- 1Department of Psychology, Virginia Commonwealth University, Richmond, VA, United States
- 2Department of Psychiatry, University of Michigan, Ann Arbor, MI, United States
The purpose of this study was to examine if personality traits can be used to characterize subgroups of youth diagnosed with childhood-onset conduct disorder (CD). Participants were 11,552 youth from the Adolescent Brain Cognitive Development study. Data used in this report came from doi: 10.15154/1504041 (M age 9.92; 45.3% female, 49.6% white, 19.0% Hispanic). A subset of this sample (n = 365) met criteria for CD. Latent profile analyses (LPA) were performed on this subgroup (n = 365) to define profiles of individuals with CD based on self-report measures of impulsivity, punishment sensitivity, reward response, and callous-unemotional traits. Follow up analyses determined if these groups differed on clinically relevant variables including psychopathology, environmental risk factors, social risk factors, and neurocognitive functioning. Participants with a CD diagnosis scored significantly higher on psychological, environmental, social, and neurocognitive risk factors. The LPA revealed three unique profiles, which differed significantly on liability for broad psychopathology and domain-specific liability for externalizing psychopathology but were largely matched on environmental and social risk factors. These unique configurations provide a useful way to further parse clinically relevant subgroups within youth who meet criteria for childhood-onset CD, setting the stage for prospective longitudinal research using these latent profiles to better understand the development of youth with childhood-onset CD.
Introduction
Conduct disorder (CD) is a set of serious emotional and behavioral problems that manifests in children and adolescents, characterized by repetitive and persistent patterns of antisocial and rule-breaking behavior. Individuals with childhood-onset CD represent a particularly high-risk group as they are more likely to have a persistent life course of CD and chronic antisocial behaviors compared to adolescent-onset subtypes (1). Childhood-onset CD is also associated with a number of unique risk factors, including comorbid psychopathology and environmental influences [for review, see (2)]. However, there is evidence that a significant number of youth with childhood-onset CD desist from antisocial behavior by early adulthood (3), suggesting that age of onset alone still designates a relatively heterogeneous group. Additional factors such as callous-unemotional (CU) traits, impulsivity, and reactivity to punishment and reward have also been shown to designate subgroups of children with CD (4–7), indicating that these traits may further clarify the heterogeneity within this high-risk group. Therefore, the current study utilized person-centered analyses in a large, diverse sample of emerging adolescents to determine if individual differences in relevant traits can define clinically meaningful subgroups of youth with childhood-onset CD.
Research on CD has focused on age of onset as one way to predict severity and recidivism. Seminal work has supported the distinction between a childhood-onset CD group, who begin showing conduct problems as early as preschool or early elementary school (8), and an adolescent-onset CD group, who begin displaying antisocial behavior with the onset of puberty (1). Research on the outcomes of these two subtypes of CD indicates that individuals with childhood-onset are more likely to continue showing antisocial behaviors into adolescence and adulthood relative to those whose behavior onsets in adolescence and are more likely to desist in adulthood (9). Childhood-onset CD is thought to reflect a more severe condition, potentially influenced by genetic predispositions, neuropsychological deficits, and exacerbated by childhood familial risk factors (e.g., parental psychopathology, family conflict) (1, 9). While the age of symptom onset is clinically relevant, the designation does not necessarily define a homogeneous group. Therefore, additional information regarding where these youth fall on relevant personality traits may inform our understanding of heterogeneity within this diagnosis.
Three relevant personality domains that may further define heterogeneity within youth diagnosed with childhood-onset CD are impulsivity, CU traits, and sensitivity to punishment and reward. There are well-established links between childhood-onset CD symptoms and greater trait impulsivity, manifesting in comorbid diagnosis of ADHD (10–14). Youth diagnosed with childhood-onset CD have higher rates of comorbid ADHD compared to those with adolescent-onset CD (15, 16) and the presence of a comorbid ADHD diagnosis predicts the persistence of antisocial behavior into adulthood (16). These findings suggest that the presence of higher levels of trait impulsivity reflect a greater risk for persistent antisocial behavior and may serve to further differentiate a high-risk group of youth.
CU traits are another personality feature that is known to increase risk for persistent antisocial behavior in youth. High levels of CU traits are exhibited by a subset of youth who meet criteria for CD (designated by the Limited Prosocial Emotions specifier in DSM-5) (17, 18). Researchers have found that youth high in CU traits have a more severe and stable trajectory of problem behavior (19–21) but also may have less anxiety, fearfulness, and sensitivity to punishment (22). Consistent with broader research on psychopathy in adults (23, 24), previous work suggests that, although impulsivity and CU traits are often correlated, these personality dimensions are dissociable and can be thought of as distinct pathways that lead to CD symptoms in youth (25–28). Research suggests that heightened levels of CU traits designate a significantly more severe group of youth, even among those who meet criteria for childhood-onset CD suggesting that level of CU traits is a clinically relevant dimension to quantify even among youth with childhood-onset CD (29, 30). Therefore, impulsive and CU traits represent two dimensions that, through different configurations, could produce different clinical outcomes for youth with a CD diagnosis.
Altered sensitivity to reward and punishment, constructs that also are particularly relevant to broader research on antisocial behavior (31, 32), have likewise been linked to CD. Specifically, research has found that youth who display CD symptoms have heightened sensitivity to reward and reduced sensitivity to punishment (33–37), with some evidence to suggest this is more pronounced in youth with childhood-onset CD (38), although inferences about the former have been somewhat inconsistent between samples and measurement modalities (39). Despite these findings, researchers have also found evidence for a subgroup of youth with CD and co-morbid anxiety disorders (i.e., psychopathology marked by hyperreactivity to threat and punishment) who demonstrate more antisocial behaviors relative to those without co-occurring internalizing psychopathology (40). Therefore, trait sensitivities to reward and punishment represent another two dimensions whereon an individual might differ but still meet criteria for CD. As these traits are closely linked to distinct neural and biological systems (31, 41, 42), determining how they co-occur could be informative for understanding the etiologic pathways to early expression of CD.
Taken together, this work demonstrates that an array of personality dimensions contribute to the early emergence of CD in youth. Latent profile analysis [LPA; (43)] uses individual data points to determine heterogeneity (i.e., different classes) among participants. While variable centered approaches such as confirmatory factor analyses use multiple variables to reduce the dimensionality of data and find homogeneity, LPA uses indicator variables to determine heterogeneity (i.e., different class membership) among participants. This analytic approach is particularly useful when there is evidence that considerable variance within each indicator variable is present, uncovering subgroups that simple group averages may fail to capture. LPA has been used to characterize heterogeneity in children with ADHD (44, 45) and in relation to other behaviors including substance use (46). The use of LPA to determine person-specific processes in CD, including the formation of meaningful subgroups through dimensional interactions, has yet to be explored. One likely reason for this limitation is that LPA often require considerably larger sample sizes than those typically present in the CD literature (47). While CD has a relatively low rate of diagnosis [lifetime prevalence of 9.5%; (48)], data from the Adolescent Brain Cognitive Development (ABCD) study are uniquely well-suited to examine subgroups within this diagnosis due to the large overall sample size and comprehensive assessments of participants and their parents.
The current study sought to first determine the trait profile of youth diagnosed with childhood-onset CD (CD+). Given that this disorder is defined by impulsive, unconstrained behavior, we hypothesized that individuals meeting criteria for childhood-onset CD would have significantly higher rates of impulsivity, lower responsivity to punishment, higher responsivity to reward, and higher levels of callous traits than the non-CD group (CD-). Given previous research detailing childhood-onset CD (6, 13) we also hypothesized that the CD+ group would have a higher proportion of males, lower levels of socioeconomic advantages (e.g., household income, parental education) and environmental enrichment (e.g., school environment, family conflict), higher rates of general psychopathology, and lower neurocognitive functioning.
Next, we predicted that different trait profiles could be defined using information regarding trait levels of impulsivity, responsivity to reward and punishment, and CU traits. To our knowledge, this is the first study to examine heterogeneity on these traits simultaneously within youth with childhood-onset CD; therefore, there is no previous research defining how these trait profiles might emerge. Based on research describing CU traits as a specifier of a high-risk subtype of CD (17, 20), we surmised that profiles would differ on this variable (i.e., defining a high-CU and low-CU groups). Similarly, previous work has defined a subgroup of youth who meet criteria for CD and also exhibit high levels of internalizing psychopathology (40). Therefore, we predicted that youth would differ on trait indices related to emotional distress and anxiety (i.e., a group high in emotional urgency and enhanced response to punishment).
Based on work examining patterns of psychopathology in emerging adolescence (49), we predicted that CD+ youth would exhibit high levels of both a general liability for broad psychopathology and variance specific to externalizing disorders. We also predicted that these indicators would differ as a function of personality profile, specifically with individuals with a high distress personality profile also scoring high on a broad liability for psychopathology, while a group marked by high levels of CU traits would display greater externalizing psychopathology. Given the exploratory nature of these analyses we did not have strong a priori hypotheses regarding differences in social, environmental, and neurocognitive factors by profiles.
Methods
Participants
The present study used data collected from youth and parents from the ABCD study, a large-scale study of youth aged 9–10 years (N = 11,875), recruited from 21 research sites across the United States (50–52), collected from baseline visits between September 1, 2016 and November 15, 2018 (ABCD Release 2.01, doi: 10.15154/1504041) We removed 323 participants from the analyses owing to non-response on the Kiddie-Structured Assessment for Affective Disorders and Schizophrenia for DSM-5 (KSAD-COMP), which was used to determine CD diagnosis, or grouping variables (Urgency, Premeditation, Perseverance, Sensation-seeking-Positive urgency [UPPS-P], Behavioral Inhibition System/Behavioral Activation System [BIS/BAS], CU traits), leaving a final sample size of 11,552 individuals, with 365 youth meeting criteria for CD. The participants with available data did not differ significantly from the full sample on key demographic variables (sex, race/ethnicity, household income, parental education, and marital status). A single IRB is maintained by the University of California San Diego Human Research Protections Program (160091). All parents provided written informed consent and all children provided assent.
The sample of 11,552 was roughly gender balanced (45.3% female) with a mean age of 9.92 years (SD = 0.62 years). Around half (49.6%) of the sample was white, with the remaining participants identifying themselves as Hispanic (19.0%), Black (14.2%), or Other/Multi-racial (10.4%). Approximately two-thirds of youth (64%) came from households in which the parents were married. Most parents (85.7%) reported an education level of at least some college, and most households reported an annual income of at least $50,000 (61.3%).
Measures
Measures used in the study are described briefly below; however, please refer to the following papers for a more detailed description of the measures used in this study and their psychometric performance in the ABCD sample: personality and mental health (50); culture and environment (53); neurocognition (54).
Selection Variable
The KSAD-COMP is a structured, diagnostic interview that was administered to parents via computer in reference to their child (55). Parents completed all modules of the KSAD-COMP with the exception of the enuresis, encopresis, and selective mutism modules (50). For the purposes of the current study, participants were placed in the CD-positive (CD+) group if they met past or present DSM-5 criteria (e.g., at least three symptoms endorsed in the past 12 months, with at least one criterion present in the past 6 months) for CD at the time of the baseline assessment (age 9–10; e.g., childhood onset; n = 365).
Grouping Variables
A 20-item youth short-version of the UPPS-P scale, developed for use in the ABCD study (50), was administered via self-report at baseline to index trait impulsivity. The UPPS-P has five subscales: Negative Urgency, Positive Urgency, Lack of Perseverance, Lack of Planning, and Sensation Seeking.
The BIS/BAS measure (50, 56) is a 24-item youth-report scale designed to assess three facets of behavioral activation (BAS): Drive (intensity of goal directed behavior), Fun Seeking (spontaneity), and Reward Responsiveness (excitement over reinforcing outcomes), as well as a Behavioral Inhibition (BIS) scale, comprised of items tapping worry and fearfulness, with scores related to sensitivity to punishment as well as avoidance motivation.
A four-item youth-report measure of CU traits was developed to index lack of empathic concern, shallow affect, and low moral regulation within the ABCD study (57). This measure of CU traits was derived from three items (reversed) from the Strengths and Difficulties Questionnaire [SDQ; (58)] and one item from the Child Behavior Checklist [CBCL; (59)]. Scores were computed using a traditional summed score approach. This brief scale demonstrated adequate convergent and discriminant validity both in a subsample of the ABCD study as well as in separate validation samples (57).
Criterion Variables: Family History
Family history of substance problems was computed from ABCD's Family History Assessment (50). A threshold was established for a family member counting as an “affected case” based on the number of serious problems that person has had due to alcohol use and substance use. The following coding was used: 0 = neither parent met the threshold; 1 = at least one parent met threshold.
Family history of psychopathology was computed based on previously published protocols (60, 61). A family history composite score was constructed from responses for ABCD's Family History Assessment (50). Responses for the eight categories of psychopathology problems (e.g., depression, mania, ever psychiatrically hospitalized) were tabulated separately for first-degree relatives (mother, father, full siblings) and second-degree relatives (i.e., everyone else including aunts and uncles, grandparents, etc.). A weighted sum score was computed as follows: first degree cases + 0.5 * second degree cases. This number was then divided by the total possible score for the given subject, given the relations present in their own family tree. These proportion scores were calculated for each category (e.g., depression) and then summed across categories.
Criterion Variables: Dimensional Measures of Psychopathology
The CBCL [age 6–18 form; (59)] is a 119-item parent-report on child psychopathology. A general psychopathology [P-factor; (62, 63)] and orthogonal externalizing (EXT) and internalizing (INT) factors were modeled, and factor scores were used in subsequent analyses. Factor scores were derived by fitting a bifactor model to 8 CBCL scales [Withdrawn, Somatic Complaints, Anxious/Depressed, Social Problems, Thought Problems, Attention Problems, Delinquent Behavior, and Aggressive Behavior; (64)]. In this model there was a general P factor that all scales loaded onto (average scale loading on P = 0.69), and two specific factors: EXT and INT (average scale loading on sub-factors = 0.43). The EXT specific factor included the Delinquent and Aggressive Behaviors scales, while the INT specific factor included the Withdrawn, Somatic Complaints, and Anxious/Depressed scales. This model fit well-based on conventional fit thresholds (χ2 = 747.73, df = 16, p < 0.001; RMSEA = 0.062; CFI = 0.985; TLI = 0.974; SRMR = 0.015) and was chosen for its good model fit and theoretical interpretability (64). For additional information regarding modeling please refer to Clark et al. (64). Associations with the traditional CBCL scales were also included for comparison (see Supplementary Table 1).
Criterion Variables: Social Environment
Youth reported on School Risk and Protective Factors (SRPF) to assess their connection to the school environment (53). This 12-item measure was derived from the PhenX Toolkit, yielding three subscales: a six-item School Environment scale, a four-item School Involvement scale, and a two-item School Disengagement scale.
Both parents and children reported on neighborhood safety and crime, with items from the PhenX Toolkit (53). Parents responded to three statements regarding feelings of safety and presence of crime in their neighborhood, rated on a five-point Likert scale. Youth responded to only one item (“My neighborhood is safe from crime”), rated on the same 5-point Likert scale.
Criterion Variables: Social Functioning
Parent and child both rated the quality of family environment with the Family Conflict subscale from the Family Environment Scale (53). This 9-item measure from the PhenX Toolkit has a binary (true/false) response format to items related to presence of family conflict.
Youth reported on their perceived level of parental monitoring via the Parental Monitoring Survey, a five-item scale that was developed to assess parents efforts to keep track of their child's whereabouts at home as well as outside of the home (53).
Parents reported on their child's prosocial behavior using the Prosocial Behavior Scale, which is a three-item scale formed from the SDQ (65). Youth also responded; however, these three items were used in part to compute the 4-item CU Traits scale and were therefore not evaluated as a criterion variable.
Criterion Variables: Neurocognition
General Cognitive Ability (GCA) scores were computed by fitting a bifactor model to behavioral tasks from the NIH toolbox, the Rey Auditory Verbal Learning Task, the WISC-V, and the “Little Man” task (66). GCA factor scores were generated using expected a posteriori scoring (67).
Data Analyses
We first examined whether youth with (n = 365) vs. without (n = 11,187) a CD diagnosis differed in demographic characteristics, personality traits, presence of comorbid psychopathology, or social environment characteristics. These analyses were conducted in SPSS (Version 25) and analyzed using data nested by site and family. Given the large sample size used for these analyses, effect sizes are also reported alongside the use of a strict significance threshold (p < 0.005) to increase interpretability of results. Then, in Mplus [version 8.4; (68)], we used LPA to identify mutually exclusive, latent subgroups of youth. Each of the 10 grouping variables (i.e., Positive Urgency, Negative Urgency, Lack of Planning, Lack of Perseverance, Sensation Seeking, BIS, BAS-Reward Responsivity, BAS-Drive, BAS-Fun Seeking, and CU traits) were input as profile indicators. We used the two-level, complex mixture analysis type in Mplus in order to account for clustering by study site and family identifiers. We tested six different LPA models using a step-wise approach, beginning with a one-profile model (see Table 4). We used empirical indicators to inform our selection of the best fitting model: (1) lower Akaike's Information Criterion (AIC)/Bayesian Information Criterion (BIC) values; (2) entropy closer to 1.00; and (3) non-significant Lo-Mendell-Rubin test. We then used class interpretability to determine the final model. As described in the literature, additional classes may show an improvement via empirical indicators but are not meaningful in relation to observable group differences (69).
Follow-up analyses examining latent profile differences on categorical covariates (i.e., demographics) were performed using the R3STEP auxiliary command in Mplus (70), which corrects for classification errors and provides model stability. The results of the R3STEP auxiliary command are provided through logistic regression models with each possible profile by profile comparison used as the outcome variable (i.e., Profile 1 vs. Profile 2, etc.). The Bolck, Croon, and Hagenaars (BCH) method was used to determine if there were latent profile differences on continuous outcome variables (70). The BCH method allows for the examination of continuous outcome variables while accounting for unequal variance among the outcome variables and measurement error of the latent profile using probabilities accounts (71). Given the relatively high number of omnibus and between-group analyses conducted, to minimize Type I error, the statistical significance threshold was p < 0.005.
Results
Characteristics of Youth With Childhood-Onset Conduct Disorder
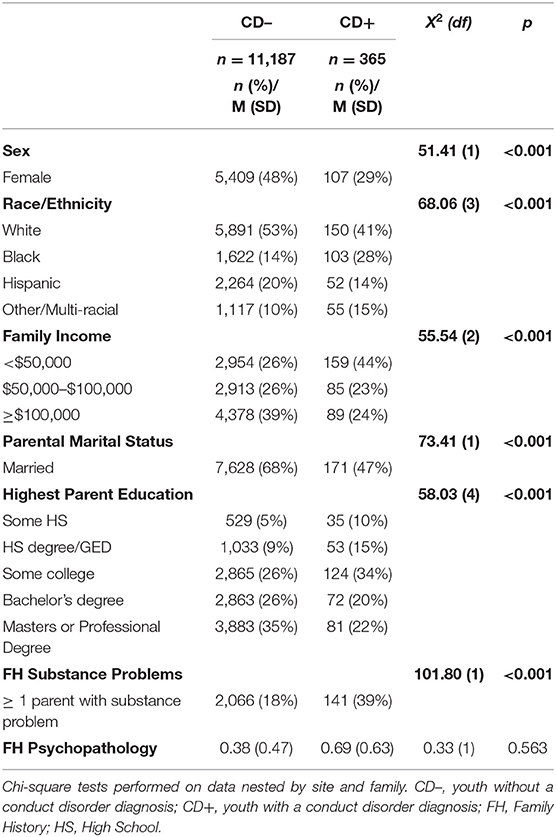
Demographic characteristics for youth with (CD+) and without (CD–) a CD diagnosis are presented in Table 1. As expected, these groups differed in composition by sex (φ = −0.07), race/ethnicity (Cramer's V = 0.08), family income (V = 0.07), parental marital status (V = 0.08), highest parental education (V = 0.07), and family history of substance problems (φ = 0.10). The CD+ group had a higher proportion of males and Black and other/multiracial youth and were more likely to: (1) come from a lower income household, (2) have an unmarried parent, (3) have a lower rate of parents with at least a bachelor's degree, and (4) have a higher incidence rate of at least one parent having a substance use problem. The two groups did not differ significantly based on family history of psychopathology.
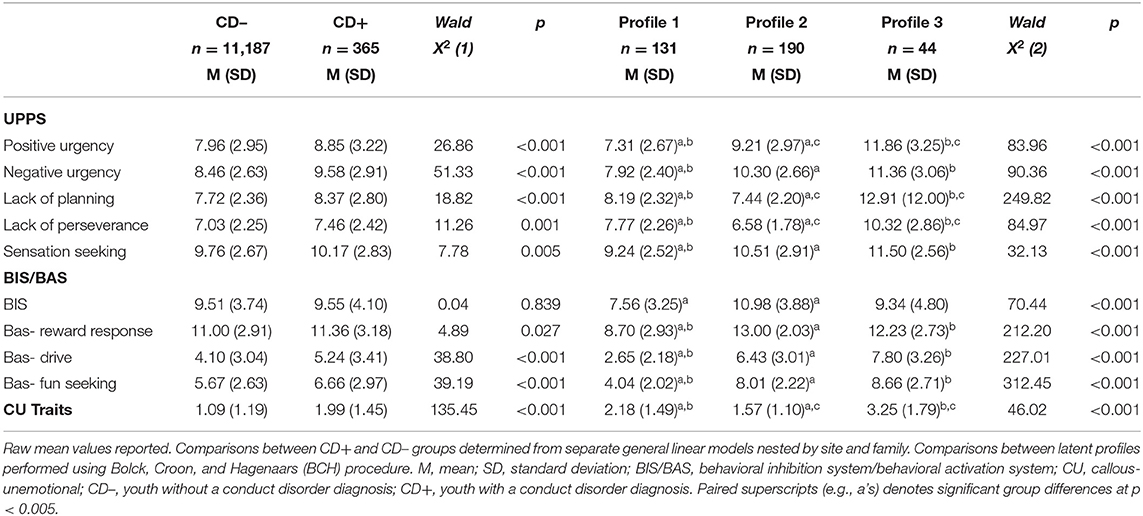
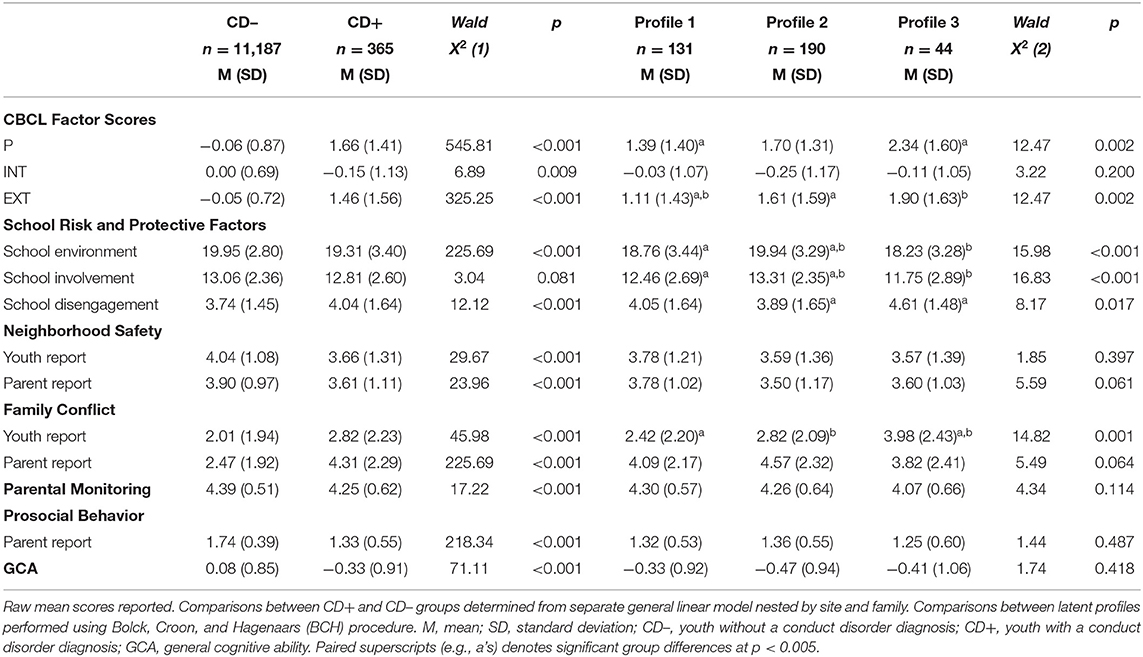
Regarding personality variables (Table 2), the CD+ group had significantly higher scores on all of the UPPS subscales as hypothesized (Cohen's d's ranged from 0.41 for Negative Urgency to 0.15 for Sensation Seeking). The CD+ and CD- groups did not differ on BIS or on the BAS-Reward Response subscale; however, the CD+ group did score significantly higher on the BAS-Drive (d = 0.36), BAS-Fun Seeking (d = 0.37), and CU Traits (d = 0.73) scales. The CD+ group also scored higher on levels of broad psychopathology (d = 1.82) and EXT (d = 1.96) and there was a trend toward lower scores on the INT subfactor (d = −0.22; p = 0.009) in the CD+ group (Table 3). Youth in the CD+ group reported significantly lower scores on the School Environment scale (d = −0.22; Table 3), reflecting less educational resources, as well as significantly higher on the School Disengagement scale (d = 0.20). Both youth (d = −0.33) and parents (d = −0.27) in the CD+ group reported living in significantly less safe neighborhoods and had higher levels of family conflict (d youth= 0.40; d parent = 0.84). Youth in the CD+ group also reported having less parental monitoring (d = −0.26), and their parents reported they exhibited less prosocial behavior in comparison to youth in the CD– group (d = −1.05). Lastly, regarding neurocognitive functioning, youth in the CD+ group scored significantly lower on the GCA index (d = −0.46).
Trait Profiles of Youth With Childhood-Onset Conduct Disorder
Next, different patterns of trait impulsivity, inhibition, behavioral activation, and callousness were examined to account for heterogeneity within the CD+ group. Model fit and entropy statistics are presented in Table 4. The three-profile solution provided the best classification certainty via the highest entropy, and while the AIC and BIC improved slightly when defining a four-profile solution, the Lo-Mendell-Rubin test provided evidence that there was not a significant improvement in moving from a three- to four-profile model. Models were tested up to and including a six-profile model (Table 4); however, the three-profile solution was deemed to be substantively interpretable and therefore was retained for further analyses.
The trait profile of the three-profile solution is depicted in Figure 1, and the trait values and results of difference tests are presented in Table 2. Profile 1 (n = 131) had the lowest scores on the Negative Urgency, Positive Urgency, Sensation Seeking, BIS, and BAS scales, and scored moderately high on Lack of Planning, Lack of Perseverance, and CU traits, defining a low impulsivity/BAS group. Profile 2 (n = 190) scored moderately high on Negative Urgency, Positive Urgency, BIS, and BAS scales, and lowest on Lack of Planning, Lack of Perseverance, and CU traits, defining a high Urgency/BAS group. Lastly, Profile 3 (n = 44) had the highest scores on all UPPS subscales, excluding Sensation Seeking, did not differ significantly from Profile 2 on BIS/BAS scale scores, and had the highest score on CU traits, defining a global high severity group.
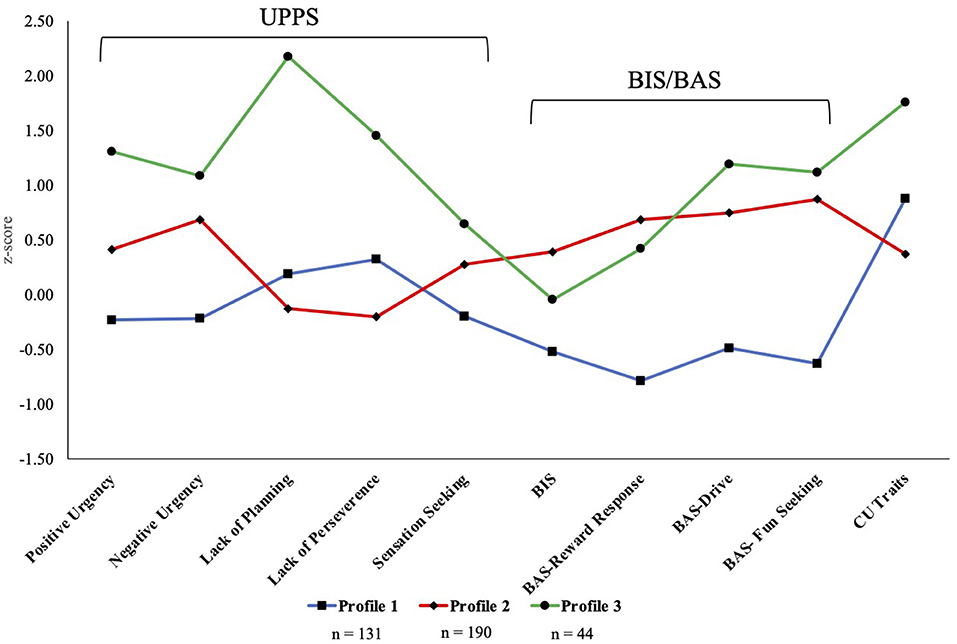
Figure 1. Personality type profiles. BIS, behavioral inhibition system; BAS, behavioral activation system; CU, callous unemotional.
Characteristics of Trait Profiles
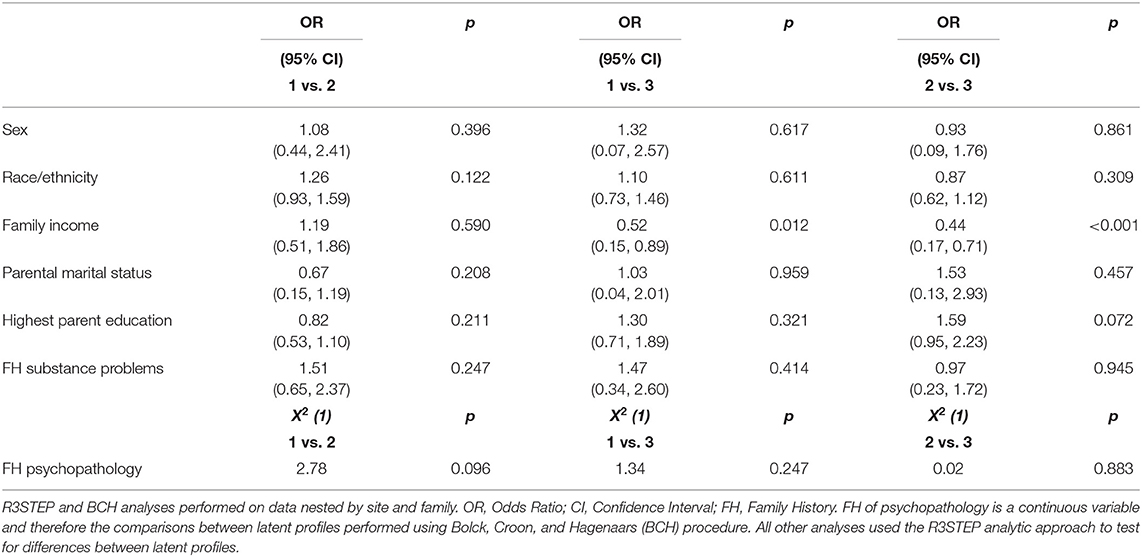
Demographic characteristics for the trait profiles are presented in Table 5. Youth in Profile 3 had significantly lower family income than youth in Profiles 1 and 2 (Odds Ratios = 0.52 and 0.44 respectively; Table 5). No other significant differences between profiles were observed for demographic variables. Profile differences in psychopathology, social environment, and neurocognition are presented in Table 3. Youth in Profile 3 (global high severity) were significantly higher than those in Profile 1 (low impulsivity/BAS) on P and EXT factor scores, while Profile 2 (high Urgency/BAS) was significantly higher than Profile 1 on EXT scores only (Table 3, Figure 2). The groups did not differ significantly on INT factor scores. Youth in Profile 2 reported significantly better school environment and higher rates of school involvement, and the lowest rates of school disengagement. The youth in Profile 3 reported rates of family conflict that were significantly higher than individuals in Profile 1 and 2; however, this finding was not consistent in the parent report of family conflict, where none of the profiles differed significantly. The profiles did not differ significantly on level of parental monitoring or parent report of prosocial behavior. Regarding neurocognition, the three profile types also did not differ significantly from each other.

Figure 2. Latent profiles by General Factor of Psychopathology (P), Internalizing (INT), and Externalizing (EXT) factor scores from the Parent Report CBCL. *denotes differences in P, INT, and EXT factor scores that are significantly different at p < 0.005.
Discussion
The current study used person-centered analyses to characterize heterogeneity on multiple trait dimensions of youth who met criteria for childhood-onset CD. As expected, and consistent with previous studies on childhood-onset CD (1, 9, 48), youth who met criteria for CD were higher on trait measures of impulsivity, behavioral activation subscales, and CU traits. Of note, these youth did not differ from the CD- group on sensitivity to punishment (BIS) and the BAS-Reward Responsivity subscale. While these subscales proved informative for defining latent profiles, this heterogeneity is lost when examining differences between the CD+ vs. CD– youth. As scores on these subscales have been linked to differences in neural and psychophysiological response (31, 41, 42), these findings demonstrate a strength of the study: the characterization of meaningful groups that would not otherwise emerge when simply examining groups defined by the DSM-5 criteria. CD+ youth also scored significantly higher on an aggregate liability for broad psychopathology and externalizing psychopathology with a trend-level lower scores on liability for internalizing psychopathology, consistent with previous research on the nomological networks of the psychopathology factors (49). In addition, the CD+ youth had significant environmental, social, and neurocognitive impairments.
We were also able to define meaningful profiles based on differing personality trait scores within the CD+ group, further accounting for heterogeneity within this high-risk group. The LPA identified three personality profiles that were generally consistent with our hypotheses. For example, while Profiles 1 and 3 included youth who scored relatively high on CU traits, they differed on trait impulsivity, suggesting that although these two traits can co-occur, they represent distinct dimensions relevant to CD symptoms. In addition, the youth who scored lower on CU traits (Profile 2) also had the highest scores on BIS, reflecting a sensitivity to punishment that is thought to be reduced in individuals high on CU traits (33–37). Researchers have found mixed evidence for the association between CU traits and reward responsivity (12, 39). The profiles that emerged in the current study may reconcile this somewhat, as youth in Profiles 2 and 3 were relatively matched on BAS-Reward Response scores but differed significantly on level of CU traits. Furthermore, Profiles 1 and 3 significantly differed on emotional impulsivity, with one group scoring in a normative range on Negative and Positive Urgency (Profile 1) and the other group scoring approximately one standard deviation higher than the full sample (N = 11,552; Profile 3).
These profiles also defined groups that differed significantly on clinically relevant variables. The P factor is conceptualized as a broad liability for all forms of prevalent psychiatric symptomatology, while the EXT and INT factors represent more of a domain-specific liability (49, 72, 73). Therefore, different factor scores on P and EXT for the different profiles suggests that these latent profiles provide meaningful information regarding risk for psychopathology. For example, individuals in Profile 3 scored significantly higher on both the P factor and the EXT subfactor (in comparison to Profile 1) consistent with the characterization of a high global severity group. This suggests that these youth are exhibiting psychopathology beyond CD and may also be at risk for displaying this pattern of broad psychological distress as they develop. In comparison, youth in Profile 2 scored significantly higher only on EXT compared to Profile 1, suggesting that this personality profile is selectively associated with risk for externalizing, but not general psychopathology. Future work to better characterize the patterns of comorbidity of these profiles is needed to determine the stability of these associations, as well as to examine associations with psychopathology that typically has an onset in adolescence (i.e., substance use disorders), and therefore cannot be reliably studied at this age in a community sample.
The groups defined by the latent profiles also differed on some environmental and social variables. Youth in Profile 2 had significantly higher levels of school enrichment and involvement than those in Profiles 1 and 3 and were less disengaged in school compared to the youth in Profile 3. In addition, Profile 3 youth reported significantly higher levels of family conflict than those in Profiles 1 and 3. These findings are of interest as the youth in Profile 1 appear to be relatively low risk—they have the lowest scores on the P and EXT factors, are only elevated on CU traits, and score in a relatively normative range (within ±0.50 standard deviation of the full sample) on impulsivity and responsivity to punishment and reward. Further research is needed to determine the developmental trajectory of these youth as, based on the current cluster of risk/protective factors, we would hypothesize that CD symptoms in this group is likely to remit over time. Beyond these findings, these youth reported relatively similar scores on environmental variables such as neighborhood safety and parental monitoring. It appears that these variables instead may act as general contextual risk factors for CD, but not through pathways unique to the characteristics of one of the profiles defined by the LPA.
Limitations
While the findings from the current study are novel, there are limitations that must be noted. One limitation of the present study is that of generalizability. While the ABCD study was recruited to be nationally representative based on demographic variables, this does not mean that these findings will generalize into other samples of interest including clinical populations. Additionally, the three subgroups can also be interpreted as being “severity” profiles within individuals that meet criteria for a CD diagnosis. A deeper understanding of how CD symptom severity relates to psychopathology, social functioning, and neurocognition has important implications for clinical practice. For example, the high severity group defined by these analyses (i.e., Profile 3) was also at highest risk for general psychopathology (i.e., the P factor) and therefore youth with severe CD symptoms should be assessed for mental health problems beyond externalizing disorders.
In addition, the study was limited by the measures available for use in the LPA. The ABCD study was not explicitly designed to answer this research question and therefore additional indicators [e.g., the Inventory of Callous Unemotional Traits, (74)] and criterion variables (e.g., detailed information about delinquency) were not available. In addition, alternative models that describe the emergence and persistence of antisocial behavior in youth emphasize the presence of grandiose-manipulative traits (75, 76) alongside CU and impulsive-irresponsible traits. Therefore, future work will be needed to determine if self-report of grandiose-manipulative traits provides additional differentiation of profiles and if these profiles replicate in datasets that have additional scales and criterion variables.
Lastly, the diagnostic instrument (KSAD-COMP) was completed by a parent and not a trained clinician. As symptoms of CD are highly behavioral and observable, parent-ratings are likely to be valid. In support of this, youth with CD diagnoses scored significantly higher on CBCL Externalizing Problems and the Conduct Problems scale (Supplementary Table 1) providing convergent evidence for the validity of the measure. Future waves of data collection of the ABCD study will include youth self-report of DSM-5 symptoms, which can be used for further validation of the profiles identified in this study.
Conclusions and Future Directions
These results are valuable for understanding antisocial behavior in youth and how different configurations of personality traits can provide relevant information to further understand heterogeneity within the childhood-onset CD diagnosis. For example, youth within Profile 3 were elevated on CU trait as well as trait indices of distress (Negative/Positive Urgency) and behavioral activation. These youth might therefore benefit from treatments focused on regulating emotions, increasing prosocial behavior, and implementing behavioral interventions to increase planfulness. In comparison, the youth in Profile 1 also scored relatively high on CU traits and therefore would likely benefit from interventions to increase prosocial behavior but would not need additional interventions targeting distress and impulsivity.
In addition, these findings provide information regarding how these dimensions interact to form distinct profiles within youth diagnosed with childhood-onset CD. While impulsivity, punishment and reward responsivity, and CU traits have each been studied as unique risk factors for antisocial behavior, this is the first study to examine how these risk factors co-occur. As these systems rely on shared neural architecture [e.g., amygdala response is linked to both reward responsivity and CU traits; (17, 39, 77)], a nuanced understanding of how these traits co-occur may help to clarify our understanding of individual differences in neural response of youth who demonstrate early antisocial behavior. Future research with the goal of replicating these profiles in additional datasets and across development is needed to determine the generalizability and stability of these patterns. Although the data used in this study are cross-sectional, data collection in the ABCD study is ongoing, and these findings therefore set the stage for prospective longitudinal research using multimodal data—such as neuroimaging and parent- and teacher-reports—to more fully determine how these latent profiles account for the course, severity, and comorbidity of psychopathology in these groups of high-risk youth.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: The ABCD data repository grows and changes over time. The ABCD data used in this report came from doi: 10.15154/1504041 DOIs can be found at http://dx.doi.org/10.15154/1504041.
Ethics Statement
The studies involving human participants were reviewed and approved by The ABCD Study Coordinating Center (CC) has already established a single IRB to facilitate uniform ethical standards are applied across sites and to comply with the NIH Policy on the use of a single IRB for multi-site research. The UCSD Human Research Protections Program (HRPP) is acting as the single IRB for the ABCD-USA consortium. This has improved quality and efficiency in protection of research participants. The University of Michigan has entered into a reliance agreement with the UCSD IRB and has ceded review to the single IRB at UCSD. The UCSD single IRB maintains all documents relating to the reliance agreements with the relying IRBs. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
SB and MH developed the study concept and design. SB and MM performed the data analysis. All authors contributed to the interpretation of the results, drafted the paper, and provided critical revisions. All authors approved the final version of the paper for submission.
Funding
This work was supported by funding from the National Institute on Alcohol Abuse and Alcoholism (T32 AA007477, K01 AA024804, and K01027558) and the National Institute on Drug Abuse (K01 DA044270). Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report.
Disclaimer
This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
A pre-print of manuscript has been made available online (https://psyarxiv.com/shp6c/).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.701199/full#supplementary-material
References
1. Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev. (1993) 100:674. doi: 10.1037/0033-295X.100.4.674
2. Fairchild G, Hawes DJ, Frick PJ, Copeland WE, Odgers CL, Franke B, et al. Conduct disorder. Nat Rev Dis Primers. (2019) 5:1–25. doi: 10.1038/s41572-019-0095-y
3. Odgers CL, Moffitt TE, Broadbent JM, Dickson N, Hancox RJ, Harrington H, et al. Female and male antisocial trajectories: from childhood origins to adult outcomes. Dev Psychopathol. (2008) 20:673–716. doi: 10.1017/S0954579408000333
4. Frick PJ, Ray JV, Thornton LC, Kahn RE. Annual research review: a developmental psychopathology approach to understanding callous-unemotional traits in children and adolescents with serious conduct problems. J Child Psychol Psychiatry. (2014) 55:532–48. doi: 10.1111/jcpp.12152
5. Longman T, Hawes DJ, Kohlhoff J. Callous–unemotional traits as markers for conduct problem severity in early childhood: a meta-analysis. Child Psychiatry Human Dev. (2016) 47:326–34. doi: 10.1007/s10578-015-0564-9
6. Moffitt TE, Arseneault L, Jaffee SR, Kim-Cohen J, Koenen KC, Odgers CL, et al. Research review: DSM-V conduct disorder: research needs for an evidence base. J Child Psychol Psychiatry. (2008) 49:3–33. doi: 10.1111/j.1469-7610.2007.01823.x
7. Platje E, Huijbregts SC, van Goozen SH, Popma A, Cima M, Swaab HJ. Executive functioning, reward/punishment sensitivity, and conduct problems in boys with callous-unemotional traits. Int J Offender Ther Comp Criminol. (2018) 62:4008–23. doi: 10.1177/0306624X18758897
8. Lahey BB, Loeber R. Framework for a developmental model of oppositional defiant disorder and conduct disorder. In: D. K. Routh, editor. Disruptive Behavior Disorders in Childhood. New York, NY: Plenum (1994). p. 139–80. doi: 10.1007/978-1-4899-1501-6_6
9. Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Dev Psychopathol. (2002) 14:179–207. doi: 10.1017/S0954579402001104
10. Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: biological, environmental, developmental mechanisms. Clin Psychol. (2010) 17:327–36. doi: 10.1111/j.1468-2850.2010.01224.x
11. Colledge E, Blair R. The relationship in children between the inattention and impulsivity components of attention deficit and hyperactivity disorder and psychopathic tendencies. Person Individ Diff. (2001) 30:1175–87. doi: 10.1016/S0191-8869(00)00101-X
12. Haas SM, Derefinko KJ, Waschbusch DA. The use of multimethod impulsivity assessment in the prediction of ADHD conduct problems, callous-unemotional symptoms. Pers Individ Dif. (2017) 116:289–95. doi: 10.1016/j.paid.2017.04.028
13. Snyder J, Prichard J, Schrepferman L, Patrick MR, Stoolmiller M. Child impulsiveness—inattention, early peer experiences, and the development of early onset conduct problems. J Abnorm Child Psychol. (2004) 32:579–94. doi: 10.1023/B:JACP.0000047208.23845.64
14. White JL, Moffitt TE, Caspi A, Bartusch DJ, Needles DJ, Stouthamer-Loeber M. Measuring impulsivity and examining its relationship to delinquency. J Abnorm Psychol. (1994) 103:192. doi: 10.1037/0021-843X.103.2.192
15. Connor DF, Ford JD, Albert DB, Doerfler LA. Conduct disorder subtype and comorbidity. Ann Clin Psychiatry. (2007) 19:161–8. doi: 10.1080/10401230701465269
16. Silberg J, Moore AA, Rutter M. Age of onset and the subclassification of conduct/dissocial disorder. J Child Psychol Psychiatry. (2015) 56:826–33. doi: 10.1111/jcpp.12353
17. Blair RJR, Leibenluft E, Pine DS, Frick PJ, Ray JV, Thornton LC, et al. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. New Eng J Med. (2014) 140:1. doi: 10.1037/a0033076
18. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub (2013). doi: 10.1176/appi.books.9780890425596
19. Frick PJ, Dickens C. Current perspectives on conduct disorder. Curr Psychiatry Rep. (2006) 8:59–72. doi: 10.1007/s11920-006-0082-3
20. Frick PJ, White SF. Research review: the importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. J Child Psychol Psychiatry. (2008) 49:359–75. doi: 10.1111/j.1469-7610.2007.01862.x
21. Rowe R, Maughan B, Moran P, Ford T, Briskman J, Goodman R. The role of callous and unemotional traits in the diagnosis of conduct disorder. J Child Psychol Psychiatry. (2010) 51:688–95. doi: 10.1111/j.1469-7610.2009.02199.x
22. Frick PJ. Developmental pathways to conduct disorder: implications for future directions in research, assessment, and treatment. J Clin Child Adolesc Psychol. (2012) 41:378–89. doi: 10.1080/15374416.2012.664815
23. Patrick CJ, Drislane LE. Triarchic model of psychopathy: origins, operationalizations, and observed linkages with personality and general psychopathology. J Pers. (2015) 83:627–43. doi: 10.1111/jopy.12119
24. Venables N, Hall J, Patrick C. Differentiating psychopathy from antisocial personality disorder: a triarchic model perspective. Psychol Med. (2014) 44:1005–13. doi: 10.1017/S003329171300161X
25. Fanti KA, Kyranides MN, Lordos A, Colins OF, Andershed H. Unique and interactive associations of callous-unemotional traits, impulsivity and grandiosity with child and adolescent conduct disorder symptoms. J Psychopathol Behav Assess. (2018) 40:40–9. doi: 10.1007/s10862-018-9655-9
26. Pardini D, Obradovic J, Loeber R. Interpersonal callousness, hyperactivity/impulsivity, inattention, and conduct problems as precursors to delinquency persistence in boys: a comparison of three grade-based cohorts. J Clin Child Adolesc Psychol. (2006) 35:46–59. doi: 10.1207/s15374424jccp3501_5
27. Sica C, Ciucci E, Baroncelli A, Frick PJ, Patrick CJ. Not just for adults: using the triarchic model of psychopathy to inform developmental models of conduct problems in adolescence. J Clin Child Adolesc Psychol. (2019) 49:897–911. doi: 10.1080/15374416.2019.1574228
28. Urben S, Habersaat S, Pihet S, Suter M, de Ridder J, Stéphan P. Specific contributions of age of onset, callous-unemotional traits and impulsivity to reactive and proactive aggression in youths with conduct disorders. Psychiatr Q. (2018) 89:1–10. doi: 10.1007/s11126-017-9506-y
29. McMahon RJ, Witkiewitz K, Kotler JS, Conduct Problems Prevention Research Group. Predictive validity of callous-unemotional traits measured in early adolescence with respect to multiple antisocial outcomes. J Abnorm Psychol. (2010) 119:752–63. doi: 10.1037/a0020796
30. Pardini DA, Fite PJ. Symptoms of conduct disorder, oppositional defiant disorder, attention-deficit/hyperactivity disorder, and callous-unemotional traits as unique predictors of psychosocial maladjustment in boys: advancing an evidence base for DSM-V. J Am Acad Child Adolesc Psychiatry. (2010) 49:1134–44. doi: 10.1016/j.jaac.2010.07.010
31. Arnett PA. Autonomic responsivity in psychopaths: a critical review and theoretical proposal. Clin Psychol Rev. (1997) 17:903–36. doi: 10.1016/S0272-7358(97)00045-7
32. Ross SR, Molto J, Poy R, Segarra P, Pastor MC, Montanés S. Gray's model and psychopathy: BIS but not BAS differentiates primary from secondary psychopathy in noninstitutionalized young adults. Person Individ Diff. (2007) 43:1644–55. doi: 10.1016/j.paid.2007.04.020
33. Byrd AL, Hawes SW, Burke JD, Loeber R, Pardini DA. Boys with conduct problems and callous-unemotional traits: neural response to reward and punishment and associations with treatment response. Dev Cogn Neurosci. (2018) 30:51–9. doi: 10.1016/j.dcn.2017.12.004
34. Fairchild G, Van Goozen SH, Stollery SJ, Goodyer IM. Fear conditioning and affective modulation of the startle reflex in male adolescents with early-onset or adolescence-onset conduct disorder and healthy control subjects. Biol Psychiatry. (2008) 63:279–85. doi: 10.1016/j.biopsych.2007.06.019
35. Fonseca A, Yule W. Personality and antisocial behavior in children and adolescents: an enquiry into Eysenck's and Gray's theories. J Abnorm Child Psychol. (1995) 23:767–81. doi: 10.1007/BF01447476
36. Morgan JE, Bowen KL, Moore SC, Van Goozen. S. H. The relationship between reward and punishment sensitivity and antisocial behavior in male adolescents. Pers Individ Dif. (2014) 63:122–7. doi: 10.1016/j.paid.2014.01.054
37. Syngelaki EM, Fairchild G, Moore SC, Savage JC, van Goozen SH. Affective startle potentiation in juvenile offenders: the role of conduct problems and psychopathic traits. Soc Neurosci. (2013) 8:112–21. doi: 10.1080/17470919.2012.712549
38. Fairchild G, van Goozen SHM, Stollery SJ, Aitken MRF, Savage J, Moore SC, et al. Decision making and executive function in male adolescents with early-onset or adolescence-onset conduct disorder and control subjects. Biol Psychiatry. (2009) 66:162–8. doi: 10.1016/j.biopsych.2009.02.024
39. Byrd AL, Loeber R, Pardini DA. Antisocial behavior, psychopathic features and abnormalities in reward and punishment processing in youth. Clin Child Fam Psychol Rev. (2014) 17:125–56. doi: 10.1007/s10567-013-0159-6
40. Polier GG, Vloet TD, Herpertz-Dahlmann B, Laurens KR, Hodgins S. Comorbidity of conduct disorder symptoms and internalising problems in children: investigating a community and a clinical sample. Eur Child Adolesc Psychiatry. (2012) 21:31–8. doi: 10.1007/s00787-011-0229-6
41. Kim SH, Yoon H, Kim H, Hamann S. Individual differences in sensitivity to reward and punishment and neural activity during reward and avoidance learning. Soc Cogn Affect Neurosci. (2015) 10:1219–27. doi: 10.1093/scan/nsv007
42. Simon JJ, Walther S, Fiebach CJ, Friederich H-C, Stippich C, et al. Neural reward processing is modulated by approach-and avoidance-related personality traits. Neuroimage. (2010) 49:1868–74. doi: 10.1016/j.neuroimage.2009.09.016
43. Ferguson SLG, Moore EW, Hull DM. Finding latent groups in observed data: a primer on latent profile analysis in Mplus for applied researchers. Int J Behav Dev. (2019) 44:458–68. doi: 10.1177/0165025419881721
44. Fair DA, Bathula D, Nikolas MA, Nigg JT. Distinct neuropsychological subgroups in typically developing youth inform heterogeneity in children with ADHD. Proc Natl Acad Sci USA. (2012) 109:6769–74. doi: 10.1073/pnas.1115365109
45. van Hulst BM, De Zeeuw P, Durston S. Distinct neuropsychological profiles within ADHD: a latent class analysis of cognitive control, reward sensitivity and timing. Psychol Med. (2015) 45:735–45. doi: 10.1017/S0033291714001792
46. Evans-Polce R, Lanza S, Maggs J. Heterogeneity of alcohol, tobacco, and other substance use behaviors in US college students: a latent class analysis. Addict Behav. (2016) 53:80–5. doi: 10.1016/j.addbeh.2015.10.010
47. Peugh J, Fan X. Modeling unobserved heterogeneity using latent profile analysis: a Monte Carlo simulation. Struct Equat Model. (2013) 20:616–39. doi: 10.1080/10705511.2013.824780
48. Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the national comorbidity survey replication. Psychol Med. (2006) 36:699–710. doi: 10.1017/S0033291706007082
49. Brislin S, Martz M, Joshi S, Duval E, Gard A, Clark D, et al. Differentiated nomological networks of internalizing, externalizing, and the general factor of psychopathology (‘p factor') in emerging adolescence in the ABCD study. Psychol Med. (2021) 1–11. doi: 10.1017/S0033291720005103
50. Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Dev Cogn Neurosci. (2018) 32:55–66. doi: 10.1016/j.dcn.2017.10.010
51. Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. (2018) 32:16–22. doi: 10.1016/j.dcn.2018.04.004
52. Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, et al. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev Cogn Neurosci. (2018) 32:4–7. doi: 10.1016/j.dcn.2017.10.002
53. Zucker RA, Gonzalez R, Ewing SWF, Paulus MP, Arroyo J, Fuligni A, et al. Assessment of culture and environment in the adolescent brain and cognitive development study: rationale, description of measures, early data. Dev Cogn Neurosci. (2018) 32:107–20. doi: 10.1016/j.dcn.2018.03.004
54. Luciana M, Bjork J, Nagel B, Barch D, Gonzalez R, Nixon S, et al. Adolescent neurocognitive development and impacts of substance use: overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev Cogn Neurosci. (2018) 32:67–79. doi: 10.1016/j.dcn.2018.02.006
55. Kobak KA, Kratochvil C, Stanger C, Kaufman J. Computerized screening of comorbidity in adolescents with substance or psychiatric disorders. In: Anxiety Disorders and Depression. La Jolaa, CA (2013).
56. Pagliaccio D, Luking KR, Anokhin AP, Gotlib IH, Hayden EP, Olino TM, et al. Revising the BIS/BAS Scale to study development: measurement invariance and normative effects of age and sex from childhood through adulthood. Psychol Assess. (2016) 28:429. doi: 10.1037/pas0000186
57. Hawes SW, Waller R, Thompson WK, Hyde LW, Byrd AL, Burt SA, et al. Assessing callous-unemotional traits: development of a brief, reliable measure in a large and diverse sample of preadolescent youth. Psychol Med. (2019) 50:456–64. doi: 10.1017/S0033291719000278
58. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
59. Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev. (2000) 21:265–71. doi: 10.1542/pir.21-8-265
60. Milne B, Moffitt T, Crump R, Poulton R, Rutter M, Sears M, et al. How should we construct psychiatric family history scores? A comparison of alternative approaches from the Dunedin Family Health History Study. Psychol Med. (2008) 38:1793–802. doi: 10.1017/S0033291708003115
61. Milne BJ, Caspi A, Harrington H, Poulton R, Rutter M, Moffitt TE. Predictive value of family history on severity of illness: the case for depression, anxiety, alcohol dependence, drug dependence. Arch Gen Psychiatry. (2009) 66:738–47. doi: 10.1001/archgenpsychiatry.2009.55
62. Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci. (2014) 2:119–37. doi: 10.1177/2167702613497473
63. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. (2018) 175:831–44. doi: 10.1176/appi.ajp.2018.17121383
64. Clark DA, Hicks BM, Angstadt M, Rutherford S, Taxali A, Hyde LW, et al. The general factor of psychopathology in the adolescent brain cognitive development (ABCD) study: a comparison of alternative modeling approaches. Clin Psychol Sci. (2020) 9:169–82. doi: 10.31234/osf.io/b6uy7
65. Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. (2001) 40:1337–45. doi: 10.1097/00004583-200111000-00015
66. Sripada C, Angstadt M, Rutherford S, Taxali A. Brain network mechanisms of general intelligence. BioRxiv. (2019) 657205. doi: 10.1101/657205
67. MacCallum RC. Factor analysis. In: Millsap R, Maydeu-Olivares A, editors. The SAGE Handbook of Quantitative Methods in Psychology. Thousand Oaks, CA: SAGE Publications Ltd (2009). p. 123–47. doi: 10.4135/9780857020994.n6
69. Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences, Vol. 718. New York, NY; John Wiley and Sons (2010).
70. Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes. (2014) 21:1–22. doi: 10.1080/10705511.2014.915181
71. Bauer DJ, Shanahan MJ. Modeling complex interactions: Person-centered and variable-centered approaches. In: Little TD, Bovaird JA, Card NA, editors. Modeling Contextual Effects in Longitudinal Studies. Hillsdale, NJ: Lawrence Erlbaum Associates Publishers (2007). p. 255–83.
72. Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? J Abnormal Psychol. (2012) 121:971. doi: 10.1037/a0028355
73. Lahey BB, Rathouz PJ, Keenan K, Stepp SD, Loeber R, Hipwell AE. Criterion validity of the general factor of psychopathology in a prospective study of girls. J Child Psychol Psychiatry. (2015) 56:415–22. doi: 10.1111/jcpp.12300
75. Andershed H, Colins OF, Salekin RT, Lordos A, MKyranides MN, Fanti KA. Callous-unemotional traits only versus the multidimensional psychopathy construct as predictors of various antisocial outcomes during early adolescence. J Psychopathol Behav Assess. (2018) 40:16–25. doi: 10.1007/s10862-018-9659-5
76. Salekin RT. Research review: what do we know about psychopathic traits in children? J Child Psychol Psychiatry. (2017) 58:1180–200. doi: 10.1111/jcpp.12738
Keywords: conduct disorder, latent profile analysis, CU traits, impulsivity, BIS/BAS, UPPS-P impulsive behavior scale
Citation: Brislin SJ, Martz ME, Cope LM, Hardee JE, Weigard A and Heitzeg MM (2021) Heterogeneity Within Youth With Childhood-Onset Conduct Disorder in the ABCD Study. Front. Psychiatry 12:701199. doi: 10.3389/fpsyt.2021.701199
Received: 27 April 2021; Accepted: 22 June 2021;
Published: 16 July 2021.
Edited by:
Patrick W. L. Leung, The Chinese University of Hong Kong, ChinaReviewed by:
Randall Salekin, University of Alabama, United StatesJustin Parent, Florida International University, United States
Copyright © 2021 Brislin, Martz, Cope, Hardee, Weigard and Heitzeg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah J. Brislin, YnJpc2xpbnNqQHZjdS5lZHU=
 Sarah J. Brislin
Sarah J. Brislin Meghan E. Martz2
Meghan E. Martz2 Lora M. Cope
Lora M. Cope Alexander Weigard
Alexander Weigard