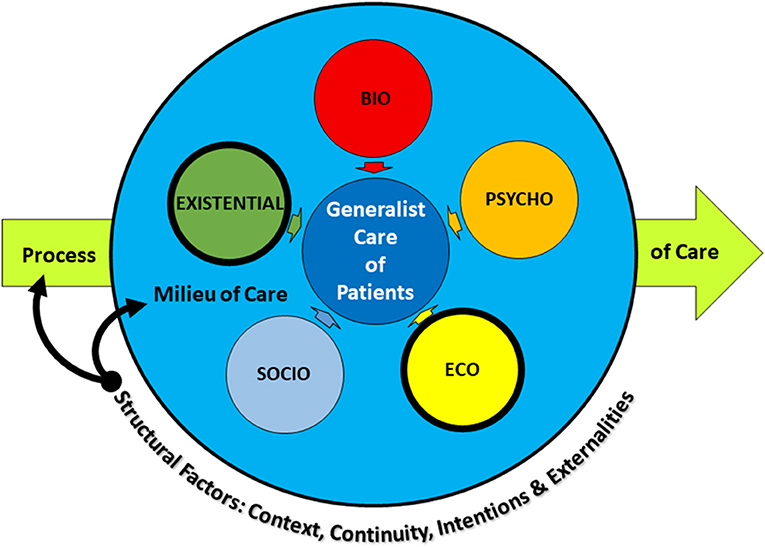
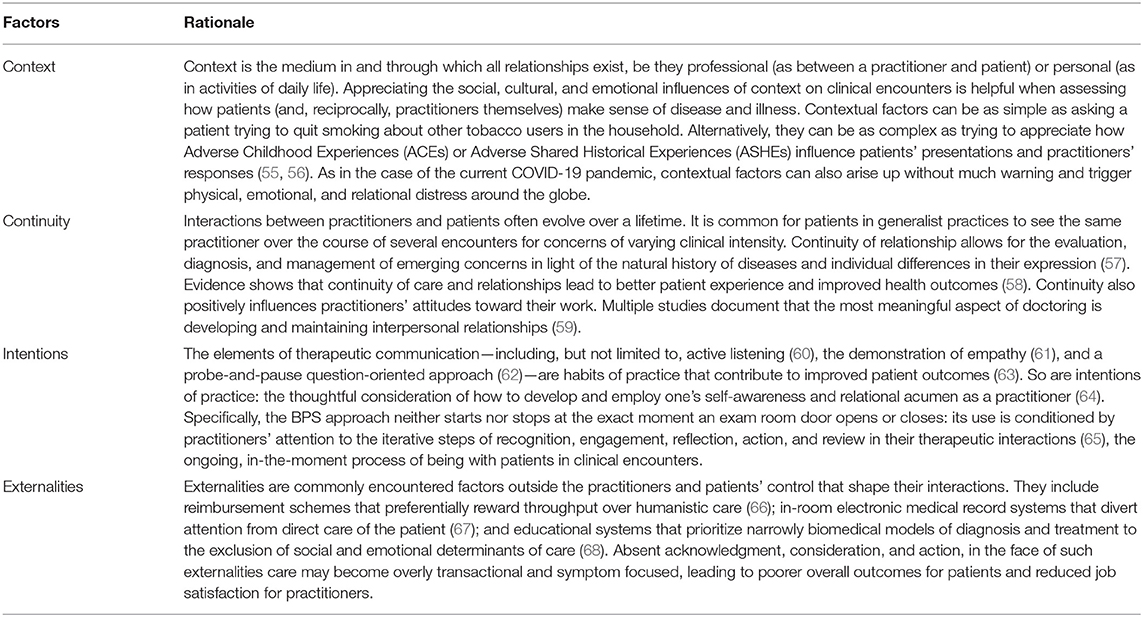
In addition, add-ons can take the form of specific structural factors that affect the milieu in and the process by which practitioners interpret the BPS approach (Figure 1). Differences in these factors invariably alter how individual practitioners implement the approach. These specific factors reflect the location and setting of care, the nature of any particular patient's concerns, and the characteristics of the practitioner's professional background (53). Drawing from literature that speaks to the nature of generalist practice—specifically, that generalists are likely to see patients across the lifespan in short visits over long periods of time; attend to concerns both acute and chronic; strategize care that simultaneously bridges prevention, management, and cure; and address multiple undifferentiated problems across a range of concerns (54)—we suggest four structural factors are key: context, continuity, intentions, and externalities (Table 2).
Adding-in to the BPS Approach
The BPS approach initially focused on individual patients embedded in complex bureaucratic systems. We agree this perspective is important. We also suggest that generalist practitioners develop the ability to see themselves as integral parts of these systems. We encourage them to appreciate their use of the BPS approach with patients as a means of identifying add-ins—organically produced insights that arise in the course of patient encounters—in order to critically consider how to do the best they can, in any moment at hand, given the circumstances of any clinical situation, and help patients move toward health.
Given the current culture of medicine that marginalizes the holistic practice of generalist medicine, attending to these tasks may not be easy. We suggest, however, the BPS approach is bi-directional, and that by applying it with patients in everyday practice generalists can develop their professional identities as caring and humanistic healers. They can come to understand how clinical encounters are coproduced (69), examine how practitioners' own implicit biases influence the provision of care as well as the healing process (70), and consider how personal histories and professional socializations affect the processes and outcomes of care (71). Additionally, they can appreciate how to employ cultural sensitivity (72), with cultural humility (73), relative to patients and their concerns and as influenced by where they practice and the resources available. They can learn how to recognize, investigate, and manage the feelings and thoughts that are integral to enhancing practitioner equanimity in the face of anxiety and contentment in the face of stress.
Adding-in the BPS approach, with the aim of strategically cultivating professional growth, calls for generalist practitioners to use other key principles of practice [including such longstanding principles as affinity, intimacy, curiosity, and fidelity (74)] in the moral and ethical milieu that exists between them and their patients (75). It encourages them to nurture attributes such as emotional intelligence (76), adaptive expertise (77), and clinical courage as instruments of therapeutic change (78). It also encourages generalists to engage in the communities they serve (79), to use and cultivate an anthropological gaze as to the world around them (80), and to see their role as a call to action for social accountability (81). The BPS approach, in this way, is an expression of the interconnected nature not only of the doctor-patient relationship, but also a guide for generalists to become more adept—clinically wise—on their professional path from competency to capability to capacity and beyond (82).
Generalists (and, indeed, specialists, subspecialists, and other health care professionals) can consciously develop their clinical wisdom by attending to add-ins as personalized insights into growing their professional identities (83). This growth emerges from thinking about thinking (metacognition) (84), feeling (values education) (85), and doing (experiential learning) (86). In turn, such reflective thinking can help generalists enhance their cognitive abilities, expand their affective awareness, and develop their performative proficiencies (Figure 2).
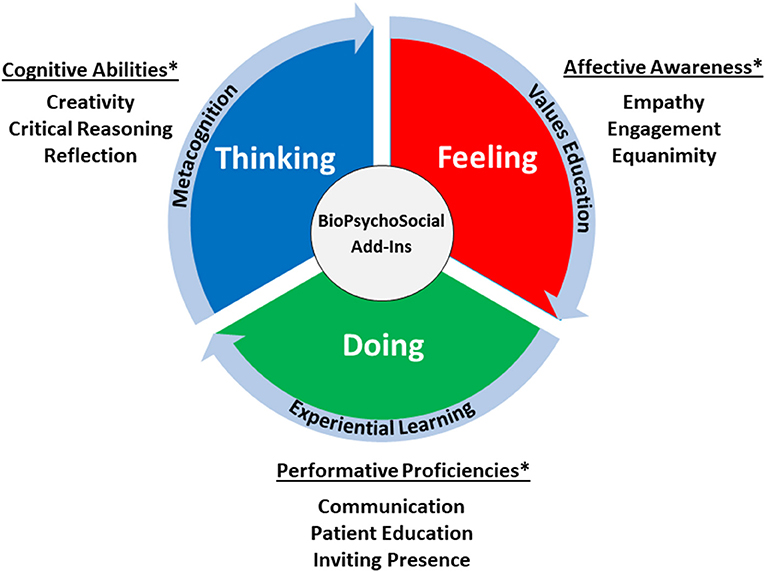
Figure 2. Developing clinical wisdom—dimensions of personal growth. *We list examples in these categories for illustrative purposes only; they are not all-inclusive in nature.
Clinical Case Study
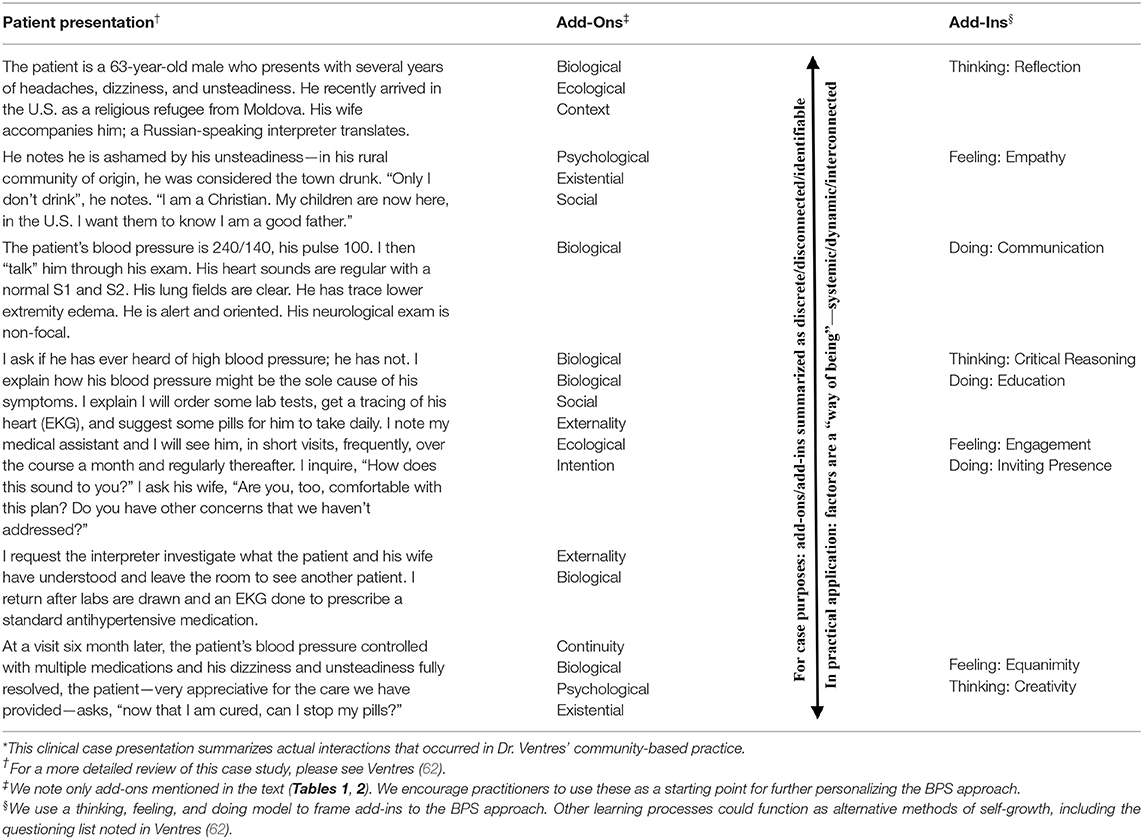
We present a brief clinical case study to illustrate how add-ons and add-ins are intermingled with the process of applying a BPS approach in clinical encounters (Table 3). For demonstration purposes only, we list both add-on themes and factors and add-in insights separately and sequentially; the reality is that the BPS approach and the themes, factors, and insights we enumerate are more dynamic than static and more systemic than linear in nature. As many generalists have previously noted, using this kind of approach is a “way of being” in practice that is incorporates practitioner awareness, patient- and relationship-centeredness, in-the-moment flexibility, integrated teamwork, and shared presence as regularly practiced habits (11).
Discussion
The point of introducing these considerations is to suggest that generalist practitioners consider the BPS approach not as a model set in stone, but as (1) an inspiration for further integrating BPS concepts into practice, (2) a stimulus to promote patient- and relationship- centered approaches to patient care, and (3) a means to of repositioning themselves in the space between patients' lived experience and the culture of medicine (87). The BPS approach offers generalists not only a broad understanding of the many factors that contribute to the evaluation, diagnosis, and management of presenting problems, but also a path to reconceptualize professional growth in service of therapeutic agency (one's ability to affect positive change) and well-being on both sides of the stethoscope.
More important, the point is that generalist practitioners consider the BPS approach as a template for exploring their own contributions to the healing process by examining not only their roles and relationships vis-à-vis the patients they serve, but also the attributes of clinical wisdom they develop and express along the course of their professional lives. The add-ons and add-ins we suggest can and should be modified or supplemented by others considerations, as appropriate—the overriding goal is doing the right thing at the right time, under the circumstances at hand, for the betterment of patients' health and with the intent of improving their well-being. The BPS approach in this way can help generalists envision, create, and incorporate original add-ons and add-ins to enrich their healing talents.
In fact, we encourage generalist practitioners to take personal ownership of the BPS approach and apply it, distinctively, with all patients in their daily work. We hope they use the approach as a directional marker pointing the way toward individual clinical excellence in holistic patient care. Collectively, we hope they and their colleagues in other disciplines use it as guide to making the practice of generalist medicine and medicine as a whole more inclusive, humane, efficacious, and satisfying. Given current circumstances, external incentives tying compensation to patient experience may be helpful in nudging these aspirations along (88).
These aspirations are particularly fitting as means of countering the increasingly fragmented, hyper-technical, production-oriented, industrialized model of medical practice that exists at this very moment in time, especially in the United States. The BPS approach may also help remediate traditional medicine's acknowledged failures in the face of injustice, inequity, and political polarization, forces that increasingly appear to negate not only the ultimate effectiveness of medicine, but also the healing satisfaction characteristic of its practice.
Further Thoughts
First, we are fully aware, and have noted above, that the BPS approach is applicable beyond generalist medicine. The approach has utility in specialty and subspecialty medical practice as well as in a variety of other health care disciplines, and literature emergent from those disciplines has enlightened our own understandings of the BPS approach. Our purpose in focusing on generalist practice is not to exclude others who attend to patients. It emerges, however, from our assessment that the BPS approach is central to the everyday practice of generalist medicine: with the exception of those patients who present with imminently life threatening conditions, the BPS approach is applicable, to greater or lesser degree, at all times in all situations with all patients who present to generalist practitioners. Due to the nature of clinical interactions in specialty and subspecialty care, the BPS approach is generally—and appropriately—a supplement to the biomedical model, invoked either in response to certain presenting problems or when the traditional linear course of diagnoses and treatment has been tried and failed.
Second, any approach to understanding the complexity of human life in relationship to the very real experience of disease, illness, and sickness will inherently find itself limited by the words used to describe it. This is especially true when considered independently of the context of a particular patient's individual history, current experience, or the circumstances under which individuals turn to the medical care system in times of need. No textual explanation or graphic representation can wholly represent the dynamic process of clinical encounters (36), just as no single recommendation for enhancing such encounters is applicable or appropriate in each and every setting. The reality is that the BPS approach, with or without add-ons or add-ins, can only approximate some of what goes on between practitioners and patients (89), let alone what goes on in the consciousness of individual patients or practitioners beyond the veil of clinical presentations.
Third, another reality is that interactions between practitioners and patients do not always go as planned or go well. No conceptual approach or practiced skill can guarantee perfection in all clinical encounters, especially in light of the many influences that shape them. While challenging to endure, conflicts and mistakes can provide generalist practitioners with opportunities to learn and incorporate new knowledge, new patterns of thought, and new expressions of care in their work with patients. Often it is not what one does, but what one does next that counts—communication strategies such as conversational repair and apology can be taught, learned, and put into practice, benefitting patients, practitioners, and the therapeutic relationships that exist between them (90, 91).
Conclusion
The BPS approach has been a part of the practice and teaching of generalist medicine since its introduction over fifty years ago. It provides an important foundation for considering, conducting, observing, reflecting upon, and providing feedback about the intricacies of clinical care, healing interactions, and practitioner-patient communication. It has, however, struggled to gain broad acceptance in the face of a dominant linear model of biomedical practice. Given new developments in the practice of generalist medicine and the world as we know it, we suggest that generalist practitioners view the BPS approach and its offspring, Patient- and Relationship-Centered Care, as dynamic and modifiable templates in service of both addressing patient concerns and improving their own clinical awareness. We offer for reflection ways to add-on to the BPS approach several thematic considerations and structural factors in order to further develop its efficacy with patients. We also suggest how generalists can use the BPS approach as an add-in to enhance self-awareness and understand their own signature presence as healing professionals. We encourage generalist practitioners to view the BPS approach as an invitation to explore ways to improve patients' health and well-being as well as their own joy and resilience in the practice of medicine.
Author Contributions
WBV and RMF contributed to the conception and design of this manuscript. WBV wrote the first draft of the manuscript. WBV and RMF contributed to manuscript revision, read the final version of the manuscript, and approved the submission version. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Engel G. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196:129–36. doi: 10.1126/science.847460
2. Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. (1980) 137:535–44. doi: 10.1176/ajp.137.5.535
3. Stewart M. Towards a global definition of patient centered care. BMJ. (2001) 322:444–5. doi: 10.1136/bmj.322.7284.444
4. Beach MC, Inui T. Relationship-centered care research network. Relationship-centered care: a constructive reframing. J Gen Intern Med. (2006) 21:S3–8. doi: 10.1111/j.1525-1497.2006.00302.x
6. Bartz R. Beyond the biopsychosocial model: new approaches to doctor-patient interactions. J Fam Pract. (1999) 48:601–7.
7. Kontos N. Biomedicine—menace or straw man? Re-examining the biopsychosocial argument. Acad Med. (2011) 86:509–15. doi: 10.1097/ACM.0b013e31820e0d16
8. Edozien LC. Beyond biology: the biopsychosical model and its application in obstetrics and gynaecology. BJOG. (2015) 122:900–3. doi: 10.1111/1471-0528.13328
9. Tripathi A, Das A. Kar SK. biopsychosocial model in contemporary psychiatry: current validity and future prospects. Indian J Psychol Med. (2019) 41:582–5. doi: 10.4103/IJPSYM.IJPSYM_314_19
10. Novy DM, Aigner CJ. The biopsychosocial model in cancer pain. Curr Opin Support Palliat Care. (2014) 8:117–23. doi: 10.1097/SPC.0000000000000046
11. Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med. (2004) 2:576–82. doi: 10.1370/afm.245
12. McWhinney IR. Beyond diagnosis: an approach to the integration of behavioral science and clinical medicine. N Engl J Med. (1972) 287:384–7. doi: 10.1056/NEJM197208242870805
13. Brody H. The systems vie of man: implications for medicine, science, and ethics. Perspect Biol Med. (1973) 17:71–92. doi: 10.1353/pbm.1973.0007
14. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. (2005) 83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x
15. Shi L. The impact of primary care: a focused review. Scientifica. (2012) 2012:432892. doi: 10.6064/2012/432892
16. Smith RC, Dwamena FC. Classification and diagnosis of patients with medically unexplained symptoms. J Gen Intern Med. (2007) 22:685–91. doi: 10.1007/s11606-006-0067-2
17. Budtz-Lilly A, Schröder A, Rask MT, et al. Bodily distress syndrome: a new diagnosis for functional disorders in primary care?. BMC Fam Pract. (2015) 16:180. doi: 10.1186/s12875-015-0393-8
18. Ventres W. PRESSS: a new patient-centered name for an old problem? J Am Board Fam Med. (2021) 34:1030–2. doi: 10.3122/jabfm.2021.05.200647
19. Stewart MS, Brown JB, Weston W, McWhinney IR, McWilliam CL, Freeman T. Patient Centered Medicine: Transforming the Clinical Method. 3rd ed. London, UK: Radcliffe Publishing Ltd. (2014). p. 442. doi: 10.1201/b20740-1
20. Tresolini CP, The Pew-Fetzer Task Force. Health Professions Education and Relationship-Centered Care. San Francisco, CA: Pew Health Professions Commission (1994). p. 76.
21. Frankel RM, Quill T. Integrating biopsychosocial and relationship-centered care into mainstream medical practice: a challenge that continue to produce positive result. Fam Syst Health. (2005) 23:413–21. doi: 10.1037/1091-7527.23.4.413
22. Bedos C, Apelian N, Vergnes JN. Towards a biopsychosocial approach in dentistry: the Montreal-Toulouse Model. Br Dent J. (2020) 228:465–8. doi: 10.1038/s41415-020-1368-2
23. Garland EL, Howard MO. Neuroplasticity, psychosocial genomics, and the biopsychosocial paradigm in the 21st century. Health Soc Work. (2009) 34:191–9. doi: 10.1093/hsw/34.3.191
24. Smith RC, Fortin AH, Dwamena F. An evidence-based patient-centred method makes the biopsychosocial model scientific. Patient Educ Couns. (2013) 91:265–70. doi: 10.1016/j.pec.2012.12.010
25. Wade DT., Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil. (2017) 31:995–1004. doi: 10.1177/0269215517709890
26. Smith RC. Making the biopsychosocial model more scientific-its general and specific models. Soc Sci Med. (2021) 272:113568. doi: 10.1016/j.socscimed.2020.113568
28. Kusnanto H, Agustian D. Hilmanto D. Biopsychosocial model of illnesses in primary care: a hermeneutic literature review. J Fam Med Prim Care. (2018) 7:497–500. doi: 10.4103/jfmpc.jfmpc_145_17
29. Epstein RM. Realizing Engel's biopsychosocial vision: resilience, compassion, and quality of care. Int J Psychiatry Med. (2014) 47:275–87. doi: 10.2190/PM.47.4.b
30. Dezutter J, Offenbaecher M, Vallejo MA, Vanhooren S, Thauvoye E, Toussaint L. Chronic pain care. Int J Psychiatry Med. (2016) 51:563–75. doi: 10.1177/0091217417696738
31. Sulmasy DP. A biopsychosocial-spiritual model for the care of patients at the end of life. Gerontologist. (2002) 42:24–33. doi: 10.1093/geront/42.suppl_3.24
32. Dyer AR. The need for a new “new medical model”: a bio-psychosocial-spiritual model. South Med J. (2011) 104:297–8. doi: 10.1097/SMJ.0b013e318208767b
33. Yamada S, Palafox N. On the biopsychosocial model: the example of political economic causes of diabetes in the Marshall Islands. Fam Med. (2001) 33:702–4.
34. Strauss J, Bernard P, Harper A. Towards a biopsychosocial psychiatry. Psychiatry. (2019) 82:103–12. doi: 10.1080/00332747.2019.1579609
35. Kelly MA, Barnert E, Bath E. Think, ask, act: the intersectionality of mental and reproductive health for judicially involved girls. J Am Acad Child Adolesc Psychiatry. (2018) 57:715–8. doi: 10.1016/j.jaac.2018.07.870
36. Haslam SA, Haslam C, Jetten J, Cruwys T, Bentley SV. Rethinking the nature of the person at the heart of the biopsychosocial model: exploring social changeways not just personal pathways. Soc Sci Med. (2021) 272:113566. doi: 10.1016/j.socscimed.2020.113566
37. Lehman BJ, David DM, Gruber JA. Rethinking the biopsychosocial model of health: understanding health as a dynamic system. Soc Personal Psychol Compass. (2017) 11:e12328. doi: 10.1111/spc3.12328
38. Mescouto K, Olson RE, Hodges PW, Setchell. A critical review of the biopsychosocial mode of low back pain care: time for a new approach. Disability Rehabil. (2020). doi: 10.1080/09638288.2020.1851783. [Epub ahead of print].
39. Renalds A, Smith TH, Hale PJ. A systematic review of built environment and health. Fam Community Health. (2010) 33:68–78. doi: 10.1097/FCH.0b013e3181c4e2e5
40. Pottie K, Batista R, Mayhew M, Mota L. Grant K. Improving delivery of primary care for vulnerable migrants: Delphi consensus to prioritize innovative practice strategies. Can Fam Physician. (2014) 60:e32–40.
41. Mainous AG, Kohrs FP. A comparison of health status between rural and urban adults. J Community Health. (1995) 20:423–31. doi: 10.1007/BF02260438
42. Blashki G, McMichael T, Karoly DJ. Climate change and primary health care. Aust Fam Physician. (2007) 36:986–9.
43. Lau F, Price M, Boyd J, Partridge C, Bell H, Raworth R. Impact of electronic medical record on physician practice in office settings: a systematic review. BMC Med Inform Decis Mak. (2012) 12:10. doi: 10.1186/1472-6947-12-10
44. Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. (2011) 4:47–55. doi: 10.2147/RMHP.S12985
45. Kissler MJ, Kissler K, Burden M. Toward a medical “ecology of attention”. N Engl J Med. (2021) 384:299–301. doi: 10.1056/NEJMp2027190
46. Ventres W, Kooienga S, Vuckovic N, Marlin R, Nygren P, Stewart V. Physicians, patients, and the electronic health record: an ethnographic analysis. Ann Fam Med. (2006) 4:124–31. doi: 10.1370/afm.425
47. Johansen ME, Kircher SM, Huerta TR. Reexamining the ecology of medical care. N Engl J Med. (2016) 374:495–6. doi: 10.1056/NEJMc1506109
48. Egnew TR. Suffering, meaning, and healing: challenges of contemporary medicine. Ann Fam Med. (2009) 7:170–5. doi: 10.1370/afm.943
49. Egnew TR. A narrative approach to healing chronic illness. Ann Fam Med. (2018) 16:160–5. doi: 10.1370/afm.2182
50. Ventres W, Dharamsi S. Beyond religion and spirituality: faith in the study and practice of medicine. Perspect Biol Med. (2013) 56:352–61. doi: 10.1353/pbm.2013.0023
51. Matthews DA, Suchman AL, Branch WT. Making “connexions”: enhancing the therapeutic potential of patient-clinician relationships. Ann Intern Med. (1993) 118:973–7. doi: 10.7326/0003-4819-118-12-199306150-00010
52. Ventres WB, Frankel RM. Shared presence in physician-patient communication: a graphic representation. Fam Syst Health. (2015) 33:270–9. doi: 10.1037/fsh0000123
53. Farre A. Rapley T. The new old (and old new) medical model: four decades navigating the biomedical and psychosocial understandings of health and illness. Healthcare. (2017) 5:88. doi: 10.3390/healthcare5040088
55. Herzog JI. Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front Psychiatry. (2018) 9:420. doi: 10.3389/fpsyt.2018.00420
56. Ventres W, Messias E. From ACEs to ASHEs: adverse shared historical experiences and their impact on health outcomes. South Med J. (2021) In press.
57. Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. (2018) 8:e021161. doi: 10.1136/bmjopen-2017-021161
58. Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. (2005) 3:159–66. doi: 10.1370/afm.285
59. Horowitz CR, Suchman AL, Branch WT, Frankel RM. What do doctors find meaningful about their work? Ann Intern Med. (2003) 138:772–5. doi: 10.7326/0003-4819-138-9-200305060-00028
60. Lang F, Floyd MR, Betne KJ. Clues to patients' explanations and their concerns about their illnesses. A call for active listening. Arch Fam Med. (2000) 9:222–7. doi: 10.1001/archfami.9.3.222
61. Jani BD, Blane DN, Mercer SW. The role of empathy in therapy and the physician-patient relationship. Forsch Komplementmed. (2012) 19:252–7. doi: 10.1159/000342998
62. Ventres WB. The Q-list manifesto: how to get things right in generalist medical practice. Fam Syst Health. (2015) 33:5–13. doi: 10.1037/fsh0000100
63. Frankel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. J Med Pract Manage. (2001) 16:184–91.
64. Ventres WB. Looking inward: intentions of practice for patient-centered care. Ann Fam Med. (2017) 15:171–4. doi: 10.1370/afm.2037
65. Ventres W, Haq C. Toward a cultural consciousness of self-in-relationship: from “us and them” to “we”. Fam Med. (2014) 46:691–5.
66. Adashi EY. Money and medicine: indivisible and irreconcilable. AMA J Ethics. (2015) 17:780–6. doi: 10.1001/journalofethics.2015.17.8.msoc1-1508
68. Hewa S, Hetherington RW. Specialists without spirit: limitations of the mechanistic biomedical model. Theor Med. (1995) 16:129–39. doi: 10.1007/BF00998540
69. Wilson HJ. The myth of objectivity: is medicine moving toward a social constructivist medical paradigm? Fam Pract. (2000) 17:203–9. doi: 10.1093/fampra/17.2.203
70. FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. (2017) 18:19. doi: 10.1186/s12910-017-0179-8
71. Vaidyanathan B. Professional socialization in medicine. AMA J Ethics. (2015) 17:160–6. doi: 10.1001/virtualmentor.2015.17.2.msoc1-1502
72. Vidaeff AC, Kerrigan AJ, Monga M. Cross-cultural barriers to health care. South Med J. (2015) 108:1–4. doi: 10.14423/SMJ.0000000000000221
73. Tervalon M, Murray-Garcia J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Healthcare Poor Underserved. (1998) 9:117–25. doi: 10.1353/hpu.2010.0233
74. Carmichael LP, Carmichael JS. The relational model in family practice. Marriage Fam Rev. (1982) 4:123–33. doi: 10.1300/J002v04n01_07
75. Ventres W, Tunzi M. Ways of being in generalist practice: using five “T” habits of mind to guide ethical behavior. J Clin Ethics. (2020) 31:184–90.
76. Birks YF. Watt IS. Emotional intelligence and patient-centred care. J R Soc Med. (2007) 100:368–74. doi: 10.1177/014107680710000813
77. Woods NN, Mylopoulos M, Nutik M, Freeman R. Defining the specialist generalist: the imperative for adaptive expertise in family medicine. Can Fam Physician. (2021) 67:321–2. doi: 10.46747/cfp.6705321
78. Konkin J, Grave L, Cockburn E, Couper I, Stewart RA, Campbell D, et al. Exploration of rural physicians' lived experience of practising outside their usual scope of practice to provide access to essential medical care (clinical courage): an international phenomenological study. BMJ Open. (2020) 10:e037705. doi: 10.1136/bmjopen-2020-037705
79. Strasser R, Worley P, Cristobal F, Marsh DC, Berry S, Strasser S, Ellaway R. Putting communities in the driver's seat: the realities of community-engaged medical education. Acad Med. (2015) 90:1466–70. doi: 10.1097/ACM.0000000000000765
80. Ventres W, Crowder J. When I say … anthropological gaze. Med Educ. (2018) 52:590–1. doi: 10.1111/medu.13502
81. Ventres W, Boelen C, Haq C. Time for action: key considerations for implementing social accountability in the education of health professionals. Adv Health Sci Educ Theory Pract. (2018) 23:853–62. doi: 10.1007/s10459-017-9792-z
82. Ventres WB. Becoming a doctor: one physician's journey beyond competence. J Grad Med Educ. (2014) 6:631–3. doi: 10.4300/JGME-D-14-00144.1
83. Wald HS. Professional identity (trans)formation in medical education: reflection, relationship, resilience. Acad Med. (2015) 90:701–6. doi: 10.1097/ACM.0000000000000731
84. Colbert CY, Graham L, West C, White BA, Arroliga AC, Myers JD, et al. Teaching metacognitive skills: helping your physician trainees in the quest to 'know what they don't know'. Am J Med. (2015) 128:318–24. doi: 10.1016/j.amjmed.2014.11.001
85. Kumagai AK, Naidu T. Reflection, dialogue, and the possibilities of space. Acad Med. (2015) 90:283–8. doi: 10.1097/ACM.0000000000000582
86. Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE Guide No. 63. Med Teach. (2012) 34:e102–15. doi: 10.3109/0142159X.2012.650741
87. Ventres WB. Where I practice: on the spaces of family medicine. J Am Board Fam Med. (2015) 28:841–4. doi: 10.3122/jabfm.2015.06.150021
88. Browne K, Roseman D, Shaller D, Edgman-Levitan S. Analysis & commentary. Measuring patient experience as a strategy for improving primary care. Health Aff . (2010) 29:921–5. doi: 10.1377/hlthaff.2010.0238
90. Platt FW. Conversation Repair: Case Studies in Doctor-Patient Communication. Boston: Little, Brown and Company (1995). 194 p.
Keywords: biopsychosocial models, general practitioners, medical education, medical philosophy, physician-patient relations, primary care, systems theory
Citation: Ventres WB and Frankel RM (2021) Personalizing the BioPsychoSocial Approach: “Add-Ons” and “Add-Ins” in Generalist Practice. Front. Psychiatry 12:716486. doi: 10.3389/fpsyt.2021.716486
Received: 28 May 2021; Accepted: 26 October 2021;
Published: 24 November 2021.
Edited by:
Tziporah Rosenberg, University of Rochester, United StatesReviewed by:
Marcelo Saad, Albert Einstein Israelite Hospital, BrazilJames Olumide Olufowote, University of Oklahoma, United States
Shmuel Reis, Hebrew University of Jerusalem, Israel
Copyright © 2021 Ventres and Frankel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: William B. Ventres, V3ZlbnRyZXNAVWFtcy5lZHU=
 William B. Ventres
William B. Ventres Richard M. Frankel
Richard M. Frankel