
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 06 August 2021
Sec. Psychological Therapy and Psychosomatics
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.709295
This article is part of the Research TopicResilience in Chronic DiseaseView all 13 articles
Background: Improving Quality of Life (QOL) is an essential objective in the management of inflammatory bowel disease. An accumulating body of research has been conducted to explore the association between perceived stigma and QOL among patients with chronic illness. Still, underlying mechanisms behind this pathway have not been thoroughly examined.
Objective: To investigate (a) the effect of perceived stigma on QOL among patients with inflammatory bowel disease; and (b) the mediating role of resilience in the association between perceived stigma and QOL.
Methods: This cross-sectional study included a convenient sample of patients diagnosed with inflammatory bowel disease from four tertiary hospitals in Jiangsu Province, China. Patients completed the Perceived Stigma Scale in Inflammatory Bowel Disease (PSS-IBD), the Resilience Scale for Patients with Inflammatory Bowel Disease (RS-IBD), and the Inflammatory Bowel Disease Questionnaire (IBDQ). A bootstrapping analysis was implemented using the SPSS macro PROCESS.
Results: A total of 311 patients with Cohn's disease and ulcerative colitis participated in this study, and 57.6% were men. The mean disease duration was 3.51 ± 1.04 years. Approximately 40% of the sample exceeded the criterion score for moderate stigma. Patients who perceived moderate or severe stigma reported lower QOL compared with those with mild stigma. After controlling for sociodemographic and clinical variables, we observed that perceived stigma was negatively associated with resilience. Moreover, resilience was found to mediate the relationship between perceived stigma and all aspects of QOL.
Conclusions: These findings suggested that QOL of patients with inflammatory bowel disease was associated with perceived stigma and resilience and identified the mediating effects of resilience in the relationship between perceived stigma and QOL. Furthermore, this suggests that integrating intervention techniques to target resilience into the QOL improvement program of individuals with perceived stigma is possible.
Inflammatory bowel disease (IBD), mainly comprising Cohn's disease (CD) and ulcerative colitis (UC), are immune-mediated intestinal inflammatory disorders characterized by early-onset. Recently epidemiological data show that approximately 6.9 million individuals worldwide are living with IBD (1). Moreover, the incidence and prevalence of IBD are still increasing, especially in newly industrialized countries. Patients with IBD suffer from abdominal pain, diarrhea, rectal bleeding, and frequent bowel movements throughout their lifetime repeatedly (2, 3). Treatment for IBD largely depends on pharmacological means, but surgery is often needed when complications occur (4). It is estimated that the overall 10-year risk of surgery after diagnosis is 39.5% for CD and 13.3% for UC (5).
The quality of life (QOL) among patients with IBD is of growing significance since the patient-reported outcomes are recognized as primary endpoints by regulatory agencies (6). QOL is a broad multidimensional concept that involves objective and subjective aspects, focusing on the physical, emotional, mental, and social impact of the disease on patients' lives (7). Traumatic childhood experiences, sensory processing patterns, and chronic disease are recognized risk factors for QOL (8, 9). As an uncommon, chronic disease, IBD seriously impairs the QOL of patients (10–12). A recent meta-analysis performed by Knowles and his colleagues indicated that QOL was significantly lower for those with IBD relative to healthy controls (13). QOL among patients with IBD may be influenced by disease symptoms, treatment regimen, and various psychosocial variables (14). Psychosocial variables could affect the patients' psychological and social functions and alter gastrointestinal physiology by activating the microbiota-brain-gut axis, leading to decreased or improved QOL (15–18). Sweeney and her colleagues reported that depression, fear avoidance, and catastrophizing were risk factors for IBD -related pain, while self-efficacy and mental well-being were protective factors (19). Recently, the perceived stigma has been considered a prominent psychosocial variable that damage QOL (20). Therefore, the understanding of QOL should pay attention to the physical distress caused by IBD and consider perceived stigma and other psychosocial factors.
Perceived stigma is defined as individuals' feelings that other persons hold negative attitudes or negative beliefs about them and their condition (21). Risks of incontinence in public, the changes in body image, negative impacts on sexual life, and burdens to others make patients with IBD susceptible to perceived stigma (22). Taft TH et al. investigated the prevalence of stigma in patients with IBD and reported that 84% of participants had perceived stigma (23). Literature outside the field of IBD has demonstrated that higher levels of perceived stigma are associated with poorer QOL (24–26). While perceived stigma is identified as a specific concern for patients with IBD, only one study to date has proved the negative relationship between perceived stigma and QOL (23).
Moreover, the specific mechanisms by which perceived stigma affects QOL in patients with IBD remain elucidated. As not all IBD patients who perceive stigma have poor QOL, it is plausible to assume that some factors may mediate such a connection (27, 28). Resilience, one of the most mentioned positive psychological resources, is usually defined from three perspectives in chronic disease: traits, outcome, and process. For example, (1) traits reflecting the characteristics of tenacity and flexibility in response to disease-related stress; (2) positive health outcomes in high-risk patients; (3) a dynamic process of successful adaptation when exposed to chronic disease (29). There is a debate concerning how to define resilience, but previous research has identified the role of 'resiliency training programs,' which infers it is modifiable (29). In our study, resilience is a quantifiable and modifiable personal quality that enables individuals to bounce back from IBD-related adversity (30). Resilient patients could cope with their disease adaptively. Neurological evidence revealed that resilience could invoke specific brain structures and neural circuits to help the individual to regulate emotion and adopt adaptive social behavior (17, 18). Resilience was reported to positively predict QOL in adolescents with type 1 diabetes and patients with acute myocardial infarction (31). Among people living with IBD, higher levels of resilience were significantly associated with better QOL (32, 33). Perceived stigma from family members, spouse, friends, employers, and colleagues affects resilience. A qualitative study revealed that stigma is more pronounced in less resilient IBD patients, especially in those lacking support networks (34). Self-esteem, mastery, and optimism, which are essential components of resilience, could be reduced by perceived stigma (35). Hsiung et al. found that mastery mediates the association between perceived stigma and QOL in patients with schizophrenia (36). The above evidence suggested that perceived stigma might impair resilience by causing low self-esteem, mastery, and pessimism, sequentially affecting QOL. However, no studies have analyzed the relationship between perceived stigma, resilience, and QOL among patients with IBD to our knowledge.
The present study aims to explore the impact of perceived stigma on QOL and investigate the mediating effects of resilience in the path from perceived stigma to QOL among patients with IBD. First, we hypothesized that perceived stigma was negatively associated with QOL among patients with IBD. Second, we further supposed that resilience could mediate the link between perceived stigma and QOL in these patients.
Patients with IBD were recruited from the Digestive Department of four tertiary hospitals in Jiangsu Province, China, using consecutive sampling. Participants were referred by their charge nurse if they were (1) diagnosed with UC or CD according to the current diagnostic criteria (2, 3); age≥18 years; (3) disease duration of more than 6 months; (4) education level of all participants was elementary school or above, able to read and understand the questionnaire. Exclusion criteria included: (1) severe mental illness (such as schizophrenia, bipolar disorder, paranoiac psychosis); (2) malignant tumors or other chronic diseases (such as heart failure, diabetes); (3) combined with other intestines or anorectal disease. The first authors introduced the purpose, procedures, and potential benefits and risks of the study. All the patients were asked to give written informed consent if they were eligible for the study. Next, the patients completed a set of self-reported questionnaires in a quiet room at each clinical site, including demographic (age, gender, education level, marital status, residence, family income) and clinical (disease type, duration) information. Modified Truelove and Witts' Severity Index and Harvey Bradshaw Simple Index were used to measure the disease activity of UC and CD patients, respectively, by their nurse in charge. We used G.Power 3.1 to calculate the sample size. The results showed that the data from 257 patients with UC and CD would give sufficient power (0.90) to detect a small effect size (0.05) on quality of life, explained by 13 independent variables (the perceived stigma, resilience, demographic, and clinical variables), with alpha = 0.05.
Of the 343 patients who were interested in participating and screened for eligibility, 320 were eligible. Three hundred twenty patients signed the informed consent and finished the questionnaires. Because of the incompletely filled questionnaires, nine respondents were excluded from the study. Finally, the data of 311 participants were used for the data analysis. Figure 1 showed the participant recruitment process in detail.
The Perceived Stigma Scale in IBD (PSS-IBD) is a 10-item instrument designed to determine the presence of perceived stigma (23). Items are rated on a five-point scale ranging from 0 (Never) to 4 (always) and evaluated for six social domains. A total score of perceived stigma can be obtained by summing the scores of all six social dimensions. Scores of 1–80 indicate low stigma, 81–160 represent moderate stigma, and scores equal to or above 161 suggest high stigma. The PSS-IBD has been proved to have adequate reliability in American and Chinese patients with IBD (Cronbach's alpha = 0.89 and 0.96, respectively) (23, 37).
The Resilience Scale for Patients with Inflammatory Bowel Disease (RS-IBD) is a specific resilience instrument for patients with IBD developed in China (38). The RS-IBD includes 25 items that are classified into six dimensions. Each item is scored on a five-point scale ranging from 1 (not true at all) to 5 (true all the time), with higher scores suggesting higher resilience. The RS-IBD was reported to have adequate reliability and construct validity in Chinese people with IBD (38).
Quality of life was assessed using the Inflammatory Bowel Disease Questionnaire (IBDQ), a 32 items instrument developed in Canada (39). The IBDQ comprises four dimensions: bowel symptoms, systemic symptoms, emotional function, and social function. The IBDQ rated on a seven-point Likert scale, ranging from 1 to 7. The scale's total score can be calculated by summing the scores of all dimensions, with higher scores indicating better QOL. The Chinese version of the IBDQ was reported to exhibit adequate internal consistency reliability (Cronbach's alpha, 0.95), split-half reliability (0.90), and construct validity (four factors accounted for 60.99% of the variation) (40).
For UC, the disease activity was assessed by modified Truelove and Witts' Severity Index (41, 42). Truelove and Witts' Severity Index involves the number of bloody stools per day, body temperature, pulse, hemoglobin, and erythrocyte sedimentation rate. Patients with UC stratified as having four scores or less were regarded as being in remission, while those with four or more were in the active stage. We adopted the Harvey Bradshaw Simple Index to assess the disease activity of CD. This scale is widely used in clinical practice and scientific research (41, 43). It comprises five aspects: overall well-being, the severity of abdominal pain, the daily number of liquid stools, abdominal lumps, and complications. Patients with CD categorized as having four scores or less were regarded as being in remission, while those with four or more were considered with active disease.
Statistical analyses were performed using IBM SPSS 20.0 for Windows (IBM Corp., Armonk, NY, USA). In this cross-sectional study, descriptive statistics were computed for all study variables. Before the analysis, the Kolmogorov-Smirnov test was used to determine whether the numeric variables showed a normal distribution. Next, the t-test and analysis of variance (ANOVA) were applied to compare the QOL among patients with different sociodemographic and clinical characteristics. The relationships between perceived stigma, resilience, and QOL were assessed utilizing Pearson's bivariate Correlation. Finally, we performed a bias-corrected bootstrapping analysis (with 5000 resamples) using the SPSS macro–PROCESS Model 4 to verify the mediating effects of resilience. The mediating effect was considered statistically significant if the 95% bootstrap confidence interval did not contain zero (44). Sub-group analysis was performed based on disease activity (remission vs. active disease). The interactions of disease activity and perceived stigma and resilience were also explored. All statistical tests were performed at a 0.05 level of significance.
The final sample consisted of 311 patients with IBD. Their mean age was 33.70 ± 11.62 (mean ± standard deviation) years, and 57.6% were men. Nearly half of the participants (42.7%) had a higher education level, and 224 participants (72.0%) lived in the cities. Seventy-nine patients (25.4%) were divorced, and 149 patients (47.9%) were married. More than half of the sample (60.1%) had an annual household income of 50,000 Yuan or more. On disease type, 69.5% of patients were diagnosed with CD. The mean duration time since diagnosis was 3.51 ± 1.04 years. Most of them (67.2%) were in remission (Table 1).
Quality of life did not differ significantly among patients of different ages, gender, education level, or disease duration groups. However, there were differences related to marital status, residence, income, disease type, and disease activity (all P <0.05). The details of participants' characteristics and differences in quality of life were summarized in Table 1.
The mean score for perceived stigma was 71.60 ± 18.73, with 38.9% of the participants having scores above the criterion score of 80 for moderate stigma. The mean score for resilience was 95.63 ± 15.57 of 125. In terms of QOL, the mean score was 139.01 ± 21.13. The subscale of bowel symptoms had the highest mean score of the items (5.50), followed by emotional function (5.20), social function (5.16), and systemic symptoms (4.87).
Table 2 presents the results of bivariate analyses. Significant correlation was found between perceived stigma and resilience (r = −0.326, P < 0.01). All subscales of QOL were found to be negatively associated with perceived stigma but positively correlated with resilience. Moreover, patients who reported moderate or severe stigma had significantly lower scores in QOL compared with those who reported mild stigma (See detail in Table 3).
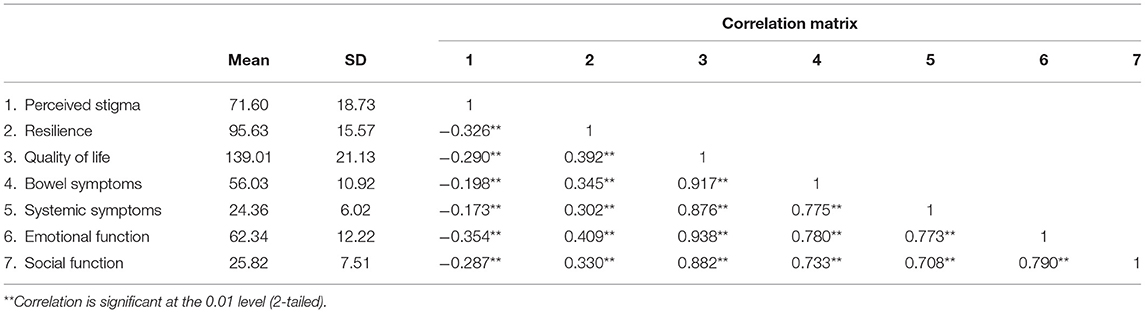
Table 2. Levels and association of patients' quality of life with perceived stigma and resilience (N = 311).
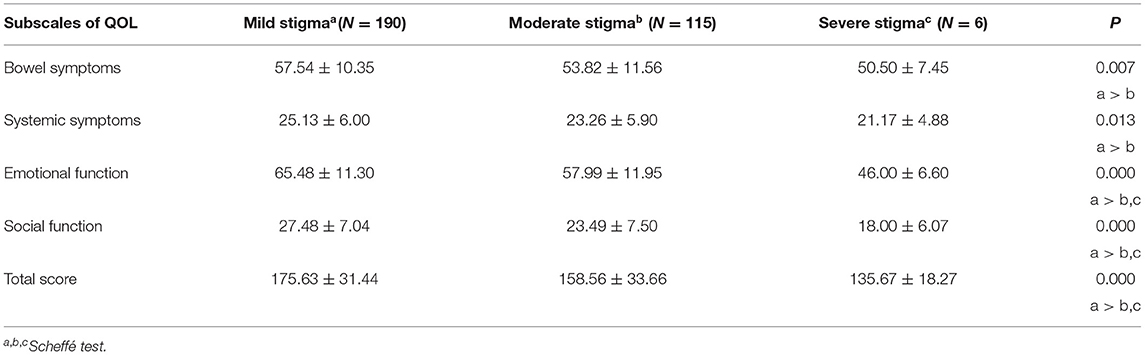
Table 3. Comparison of quality of life between the patients with mild, moderate and severe perceived stigma (N = 311).
We used “Model 4” in the PROCESS macro to test the mediating effect of resilience on the association between perceived stigma and QOL. Quality of life varied significantly depending on marital status, residence, income, disease type, and disease activity (Table 1). Therefore, those five variables were dummy coded and assigned as covariates in the test.
As seen in Table 4, the total effect of perceived stigma on all aspects of QOL were significant [bowel symptoms (β = −0.052, SE = 0.014, P = 0.000), systemic symptoms (β = −0.025, SE = 0.008, P = 0.002), emotional function (β = −0.109, SE = 0.016, P = 0.000), and social function (β = −0.052, SE = 0.010, P = 0.000)].
Figure 2 shows the mediation model. The paths from perceived stigma through resilience to all aspects of QOL were significant. These included the products of the path from perceived stigma to resilience (P = 0.000) and the path from resilience to bowel symptoms (P = 0.000), systemic symptoms (P = 0.000), emotional function (P = 0.001) and social function (P = 0.000). Although perceived stigma had no direct effects on bowel symptoms and systemic symptoms, it directly affected emotional function and social function.
The result from bias-corrected bootstrapping indicated a significant indirect effect from perceived stigma to resilience to all aspects of QOL [bowel symptoms (β = −0.026, SEBoot = 0.007, 95%CI: −0.041, −0.014), systemic symptoms (β = −0.014, SEBoot = 0.004, 95%CI: −0.023, −0.007), emotional function (β = −0.033, SEBoot = 0.009, 95%CI: −0.053, −0.018), and social function (β = −0.016, SEBoot = 0.005, 95% CI: −0.026,−0.008)]. Therefore, resilience was found to mediate the relationship between perceived stigma and QOL.
In subgroup analysis stratified by disease activity, the perceived stigma was significantly negatively associated with QOL in both remission group (β = −0.304, t = −4.598, P = 0.000) and active disease group (β = −0.288, t = −3.005, P = 0.003), Pperceivedstigma−interaction = 0.425. Moreover, the resilience was significantly positively associated with QOL in both remission group (β = 0.401, t = 6.295, P = 0.000) and active disease group (β = 0.210, t = 3.811, P = 0.000), Presilience−interaction = 0.639.
The main finding of the present study was that resilience could mediate the effect of perceived stigma on QOL in patients with IBD after statistically controlling for marital status, residence, income, disease type, and disease activity. In other words, perceived stigma might impair an individual's resilience and subsequently influenced QOL. Therefore, perceived stigma and resilience should be considered significant psychosocial variables in promoting QOL among patients with IBD.
This study revealed that the perceived stigma directly affected the emotional function and social function dimensions of QOL. Consistent with this finding, Gamwell et al. observed that more significant perceived stigma directly aggravated depressive symptoms and weakened the bonds between youth with IBD and society (45). Patients with IBD tend to perceive illness-related stigma because of public misconceptions about etiology, variability in course, and fear of incontinence, which leads to concealment and social withdrawal (22, 46). The concealment of disease could probably decrease communication and connections with others, increasing feelings of isolation and depression (47). However, since not all patients perceived stigma had a poor QOL, some authors pointed out that additional factors should be considered when explaining how psychosocial burden exerts adverse effects. Similar to earlier conclusions, we illustrated that resilience played a mediating role in the associations between perceived stigma and emotional and social function (48, 49). Resilience could help individuals adopt positive coping strategies (disclosure and seeking support) to maintain good psychosocial function (34). Higher levels of resilience are reportedly associated with fewer negative emotions and better interpersonal communication (15, 16, 50). In terms of neuro mechanisms, resilience could invoke specific brain structures and neural circuits, prompting the individual to regulate emotion and engage in prosocial behavior (17, 18).
Although we failed to find direct associations between perceived stigma and bowel symptoms and systematic symptoms dimensions of QOL, perceived stigma affected the bowel and systematic symptoms by reducing resilience. Resilience is a positive predictor of self-management in patients with chronic diseases (51, 52). Resilient patients are prone to adopt more self-management behaviors to achieve disease control (53, 54). Mediating effects between psychosocial burden and physical outcomes have been shown for various positive personality traits. Cherrington et al. reported that self-efficacy played an intermediary role in the path from depression to glycemic control in male diabetic patients (55). In a cross-sectional study conducted in patients with colorectal cancer, the variance anxiety accounted for preoperative insomnia increased after adding self-esteem to the hierarchical regression model (56). Resilience as a mediator of the association between perceived stigma and bowel and systematic symptoms has never been reported. Still, it is plausible considering that self-efficacy and self-esteem are integral parts of resilience (54). In other aspects, earlier studies demonstrated that perceived stigma was a prominent risk factor of depression and anxiety, especially for people with low resilience (49, 57, 58). The physiological mechanism of microbiota-brain-gut axis regulation could clarify how psychosocial burden can aggravate bowel and systematic symptoms in patients with IBD (59). The microbiota-brain-gut axis involved the central systems, autonomic nervous systems, endocrine system, immune system, and intestinal microenvironment. Stress responses caused by psychological disorders might activate the microbiota-brain-gut axis and further bring about altered gastrointestinal physiology, resulting in bowel and systematic symptoms (59, 60). These previous studies supported our current findings that resilience played a mediating role between perceived stigma and somatic symptoms.
Several limitations should be noted in the present study. Firstly, our study adopted a cross-sectional design, which could not confirm the causal associations between study variables. The effects of perceived stigma and resilience on QOL should be investigated and verified in more prospective studies to provide more reliable evidence. Secondly, the findings of this study should be generalized with caution because the sample in this study was mainly based on no-random participation. Random sampling could be considered in future research to confirm the findings of this study. Thirdly, except for the questionnaires measuring disease activity index, most questionnaires used in this survey, including PSS-IBD, RS-IBD, and IBDQ, came from the patients' self-reports which have subjectivities and thus easy to cause measure bias. In addition, we only included 95 patients with UC, which was insufficient to perform a subgroup analysis to determine the stability of the model in different disease types. Furthermore, the potential psychosocial mediating variables (such as self-esteem, mastery, and optimism), which are essential components of resilience, have not been analyzed. Last but not least, although CD and UC account for approximately 90% of IBD cases, there exist some patients with indeterminate colitis (1). This study only recruited patients with UC and CD. Despite the above limitations, the results presented here have significant implications. We tested the hypothesis that perceived stigma negatively affected QOL in patients with IBD and indirectly predicted QOL through resilience. The contribution of this study is to demonstrate the mediating effect of resilience on perceived stigma and QOL, which can add to the previous literature a potential mechanism whereby perceived stigma affects QOL. These findings implied that integrating intervention techniques to target resilience into the QOL improvement program of individuals with perceived stigma is feasible. There exist some resilience-enhancing programs for patients with chronic disease, such as the Be Resilient to Breast Cancer (BRBC) and Mindfulness-Based Stress Reduction (MBSR) (61, 62). Cognitive reframing is regarded as the active ingredient of resilience interventions (29). Lillis and his colleague adopted positive cognitive reframing strategies to interfere with obesity-related stigma (63). They found that the intervention group compared to the control group showed more significant mitigation of obesity-related stigma and improvement in QQL. Moreover, Kumpfer KL et al. suggested that the environmental resources (such as family and peer support) can promote resilience to help individuals positively cope with stressful events (64). A peer-led group program performed in adolescents with mental illness displayed a significant effect post-intervention, including reduced stigma stress and increased QOL (65). Therefore, resilience-oriented interventions that deliver disease knowledge and train interpersonal skills can be given to family members, peers, and coworkers of patients with IBD to increase social support and reduce perceived stigma (22, 66). As applied to clinical care, we recommend that healthcare providers incorporate perceived stigma and resilience assessment in patients' psychological screening and include cognitive reframing and support promotion in QOL improvement programs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Ethics Committee of the First Affiliated Hospital of Nanjing Medical University approved all study procedures (no. 2019-SRFA-122). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
DL and MZ designed the study, enrolled participants, analyzed and interpreted the data, and wrote the manuscript. LS, QB, ML, and SR were responsible for collecting data. ZL supervised this research project. All authors contributed to the article and approved the submitted version.
This work was supported by a grant from the Foundation of 333High-level personnel training Project from the Department of Science and Technology of Jiangsu Province (BRA2020069); Jiangsu Provincial Medical Innovation Team (CXTDA2017019); Priority Discipline Development Program of Jiangsu Higher Education Institutions from the General Office of the People's Government of Jiangsu Province (2018 No. 87); Clinical ability improvement project from The First Affiliated Hospital of Nanjing Medical University (JSPH-NB-2020-1).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Alatab S, Sepanlou SG, Ikuta K, Vahedi H, Bisignano C, Safiri S, et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. (2020) 5:17–30. doi: 10.1016/S2468-1253(19)30333-4
2. Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn's Disease 2016: Part 1: Diagnosis and Medical Management. J Crohns Colitis. (2017) 11:3–25. doi: 10.1093/ecco-jcc/jjw168
3. Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and Ileo-anal pouch disorders. J Crohns Colitis. (2017) 11:649–70. doi: 10.1093/ecco-jcc/jjx008
4. Duff W, Haskey N, Potter G, Alcorn J, Hunter P, Fowler S. Non-pharmacological therapies for inflammatory bowel disease: Recommendations for self-care and physician guidance. World J Gastroenterol. (2018) 24:3055–70. doi: 10.3748/wjg.v24.i28.3055
5. Tsai L, Ma C, Dulai PS, Prokop LJ, Eisenstein S, Ramamoorthy SL, et al. Contemporary risk of surgery in patients with ulcerative colitis and crohn's disease: a meta-analysis of population-based Cohorts. Clin Gastroenterol Hepatol. (2020). doi: 10.1016/j.cgh.2020.10.039. [Epub ahead of print].
6. Williet N, Sandborn WJ, Peyrin-Biroulet L. Patient-reported outcomes as primary end points in clinical trials of inflammatory bowel disease. Clin Gastroenterol Hepatol. (2014) 12:1246–56. e6. doi: 10.1016/j.cgh.2014.02.016
7. Alrubaiy L, Rikaby I, Dodds P, Hutchings HA, Williams JG. Systematic review of health-related quality of life measures for inflammatory bowel disease. J Crohns Colitis. (2015) 9:284–92. doi: 10.1093/ecco-jcc/jjv002
8. Serafini G, Canepa G, Adavastro G, Nebbia J, Belvederi Murri M, Erbuto D, et al. The relationship between childhood maltreatment and non-suicidal self-injury: a systematic review. Front Psychiatry. (2017) 8:149. doi: 10.3389/fpsyt.2017.00149
9. Serafini G, Gonda X, Pompili M, Rihmer Z, Amore M, Engel-Yeger B. The relationship between sensory processing patterns, alexithymia, traumatic childhood experiences, and quality of life among patients with unipolar and bipolar disorders. Child Abuse Negl. (2016) 62:39–50. doi: 10.1016/j.chiabu.2016.09.013
10. Liu R, Tang A, Wang X, Shen S. Assessment of Quality of Life in Chinese Patients With Inflammatory Bowel Disease and their Caregivers. Inflamm Bowel Dis. (2018) 24:2039–47. doi: 10.1093/ibd/izy099
11. Gracie DJ, Hamlin JP, Ford AC. Longitudinal impact of IBS-type symptoms on disease activity, healthcare utilization, psychological health, and quality of life in inflammatory bowel disease. Am J Gastroenterol. (2018) 113:702–12. doi: 10.1038/s41395-018-0021-z
12. Casellas F, Arenas JI, Baudet JS, Fábregas S, García N, Gelabert J, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis. (2005) 11:488–96. doi: 10.1097/01.MIB.0000159661.55028.56
13. Knowles SR, Graff LA, Wilding H, Hewitt C, Keefer L, Mikocka-Walus A. Quality of Life in Inflammatory Bowel Disease: A Systematic Review and Meta-analyses-Part I. Inflamm Bowel Dis. (2018) 24:742–51. doi: 10.1093/ibd/izx100
14. Zhao M, Gönczi L, Lakatos PL, Burisch J. The burden of inflammatory bowel disease in Europe in 2020. J Crohns Colitis. (2021) doi: 10.1093/ecco-jcc/jjab029. [Epub ahead of print].
15. Bellido-González M, Robles-Ortega H, Castelar-Ríos MJ, Díaz-López M, Gallo-Vallejo JL, Moreno-Galdó MF, et al. Psychological distress and resilience of mothers and fathers with respect to the neurobehavioral performance of small-for-gestational-age newborns. Health Qual Life Outcomes. (2019) 17:54. doi: 10.1186/s12955-019-1119-8
16. Ungar M, Theron L. Resilience and mental health: how multisystemic processes contribute to positive outcomes. Lancet Psychiatry. (2020) 7:441–8. doi: 10.1016/S2215-0366(19)30434-1
17. van der Werff SJ, van den Berg SM, Pannekoek JN, Elzinga BM, van der Wee NJ. Neuroimaging resilience to stress: a review. Front Behav Neurosci. (2013) 7:39. doi: 10.3389/fnbeh.2013.00039
18. Haglund ME, Nestadt PS, Cooper NS, Southwick SM, Charney DS. Psychobiological mechanisms of resilience: relevance to prevention and treatment of stress-related psychopathology. Dev Psychopathol. (2007) 19:889–920. doi: 10.1017/S0954579407000430
19. Sweeney L, Moss-Morris R, Czuber-Dochan W, Murrells T, Norton C. Developing a better biopsychosocial understanding of pain in inflammatory bowel disease: a cross-sectional study. Eur J Gastroenterol Hepatol. (2020) 32:335–44. doi: 10.1097/MEG.0000000000001615
20. Kim SY, Kim JM, Kim SW, Kang HJ, Lee JY, Bae KY, et al. Perceived Stigma and Quality of Life in Patients Following Recovery From Delirium. J Clin Psychiatry. (2017) 78: e744–e749. doi: 10.4088/JCP.16m11076
21. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
22. Taft TH, Keefer L. A systematic review of disease-related stigmatization in patients living with inflammatory bowel disease. Clin Exp Gastroenterol. (2016) 9:49–58. doi: 10.2147/CEG.S83533
23. Taft TH, Keefer L, Leonhard C, Nealon-Woods M. Impact of perceived stigma on inflammatory bowel disease patient outcomes. Inflamm Bowel Dis. (2009) 15:1224–32. doi: 10.1002/ibd.20864
24. Degnan A, Berry K, Humphrey C, Bucci S. The relationship between stigma and subjective quality of life in psychosis: A systematic review and meta-analysis. Clin Psychol Rev. (2021) 85:102003. doi: 10.1016/j.cpr.2021.102003
25. Shi Y, Wang S, Ying J, Zhang M, Liu P, Zhang H, et al. Correlates of perceived stigma for people living with epilepsy: A meta-analysis. Epilepsy Behav. (2017) 70:198–203. doi: 10.1016/j.yebeh.2017.02.022
26. Wu X, Chen J, Huang H, Liu Z, Li X, Wang H. Perceived stigma, medical social support and quality of life among people living with HIV/AIDS in Hunan, China. Appl Nurs Res. (2015) 28:169–74. doi: 10.1016/j.apnr.2014.09.011
27. Ammirati RJ, Lamis DA, Campos PE, Farber EW. Optimism, well-being, and perceived stigma in individuals living with HIV. AIDS Care. (2015) 27:926–33. doi: 10.1080/09540121.2015.1018863
28. Vodermaier A, Esplen MJ, Maheu C. Can self-esteem, mastery and perceived stigma predict long-term adjustment in women carrying a BRCA1/2-mutation? Evidence from a multi-center study. Fam Cancer. (2010) 9:305–11. doi: 10.1007/s10689-010-9325-x
29. Kim GM, Lim JY, Kim EJ, Park SM. Resilience of patients with chronic diseases: a systematic review. Health Soc Care Community. (2019) 27:797–807. doi: 10.1111/hsc.12620
30. Lenti MV, Cococcia S, Ghorayeb J, Di Sabatino A, Selinger CP. Stigmatisation and resilience in inflammatory bowel disease. Intern Emerg Med. (2020) 15:211–23. doi: 10.1007/s11739-019-02268-0
31. Liu Z, Zhou X, Zhang W, Zhou L. Factors associated with quality of life early after ischemic stroke: the role of resilience. Top Stroke Rehabil. (2019) 26:335–41. doi: 10.1080/10749357.2019.1600285
32. Sehgal P, Ungaro RC, Foltz C, Iacoviello B, Dubinsky MC, Keefer L. High levels of psychological resilience associated with less disease activity, better quality of life, and fewer surgeries in inflammatory bowel disease. Inflamm Bowel Dis. (2020) 27:791–6. doi: 10.1093/ibd/izaa196
33. Taylor K, Scruggs PW, Balemba OB, Wiest MM, Vella CA. Associations between physical activity, resilience, and quality of life in people with inflammatory bowel disease. Eur J Appl Physiol. (2018) 118:829–36. doi: 10.1007/s00421-018-3817-z
34. Dibley L, Norton C, Whitehead E. The experience of stigma in inflammatory bowel disease: An interpretive (hermeneutic) phenomenological study. J Adv Nurs. (2018) 74:838–51. doi: 10.1111/jan.13492
35. Kawi J, Reyes AT, Arenas RA. Exploring Pain Management Among Asian Immigrants with Chronic Pain: Self-Management and Resilience. J Immigr Minor Health. (2019) 21:1123–36. doi: 10.1007/s10903-018-0820-8
36. Hsiung PC, Pan AW, Liu SK, Chen SC, Peng SY, Chung L. Mastery and stigma in predicting the subjective quality of life of patients with schizophrenia in Taiwan. J Nerv Ment Dis. (2010) 198:494–500. doi: 10.1097/NMD.0b013e3181e4d310
37. Luo D, Lin Z, Bian Q, Xu N, Wang M. Perceived stigma in patients with inflammatory bowel disease and its effect on psychology, medication compliance and quality of life. Chin J Nurs. (2018) 53:1078–83. doi: 10.3761/j.issn.0254-1769.2018.09.012
38. Luo D, Lin Z, Bian Q, Xu N, Wang M. Development and structure exploration of inflammatory bowel disease dominance and toughness scale. Chin J Prac Nurs. (2018) 34:1623–7. doi: 10.3760/cma.j.issn.1672-7088.2018.21.005
39. Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. (1989) 96:804–10. doi: 10.1016/0016-5085(89)90905-0
40. Zhou W, You L, Li Y, Chen B. The reliability and validity of inflammatory bowel diseases questionnaire in Chinese version. Int J Nurs. (2006) 25:620–22. doi: 10.3760/cma.j.issn.1673-4351.2006.08.020
41. Walsh AJ, Bryant RV, Travis SP. Current best practice for disease activity assessment in IBD. Nat Rev Gastroenterol Hepatol. (2016) 13:567–79. doi: 10.1038/nrgastro.2016.128
42. Truelove SC, Witts LJ. Cortisone in ulcerative colitis. Br Med J. (1955) 2:1041–8. doi: 10.1136/bmj.2.4947.1041
43. Harvey RF, Bradshaw JM. A simple index of Crohn's-disease activity. Lancet. (1980) 1:514. doi: 10.1016/S0140-6736(80)92767-1
44. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications (2017).
45. Gamwell KL, Baudino MN, Bakula DM, Sharkey CM, Roberts CM, Grunow JE, et al. Perceived illness stigma, thwarted belongingness, and depressive symptoms in youth with inflammatory bowel disease (IBD). Inflamm Bowel Dis. (2018) 24:960–5. doi: 10.1093/ibd/izy011
46. Barned C, Stinzi A, Mack D, O'Doherty KC. To tell or not to tell: A qualitative interview study on disclosure decisions among children with inflammatory bowel disease. Soc Sci Med. (2016) 162:115–23. doi: 10.1016/j.socscimed.2016.06.023
47. Guo L, Rohde J, Farraye FA. Stigma and disclosure in patients with inflammatory bowel disease. Inflamm Bowel Dis. (2020) 26:1010–6. doi: 10.1093/ibd/izz260
48. Galderisi S, Rossi A, Rocca P, Bertolino A, Mucci A, Bucci P, et al. Pathways to functional outcome in subjects with schizophrenia living in the community and their unaffected first-degree relatives. Schizophr Res. (2016) 175:154–60. doi: 10.1016/j.schres.2016.04.043
49. Yan H, Li X, Li J, Wang W, Yang Y, Yao X, et al. Association between perceived HIV stigma, social support, resilience, self-esteem, and depressive symptoms among HIV-positive men who have sex with men (MSM) in Nanjing, China. AIDS Care. (2019) 31:1069–76. doi: 10.1080/09540121.2019.1601677
50. Ma X, Wang Y, Hu H, Tao XG, Zhang Y, Shi H. The impact of resilience on prenatal anxiety and depression among pregnant women in Shanghai. J Affect Disord. (2019) 250:57–64. doi: 10.1016/j.jad.2019.02.058
51. Verma T, Rohan J. Examination of transition readiness, medication adherence, and resilience in pediatric chronic illness populations: a pilot study. Int J Environ Res Public Health. (2020) 17:1905. doi: 10.3390/ijerph17061905
52. Ogilvie R, Foster K, McCloughen A, Curtis K. Young peoples' experience and self-management in the six months following major injury: a qualitative study. Injury. (2015) 46:1841–7. doi: 10.1016/j.injury.2015.05.036
53. Hadj-Abo A, Enge S, Rose J, Kunte H, Fleischhauer M. Individual differences in impulsivity and need for cognition as potential risk or resilience factors of diabetes self-management and glycemic control. PLoS ONE. (2020) 15:e0227995. doi: 10.1371/journal.pone.0227995
54. Luo D, Xu JJ, Cai X, Zhu M, Wang H, Yan D, et al. The effects of family functioning and resilience on self-management and glycaemic control among youth with type 1 diabetes. J Clin Nurs. (2019) 28:4478–87. doi: 10.1111/jocn.15033
55. Cherrington A, Wallston KA, Rothman RL. Exploring the relationship between diabetes self-efficacy, depressive symptoms, and glycemic control among men and women with type 2 diabetes. J Behav Med. (2010) 33:81–9. doi: 10.1007/s10865-009-9233-4
56. Sun GW, Yang YL, Yang XB, Wang YY, Cui XJ, Liu Y, et al. Preoperative insomnia and its association with psychological factors, pain and anxiety in Chinese colorectal cancer patients. Support Care Cancer. (2020) 28:2911–9. doi: 10.1007/s00520-019-05151-y
57. Cantwell J, Muldoon O, Gallagher S. The influence of self-esteem and social support on the relationship between stigma and depressive symptomology in parents caring for children with intellectual disabilities. J Intellect Disabil Res. (2015) 59:948–57. doi: 10.1111/jir.12205
58. Birtel MD, Wood L, Kempa NJ. Stigma and social support in substance abuse: Implications for mental health and well-being. Psychiatry Res. (2017) 252:1–8. doi: 10.1016/j.psychres.2017.01.097
59. Gracie DJ, Hamlin PJ, Ford AC. The influence of the brain-gut axis in inflammatory bowel disease and possible implications for treatment. Lancet Gastroenterol Hepatol. (2019) 4:632–42. doi: 10.1016/S2468-1253(19)30089-5
60. Sgambato D, Miranda A, Ranaldo R, Federico A, Romano M. The Role of Stress in Inflammatory Bowel Diseases. Curr Pharm Des. (2017) 23:3997–4002. doi: 10.2174/1381612823666170228123357
61. Ye ZJ, Liang MZ, Qiu HZ, Liu ML, Hu GY, Zhu YF, et al. Effect of a multidiscipline mentor-based program, Be Resilient to Breast Cancer (BRBC), on female breast cancer survivors in mainland China-A randomized, controlled, theoretically-derived intervention trial. Breast Cancer Res Treat. (2016) 158:509–22. doi: 10.1007/s10549-016-3881-1
62. Kovacs AH, Bandyopadhyay M, Grace SL, Kentner AC, Nolan RP, Silversides CK, et al. Adult Congenital Heart Disease-Coping And REsilience (ACHD-CARE): Rationale and methodology of a pilot randomized controlled trial. Contemp Clin Trials. (2015) 45:385–93. doi: 10.1016/j.cct.2015.11.002
63. Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med. (2009) 37:58–69. doi: 10.1007/s12160-009-9083-x
64. Kumfer KL. Factors and processes contributing to resilience: the resilience framework. In: Glantz MD, Johnson JL, editor. Resilience and Development: Positive Life Adaptation. FL: Kluwer Academic (1999). p. 179–224.
65. Mulfinger N, Müller S, Böge I, Sakar V, Corrigan PW, Evans-Lacko S, et al. Honest, Open, Proud for adolescents with mental illness: pilot randomized controlled trial. J Child Psychol Psychiatry. (2018) 59:684–91. doi: 10.1111/jcpp.12853
Keywords: resilience, perceived stigma, quality of life, mediating effect, inflammatory bowel disease
Citation: Luo D, Zhou M, Sun L, Lin Z, Bian Q, Liu M and Ren S (2021) Resilience as a Mediator of the Association Between Perceived Stigma and Quality of Life Among People With Inflammatory Bowel Disease. Front. Psychiatry 12:709295. doi: 10.3389/fpsyt.2021.709295
Received: 13 May 2021; Accepted: 12 July 2021;
Published: 06 August 2021.
Edited by:
Zeng-Jie Ye, Guangzhou University of Chinese Medicine, ChinaReviewed by:
Louise Sweeney, King's College London, United KingdomCopyright © 2021 Luo, Zhou, Sun, Lin, Bian, Liu and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng Lin, bGluemhlbmcxMDBAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.