
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 22 June 2021
Sec. Mood Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.684579
This article is part of the Research Topic Neurological and Clinical Aspects of Perinatal Mental Health View all 9 articles
 Alexia Koukopoulos1,2†
Alexia Koukopoulos1,2† Cristina Mazza3
Cristina Mazza3 Lavinia De Chiara2,4†
Lavinia De Chiara2,4† Gabriele Sani5,6
Gabriele Sani5,6 Alessio Simonetti1,2,7
Alessio Simonetti1,2,7 Georgios D. Kotzalidis2,4*
Georgios D. Kotzalidis2,4* Giulia Armani4,8
Giulia Armani4,8 Gemma Callovini2,9
Gemma Callovini2,9 Marco Bonito10
Marco Bonito10 Giovanna Parmigiani4
Giovanna Parmigiani4 Stefano Ferracuti1
Stefano Ferracuti1 Susanne Somerville11
Susanne Somerville11 Paolo Roma1
Paolo Roma1 Gloria Angeletti2,4
Gloria Angeletti2,4Literature stressed the importance of using valid, reliable measures to assess anxiety in the perinatal period, like the self-rated Perinatal Anxiety Screening Scale (PASS). We aimed to examine the psychometric properties of the Italian PASS version in a sample of Italian women undergoing mental health screening during their third trimester of pregnancy and its diagnostic accuracy in a control perinatal sample of psychiatric outpatients. Sample comprised 289 women aged 33.17 ± 5.08, range 19–46 years, undergoing fetal monitoring during their third trimester of pregnancy, with 49 of them retested 6 months postpartum. Controls were 60 antenatal or postnatal psychiatric outpatients aged 35.71 ± 5.02, range 22–50 years. Groups were assessed through identical self- and clinician-rating scales. Confirmatory Factor Analysis (CFA), Principal Component Analysis (PCA), Pearson's correlations and receiver operating characteristic were conducted for PASS. PCA and CPA confirmed four-factor structure with slight differences from the original version. Construct validity and test-retest reliability were supported. Cut-off was 26. The PASS correlated with principal anxiety scales. Despite small sample size, findings confirm reliability and validity of the Italian PASS version in assessing anxiety symptoms in the perinatal period. Its incorporation in perinatal care will improve future mother and child psychological health.
Studies on perinatal psychiatric disorders have focused for several years on depressive and psychotic symptoms (1, 2), with less attention paid to perinatal anxiety, probably due to the overlap of anxiety symptoms on depressive syndromes (3, 4). However, anxiety may be more common than depression among women during the first perinatal period (5–7) and significantly higher in the maternal population than in the general adult population (8). This could be due to the higher prevalence of medical conditions during pregnancy, that predispose to anxiety disorders (9). Furthermore, perinatal anxiety is associated with obstetric problems and can negatively affect offspring's emotional and cognitive development (10–19), possibly due also to connectivity changes shown in 32-week fetal brain (20). Taken together, these data suggest that anxiety in the perinatal period should be considered on its own.
Available data suggest that 13–25% of pregnant women (21, 22) and 11–21% of postpartum women (23) experience clinically significant anxiety, with an estimated 20.7% for having at least one anxiety disorder in the peripartum (95% highest density interval from 16.7 to 25.4%) (24). When diagnostic interviews were employed, the prevalence rate for any anxiety disorder during the first trimester was 18%, decreasing marginally to approximately 15% in the final two trimesters of pregnancy, with a continuous decrease postnatal pattern across the 1st year (8). A meta-analysis estimated the prevalence of anxiety disorders in the postpartum to be around 8.5% (25), compared to 10–15% of depression (26). A large percentage of perinatal women who do not meet diagnostic criteria for a specific anxiety disorder, experience clinically significant anxiety symptoms, which they distinguish from anxiety experienced at other times of life (27, 28). Pregnant women often have concerns about the health and well-being of their babies, labor and delivery, finances, and the maternal role and responsibilities. These concerns are termed pregnancy-related anxiety (PrA) or pregnancy-specific anxiety (29). Despite its demonstrated importance, pregnancy-specific anxiety is a relatively new concept in maternal and child health research (30). Clinically relevant symptoms of pregnancy-specific anxiety will differ from common worries and concerns by virtue of their intensity, persistence, and impact on a woman's functioning (31).
Perinatal anxiety has typically been measured by standardized anxiety scales. Controversy exists over which screening tools should be used during the perinatal period to detect perinatal anxiety and the cutoffs that should be adopted for identifying women at risk. General anxiety measures may include questions about physical symptoms of anxiety common in pregnancy. Hence it has been suggested that PrA needs its own scale, as it appears to have distinctive features that are not captured by the standardized anxiety scales (32).
In recent years, maternal mental health investigators have been trying to improve knowledge of perinatal anxiety and to develop screening tools for identification of specific symptoms. A good understanding of pregnancy related anxiety is of key importance so to carry out preventive interventions or treatment strategies. The American Congress of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) widely recommend routine screening for anxiety at least once during the perinatal period with a standardized, validated tool (33, 34).
In the search for specific anxiety rating scales in the perinatal period, two scales were developed, the Postpartum Worry Scale (35) and the Postpartum Specific Anxiety Scale (36); however, these have not been validated for the entire perinatal period. The Perinatal Anxiety Screening Scale [PASS; (37, 38)] is a self-rating scale used to screen for anxiety disorders in the entire perinatal period. It has a four-factor structure, i.e., (1) acute anxiety and adjustment, (2) general worry and specific fears, (3) perfectionism, control, and trauma and (4) social anxiety.
Given the importance to assess anxiety symptoms specifically during the perinatal period, the main aim of the present cross-sectional/longitudinal study was to validate the psychometric properties of the self-rated PASS in a sample of Italian women undergoing mental health screening during their third trimester of pregnancy, and in those agreeing to be retested, 6 months postpartum. The second aim was to investigate its diagnostic accuracy in a clinical perinatal sample and compare it with the HAM-A, a gold standard clinician-rated instrument.
The study involved two separate groups of participants. Demographic data of both samples are shown in Table 1. Participants provided written informed consent, in accordance with all applicable regulatory and Good Clinical Practice guidelines and in full respect of the Ethical Principles for Medical Research Involving Human Subjects, as adopted by the 18th World Medical Association General Assembly (WMA GA), Helsinki, Finland, June 1964, and subsequently amended by the 64th WMA GA, Fortaleza, Brazil, October 2013. It was approved by the local ethics committees (Board of the Sant'Andrea Hospital, Rome and San Pietro Fatebenefratelli Hospital, Rome).
The screening sample included Italian-fluent adult women of the general population screened once during their third trimester of pregnancy (T0) and again 6 months postpartum (T1). We recruited all consecutive women attending fetal monitoring at the Gynecology and Obstetrics unit of San Pietro Fatebenefratelli Hospital of Rome between July and December 2019 during their routine third trimester screening.
Exclusion criteria were failure to provide free informed consent and incomplete comprehension of the Italian language that prevented participants from completing the questionnaires. Participants with an incomplete PASS were also excluded from the final analysis.
Antenatal participants who had consented to being contacted in the postnatal period, were phoned by two trained psychologists of our Center for Prevention and Treatment of Women's Mental Health, 6 months following the birth of their baby and invited to complete the questionnaires again through an online system (Google Form).
CS included antenatal and postnatal psychiatric outpatients referring to the Center for Prevention and Treatment of Women's Mental Health at Sant'Andrea Hospital of Rome (Supplementary Table 1).
Screening tools were administered by physicians and psychologists of our Center for Prevention and Treatment of Women's Mental Health Problems at Sant'Andrea Hospital, Rome, Italy.
Both groups were evaluated using the sociodemographic, clinical and obstetric data collection sheet (Perinatal Interview; PI), the Perinatal Anxiety Screening Scale (PASS), the Edinburgh Postnatal Depression Scale (EPDS), the Temperament Evaluation of the Memphis, Pisa, Paris and San Diego-Autoquestionnaire (TEMPS-A), the Hypomania CheckList-32 (HCL-32), the Zung Self-Rating Anxiety Scale (SAS), and the Mood Disorders Questionnaire (MDQ).
CS patients were also evaluated with The Hamilton Rating Scale for Anxiety [HAM-A; (39)], a semi-structured interview. To assess anxiety diagnosis among patients in the CS group we used the Structured Clinical Interview for DSM-5 (SCID-5).
Measures, valid for the purpose of screening symptoms of depression and anxiety, took 30–50 min to complete. Included measures were the following:
The Perinatal Anxiety Screening Scale (PASS; 37) is a 31-item self-rated questionnaire investigating anxiety symptoms during the last month in child-bearing women. Each item is rated on a Likert 0–3 scale; the total score is the addition of scores on each item, with higher scores representing more anxiety. Scores may range 0–93. Cutoff for clinical anxiety is ≥26. A further study stratified the investigated population into minimal anxiety (scoring 0–20), mild–moderate anxiety (21–41), and severe anxiety symptoms (42–93) (38). The scale showed adequate test–retest reliability (rho = 0.74), a sensitivity of 70% and specificity of 30% at the 26 cutoff. The PASS showed adequate convergent validity, with its global scores significantly correlating with the anxiety subscale of the EPDS and the total EPDS scores, and with both STAI-State and STAI-Trait scores; its reliability is rated excellent for the entire scale (Cronbach's α = 0.96). Its best fit is a four-factor structure explaining 59.37% of total variance. Factor 1 (acute anxiety and adjustment) consists of 8 items related to panic, dissociation and adjustment, factor 2 (general worry and specific fears) includes 10 items related to generalized anxiety (GAD) and phobia, factor 3 (perfectionism, control and trauma) consists of eight items related to obsessive-compulsive (OCD) and posttraumatic symptoms, and factor 4 (social anxiety) is composed of five items focusing on social anxiety (37).
The Edinburgh Postnatal Depression Scale [EPDS; (40)] is a 10-item self-report questionnaire administered to screen for depressive symptoms over the past week. The EPDS has been shown to have high reliability and adequate sensitivity and specificity for detecting depressive symptoms in both the antenatal and postnatal periods (41, 42). A score of 10 or greater suggests possible depression. Scores above 12 are likely depressive illness of varying severity. We used the recommended score of 13 or more that indicate probable major depression in postnatal Italian-speaking women (43). Three items of the EPDS (EPDS 3-A, items 3, 4, and 5) have been found to cluster together on an anxiety factor in postpartum women with optimum cut-off scores ranging from 4 to 6 in different studies (44–47). However, the authors maintain that the scale does not confirm an anxiety disorder and does not distinguish whether anxiety scores on these three items are a feature of depression or a distinct entity.
The Temperament Evaluation of the Memphis, Pisa, Paris and San Diego-Autoquestionnaire [TEMPS-A; (48)], is a 110-item yes-or-no self-report questionnaire designed to assess affective temperament in psychiatric and healthy subjects. It consists of five temperament-traits, i.e., depressive (D), cyclothymic (C), hyperthymic (H), irritable (I), and anxious (A) subscales. The prevailing temperament is considered the one on which the completer obtains the higher score. We used the validated Italian version (49). The instrument has shown intrasubject diachronic stability (50, 51).
The Hypomania CheckLList-32 (52) is a self-rating questionnaire investigating lifetime history of hypomanic symptoms. It may be applied to normal people and outpatients. However, it was mainly developed for screening patients with a diagnosis of depression (major depressive disorder, dysthymia, “minor” depression, and recurrent brief depression) for hypomanic symptoms. The total score is the number of positive answers to the 32 items listed in question 3 of the second revision of the tool (HCL-32-R2) (53). Individuals scoring ≥14 are potentially with bipolar disorder/diathesis and should be carefully interviewed. The R2 version, which we used in this study, showed good psychometric properties (54).
The Zung Self-Rating Anxiety Scale [SAS; (55)] is a 20-item self-report assessment tool built to measure state anxiety levels, based on scoring in four groups of manifestations: cognitive, autonomic, motor and central nervous system symptoms. Raw scores range from 20 to 80; scores between 20 and 44 are considered to be in the normal range, between 45 and 59 indicate mild-to-moderate anxiety, 60–74 indicate marked-to-severe anxiety, and ≥75 extreme anxiety. The initial cutoff was 50 (56), but the author later lowered it to 45 (57). The best cutoff was later proposed to be 40 for clinical settings and 36 for screening purposes (58). The instrument is suited to investigate anxiety disorders (59) and showed strong correlations with other similar instruments (60).
The Mood Disorder Questionnaire [MDQ; (61)] is a 13-item self-report, validated questionnaire (62) designed to assess bipolar diathesis in psychiatric and healthy subjects. Its specificity was found to be 97% and its sensitivity 70% for bipolar type I disorder, much less for bipolar type II disorder (52%) and even less (31%) for bipolar disorder not otherwise specified (63). It is able to detect bipolar propensity (64). The test has shown convergent validity (65) and the same sensitivity as the HCL-32, but better specificity (66).
The Hamilton Rating Scale for Anxiety [HAM-A; (39)] was one of the first clinician report rating scales developed to measure the severity of both psychic and somatic anxiety symptoms, and is still widely used today in both clinical and research settings. The scale consists of 14 items, with a total score of 17 or less indicating mild anxiety severity, 18–24 mild-to-moderate, 25–30 moderate-to-severe, and more than 30 severe anxiety.
The Italian translation of the PASS was carried out through a direct and reverse translation process (67). Specifically, a bilingual Italian/English psychologist translated the PASS from English to Italian. After that, a bilingual Italian/English researcher back translated the scale.
After discussing any differences between the two translations with the author of the original version of the scale (Dr. Somerville), the scale was translated again into English by a native speaker researcher, unaware of previous translation processes. The Italian version of the PASS includes 31 items. Items are rated as in the original version.
Confirmatory Factor Analysis (CFA) was conducted using JASP Version 0.13.1 (68). The quality of the measurement model was examined through the fit indices estimates of Comparative Fit Index (CFI), and Root Mean Square Error of Approximation (RMSEA). According to literature (69), a model is considered to have a good fit if the comparative fit index (CFI) are all >0.90; and the root mean square error of approximation (RMSEA) values are approximately 0.06.
Subsequently, the factor structure of the Italian version of the PASS was analyzed using the Principal Component Analysis (PCA) with oblique (Oblimin) rotation, as recommended (70). To enter in a factor, an item should load with a score of ≥0.4. Should an item score ≥0.4 on more than one factor, the item was assigned to the factor where it obtained the higher score.
The convergent and discriminant validity of the Italian version of the PASS has been assessed by conducting Pearson's correlations between the PASS global score and the EPDS, EPDS 3-A, TEMPS-A, HCL-32 and SAS. Point-biserial correlations were compute between PASS global score and MDQ. The cutoff for all correlations was set at p < 0.05.
Test-retest reliability of the PASS was assessed by examining the correlation between the total PASS score in the antenatal and postnatal period for a subsample of participants (N = 49) who completed the PASS both antenatally and postnatally.
To assess the diagnostic accuracy of the PASS and to determine the best cutoff score that optimally detected cases defined by a presence or absence of an DSM-5 diagnosis for an anxiety disorder the receiver operating characteristic (ROC) curve analysis was run for a subsample of 60 with an anxiety disorder diagnosis. The IBM SPSS-25 statistical package (IBM Inc., Armonk, New York, 2017) was used for all these analyses.
SS included 312 Italian-speaking adult women of the general population screened once at T0; those 49 who agreed with follow-up were again tested at T1. Participants with an incomplete PASS were excluded from the final analysis (N = 23), hence, the final sample consisted of 289 women (Mage = 33.17 years; SDage = 5.08, range, 19–46). All women had currently a partner (Mage = 36.27 years, SDage = 5.64, range, 21–54).
CS included 60 (Mage = 35.71 years; SDage = 5.02, range, 22–50) antenatal and postnatal psychiatric outpatients. CS was composed by 23.3% of women with anxiety disorder (N = 14), 13.3% with major depressive disorder (N = 8), 30% with comorbid anxiety and depressive disorders (N = 18), and 33.4% with other psychiatric diagnoses (e.g., psychosis) (N = 20).
Scores obtained on the administered rating scales are shown in Supplementary Table 2. For the MDQ, 22 participants showed a positive result, 190 a negative one.
CFA revealed inadequate fit indexes for the tested four-factors model proposed by Somerville et al. (37) [x2 (428) = 1283.267, p < 0.001, CFI = 0.780, RMSEA = 0.085].
Inter-item correlations were sufficiently large for PCA (Bartlett's test of sphericity= χ2 (465) = 4164.67, p < 0.001). Sampling adequacy was excellent (Kaiser-Meyer-Olkin test, KMO = 0.92). Four factors were retained based on the results of the scree test (71), the Parallel Analysis test and MAP test (72), which cumulatively explained 52.53% of total variance.
An examination of the factor loadings after Oblimin rotation (Table 2) suggested a slightly different factor structure of the PASS compared to the previous identified (37). More in detail, Factor 1 (Anxiety and worry) had 15 items that addressed symptoms of anxiety, dissociative disorder and adjustment difficulties; Factor 2 (Social anxiety) included six items that addressed social anxiety and adjustment difficulties; Factor 3 (Perfectionism and control) had six items that addressed symptoms of OCD; and Factor 4 (Fears) included four items that addressed GAD and specific fears.
Three items with factor loading below the 0.4 threshold were retained due to their clinical relevance. These items were the following: item 15 “Sudden rushes of extreme fear or discomfort,” item 21 “Losing track of time and can't remember what happened,” and item 27 “Difficulty sleeping even when I have the chance to sleep.” There was only one cross-loading item, i.e., item 23, “Avoiding things which concern me” and was retained in the factor showing the highest loading and consistency with clinical anxiety presentations, i.e., Factor 2 (Social anxiety). The four subscales had high reliabilities (Cronbach's α ranged from 0.721 to 0.926) and were weakly to moderately correlated (r values ranged from 0.16 to 0.46). The entire scale showed also excellent reliability (Cronbach's α = 0.929).
The PASS global score was significantly correlated with all the scales employed, except for the TEMPS-A and the MDQ, which are indicative of adequate convergent and discriminant validity (Table 3).
The Pearson correlation coefficients were calculated to assess the test-retest reliability of the PASS for a subsample of participants (N = 49) who completed the PASS antenatally and postnatally (with a 6-month interval). The correlation for the PASS global scores was 0.482, p < 0.001.
In line with the hypothesis, the PASS offers a good diagnostic accuracy within the collected clinical sample. PASS total score showed an AUC value of 0.852 (SE = 0.051) (Figure 1). Additionally, because in a clinical assessment, sensitivity has priority over specificity, given the high cost of false-negative errors, we also identified the PASS cutoff that would yield, in our data, values of sensitivity as close as possible to 90. This value is 25.5 with a positive predictive power (PPP) of 69% and a negative predictive power (NPP) of 93%. For the screening sample, these figures were 77.94 and 86.96%, respectively. The results revealed that the PASS, at the recommended cutoff score of 26 detected correctly 96.9% of women with anxiety disorder, performing better than the EPDS 3-A, SAS and HAM-A. Indeed, EPDS 3-A, with its cutoff of 6, detected 86.7% (AUC = 0.799) of the cases; SAS, with a cutoff of 45 detected 42.9% (AUC = 0.693) of the cases, whereas the HAM-A at a cutoff of 18 detected 88.9% (AUC = 0.714) (Supplementary Table 3). A significant and positive correlation was found between the PASS and the HAM-A (r = 0.577).
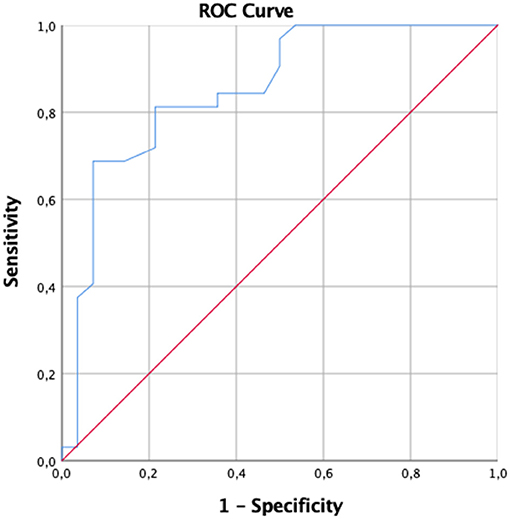
Figure 1. Graphical representation of receiver operator characteristic curve of the PASS total score.
In this study, we showed the validity and reliability of the Italian version of the PASS in assessing anxiety symptoms and disorders in general and clinical perinatal samples and a better diagnostic accuracy than other valid instruments. Factor analysis showed a four-factor structure with PCA, which however differed from the original version, as assessed with CFA. The PASS showed construct validity and convergence with other reliable measures and test-retest reliability; it also showed excellent sensitivity and specificity, as shown by an AUC of 0.85 at the same cutoff of 26, as per the original version. This is above the 0.8 cutoff suggested by Fairbrother et al. (73), it should be noted that in this study, only one, non-specific scale was found to perform above this cutoff, while both EPDS and EPDS 3-A were found to have an AUC of 0.744 and 0.757, respectively.
It is important to assess anxiety symptoms and disorders in perinatal women through valid and reliable measures (32, 74). A careful assessment may provide important information for the medical staff and for women themselves on the challenges and burden experienced with pregnancy and maternity. If perinatal anxiety is detected, women's well-being and motherhood could improve by providing prompt psychological support. From this perspective, we evaluated the psychometric properties of the PASS Italian version in a sample of women undergoing mental health screening during their third trimester of pregnancy. Overall, findings confirm that the Italian version of the PASS is a reliable and valid questionnaire for assessing anxiety symptoms in the perinatal period.
Consistently with the original model (37), the PCA has identified a four-factor structure, slightly different from the previous one in item composition. Slightly different item compositions of the four identified factors were also observed with the Turkish (75), Bangladeshi (76), Iranian (77), and Sri-Lankan versions of the PASS (78), while the Arabic versions diverged, with the Saudi Arabian one agreeing on the four-factor solution (79), while the Lebanese found seven (80) (submitted). However, this is a frequent encounter in literature, especially when some years elapse from one factor analysis to another [cfr. (81) vs, (82)]. The reliability of the scores of the Italian version of the PASS, assessed trough their internal consistency, was excellent or at least good, as indicated by Cronbach's alpha coefficients ranging from 0.72 to 0.93.
Our results supported the convergent validity of the Italian version of the PASS through significant and positive correlation with other measures of anxiety, showing higher correlation values with the EPDS, TEMPS-A and the EPDS 3-A. The PASS total score correlated significantly and positively also with measures of depression. Discriminant validity of the PASS was substantiated by the lack of significant correlations with the MDQ and the TEMPS-A.
Another interesting result emerges from test-retest reliability. Compared to the retest correlation coefficient (r = 0.74) reported by Somerville et al. (37), we found a lower association between the T0 and T1. This lower association with respect to Somerville et al. (37) could be attributed to the antenatal-postnatal interval; in fact, in that study patients were contacted 2–6 months after delivery, while we contacted our subsample 6 months after delivery. The possibly longer interval could account for this slight difference, as anxiety related to childbirth tends to progressively subside after delivery (8).
The PASS had similar sensitivities and specificities in both the SS and the CS, as shown by PPP and NPP; this means that it is suitable for both general screening and clinical application in women with clinically significant anxiety.
Aligning with the validation study (37), the screening accuracy indicated that the Italian PASS performed better in detecting women with anxiety disorder diagnosis than the other measures employed, which are frequently used in clinical practice. It is interesting to notice that we found a positive correlation between the PASS, a self-report measure, and the HAM-A, a clinician-rated instrument. This correlation, together with the higher classification accuracy of the PASS, could support the use of the PASS in clinical settings where saving time and resources for the practitioners are mandatory. Giving higher priority to sensitivity over specificity, we identified an optimal threshold of 26, the same found by Somerville et al. (37). At this cutoff score, 97% of women with an anxiety disorder were detected and, consequently, may benefit from immediate psychological assessment and support. Furthermore, it is worth noting that about 18% of the SS (N = 52 of 289) score above the cutoff of 26, in line with epidemiological data on the prevalence of anxiety disorder in women during the perinatal period.
The main limitation of this study is the small sample size that did not allow for investigating differences among its subgroups.
It is commonly believed that self-rating is inferior to clinician-rating in validity (83); however, this by no means the rule (84), and the combined use of both types of tools has been advocated to rate anxiety (85, 86). We here used the HAM-A to cross-validate the PASS, and the latter outperformed the clinician-rated tool in the CS.
The implications for future research would entail looking at the interventions needed to further decrease the effects of maternal pregnancy anxiety both for parenting style and child's development (87).
The PASS is the first screening and clinical tool available in Italian to assess perinatal anxiety. The PASS is designed for use in heterogeneous populations and could be easily administered by obstetrics staff in everyday clinical practice. A simple screening task completed once per trimester during pregnancy could help clinicians to target women who are most in need of mental support. Furthermore, women who are experiencing pregnancy-specific anxiety can recognize themselves over the items of the PASS.
We strengthened the validation of the Italian version of the PASS using a standardized diagnostic interview, the HAM-A in a clinical population and obtained a good convergence.
Due to our design, we did not assess the validity of the instrument in the same woman across the entire prepartum and postpartum periods, so we have to limit our conclusions to late-pregnancy and 6 months postpartum. Future studies will confirm and extend the validity to the entire perinatal period.
Assessing anxiety in prepartum and postpartum with specific scales is crucial for new mothers' mental health and new-born babies' upbringing. The PASS showed to be reliable to this end more than other existing instruments. We suggest that its use should enter standard clinical practice.
The datasets presented for this article are available and contained in the online Supplement. Further requests regarding datasets should be directed to Z2lvcmdpby5rb3R6YWxpZGlzQHVuaXJvbWExLml0.
The studies involving human participants were reviewed and approved by Board of the Sant'Andrea Hospital, Rome and San Pietro Fatebenefratelli Hospital, Rome. The patients/participants provided their written informed consent to participate in this study.
AK, LD, and GAn conceived and designed the study. CM, LD, GK, and AS performed statistics. AS, GK, GAr, and GC performed literature searches. AK, LD, GAn, GAr, GC, and MB saw the patients involved in the study. GAn and MB addressed ethical issues. GK, GAr, LD, AK, and GAn translated the scale. AK, LD, CM, and GAn wrote the first draft. AK, LD, GS, AS, GP, and GK wrote the Introduction. CM, LD, GK, GAr, GP, and GC wrote the Methods and Results. SF, AK, LD, PR, SS, GP, GK, GAr, and GC wrote the Discussion. SS, AK, LD, GK, SF, GS, AS, and GAn supervised the final draft. All authors viewed and approved the final version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We wish to thank all our participants and the Staff of the Department of Obstetrics of the San Pietro Hospital-Fatebenefratelli and of the Sant'Andrea Unit of Psychiatry. We appreciate the help of our secretary Ms. Tatiana Renzi for providing us useful tips for completing our manuscript. We were also grateful to Ms. Mimma Ariano, Ms. Ales Casciaro, Ms. Teresa Prioreschi, and Ms. Susanna Rospo, Librarians of the Sant'Andrea Hospital, School of Medicine and Psychology, Sapienza University, Rome, for rendering precious bibliographical material accessible.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.684579/full#supplementary-material
1. Tebeka S, Strat YL, Dubertret C. Developmental trajectories of pregnant and postpartum depression in an epidemiologic survey. J Affect Disord. (2016) 203:62–68. doi: 10.1016/j.jad.2016.05.058
2. VanderKruik R, Barreix M, Chou D, Allen T, Say L, Cohen S, et al. The global prevalence of postpartum psychosis: a systematic review. BMC Psychiatry. (2017) 17:272. doi: 10.1186/s12888-017-1427-7
3. Wenzel A, Haugen EN, Jackson LC, Brendle JR. Anxiety symptoms and disorders at eight weeks postpartum. J Anxiety Disord. (2005) 19:295–311. doi: 10.1016/j.janxdis.2004.04.001
4. Falah-Hassani K, Shiri R, Dennis CL. Prevalence and risk factors for comorbid postpartum depressive symptomatology and anxiety. J Affect Disord. (2016) 198:142–7. doi: 10.1016/j.jad.2016.03.010
5. Grigoriadis S, de Camps Meschino D, Barrons E, Bradley L, Eady A, Fishell A, et al. Mood and anxiety disorders in a sample of Canadian perinatal women referred for psychiatric care. Arch Womens Ment Health. (2011) 14:325–33. doi: 10.1007/s00737-011-0223-5
6. Giardinelli L, Innocenti A, Benni L, Stefanini MC, Lino G, Lunardi C, et al. Depression and anxiety in perinatal period: prevalence and risk factors in an Italian sample. Arch Womens Ment Health. (2012) 15:21–30. doi: 10.1007/s00737-011-0249-8
7. Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH. Perinatal anxiety disorder prevalence and incidence. J Affect Disord. (2016) 200:148–55. doi: 10.1016/j.jad.2015.12.082
8. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
9. Fairbrother N, Young AH, Zhang A, Janssen P, Antony MM. The prevalence and incidence of perinatal anxiety disorders among women experiencing a medically complicated pregnancy. Arch Womens Ment Health. (2017) 20:311–9. doi: 10.1007/s00737-016-0704-7
10. O'Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children's behavioural/emotional problems at 4 years. Report from the Avon Longitudinal Study of Parents Children. Br J Psychiatry. (2002) 180:502–8. doi: 10.1192/bjp.180.6.502
11. O'Connor TG, Heron J, Golding J, Glover V, ALSPAC., Study Team. Maternal antenatal anxiety behavioural/emotional problems in children: a test of a programming hypothesis. J Child Psychol Psychiatry. (2003) 44:1025–36. doi: 10.1111/1469-7610.00187
12. Davis E, Snidman N, Wadhwa P, Glynn LM, Dunkel Schetter C, Sandman CA. Prenatal maternal anxiety and depression predict negative behavioral reactivity in infancy. Infancy. (2004) 6:319–31. doi: 10.1207/s15327078in0603_1
13. Glasheen C, Richardson GA, Fabio A. A systematic review of the effects of postnatal maternal anxiety on children. Arch Womens Ment Health. (2010) 13:61–74. doi: 10.1007/s00737-009-0109-y
14. Van Batenburg-Eddes T, Brion MJ, Henrichs J, Jaddoe VW, Hofman A, Verhulst FC, et al. Parental depressive and anxiety symptoms during pregnancy and attention problems in children: a cross-cohort consistency study. J Child Psychol Psychiatry. (2013) 54:591–600. doi: 10.1111/jcpp.12023
15. Farr SL, Dietz PM, O'Hara MW, Burley K, Ko JY. Postpartum anxiety and comorbid depression in a population-based sample of women. J Womens Health (Larchmt). (2014) 23:120–8. doi: 10.1089/jwh.2013.4438
16. Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. (2014) 384:1800–19. doi: 10.1016/S0140-6736(14)61277-0
17. Ding XX, Wu YL, Xu SJ, Zhu RP, Jia XM, Zhang SF, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. (2014) 159:103–10. doi: 10.1016/j.jad.2014.02.027
18. Christian LM. Effects of stress and depression on inflammatory immune parameters in pregnancy. Am J Obstet Gynecol. (2014) 211:275–7. doi: 10.1016/j.ajog.2014.06.042
19. Field T. Prenatal anxiety effects: a review. Infant Behav Dev. (2017) 49:120–8. doi: 10.1016/j.infbeh.2017.08.008
20. De Asis-Cruz J, Krishnamurthy D, Zhao L, Kapse K, Vezina G, Andescavage N, et al. Association of prenatal maternal anxiety with fetal regional brain connectivity. JAMA Netw Open. (2020) 3:e2022349. doi: 10.1001/jamanetworkopen.2020.22349
21. Woods SM, Melville JL, Guo Y, Fan MY, Gavin A. Psychosocial stress during pregnancy. Am J Obstet Gynecol. (2010) 202:61.e1–7. doi: 10.1016/j.ajog.2009.07.041
22. Verly-Miguel MVB, Farias DR, Pinto T de JP, Lepsch J, Nardi AE. Kac G. Serum docosahexaenoic acid (DHA) is inversely associated with anxiety disorders in early pregnancy. J Anxiety Disord. (2015) 30:34–40. doi: 10.1016/j.janxdis.2014.12.002
23. Kang YT, Yao Y, Dou J, Guo X, Li SY, Zhao CN, et al. Prevalence and risk factors of maternal anxiety in late pregnancy in China. Int J Environ Res Public Health. (2016) 13:468. doi: 10.3390/ijerph13050468
24. Fawcett EJ, Fairbrother N, Cox ML, White IR, Fawcett JM. The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate Bayesian meta-analysis. J Clin Psychiatry. (2019) 80:18r12527. doi: 10.4088/JCP.18r12527
25. Goodman JH, Watson GR, Stubbs B. Anxiety disorders in postpartum women: a systematic review and meta-analysis. J Affect Disord. (2016) 203:292–331. doi: 10.1016/j.jad.2016.05.033
26. Tahirkheli NN, Cherry AS, Tackett AP, McCaffree MA, Gillaspy SR. Postpartum depression on the neonatal intensive care unit: current perspectives. Int J Womens Health. (2014) 6:975–87. doi: 10.2147/IJWH.S54666
27. Huizink AC, Mulder EJ, Robles de Medina PG, Visser GH, Buitelaar JK. Is pregnancy anxiety a distinctive syndrome? Early Hum Dev. (2004) 79:81–91. doi: 10.1016/j.earlhumdev.2004.04.014
28. Phillips J, Sharpe L, Matthey S, Charles M. Maternally focused worry. Arch Womens Ment Health. (2009) 12:409–18. doi: 10.1007/s00737-009-0091-4
29. Accortt EE, Wong MS. It is time for routine screening for perinatal mood and anxiety disorders in obstetrics and gynecology settings. Obstet Gynecol Surv. (2017) 72:553–68. doi: 10.1097/OGX.0000000000000477
30. Guardino CM, Dunkel Schetter C. Understanding Pregnancy Anxiety: Concepts, Correlates and Consequences. Zero to Three (2014). p. 12–21. Available online at: https://www.researchgate.net/publication/285496474_Understanding_pregnancy_anxiety_concepts_correlates_and_consequences (accessed June 3, 2021).
31. Thorsness KR, Watson C, LaRusso EM. Perinatal anxiety: approach to diagnosis and management in the obstetric setting. Am J Obstet Gynecol. (2018) 219:326–45. doi: 10.1016/j.ajog.2018.05.017
32. Blackmore ER, Gustafsson H, Gilchrist M, Wyman CG, O'Connor T. Pregnancy-related anxiety: evidence of distinct clinical significance from a prospective longitudinal study. J Affect Disord. (2016) 197:251–8. doi: 10.1016/j.jad.2016.03.008
33. Committee on Obstetric Practice. The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstet Gynecol. (2015) 125:1268–71. doi: 10.1097/01.AOG.0000465192.34779.dc
34. Siu AL, US Preventive Services Task Force (USPSTF);, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, et al. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. (2016) 315:380–7. doi: 10.1001/jama.2015.18392
35. Moran TE, Polanin JR, Wenzel A. The Postpartum Worry Scale-Revised: an initial validation of a measure of postpartum worry. Arch Womens Ment Health. (2014) 17:41–8. doi: 10.1007/s00737-013-0380-9
36. Fallon V, Halford JCG, Bennett KM, Harrold JA. The Postpartum Specific Anxiety Scale: development and preliminary validation. Arch Womens Ment Health. (2016) 19:1079–90. doi: 10.1007/s00737-016-0658-9
37. Somerville S, Dedman K, Hagan R, Oxnam E, Wettinger M, Byrne S, et al. The Perinatal Anxiety Screening Scale: development and preliminary validation. Arch Womens Ment Health. (2014) 17:443–54. doi: 10.1007/s00737-014-0425-8
38. Somerville S, Byrne SL, Dedman K, Hagan R, Coo S, Oxnam E, et al. Detecting the severity of perinatal anxiety with the Perinatal Anxiety Screening Scale (PASS). J Affect Disord. (2015) 186:18–25. doi: 10.1016/j.jad.2015.07.012
39. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
40. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
41. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh depression scale (EPDS). J Reprod Infant Psychol. (1990) 8:99–107. doi: 10.1080/02646839008403615
42. McBride HL, Wiens RM, McDonald MJ, Cox DW, Chan EKH. The Edinburgh Postnatal Depression Scale (EPDS): a review of the reported validity evidence. In: Zumbo BD. Chan EKH, editors. Validity and Validation in Social, Behavioral, Health Sciences. Social Indicators Research Series 54. Cham (CH): Springer International Publishing Switzerland (2014). p. 157–74. doi: 10.1007/978-3-319-07794-9_9
43. Benvenuti P, Ferrara M, Niccolai C, Valoriani V, Cox JL. The Edinburgh Postnatal Depression Scale: validation for an Italian sample. J Affect Disord. (1999) 53:137–41. doi: 10.1016/S0165-0327(98)00102-5
44. Ross LE, Gilbert Evans SE, Sellers EM, Romach MK. Measurement issues in postpartum depression part 1: anxiety as a feature of postpartum depression. Arch Womens Ment Health. (2003) 6:51–7. doi: 10.1007/s00737-002-0155-1
45. Matthey S. Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders. Depress Anxiety. (2008) 25:926–31. doi: 10.1002/da.20415
46. Phillips J, Charles M, Sharpe L, Matthey S. Validation of the subscales of the Edinburgh Postnatal Depression Scale in a sample of women with unsettled infants. J Affect Disord. (2009) 118:101–12. doi: 10.1016/j.jad.2009.02.004
47. Matthey S, Fisher J, Rowe H. Using the Edinburgh postnatal depression scale to screen for anxiety disorders: conceptual and methodological considerations. J Affect Disord. (2013) 146:224–30. doi: 10.1016/j.jad.2012.09.009
48. Akiskal HS, Akiskal KK, Haykal RF, Manning JS, Connor PD. TEMPS-A: progress towards validation of a self-rated clinical version of the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J Affect Disord. (2005) 85:3–16. doi: 10.1016/j.jad.2004.12.001
49. Pompili M, Girardi P, Tatarelli R, Iliceto P, De Pisa E, Tondo L, et al. TEMPS-A (Rome): psychometric validation of affective temperaments in clinically well subjects in mid- and south Italy. J Affect Disord. (2008) 107:63–75. doi: 10.1016/j.jad.2007.07.031
50. Dembińska-Krajewska D, Rybakowski J. Skala TEMPS-A (Temperament Evaluation of Memphis, Pisa, Paris and San Diego Autoquestionnaire) – wazne narzedzie do badania temperamentów afektywnych [The Temperament Evaluation of Memphis, Pisa and San Diego Autoquestionnaire (TEMPS-A)—an important tool to study affective temperaments–Polish]. Psychiatr Pol. (2014) 48:261–76.
51. Jović J, Hinić D, Corac A, Akiskal HS, Akiskal K, Maremmani I, et al. The development of temperament evaluation of Memphis, Pisa, Paris, and San Diego - Auto-questionnaire for Adolescents (A-TEMPS-A) in a Serbian Sample. Psychiatr Danub. (2019) 31:308–15. doi: 10.1037/t76127-000
52. Angst J, Adolfsson R, Benazzi F, Gamma A, Hantouche E, Meyer TD, et al. The HCL-32: towards a self-assessment tool for hypomanic symptoms in outpatients. J Affect Disord. (2005) 88:217–33. doi: 10.1016/j.jad.2005.05.011
53. Angst J, Azorin JM, Bowden CL, Perugi G, Vieta E, Gamma A, et al. Prevalence and characteristics of undiagnosed bipolar disorders in patients with a major depressive episode: the BRIDGE study. Arch Gen Psychiatry. (2011) 68:791–8. doi: 10.1001/archgenpsychiatry.2011.87
54. Yoon BH, Angst J, Bahk WM, Wang HR, Bae SO, Kim MD, et al. Psychometric properties of the Hypomania Checklist-32 in Korean patients with mood disorders. Clin Psychopharmacol Neurosci. (2017) 15:352–60. doi: 10.9758/cpn.2017.15.4.352
55. Zung WWK. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
56. Zung WWK. The measurement of affects: depression and anxiety. Mod Probl Pharmacopsychiatry. (1974) 7:170–88. doi: 10.1159/000395075
58. Dunstan DA, Scott N. Norms for Zung's self-rating anxiety scale. BMC Psychiatry. (2020) 20:90. doi: 10.1186/s12888-019-2427-6
59. Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. (2017) 17:329. doi: 10.1186/s12888-017-1489-6
60. Tanaka-Matsumi J, Kameoka VA. Reliabilities and concurrent validities of popular self-report measures of depression, anxiety, social desirability. J Consult Clin Psychol. (1986) 54:328–33. doi: 10.1037/0022-006X.54.3.328
61. Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck E Jr., et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. (2000) 157:1873–5. doi: 10.1176/appi.ajp.157.11.1873
62. Hirschfeld RM, Holzer C, Calabrese JR, Weissman M, Reed M, Davies M, et al. Validity of the mood disorder questionnaire: a general population study. Am J Psychiatry. (2003) 160:178–80. doi: 10.1176/appi.ajp.160.1.178
63. Zaratiegui RM, Vázquez GH, Lorenzo LS, Marinelli M, Aguayo S, Strejilevich SA, et al. Sensitivity and specificity of the mood disorder questionnaire and the bipolar spectrum diagnostic scale in Argentinean patients with mood disorders. J Affect Disord. (2011) 132:445–9. doi: 10.1016/j.jad.2011.03.014
64. Glaus J, Van Meter A, Cui L, Marangoni C, Merikangas KR. Factorial structure and familial aggregation of the Hypomania Checklist-32 (HCL-32): results of the NIMH Family Study of Affective Spectrum Disorders. Compr Psychiatry. (2018) 84:7–14. doi: 10.1016/j.comppsych.2018.03.010
65. Leão IA, Del Porto JA. Cross validation with the mood disorder questionnaire (MDQ) of an instrument for the detection of hypomania in Brazil: The 32 item hypomania symptom check-list, first Revision (HCI-32-R1). J Affect Disord. (2012) 140:215–21. doi: 10.1016/j.jad.2011.12.033
66. Wang Y-Y, Xu D-D, Liu R, Yang Y, Grover S, Ungvari GS, et al. Comparison of the screening ability between the 32-item Hypomania Checklist (HCL-32) and the Mood Disorder Questionnaire (MDQ) for bipolar disorder: a meta-analysis and systematic review. Psychiatry Res. (2019) 273:461–6. doi: 10.1016/j.psychres.2019.01.061
67. Behling O, Law KS. Translating Questionnaires and Other Research Instruments: Problems and Solutions. Thousand Oaks, CA: SAGE Publications, Inc. (2000). doi: 10.4135/9781412986373
68. JASP Team. JASP (Version 0.13.1) [Computer software]. Released July 16th, 2020. Universiteit van Amsterdam, Department of Psychological Methods, Amsterdam, NL (2020). Available online at: https://jasp-stats.org/
69. Hu L, Bentler PM. Cuto? criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
71. Cattell RB. The scree test for the number of factors. Multivariate Behav Res. (1966) 1:245–76. doi: 10.1207/s15327906mbr0102_10
72. Velicer WF, Eaton CA, Fava JL. Construct explication through factor or component analysis: a review evaluation of alternative procedures for determining the number of factors or components. In: Goffin RD, Helmes E, editors. Problems and Solutions in Human Assessment: Honoring Douglas N Jackson at Seventy. Boston, MA: Kluwer Academic Publishers (2000). p. 41–71. doi: 10.1007/978-1-4615-4397-8_3
73. Fairbrother N, Corbyn B, Thordarson DS, Ma A, Surm D. Screening for perinatal anxiety disorders: room to grow. J Affect Disord. (2019) 250:363–70. doi: 10.1016/j.jad.2019.03.052
74. Giakoumaki O, Vasilaki K, Lili L, Skouroliakou M, Liosis G. The role of maternal anxiety in the early postpartum period: screening for anxiety and depressive symptomatology in Greece. J Psychosom Obstet Gynaecol. (2009) 30:21–8. doi: 10.1080/01674820802604839
75. Yazici E, Pek TM, Yuvaci HU, Köse E, Cevrioglu S, Yazici AB, et al. Perinatal Anxiety Screening Scale validity and reliability study in Turkish (PASS-TR validity and reliability). Psychiatry Clin Psychopharmacol. (2018) 29:609–17. doi: 10.1080/24750573.2018.1506247
76. Yasmin F, Islam S. Adaptation of the perinatal anxiety screening scale in Bangladeshi context. Psychol Psychol Res Int J. (2018) 3:000144. doi: 10.23880/PPRIJ-16000144
77. Barzgar-Molan S, Farshbaf-Khalili A, Asghari Jafarabadi M, Babapour J, Yavarikia P. Psychometric properties of the Iranian version of a perinatal anxiety screening scale in Iranian perinatal population: a methodological study. Cresc J Med Biol Sci. (2020) 7:551–9.
78. Priyadarshanie MN, Waas MDIA, Goonewardena CSE, Balasuriya A, Senaratna BCV, Fernando DMS. Sinhala translation of the Perinatal Anxiety Screening Scale: a valid and reliable tool to detect anxiety disorders among antenatal women. BMC Psychiatry. (2020) 20:381. doi: 10.1186/s12888-020-02757-z
79. Jradi H, Alfarhan T, Alsuraimi A. Validation of the Arabic version of the Perinatal Anxiety Screening Scale (PASS) among antenatal and postnatal women. BMC Pregnancy Childbirth. (2020) 20:758. doi: 10.1186/s12884-020-03451-4
80. Hobeika E, Malaeb D, Hobeika E, Salameh P, Obeid S, Kheir N, et al. Postpartum Depression and Anxiety among Lebanese women: correlates and scales validation. BMC Psychiatry. (2020). doi: 10.21203/rs.3.rs-15821/v1. [Epub ahead of print].
81. Comparelli A, Savoja V, Kotzalidis GD, Woods SW, Mosticoni S, Vassallo F, et al. Factor-structure of the Italian version of the Scale Of Prodromal Symptoms (SOPS): a comparison with the English version. Epidemiol Psychiatr Sci. (2011) 20:45–54. doi: 10.1017/S2045796011000114
82. Kotzalidis GD, Solfanelli A, Piacentino D, Savoja V, Fiori Nastro P, Curto M, et al. The Italian version of the 92-item Prodromal Questionnaire: concurrent validity with the SIPS and factor analysis in a sample of 258 outpatients aged 11-36 years. Schizophr Res. (2017) 189:50–6. doi: 10.1016/j.schres.2017.02.008
83. Möller H-J. Rating depressed patients: observer- vs self-assessment. Eur Psychiatry. (2000) 15:160–72. doi: 10.1016/S0924-9338(00)00229-7
84. Tondo L, Burrai C, Scamonatti L, Weissenburger J, Rush J. Comparison between clinician-rated and self-reported depressive symptoms in Italian psychiatric patients. Neuropsychobiology. (1988) 19:1–5. doi: 10.1159/000118423
85. Leentjens AF, Dujardin K, Marsh L, Richard IH, Starkstein SE, Martinez-Martin P. Anxiety rating scales in Parkinson's disease: a validation study of the Hamilton anxiety rating scale, the Beck anxiety inventory, and the hospital anxiety and depression scale. Mov Disord. (2011) 26:407–15. doi: 10.1002/mds.23184
86. Harrison S, Alderdice F. Challenges of defining and measuring perinatal anxiety. J Reprod Infant Psychol. (2020) 38:1–2. doi: 10.1080/02646838.2020.1703526
Keywords: pregnancy, screening, psychometric properties, factor analysis, anxiety, perinatal
Citation: Koukopoulos A, Mazza C, De Chiara L, Sani G, Simonetti A, Kotzalidis GD, Armani G, Callovini G, Bonito M, Parmigiani G, Ferracuti S, Somerville S, Roma P and Angeletti G (2021) Psychometric Properties of the Perinatal Anxiety Screening Scale Administered to Italian Women in the Perinatal Period. Front. Psychiatry 12:684579. doi: 10.3389/fpsyt.2021.684579
Received: 23 March 2021; Accepted: 25 May 2021;
Published: 22 June 2021.
Edited by:
Karen Tabb, University of Illinois at Urbana-Champaign, United StatesReviewed by:
Tom Kingstone, Keele University, United KingdomCopyright © 2021 Koukopoulos, Mazza, De Chiara, Sani, Simonetti, Kotzalidis, Armani, Callovini, Bonito, Parmigiani, Ferracuti, Somerville, Roma and Angeletti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Georgios D. Kotzalidis, Z2lvcmdpby5rb3R6YWxpZGlzQHVuaXJvbWExLml0
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.