
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 23 August 2021
Sec. Public Mental Health
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.714597
This article is part of the Research Topic Coercion in Psychiatry: Epidemiology, Effects and Prevention View all 16 articles
Background: The Liangshan Yi Autonomous Prefecture has one of the most serious human immunodeficiency virus (HIV) epidemics in China. Evidence shows HIV-related stigma toward people living with HIV (PLWH) among nurses impedes HIV prevention and treatment. However, only limited research about HIV-related stigma toward PLWH from the perspective of nurses in Liangshan has been conducted.
Objective: This study aimed to assess HIV-related stigma toward PLWH among nurses and determine factors associated with it in Liangshan, China.
Design: We conducted a cross-sectional survey using a stratified, random cluster sampling method.
Participants: Registered nurses (N = 1,248; primary hospitals = 102, secondary hospitals = 592, tertiary hospitals = 554) who were aged 18 or older, worked in the selected hospitals for at least 6 months, and consented to participate were recruited.
Methods: All participants completed an anonymous online survey measuring sociodemographic characteristics, HIV-related stigma and HIV knowledge. We used multiple stepwise regression analysis to examine factors associated with HIV-related stigma toward PLWH among these nurses.
Results: The mean score of HIV-related stigma among nurses was 50.7 (SD = 8.3; range 25–78). Nurses who were more experienced, had higher levels of education, and were working in tertiary hospitals reported higher level of HIV-related stigma. Those who had better HIV knowledge, reported a willingness to receive HIV-related training, were working in areas that had a high prevalence of HIV, had prior experience working in AIDS specialized hospitals, and worked in hospitals that had policies to protect PLWH showed a lower level of HIV-related stigma toward PLWH.
Conclusions: Our findings suggested that providing culturally congruent education and training about HIV and care, and having hospitals that promoted policies protecting PLWH, may reduce HIV-related stigma toward PLWH among nurses in China.
Stigma related to the human immunodeficiency virus (HIV) is prevalent and has been identified to be a major barrier for HIV prevention and treatment (1). Researchers suggest that HIV-related stigma is also still a barrier for people living with HIV (PLWH) to disclose their HIV status and to seek and adhere to treatments; consequently, this barrier has an adverse impact on their health (2–4). HIV-related stigma exists in nursing care worldwide and has large impact on the health outcomes of PLWH (5–9).
Herek (10) defined HIV-related stigma as “prejudice, discounting, discrediting, and discrimination directed at people perceived to have acquired immune deficiency syndrome (AIDS) or HIV” (p. 1107). Manifestations of HIV-related stigma within the healthcare system include neglecting and avoidance of nursing care, exaggerated precautions, judgmental remarks and behavior, labeling patients and viewing them as attention seekers and breaches of confidentiality (11–14). Empirical evidence shows that the main causes of HIV-related stigma among healthcare providers are their lack of awareness of the stigma perceived by PLWH and the negative impact of stigma on PLWH, fear of casual contact due to poor knowledge about HIV transmission and the association of HIV with improper or immoral behavior (15).
Researchers have found that certain sociodemographic characteristics of nurses, such as age, gender, race, marital status, educational level, and certain religious belief are associated with HIV-related stigma toward PLWH (16–21). Furthermore, longer working experience, lower levels of HIV knowledge and nurses working at Islamic hospitals have also been associated with higher levels of stigmatizing attitudes (5, 17, 20, 22).
Findings about the relationship of working at HIV clinics with the level of HIV-related stigma among healthcare providers are mixed in the literature (11, 19, 23). Structural and policy support in HIV clinics have been found to reduce HIV-related stigma toward PLWH in healthcare providers, including HIV-related training, resources for universal precaution and available access to post-exposure prophylaxis (11, 15).
Due to the rapid increase of HIV epidemic in China, Chinese government announced a national AIDS control policy—“Four Frees and One Care”—in 2003. This national policy refers to free antiretroviral drugs treatment to AIDS patients living in rural areas or individuals without insurance living in urban areas, free voluntary counseling and testing (VCT), free drugs treatment to HIV-infected pregnant women to prevent mother-to-child transmission (PMCT) and HIV testing of newborns, free schooling for AIDS orphans, and care and financial assistance to PLWH (24). Under this national policy, a growing number of PLWH have received free tests, consultations, and treatments, and the associated mortality rate has been reduced (24).
In China, the Liangshan Yi Autonomous Prefecture is unique; it has the largest concentration of Yi (彝 族), one of the largest minority groups in China, and has one of the most serious epidemics of HIV in China (25). In fact, nearly 50% of PLWH in Liangshan were infected through injecting drugs (26). Its special cultural background, extreme poverty, low level of education, and prevalent substance use through shared needles in this geographic area have made Yi people particularly vulnerable to HIV infection (27). In order to provide the best possible and culturally congruent care for PLWH, it is critical to optimize nurses' roles in providing HIV-related care (28). However, there is a very little understanding of nurses' HIV-related stigma toward PLWH and factors associated with the stigma in Liangshan. To address this gap, our study aimed to answer the following research questions: (a) what is the status of HIV-related stigma toward PLWH among nurses in Liangshan, and (b) what are the factors associated with HIV-related stigma toward PLWH in nurses in Liangshan?
We conducted a cross-sectional study from September to November 2017 in Liangshan. Hospitals in China are designated as primary, secondary and tertiary hospitals based on a hospital's capacity of providing medical care, education and research. Primary hospitals have <100 beds and focus on health education, disease prevention and health care, rehabilitation, family planning, and common and frequent disease management. Secondary hospitals usually have beds between 100 and 500 and provide comprehensive health care, medical education and research. Tertiary hospitals typically have more than 500 beds and provide comprehensive health services at the city, provincial or national level and carry a more important role in medical education and research (29). In total, there are 15 primary, 33 secondary, 4 tertiary hospitals in Liangshan.
In total, there are 15 primary, 33 secondary, 4 tertiary hospitals in Liangshan. Using a stratified, random cluster sampling method, we selected three primary, five secondary, and two tertiary hospitals in Liangshan by random number. Our target participants were registered nurses aged 18 or older who had worked in the selected hospitals for at least 6 months and consented to participate.
We calculated the required sample size based on the formula below (30). The required study size was 1,223 (SD = 8.92; effective size δ = 0.50; α = 0.05; Zα/2 = 1.96)
In each hospital, we first contacted the head nurse of its nursing department for approval and assistance in recruiting nurses. Once we received approval, we sent eligible nurses an online survey link, including a consent form describing the purpose, procedures, the potential risks and benefits of the study. Nurses who consented to participate received a link to access the online anonymous survey.
We received approval from the West China Hospital Medical Ethics Committee prior to implementation of the study [No. 430(2017)]. The electronic version of informed consent was received from all participants.
Our survey consisted of variables shown in the literature to be related to HIV-related stigma in healthcare providers. It included questions about individual and workplace characteristics, HIV-related stigma scale for health care workers (31), and HIV knowledge scale (32). Both the stigma and knowledge scales have been tested in China's population (31, 32).
Individual characteristics included age, gender, ethnicity, educational level, years of experience working as a nurse, experience of providing care to PLWH, prior experience of HIV-related training, and willingness to receive HIV-related training. Workplace characteristics consisted of questions regarding level of hospital s/he worked, HIV prevalence area (high vs. low; high prevalence was defined as an area with ≥1% HIV prevalence), prior experience working in AIDS specialized hospitals, universal precaution supplies and policies in workplace that protect PLWH from stigma.
We used a 17-item “HIV-related stigma scale for health care workers” developed by Stein and Li (31) to assess the HIV-related stigma among nurses. This multidimensional scale includes five subscales: Discrimination Intent at Work (four items), Opinion about Health Care for HIV-infected Patients (three items), Prejudiced Attitudes (four items), Internalized Shame (three items), and Fear of PLWHA (three items). Scores for each item ranges from 1 (strongly agree) to 5 (strongly disagree). All items were reverse-scored when appropriate to have higher total score suggesting higher levels of HIV-related stigma toward PLWH. Stein and Li (31) reported adequate internal consistency (alpha = 0.68–0.82) and construct validity of the scale.
We measured HIV knowledge using a Chinese version HIV knowledge scale (32), adapted from Jemmott et al. (33). It is a 24-item scale assessing nurses' knowledge of basic characteristic and transmission routes of HIV. Responses of each scale item were: “true,” “false” or “not sure.” Participants received 1 point if their answers were correct, and they received 0 points if their answers were incorrect or “not sure.” A higher total score indicated higher levels of HIV knowledge.
We used IBM SPSS 22.0 (34) to manage and analyze data. We used the mean, standard deviation (SD), frequency and percentage to describe distributions of individual and workplace variables, HIV knowledge and HIV-related stigma scores. Pearson's r correlation was used to examine correlations between age, years of working experience, HIV knowledge and HIV-related stigma. One-way analyses of variance (ANOVA) for polytomous variables and t-tests for dichotomous variables were used to examine variables that were associated with HIV-related stigma toward PLWH. Variables that were found to be theoretically important and associated with HIV-related stigma at a significant level of P < 0.05 at the univariate analysis were entered into the multivariate analysis. We further conducted multiple stepwise regression analysis to investigate associated factors of HIV-related stigma toward PLWH. A P-value < 0.05 was used to indicate statistical significance.
This study recruited 1,289 registered nurses. In total, 9 refused to participate, 22 did not respond and 2 did not complete the questionnaire. Eight of them were excluded because they were younger than 18 years old or had <6 months of work experience. Thus, a final sample of 1,248 participants was included in the analysis.
As shown in Table 1, the mean age of nurses was 30.2 years old (SD = 7.2), with a range of 19–55. Almost all (98.4%) respondents were females; 72.2% (n = 902) were Han ethnicity; 62.8% (n = 784) had an associated degree; and 90.4% (n = 1,128) worked in low prevalence areas. In terms of working experience, the mean year was 8.8 (SD = 7.8). Regarding HIV-related experience and training, although only 12.7% (n = 158) of the participants had prior experience working in AIDS specialized hospitals, 84.2% (n = 1,051) of them had provided care for PLWH. While 90.1% (n = 1,124) of the participants were willing to receive HIV-related training, only 63.1% (n = 787) of them had received the training in the past. Majority (95.5%) of the participants reported that the hospitals where they worked provided sufficient universal precaution supplies, and 86.9% (n = 1,084) reported that the hospitals had policies to protect PLWH from stigma.
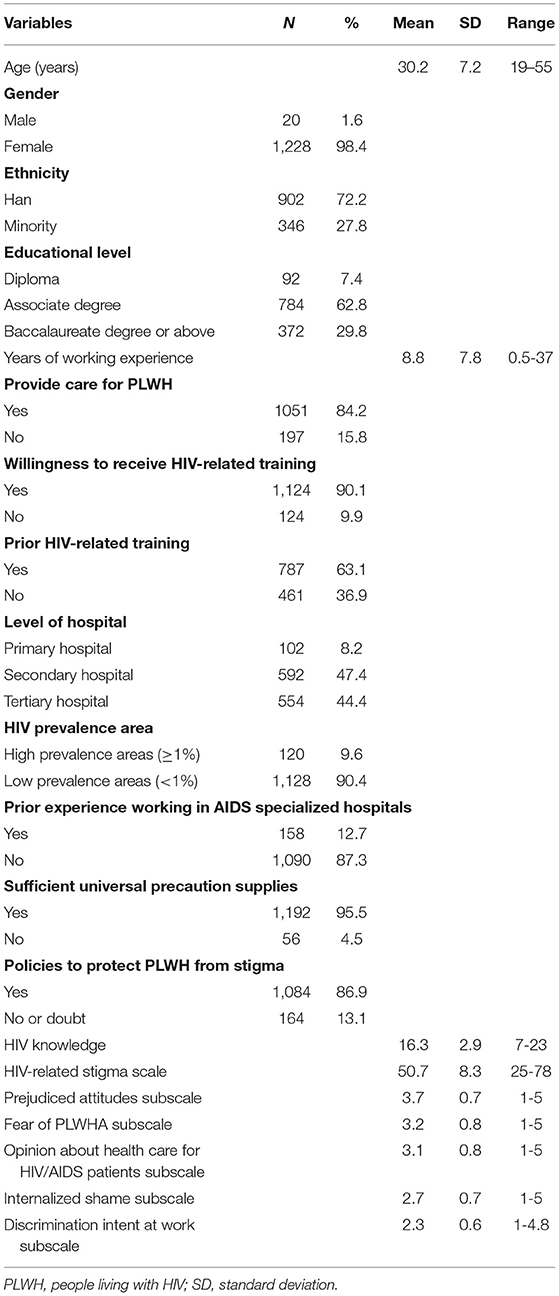
Table 1. Individual and workplace characteristics, HIV knowledge and HIV-related stigma toward PLWH.
As for HIV knowledge, the mean total score was 16.3 (SD = 2.9). The mean total score for HIV-related stigma among registered nurses was 50.7 (SD = 8.3). Among the five subscales, “prejudiced attitudes” had the highest scores (M = 3.7, SD = 0.7) while “discrimination intent at work” had the lowest scores (M = 2.3, SD = 0.6).
The relationships between HIV-related stigma and other study variables are shown in Table 2. A higher HIV-related stigma score was significantly related to longer years of work experience (r = 0.06, P < 0.05), and lower levels of HIV knowledge(r = −0.23, P < 0.01). The results of group differences in HIV-related stigma score are presented in Table 3. Nurses who were members of the Han ethnic group (t = 3.70, P < 0.01), were working in low HIV prevalence areas (t = 6.06, P < 0.01), had higher educational levels (F = 5.89, P < 0.05), worked at a higher hospital level (F = 11.85, P < 0.01), and had not worked in specialized AIDS hospitals (t = 4.62, P < 0.01) reported higher HIV-related stigma score. Nurses' willingness to receive HIV-related training (t = 6.21, P < 0.01), experience of having received HIV-related training in the past (t = 2.65, P < 0.05), and working at a hospital where had policies to protect PLWH from stigma (t = 5.70, P < 0.01) reported a lower level of HIV-related stigma toward PLWH.
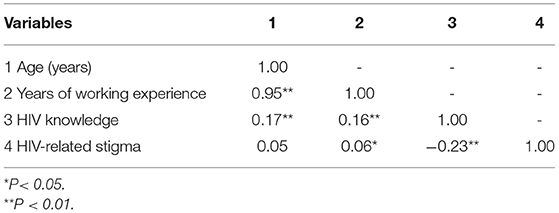
Table 2. Correlations between age, years of working experience, HIV knowledge and HIV-related stigma.
Table 4 presents the multiple stepwise regression analysis results. The findings suggested that a higher HIV-related stigma was associated with nurses who were more educated (associated degree or higher vs. diploma), had longer years of working experience, were working in the tertiary hospitals, did not have prior experience working in specialized AIDS hospitals, were not willing to receive HIV-related training, worked in low HIV prevalence areas, working in a hospital that had policies to protect PLWH from stigma and had higher levels of HIV knowledge (all P < 0.05).
To the best of our knowledge, this study is the first to exam HIV-related stigma toward PLWH and factors associated with it among nurses in Liangshan, China. The mean score for HIV-related stigma was high, which is similar to findings from research conducted in other regions of China (30, 35). As high levels of HIV-related stigma toward vulnerable PLWH population are related poor nursing care and negative health outcomes (36, 37), PLWH may not receive proper nursing care due to nurses' high levels of HIV-related stigma toward this population in Liangshan.
Compared with nurses who had an associate degree or higher level of education, diploma-educated nurses reported a lower level of HIV-related stigma, consistent with prior research (38, 39). Deacon and Boulle (40) suggested that higher-educated nurses might have more prejudicial attitudes due to a greater gap in social status between them and PLWH. Similar to other researchers (7, 9, 21), we found that nurses with better HIV knowledge reported no matter what the level of education, a lower level of HIV-related stigma toward PLWH overall, and in particularly, less fear of AIDS. This finding suggested the critical role of HIV knowledge in reducing fear-based stigma (41). Since there was no significant difference of HIV knowledge between nurses with different educational levels, HIV education should target all nurses.
We also found that nurses who had longer years of working experience reported a higher level of HIV-related stigma toward PLWH, a finding similar to that in other studies (17, 22). A possible explanation is that nurses who were more experienced might assign nursing care to nurses with less experience (14). Thus, junior nurses were more likely to provide care to PLWH and this experience might reduce their levels of HIV-related stigma compared with nurses who were more experienced.
Consistent with Li et al. (38), we found that nurses working in the tertiary hospitals had a higher level of HIV-related stigma toward PLWH. In China, tertiary hospitals that provide comprehensive services to a larger patient population are more likely to receive referrals of PLWH with opportunistic infections or other illnesses that might not be able to be cured. The complexities of providing care to terminally ill AIDS patients may make these nurses experience burnout and form avoidance attitudes (5, 42).
Our findings supported that nurses working in high HIV prevalence areas and having prior working experience in AIDS specialized hospitals had a lower level of HIV-related stigma, which is also similar to findings in prior research (43, 44). Nurses who worked in high HIV prevalence areas and had prior working experience in AIDS specialized hospitals had more experience in taking care of PLWH. Increasing exposure to and more experience of interacting with PLWH were found to be related to a lower level of HIV-related stigma and higher confidence in taking care of this vulnerable population (23, 45). Moreover, nurses working in high HIV prevalence areas and having prior working experience in AIDS specialized hospitals received more institutional supports and training (43, 44), which were found to reduce their anxiety about HIV infection, thereby reducing their stigma toward PLWH (19, 36, 38).
The significant relationship between nurses' prior HIV-related training and their HIV-related stigma was indicated in t-test but not in regression analyses when other variables were held constant. This inconsistent finding may be due to the differences in HIV training, such as content, format and frequency, as they have significant impact on the effectiveness of the training. Further, nurses who were willing to receive HIV-related training reported lower levels of HIV-related stigma. Thus, future research should examine characteristics of successful HIV training for nurses to reduce HIV-related stigma toward PLWH and promote PLWH's optimal health outcomes.
Research has supported the conclusion that stigma-reduction interventions, including policy development, led to positive changes in HIV-related stigma in health care settings (46), which is consistent with our findings. The results indicated that nurses working in the hospitals that implemented policies to protect PLWH from stigma had lower levels of HIV-related stigma toward PLWH. However, we did not find a significant relationship between hospitals that provided sufficient universal precaution supplies and nurses' HIV-related stigma. This might be explained by a lack of variance in this variable, as the majority (95.5%) of nurses reported that universal precaution supplies were provided in the hospitals where they worked.
Given the high prevalence rate of PLWH in Liangshan, providing nurses with comprehensive HIV-related training and requiring hospitals to have policies to reduce HIV-related stigma toward PLWH are critical to reducing the high prevalence rate of PLWH.
Several study limitations should be noted. Given the nature of cross-sectional survey design, it is challenging to draw causal relationships between variables. Further, HIV-related stigma is a sensitive topic in China, and so the validity of self-reported data may not be optimal. With these limitations in mind, our anonymous survey should have minimized the participants' social desirability and bias. However, this online study might exclude people who are not comfortable using technology. Using the stratified random cluster sampling to obtain a powered sample with sufficient sample size enhanced the representation of our target population and therefore increased the external validity of the findings.
The present study was the first to examine the level of HIV-related sigma toward PLWH and factors associated with the stigma in nurses in Liangshan, an area that has one of the most serious HIV epidemics in China. The findings revealed high levels of HIV-related stigma among nurses in Liangshan. Nurses' high levels of HIV knowledge, willingness to receive HIV-related training, and working in the hospitals that had anti-stigma policies were significantly related to their lower levels of stigma toward PLWH. Comprehensive HIV-related training that addresses these factors and incorporates the unique economic and cultural contexts of Liangshan will help nurses to reduce associated stigma and, in turn, provide culturally congruent care to PLWH and promote their optimal health outcomes.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
We received approval from the West China Hospital Medical Ethics Committee prior to implementation the study [No. 430(2017)]. The participants provided their electronic informed consent to participate in this study.
YY, SW, and HC: study design and data collection. YY and AC: analysis and interpretation of data. YY: writing. AC, SW, and HC: critical revisions of manuscript for important intellectual content. SW and HC: supervision of the study. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to express our sincere gratitude to the nurse who participated in this research and to hospital administrators who approved and assisted with recruitment.
1. Joint United Nations Programme on HIV/AIDS (UNAIDS): Global AIDS update 2016. Available online at: http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf (accessed December 2, 2019).
2. Brinsdon A, Abel G, Desrosiers J. “I'm taking control”: how people living with HIV/AIDS manage stigma in health interactions. AIDS Care. (2017) 29:185–8. doi: 10.1080/09540121.2016.1204420
3. Essomba EN, Kollo B, Ngambi MK, Assomba L, Etang K, Mapoure Y, et al. Stigma and discrimination associated with HIV/AIDS in health care settings: a comparative study in two hospitals of different categories in Douala-Cameroon. J MedBiomed Sci. (2017) 3:14–22. doi: 10.4314/jmbs.v3i1.3
4. Saki M, Kermanshahi SMK, Mohammadi E, Mohraz M. Perception of patients with HIV/AIDS from stigma and discrimination. Iran Red Crescent Med J. (2015) 17:e23638. doi: 10.5812/ircmj.23638v2
5. Delobelle P, Rawlinson JL, Ntuli S, Malatsi I, Decock R, Depoorter AM. HIV/AIDS knowledge, attitudes, practices and perceptions of rural nurses in south Africa. J Adv Nurs. (2009) 65:1061–73. doi: 10.1111/j.1365-2648.2009.04973.x
6. Kermode M, Holmes W, Langkham B, Thomas MS, Gifford S. HIV-related knowledge, attitudes & risk perception amongst nurses, doctors & other healthcare workers in rural India. Indian J Med Res. (2005) 122:258–64.
7. Li L, Li Y, Zeng K, Wu Y. Knowledge and attitudes to HIV/AIDS in Chinese registered nurses. J Centr South Univ. (2011) 36:121–7. doi: 10.3969/j.issn.1672-7347.2011.02.005
8. Vorasane S, Jimba M, Kikuchi K, Yasuoka J, Nanishi K, Durham J, et al. An investigation of stigmatizing attitudes towards people living with HIV/AIDS by doctors and nurses in Vientiane, Lao PDR. BMC Health Serv Res. (2017) 17:125. doi: 10.1186/s12913-017-2068-8
9. Wu HC, Ko NY, Shih CC, Feng MC. HIV/AIDS: an exploration of the knowledge, attitude, infection risk perceptions, and willingness to care of nurses. Hu Li Za Zhi. (2014) 61:43–53. doi: 10.6224/JN.61.5.43
11. Andrewin A, Chien LY. Stigmatization of patients with HIV/AIDS among doctors and nurses in Belize. AIDS Patient Care STDs. (2008) 22:897–906. doi: 10.1089/apc.2007.0219
12. Greeff M, Phetlhu R, Makoae LN, Dlamini PS, Holzemer WL, Naidoo JR, et al. Disclosure of HIV status: experiences and perceptions of persons living with HIV/AIDS and nurses involved in their care in Africa. Qual Health Res. (2008) 18:311–24. doi: 10.1177/1049732307311118
13. Kohi TW, Makoae L, Chirwa M, Holzemer WL, Phetlhu DR, Uys L, et al. HIV and AIDS stigma violates human rights in five African countries. Nurs Ethics. (2006) 13:404–15. doi: 10.1191/0969733006ne865oa
14. Manganye BS, Maluleke TX, Lebese RT. Professional nurses' views regarding stigma and discrimination in the care of HIV and AIDS patients in rural hospitals of the Limpopo province, South Africa. Afr J AIDS Res. (2013) 12:33–40. doi: 10.2989/16085906.2013.815411
15. Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: what works? J Int AIDS Soc. (2009) 12:15. doi: 10.1186/1758-2652-12-15
16. Aghamolaei T, Tavafian SS, Hasani L, Zare S. Attitudes of healthcare providers towards patients with HIV/AIDS in Bandar Abbas. Arch Iran Med. (2009) 12:298–301.
17. Kostak MA, Unsar S, Kurt S, Erol O. Attitudes of turkish midwives and nurses working at hospitals towards people living with human immunodeficiency virus/acquired immune deficiency syndrome. Int J Nurs Pract. (2012) 18:437–44. doi: 10.1111/j.1440-172X.2012.02062.x
18. Ekstrand ML, Ramakrishna J, Bharat S, Heylen E. Prevalence and drivers of HIV stigma among health providers in urban India: implications for interventions. J Int AIDS Soc. (2013) 16:18717. doi: 10.7448/IAS.16.3.18717
19. Stringer KL, Turan B, Mccormick L, Durojaiye M, Nyblade L, Kempf M-C, et al. HIV-related stigma among healthcare providers in the Deep South. AIDS Behav. (2016) 20:115–25. doi: 10.1007/s10461-015-1256-y
20. Waluyo A, Culbert GJ, Levy J, Norr KF. Understanding HIV-related stigma among Indonesian nurses. J Assoc Nurs AIDS Care. (2015) 26:69–80. doi: 10.1016/j.jana.2014.03.001
21. Zarei N, Joulaei H, Darabi E, Fararouei M. Stigmatized attitude of healthcare providers: a barrier for delivering health services to HIV positive patients. Int J Community Based Nurs Midwifery. (2015) 3:292–300.
22. Suominen T, Koponen N, Mockiene V, Raid U, Istomina N, Vänskä M-L, et al. Nurses' knowledge and attitudes to HIV/AIDS—an international comparison between Finland, Estonia and Lithuania. Int J Nurs Pract. (2010) 16:138–47. doi: 10.1111/j.1440-172X.2010.01822.x
23. Feyissa GT, Abebe L, Girma E, Woldie M. Stigma and discrimination against people living with HIV by healthcare providers, Southwest Ethiopia. BMC Public Health. (2012) 12:522. doi: 10.1186/1471-2458-12-522
24. Ministry of Foreign Affairs People's Republic of China (MFA). Report on China's implementation of the millennium development goals (2000–2015). Available online at: http://www.undp.org/content/dam/china/docs/Publications/UNDP-CH-SSC-MDG2015_English.pdf (accessed December 2, 2019).
25. National Health Commission of the People's Republic of China (NHC). 2015 China AIDS response progress report. Available online at: http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf (accessed December 2, 2019).
26. Mo SD, Wang Z, Deng F. Analysis of epidemilogical characteristics and countermeaure of AIDS in Liangshan state. Mod Prevent Med. (2008) 35:630–5.
27. Zhu C, Zhou Y, Song X, Jiang Q. Review on the influene factors of AIDS epidemic and control in Liangshan Prefecture Sichuan Province of China. Fudan Univ J Med Sci. (2015) 42:675–9. doi: 10.3969/j.issn.1672-8467.2015.05.020
28. Chen WT, Shiu CS, Simoni J, Fredriksen-Goldsen K, Zhang F, Zhao H. Optimizing HIV care by expanding the nursing role: patient and provider perspectives. J Adv Nurs. (2010) 66:260–8. doi: 10.1111/j.1365-2648.2009.05165.x
29. World Health Organization (WHO). People's Repuclic of China health system review. Available online at: http://apps.who.int/iris/bitstream/handle/10665/208229/9789290617280_eng.pdf?sequence=1&isAllowed=y
30. Yang J, Liu H, Niu L. Research on correlation between nurses' discrimination and their nursing behaviors for HIV infections and AIDS patients. Chin Nurs Res. (2015) 29:2448–52. doi: 10.3969/j.issn.1009-6493.2015.20.006
31. Stein JA, Li L. Measuring HIV-related stigma among Chinese service providers: confirmatory factor analysis of a multidimensional scale. AIDS Behav. (2008) 12:789–95. doi: 10.1007/s10461-007-9339-z
32. Wang H, Yang A, Williams AB. Knowledge, attitudes, willingness of care about HIV/AIDS among nursing college students. J Nurs Sci. (2003) 18:166–8. doi: 10.3969/j.issn.1001-4152.2003.03.002
33. Jemmott LS, Jemmott JB, Cruzcollins M. Predicting AIDS patient care intentions among nursing students. Nurs Res. (1992) 41:172–7. doi: 10.1097/00006199-199205000-00009
34. IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp (2013).
35. Han Y. The study of correlation between nurses' stigma toward PLWHA and nurse caring behaviors (master's thesis). Central South University, Changsha, China (2009).
36. Mill J, Harrowing J, Rae T, Richter S, Minnie K, Mbalinda S, et al. Stigma in AIDS nursing care in sub-Saharan Africa and the Caribbean. Qual Health Res. (2013) 23:1066–78. doi: 10.1177/1049732313494019
37. Kay ES, Rice WS, Crockett KB, Atkins GC, Batey DS, Turan B. Experienced HIV-Related stigma in health care and community settings: mediated associations with psychosocial and health outcomes. J Acquir Immune Defic Syndr. (2018) 77:257–63. doi: 10.1097/QAI.0000000000001590
38. Li L, Wu Z, Wu S, Zhaoc Y, Jia M, Yan Z. HIV-related stigma in health care settings: a survey of service providers in China. AIDS Patient Care STDs. (2007) 21:753–62. doi: 10.1089/apc.2006.0219
39. Vyas KJ, Patel GR, Shukla D, Mathews WC. A comparison in HIV-associated stigma among healthcare workers in urban and rural Gujarat. SAHARA J. (2010) 7:71–5. doi: 10.1080/17290376.2010.9724959
40. Deacon H, Boulle A. Commentary: factors affecting HIV/AIDS-related stigma and discrimination by medical professionals. Int J Epidemiol. (2007) 36:185–6. doi: 10.1093/ije/dyl255
41. Abdelrahman I, Lohiniva AL, Kandeel A, Benkirane M, Atta H, Saleh H, et al. Learning about barriers to care for people living with HIV in Egypt: a qualitative exploratory study. J Int Assoc Providers AIDS Care. (2015) 14:141–7. doi: 10.1177/2325957413488180
42. Roomaney R, Steenkamp J, Kagee A. Predictors of burnout among HIV nurses in the Western Cape. Curationis. (2017) 40:e1–e9. doi: 10.4102/curationis.v40i1.1695
43. Hamama L, Tartakovsky E, Eroshina K, Patrakov E, Golubkova A, Bogushevich J, et al. Nurses' job satisfaction and attitudes towards people living with HIV/AIDS in Russia. Int Nurs Rev. (2014) 61:131–9. doi: 10.1111/inr.12074
44. Li L, Lin C, Wu Z, Comulada WS, Ding Y. Regional differences in HIV prevalence and individual attitudes among service providers in China. Soc Sci Med. (2012) 75:283–7. doi: 10.1016/j.socscimed.2012.02.054
45. Salih MH, Tessema GA, Cherkos EA, Ferede AJ, Anlay DZ. Stigma towards people living on HIV/AIDS and associated factors among nurses' working in Amhara region referral hospitals, Northwest Ethiopia: a cross-Sectional study. Adv Nurs. (2017) 2017:1–7. doi: 10.1155/2017/6792735
Keywords: HIV-related stigma, HIV knowledge, HIV/AIDS & infectious diseases, nurses, China
Citation: Yin Y, Chen AC, Wan S and Chen H (2021) Factors Associated With HIV-Related Stigma Toward People Living With HIV Among Nurses in Liangshan Yi Autonomous Prefecture, China: A Cross-Sectional Study. Front. Psychiatry 12:714597. doi: 10.3389/fpsyt.2021.714597
Received: 25 May 2021; Accepted: 26 July 2021;
Published: 23 August 2021.
Edited by:
Bridget Hamilton, The University of Melbourne, AustraliaReviewed by:
Preethy Kathiresan, National AIDS Control Organisation, IndiaCopyright © 2021 Yin, Chen, Wan and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Chen, MTM2NjEwOTg3OEBxcS5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.