- 1Department of Learning, Informatics, Management and Ethics, Health Informatics Centre, Karolinska Institutet, Stockholm, Sweden
- 2Division of Psychology, Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
- 3Pain Clinic, Capio S:t Görans Hospital, Stockholm, Sweden
- 4Department of Physiology and Pharmacology, Karolinska Institutet, Stockholm, Sweden
The COVID-19 pandemic highlighted the need for psychological support initiatives directed toward frontline healthcare workers, which can be rapidly and sustainably implemented during an infectious disease outbreak. The current case study presents a comprehensive model of psychological support that was implemented at an intensive care unit (ICU) during the first wave of the COVID-19 pandemic. The psychological support model aimed at promoting a resilient stress reaction among frontline staff by protecting physical, social, and psychological resources. The initiatives, targeting different groups of workers, included education and training, peer support, psychologist-supervised and unsupervised group sessions, on-boarding for transferred staff, manager support, and individual sessions for workers experiencing strong stress reactions. The results of the process evaluation of this rapid implementation suggest that peer support initiatives as well as daily group sessions were the most appreciated forms of psychological support. Psychologists involved in organizing and providing the support highlighted several aspects of a successful implementation of the support model: offering support during work hours (preferably after shift), positive attitude of line managers that framed support initiatives as a team effort, and involvement of experienced psychologists able to quickly adjust the content of the support according to the current needs. The study also identified two main problems of the current implementation: the lack of efficient planning due to the use of volunteer work and the need for more structural resources on the organizational level to ensure long-term sustainability of the support model and its implementation among all groups of healthcare staff. The current case study highlights the importance of establishing permanent structural resources and routines for psychological support integrated in clinical practice by healthcare organizations to improve both rapid and sustainable response to future crises.
Introduction
The COVID-19 pandemic highlighted an urgent need for early interventions to mitigate the psychological effects of extreme work demands that healthcare workers currently experience (1). Research regarding the mental health of nurses and physicians during the current pandemic paints a worrisome picture. Symptoms indicating possibly pathological stress reactions among healthcare workers are more prevalent during the current pandemic than they were before (2–5), with a pooled prevalence of about 26% of anxiety, 24% of depressive symptoms, and almost 45% of stress symptoms among frontline workers (3). Moreover, data from previous and the current coronavirus outbreaks point out the exposure level, such as working at the frontline, as a risk factor for the development of PTSD among health care workers (6). Possible reasons for the increase in stress symptoms include higher levels of known risk factors such as cognitive, emotional, and physical demands at work (7, 8); new stressors such as risk for moral injury and worry about personal safety (9); and diminished protective mechanisms, which include recovery opportunities and psychological detachment (10).
Even before the current pandemic, work environment at intensive care units (ICU) was experienced as demanding and stressful. Up to 70% of healthcare workers at the ICU were at high risk for burnout (11), which is more than double compared to, for example, palliative care (12). This difference is attributed to higher prevalence of stressors at the ICU, including high workload, interpersonal conflicts, and moral distress (11–16).
Consequently, healthcare staff working at the ICU were recommended to be given priority in access to psychological support during the current pandemic (17). When offered appropriate psychological support, a majority of those experiencing distress during a crisis will recover (18). However, uncertainty regarding the scale and progress of a pandemic caused by an unknown virus makes it difficult to plan for effective psychological support initiatives. For this reason, a rapid implementation of psychological support for healthcare workers has proved to be challenging, both during previous crises and the current pandemic (19–21).
In this paper, we present a case study of a rapidly implemented psychological support model provided to frontline healthcare workers at an ICU during the COVID-19 pandemic. We describe the guiding principles and key interventions including various initiatives and support formats, as well as a summary of quantitative and qualitative data collected to evaluate the implementation and feasibility of the psychological support model.
The Psychological Support Model
Context and Population
During the spring of 2020, the Stockholm region was severely affected by COVID-19, as compared to other parts of Sweden and the surrounding Nordic countries. The official plan within the region was to direct patients with suspected or confirmed COVID-19 to hospitals in a specific order, and it was decided that Capio S:t Göran, an emergency hospital in the outskirts of central Stockholm, was the fifth option to use when the resources at the other large hospitals in the region were exhausted. However, due to geographical location of the hospital and the initial cluster spread pattern of the virus, many cases were presented at the Capio S:t Göran hospital much earlier than expected. Consequently, the ICU at this hospital admitted COVID-19 positive patients with respiratory failure early on, with the first patient admitted on March 8, 2020. The magnitude and severity of these cases created an extreme demand for the ICU resources, including the need for more trained staff. During the last 2 weeks of March, additional beds had to be made available and parts of the operation theater were transformed into new intensive care units, resulting in an increase of available beds from 8 to 24 (an overview of the number of additional beds and the number of patients admitted to the ICU during this period is provided in the Supplementary Figure 1).
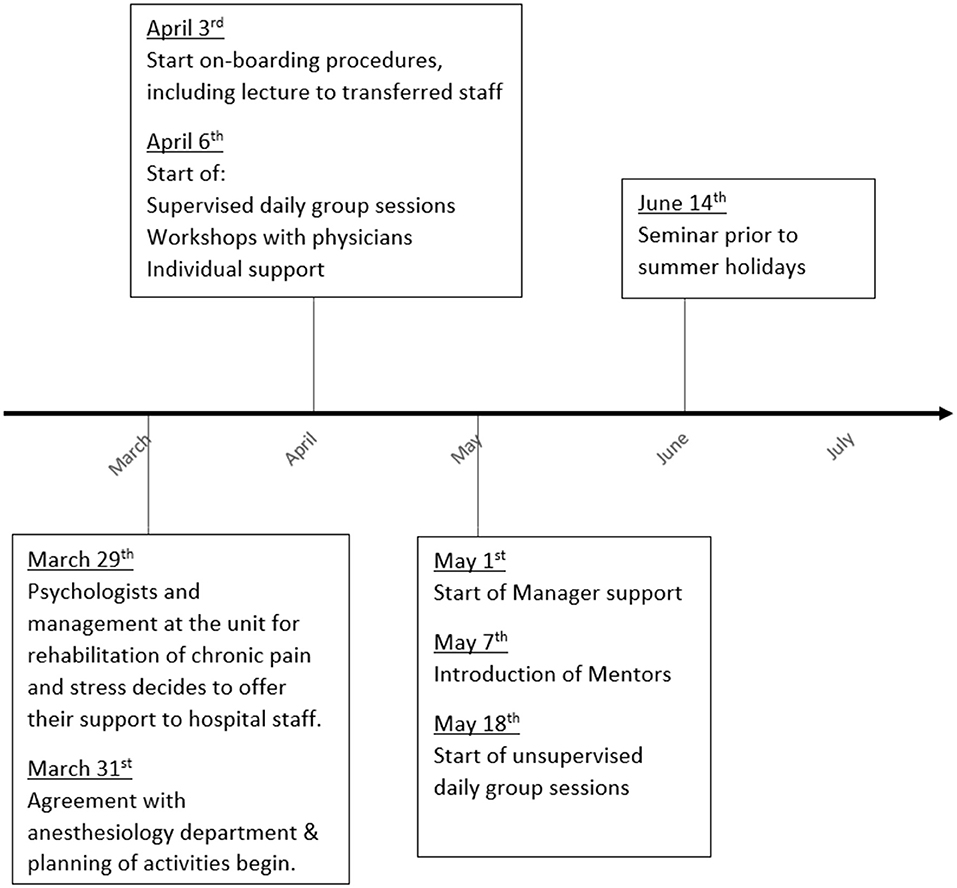
Due to the severity of the pandemic outbreak in the Stockholm Region, the employer organization and the unions decided on utilizing a time-limited crisis agreement for nurses, allowing for longer work hours to ascertain the supply of staff. In short, this agreement resulted in a work schedule based on two shifts (rather than the normal three), with weekly rotations of the schedule (i.e., every second week with 72/50 work hours). The crisis agreement was initiated by the Region on April 3 (22) and the two-shift work schedules were implemented by April 6. However, due to the increased number of patients during March, the staff was already working overtime. To meet the demand for ICU staff, nurses at other units (primarily anesthesiology and surgery) were transferred to the ICU from March 23.
The psychological support was offered to, and accepted by, the director of the anesthesiology department (including the ICU) a few days before the crisis agreement was initiated. A psychological support team was put together rapidly, consisting of three psychologists from the unit for rehabilitation of chronic pain and stress at the hospital, that operated the initiative, as well as four affiliated psychologists from Karolinska Institutet with relevant expertise. Participation was voluntary for all psychologists and provided in parallel to regular work schedules and commitments.
Model Principles
The psychological support model was developed based on a set of principles presented below.
First, the model was built based on current needs and feasibility rather than by implementing standardized interventions used in other contexts. Due to the time pressure, most of the initiatives were developed ad hoc and hastily implemented. This called for an agile approach to the development of the current model (23), which implies continuous modifications based on feedback and ongoing discussions with staff and managers. The day-to-day observations and frequent communication with managers guided the development of the support initiatives.
Second, the interventions provided at the ICU were integrated into the clinical routines. Guidelines regarding the organization of support during crises underline the necessity of close real-time monitoring for the early identification of at-risk populations and individuals, which should be seeking professional support (24–26). Thus, the support was primarily provided face-to-face at the ICU with sessions scheduled during work hours.
Third, the development of the psychological support model was guided by well-established knowledge from organizational and occupational psychology (27) and a contextual behavioral theoretical framework (28). Models of healthy work environments highlight the importance of resources and recovery in the prevention of work-related stress problems. This is especially valid when the demands are high and difficult or impossible to reduce at a given time point (29–31).
Fourth, the concept of resilience has gained increasing attention as a factor explaining the variation in individual response patterns to common stressors (32). In occupational health, resilience has been promoted as an important factor describing the ability to adapt and function well despite high demands (33, 34). Thus, when implementing the psychological support model at the ICU, we aimed at promoting resilience (i.e., resilient stress reaction) among frontline staff by protecting the most important resources: physical (sleep and recovery), social (social support networks), and psychological (competence and autonomy).
Fifth, the support model was built around diverse initiatives described below, targeting distinct groups of workers (see online Supplementary Figure 2).
Education and Training
On April 3, a 90-min lecture was provided to staff from other units that were being transferred to the ICU as part of their on-boarding. The lecture focused on stress and psychological reactions, with an emphasis on the individual's ability to actively manage the stressors in an adaptive way.
Moreover, workshops were conducted with physicians working at the ICU, aimed at increasing the awareness of stress reactions and the willingness to share these experiences with colleagues to provide and receive peer support. The workshops also contained basic training in behavioral analysis to improve the understanding of their own and other's behaviors, which promotes self-management and the ability to provide peer-support (35).
Also, seminars for all staff were offered prior to the start of summer holidays, focusing on communication with family and friends about one's own reactions and needs. A support document (available in the online Supplementary Document 3) was provided to facilitate own reflections as well as discussion with family members. Figure 1 provides a timeline over the different modules.
Daily Group Sessions
From April, daily group sessions were scheduled and supervised by psychologists. Each session lasted 30–45 min. Typically, the session started with a reminder that the session was about the own reactions of participants to stressful situations, and a brief statement from each of the participants regarding their current state of mind. Participants were also asked for any urgent concerns that they would like to address during the session. When a topic (or topics) of general interest was identified, the session focused on that. Examples of frequently occurring topics:
• feelings of insufficiency in relation to patient's and patient relative's needs
• fatigue and worrying regarding own work capacity
• uncertainties regarding the development of the pandemic and implications for health care
• problems with work-life balance including feelings of guilt in relation to children and spouse
• problems with fatigue and recovering between work shifts
• concerns regarding own safety and risks of spreading the virus to own family
• issues related to communication and need for social support from colleagues
These topics were addressed and discussed within a contextual cognitive–behavioral framework, with the objective to promote resilience in individuals and groups (28, 36). Sessions were planned to balance between actively reflecting on the current topics, communicating within the group about thoughts and feelings, and education regarding, for example, psychological reactions to stress, avoidance vs. acceptance of unwanted thoughts and feelings, or pro-social behaviors. Some sessions were more oriented toward experiential exercises, such as relaxation or present-moment awareness, as an approach to manage negative thoughts or emotions.
Mid May, psychologist-supervised group sessions were replaced by unsupervised group sessions, which used a similar predefined format and agenda. The daily sessions were prompted by the senior nurse in charge of each respective work shift. Normally, sessions were performed in small groups, sometimes in the lunchroom, but frequently in the wards due to time constraints and work demands. After each session, a standardized report was completed to keep track of the attendance and experienced meaningfulness of the sessions (see online Supplementary Document 4).
Peer Support
Starting in May, a small group of nurses involved at the ICU during the pandemic were named as mentors. Their role was to enhance the social resources by taking a proactive role, for example, facilitating communication between staff and managers, as well as providing active support to colleagues during their respective work shift. Mentors were provided a written role description (provided in Supplementary Document 5) with examples of specific behaviors, and received an introduction, where they also explicitly stated their willingness to serve as mentors.
On-boarding
To facilitate the transition of staff from other units to the ICU, an on-boarding procedure was gradually developed from early April that included (a) setting a clear time-frame for the introduction phase (3 weeks); (b) providing all managers, at both the ICU as well as the surgery and anesthesiology units, with a list of individuals who were transferred to make sure they were receiving sufficient attention; (c) subsequent to the introduction of the mentor role, staff transitioning into the ICU were assigned to one of the mentors; (d) providing technical and procedural training in specific intensive care routines.
Manager Support
Starting from May, managers at all levels in the anesthesiology department were offered targeted management support. The primary focus of this initiative was to discuss strategies to improve resilience in the staff. Support was provided according to individual needs and conducted individually or in small groups, usually weekly or bi-weekly.
Individual Support Including Risk Assessment
Individual workers experiencing strong reactions such as fatigue or anxiety that impacted on their work performance, and/or that were at risk for developing more severe problems, as perceived by themselves or the first line manager, were assessed by a psychologist in a clinical interview. The objective was to clarify the nature and level of the psychological reaction, for example, identifying work stressors, psychological symptoms, prior and co-occurring psychological concerns, stress management strategies, and social support, and to decide if additional support was needed in order to continue or return to work. Also, the individual assessment included an evaluation of potential risks (e.g., health care safety) of remaining on duty. Assessments were carried out continuously throughout the support period, normally within 3 days. For staff with work-related stress symptoms affecting the ability to perform clinical tasks, individual support was provided by a psychologist at the unit for rehabilitation of chronic pain and stress based on individual needs and a contextual behavioral framework, that is, cognitive behavioral therapy (CBT) and acceptance and commitment therapy (ACT).
Implementation and Acceptability
The rapidly implemented model of psychological support was evaluated by means of (1) a questionnaire administered to all staff and managers at the anesthesiology department (including ICU, surgery, and anesthesiology clinics), (2) an analysis of the reports completed during the unsupervised group sessions, and (3) interviews with psychologists participating in the support initiatives.
Participation in Different Initiatives
The questionnaire was administrated during late May and early June as a part of a broader research project examining psychological reactions among health care staff during the COVID-19 pandemic (37). The study was approved by the Swedish Ethical Review Authority (2020-01795). Since participation in all support initiatives was voluntary, although strongly recommended by managers, an important measure of successful implementation of the support was defined as the extent to which employees were aware of and chose to participate in the different initiatives.
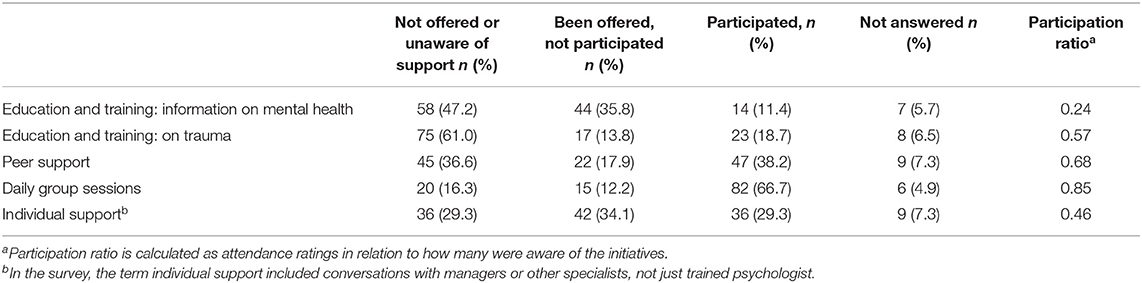
Out of 329 invited (all members of staff at the ICU, including administrative and transferred staff from operation and anesthesiology), 123 members (37.4%) of the health care staff consisting of assistant nurses (26.0%), nurses (53.7%), and physicians (20.3%) answered the survey. We calculated a participation ratio, showing relative proportion of respondents aware of an initiative that engaged in the activity. Table 1 shows participation ratio, awareness, and attendance of different types of support initiatives.
Based on questionnaire ratings, the most used support initiative was the daily group sessions with as many as 97 (78.9%) participants stating that they had been informed of the sessions, and out of these 82 (85.0%) also participated in the support at some point. A larger portion of the respondents were unaware of or chose not to participate in the educational support such as information on mental health (n = 58, 47.2%) or education on potentially traumatic events at work (n = 75, 61.0%). Looking at participation ratio, daily group sessions followed by peer support had the highest attendance ratings in relation to how many were aware of these initiatives.
Participation and Meaningfulness of Unsupervised Group Sessions
During the unsupervised group sessions, staff was instructed to complete a form stating the number of participants and perceived meaningfulness of the session assessed on a group level using a scale from 0 to 10. In sum, 96 sessions (two sessions per day) were carried out from May to August, with a mean attendance of 5 (ranging from 2 to 14) staff members per session. The level of meaningfulness was rated as follows: high (>7) = 36.5%, moderate (4–7) = 39.6%, and low (<4) = 10%. The remaining sessions were not rated.
In sessions considered to have been highly meaningful (i.e., ratings from 8 to 10), staff commented on the importance of a shared reflection at the end of the shift, cooperation, or general positive feelings within the group. While in sessions with low meaningfulness ratings (0–3), staff comments included that the group sessions were no longer needed, and that few had attended due to colleagues prioritizing to go home and rest after the shift (particularly during sessions during late summer).
Psychologists' Reflections
All psychologists who were involved in daily support sessions and support to managers were interviewed regarding the content and implementation of the psychological support model. In total, five semi structured interviews were conducted over video call by one of the first authors (SA), and all interviewees provided their written consent. Interviews were then transcribed, anonymized, and analyzed by the same author (SA). Using a thematic analysis (38), all aspects of the data that provided information on the support efforts were coded and grouped into the three themes: Utility, Challenges, and Keys to implementation, and presented in Table 2.
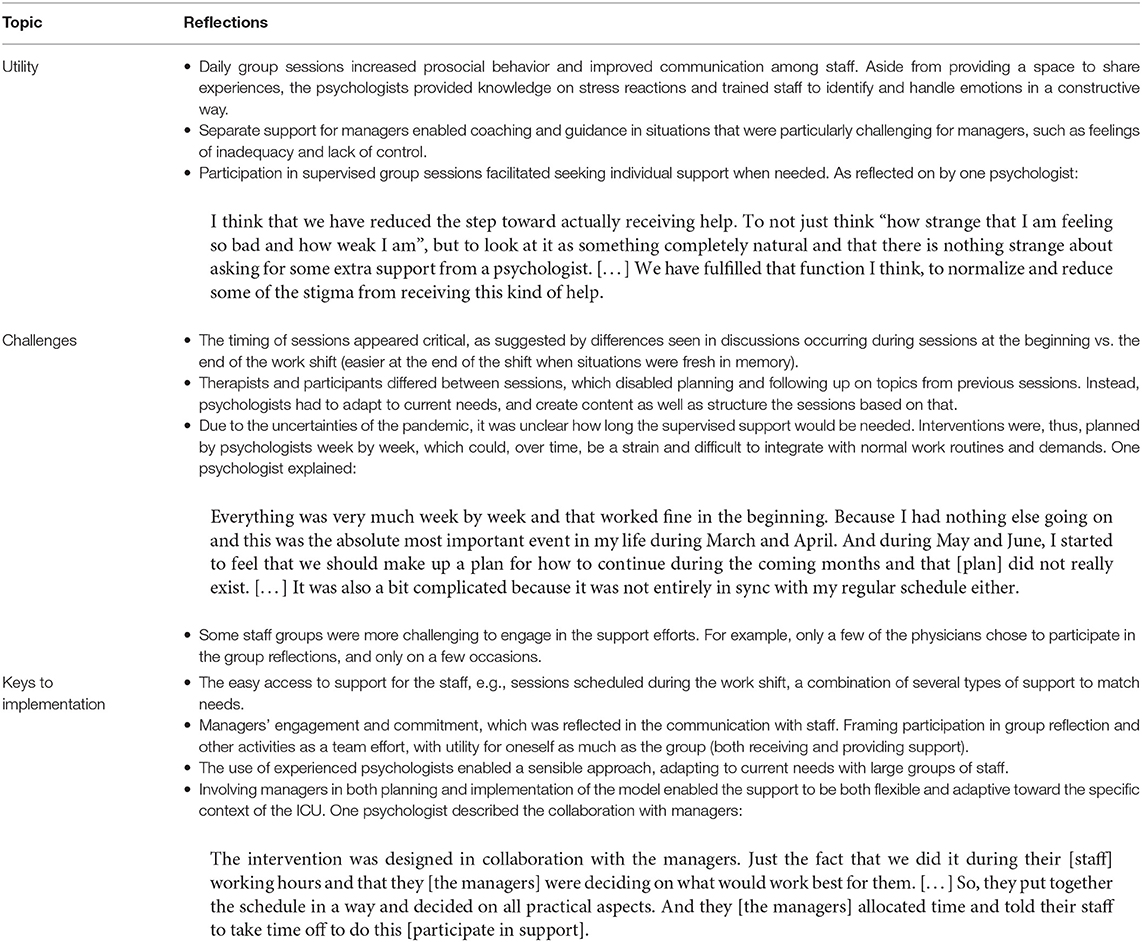
Table 2. Summary of psychologists' reflections on content and implementation of the support efforts.
Discussion
In this paper, we have presented a psychological support model rapidly implemented among frontline healthcare workers at the ICU during the first wave of the COVID-19 pandemic. The model was built, and continuously modified, based on current needs and feedback from all the participating parties. All interventions were integrated into the clinical practice and carried out face-to-face at the ICU during work hours. The psychological support aimed at promoting a resilient stress reaction among frontline staff by protecting physical, social, and psychological resources. The initiatives, targeting different groups of workers included education and training, peer support, group sessions (both supervised by psychologists and unsupervised), on-boarding for transferred staff, support to managers, and individual sessions for workers experiencing strong stress reactions.
The early guidelines for psychological support initiatives during the current pandemic were largely in agreement regarding the content and focus of such support (20, 39, 40). However, the actual attempts to implement these guidelines resulted in a variety of formats, time frames, and practical solutions. This included both onsite and online format of support (41, 42), centralized nationwide top-down interventions (43) and local support models developed for a particular hospital or unit (21), as well as initiatives based on established protocols (24) and approaches where the topics of support were dynamically adjusted according to the current needs (19). This large variety of models and protocols for psychological support calls for more integrative and reflective analyses of different approaches, their advantages, and problems (44).
Reflecting on the appropriate format of the psychological support during the pandemic, experiences from this initiative suggest a rapid implementation when needs occur. This implies that a successful implementation builds on readily available resources at a particular site. Also, reflections by the psychologists highlighted the importance of early and continuous assessment of the needs of the staff and managers to tailor the support format for different groups and individuals, as well as gradually modify and improve the interventions over time, as needed. The psychologists highlighted both the utility of providing support directed specifically toward different professions and the difficulty of reaching all groups (e.g., physicians, night shifts). Therefore, implementation requires support from first-line management and a proactive organization and planning of support efforts that are feasible and adequate to meet the needs of different groups of staff. If successful, providing support to all members of staff and managers may then trigger a positive spiral of support within the organization (45), improving self-management and the sustainability of the support.
On a related note, the results showed that support types integrated into the daily practice and work hours, such as group reflections and peer-support, were most successful in terms of participation rate. The integration of such support initiatives into daily routines requires full support and engagement not only from the managers but also from the leadership of the organization (46). Securing such formal support and resources from stakeholders at all organizational levels often involves a coordinated effort and procedural changes, which will unavoidably take time. Nonetheless, to ensure a long-term sustainability of psychological support initiatives, such process seems crucial.
A rapid implementation process of effective interventions with long-term sustainability presents the main challenge in planning for psychological support during a long-term crisis such as the COVID-19 pandemic. The rapidly implemented support initiatives, such as those presented in the current article, are built largely on volunteer work and ad hoc adjustments in clinical routines to meet the needs of the staff. However, due to conflicting demands from regular work roles and tasks, such initiatives may decline over time. Also, supporters may run out of emotional and physical resources necessary to provide extensive and continuous support (47). At the same time, health care staff will likely experience the psychological effects of the pandemic for a considerable time, perhaps years. This implies the need for health care organizations to have direct access to empirically supported and feasible psychological support programs, as well as the resources (e.g., psychologists) to run these (48). Furthermore, it is recommended for healthcare organizations to establish a professional support network of psychologists or other mental health professionals that are present at the sites and able to rapidly and sustainably allocate resources to implement psychological support when and where needed. Such a network could also support managers in how to respond to, and prevent, stress reactions among staff, and establish regular communication around work-related stress within the unit. This is especially important for units that, regardless of the COVID-19 pandemic, are exposed to a demanding work environment such as the ICU (11) or the Emergency Room (49).
The present study presents the development and rapid implementation of a psychological support model to healthcare workers during the health care crisis caused by the COVID-19 pandemic and provides preliminary support for the utility and feasibility of the model. However, the design and data available limit the conclusions that can be drawn on how both managers and members of staff have experienced the support and calls for more studies systematically tracking healthcare workers' experience of psychological support during a health care crisis, such as the COVID-19 pandemic.
Conclusion
Already after previous infectious diseases outbreaks, recommendations for employers were presented to ensure that psychological support structures are in place for those healthcare workers who are at most risk, for example, those with most patient contact (50). The COVID-19 pandemic has certainly emphasized and broadened the perspective on this need. The current case study highlights the importance of establishing permanent structural resources and routines for psychological support integrated in clinical practice by healthcare organizations to improve both rapid and sustainable response to future crises.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by The Swedish Ethical Review Authority (2020-01795). The participants provided their written informed consent to participate in this study.
Author Contributions
SA has contributed to the data curation, formal analysis, investigation, project administration, visualization, writing the original draft, reviewing, and editing the manuscript. AB has contributed to the conceptualization, funding acquisition, investigation, methodology, project administration, supervision, writing the original draft, reviewing, and editing the manuscript. AF has contributed to the conceptualization, funding acquisition, investigation, resources, methodology, and writing the original draft, reviewing, and editing the manuscript. KA has contributed to resources, validation, reviewing, and editing the manuscript. BO has provided resources and validation. FB, JH, LL, and DW have contributed to the investigation and resources. MW has contributed to the investigation, resources, validation, reviewing, and editing of the manuscript. RW has contributed to the conceptualization, funding acquisition, investigation, methodology, supervision, resources, writing of the original draft, reviewing, and editing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by a grant from AFA insurance Dnr 200136 awarded to AB, AF, and RW. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Charlotta Löwendahl and all members of staff at the Anesthesiology Department at Capio S:t Göran hospital for their support and collaboration.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.713251/full#supplementary-material
References
1. Sharifi M, Asadi-Pooya AA, Mousavi-Roknabadi RS. Burnout among healthcare providers of COVID-19; a systematic review of epidemiology and recommendations. Arch Acad Emerg Med. (2020) 9:e7. doi: 10.22037/aaem.v9i1.1004
2. Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. (2021) 141:110343. doi: 10.1016/j.jpsychores.2020.110343
3. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, Shohaimi S, Daneshkhah A, Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18:100. doi: 10.1186/s12960-020-00544-1
4. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
5. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:1–5. doi: 10.1016/j.bbi.2020.05.026
6. Carmassi C, Foghi C, Dell'Oste V, Cordone A, Bertelloni CA, Bui E, Dell'Osso L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. (2020) 292:113312. doi: 10.1016/j.psychres.2020.113312
7. Aronsson G, Theorell T, Grape T, Hammarström A, Hogstedt C, Marteinsdottir I, Skoog I, Träskman-Bendz L, Hall C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health. (2017) 17:264. doi: 10.1186/s12889-017-4153-7
8. Madsen IEH, Nyberg ST, Hanson LLM, Ferrie JE, Ahola K, Alfredsson L, Batty GD, Bjorner JB, Borritz M, Burr H, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med. (2017) 47:1342–1356. doi: 10.1017/S003329171600355X
9. Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, Zhuang Q. Psychological impacts and coping strategies of front-line medical staff during COVID-19 outbreak in Hunan, China. Med Sci Monit. (2020) 26:1–16. doi: 10.12659/msm.924171
10. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. (2020) 369:m1642. doi: 10.1136/bmj.m1642
11. Mol MMC van, Kompanje EJO, Benoit DD, Bakker J, Nijkamp MD. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS ONE. (2015) 10:e0136955. doi: 10.1371/journal.pone.0136955
12. Pereira SM, Teixeira CM, Carvalho AS, Hernández-Marrero P, InPalIn. Compared to palliative care, working in intensive care more than doubles the chances of burnout: results from a nationwide comparative study. PLoS ONE. (2016) 11:e0162340. doi: 10.1371/journal.pone.0162340
13. Crickmore R. A review of stress in the intensive care unit. Intensive Care Nurs. (1987) 3:19–27. doi: 10.1016/0266-612X(87)90006-X
14. Elshaer NSM, Moustafa MSA, Aiad MW, Ramadan MIE. Job stress and burnout syndrome among critical care healthcare workers. Alexandria J Med. (2018) 54:273–7. doi: 10.1016/j.ajme.2017.06.004
15. Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. (2007) 13:482–8. doi: 10.1097/MCC.0b013e3282efd28a
16. Kwiatosz-Muc M, Fijałkowska-Nestorowicz A, Fijałkowska M, Aftyka A, Kowalczyk M. Stress prevalence and stressors among anaesthesiology and intensive care unit workers: a multicentre survey study. Aust Crit Care. (2018) 31:391–5. doi: 10.1016/j.aucc.2017.11.001
17. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 366:1–14. doi: 10.1016/S2215-0366(20)30168-1
18. Williams R, Kemp V. Principles for designing and delivering psychosocial and mental healthcare. BMJ Mil Health. (2020) 166:105–10. doi: 10.1136/jramc-2017-000880
19. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, He L, Sheng C, Cai Y, Li X, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X
20. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. (2020) 368:m1211. doi: 10.1136/bmj.m1211
21. Ripp J, Peccoralo L, Charney D. Attending to the emotional well-being of the health care workforce in a New York city health system during the covid-19 pandemic. Acad Med. (2020) 95:1–1. doi: 10.1097/ACM.0000000000003414
22. Region Stockholm. Krislägesavtalet aktiveras i Region Stockholm. Available online at: https://www.sll.se/nyheter-stockholms-lans-landsting/2020/04/krislagesavtalet-aktiveras-i-region-stockholm/ (accessed July 9, 2021).
23. Wilson K, Bell C, Wilson L, Witteman H. Agile research to complement agile development: a proposal for an mHealth research lifecycle. Digital Med. (2018) 1:46. doi: 10.1038/s41746-018-0053-1
24. Albott CS, Wozniak JR, McGlinch BP, Wall MH, Gold BS, Vinogradov S. Battle buddies: rapid deployment of a psychological resilience intervention for healthcare workers during the Covid-19 pandemic. Anesth Analg. (2020) 131:43–54. doi: 10.1213/ANE.0000000000004912
25. Maben J, Bridges J. Covid-19: supporting nurses' psychological and mental health. J Clin Nurs. (2020) 29:2742–50. doi: 10.1111/jocn.15307
26. Wu AW, Connors C, Everly Jr. GS. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. (2020) 172:8–10. doi: 10.7326/M20-1236
27. Tetrick LE, Winslow CJ. Workplace stress management interventions and health promotion. Ann Rev Organ Psychol Organ Behav. (2015) 2:583–603. doi: 10.1146/annurev-orgpsych-032414-111341
28. Hayes SC, Barnes-Holmes D, Wilson KG. Contextual behavioral science: creating a science more adequate to the challenge of the human condition. J Context Behav Sci. (2012) 1:1–16. doi: 10.1016/j.jcbs.2012.09.004
29. Geurts SA, Sonnentag S. Recovery as an explanatory mechanism in the relation between acute stress reactions and chronic health impairment. Scand J Work Environ Health. (2006) 32:482–92. doi: 10.5271/sjweh.1053
30. Bakker AB, Demerouti E, Sanz-Vergel AI. Burnout and work engagement: the JD–R approach. Ann Rev Organ Psychol Organ Behav. (2014) 1:389–411. doi: 10.1146/annurev-orgpsych-031413-091235
31. World Health Organization. (2020). Mental Health and Psychosocial Considerations During COVID-19 Outbreak. Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1 (accessed May 25, 2021).
32. Sturgeon J, Zautra A. Psychological resilience, pain catastrophizing, and positive emotions: perspectives on comprehensive modeling of individual pain adaptation. Curr Pain Headache Rep. (2013) 17:317. doi: 10.1007/s11916-012-0317-4
33. Yu F, Raphael D, Mackay L, Smith M, King A. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud. (2019) 93:129–40. doi: 10.1016/j.ijnurstu.2019.02.014
34. Mealer M, Jones J, Moss M. A qualitative study of resilience and posttraumatic stress disorder in United States ICU nurses. Intensive Care Med. (2012) 38:1445–51. doi: 10.1007/s00134-012-2600-6
35. Ramnero J, Törneke N. The ABCs of Human Behavior: Behavioral Principles for the Practicing Clinician. Oakland, CA: New Harbinger Publications (2008).
36. Gentili C, Rickardsson J, Zetterqvist V, Simons LE, Lekander M, Wicksell RK. Psychological flexibility as a resilience factor in individuals with chronic pain. Front Psychol. (2019) 10:2016. doi: 10.3389/fpsyg.2019.02016
37. Appelbom S, Berhardtz R, Bujacz A. Risk för psykisk ohälsa och behov av psykologiska stödinsatser i samband med covid-19-pandemin: Teknisk rapport. Karolinska Institutet (2020).
38. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
39. Fukuti P, Uchôa CLM, Mazzoco MF, Corchs F, Kamitsuji CS, Rossi LD, et al. How institutions can protect the mental health and psychosocial well-being of their healthcare workers in the current COVID-19 pandemic. Clinics. (2020) 75:e1963. doi: 10.6061/clinics/2020/e1963
40. Gonzalez A, Cervoni C, Lochner M, Marangio J, Stanley C, Marriott S. Supporting health care workers during the COVID-19 pandemic: mental health support initiatives and lessons learned from an academic medical center. Psychol Trauma Theory Res Pract Policy. (2020) 12:S168–70. doi: 10.1037/tra0000893
41. Jiang X, Deng L, Zhu Y, Ji H, Tao L, Liu L, Yang D, Ji W. Psychological crisis intervention during the outbreak period of new coronavirus pneumonia from experience in Shanghai. Psychiatry Res. (2020) 286:112903. doi: 10.1016/j.psychres.2020.112903
42. Blake H, Yildirim M, Wood B, Knowles S, Mancini H, Coyne E, Cooper J. COVID-well: evaluation of the implementation of supported wellbeing centres for hospital employees during the COVID-19 Pandemic. Int J Environ Res Public Health. (2020) 17:9401. doi: 10.3390/ijerph17249401
43. Zgueb Y, Bourgou S, Neffeti A, Amamou B, Masmoudi J, Chebbi H, et al. Psychological crisis intervention response to the COVID 19 pandemic: a Tunisian centralised protocol. Psychiatry Res. (2020) 289:113042. doi: 10.1016/j.psychres.2020.113042
44. Juan NVS, Aceituno D, Djellouli N, Sumray K, Regenold N, Syversen A, et al. Mental health and well-being of healthcare workers during the COVID-19 pandemic in the UK: contrasting guidelines with experiences in practice. BJPsych Open. (2021) 7:e15. doi: 10.1192/bjo.2020.148
45. Woerkom M van, Bakker AB, Leiter MP. Positive psychology interventions in organizations. J Occup Organ Psychol. (2021) 94:221–9. doi: 10.1111/joop.12350
46. von Thiele Schwarz U, Nielsen K, Edwards K, Hasson H, Ipsen C, Savage C, et al. How to design, implement and evaluate organizational interventions for maximum impact: the Sigtuna Principles. Eur J Work Organ Psychol. (2021) 30:415–27. doi: 10.1080/1359432X.2020.1803960
47. Drury J, Carter H, Ntontis E, Guven ST. Public behaviour in response to the COVID-19 pandemic: understanding the role of group processes. BJPsych Open. (2021) 7:e11. doi: 10.1192/bjo.2020.139
48. Holmes E, Västfjäll D. Beteende och psykisk hälsa ett år in i Covid-19-pandemin—insikter från beteendevetenskap. Vetenskapsakademiens expertgrupp om Codid-19. (2021).
49. Somville FJ, De Gucht V, Maes S. The impact of occupational hazards and traumatic events among Belgian emergency physicians. Scand J Trauma Resusc Emerg Med. (2016) 24:59. doi: 10.1186/s13049-016-0249-9
Keywords: psychological support, implementation, process evaluation, COVID-19, healthcare workers, intensive care
Citation: Appelbom S, Bujacz A, Finnes A, Ahlbeck K, Bromberg F, Holmberg J, Larsson L, Olgren B, Wanecek M, Wetterborg D and Wicksell R (2021) The Rapid Implementation of a Psychological Support Model for Frontline Healthcare Workers During the COVID-19 Pandemic: A Case Study and Process Evaluation. Front. Psychiatry 12:713251. doi: 10.3389/fpsyt.2021.713251
Received: 22 May 2021; Accepted: 30 July 2021;
Published: 03 September 2021.
Edited by:
Michael Grady Wheaton, Columbia University, United StatesCopyright © 2021 Appelbom, Bujacz, Finnes, Ahlbeck, Bromberg, Holmberg, Larsson, Olgren, Wanecek, Wetterborg and Wicksell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aleksandra Bujacz, YWxla3NhbmRyYS5idWphY3pAa2kuc2U=
†These authors share first authorship
 Sophia Appelbom
Sophia Appelbom Aleksandra Bujacz
Aleksandra Bujacz Anna Finnes2
Anna Finnes2 Johan Holmberg
Johan Holmberg Birgitta Olgren
Birgitta Olgren Rikard Wicksell
Rikard Wicksell