- 1School of Psychological Science, University of Western Australia, Perth, WA, Australia
- 2School of Psychology, University of Santiago, Santiago, Chile
- 3School of Psychology, Curtin University, Perth, WA, Australia
Alexithymia is a trait composed of difficulties identifying feelings (DIF), difficulties describing feelings (DDF), and externally orientated thinking (EOT). It is an important transdiagnostic risk factor for psychosomatic disorders and other types of emotion-based psychopathologies, and can reduce the efficacy of some treatment approaches. Alexithymia assessments are therefore important in psychiatric and research settings. The Perth Alexithymia Questionnaire (PAQ) was recently developed to enable more comprehensive alexithymia assessments, however, its psychometric properties need further examination and it is so far only available in English. In this study, we sought to address this by translating the PAQ into Spanish and testing its psychometric properties in an adult sample from Chile (N = 370). Confirmatory factor analyses found the PAQ to have a theoretically congruent factor structure, supporting the contemporary status of alexithymia as a multifaceted construct and the PAQ's capacity to assess the DIF, DDF, and EOT facets of alexithymia across negative and positive emotions. All subscale and composite scores had high internal consistency reliability, and demonstrated good concurrent and discriminant validity. The PAQ therefore appears to provide a robust and detailed alexithymia profile. This Spanish version should help to enable more comprehensive cross-cultural research into alexithymia and its role in and psychological disorders.
Introduction
Alexithymia is a trait composed of three facets: difficulty identifying one's own feelings (DIF), difficulty describing feelings (DDF), and an externally orientated thinking style (EOT) whereby one rarely focuses attention on their internal emotional states (1–4). People with high alexithymia experience their emotions in a more diffuse or undifferentiated manner, such as being unsure if an unpleasant feeling is sadness, anger, or fear (5). Alexithymia was first coined by American psychiatrists in the 1970s, who often observed high levels of the trait in treatment resistant patients with psychosomatic disorders (4, 6). The relevance of the valid assessment of alexithymia in psychiatry in general and psychosomatic disorders in particular, becomes apparent upon inspection of the prevalence of alexithymia in these domains. Alexithymia has been found to be overrepresented in numerous psychiatric disorders, including substance abuse (7), alcohol dependence (8), depression (9), anxiety disorders (10), addictive disorders in general (11), and in general psychiatric samples with varied diagnoses (12). Similarly, alexithymia has been found to be present in numerous medical presentations with associations with psychosomatic conditions, including gastrointestinal problems (13), dermatological issues (14), and cardiovascular complications (15). Importantly, the presence of high alexithymia has been found to impair treatment effectiveness if unaccounted for [e.g., (16)]. Therefore, the role of alexithymia in clinical practice appears to warrant its close examination from both the intervention and assessment points of view. Assessing alexithymia should thus be relevant to clinicians working with psychiatric patients and/or patients with medical illnesses found to have associations with psychosomatic conditions.
Since the 1990s, researchers and practitioners have most frequently used the 20-item Toronto Alexithymia Scale [TAS-20; (17)] to assess alexithymia, a strength of which is its availability in 24 languages. However, researchers and practitioners are increasingly wanting to examine alexithymia at the facet (subscale) level as well as conduct valence-specific analyses [i.e., examine DIF, DDF, and EOT across both negative and positive emotions; (18–20)]. This parallels trends in the broader psychological assessment field, where contemporary assessment tools are increasingly providing valence-specific scores and emphasizing facet level profiles for other multidimensional emotional constructs [e.g., emotion regulation, emotional reactivity, beliefs about emotions; (21–25)]. However, the TAS-20 was not designed with these functions in mind [it was designed only to provide a total scale score as a measure of overall alexithymia; see (26)] and psychometric studies have consistently noted low reliability (α < 0.70) and factor loading problems with its EOT items [e.g., (27–33)]. Furthermore, recent data have suggested that a significant portion of the variance in the TAS-20 DIF items reflects people's current levels of negative affect rather than their underlying levels of the alexithymia trait [i.e., discriminant validity problems; see (34–36, 50)].
To try to enable more detailed facet-level and valence-specific analyses of alexithymia, Preece et al. (37) recently developed the Perth Alexithymia Questionnaire (PAQ). The PAQ is a 24-item self-report measure designed to assess all three components of the construct (DIF, DDF, EOT). For the DIF and DDF components, valence-specific scores can be derived for processing negative and positive emotions. Thus, the PAQ has five intended subscales: Negative-Difficulty identifying feelings (N-DIF; 4 items, e.g., “When I'm feeling bad, I can't tell whether I'm sad, angry, or scared”), Positive-Difficulty identifying feelings (P-DIF; 4 items, e.g., “When I'm feeling good, I can't make sense of those feelings”), Negative-Difficulty describing feelings (N-DDF; 4 items, e.g., “When I'm feeling bad, if I try to describe how I'm feeling I don't know what to say”), Positive-Difficulty describing feelings (P-DDF; 4 items, e.g., “When I'm feeling good, I can't talk about those feelings in much depth or detail”), and General-Externally orientated thinking (G-EOT; 8 items, e.g., “I prefer to focus on things I can actually see or touch, rather than my emotions”). These subscales can also be combined into several composite scores, including summing all items into a total scale score as an overall marker of alexithymia. All PAQ items are answered on a 7-point Likert scale, with higher scores indicating higher levels of alexithymia. The scale takes approximately between 3 and 5 min to complete, therefore it can be used in a non-intrusive manner in any clinical setting.
The psychometric properties of the PAQ have so far been examined in four published studies (34, 37–39), all using the original English version with Australian or United States adults. The PAQ has displayed a theoretically congruent structure, consisting of five narrow factors (corresponding to the five intended subscales), with support also found for a bifactor model with an additional general alexithymia factor loading on all items (37)1. All subscale and composite scores in these studies had high internal consistency, and good concurrent and discriminant validity against measures of depression and anxiety symptoms and emotion regulation. Supporting the potential value of valence-specific assessment, participants reported more difficulties identifying and describing their negative emotions as compared to positive emotions, and the PAQ displayed better reliability coefficients and factorial validity than the TAS-20 (34, 38, 39).
Whilst these results are promising, there is a need for further validation studies to confirm the PAQ's utility. The PAQ is presently also only available in English, which limits cross-cultural applications. To help address these gaps, in this study we translated the PAQ into Spanish and examined its psychometric properties in a Spanish-speaking sample. Options for alexithymia assessments in Spanish-speaking populations are presently limited [e.g., a recent study of the Spanish TAS-20 found the aforementioned factorial validity and reliability problems, with the authors recommending that the scale “needs improvement (theoretical and empirical) to ensure optimal indices”; (28), p.1; see also (42)]. Thus, there is a pressing need to develop more optimized measures for alexithymia assessments in Spanish-speaking populations.
Method
Participants, Procedure, and Materials
Ethics approval for this study was granted by the Human Research Ethics Committee from the University of Santiago. All participants provided informed consent. The first author, who is a Spanish-English bilingual psychologist with expertise in scale development, translated the English PAQ items into Spanish. This Spanish translation was then sent to the second and third authors (both Spanish-English bilingual psychologists) who suggested minor modifications. This version was back-translated into English, and checked by the first author and last author (an English-speaking psychologist with expertise in scale development). The final version of the Spanish PAQ (see Supplementary Materials) was administered to 370 Spanish speaking adults (63.2% female) in Chile. Their average age was 28.14 years (SD = 11.97, range = 18–66). The sample was 55% undergraduate students (from the School of Humanities at the University of Santiago), 25% professionals, and 20% technical workers or homemakers. 79% of the sample were single, 16% married, and 5% divorced or separated. Less than 6% of the sample reported having a psychological disorder, which included depression (n = 11), anxiety (n = 4), both anxiety and depression (n = 2), bipolar disorder (n = 2), ADHD (n = 1), and Asperger syndrome (n = 1).
As a concurrent and discriminant validity marker, participants also completed a measure of emotional reactivity, the Perth Emotional Reactivity Scale [PERS; (43)]2. The PERS is a 30-item self-report questionnaire that assesses the typical ease of activation, intensity, and duration of people's emotions, and does so for negative and positive emotions separately. Higher scores indicate higher levels of emotional reactivity. The PERS has demonstrated good validity and reliability [e.g., (43)].
Analytic Strategy
Confirmatory factor analyses (CFA) were conducted using AMOS 25. All other analyses used SPSS 25.
Factorial Validity
We examined the factor structure of the PAQ using a series of CFAs (maximum likelihood estimation based on a Pearson covariance matrix), following the same statistical and model testing procedure as Preece et al.'s (37) original PAQ development study3. We examined six theoretically informed models of increasing complexity (see Figure 1). As comparative baselines, first we tested several simpler models: a one-factor model, where all items loaded on single factor; a two-factor model, that only distinguished between the attention (EOT) and appraisal (DIF, DDF) stages of emotion processing; a three-factor non-valenced model, that distinguished between the DIF, DDF and EOT facets of alexithymia, but did not distinguish between negatively and positively valenced items; and a three-factor valenced model, that combined the DIF and DDF items together, but distinguished between the processing of negative (N-DIF/N-DDF) and positive emotions (P-DIF/P-DDF). Then, we tested two models reflecting the intended factor structure of the PAQ: a five-factor model, comprised of the five intended subscales as correlated factors (N-DIF, P-DIF, N-DDF, P-DDF, G-EOT), and a bifactor version of this model, where a general factor was also included loading on all the items. The bifactor model was the best solution in Preece et al.'s (37) original development study, so we expected it to be the best here.
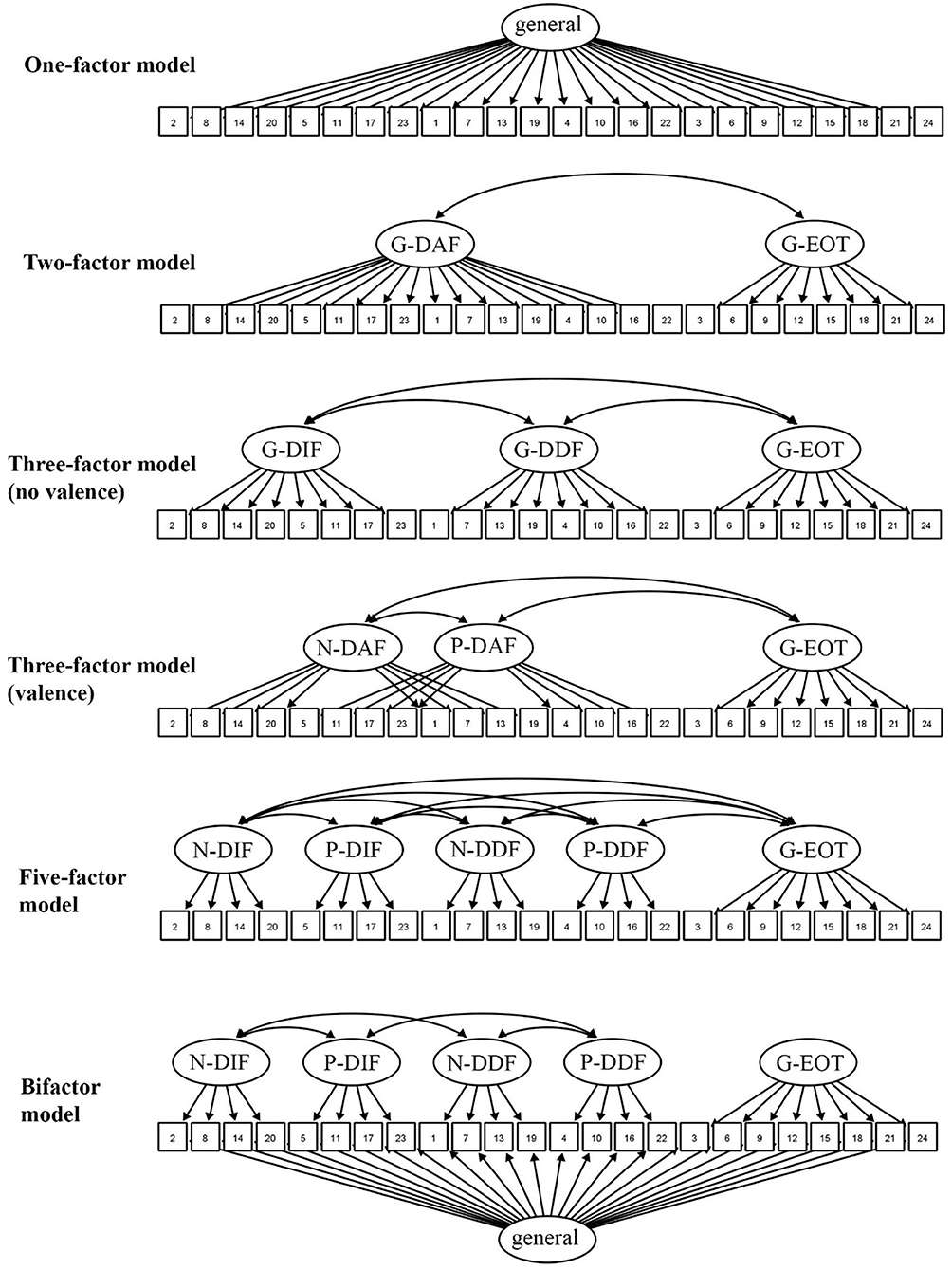
Figure 1. The examined confirmatory factor analysis models for the Perth Alexithymia Questionnaire. Ellipses = latent factors, squares = item numbers. Each item had an associated error term.
The goodness-of-fit of each model was judged based on four fit index values: CFI, TLI, RMSEA, and SRMR. CFI and TLI values around ≥0.90 indicate acceptable fit. RMSEA and SRMR values around ≤ 0.08 are acceptable. AIC values were also used to directly compare each model, with lower AIC values indicating a better fit (44, 46). Factor loadings ≥0.40 were judged as meaningful loadings (47).
Internal Consistency
Cronbach's α reliability coefficients were calculated for all PAQ subscale and composite scores. Coefficients ≥0.70 were viewed as acceptable, ≥0.80 as good, and ≥0.90 as excellent (48).
Concurrent and Discriminant Validity
We calculated Pearson correlations between PAQ and PERS scores. People's emotion regulation attempts are typically focused on up-regulating negative emotions and down-regulating positive emotions, and because alexithymia impairs emotion regulation abilities people with high alexithymia should be less successful at achieving these regulation goals (49). Alexithymia should therefore be associated with an emotional reactivity profile characterized by high negative reactivity (i.e., more easily activated, more intense, and more prolonged negative emotions) and low positive reactivity (49). Alexithymia measures should, however, still assess a construct that is separable from emotional reactivity [i.e., should demonstrate discriminant validity in terms of not being a measure of negative or positive affect; (50)]. We examined this discriminant validity by conducting a second-order exploratory factor analysis (EFA; principal axis factoring with direct oblimin rotation) of the PAQ and PERS subscale scores together, to see whether their subscales successfully extracted onto different factors.
Results and Discussion
Factorial Validity
Our CFA results replicated the previous findings of Preece et al. with the English PAQ. Those models which included the five intended subscales as factors (i.e., the five-factor model and the bifactor model) were the best solutions. Fit index values, factor loadings, and factor intercorrelations are provided in Tables 1, 2, and Supplementary Table 1, respectively. The simpler models that did not account for valence had poor fit (e.g., CFI <0.90). In contrast, the five-factor model fit well according to all examined fit indexes [χ2 = 702.485 (p < 0.001), CFI = 0.921, TLI = 0.910, RMSEA = 0.072 (0.066–0.078), SRMR = 0.0483, AIC = 818.785], thus highlighting that it was useful to distinguish between the DIF, DDF and EOT components of alexithymia, and distinguish between the processing of negative and positive emotions for DIF and DDF. All items in the five-factor model loaded well on their intended factor (factor loadings = 0.60–0.89) and these five factors were positively correlated (estimated rs = 0.47–0.91). The addition of the general factor in the bifactor model improved model fit further [χ2 = 636.515 (p < 0.001), CFI = 0.929, TLI = 0.913, RMSEA = 0.071 (0.064–0.077), SRMR = 0.0522, AIC = 788.515], and item variance was split well between the five narrow factors and the general factor (see Table 2). Overall, our CFA results were therefore consistent with the theoretical status of alexithymia as a coherent multidimensional construct (1, 4, 41), and supported the intended subscale and composite score structure of the PAQ. Taken together with previous factor analytic findings in English-speaking samples, our results therefore support the consistency of the structure of alexithymia across these cultural groups.
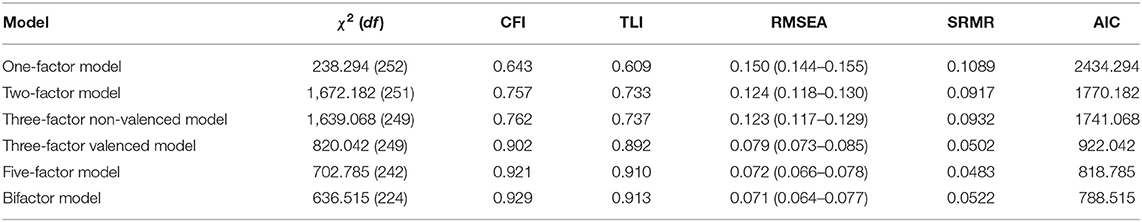
Table 1. Goodness-of-fit index values for the different confirmatory factor analysis models of the Perth alexithymia questionnaire.
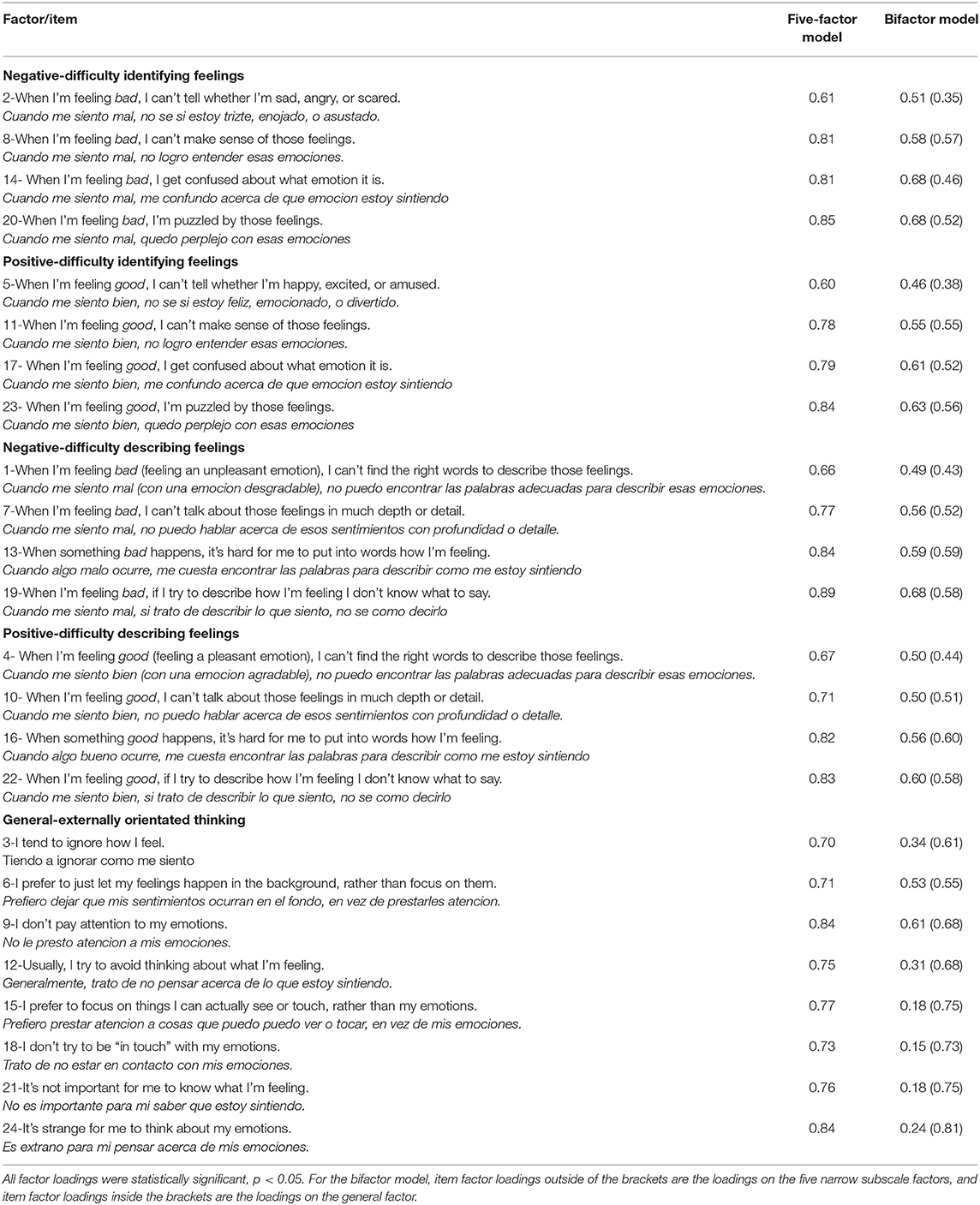
Table 2. Standardized factor loadings from confirmatory factor analyses of the Perth alexithymia questionnaire (five-factor model and bifactor model).
Descriptive Statistics, Reliability, and Concurrent/Discriminant Validity
Descriptive statistics and Cronbach's α coefficients are provided in Table 3. All PAQ subscales and composite scores had good to excellent levels of reliability (α = 0.83–0.94). Consistent with previous findings (37–39), participants reported significantly more difficulties appraising their negative emotions compared to their positive emotions [t(369) = 9.950, p < 0.001, d = 0.52], thus reinforcing the utility of valence-specific measurement.

Table 3. Descriptive statistics and Cronbach's α reliability coefficients for the Perth alexithymia questionnaire.
Our results also supported the concurrent and discriminant validity of the PAQ. In line with theoretical expectations (49), alexithymia was associated with an emotional reactivity profile comprised of high negative reactivity and low positive reactivity. High PAQ total scores were significantly associated (p < 0.01) with more easily activated (r = 0.30), more intense (r = 0.20) and more persistent (r = 0.35) negative emotions, and less easily activated (r = −0.16), less intense (r = −0.18) and less persistent (r = −0.23) positive emotions. The full correlation matrix is provided in Supplementary Table 2.
The PAQ and PERS were, moreover, measuring separate constructs statistically. Our second-order EFA of the PAQ and PERS subscales extracted three correlated factors (general alexithymia, positive reactivity, negative reactivity), with all the PAQ subscales loading cleanly on the general alexithymia factor (loadings = 0.70–0.81) and not loading on either of the emotional reactivity factors (loadings = −0.19–0.09; see Supplementary Table 3). As such, whilst previous work has highlighted that TAS-20 scores may be confounded by respondents' current levels of negative affect [e.g., (50)], this issue was not present for the PAQ in our data-set [see also (34, 37)].
Conclusions, Implications, and Limitations
Overall, our results suggest that the PAQ has strong psychometric properties and can provide a robust alexithymia profile at the subscale and composite score level. Our Spanish language version appears to function similarly to the original English version in this respect, and so may be helpful in enabling cross-cultural studies [e.g., (30)] and more detailed assessments of alexithymia in Spanish-speaking populations. In psychiatric contexts, high PAQ scores could indicate cases where treatment approaches need to account for alexithymic deficits, or directly target alexithymia as part of the treatment approach [for a discussion of alexithymia treatment approaches, see (1, 41)]. A limitation of our study, however, is that our sample was from the community, so we cannot comment on psychometric performance in specialized psychiatric populations. Previous studies have found the alexithymia construct to manifest similarly across community and psychiatric samples [e.g., (17)], but it will be important for future work to test the generalizability of our PAQ findings. Similarly, future work would be beneficial to examine the test-retest reliability of the PAQ, and its concurrent validity against observer-rated, behavioral, and lab-based markers of emotion processing and other emotional constructs [e.g., (3)].
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Research Committee, University of Santiago, Chile. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
RB translated the questionnaire. RB and DP contributed the majority of the manuscript writing. DP completed the statistical analyses. AF and CB recruited and administered the questionnaire to the sample, and helped refine the manuscript and translation. All authors have approved the final article and agreed to the authorship order.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.710398/full#supplementary-material
Footnotes
1. ^Bifactor models are a theoretically congruent representation for measures that “primarily reflect a strong common trait [i.e., alexithymia], but there is multidimensionality caused by well-defined clusters of items from diverse subdomains” [(40), p. 692]. This is the case for alexithymia, which authors conceptualize as a multidimensional construct with several subcomponents (1, 40, 41).
2. ^Some (n = 36) of the 370 participants had a small amount of missing data (i.e., data for 20% or less of the items were missing) for at least one of the administered questionnaires. In these cases, missing data were replaced using the expectation maximization method.
3. ^CFA was used because it is appropriate for hypothesis testing when there is a clear theoretical rationale to expect a certain factor structure (44). In the interest of comparability with previous research, the maximum likelihood estimation method was used, as it is the most commonly used estimation method in the alexithymia field [e.g., (17, 27)], and was used in the original CFA studies of the PAQ (34). All PAQ items were reasonably normally distributed in this data-set (average skew = 0.67, average kurtosis = −0.61), so we judged the maximum likelihood method to be appropriate (45).
References
1. Preece D, Becerra R, Allan A, Robinson K, Dandy J. Establishing the theoretical components of alexithymia via factor analysis: introduction and validation of the attention-appraisal model of alexithymia. Pers Individ Dif. (2017) 119:341–52. doi: 10.1016/j.paid.2017.08.003
2. Preece DA, Becerra R, Robinson K, Allan A, Boyes M, Chen W, et al. What is alexithymia? Using factor analysis to establish its latent structure and relationship with fantasizing and emotional reactivity. J Pers. (2020) 88:1162–76. doi: 10.1111/jopy.12563
3. Sekely A, Taylor GJ, Bagby RM. Developing a short version of the Toronto Structured Interview for Alexithymia using item response theory. Psychiatry Res. (2018) 266:218–27. doi: 10.1016/j.psychres.2018.03.002
4. Sifneos PE. The prevalence of 'alexithymic' characteristics in psychosomatic patients. Psychother Psychosom. (1973) 22:255–62. doi: 10.1159/000286529
5. Lane RD, Schwartz GE. Levels of emotional awareness: a cognitive-developmental theory and its application to psychopathology. Am J Psychiatry. (1987) 144:133–43. doi: 10.1176/ajp.144.2.133
6. Nemiah JC, Sifneos PE. Psychosomatic illness: a problem in communication. Psychother Psychosom. (1970) 18:154–60. doi: 10.1159/000286074
7. Palma-Álvarez RF, Ros-Cucurull E, Daigre C, Perea-Ortueta M, Serrano-Pérez P, Martínez-Luna N, et al. Alexithymia in patients with substance use disorders and its relationship with psychiatric comorbidities and health-related quality of life. Front Psychiatry. (2021) 12:659063. doi: 10.3389/fpsyt.2021.659063
8. Pombo S, Félix da Costa N, Ismail F, Cardoso JMN, Figueira ML. Alexithymia and alcohol dependence: Do different subtypes manifest different emotion regulations? Addict Res Theory. (2015) 23:187–95. doi: 10.3109/16066359.2014.949697
9. Celikel FC, Kose S, Erkorkmaz U, Sayar K, Cumurcu BE, Cloninger CR. Alexithymiaand temperament and character model of personality in patients with major depressive disorder. Compr Psychiatry. (2010) 51:64–70. doi: 10.1016/j.comppsych.2009.02.004
10. Frewen PA, Lanius RA, Dozois DJ, Neufeld RW, Pain C, Hopper JW, et al. Clinical and neural correlates of alexithymia in posttraumatic stress disorder. J AbnormalPsychol. (2008) 117:171–81. doi: 10.1037/0021-843X.117.1.171
11. Coriale G, Bilotta E, Leone L, Cosimi F, Porrari R, De Rosa F, et al. Avoidancecoping strategies, alexithymia and alcohol abuse: a mediation analysis. Addict Behav. (2012) 37:1224–9. doi: 10.1016/j.addbeh.2012.05.018
12. McGillivray L, Becerra R, Harms C. Prevalence and demographic correlates of alexithymia: a comparison between Australian psychiatric and community samples. J Clin Psychol. (2017) 73:76–87. doi: 10.1002/jclp.22314
13. Kano M, Endo Y, Fukudo S. Association between alexithymia and functional gastrointestinal disorders. Front Psychol. (2018) 9:599. doi: 10.3389/fpsyg.2018.00599
14. Picardi A, Abeni D, Melchi CF, Puddu P, Pasquini P. Psychiatric morbidity in dermatological outpatients: an issue to be recognized. Br J Dermatol. (2000) 143:983–91. doi: 10.1046/j.1365-2133.2000.03831.x
15. Vadini F, Sozio F, Madeddu G, De Socio G, Maggi P, Nunnari G, et al. Alexithymia predicts carotid atherosclerosis, vascular events, and all-cause mortality in human immunodeficiency virus-infected patients: an Italian multisite prospective cohort study. Open Forum Infect Dis. (2019) 6:ofz331. doi: 10.1093/ofid/ofz331
16. Leweke F, Bausch S, Leichsenring F, Walter B, Stingl M. Alexithymia as a predictor of outcome of psychodynamically oriented inpatient treatment. Psychother Res. (2009) 19:323–31. doi: 10.1080/10503300902870554
17. Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto alexithymia scale-I. Item selection and cross-validation of the factor structure. J Psychosom Res. (1994) 38:23–32. doi: 10.1016/0022-3999(94)90005-1
18. Leweke F, Leichsenring F, Kruse J, Hermes S. Is alexithymia associated with specific mental disorders. Psychopathology. (2012) 45:22–8. doi: 10.1159/000325170
19. van der Velde J, Servaas MN, Goerlich KS, Bruggeman R, Horton P, Costafreda SG, et al. Neural correlates of alexithymia: A meta-analysis of emotion processing studies. Neurosci Biobehav Rev. (2013) 37:1774–85. doi: 10.1016/j.neubiorev.2013.07.008
20. Demers LA, Schreiner MW, Hunt RH, Mueller BA, Klimes-Dougan B, Thomas K, et al. Alexithymia is associated with neural reactivity to masked emotional faces in adolescents who self-harm. J Affect Disord. (2019) 249:253–61. doi: 10.1016/j.jad.2019.02.038
21. Becerra R, Preece DA, Gross JJ. Assessing beliefs about emotions: development and validation of the Emotion Beliefs Questionnaire. PLoS ONE. (2020) 15:e0231395. doi: 10.1371/journal.pone.0231395
22. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
23. Preece DA, Becerra R, Robinson K, Dandy J, Allan A. Measuring emotion regulation ability across negative and positive emotions: the perth emotion regulation competency inventory (PERCI). Pers Individ Dif. (2018) 135:229–41. doi: 10.1016/j.paid.2018.07.025
24. Ripper CA, Boyes ME, Clarke PJ, Hasking PA. Emotional reactivity, intensity, and perseveration: independent dimensions of trait affect and associations with depression, anxiety, and stress symptoms. Pers Individ Dif. (2018) 121:93–9. doi: 10.1016/j.paid.2017.09.032
25. Weiss NH, Gratz KL, Lavender JM. Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: the DERS-Positive. Behav Modif. (2015) 39:431–53. doi: 10.1177/0145445514566504
26. Bagby RM, Taylor GJ, Quilty LC, Parker JD. Reexamining the factor structure of the 20-item Toronto alexithymia scale: commentary on gignac, palmer, and stough. J Pers Assess. (2008) 89:258–64. doi: 10.1080/00223890701629771
27. Gignac GE, Palmer BR, Stough C. A confirmatory factor analytic investigation of the TAS-20: corroboration of a five-factor model and suggestions for improvement. J Pers Assess. (2007) 89:247–57. doi: 10.1080/00223890701629730
28. González-Arias M, Martínez-Molina A, Galdames S, Urzúa A. Psychometric properties of the 20-item Toronto Alexithymia Scale in the Chilean population. Front Psychol. (2018) 9:963. doi: 10.3389/fpsyg.2018.00963
29. Kooiman CG, Spinhoven P, Trijsburg RW. The assessment of alexithymia: a critical review of the literature and a psychometric study of the Toronto Alexithymia Scale-20. J Psychosom Res. (2002) 53:1083–90. doi: 10.1016/S0022-3999(02)00348-3
30. Taylor GJ, Bagby RM, Parker JD. The 20-item Toronto alexithymia scale: IV. Reliability and factorial validity in different languages and cultures. J Psychosom Res. (2003) 55:277–83. doi: 10.1016/S0022-3999(02)00601-3
31. Preece D, Becerra R, Robinson K, Dandy J. Assessing alexithymia: psychometric properties and factorial invariance of the 20-Item Toronto alexithymia scale in nonclinical and psychiatric samples. J Psychopathol Behav Assess. (2018) 40:276–87. doi: 10.1007/s10862-017-9634-6
32. Kroner DG, Forth AE. The Toronto alexithymia scale with incarcerated offenders. Pers Individ Dif. (1995) 19:625–34. doi: 10.1016/0191-8869(95)00116-N
33. Parker JD, Austin EJ, Hogan MJ, Wood LM, Bond BJ. Alexithymia and academic success: examining the transition from high school to university. Pers Individ Dif. (2005) 38:1257–67. doi: 10.1016/j.paid.2004.08.008
34. Preece DA, Becerra R, Boyes ME, Northcott C, McGillivray L, Hasking PA. Do self-report measures of alexithymia measure alexithymia or general psychological distress? A factor analytic examination across five samples. Pers Indiv Diff. (2020) 155:1–8. doi: 10.1016/j.paid.2019.109721
35. Marchesi C, Brusamonti E, Maggini C. Are alexithymia, depression, and anxiety distinct constructs in affective disorders? J Psychosom Res. (2000) 49:43–9. doi: 10.1016/S0022-3999(00)00084-2
36. Marchesi C, Ossola P, Tonna M, De Panfilis C. The TAS-20 more likely measures negative affects rather than alexithymia itself in patients with major depression, panic disorder, eating disorders and substance use disorders. Compr Psychiatry. (2014) 55:972–8. doi: 10.1016/j.comppsych.2013.12.008
37. Preece D, Becerra R, Robinson K, Dandy J, Allan A. The psychometric assessment of alexithymia: development and validation of the Perth Alexithymia Questionnaire. Pers Individ Dif. (2018) 132:32–44. doi: 10.1016/j.paid.2018.05.011
38. Greene D, Hasking P, Boyes M, Preece D. Measurement invariance of two measures of alexithymia in students who do and who do not engage in non-suicidal self-injury and risky drinking. J Psychopathol Behav Assess. (2020) 42:808–25. doi: 10.1007/s10862-020-09806-7
39. Preece DA, Becerra R, Allan A, Robinson K, Chen W, Hasking P, et al. Assessing alexithymia: psychometric properties of the Perth Alexithymia Questionnaire and 20-item Toronto Alexithymia Scale in United States Adults. Pers Indiv Diff. (2020) 166:110138. doi: 10.1016/j.paid.2020.110138
40. Reise SP. The rediscovery of bifactor measurement models. Multivariate Behav Res. (2012) 47:667–96. doi: 10.1080/00273171.2012.715555
41. Taylor GJ, Bagby RM, Parker JD. Disorders of Affect Regulation: Alexithymia in Medical and Psychiatric Illness. Cambridge: Cambridge University Press (1999).
42. Loiselle CG, Cossette S. Cross-cultural validation of the Toronto Alexithymia Scale (TAS-20) in US and Peruvian populations. Transcult Psychiatry. (2001) 38:348–62. doi: 10.1177/136346150103800305
43. Becerra R, Preece D, Campitelli G, Scott-Pillow G. The assessment of emotional reactivity across negative and positive emotions: development and validation of the Perth Emotional Reactivity Scale (PERS). Assessment. (2019) 26:867–79. doi: 10.1177/1073191117694455
44. Byrne BM. Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming. New York, NY: Routledge (2016).
45. Beauducel A, Herzberg PY. On the performance of maximum likelihoomeans and variance adjusted weighted least squares estimation in CFA. Struct Equat Model. (2006) 13:186–203. doi: 10.1207/s15328007sem1302_2
46. Marsh HW, Hau KT, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Struct Equat Model. (2004) 11:320–41. doi: 10.1207/s15328007sem1103_2
47. Stevens JP. Applied Multivariate Statistics for the Social Sciences. Hillsdale, NJ: Erlbaum (2002).
49. Gross JJ. Emotion regulation: conceptual and empirical foundations. In: Gross JJ, editor. Handbook of emotion regulation. New York, NY: Guilford Press (2014). p. 3–20.
Keywords: alexithymia, Perth alexithymia questionnaire, Spanish, factor structure, emotion
Citation: Becerra R, Baeza CG, Fernandez AM and Preece DA (2021) Assessing Alexithymia: Psychometric Properties of the Perth Alexithymia Questionnaire in a Spanish-Speaking Sample. Front. Psychiatry 12:710398. doi: 10.3389/fpsyt.2021.710398
Received: 16 May 2021; Accepted: 09 September 2021;
Published: 12 October 2021.
Edited by:
Laura Orsolini, Marche Polytechnic University, ItalyReviewed by:
Roberta Vecchiotti, Hermanas Hospitalarias, ItalyMiguel Angel Alvarez-Mon, University Clinic of Navarra, Spain
Copyright © 2021 Becerra, Baeza, Fernandez and Preece. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rodrigo Becerra, rodrigo.becerra@uwa.edu.au
 Rodrigo Becerra
Rodrigo Becerra Carmen Gloria Baeza
Carmen Gloria Baeza Ana Maria Fernandez
Ana Maria Fernandez David A. Preece
David A. Preece