- 1Department of Psychiatry, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 2Center for Geriatrics and Gerontology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 3Graduate Institute of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 4Department of Psychiatry, China Medical University Hsinchu Hospital, China Medical University, Hsinchu, Taiwan
- 5Department of Psychiatry, China Medical University Hospital, China Medical University, Taichung, Taiwan
- 6Department of Biological Science and Technology, National Chiao Tung University, Hsinchu, Taiwan
- 7Biological Optimal Imaging Lab, Department of Photonics, College of Electrical and Computer Engineering, National Chiao Tung University, Hsinchu, Taiwan
- 8Department of Psychiatry, Taoyuan General Hospital, Ministry of Health and Welfare, Taoyuan, Taiwan
- 9Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- 10Department of Medical Laboratory Science and Biotechnology, Chung Hwa University of Medical Technology, Tainan, Taiwan
- 11National Center for Cognitive-Behavior Therapy and Research, National Center of Neurology and Psychiatry, Tokyo, Japan
Objective: The association between posttraumatic stress disorder (PTSD) and suicidal ideation (SI) is well-known. However, a few studies have investigated the associations between PTSD symptom clusters based on the fifth edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) and changes in suicide risk longitudinally.
Methods: We adopted a longitudinal study design using data from the National Survey for Stress and Health of 3,090 of the Japanese population. The first and second surveys were conducted on November 2016 and March 2017, respectively. The suicidal ideation attributes scale was applied to assess the severity of suicidal ideation at baseline and the follow-up period. A multivariate linear regression model was conducted to examine the associations between the 4- or 7-factor model of PTSD symptom clusters at baseline and longitudinal changes in SI.
Results: Overall, 3,090 subjects were analyzed (mean age, 44.9 ± 10.9 years; 48.8% female) at Baseline, and 2,163 completed the second survey. In the 4-factor model, we found that the severity of negative alternations in cognition and mood were significantly associated with increased SI after 4 months. In the 7-factor model, we found that the severity of anhedonia and externalizing behavior at baseline was significantly associated with increased SI during the follow-up period.
Conclusions: We found that the seven-factor model of DSM-5 PTSD symptoms may provide greater specificity in predicting longitudinal SI change in the general population. Closely monitoring specific PTSD core symptoms may be more effective in mitigating key clinical and functional outcomes.
Introduction
According to the World Health Organization report, the crude suicide rate is estimated at 9.0 per 100,000 of the populations worldwide, with the highest at 16.1 in the United States of America (USA) (1). Suicide takes a tremendous emotional and economic burden for individuals, families, and communities. In 2013, ~93.5 billion was the national cost of suicide, and suicide attempts reported in the USA. Lost productivity represents most of the cost (2). Therefore, early detection and management of suicide are vital, especially for those who have risk factors.
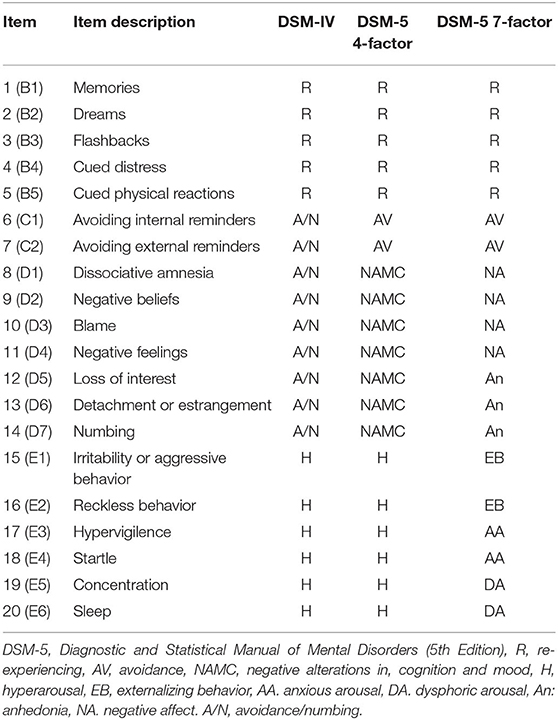
Emerging evidence has demonstrated that posttraumatic stress disorder (PTSD) can be an independent predictor of suicide attempt (3). In a nationwide study of 3.1 million people in Sweden, individuals diagnosed with PTSD were twice more likely to die by suicide than those without PTSD (4). A meta-analysis showed that PTSD is strongly associated with increased suicidality, including suicidal thoughts, behaviors, plans, attempts, and suicides (5). PTSD has been reorganized into four clusters: intrusion symptoms, avoidance, negative alternations in cognition and mood (NCAM), and alterations in arousal and reactivity (AAR) based on the Diagnostic and Statistical Manual of Mental Disorder (DSM-5) (6). The PTSD checklist (PCL), a brief and self-reported instrument, is mostly used to quantify and monitor symptoms of PTSD over time, and to screen individuals for PTSD in both research and clinical settings (7). The PCL, which was recently updated to PCL-5, includes 20 items that correspond to the 20 PTSD symptoms in accordance with DSM-5 (8). PCL-5 appears to have excellent temporal stability and yields PTSD prevalence estimates similar to that of the previous version (9). However, recently, several confirmatory factor analysis (CFA) studies, in contrast to the four-factor model, have found that the best-fitting model is a seven-factor model, which includes intrusion symptoms, avoidance, negative affect, anhedonia, externalizing behaviors, anxious arousal, and dysphoric arousal (10–13).
A growing amount of evidence has demonstrated a positive relationship between specific PTSD symptoms and suicide risk or suicidal ideation (SI) (14). However, evidence is equivocal regarding the specific PTSD symptom clusters that may confer SI via DSM-IV and DSM-5. For example, some studies have linked hyperarousal (15, 16) or re-experiencing (14, 17–19) to increased SI, whereas others have linked numbing (16, 18), avoidance (20), and dysphoria (21) to elevated SI. Although the results of specific symptoms linked to SI have been inconsistent, overall evidence shows a positive relationship between at least one PTSD cluster and SI. Explanations for the inconsistent findings might be derived from cross-sectional study design, small sample sizes, the enrollment of specific occupation population such as military personnel (16), veterans (17), or firefighters (18), and even ethnic differences (22); therefore, the findings may have been confounded by selection bias.
To the best of our knowledge, there have been no studies to date that have examined the associations between PTSD symptoms and longitudinal changes in the risk of SI using a nationwide survey database. The aim of our study was to examine the associations between specific PTSD symptom clusters in four- and seven-factorial models and longitudinal SI changes in a sample of the Japanese population.
Methods
Database
Data were obtained from the National Survey for Stress and Health (NSSH), which was conducted between 2016 and 2017. A flow chart of the survey is shown in Supplementary Figure 1. To control the seasonal effect, two waves of the survey were conducted. In Wave 1, participants were screened since November 2016, and the survey was administered twice (Time 1 in November 2016 and Time 2 in March 2017). Wave 2 consisted of screening and a Time 1 survey (both in March 2017). The questions used in the screen and the Time 1 surveys were the same across Waves 1 and 2, with a random scale order in Wave 2 only. We sent an advertising email to 100,077 panelists in November (Wave 1) and to 56,953 panelists in March (Wave 2). Of these, 20,000 participated in each screen on November 15–30, 2016 (Wave 1) and March 23–25, 2017 (Wave 2). At the screening, participants were identified their index traumatic event at the beginning of the questionnaire packet. Participants who reported no traumatic events were asked to identify their most stressful or heartbreaking life event. The identified index event automatically appeared in the instructions for answering all subsequent PCL-5 or other PTSD-related assessments. In the screen, participants answered the PCL-5 and questions regarding the status of the diagnosis and treatment of PTSD. Our target sample size was 6,000 individuals, including 3,000 patients with PTSD who met the probable DSM-5 diagnostic criteria using the PCL-5, 1,000 nonclinical panelists without any traumatic experience, and 2,000 nonclinical or subclinical panelists with traumatic experiences. We terminated the screen in Waves 1 and 2 upon reaching half of the target sample size. The screened participants answered measures of psychiatric symptoms and psychological processes at Times 1 and 2 for the purposes of examining the various study hypotheses beyond this report. Only Wave 1 participants took part in the Time 2 survey 4 months after Time 1. Detailed information regarding the NSSH could be found in our previous work (11, 19).
All participants read a full explanation of the study and gave informed consent before answering the questionnaires during the screen and the Time 1 and Time 2 surveys. All survey content was examined for logical flow, face validity, design, and miscellaneous errors by nine clinical psychologists and was double-checked by two Macromill survey engineers. To enhance data quality, the survey system automatically excluded participants who showed extremely short response times. Because the questionnaire did not allow participants to proceed with unanswered items, no data were missing except for income. The institutional review board at the National Center of Neurology and Psychiatry approved the study (Approval Number: A2015-086). We conducted the study with a longitudinal design and used the data collected at Wave 1 (n = 3,090). The measurements at Time 1 and Time 2 surveys are shown in Supplementary Figure 2.
Demographics
Personal information including sex, age, marital status, income, history of physical or psychological abuse, history of habitual use of alcohol/tobacco, history of self-harm behavior, history of being diagnosed and treated for any mental disorder including major depressive disorder (MDD), obsessive–compulsive disorder (OCD), seasonal affective disorder (SAD), panic disorder (PAD), psychotic disorder, bipolar disorder, PTSD, eating disorder, generalized anxiety disorder (GAD), and dysthymic disorder were included (Table 1).
Measures
PCL-5
We used the Japanese version of the PCL-5 to assess PTSD symptoms (11). The PCL-5 included a 20-item assessment (8). The 20 items, which were concordant with the DSM-5 diagnostic items, were answered on a five-point Likert scale (0 = Not at all, 1 = A little bit, 2 = Moderately, 3 = Quite a bit, and 4 = Extremely). The item mapping for the four- and seven-factorial models are shown in Table 2.
Traumatic Events
We used the 25 traumatic experience items in the PTSD module of the World Health Organization Composite International Diagnostic Interview, version 3.0 (WHO-CIDI) (23). If a participant answered 0 (never experienced) on all the 25 items, the participant was asked to recall the most stressful and heartbreaking event in their life was and then answered the items in the questionnaire. We used a four-point scale to assess the lifetime experiences of the participants (0, “never experienced”; 1, “experienced within the last month”; 2, “experienced once more than 1 month ago”; and 3, “experienced at least twice more than 1 month ago”). After completing the list of traumatic events, participants were asked to select one item from which they replied a 1, 2, or 3 as the worst that they had experienced.
Suicidal Ideation Attributes Scale
The Suicidal Ideation Attributes Scale (SIDAS) assesses the severity of suicidal ideation during the past month. Its five items ask about frequency, controllability, closeness to attempt, level of distress associated with the thoughts, and impact on daily functioning (24). Answers are reported on an 11-point Likert scale. The SIDAS exhibits high internal consistency (Cronbach's alpha = 0.91). Scores ≥ 21 indicated a high risk of suicide ideation (24).
Statistical Analysis
For sensitivity analysis, Student's t-tests and chi-square were used to compare the characteristics between those who were lost to follow-ups and under follow-ups at Time 2. Multivariate linear regression models with longitudinal changes in SIDAS scores as the dependent variable and PTSD symptom clusters based on the four- or seven-factor model as the independent variables were adjusted for sociodemographic variables, history of self-harm, history of physical and psychological abuse, psychiatric comorbidities, and baseline SIDAS score as confounding factors. The multivariate linear regression models calculated the beta coefficients and found a 95% confidence interval. A p-value of < 0.05 indicated statistical significance, and all results were analyzed using STATA version 15.1.
Results
Clinical Characteristics of the Study Population
The baseline sociodemographic characteristics are shown in Table 1. Data from a total of 3,090 subjects were analyzed (mean age, 44.9 ± 10.9 years; 48.8% female) at Time 1 of Wave 1, and 2,163 subjects completed the survey at Time 2. There was no significant difference in demographic characteristics between those who were lost to follow-ups and under follow-ups at Time 2 in the sensitivity analysis. A DSM-5 diagnostic status based on the PCL-5 was obtained and showed that PTSD (50%) was the most common diagnosis, followed by trauma experienced without PTSD (30.1%), and no trauma experienced (16.7%). The most common traumatic experiences were emotional abuse (60.7%, n = 1,875), followed by physical violence (39.6%, n = 1,222). Among the recruited subjects, the most common psychiatric comorbidity was MDD (52.8%), followed by panic disorder (20.4%), SAD (15.8%), and GAD (15.8%). The mean baseline SIDAS scores were 20.0 ± 9.7 at Time 1.
Risk Factors Associated With Posttraumatic Stress Disorder Symptoms and Change in Suicidal Ideation in the Four-Factor Model
After multiple linear regression analysis (adjusted R2 = 0.313), we found an history of physical abuse [beta = 1.16, 95% confidence interval (95% CI) = 0.34–1.97, and p = 0.005], previous suicide attempt (beta = 0.78, 95% CI = 0.40–1.17, and p < 0.001), comorbid with diagnosis of MDD (beta = 0.74, 95% CI = 0.44–1.43, and p = 0.037), and NACM symptoms based on the DSM-5 four-factor model (beta = 0.12, 95% CI = 0.02–0.22, and p = 0.016) were significantly associated with an increased SIDAS score (Table 3).
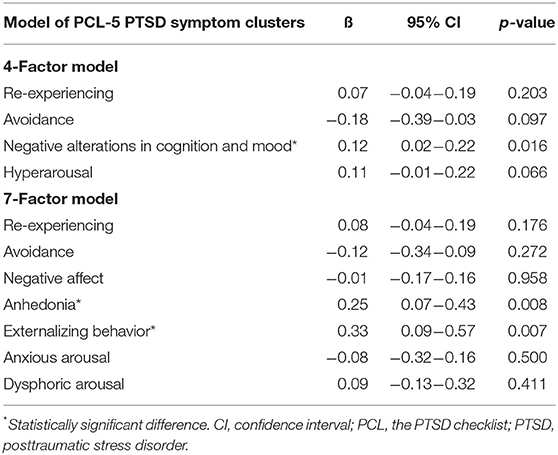
Table 3. Results of linear regression for the associations between PTSD symptom clusters and suicide risk in different models.
Risk Factors Associated With Posttraumatic Stress Disorder Symptoms and Longitudinal Change in Suicidal Ideation in the Seven-Factor Model
In the seven-factor model (adjusted R2 = 0.315), history of physical abuse (beta = 1.19, 95% CI = 0.38–2.01, and p = 0.004), previous suicide attempt (beta = 0.74, 95% CI = 0.35–1.13, and p < 0.001), comorbid with diagnosis of OCD (beta = 1.17, 95% CI = 0.03–2.32, and p = 0.045), PTSD symptom clusters of anhedonia (beta = 0.25, 95% CI = 0.07–0.43, and p = 0.008), and externalizing behavior (beta = 0.33, 95% CI = 0.09–0.57, and p = 0.007) were significantly associated with increased SIDAS score (Table 3).
Discussion
To our knowledge, the is the first study investigating the associations between PTSD symptom clusters and longitudinal change in SI using a nationwide survey dataset. In the four-factor model, we found that history of physical abuse, previous suicide attempt, comorbid with diagnosis of MDD, and NACM symptom clusters were associated with higher risk of increasing SI. In the seven-factor model, we found that history of physical abuse, previous suicide attempt, comorbid with diagnosis of OCD, and anhedonia and externalizing behavior were associated with higher risk of increasing SI.
Comparison Between the Four- and Seven-Factor Model of Posttraumatic Stress Disorder Symptoms in PCL-5
In both the four- and seven-factor model of PTSD symptoms, we found that physical abuse, previous suicide attempt, and comorbid with diagnosis of MDD or OCD were significant predictors for future suicide risk. These are well-known risk factors and are consistent with previous studies (25, 26). For psychometric properties of the PCL-5, we found more significant and specific clusters of symptoms predicting longitudinal changes in SI in the seven-factor model compared with the four-factor model. So far, no such study has compared the ability of the four- and 7-factor model to predict future SI among people who have experienced various traumatic event types. Results of this study extend previous CFA studies of DSM-5 PTSD, indicating that a seven-factor hybrid model of DSM-5 PTSD symptom clusters provides greater specificity in understanding associations with comorbid psychopathology and suicidal ideation (10–14).
Specific Posttraumatic Stress Disorder Symptom Clusters of the Four-Factor Model Predict Change in Suicidal Ideation
The present longitudinal follow-up study is the first to report NACM as a predictor for future SI change. A few studies have examined the association between this factor and SI, as the NACM factor was newly introduced with the release of the DSM-5. Similar to previous studies, NACM symptoms were associated with increased SI (16, 18, 19, 21, 27). In a study conducted by Brown et al., all PTSD factors were positively correlated with SI, and NACM and AAR had the strongest associations (27). Another study demonstrated that the NACM cluster, anhedonia, and negative beliefs based on symptom-level analysis were most strongly correlated with a history of suicide attempts (28). NACM symptoms are conceptualized as being distress based and hypothesized to co-occur with PTSD and depression, as supported by comorbidity with MDD predicting SI change in our study (29). The reason for NACM prediction of SI change might be explained at the symptom level. NACM consists of negative beliefs, blame, loss of interest, social detachment, and numbing, which were highly correlated with SI. For example, a systemic review study has shown that social detachment, especially subjective feeling of loneliness, is strongly associated with suicide risk (30).
Specific Posttraumatic Stress Disorder Symptom Clusters of the Seven-Factor Model to Predict Changes in Suicidal Ideation
In the seven-factor model, previous studies have found that hyperarousal (15, 16), re-experiencing (14, 17–19), anhedonia (19, 31), and externalizing behavior (19, 31) were associated with increased SI. The present study found that anhedonia and externalizing behavior were strong predictors of future worsening SI. Anhedonia symptom could be considered as a core construct in contemporary transdiagnostic models of psychopathology (31, 32). Anhedonia is a common feature following exposure to traumatic stress and, thus, as a potential predictor for disease course. Furthermore, a new externalizing behavior factor, which combined irritability or aggressive behavior with reckless behavior, was another significant predictor for suicidal outcome. The externalizing behaviors reflect the difficulties with impulse control and emotional regulation (33). Taken together, both subjective trauma-related symptoms (e.g., anhedonia) and objective externalizing behaviors (e.g., risk-taking behaviors) may have value in predicting suicide risk in the trauma-exposed general population. However, the present study consisted of a representative cohort of the Japanese general population and was the first to use the seven-factor model of DSM-5 PTSD symptoms to predict SI change. Therefore, future studies enrolling different populations (such as veterans or clinic-based settings) from different countries are warranted to confirm our findings.
Clinical Implications
The present study has important clinical implications for clinical practice and for the basic research of PTSD phenomenology. First, our study suggested that a seven-factor model of DSM-5 PTSD symptoms provides greater specificity than a four-factor model in predicting future longitudinal changes in SI. Second, patients who experienced trauma with symptoms of anhedonia and externalizing behaviors represent a highly risky population for suicide and warrants careful evaluation. Clinicians should be cautious about conducting comprehensive suicide risk assessments and to engage in brief suicide mitigation interventions to prevent unwanted accidents.
Limitations and Strengths
Several limitations of the study should be addressed. First, the self-report online instruments were adopted to evaluate the PTSD symptoms and clinical outcomes. The possibility of increasing endorsements of sensitive responses of online surveys because of anonymity should be considered (27). Second, the participants were limited to those who had internet access and registered as panelists for the survey company. Third, the subjects of the study were Japanese. Hence, it is hard to generalize the present findings to different ethnic groups. Fourth, some subjects replied no experiences of traumatic events but have symptoms of PTSD, and we cannot exclude the possibility that some participants may misunderstand the instruction as this survey was conducted online.
Despite the limitations, a notable strength of the present study was to include the large Japanese population using DSM-5-based PTSD symptoms. Additionally, this is the first study to compare the four- and seven-factor models of PTSD symptoms to predict longitudinal changes in SI.
Conclusion
Our study found that some factors of the seven-factor model might be more useful to predict suicidality and might, therefore, have more value than the four-factor model factors. In the seven-factor model, symptoms specifically for anhedonia and externalizing behaviors may be meaningful predictors for future SI worsening in the general population.
Close monitoring of these core PTSD symptoms and implementing established treatments are vital to prevent further accidents in the general population.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the institutional review board at the National Center of Neurology and Psychiatry, Japan. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MI conceptualized the study and took charge of the project administration. P-HC, S-CW, and MI formulated the methodology and validated the study. P-HC and S-CW performed the formal analysis. C-SC, P-HC, and S-CW wrote the original draft. C-SC, P-HC, S-CW, and MH reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a Grant-in-Aid for Scientific Research (A) (15H01979), awarded to MH, from the Japan Society for the Promotion of Science, Tokyo, Japan. The funders had no role in the study design, data collection or analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge Matthew Yoder, Ph.D., at the National Center for PTSD (Washington DC, United States), Frank W. Weathers, Ph.D., at the Auburn University (Alabama, United States), Peter J. Bernick, MA, at the Nagasaki University (Nagasaki, Japan), and Hiromi Akiyama, MA, at the Community Mental Health Welfare Bonding Organization (Ichikawa, Japan) for developing the Japanese version of the PCL-5. Dr. Yoder, Dr. Weathers, Mr. Bernick, Ms. Hitomi Akiyama, and Dr. Ikka have no conflicts of interest to declare. The authors also appreciate the effort of all participants who took part in this study. P-HC also wants to thank Professor Karestan Koenen from Harvard T.H. Chan School of Public Health for her supervision of this article.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.680434/full#supplementary-material
Abbreviations
PTSD, posttraumatic stress disorder; SI, suicidal ideation; DSM-5, Diagnostic and Statistical Manual for Mental Disorders; NCAM, negative alternations in cognition and mood; AAR, alterations in arousal and reactivity; PCL, PTSD checklist; CFA, confirmatory factor analysis; MDD, major depressive disorder; OCD, obsessive compulsive disorder; SAD, seasonal affective disorder; PAD, panic disorder; GAD, generalized anxiety disorder; NSSH, National Survey for Stress and Health; WHO-CIDI, World Health Organization Composite International Diagnostic Interview, version 3.0; SIDAS, Suicidal Ideation Attributes Scale.
References
1. WHO Global Health Observatory Data Repository. Available online at: https://apps.who.int/gho/data/view.main.MHSUICIDEv?lang=en (accessed February 29, 2021).
2. Shepard DS, Gurewich D, Lwin AK, Reed GA Jr, Silverman MM. Suicide and suicidal attempts in the United States: costs and policy implications. Suicide Life Threat Behav. (2016) 46:352–62. doi: 10.1111/sltb.12225
3. Stevens D, Wilcox HC, MacKinnon DF, Mondimore FM, Schweizer B, Jancic D, et al. Posttraumatic stress disorder increases risk for suicide attempt in adults with recurrent major depression. Depress Anxiety. (2013) 30:940–6. doi: 10.1002/da.22160
4. Fox V, Dalman C, Dal H, Hollander AC, Kirkbride JB, Pitman A. Suicide risk in people with post-traumatic stress disorder: a cohort study of 3.1 million people in Sweden. J Affect Disord. (2021) 279:609–16. doi: 10.1016/j.jad.2020.10.009
5. Panagioti M, Gooding PA, Tarrier N. A meta-analysis of the association between posttraumatic stress disorder and suicidality: the role of comorbid depression. Compr Psychiatry. (2012) 53:915–30. doi: 10.1016/j.comppsych.2012.02.009
6. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder, 5th Edn. Arlington, VA: American Psychiatric Association (2013).
7. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. (1996) 34:669–73. doi: 10.1016/0005-7967(96)00033-2
8. Weathers FW LB, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5). Boston, MA: National Center for PTSD (2013).
9. Keane TM, Rubin A, Lachowicz M, Brief D, Enggasser JL, Roy M, et al. Temporal stability of DSM-5 posttraumatic stress disorder criteria in a problem-drinking sample. Psychol Assess. (2014) 26:1138–45. doi: 10.1037/a0037133
10. Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, et al. Dimensional structure of DSM-5 posttraumatic stress symptoms: support for a hybrid Anhedonia and Externalizing Behaviors model. J Psychiatr Res. (2015) 61:106–13. doi: 10.1016/j.jpsychires.2014.10.012
11. Ito M, Takebayashi Y, Suzuki Y, Horikoshi M. Posttraumatic stress disorder checklist for DSM-5: psychometric properties in a Japanese population. J Affect Disord. (2019) 247:11–9. doi: 10.1016/j.jad.2018.12.086
12. Liu P, Wang L, Cao C, Wang R, Zhang J, Zhang B, et al. The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. J Anxiety Disord. (2014) 28:345–51. doi: 10.1016/j.janxdis.2014.03.008
13. Tsai J, Harpaz-Rotem I, Armour C, Southwick SM, Krystal JH, Pietrzak RH. Dimensional structure of DSM-5 posttraumatic stress disorder symptoms: results from the National Health and Resilience in Veterans Study. J Clin Psychiatry. (2015) 76:546–53. doi: 10.4088/JCP.14m09091
14. Davis MT WT, Weathers FW, Blevins CA. The role of posttraumatic stress disorder symptom clusters in the prediction of passive suicidal ideation. Psychol Trauma. (2014) 6:S82–S91. doi: 10.1037/a0035966
15. Briere J, Godbout N, Dias C. Cumulative trauma, hyperarousal, and suicidality in the general population: a path analysis. J Trauma Dissociation. (2015) 16:153–69. doi: 10.1080/15299732.2014.970265
16. Pennings SM, Finn J, Houtsma C, Green BA, Anestis MD. Posttraumatic stress disorder symptom clusters and the interpersonal theory of suicide in a large military sample. Suicide Life Threat Behav. (2017) 47:538–50. doi: 10.1111/sltb.12317
17. Barr NU SK, Kintzle S, Castro CA. PTSD symptoms, suicidality and non-suicidal risk to life behavior in a mixed sample of pre- and post-9/11 veterans. Soc Work Mental Health. (2016) 14:465–73. doi: 10.1080/15332985.2015.1081666
18. Boffa JW, Stanley IH, Hom MA, Norr AM, Joiner TE, Schmidt NB. PTSD symptoms and suicidal thoughts and behaviors among firefighters. J Psychiatr Res. (2017) 84:277–83. doi: 10.1016/j.jpsychires.2016.10.014
19. Chou PH, Ito M, Horikoshi M. Associations between PTSD symptoms and suicide risk: A comparison of 4-factor and 7-factor models. J Psychiatr Res. (2020) 129:47–52. doi: 10.1016/j.jpsychires.2020.06.004
20. Selaman ZM, Chartrand HK, Bolton JM, Sareen J. Which symptoms of post-traumatic stress disorder are associated with suicide attempts? J Anxiety Disord. (2014) 28:246–51. doi: 10.1016/j.janxdis.2013.12.005
21. Legarreta M, Graham J, North L, Bueler CE, McGlade E, Yurgelun-Todd D. DSM-5 posttraumatic stress disorder symptoms associated with suicide behaviors in veterans. Psychol Trauma. (2015) 7:277–85. doi: 10.1037/tra0000026
22. Perilla JL NF, Lavizzo EA. Ethnicity, culture, and disaster response: identifying and explaining ethnic differences in PTSD six months after hurricane andrew. J Soc Clin Psychol. (2002) 21:20–45. doi: 10.1521/jscp.21.1.20.22404
23. Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. (2004) 13:93–121. doi: 10.1002/mpr.168
24. van Spijker BA, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, et al. The suicidal ideation attributes scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat Behav. (2014) 44:408–19. doi: 10.1111/sltb.12084
25. Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. (2010) 15:868–76. doi: 10.1038/mp.2009.29
26. Serafini G, Muzio C, Piccinini G, Flouri E, Ferrigno G, Pompili M, et al. Life adversities and suicidal behavior in young individuals: a systematic review. Eur Child Adolesc Psychiatry. (2015) 24:1423–46. doi: 10.1007/s00787-015-0760-y
27. Brown LA, Contractor A, Benhamou K. Posttraumatic stress disorder clusters and suicidal ideation. Psychiatry Res. (2018) 270:238–45. doi: 10.1016/j.psychres.2018.09.030
28. Guina J, Nahhas RW, Mata N, Farnsworth S. Which posttraumatic stress disorder symptoms, trauma types, and substances correlate with suicide attempts in trauma survivors? Prim Care Companion CNS Disord. (2017) 19:17m02177. doi: 10.4088/PCC.17m02177
29. Contractor AA, Durham TA, Brennan JA, Armour C, Wutrick HR, Frueh BC, et al. DSM-5 PTSD's symptom dimensions and relations with major depression's symptom dimensions in a primary care sample. Psychiatry Res. (2014) 215:146–53. doi: 10.1016/j.psychres.2013.10.015
30. Calati R, Ferrari C, Brittner M, Oasi O, Olie E, Carvalho AF, et al. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J Affect Disord. (2019) 245:653–67. doi: 10.1016/j.jad.2018.11.022
31. Pietrzak RH, Tsai J, Armour C, Mota N, Harpaz-Rotem I, Southwick SM. Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: results from the National Health and Resilience in Veterans study. J Affect Disord. (2015) 174:522–6. doi: 10.1016/j.jad.2014.12.007
32. Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry. (2014) 13:28–35. doi: 10.1002/wps.20087
Keywords: posttraumatic stress disorder, suicide ideation, DSM, symptomatology, anhedonia, externalizing behavior, PTSD
Citation: Chu C-S, Chou P-H, Wang S-C, Horikoshi M and Ito M (2021) Associations Between PTSD Symptom Custers and Longitudinal Changes in Suicidal Ideation: Comparison Between 4-Factor and 7-Factor Models of DSM-5 PTSD Symptoms. Front. Psychiatry 12:680434. doi: 10.3389/fpsyt.2021.680434
Received: 14 March 2021; Accepted: 20 October 2021;
Published: 16 November 2021.
Edited by:
Natalie Mota, University of Manitoba, CanadaReviewed by:
Laura E. Watkins, Emory University, United StatesSebastian Trautmann, Medical School Hamburg, Germany
Copyright © 2021 Chu, Chou, Wang, Horikoshi and Ito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Po-Han Chou, cGhjaG91QGdtYWlsLmNvbQ==; Shao-Cheng Wang, V1NoYW9jaGVuZ0BnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 Che-Sheng Chu
Che-Sheng Chu Po-Han Chou
Po-Han Chou Shao-Cheng Wang
Shao-Cheng Wang Masaru Horikoshi11
Masaru Horikoshi11 Masaya Ito
Masaya Ito