- 1School of Psychiatry, North Sichuan Medical College, Nanchong, China
- 2Department of Neurology, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
- 3School of International Education and Cooperation, North Sichuan Medical College, Nanchong, China
Background: The association between migraine and suicide ideation has been identified. However, the predictive factors of suicidal ideation are still controversial and whether migraine with aura can serve as an independent associated factor is uncertain. This manuscript studied the association between migraine with aura and suicidal ideation and explored the predictive factors for suicidal ideation.
Methods: We surveyed 9,057 medical students and included 579 medical students with migraine into our study population. All students completed the General Situation Questionnaire, the Verified Headache Questionnaire, Hamilton Anxiety Scale (24 items), Hamilton Depression Scale (24 items), 36-item Health Survey Brief (SF-36), Headache Impact Text-6 (HIT-6), Test Anxiety Scale (TAS), and Pittsburgh Sleep Quality Index (PSQI). Suicidal ideation was measured by the Self-rating Idea of Suicide Scale (SIOSS).
Results: Out of the 579 migraine medical college students, 562 (age 19.6 ± 1.6; 448 women and 114 men) were included in the final study. The positive rate of suicidal ideation was 13.7%. Compared with students suffering from migraine without aura, those having migraine with aura had higher suicidal ideation (p < 0.015). After adjusting for demographic factors and headache characteristics, migraine with aura was found to be independently associated with suicidal ideation. Other independent associated factors include anxiety, depression, test anxiety, sleep, headache, and quality of life. Among these various factors, high quality of life was found to play a protective role against suicidal ideation.
Conclusions: Migraine with aura is independently associated with suicidal ideation. Furthermore, anxiety, depression, text anxiety, poor sleep quality, and headache frequency are associated with suicidal ideation among medical college students with migraine.
Introduction
Migraine is one of the most common types of primary headache with the prevalence of 10–18% (1) globally (2–4). Studies have shown that chronic pain may increase the frequency of thoughts of ending one's life (5). Psychogenic pain is significantly associated with increased suicidal ideation in all types of pain, especially migraine (6, 7). In addition, in the past few years, the burden of disease caused by migraine has made people more concerned about their consequences, such as the appearance of suicidal ideation (8).
Suicide has occurred more frequently in colleges and universities in recent years, making it a major public issue (9). For adolescence, suicide remains a leading cause of mortality worldwide (10). Suicidal behavior includes suicidal ideation, suicide plan, and suicide attempt. Among them, suicidal ideation is the most sensitive predictor (3). A meta-analysis of 34,904 college students showed that the overall prevalence of migraines among them was 16.1% (11), indicating that the college population is heavily affected by migraine. Migraine, which is the third most common disability factor, can undermine learning ability and life quality by severely affecting patients' social functions (12, 13). Once it affects the mental and psychological health of patients (14), the suicide risk rises, bringing greater social impacts. Therefore, it is necessary to explore the risk factors of suicidal ideation related to migraine.
Previous studies have shown the relationship between migraine and suicide (8, 15), but the suicidal ideation among each subtype of migraine remains controversial (5, 8). In 1992, Breslau et al. reported that migraine with aura had a higher rate of suicidal ideation (16). Wang et al. found a relationship between migraine with aura and suicidal ideation among adolescents aged 13–15 (5). However, they did not consider whether migraine with aura alone is independently associated with suicidal ideation after adjusting non-specific headache factors (headache frequency, headache intensity, and the duration of headache), and psychiatric comorbidities. Moreover, migraine is often accompanied by various psychiatric complications, which also affect the prognosis of this disease (17–19). Therefore, it is crucial to investigate the confounding factors, which will be done in this paper by exploring the relationship between migraine and suicidal ideation, as well as the related factors.
Methods
Study Design
This study was part of a cross-sectional survey carried out on the North Sichuan Medical College Students Headache Survey, aiming to determine the epidemiologic profile of headache and the relationship between psychiatric disorders and headache. This study consisted of multiple self-administered and other-rated scales with one-to-one information collection by a research group member from a medical college in Sichuan, China, from July 2018 to July 2019. This study was approved by the ethics committee of the Affiliated Hospital of North Sichuan Medical College and was filed on the clinical research platform of West China Hospital (No. NSMC20170420). All participants signed an informed consent form. This research is voluntary, confidential, practical, and non-harmful. Participants can choose to withdraw from the study at any time without any reason provided.
Data Collection
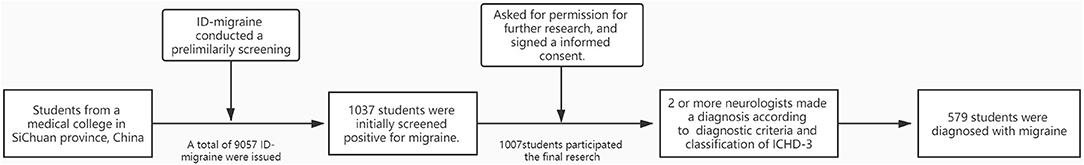
The ID-Migraine was used to conduct a preliminary screening of migraine cases at a medical college in Sichuan Province, China. A total of 9,057 ID-Migraine screening questionnaires were issued, and 8,783 valid questionnaires were retrieved, with an effective response rate of 96.97%. We evaluated all valid questionnaires, of which 1,037 were initially screened positive for migraine.
The members of our research team were divided into many groups (Each group was trained with long-term professional knowledge and passed relevant tests, which ensured that each research group member can independently complete one-to-one information collection in accordance with unified standards). The group members asked students with positive initial screening result for headaches via telephone or email if whether they are willing to give basic information about themselves and headaches. During the collection, the information was recorded in strict accordance with uniform criteria, and all information was kept confidential.
A total of 1,007 students participated in further research information collection. Should there be any information missing, we made another telephone call or wrote an email to complete the collection. Next, these students were diagnosed by two or more specialized neurologists according to the diagnostic criteria and the classification of ICHD-3 (14).
Finally, 579 students were diagnosed with migraines (The flow chart diagram is shown in Figure 1).
Target Group
In China, over 90% of medical students attend public universities and the rest attend private universities. After screening for ID-Migraine, we had 579 students suffering from migraine out of 8,783 participants. The overall prevalence of migraine was slightly lower than medical students in Northern China (8.6%) and Suzhou, China (7.91%). Moreover, it was lower than the global prevalence of migraine (10–18%). Thus, our study cohort is generally representative of the sample obtained from the medical students.
Headache Diagnosis
The ID-Migraine was used for the screening of headaches. Migraine can be further divided into migraine with aura (MA) and migraine without aura (MO), and the diagnosis is based on the ICHD-3 version (20). Exclusion criteria are as follows: students with secondary headaches, other chronic diseases, anxiety, depression, or other mental illnesses clinically diagnosed before the onset of headache; students who were taking medications for migraine, anxiety, or depression; and students who refused to sign the consent form.
Questionnaires
1. Demographic data: name, sex, nation, age, height (cm), weight (kg), grade, major, living expenses(¥)/month, smoking history (smoke>1/day, time>1 year), drinking history (drinking in the past year), genetic history of migraine.
2. A valid screening questionnaire for headaches: the final three-item screening questions of the ID-Migraine (Pfizer Inc., New York, NY, USA) test are as follows: (1). During the last 3 months, did you feel nauseated or sick in your stomach when headaches strike? (2). Did light bother you when you had a headache (a lot more than when you do not have headaches)? (3). Did your headache restrict your ability to work, study, or do other things? The ID-Migraine is a very simple and valid tool, often used for the diagnosis of migraine (21–23). The sensitivity of ID-Migraine is 0.84, 95% CI 0.75–0.90, and the specificity of ID-Migraine is 0.76, 95% CI 0.69–0.83 (24). The overall sensitivity and specificity of the Chinese version of ID-migraine were 84 and 64% (25), respectively. If two or more of the answers are “yes,” the patient is possibly suffering from migraine and will be judged to have a positive screening result.
3. A valid headache questionnaire: based on the 3rd edition of the International Classification of Headache Disorders ICHD-3, the content of which includes the age of onset (years), the course of disease (years, the first diagnosis of headache-related diseases until this investigation), triggers (≥2 migraine attacks directly caused by this factor), the location of the headache, the nature of the headache, the duration of severe headache (hours, all time periods are divided into two categories:> 1 and <1 h), pain degree (VAS score, 0–10), the number of migraine days per month (or days, if the number of days is <1 day, it is counted as 1 day), aura symptoms 1 h before the headache, symptoms associated with the headache, and the use of painkillers.
4. A valid self-rating idea of suicide scale: we used the Self-rating Idea of Suicide Scale (SIOSS) to test. The scale has good reliability and validity for screening Chinese college students' suicidal ideation, with focus reliability of 0.86, an internal consistency coefficient of 0.79, and split-to-half reliability of 0.824 (26). It includes four factors: despair, suicide, optimism, and cover-up. Only “yes” or “no” are given as answers. If the cover factor is ≥ 4, the test is invalid. Generally, ≥12 score is taken as the critical value. The higher the score, the stronger the suicidal ideation.
5. HAMA/HAMD (Hamilton Anxiety Scale/Hamilton Depression Scale): the Hamilton Anxiety Scale and Hamilton Depression Scale have been widely used to assess the appearance and the severities of anxiety and depression (27, 28). In China, this scale is commonly used to screen anxiety and depression. In this study, all members of our research team received professional training from two psychiatrists, ensuring the consistency and professionalism of the inquiry and evaluation. In our preliminary evaluation from the Hamilton Depression Scale score, anxiety was determined if the score was > 7 points; depression if it is >8 points. In both scales, the higher the score, the severer the disorder.
6. The PSQI (Pittsburgh Sleep Quality Index): This scale test factors including subjective sleep quality, time to fall asleep, sleep efficiency, sleep disorders, sleeping medications, and daytime function. The higher the score, the poorer the sleep quality (29). In China, using a score of more than seven points to judge whether there is a sleep quality problem has good sensitivity and specificity (sensitivity and specificity are 98.3 and 90.3%, respectively) (30).
7. The TAS (Test Anxiety Scale): the new version of 37 items originally revised and compiled by Sarason on the basis of TAQ has effectively improved the sensitivity and reliability of the scale (31). The Chinese version was translated and used by Wang Caikang in 1999 (32). The scale includes tests on psychological feelings and physical discomfort before and after the test. A score of <12 is considered as low anxiety, 12–20 is considered as moderate anxiety, and 20 or more is considered as high anxiety.
8. The HIT-6 (Headache Impact Text-6): this scale evaluates the impact of headaches on the physical condition. Scores ≤49 represent little or no impact; scores between 50 and 55 represent impact to a limited extent; scores between 56 and 59 represent substantial impact; and scores ≥60 indicate severe impact (33).
9. The SF-36 (36-item Health Survey Brief): this scale contains eight health dimensions, which can also be categorized into physical health and mental health (34). The higher the 21 scores, the higher the quality of life.
Statistical Analysis
Continuous variables that conform to normality and variance are expressed as x ± s (mean ± standard deviation), while those that do not conform are expressed as M (Q1, Q3)[mean (lower quartile, upper quartile)], and the categorical variables are expressed as the rate.
The X2-test (chi-square test) was used to test the difference between the groups of the categorical variables. The Student t was used to compare the difference between the continuous variable groups that conform to normality and the uniform variance, while the Mann-Whitney U-test was used to compare the continuous variable groups (including: the scores of HAMA and HAMD, head frequency) that do not conform to the normality or uniform variance.
To assess the association of variables in Table 1 with suicidal ideation, univariable logistics regression analyses were performed with suicidal ideation as the dependent variable. All factors in Table 1 were entered as independent variables into the multivariable model to identify potentially predictive factors for suicidal ideation. The predictors for suicidal ideation were presented as odds ratios (OR) with 95% confidence intervals (95% CI).
In multivariable logistics regression, variables were divided into three models: (1) Model 1: demographic and social factors (Demo), including age, sex, grade, BMI, history of tobacco, or alcohol consumption (2); Model 2: headache-related factors (HF), including headache frequency, intensity, duration of migraine, family history of migraine; and (3) Model 3: psychological factors (PF), including HAMA, HAMD, TAS, HIT-6, PQSI, and SF-36 score. The multicollinearity among the predictive factors was checked using the variance inflation factor in which a value >10 was considered to have serious problem of collinearity.
The significance level was set to 0.05. Data were analyzed using the Statistical Package for the Social Sciences (Version 25.0 for Windows).
Results
A total of 579 medical college students were diagnosed with migraine, including 114 male and 448 female (female/male= 3.9) with a mean age of 19.6 ± 1.6 years. Among them, 17 students were excluded because the questionnaires filled by them were incomplete. Therefore, 562 students with migraines were finally included in our research sample.
Clinical Characteristics in Students With Migraine
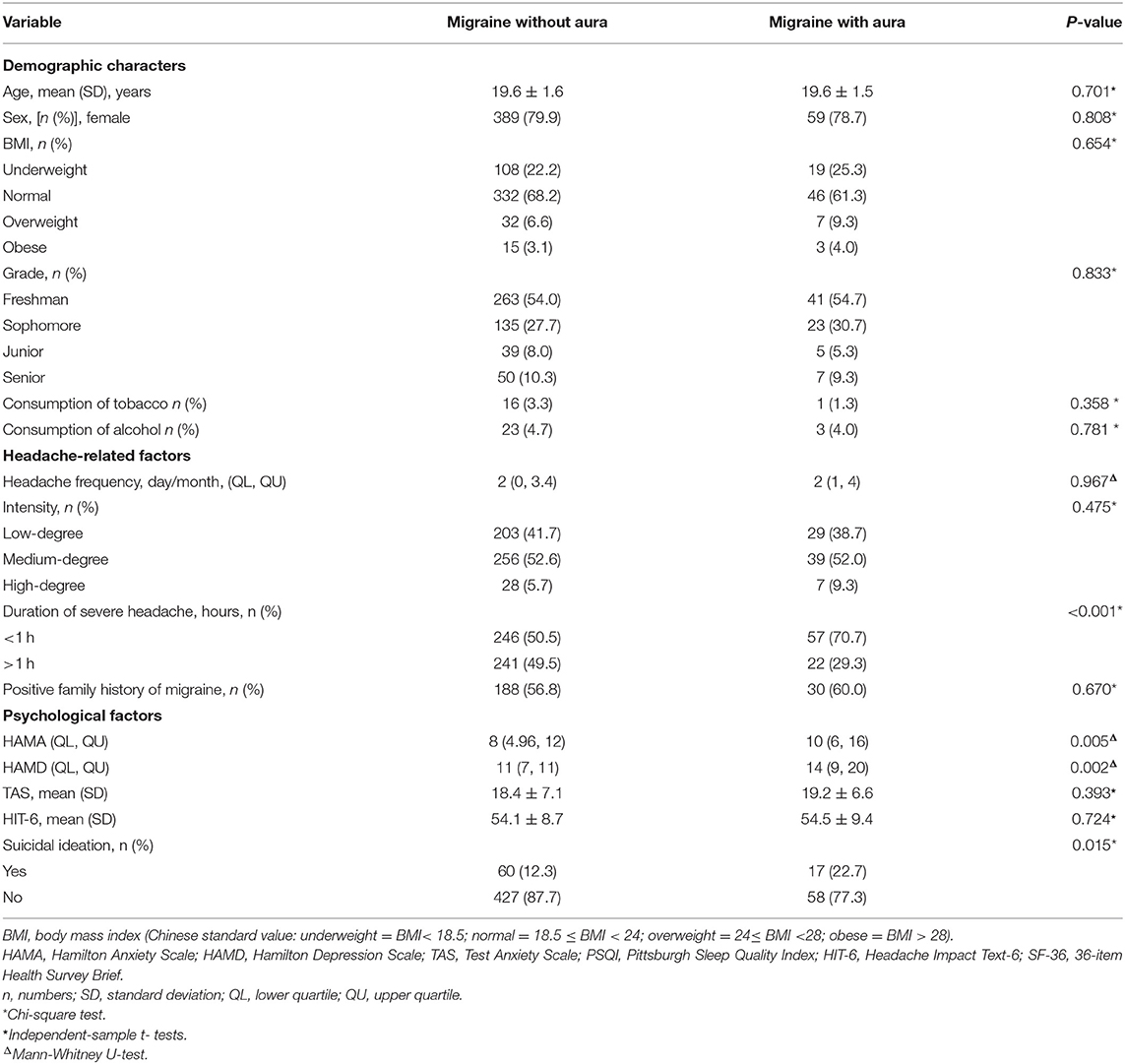
Our study showed that the overall prevalence of suicidal ideation among students suffering from migraines was 13.7%. Table 1 presents the demographic information about the participants and illustrates the differences among the different migraine subtypes. The prevalence of suicidal ideation was much higher among students with migraine with aura than those without aura (p = 0.015). The proportions of those with suicidal ideation in migraine with aura and migraine without aura were 22.1 and 12.3%, respectively. Also, the table shows that, compared to migraine without aura, migraine with aura had a longer severe headache duration (p < 0.001) and higher score for HAMA (p = 0.005) and HAMD (p = 0.002).
Factors Associated With Suicidal Ideation in Medical College Students
In Table 2, the results were obtained by using univariable logistic regression analysis to identify the factors associated with suicidal ideation. Among headache-related factors, only high-frequency headaches (OR = 1.2, 95% CI = 1.1–1.2), p < 0.01) associated with the suicidal ideation. Almost all the psychological factors had a significant association with suicidal ideation: high scores of HAMA (OR = 1.3, 95% CI = 1.2–1.3, p < 0.01), HAMD (OR = 1.2, 95% CI =1.13–1.21, p < 0.01), TAS (OR = 1.2, 95% CI = 1.2–1.3, p < 0.01), HIT-6 (OR = 1.1, 95% CI = 1.06–1.12, p < 0.01), and PSQI (OR = 1.4, 95% CI = 1.3–1.5, p < 0.01), as well as low SF-36 (OR = 0.9, 95% CI 0.87–0.92, p < 0.01) scores.
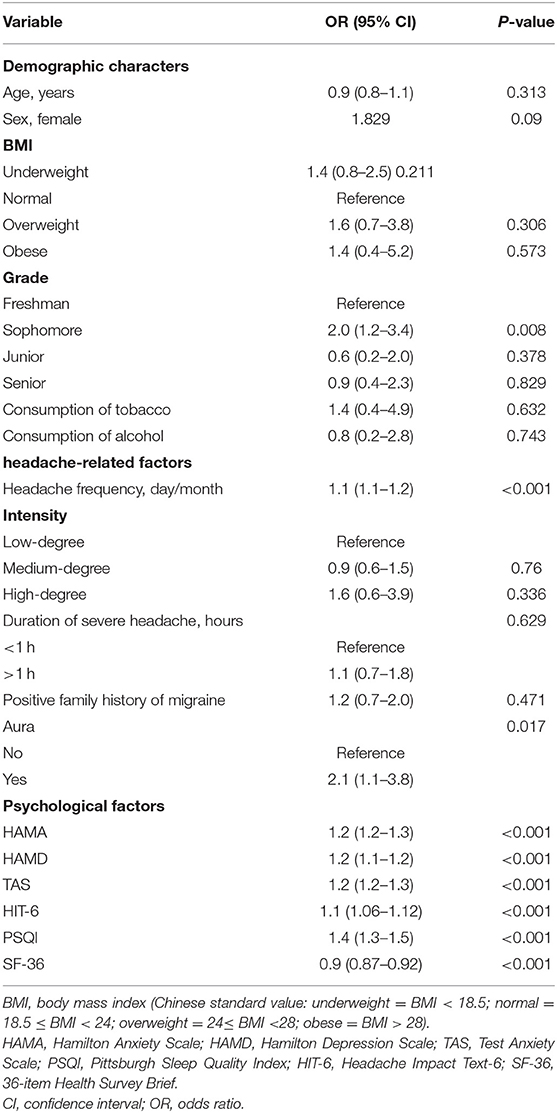
Table 2. Factors associated with suicidal ideation in students with migraine using univariable logistic regression analyses.
The Relationship Between Suicidal Ideation and Migraine With Aura, and the Predictive Factors for Suicidal Ideation
Table 3 shows the results of multivariable logistic regression analyses that identified the potential predictive factors of suicidal ideation in students with migraine. As shown in the table, when aura was added to the multivariate regression model as an explanatory variable for suicidal ideation (Table 3, unadjusted model), aura was associated with suicidal ideation. After adjusting for Demo, HF, and PF, the presence of an aura was independently predictive of suicidal ideation (OR = 2.8, 95% CI = 1.2–6.3, p = 0.014, Table 3, adjusted multivariable models 1, 2, and 3, respectively). The results showed that the presence of aura significantly predicted suicidal ideation. Other predictive factors are listed in Table 4. Except for migraines with aura, all variables were related with psychological factors. There were no clinical symptoms associated with headache that were independently predictive of suicidal ideation.
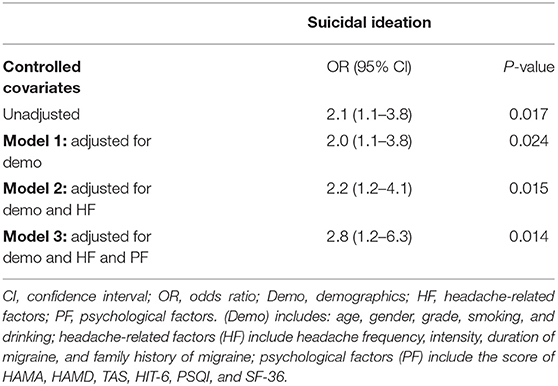
Table 3. Multivariable logistic regression analysis, demonstrating the independent association of aura on suicidal ideation.
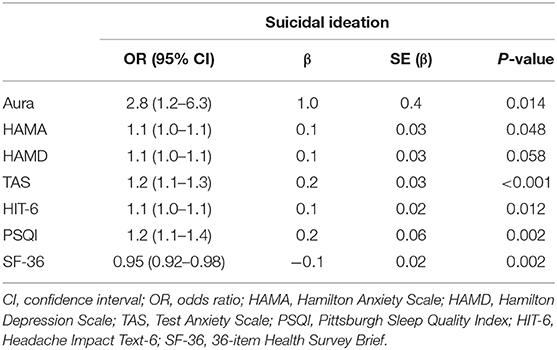
Table 4. Multivariable logistic regression analysis of factors associated with suicidal ideation in students with migraine.
Discussion
It is widely acknowledged that migraine is associated with suicidal ideation. Besides, students with migraine have a higher prevalence of psychiatric comorbidities. However, the result obtained from our study is quite different from previous ones. The present study shows that migraine with aura is associated with suicidal ideation, after adjusting demographic information, head-related factors, and a variety of psychiatry comorbidities. In addition, the population of the present study is based on a large-scale of students and is strictly screened, which helps to reflect the adolescence's suicide problems better.
The incidence of suicidal ideation among the general population is between 20 and 30% (35), while that among patients with migraine ranges from 16.8 to 26.6% in Asia (5, 36, 37). The large range for the latter population may be due to the differences in suicidal ideation determination methods and questionnaires (questions, suicidal ideation questionnaire, and a question in depression scale). In addition, the lower percentage could be because our research subjects are college students knowing a lot of knowledge about life activities and possessing higher respect for life. Moreover, due to the mental and psychological theories they learn endow them with stronger self-efficacy to resist negative emotions, our research results are lower than those of the general migraine population (38). Studies have pointed out that people suffering from migraine with aura are more likely to have suicidal ideation than those with other types of migraine (5, 7, 15); our study also supports this viewpoint. Breslau et al. had shown that migraine with aura had a higher rate of suicidal ideation, but did not consider other confoundings (16). After the demographic factors and psychiatric comorbidities are combined, migraine with aura is still independently associated with suicidal ideation. This means that some factors or characteristics of migraines with aura may influence the prevalence of suicidal ideation. In China, medical college students usually undergo an arduous training and long-term curriculum which means they experience a higher mental and physical pressure. A study shows that compared with other subject areas, the study of medicine is associated with higher stress (39). Besides, a meta-analysis based on Chinese medical students refers that Chinese medical students have relatively high prevalence of depression, anxiety, and suicidal ideation (40). Thus, paying close attention to the psychiatry comorbidities, which could affect the prevalence of suicidal ideation, is essential. According to a study based on neural electrophysiology, migraine with aura has a higher cortical response amplitude and a lower threshold compared with other types of migraine (41). The level of 5-HT is related to migraine with aura and suicidal ideation (42), and aura itself is also related to the activation of the trigeminovascular system caused by cortical spreading depression (43, 44). At the same time, regarding the effect of factors associated with headache on suicidal ideation, some studies reported that pain is a risk factor for suicidal ideation, and chronic pain can increase the risk multiples (6). The Korean article infers that any type of headache accompanying strong headache or depression intensity might predispose the patient to suicidal ideation (45). It may be our study population based on the migraine population and does not include the healthy population; our results did not support this conclusion. Using univariable logistic regression analyses, it can be concluded that the frequency of headaches is associated with suicidal ideation, but after combining other variables, the conclusion does not stand. In short, neither demographic information nor headache-related factors independently associated with suicidal ideation in our study.
Migraine is often accompanied by psychiatric comorbidities (46), seriously affecting the prognosis of migraine and the occurrence of suicidal ideation. Our study found that migraine with aura is more associated with psychiatric comorbidities, which is similar to previous studies (7, 47). We also found that suicidal ideation of migraine with aura is higher than that without aura, and it independently associated with suicidal ideation. On this basis, we also conclude that students with migraine with aura experience more severe anxiety and depression, which may mean that the migraine with aura had a greater impact on their lives. Migraine, depression, anxiety, and suicidal ideation are all associated with high levels of 5-HT (2A) receptor in the prefrontal cortex and hippocampus of the nervous system (48), which may be the reason of their accompanying syndromes. According to a meta-analysis of polysomnography, sleep depth and continuity are associated with mental disorders, including anxiety (49). Based on previous studies, it can be speculated that the hormonal dysregulation and headache-related factors in migraine patients bring anxiety and depression, which in turn can affect the quality of sleep and lead to a decrease in the quality of life. At the same time, the chronic pain and the reduced pleasant experience are risk factors for suicidal ideation (50). College students face great academic pressure, especially a variety of exams, which can play the role of external environmental stimuli for migraine-related suicidal ideation (15). All kinds of factors adding together may eventually lead to the occurrence of suicide ideation among migraine college students.
Based on our study, we should pay more attention to migraine with aura and its psychiatry comorbidities, which may result in suicidal ideation. Antidepressants are the choice of many students for concomitant psychiatric comorbidities, and although they may slightly increase suicidal ideation (51), the overall advantages overweight limitations. In terms of drug selection, SSRIs can be used instead of venlafaxine, as there has been literature indicating that it can slightly increases suicidal ideation (52).
Conclusion
Our results indicate that the prevalence of suicidal ideation among medical college students with migraine was 13.7%. Besides, migraine with aura is independently associated with suicidal ideation after adjusting headache-related factors and psychological factors. Many psychiatric comorbidities (anxiety, depression, low sleep quality, test anxiety, the severity of headache, and life quality) are the predictive factors of suicidal ideation. Moreover, the prevalence of suicidal ideation and duration of severe headache in students with migraine with aura is higher than those with migraine without aura.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study was approved by the Ethics Committee of the Affiliated Hospital of North Sichuan Medical College and was filed on the clinical research platform of West China Hospital, with the record number NSMC20170420. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
E-ZL was involved in the study design, data analysis, and the composing of this manuscript. J-ML provided the subject of this study and critically revised this manuscript. H-DY wrote the data collection part of this manuscript. C-ZD, L-JX, Z-CZ, and TL searched and reviewed the references. J-JR, J-QT, P-QT, Y-RT, and SZ collected the data. NB and AB modified this manuscript. All authors contributed to this manuscript and approved the submitted version.
Funding
This work was financially supported by the Funding Project of the Bureau of Science and Technology and Intellectual Property of Nanchong City (No. NSMC20170420).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank North Sichuan Medical College for their support during data collection and the financial support of the project.
References
1. Silberstein SD, Lipton RB. Epidemiology of migraine. Neuroepidemiology. (1993) 12:179–94. doi: 10.1159/000110317
2. Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia. (1997) 17:15–22. doi: 10.1046/j.1468-2982.1997.1701015.x
3. Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry. (1990) 147:190–5. doi: 10.1176/ajp.147.2.190
4. Yu S, Liu R, Zhao G, Yang X, Qiao X, Feng J, et al. The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache. (2012) 52:582–91. doi: 10.1111/j.1526-4610.2011.02061.x
5. Wang SJ, Fuh JL, Juang KD, Lu SR. Migraine and suicidal ideation in adolescents aged 13 to 15 years. Neurology. (2009) 72:1146–52. doi: 10.1212/01.wnl.0000345362.91734.b3
6. Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med. (2006) 36:575–86. doi: 10.1017/S0033291705006859
7. Wang SJ, Juang KD, Fuh JL, Lu SR. Psychiatric comorbidity and suicide risk in adolescents with chronic daily headache. Neurology. (2007) 68:1468–73. doi: 10.1212/01.wnl.0000260607.90634.d6
8. Colman I, Kingsbury M, Sareen J, Bolton J, van Walraven C. Migraine headache and risk of self-harm and suicide: a population-based study in Ontario, Canada. Headache. (2016) 56:132–40. doi: 10.1111/head.12710
9. Antonaci F, Nappi G, Galli F, Manzoni GC, Calabresi P, Costa A. Migraine and psychiatric comorbidity: a review of clinical findings. J Headache Pain. (2011) 12:115–25. doi: 10.1007/s10194-010-0282-4
10. Pelkonen M, Marttunen M. Child and adolescent suicide: epidemiology, risk factors, and approaches to prevention. Paediatr Drugs. (2003) 5:243–65. doi: 10.2165/00128072-200305040-00004
11. Wang X, Zhou HB, Sun JM, Xing YH, Zhu YL, Zhao YS. The prevalence of migraine in university students: a systematic review and meta-analysis. Eur J Neurol. (2016) 23:464–75. doi: 10.1111/ene.12784
12. Global Burden of Disease Study C. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2015) 386:743–800. doi: 10.1016/S0140-6736(15)60692-4
13. Roh JK, Kim JS, Ahn YO. Epidemiologic and clinical characteristics of migraine and tension-type headache in Korea. Headache. (1998) 38:356–65. doi: 10.1046/j.1526-4610.1998.3805356.x
14. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
15. Friedman LE, Gelaye B, Bain PA, Williams MA. A systematic review and meta-analysis of migraine and suicidal ideation. Clin J Pain. (2017) 33:659–65. doi: 10.1097/AJP.0000000000000440
16. Breslau NJN. Migraine, suicidal ideation, and suicide attempts. Neurology. (1992) 42:392–5. doi: 10.1212/WNL.42.2.392
17. Breslau N, Schultz L, Lipton R, Peterson E, Welch KM. Migraine headaches and suicide attempt. Headache. (2012) 52:723–31. doi: 10.1111/j.1526-4610.2012.02117.x
18. Breslau N, Davis GC, Andreski P. Migraine, psychiatric disorders, and suicide attempts: an epidemiologic study of young adults. Psychiatry Res. (1991) 37:11–23. doi: 10.1016/0165-1781(91)90102-U
19. Wang SJ, Chen PK, Fuh JL. Comorbidities of migraine. Front Neurol. (2010) 1:16. doi: 10.3389/fneur.2010.00016
20. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders 3rd edition. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
21. Al-Hashel JY, Ahmed SF, Alroughani R, Goadsby PJ. Migraine among medical students in Kuwait University. J Headache Pain. (2014) 15:26. doi: 10.1186/1129-2377-15-26
22. Wang X, Sun J, Xing Y, Zhou H, Zhao Y, Zhu Y. The prevalence and awareness of migraine among university students in Harbin, China. J Oral Facial Pain Headache. (2015) 29:384–9. doi: 10.11607/ofph.1521
23. Domingues RB, Teixeira AL, Domingues SA. Physical practice is associated with less functional disability in medical students with migraine. Arquivos Neuro-Psiquiatria. (2011) 69:39–43. doi: 10.1590/S0004-282X2011000100009
24. Cousins G, Hijazze S, Van de Laar FA, Fahey T. Diagnostic accuracy of the ID Migraine: a systematic review and meta-analysis. Headache. (2011) 51:1140–8. doi: 10.1111/j.1526-4610.2011.01916.x
25. Wang X, San YZ, Sun JM, Zhou HB, Li X, Zhang ZM, et al. Validation of the Chinese version of ID-migraine in medical students and systematic review with meta-analysis concerning its diagnostic accuracy. J Oral Facial Pain Headache. (2015) 29:265–78. doi: 10.11607/ofph.1341
26. Xia C-Y, Wang D-B, He Y-S. Study of self-rating idea of undergraduates in the mountain area of southern Zhejiang. Chin J Sch Health. (2012) 33:144–6. doi: 10.16835/j.cnki.1000-9817.2012.02.006
27. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
28. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. (1960) 23:56–62. doi: 10.1136/jnnp.23.1.56
29. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
30. Liu X, Tang M, Hu LJ. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. (1996) 29:103–7.
31. Sarason IG. The Test Anxiety Scale: concept and research. In Spielberger CD, Sarason IG, editors. Stress and Anxiety (Vol. 5). Washington, DC: Hemisphere Publishing Corp (1978). p. 193–216.
32. Wang C-C. Reliability and validity of test anxiety scale-Chinese version. Chin Ment Health J. (2001) 15:96–7.
33. Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia. (2011) 31:357–67. doi: 10.1177/0333102410379890
34. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. (1992) 30:473–83. doi: 10.1097/00005650-199206000-00002
35. Evans E, Hawton K, Rodham K, Deeks J. The prevalence of suicidal phenomena in adolescents: a systematic review of population-based studies. Suicide Life Threat Behav. (2005) 35:239–50. doi: 10.1521/suli.2005.35.3.239
36. Liu HY, Fuh JL, Lin YY, Chen WT, Wang SJ. Suicide risk in patients with migraine and comorbid fibromyalgia. Neurology. (2015) 85:1017–23. doi: 10.1212/WNL.0000000000001943
37. Pei JH, Wang XL, Yu Y, Zhang YB, Gou L, Nan RL, et al. Prevalence of suicidal ideation and suicide attempt in patients with migraine: a systematic review and meta-analysis. J Affect Disord. (2020) 277:253–9. doi: 10.1016/j.jad.2020.08.019
38. Klassen RM, Klassen JRL. Self-efficacy beliefs of medical students: a critical review. Perspect Med Educ. (2018) 7:76–82. doi: 10.1007/s40037-018-0411-3
39. Adams J. Straining to describe and tackle stress in medical students. Med Educ. (2004) 38:463–4. doi: 10.1111/j.1365-2929.2004.01810.x
40. Zeng W, Chen R, Wang X, Zhang Q, Deng W. Prevalence of mental health problems among medical students in China: a meta-analysis. Medicine. (2019) 98:e15337. doi: 10.1097/MD.0000000000015337
41. Coppola G, Di Lorenzo C, Parisi V, Lisicki M, Serrao M, Pierelli F. Clinical neurophysiology of migraine with aura. J Headache Pain. (2019) 20:42. doi: 10.1186/s10194-019-0997-9
42. Purselle DC, Nemeroff CB. Serotonin transporter: a potential substrate in the biology of suicide. Neuropsychopharmacology. (2003) 28:613–9. doi: 10.1038/sj.npp.1300092
43. Fraser CL, Hepschke JL, Jenkins B, Prasad S. Migraine aura: pathophysiology, mimics, and treatment options. Semin Neurol. (2019) 39:739–48. doi: 10.1055/s-0039-1700525
44. Hadjikhani N, Vincent M. Neuroimaging clues of migraine aura. J Headache Pain. (2019) 20:32. doi: 10.1186/s10194-019-0983-2
45. Kim SY, Park SP. Suicidal ideation and risk factors in Korean migraine patients. J Clin Neurosci. (2014) 21:1699–704. doi: 10.1016/j.jocn.2014.03.016
46. Minen MT, Begasse De Dhaem O, Kroon Diest VanA, Powers S, Schwedt TJ, Lipton R, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. (2016) 87:741–9. doi: 10.1136/jnnp-2015-312233
47. Merikangas KR, Angst J, Isler H. Migraine and psychopathology. results of the Zurich cohort study of young adults. Arch Gen Psychiatry. (1990) 47:849–53. doi: 10.1001/archpsyc.1990.01810210057008
48. Pandey GN, Dwivedi Y, Rizavi HS, Ren X, Pandey SC, Pesold C, et al. Higher expression of serotonin 5-HT(2A) receptors in the postmortem brains of teenage suicide victims. Am J Psychiatry. (2002) 159:419–29. doi: 10.1176/appi.ajp.159.3.419
49. Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
50. Berhane HY, Jamerson-Dowlen B, Friedman LE, Berhane Y, Williams MA, Gelaye B. Association between migraine and suicidal behavior among Ethiopian adults. BMC Psychiatry. (2018) 18:46. doi: 10.1186/s12888-018-1629-7
51. Brent DA. Antidepressants and suicidality. Psychiatr Clin North Am. (2016) 39:503–12. doi: 10.1016/j.psc.2016.04.002
Keywords: migraine, suicidal ideation, medical college students, psychiatry comorbidities, associated factors
Citation: Luo J-M, Liu E-Z, Yang H-D, Du C-Z, Xia L-J, Zhang Z-C, Li T, Ren J-J, Tang J-Q, Tang P-Q, Tang Y-R, Zhu S, Bhattarai N, Bhetuwal A and Pu S-X (2021) Prevalence and Factors Associated With Suicidal Ideation in Medical Students With Migraine. Front. Psychiatry 12:683342. doi: 10.3389/fpsyt.2021.683342
Received: 20 March 2021; Accepted: 16 September 2021;
Published: 21 October 2021.
Edited by:
Laura Helena Andrade, University of São Paulo, BrazilReviewed by:
Teruhisa Uwatoko, Kyoto University, JapanFaraidoon Haghdoost, University of New South Wales, Australia
Copyright © 2021 Luo, Liu, Yang, Du, Xia, Zhang, Li, Ren, Tang, Tang, Tang, Zhu, Bhattarai, Bhetuwal and Pu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng-Xiong Pu, YW5kZXJ3bGl1MDIyM0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Jia-Ming Luo
Jia-Ming Luo En-Zhuo Liu
En-Zhuo Liu Hao-Di Yang2
Hao-Di Yang2 Sheng-Xiong Pu
Sheng-Xiong Pu