
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 12 July 2021
Sec. Public Mental Health
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.696200
This article is part of the Research TopicCovid-19 and Psychological Disorders: From Molecular Basis to Social Impacts and Therapeutic InterventionsView all 27 articles
 Ruike Zhang1
Ruike Zhang1 Tianya Hou1
Tianya Hou1 Xiangyu Kong2
Xiangyu Kong2 Guibin Wang3
Guibin Wang3 Hao Wang1
Hao Wang1 Shuyu Xu1
Shuyu Xu1 Jingzhou Xu1
Jingzhou Xu1 Jingwen He4
Jingwen He4 Lei Xiao1
Lei Xiao1 Yajing Wang1
Yajing Wang1 Jing Du1
Jing Du1 Yujia Huang1
Yujia Huang1 Tong Su1*
Tong Su1* Yunxiang Tang1*
Yunxiang Tang1*Objective: To investigate the prevalence of sleep quality and post-traumatic stress disorder (PTSD) symptoms of healthcare workers (HCWs) and identify the determinants for PTSD symptoms among HCWs in high-risk and low-risk areas during the COVID-19 outbreak in China.
Methods: The Pittsburgh Sleep Quality Index and the Impact of Event Scale were used to assess sleep quality and symptoms of PTSD of 421 Chinese HCWs, respectively, from January 30 to March 2, 2020. The influencing factors of PTSD symptoms were identified by univariate analysis and multiple regression.
Results: The incidence of HCWs getting PTSD symptoms were 13.2%. HCWs from high-risk areas had significantly poorer sleep quality (p < 0.001). Poor sleep quality was the risk factor of PTSD symptoms for HCWs from high-risk (p = 0.018) and low-risk areas (p < 0.001). Furthermore, non-medical staff were found to be the risk factor for PTSD symptoms only in low-risk areas.
Discussion: HCWs in Hubei had poorer sleep quality. Non-medical HCWs from low-risk areas were associated with more severe PTSD symptoms. Mental health programs should be considered for HCWs, especially those who are often overlooked.
Several pneumonia cases of unknown etiology were first detected in Wuhan, Hubei Province, in China at the end of 2019 and the World Health Organization (WHO), China Office, was informed in a timely manner and responded to the outbreak of Novel Corona-virus (COVID-19) on January 5, 2020 (1). The outbreak of COVID-19 went from being declared as a Public Health Emergency of International Concern (PHEIC) to a global pandemic on March 11 by WHO after the epidemic had widely spread to the rest of the world (2).
Compared with SARS-CoV and MERS-CoV, COVID-19 was less severe but more infectious, according to rapidly increasing incidence and evidence of human-to-human transmission (3).
Healthcare workers (HCWs) are those at risk of confronting outbreaks and pathogens unknown to date (4) and are at high risk of being infected (5–7). In light of the magnitude of the COVID-19 pandemic and the stress experienced by HCWs, intense researches have investigated the psychological impact of the HCWs during the pandemic. Research has shown that HCWs experienced higher psychological morbidity, especially high-risk HCWs (8–11). A study has found that even in areas where the epidemic was not so severe, the risk of infection for HCWs is still higher than that of general population (12). Some research focused on low-risk epidemic areas has found that the mental problems of post-traumatic stress symptoms (PTSS), depression and anxiety were also found both in high-risk and low-risk HCWs (13, 14).
Post-traumatic stress disorder (PTSD) is a trauma related disorder that is characterized by the presence of one of the four symptoms of intrusion, avoidance, negative mood, and cognitive changes, as well as arousal and reactivity, for at least 1 month (15). A recent study has found that emergency workers had a 3-fold higher risk of PTSD than the general population (16). Hubei was the region with the most severe pandemic, and working in Hubei province was considered to be working in a high-risk area in this study, and HCWs from low-risk areas were those working outside Hubei province (including Shanghai, Beijing, Shandong, Chongqing, etc.). A study found that there were no interregional differences of stress following the outbreak among HCWs between Hubei or non-Hubei areas (17). On the contrary, other research has found that working in the high-risk epidemic area of China, Wuhan, entailed higher risk psychological distress (18).
However, most of the previous literature regarding the psychological effects of the pandemic on HCWs has focused particularly on doctors, nurses, and physicians. In comparison, there has been little research exploring the impact of the pandemic on hospital logistics and administrative staff. Research has found that nurses had a greater risk of experiencing anxiety and PTSD symptoms than other healthcare workers (19). In contrast, other research has reported more severe anxiety, depression, and insomnia problems in non-medical staff and physician in trainee compared with professional physicians (20). A study has found that workers in administration departments have similar anxiety scores to those of workers in clinical departments and fever clinics (21). These studies suggested that non-medical workers have similar mental problems with medical HCWs during the pandemic. A limited number of studies have investigated the PTSD symptoms in non-medical staff during the COVID-19 pandemic. A study has investigated the associations between the psychological health and physical symptoms among healthcare workers including doctors, nurses, administrators, and maintenance workers; however, it did not examine the psychological differences between medical HCWs and non-medical HCWs (22). Research has found that there was no significant difference in the detection rate of SARS-CoV-2 transmission in hospital in non-clinical HCWs compared with clinical HCWs (23), since non-medical HCWs were in hospital settings with less medical expertise. There is a very great demand for a study of the PTSD symptoms in medical as well as non-medical HCWs.
A systematic review of risk factors for PTSD among HCWs during pandemics has found that the position at work, level of exposure, quarantine, work experience, gender, and marital status were associated with PTSD (24). However, no previous study has investigated the different determinants of PTSD development between HCWs from high-risk and low-risk areas during the pandemic. Mental health, especially PTSD, could have a profound impact on the healthcare system. Therefore, it is necessary to investigate the prevalence of mental health disturbances and the risk factors of PTSD among HCWs during COVID-19, and specific interventions should be designed targeting those who are vulnerable to the development of PTSD during the outbreak. In this study, we assessed the prevalence of PTSD symptoms and their associated factors. We sought to analyze the predictive effect of demographic variables on PTSD symptoms in HCWs from high-risk and low-risk areas during the epidemic. As COVID-19 continues to spread over the next few months, this research may help identify HCWs who are more vulnerable to develop PTSD, which may provide a basis for further intervention.
This study was a quantitative survey using the snowball sampling strategy for HCWs in China, including doctors, nurses, medical technicians, and non-medical staff working in hospitals. The time span of the study was 33 days between January 30 and March 2, 2020. A total of 421 HCWs voluntarily participated and completed questionnaires anonymously online. Participants over 18 years of age and who can read and understand Mandarin were included, while the exclusion criteria were being outside of China and time in bed less than actual sleep time. The study was approved by the Research Ethics Commission of Naval Medical University.
Sociodemographic variables were collected, such as gender, age, years working, education level, marital status, occupation, being the only child of the family, and child status. The HCWs were divided into two categories according to their occupation: medical healthcare workers (i.e., doctors, nurses, medical technicians) and non-medical healthcare workers (i.e., administrative staff, logistical staff, and others).
The Pittsburgh Sleep Quality Index (PSQI) was used to test HCWs' sleep quality. It is a self-administered scale including 19 items consisting of seven dimensions including subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. The PSQI global score ranges from 0 to 21 (25). Scores >7 indicate poor sleep quality.
The Impact of Event Scale (IES-R) was used to assess subjective stress caused by traumatic events. The IES-R scale includes 22 items and consists of three subscales: intrusiveness, avoidance and hyperarousal. The scale ranges from 0 to 88. An IES-R total score >33 is identified as having PTSD symptoms (26).
PTSD total score were converted to dichotomous variables (presence of PTSD symptoms and no PTSD symptoms). The group comparisons of categorical variables were carried out with chi-square tests, and continuous variables were analyzed with Student's t-test. For univariate analysis of PTSD symptoms, the chi-square test was used for categorical variables. The count and frequency were presented.
Variables with p < 0.2 in univariate analysis were subjected to multiple regression analysis (27). Multiple logistic regression analysis using the forward conditional procedure was conducted for detecting risk factors for PTSD symptoms. The IES-R subscale scores were not normally distributed. Therefore, the Kruskal-Wallis test was used to compare the IES-R subscale scores across the different occupational groups and between HCWs from high-risk and low-risk areas.
A two-sided p < 0.05 was identified as statistically significant. All statistical analyses were performed using SPSS 26.0 (Statistical Package for the Social Sciences) for Windows (SPSS, Chicago, IL).
Of the 421 respondents completed the questionnaire, 401 participants were included in the study (response rate = 95.2%). The Expectation Maximization (EM) interpolation method was used to fill in the missing values. Most of the participants were distributed in Hubei, where the epidemic was the most serious across the country. Thus, HCWs in Hubei were considered HCWs from a high-risk area. Females account for 69.1% of the participants. The occupation of the HCWs in this study were classified into medical HCWs (i.e., doctors, nurses, and medical technicians) (n = 351, 87.5%) and non-medical HCWs (n = 50, 12.5%) including logistic and administrative staffs and others. Most of the participants were between 31 and 40 years old (n = 180, 44.9%) and have more than 10 years of work experience (n = 176, 43.9%). About 40% of the participants had poor sleep quality (n = 166, 41.4%). The data showed that the prevalence of PTSD symptoms was 13.2% (Table 1).
We tested the differences of PSQI, PTSD symptoms and component scores between groups of high-risk area and low-risk area. The difference in sleep quality between HCWs from high-risk and low-risk areas is significant (p < 0.001). HCWs from high-risk areas had poorer sleep quality. The scores in high-risk area groups were significantly higher in subjective sleep quality (t = −3,365, p = 0.001), sleep duration (t = −6.425, p < 0.001), habitual sleep efficiency (t = −2.072, p = 0.039), sleep disturbances (t = −2.308, p = 0.022), use of sleep medications (t = −2.275, p = 0.024) and daytime dysfunction (t = −3.176, p = 0.002). The difference of PTSD symptoms (p = 0.690) was not significant between high-risk areas (n = 21, 12.4%) and low-risk areas (n = 32, 13.8%) HCWs. However, the intrusion scores were significantly different between HCWs from high-risk and low-risk areas (p = 0.041) (Table 2).
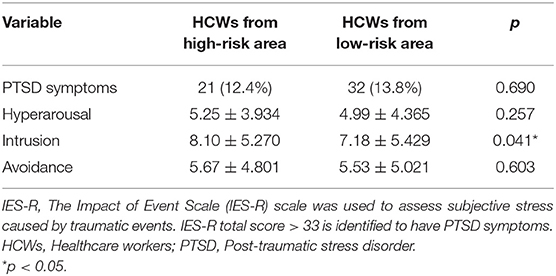
Table 2. Comparisons of the IES-R scores obtained by HCWs from high-risk area and HCWs from low-risk area.
The prevalence of PTSD symptoms of medical HCWs and non-medical HCWs are 11.4 and 26.0%, respectively. The chi-square test showed that the PTSD symptoms were significantly different across occupational groups (p = 0.004). The differences between avoidance (p = 0.630), hyperarousal (p = 0.543) and intrusion (p = 0.672) were not significant across occupational groups (Table 3).
Univariate analysis of influencing factors for PTSD symptoms showed that the variables of occupation (p = 0.004), marital status (p = 0.045), child status (p = 0.048), and sleep quality (p < 0.001) were significantly associated with PTSD symptoms (Table 4). The results of regression showed that for all HCWs, being a medical HCW (OR = 0.285, p = 0.002) was a protective factor for PTSD. Being married (OR = 2.453, p = 0.023) and having poor sleep quality (OR = 5.695, p < 0.001) were risk factors for PTSD. HCWs from high-risk and low-risk areas were used as stratification factors to explore further whether working in high-risk and low-risk areas would affect the risk factors for PTSD in HCWs. The risk factors for low-risk area HCWs were poor sleep quality and being non-medical HCWs. It should be noted that for high-risk area HCWs, the risk factor for PTSD was poor sleep quality (OR = 3.968, p = 0.018), which was different from that of HCWs from low-risk areas (Table 5). The multiple linear regression showed that poor sleep quality was a risk factor for intrusion (p < 0.001) and avoidance (p < 0.001). The risk factors for hyperarousal were poor sleep quality (p < 0.001) and being non-medical staff (p = 0.046) (Table 6).
This study investigated the prevalence of sleep quality and mental disturbances of HCWs during the pandemic and presented the potential influence value of demographic characteristics. In all, 13.2% of HCWs were shown to have PTSD symptoms in this study. The rates were lower compared with a meta-analysis that showed that 20.2% of the medical staff endured serious post-traumatic stress symptoms during and shortly after the epidemic (10). This is perhaps due to the different sample sources.
During the COVID-19 outbreak, HCWs in Hubei province had significantly poorer sleep quality (p < 0.001). When it comes to the component scores of the PSQI, the study showed that HCWs in Hubei has worse subjective sleep quality, shorter sleep duration, more sleep disturbances, worse sleep efficiency, more frequent use of sleep medications, and more severe daytime dysfunction. This finding was consistent with that of Grainne M. McAlonan et al. (28), who found that high-risk HCWs had a higher risk of fatigue and having poor sleep quality during the outbreak of SARS. Hubei Province was the center of the epidemic, where the number of confirmed cases and severe cases was significantly higher than those in other provinces. Therefore, the workload and work intensity of medical personnel in Hubei province were much greater than those in other provinces. And the HCWs working in Hubei province during this period are considered HCWs from a high-risk area with a much higher probability of being infected, which means particular attention should be paid to this group.
This study found that HCWs working in or outside Hubei province had an equal level of incidence of psychological stress. Recent research on 526 nurses found that PTSD symptoms were more severe in second-line nurses compared with that of frontline nurses (29). Other literature on the mental health of 994 HCWs in Wuhan has reported that exposure to the virus significantly increases the odds of PTSD symptoms (30). Previous studies have also indicated that similar psychological morbidity and perceived stress were found between high-risk and low-risk HCWs (31). COVID-19 has a long incubation period and the virus carriers are undetectable and could transmit virus during the latent period. Although non-Hubei provinces had a lower incidence than Hubei province, the number of confirmed cases was rising rapidly as well. The HCWs outside Hubei province did not recognize themselves as exempt from the danger. Moreover, the medical staff in Hubei might have had higher vigilance and confidence as the attention of the whole country was focused on them. Thus, medical staff in Hubei had a morale and sense of responsibility to conquer this challenge, which is beneficial for the maintenance of their mental health.
Our study has suggested that non-medical staff, such as administrative and logistic staff and others working outside Hubei province, had a higher incidence of PTSD symptoms compared with that of medical staff. Our findings match earlier observations. The attack rate among HCWs during SARS varied by occupations. The attack rate of HCWs in Vietnam, in 2003, were 16%, 35% for doctors and nurses, respectively. Those with the highest attack rate were administrative staff and “other staff with patient contact,” which accounted for 55% of cases (1). A cross-sectional study of 5,657 individuals showed that nonmedical staff endured a higher risk of depression, anxiety, and insomnia (32). This might be one of the reasons why administrative and logistic staff in our study endured a higher incidence of PTSD symptoms. Another reason could be that the logistic staff and others working in hospital might not be as psychologically prepared as doctors and nurses. Moreover, non-medical staff were not as well aware of the hallmark symptoms, precautionary measures, and hygiene issues, nor did they have the same prevention requirements as medical staff. Research showed that perception of higher risk (33) and lack of professional training (34) were the main occupational factors associated with PTSD. These suggested that the mental well-being of non-medical HCWs warrants more attention. The whole country was shut down, and the greatest responsibility of disease prevention fell to administrative staff. They were burdened with the consequences of clusters of infection, which are unpredictable. The administrative and logistic staff were faced with great pressure from both the upper authorities and the conditions of the epidemic. They were under tremendous pressure, both psychologically and physically. The tasks were arduous. Furthermore, situations of low exposure can also carry the risk of getting affected (35), as there were asymptomatic carriers. Non-medical staff in low-risk areas are easily neglected in an outbreak. We should be more concerned about their mental health.
However, the situation was different for HCWs from high-risk areas, for whom non-medical staff were no longer a risk factor for PTSD symptoms. Almost all the HCWs in Hubei province were drawn from other parts of the country. Hospitals in Hubei, like Huoshenshan and Leishenshan, have fixed management processes. All HCWs were concentrated in designated hospitals, their daily lives and protection requirements were exactly the same, and the division of labor was not that different. Their psychological conditions tend to be similar.
Our data showed that the risk of having PTSD symptoms, including avoidance, intrusion, and hyperarousal, tended to increase with poor sleep quality among HCWs. Research showed that sleep problems can affect the development of PTSD and the severity of symptoms (36). In this case, sleep disturbances are likely to be the risk factor and consequence of PTSD symptoms. Therefore, we could deal with mental health problems by coping with sleep disturbances, which are less stigmatizing.
The study has several limitations. First, it is a cross-sectional study, which cannot investigate the causal relationship. Second, there is self-report bias because all results were from self-reported questionnaires. Besides, setting up a true control group is impossible for our study, for all the HCWs in China were influenced by the COVID-19 outbreak. And we didn't recruit non-health care workers as a control group in this study. In addition, the study was conducted shortly after the outbreak of COVID-19, and the sleep quality and psychological problems of HCWs may not be really reflected in the survey. In addition, the sample of the study is relatively small, which might influence the generalization of the results. Finally, there might be selection bias that could also influence our findings.
Our study indicated the predictors of PTSD symptoms among HCWs during the early stages of COVID-19. The study found that those often neglected, such as non-medical HCWs from low-risk areas, were at high risk for PTSD symptoms. We hope the results will be helpful for psychological professionals and policymakers in developing specific policies and mental health advice for HCWs, especially those with specific characteristics.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
The studies involving human participants were reviewed and approved by Research Ethics Commission of Naval Medical University. The patients/participants provided their written informed consent to participate in this study.
RZ participated in conception, design of the work, data interpretation and analysis, drafting, and revision of the manuscript. TH, XK, JH, and LX participated in the acquisition and interpretation of data. GW, HW, SX, JD, YW, YH, and JX participated in the data analysis and revision of the draft. YT and TS made contributions to the concept and design of the study, acquisition of data, manuscript revision, and supervision. All authors approved the publication of this final version.
This research received funding from Key Scientific and Research Projects of Logistics in PLA (AWS16J033), the General Program of National Natural Science Foundation of China (81372122), and Military Medical Science and Technology Youth Cultivation Plan (2019QNP014).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank all participants and cooperating authors in this study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.696200/full#supplementary-material
HCWs, Health care workers; PTSD, Post-Traumatic Stress Disorder; PSQI, The Pittsburgh Sleep Quality Index; IES-R, The Impact of Event Scale; PHEIC, Public Health Emergency of International Concern; WHO, World Health Organization.
1. World Health Organization. Consensus Document on the Epidemiology of Severe Acute Respiratory Syndrome (SARS). (2020). Available online at: http://www.who.int/csr/sars/en/WHOconsensus.pdf (accessed March 9, 2020).
2. World Health Organization. Pneumonia of Unknown cause – China. (2020). Available online at: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ (accessed March 1, 2020).
3. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/s0140-6736(20)30185-9
4. Berger SA. GIDEON: a comprehensive web-based resource for geographic medicine. Int J Health Geogr. (2005) 4:10. doi: 10.1186/1476-072x-4-10
5. Kam JKM, Chan E, Lee A, Wei VWI, Kwok KO, Lui D, et al. Student nurses' ethical views on responses to the severe acute respiratory syndrome outbreak. Nursing Ethics. (2020) 27:924–34. doi: 10.1177/0969733019895804
6. Koh D, Sng J. Lessons from the past: perspectives on severe acute respiratory syndrome. Asia-Pacific J Public Health. (2010) 22:132S−6. doi: 10.1177/1010539510373010
7. Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. (2020) 13:40. doi: 10.1186/s12245-020-00299-5
8. Ali H, Cole A, Ahmed A, Hamasha S, Panos G. Major stressors and coping strategies of frontline nursing staff during the outbreak of coronavirus disease 2020 (COVID-19) in Alabama. J Multidisciplinary Healthcare. (2020) 13:2057–68. doi: 10.2147/jmdh.S285933
9. Cui Q, Cai ZX, Li JJ, Liu ZC, Sun SR, Chen C, et al. The psychological pressures of breast cancer patients during the COVID-19 outbreak in China-A Comparison With Frontline Female Nurses. Front Psychiatry. (2020) 11:e559701. doi: 10.3389/fpsyt.2020.559701
10. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
11. Orru G, Marzetti F, Conversano C, Vagheggini G, Miccoli M, Ciacchini R, et al. Secondary Traumatic stress and burnout in healthcare workers during COVID-19 outbreak. Int J Environ Res Public Health. (2021) 18:337. doi: 10.3390/ijerph18010337
12. Quigley AL, Stone H, Nguyen PY, Chughtai AA, MacIntyre CR. Estimating the burden of COVID-19 on the Australian healthcare workers and health system during the first six months of the pandemic. Int J Nursing Stud. (2021) 114:103811. doi: 10.1016/j.ijnurstu.2020.103811
13. Chen H, Wang B, Cheng YB, Muhammad B, Li SL, Miao ZG, et al. Prevalence of posttraumatic stress symptoms in health care workers after exposure to patients with COVID-19. Neurobiol Stress. (2020) 13:100261. doi: 10.1016/j.ynstr.2020.100261
14. Zare S, Mohammadi dameneh M, Esmaeili R, Kazemi R, Naseri S, Panahi D. Occupational stress assessment of health care workers (HCWs) facing COVID-19 patients in Kerman province hospitals in Iran. Heliyon. (2021) 7:e07035. doi: 10.1016/j.heliyon.2021.e07035
15. Compean E, Hamner M. Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): Diagnostic and treatment challenges. Prog Neuro-Psychopharmacol Biol Psychiatry. (2019) 88:265–75. doi: 10.1016/j.pnpbp.2018.08.001
16. Wild J, Smith KV, Thompson E, Bear F, Lommen MJJ, Ehlers A. A prospective study of pre-trauma risk factors for post-traumatic stress disorder and depression. Psychol Med. (2016) 46:2571–82. doi: 10.1017/s0033291716000532
17. Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J Affect Disord. (2020) 274:405–10. doi: 10.1016/j.jad.2020.05.081
18. Li WW, Li Y, Yu H, Miller DJ, Rouen C, Yang F. Mental health of chinese people during the COVID-19 pandemic: associations with infection severity of region of residence and filial piety. Front Psychol. (2021) 12:633452. doi: 10.3389/fpsyg.2021.633452
19. Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. (2020) 9:113. doi: 10.1186/s40249-020-00724-0
20. Giardino DL, Huck-Iriart C, Riddick M, Garay A. The endless quarantine: the impact of the COVID-19 outbreak on healthcare workers after three months of mandatory social isolation in Argentina. Sleep Med. (2020) 76:16–25. doi: 10.1016/j.sleep.2020.09.022
21. Liu CY, Yang YZ, Zhang XM, Xu XY, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infection. (2020) 148:e98. doi: 10.1017/s0950268820001107
22. Chew NWS, Lee GKH, Tan BYQ, Jing MX, Goh YH, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immunity. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
23. Leeds JS, Raviprakash V, Jacques T, Scanlon N, Cundall J, Leeds CM. Risk factors for detection of SARS-CoV-2 in healthcare workers during April 2020 in a UK hospital testing programme. EClinicalMedicine. (2020) 26:100513. doi: 10.1016/j.eclinm.2020.100513
24. Carmassi C, Foghi C, Dell'Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. (2020) 292:113312. doi: 10.1016/j.psychres.2020.113312
25. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index - a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
26. Asif IM, Price DE, Ewing A, Rao AL, Harmon KG, Drezner JA. The impact of diagnosis: measuring the psychological response to being diagnosed with serious or potentially lethal cardiac disease in young competitive athletes. Br J Sports Med. (2016) 50:163. doi: 10.1136/bjsports-2015-095560
27. Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. (1993) 138:923–36. doi: 10.1093/oxfordjournals.aje.a116813
28. McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KWT, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canad J Psychiatry-Revue Canadienne De Psychiatrie. (2007) 52:241–7. doi: 10.1177/070674370705200406
29. Li ZY, Ge JW, Yang ML, Feng JP, Qiao M, Jiang RY, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immunity. (2020) 88:916–9. doi: 10.1016/j.bbi.2020.03.007
30. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
31. Tam CWC, Pang EPF, Lam LCW, Chiu HFK. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol Med. (2004) 34:1197–204. doi: 10.1017/s0033291704002247
32. Wang M, Zhao Q, Hu C, Wang Y, Cao J, Huang S, et al. Prevalence of psychological disorders in the COVID-19 epidemic in China: A real world cross-sectional study. J Affect Disord. (2021) 281:312–20. doi: 10.1016/j.jad.2020.11.118
33. Wu P, Fang YY, Guan ZQ, Fan B, Kong JH, Yao ZL, et al. The psychological impact of the sars epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Canad J Psychiatry-Revue Canadienne De Psychiatrie. (2009) 54:302–11. doi: 10.1177/070674370905400504
34. Tang LL, Pan LL, Yuan LP, Zha L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int J Nursing Sci. (2017) 4:63–7. doi: 10.1016/j.ijnss.2016.12.002
35. Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philo Transact R Soc B-Biol Sci. (2004) 359:1117–25. doi: 10.1098/rstb.2004.1483
Keywords: COVID-19, healthcare workers, post-traumatic stress disorder, sleep, avoidance, intrusion, hyperarousal
Citation: Zhang R, Hou T, Kong X, Wang G, Wang H, Xu S, Xu J, He J, Xiao L, Wang Y, Du J, Huang Y, Su T and Tang Y (2021) PTSD Among Healthcare Workers During the COVID-19 Outbreak: A Study Raises Concern for Non-medical Staff in Low-Risk Areas. Front. Psychiatry 12:696200. doi: 10.3389/fpsyt.2021.696200
Received: 16 April 2021; Accepted: 03 June 2021;
Published: 12 July 2021.
Edited by:
Ghorbangol Ashabi, Tehran University of Medical Sciences, IranReviewed by:
Andreas Chatzittofis, University of Cyprus, CyprusCopyright © 2021 Zhang, Hou, Kong, Wang, Wang, Xu, Xu, He, Xiao, Wang, Du, Huang, Su and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunxiang Tang, dGFuZ3l1bjc2MzNAc2luYS5jb20=; Tong Su, c3V0b25nLTIwMDZAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.