
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 20 October 2021
Sec. Mood Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.709674
 Han Lin1†
Han Lin1† Mingxing Liu2†
Mingxing Liu2† Dongmei Zhong3†
Dongmei Zhong3† Ernest Hung Yu Ng4
Ernest Hung Yu Ng4 Jianping Liu5
Jianping Liu5 Juan Li1
Juan Li1 Yu Shi2
Yu Shi2 Chunren Zhang6
Chunren Zhang6 Xiaohui Wen1
Xiaohui Wen1 Zhefen Mai1
Zhefen Mai1 Miaoxian Ou2
Miaoxian Ou2 Hongxia Ma1*
Hongxia Ma1*Increasing evidence shows that polycystic ovary syndrome (PCOS) patients are particularly vulnerable to anxiety/depression-like behaviors. This study sought to determine the prevalence of anxiety/depression-like behaviors among women with PCOS and to identify factors associated with these behaviors. This study was a secondary analysis of three studies performed on Chinese women who were aged 18 to 40 and diagnosed with PCOS according to the modified Rotterdam criteria. We obtained 802 useable responses for the self-rating anxiety scale and 798 responses for the self-rating depression scale. The prevalence of anxiety-like and depression-like behaviors among women with PCOS was 26.1% (209/802) and 52.0% (415/798), respectively. Anxiety-like behaviors were associated with age, body image-related factors (including body mass index and waist-to-hip ratio), and hyperandrogenism-related factors (including free androgen index and hirsutism). Depression-like behaviors were associated with age, body image-related factors, hyperandrogenism-related factors, and metabolic factors (including fasting insulin, fasting plasma glucose, and homeostatic model assessment of insulin resistance). Body image-related factors and hyperandrogenism-related factors were related to both anxiety-like behaviors and depression-like behaviors in both infertile and fertile PCOS patients.
Polycystic ovary syndrome (PCOS) is a chronic gynecological endocrine and metabolic disease affecting about 6–10% of women of childbearing age worldwide (1). The etiology of PCOS mainly involves hormone imbalances that lead to irregular menstruation and to ovulation dysfunction (1). In addition to these symptoms, classic clinical symptoms of PCOS also include clinical or laboratory evidence of elevated androgens and polycystic ovarian morphology as shown by pelvic ultrasound (2). Compared to healthy women, women with PCOS are at greater risk for morbidities and complications in other systems, including diabetes, dyslipidemia, hypertension, obesity, metabolic syndrome, obstructive sleep apnea, pregnancy complications, endometrial cancer, and cardiovascular disease (3–8).
In addition to all of the long-term metabolic and endocrine outcomes, an increased prevalence of psychological disorders among women with PCOS has also been reported in some studies, including depression and anxiety (9–12). It has been reported in some studies that women with PCOS suffer from more mental stress than healthy women, with many of them reporting dissatisfaction with their body image or acne on their face or worry about their infertility (13, 14). These factors associated with PCOS make these women more vulnerable to feeling anxious and upset, but the specific causative factors, including sociological factors and molecular mechanisms, for these anxiety/depression-like behaviors in women with PCOS have not been fully elucidated.
The most common mental disorders studied in women with PCOS are anxiety and depression (15), and these usually result from changes in their body image as a result of their disease (including hirsutism, irregular menses, obesity, acne, and hair thinning) (16). The self-rating anxiety scale (SAS) and the self-rating depression scale (SDS) are commonly used for self-evaluation of the presence and severity of anxiety-like and depression-like behaviors (17–19).
In this study, we obtained a total of 802 SAS scores and 798 SDS scores after excluding those with a completion rate below 50% from the 828 women with PCOS in our three studies. By analyzing the relationship between SAS/SDS score and other baseline data, we have identified the most likely factors associated with anxiety-like and depression-like behaviors in these women.
This study was a retrospective secondary analysis of women with PCOS from three trials, including one prospective pilot trial and two randomized controlled trials. The study protocol has been described in The Effect of Acupuncture on Insulin Sensitivity Polycystic Ovary Syndrome (ClinicalTrials.gov NCT 02026323) (20), The Effect of Acupuncture on Insulin Sensitivity of Women with Polycystic Ovary Syndrome and Insulin Resistance: a Randomized Controlled Trial (ClinicalTrials.gov, NCT 02491333) (21), and The Effect of Acupuncture Pre-treatment Combined with Letrozole on Live Birth in Infertile Women with Polycystic Ovary Syndrome: a Randomized Controlled Trial (ClinicalTrials.gov NCT 02491320) (22). The ethics approvals were granted from the ethics committee of the First Affiliated Hospital of Guangzhou Medical University (ref. 2013039, ref. 2015010, ref. 2014018, respectively), as is shown in detail in Supplementary 1. These three trials were conducted in the Department of Traditional Chinese Medicine of the First Affiliated Hospital of Guangzhou Medical University, the Department of Gynecology of Xuzhou Maternity & Child Health Hospital, the Department of Traditional Chinese Medicine of Dalian Municipal Women and Children's Medical Center, the Department of Gynecology of Guangdong Women and Children's Hospital, and the Department of Traditional Chinese Medicine of Hexian Memorial Affiliated Hospital of Southern Medical University. The three studies involved a total of 828 Chinese women aged 18–40 years who met the PCOS diagnosis criteria listed, and in this study the included participants had also completed both the SDS and SAS.
Inclusion criteria:
1. Women aged between 18 and 40 years.
2. Body mass index (BMI) ≥ 18.5 kg/m2.
3. Diagnosis of PCOS as defined by the Rotterdam criteria (Supplementary 2).
4. Willingness to sign the consent form.
5. A completion rate above 50% for the SAS and SDS.
Exclusion criteria:
1. A completion rate below 50% for the SAS and SDS.
2. Other endocrine disorders, as shown in Supplementary 2.
3. Use of hormones or other medications, including Chinese herbal prescriptions, that might affect the outcome in the past 2 months.
4. Receiving acupuncture in the past 2 months.
5. Pregnancy within the past 6 weeks.
6. Abortion or having given birth within the past 6 weeks.
7. Breast feeding within the past 6 weeks.
8. Not willing to give written consent to participate.
9. Having a bariatric surgery procedure within the past 12 months or being in a period of acute weight loss.
10. Additional exclusion criteria as shown in Supplementary 2.
Both the SAS and SDS have 20 items, each of which is graded on a scale of 1–4. Adding all the scores of each question in the SAS or SDS gives a raw score with a minimum of 20 points and a maximum of 80 points, and this is then converted into a standard score. For the SAS, the standard score is equal to the raw score × 1.25 (rounded to the nearest whole number). In the general Chinese population an SAS standard score (SAS-SS) ≥50 is considered to be an indication of anxiety, with scores of 50–59 classified as mild, 60–69 classified as moderate, and ≥70 classified as severe (19). The standard score for the SDS (SDS-SS) is calculated the same as for the SAS-SS. For the general Chinese population, an SDS-SS ≥53 is regarded as a depression-like state, with scores of 53–62 classified as mild, 63–72 classified as moderate, and ≥73 classified as severe (19).
The clinical data included BMI, waist circumference (WC), waist-to-hip Ratio (WHR), acne, testosterone (T), hirsutism (Ferriman–Gallwey Score), sex hormone-binding globulin (SHBG), free androgen index [FAI, calculated as T (nmol/L)*100/SHBG (nmol/L) (23)], the ratio of luteinizing hormone to follicle-stimulating hormone (LH/FSH), fasting insulin, fasting plasma glucose (FPG), homeostatic model assessment of insulin resistance [HOMA-IR, calculated as FPG (mmol/L) * Fasting Insulin(mIU/L)/22.5 (24, 25)], number of deliveries, and age. We analyzed the correlation between SAS-SS/SDS-SS and these 14 clinical factors by Pearson and Spearman correlation analysis and linear regression analysis in order to determine which factors were independent risk factors for anxiety-like and depression-like behaviors in women with PCOS.
Among the 802 participants, there were 369 infertile PCOS patients from The Effect of Acupuncture Pre-treatment Combined with Letrozole on Live Birth in Infertile Women with Polycystic Ovary Syndrome: a Randomized Controlled Trial and 433 fertile PCOS patients from the other two RCTs. We performed baseline data analysis, correlation analysis, and linear regression analyses on the two groups of patients separately.
Descriptive statistics of the data at baseline were analyzed using the chi-square test for categorical variables and using means and standard deviations with Student's t-test for continuous variables. The Pearson and Spearman correlation coefficients assessed the association between SAS and SDS parameters and the 14 clinical characteristics. Linear regression analysis assessed the strength of the relationship between SAS-SS or SDS-SS and the 14 baseline characteristics. All statistical analyses were carried out in SPSS 26.0, and P < 0.05 was considered statistically significant.
A total of 802 women with PCOS completed the SAS, and the SAS-SS ranged from 26 to 85. Of these, 26.1% (209/802) had scores ≥50 indicating anxiety-like behaviors, with 21.8% (175/802), 3.9% (31/802), and 0.4% (3/802) showing mild, moderate, and severe anxiety, respectively.
A total of 798 women with PCOS completed the SDS, and the SDS-SS ranged from 25 to 91. Of these, 52.0% (415/798) had scores ≥53 indicating depression-like behaviors, with 37.3% (298/798), 13.4% (107/798), and 1.3% (10/798) showing mild, moderate, and severe depression, respectively.
As shown as Table 1, age, BMI, WC, WHR, T, SHBG, and FAI were significantly different (P < 0.05) when comparing participants with anxiety (SAS-SS ≥ 50) to those without (SAS-SS < 50). As shown in Table 2, age, BMI, WC, acne, T, FAI, fasting insulin, FPG, and HOMA-IR were significantly different (P < 0.05) when comparing participants with depression (SDS-SS ≥ 53) to those without (SDS-SS < 53).
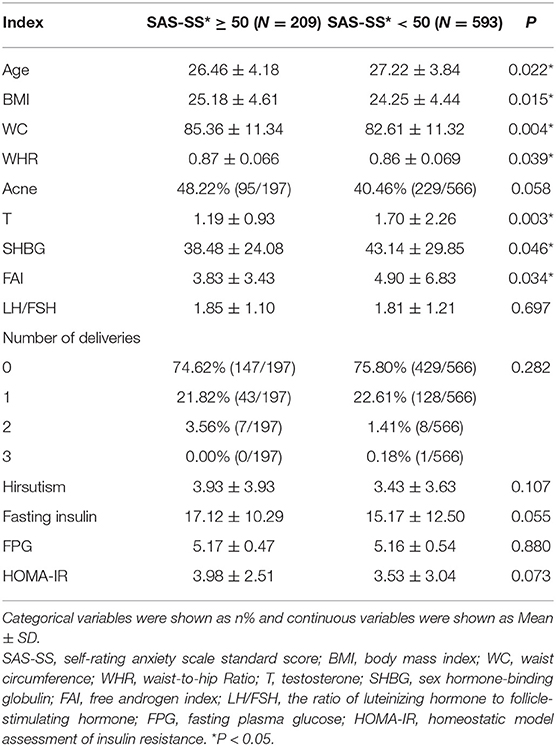
Table 1. Baseline characteristics of women with PCOS with anxiety (SAS-SS ≥ 50) and without anxiety (SAS-SS < 50).
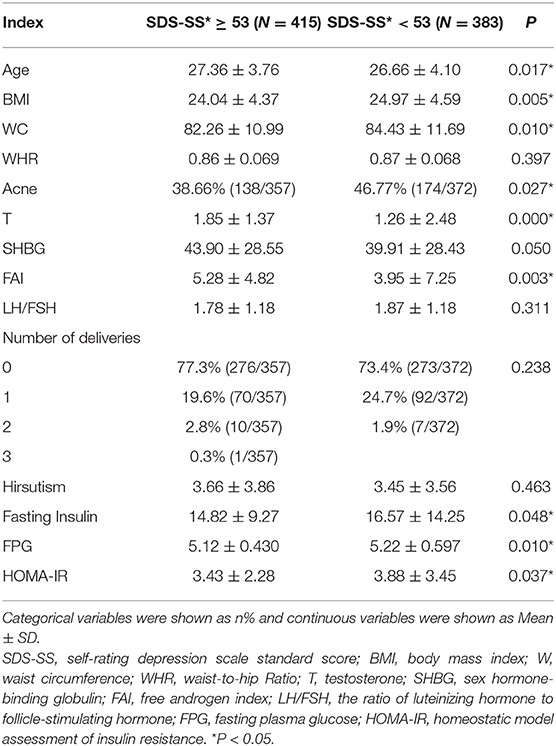
Table 2. Baseline characteristics of women with PCOS with depression (SDS-SS ≥ 53) and without depression (SDS-SS < 53).
We next analyzed the correlation between the severity of anxiety/depression-like behaviors and the baseline clinical characteristics. As shown in Figure 1A, the correlation between age, BMI, and WC and the severity of anxiety was statistically significant and their correlation coefficients were −0.081, 0.12, and 0.12, respectively (P < 0.05). BMI and WC were positively correlated with the severity of anxiety, while age was negatively correlated. A shown in Figure 1B, the correlation between age, BMI, W, and the severity of depression was statistically significant, and their correlation coefficients were 0.065, −0.087, and −0.079, respectively (P < 0.05). Age showed a positive association with the degree of depression, while BMI and WC showed a negative association.
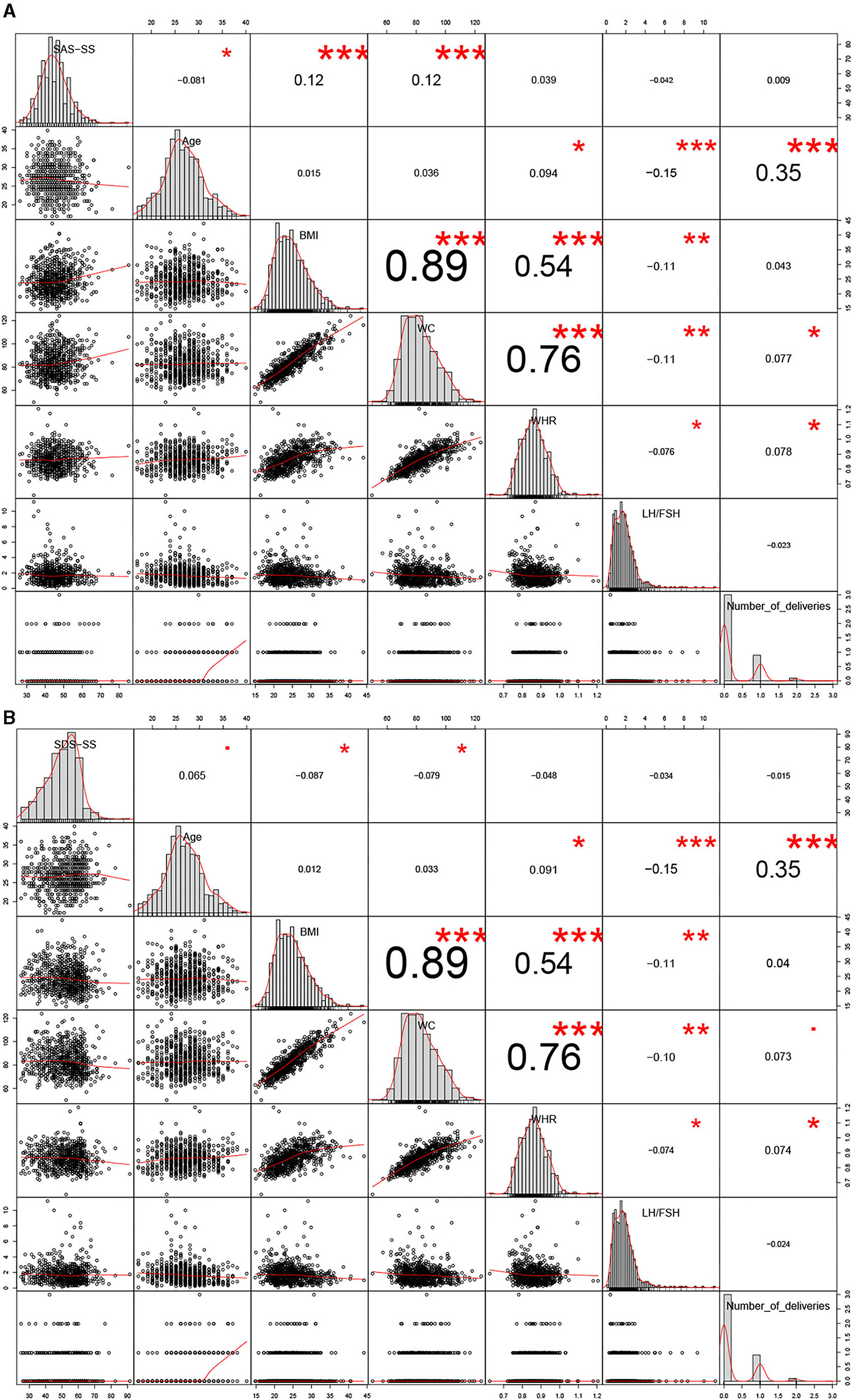
Figure 1. Correlation analyses between anxiety/depression-like behaviors and the 14 clinical parameters. *P < 0.05, **P < 0.01, ***P < 0.005.
As shown in Figure 2A, acne, T, SHBG, FAI, hirsutism, fasting insulin, and HOMA-IR were significantly correlated with SAS-SS. T, SHBG, and FAI were negatively correlated (−0.13, −0.10, and −0.11, respectively) (P < 0.05), while acne, hirsutism, fasting insulin, and HOMA-IR were positively correlated (0.079, 0.11, 0.084, and 0.082, respectively) (P < 0.05). As shown in Figure 2B, both T and FAI were significantly positively correlated with SDS-SS (0.16 and 0.12), while fasting insulin, FBG, and HOMA-IR were significantly negatively correlated with SDS-SS (−0.074, −0.10, and −0.077, respectively). It is worth noting that the factors of age, BMI, W, T, FAI, fasting insulin, and HOMA-IR were significantly correlated with both anxiety-like and depression-like behaviors.
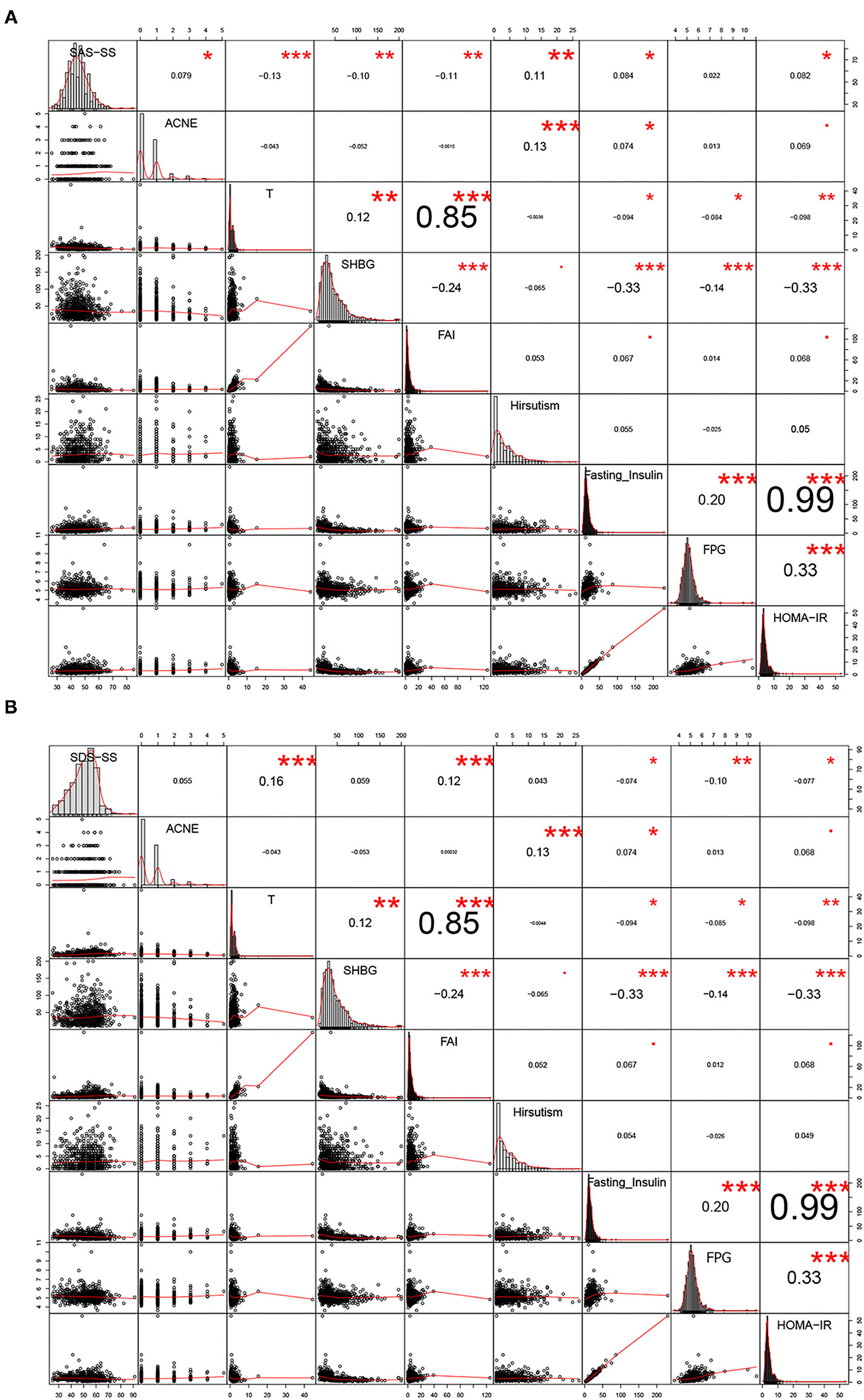
Figure 2. Correlation analyses between anxiety/depression-like behaviors and the 14 clinical parameters. *P < 0.05, **P < 0.01, ***P < 0.005.
We performed linear regression analysis to evaluate risk factors of anxiety/depression-like behaviors in women with PCOS. As shown in Table 3, FAI, age, BMI, WHR, and hirsutism were significant independent risk factors for anxiety-like behaviors in women with PCOS, with odds ratios of −0.335, −0.258, 0.265, 14.911, and 0.235, respectively (P < 0.05). For depression-like behaviors, SHBG, FAI, age, WC, WHR, number of deliveries, fasting insulin, FPG, and HOMA-IR were significant risk factors with odds ratios of 0.203, 1.268, 1.639, −0.403, 46.293, −4.199, −2.805, −11.709, and 10.749, respectively (P < 0.05) (Table 4).
Of the 369 infertile PCOS patients, 18.42% (68/369) had scores ≥50 indicating anxiety-like behaviors and 70.19% (259/369) had scores ≥53 indicating depression-like behaviors. Of the 433 fertile PCOS patients, 32.56% (141/433) had scores ≥50 indicating anxiety-like behaviors and 36.36% (156/429) had scores ≥53 indicating depression-like behaviors.
As shown as Supplementary 3, Supplementary Table S1, age, BMI, WC, WHR, acne, T, SHBG, FAI, number of deliveries, fasting insulin, FPG, and HOMA-IR were significantly different (P < 0.05) when comparing infertile PCOS patients with fertile PCOS patients. In Figure 3A, number of deliveries and hirsutism were significantly positively correlated with SAS-SS (0.09 and 0.13) in the fertile group. In Figure 3B, BMI and WC were significantly positively correlated with SDS-SS (0.094 and 0.083) in the fertile group. In the infertile PCOS group shown in Figure 4A, age was significantly negatively correlated with SAS-SS (−0.098) while BMI, WC, WHR, acne, and hirsutism were significantly positively correlated with SAS-SS (0.34, 0.35, 0.38, 0.11, and 0.16). In Figure 4B, BMI, WC, WHR, acne, and hirsutism were significantly positively correlated with SDS-SS (0.35, 0.36, 0.40, 0.12, and 0.14).
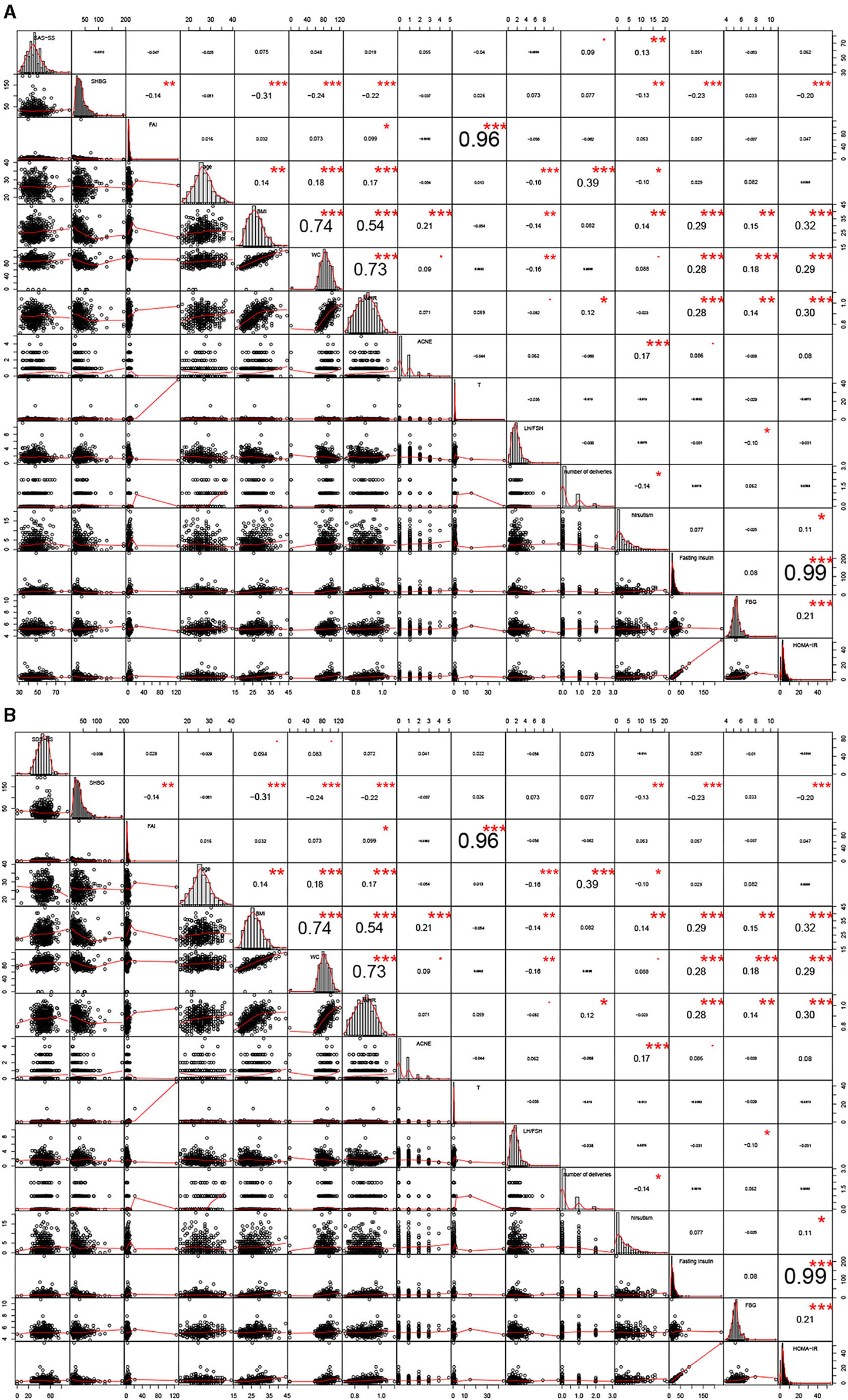
Figure 3. Correlation analyses between anxiety/depression-like behaviors and the 14 clinical parameters in fertile group. *P < 0.05, **P < 0.01, ***P < 0.005.
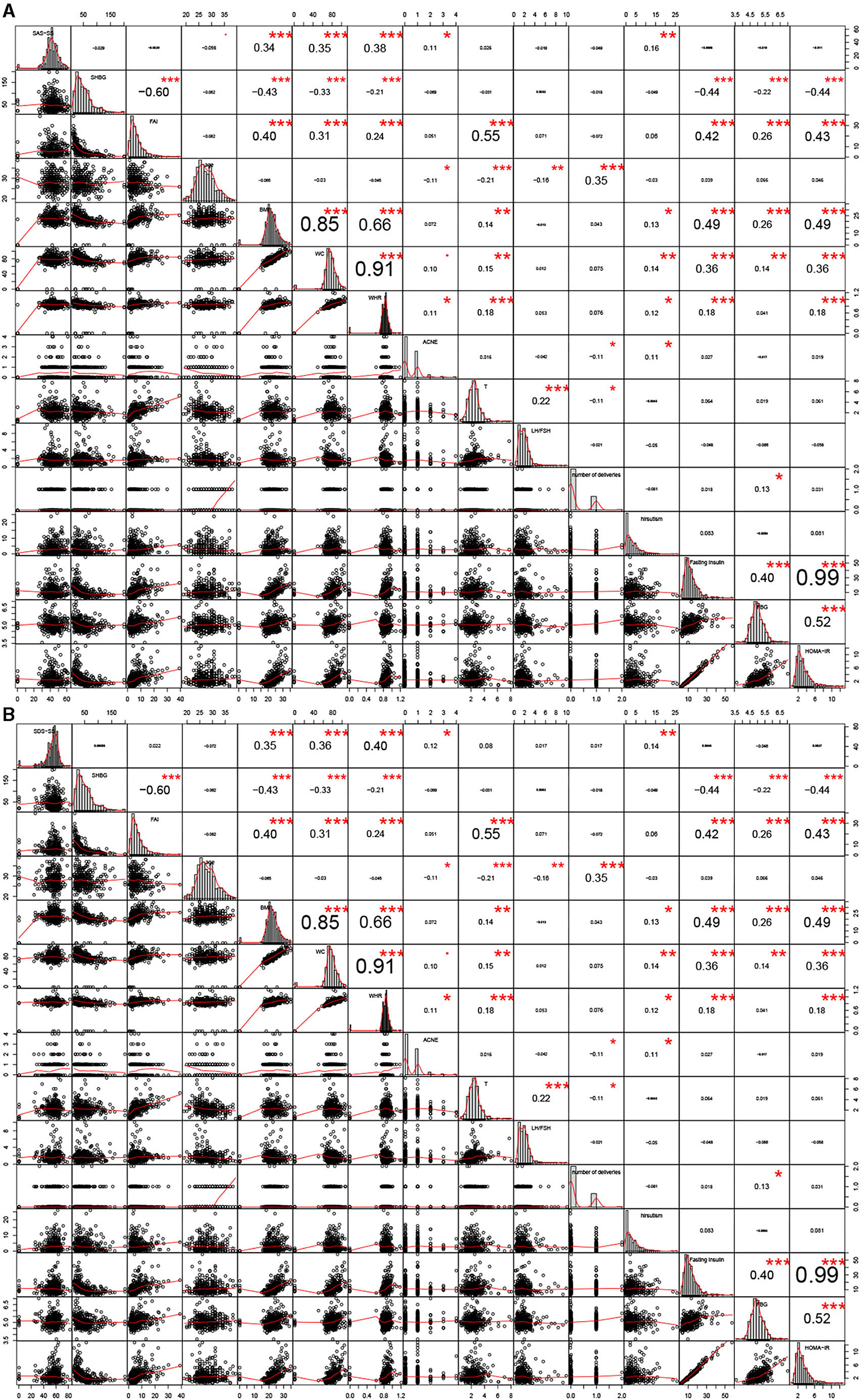
Figure 4. Correlation analyses between anxiety/depression-like behaviors and the 14 clinical parameters in infertile group. *P < 0.05, **P < 0.01, ***P < 0.005.
From the regression analysis results shown in Supplementary 3, Supplementary Tables S2–S4, SHBG was a significant independent risk factor for anxiety-like behaviors in infertile women with PCOS, with an odds ratio of 0.979, and LH/FSH was a significant independent risk factor for depression-like behaviors in fertile women with PCOS with an odds ratio of 0.754.
In this study the prevalence of anxiety-like and depression-like behaviors in women with PCOS was 26.1 and 52.0%, respectively, with the majority of these having a mild degree of anxiety/depression-like behaviors. Among infertile PCOS patients, the prevalence of anxiety-like and depression-like behaviors was 18.42 and 70.19%, compared to 32.56 and 36.36% in fertile PCOS patients, respectively. Anxiety-like behaviors were associated with age, body image-related factors (including BMI and WHR), and hyperandrogenism-related factors (including FAI and hirsutism). Depression-like behaviors were associated with age, body image-related factors (including BMI and WHR), hyperandrogenism-related factors (including FAI and hirsutism), and metabolic factors (including fasting insulin, FBG, and HOMA-IR). Among infertile PCOS patients, anxiety/depression-like behaviors were associated with body image-related factors (including BMI, WC, and WHR) and hyperandrogenism-related factors (including acne and hirsutism). As for fertile PCOS patients, anxiety-like behaviors were associated with number of deliveries and hirsutism while depression-like behaviors were associated with body image-related factors (including BMI and WC).
Different ethnic origin leads to differing manifestations of PCOS. Kakoly et al. reported that Asian, American, and European PCOS patients had 5, 4, and 3-fold increased risks of developing impaired glucose tolerance (3). Uche Ezeh et al. reported that among Americans, African Americans have the greatest BMI and WC, followed by Hispanic White and non-Hispanic White Americans and finally by Asian Americans (26). They reported that African Americans had higher Ferriman–Gallwey scores, which means they had more severe clinical hyperandrogenism but were second in severity in terms of biochemical hyperandrogenism after white Americans (26). In addition, their results showed that African Americans were more likely to have metabolic disorders than white Americans and Asian Americans (26). In all the above aspects, Asian Americans ranked last.
In China, the incidence of PCOS in the Han population is 5.6% (27). Rong Li et al. reported that compared to healthy Chinese women, PCOS patients do not show a higher prevalence of obesity but show a higher prevalence of hyperandrogenism and insulin resistance (IR) (27). Different from American or European women, among Chinese women overweight and obesity are defined as BMI ≥ 24 kg/m2 and ≥ 28 kg/m2, respectively, and abdominal obesity is defined as WC ≥ 80 cm (28). Under this standard, the prevalence of obesity in PCOS increases with age according to Rong Li (27). In our study, the PCOS patients with IR accounted for 53.62% (444/828), which was similar to the previous report that about 50%−70% of PCOS patients have varying degrees of IR (9). Thus, to a certain degree our results are applicable to the general PCOS population.
Anxiety and depression are the most common mental disorders worldwide. Anxiety disorder is a group of mental disorders characterized by feeling anxious and fearful, while depressive disorders are characterized by grief, loss of interest or happiness, feelings of guilt or low self-worth, disturbed sleep or appetite, fatigue, and poor concentration (29). According to the WHO report about depression and anxiety disorders, the proportions of the global population with depression and anxiety in 2015 were estimated to be 4.4 and 3.6%, respectively (29, 30). For women, the incidences of depression and anxiety globally are 5.1 and 4.6%, respectively. WHO data also showed that for females aged 20–40 years the prevalence of anxiety and depression ranges from 5 to 6% and from 6 to 7%, respectively (29). In our study, the prevalence of anxiety-like and depression-like behavior among all PCOS patients aged 20–40 years rose to 26.1 and 52.0%, respectively, and in the fertile group this rose to 32.56 and 36.36%. Similarly, Cooney et al. reported that the prevalence of anxiety and depression was higher in women with PCOS compared to healthy women (31). For the infertile subgroup, the prevalence of anxiety-like and depression-like behavior was 18.42 and 70.19%. Experiencing infertility brought greater sadness, and this was consistent with previous reports (32).
The pathogenesis of PCOS remains poorly understood (33–36), and PCOS presents as a diverse and complicated syndrome involving reproductive dysfunction (infertility and menstrual irregularity), metabolic problems (dyslipidemia, obesity, increased insulin levels, and glucose intolerance), cardiovascular problems (coronary heart disease), psychological disorders (anxiety and depression), and sexual dysfunction (37–41). In our study, we mainly focused on the psychological impact of PCOS. Previous studies have shown that PCOS patients tend to be under greater psychological pressure because they often experience more concern about body image-related factors as well as more worries about infertility (13, 42). Such negative thoughts can bring about negative emotions such as anxiety, worry, fear, depression, and low self-esteem (42). In this study, we similarly found that body image-related factors, including BMI, WHR, and hirsutism, were related to the occurrence of anxiety-like behaviors and that BMI, WC, and WHR were related to the occurrence of depression-like behaviors. Also, regardless of fertility status BMI and WC were related to the occurrence of depression-like behaviors. As for the occurrence of anxiety-like behaviors, acne and hirsutism were related to the infertile group while only hirsutism was related to the fertile group. Others have demonstrated that a higher BMI, which is known to be independently associated with PCOS, is linked to greater dissatisfaction with one's appearance (43, 44). Some researchers have also suggested recently that PCOS symptoms such as changes in body size and appearance might result in reduced quality of life and reduced psychological, social, and sexual well-being (45). Acne and hirsutism are prevalent in women with PCOS (46), and some studies suggest that these features are associated with more severe anxiety and depression symptoms in women with PCOS (47). Taken together, long-term negative feelings about one's appearance likely lead to a high prevalence of poor mental health such as anxiety or depression in women with PCOS.
One point worth noting was that age, body image related factors and hyperandrogenism related factors are related to the occurrence of anxiety/depression-like behaviors, the correlation coefficients of two groups were completely opposite. The PCOS patients with older age, lower BMI, lighter acne and IR but higher T tended to correlated with depression-like behaviors, while younger PCOS patients were opposite, as shown in Supplementary 3, Supplementary Table S6. We have not found relevant literature so far. Future studies needed to be undertaken to explain it.
Hyperandrogenism is another important aspect of PCOS that should be taken into consideration when exploring psychological outcomes, and we found that FAI was a significant independent factor for these two behaviors and was positively correlated with depression-like behaviors and negatively correlated with anxiety-like behaviors. Clinical hyperandrogenism, i.e., hirsutism, is present in 6.1–10.0% of women with PCOS in China, but the prevalence of biochemical hyperandrogenism could be as high as 21.1% (48, 49). A large meta-analysis reported that both clinical and biochemical hyperandrogenism are related to the prevalence of anxiety/depression-like behaviors in women with PCOS (31) and the specific manifestations of clinical hyperandrogenism—hirsutism and acne—likely lead to an increased prevalence of depression and anxiety in this population (50). Ferriman–Gallwey scores, which are used to evaluate hirsutism, were reported to be increased in women with PCOS with anxiety and depression symptoms, and free T levels were higher in women with PCOS and anxiety compared to those without anxiety (51). In our study, FAI was significantly lower in the anxiety-like group and significantly higher in the depression-like group when compared to the normal-scoring groups.
In our study, fasting insulin, FBG, and HOMA-IR were significantly negatively correlated with SDS-SS in women with PCOS, and metabolic disorder was an important factor affecting depression-like behaviors. It was reported previously that depression is linked to blood insulin tested at 2 h in a glucose tolerance test (52). However, more high-quality research should be carried out in the future.
The strength of our study is that our data on the prevalence of anxiety-like and depression-like behaviors was in a relatively large sample of women with PCOS from an ethnic background for which there are limited relevant data. A limitation of our study lies in potential selection/recruitment bias of the participants because this was a secondary analysis of three previous studies performed to study various effects of acupuncture in women with PCOS. Based on the inclusion criteria of the initial studies, some of the recruited women with PCOS had IR and some of them had infertility. Also, only Chinese women were involved in this study. Another limitation is that both anxiety-like and depression-like behaviors were self-reported. Also, some factors such as smoking and quality of sleep were not considered, and this might make our results less reliable.
In conclusion, the prevalence of anxiety-like and depression-like behaviors in women with PCOS was 26.1 and 52.0%, respectively. In fertile PCOS patients, the prevalence was 32.56 and 36.36%, respectively, and in infertile PCOS patients the prevalence was 18.42 and 70.19%. Age, BMI, WHR, and FAI were associated with both anxiety and depression-like symptoms, while hirsutism was an important factor for anxiety-like behaviors and fasting insulin, FBG, and HOMA-IR were important factors for depression-like behaviors. Body image-related factors and hyperandrogenism-related factors were related to both anxiety-like behaviors and depression-like behaviors in both infertile and fertile PCOS patients.
The data analyzed in this study is subject to the following licenses/restrictions: The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request. Requests to access these datasets should be directed to ZG9jdG9yaG9uZ3hpYUAxMjYuY29t.
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. 2013039, No. 2015010, No. 2014018). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
HM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. HL: project development, data collection, data analysis, and manuscript writing. ML, DZ, and HM: project development, data collection, manuscript writing, and revision. EN, JIL, and JUL: data collection and manuscript revision. YS, CZ, XW, ZM, and MO: data collection. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.709674/full#supplementary-material
1. Azziz R. Polycystic ovary syndrome. Obstet Gynecol. (2018) 132:321–36. doi: 10.1097/AOG.0000000000002698
2. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. (2004) 81:19–25. 81:19–25. doi: 10.1016/j.fertnstert.2003.10.004
3. Kakoly NS, Khomami MB, Joham AE, Cooray SD, Misso ML, Norman RJ, et al. Ethnicity, obesity and the prevalence of impaired glucose tolerance and type 2 diabetes in PCOS: a systematic review and meta-regression. Hum Reprod Update. (2018) 24:455–67. doi: 10.1093/humupd/dmy007
4. Wild RA, Rizzo M, Clifton S, Carmina E. Lipid levels in polycystic ovary syndrome: systematic review and meta-analysis. Fertil Steril. (2011) 95:1073–9.e1-11. 95:1073–9.e1-11. doi: 10.1016/j.fertnstert.2010.12.027
5. Behboudi-Gandevani S, Amiri M, Bidhendi Yarandi R, Noroozzadeh M, Farahmand M, Rostami Dovom M, et al. The risk of metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Clin Endocrinol. (2018) 88:169–84. doi: 10.1111/cen.13477
6. Yu HF, Chen HS, Rao DP, Gong J. Association between polycystic ovary syndrome and the risk of pregnancy complications: a PRISMA-compliant systematic review and meta-analysis. Medicine. (2016) 95:e4863. 95:e4863. doi: 10.1097/MD.0000000000004863
7. Kahal H, Kyrou I, Tahrani AA, Randeva HS. Obstructive sleep apnoea and polycystic ovary syndrome: a comprehensive review of clinical interactions and underlying pathophysiology. Clin Endocrinol. (2017) 87:313–9. 87:313–9. doi: 10.1111/cen.13392
8. Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. (2014) 20:748–58. 20:748–58. doi: 10.1093/humupd/dmu012
9. Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. (2017) 32:1075–91. 32:1075–91. doi: 10.1093/humrep/dex044
10. Barry JA, Kuczmierczyk AR, Hardiman PJ. Anxiety and depression in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. (2011) 26:2442–51. doi: 10.1093/humrep/der197
11. Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. (2018) 62:318–25. 62:318–25. doi: 10.1007/s12020-018-1692-3
12. Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, et al. Consensus on women's health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. (2012) 97:28–38.e25. doi: 10.1016/j.fertnstert.2011.09.024
13. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. (2010) 8:41. 8:41. doi: 10.1186/1741-7015-8-41
14. Podfigurna-Stopa A, Luisi S, Regini C, Katulski K, Centini G, Meczekalski B, et al. Mood disorders and quality of life in polycystic ovary syndrome. Gynecol Endocrinol. (2015) 31:431–4. 31:431–4. doi: 10.3109/09513590.2015.1009437
15. Blay SL, Aguiar JV, Passos IC. Polycystic ovary syndrome and mental disorders: a systematic review and exploratory meta-analysis. Neuropsychiatr Dis Treat. (2016) 12:2895–903. 12:2895–903. doi: 10.2147/NDT.S91700
16. Hollinrake E, Abreu A, Maifeld M, Van Voorhis BJ, Dokras A. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Steril. (2007) 87:1369–76. 87:1369–76. doi: 10.1016/j.fertnstert.2006.11.039
17. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12:63–70. 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
18. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
19. Dunstan DA, Scott N. Assigning clinical significance and symptom severity using the zung scales: levels of misclassification arising from confusion between index and raw scores. Depress Res Treat. (2018) 2018:9250972. 2018:9250972. doi: 10.1155/2018/9250972
20. Zheng Y, Stener-Victorin E, Ng EH, Li J, Wu X, Ma H. How does acupuncture affect insulin sensitivity in women with polycystic ovary syndrome and insulin resistance? Study protocol of a prospective pilot study. BMJ Open. (2015) 5:e007757. doi: 10.1136/bmjopen-2015-007757
21. Li J, Ng EH, Stener-Victorin E, Hu Z, Shao X, Wang H, et al. Acupuncture treatment for insulin sensitivity of women with polycystic ovary syndrome and insulin resistance: a study protocol for a randomized controlled trial. Trials. (2017) 18(1):115. doi: 10.1186/s13063-017-1854-2
22. Li J, Ng EH, Stener-Victorin E, Hu Z, Wu W, Lai M, et al. Comparison of acupuncture pretreatment followed by letrozole versus letrozole alone on live birth in anovulatory infertile women with polycystic ovary syndrome: a study protocol for a randomised controlled trial. BMJ Open. (2016) 6(10):e010955. 6(10):e010955. doi: 10.1136/bmjopen-2015-010955
23. Li H, Xu X, Wang X, Liao X, Li L, Yang G, et al. Free androgen index and Irisin in polycystic ovary syndrome. J Endocrinol Invest. (2016) 39:549–56. doi: 10.1007/s40618-015-0403-7
24. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. (1985) 28:412–9. doi: 10.1007/BF00280883
25. Aslam M, Mishra BK, Goyal S, Siddiqui AA, Madhu SV. Family history of diabetes determines the association of HOMA-IR with fasting and postprandial triglycerides in individuals with normal glucose tolerance. J Clin Lipidol. (2021) 15:227–34. doi: 10.1016/j.jacl.2020.11.002
26. Ezeh U, Ida Chen YD, Azziz R. Racial and ethnic differences in the metabolic response of polycystic ovary syndrome. Clin Endocrinol. (2020) 93:163–72. doi: 10.1111/cen.14193
27. Li R, Zhang Q, Yang D, Li S, Lu S, Wu X, et al. Prevalence of polycystic ovary syndrome in women in China: a large community-based study. Hum Reprod. (2013) 28:2562–9. doi: 10.1093/humrep/det262
29. Mental Health and Substance Use Depression and Other Common Mental Disorders. World Health Organization (2017) 24:WHO/MSD/MER/2017.2.
30. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/S0140-6736(16)31678-6
31. Cooney LG, Dokras A. Depression and anxiety in polycystic ovary syndrome: etiology and treatment. Curr Psychiatry Rep. (2017) 19:83. doi: 10.1007/s11920-017-0834-2
32. Rooney KL, Domar AD. The relationship between stress and infertility. Dialogues Clin Neurosci. (2018) 20:41–47. doi: 10.31887/DCNS.2018.20.1/klrooney
33. Picton HM, Balen AH. Transgenerational PCOS transmission. Nat Med. (2019) 25:1818–20. 25:1818–20. doi: 10.1038/s41591-019-0678-x
34. Patel S. Polycystic ovary syndrome (PCOS), an inflammatory, systemic, lifestyle endocrinopathy. J Steroid Biochem Mol Biol. (2018) 182:27–36. doi: 10.1016/j.jsbmb.2018.04.008
35. Dumont A, Robin G, Dewailly D. Anti-müllerian hormone in the pathophysiology and diagnosis of polycystic ovarian syndrome. Curr Opin Endocrinol Diabetes Obes. (2018) 25:377–84. 25:377–84. doi: 10.1097/MED.0000000000000445
36. Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. (2016) 37:467–520. 37:467–520. doi: 10.1210/er.2015-1104
37. Torchen LC. Cardiometabolic risk in PCOS: more than a reproductive disorder. Curr Diab Rep. (2017) 17:137. doi: 10.1007/s11892-017-0956-2
38. Anagnostis P, Tarlatzis BC, Kauffman RP. Polycystic ovarian syndrome (PCOS): long-term metabolic consequences. Metabolism. (2018) 86:33–43. doi: 10.1016/j.metabol.2017.09.016
39. Kakoly NS, Earnest A, Teede HJ, Moran LJ, Joham AE. The impact of obesity on the incidence of type 2 diabetes among women with polycystic ovary syndrome. Diabetes Care. (2019) 42:560–7. 42:560–7. doi: 10.2337/dc18-1738
40. Çoban ÖG, Tulaci ÖD, Adanir AS, Önder A. Psychiatric disorders, self-esteem, and quality of life in adolescents with polycystic ovary syndrome. J Pediatr Adolesc Gynecol. (2019) 32:600–4. 32:600–4. doi: 10.1016/j.jpag.2019.07.008
41. Firmino Murgel AC, Santos Simões R, Maciel GAR, Soares Jr JM, Baracat EC. Sexual dysfunction in women with polycystic ovary syndrome: systematic review and meta-analysis. J Sex Med. (2019) 16:542–50. 16:542–50. doi: 10.1016/j.jsxm.2019.01.313
42. Kogure GS, Ribeiro VB, Lopes IP, Furtado CLM, Kodato S, Silva de Sá MF, et al. Body image and its relationships with sexual functioning, anxiety, and depression in women with polycystic ovary syndrome. J Affect Disord. (2019) 253:385–93. doi: 10.1016/j.jad.2019.05.006
43. Dawes AJ, Maggard-Gibbons M, Maher AR, Booth MJ, Miake-Lye I, Beroes JM, et al. Mental health conditions among patients seeking and undergoing bariatric surgery: a meta-analysis. JAMA. (2016) 315:150–63. 315:150–63. doi: 10.1001/jama.2015.18118
44. Burke NL, Storch EA. A meta-analysis of weight status and anxiety in children and adolescents. J Dev Behav Pediatr. (2015) 36:133–45. doi: 10.1097/DBP.0000000000000143
45. Behboodi Moghadam Z, Fereidooni B, Saffari M, Montazeri A. Measures of health-related quality of life in PCOS women: a systematic review. Int J Womens Health. (2018) 10:397–408. 10:397–408. doi: 10.2147/IJWH.S165794
46. Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev. (2015) 36:487–525. doi: 10.1210/er.2015-1018
47. Bazarganipour F, Taghavi SA, Montazeri A, Ahmadi F, Chaman R, Khosravi A. The impact of polycystic ovary syndrome on the health-related quality of life: a systematic review and meta-analysis. Iran J Reprod Med. (2015) 13:61–70.
48. Zhang HY, Guo CX, Zhu FF, Qu PP, Lin WJ, Xiong J. Clinical characteristics, metabolic features, and phenotype of Chinese women with polycystic ovary syndrome: a large-scale case-control study. Arch Gynecol Obstet. (2013) 287:525–31. doi: 10.1007/s00404-012-2568-z
49. Zhao X, He Z, Mo Y, Chen X, Chen Y, Yang D. Determining the normal cut-off levels for hyperandrogenemia in Chinese women of reproductive age. Eur J Obstet Gynecol Reprod Biol. (2011) 154:187–91. 154:187–91. doi: 10.1016/j.ejogrb.2010.10.021
50. Veltman-Verhulst SM, Boivin J, Eijkemans MJ, Fauser BJ. Emotional distress is a common risk in women with polycystic ovary syndrome: a systematic review and meta-analysis of 28 studies. Hum Reprod Update. (2012) 18:638–51. doi: 10.1093/humupd/dms029
51. Ekbäck MP, Lindberg M, Benzein E, Årestedt K. Health-related quality of life, depression and anxiety correlate with the degree of hirsutism. Dermatology. (2013) 227:278–84. 227:278–84. doi: 10.1159/000355356
Keywords: PCOS, anxiety, depression, hyperandrogenism, metabolic syndrome
Citation: Lin H, Liu M, Zhong D, Ng EHY, Liu J, Li J, Shi Y, Zhang C, Wen X, Mai Z, Ou M and Ma H (2021) The Prevalence and Factors Associated With Anxiety-Like and Depression-Like Behaviors in Women With Polycystic Ovary Syndrome. Front. Psychiatry 12:709674. doi: 10.3389/fpsyt.2021.709674
Received: 22 May 2021; Accepted: 16 September 2021;
Published: 20 October 2021.
Edited by:
Yuan-Pang Wang, University of São Paulo, BrazilReviewed by:
Rong Li, Peking University Third Hospital, ChinaCopyright © 2021 Lin, Liu, Zhong, Ng, Liu, Li, Shi, Zhang, Wen, Mai, Ou and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongxia Ma, ZG9jdG9yaG9uZ3hpYUAxMjYuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.