- 1Department of Psychiatry, Universiti Kebangsaan Malaysia Medical Centre, Wilayah Persekutuan Kuala Lumpur, Malaysia
- 2Faculty of Health Science, Universitas Muhammadiyah Mataram, Kota Mataram, Indonesia
- 3Department of Community Health, Universiti Kebangsaan Malaysia Medical Centre, Wilayah Persekutuan Kuala Lumpur, Malaysia
- 4Department of Biochemistry, Faculty of Medicine, The National University of Malaysia, Wilayah Persekutuan Kuala Lumpur, Malaysia
Background: Natural disasters may physically and psychologically affect individuals and their surrounding community. This study determines the prevalence of post-traumatic stress (PTS) symptoms and its association with maladaptive trauma-related cognition and resilience among adolescents post-earthquake.
Materials and Methods: Data were collected, in this cross-sectional study, during an intervention program post-earthquake held in a state high school located at Lombok, Indonesia. The study sample engaged students 14–19 years of age using the purposive sampling method. The questionnaires used to measure PTS symptoms, maladaptive trauma-related cognition, and resilience were Children's Revised Impact of Event Scale-13 (CRIES-13), Child Post-Traumatic Cognitions Inventory (CPTCI), and Child and Youth Resilience Measure-Revised (CYRM-R), respectively.
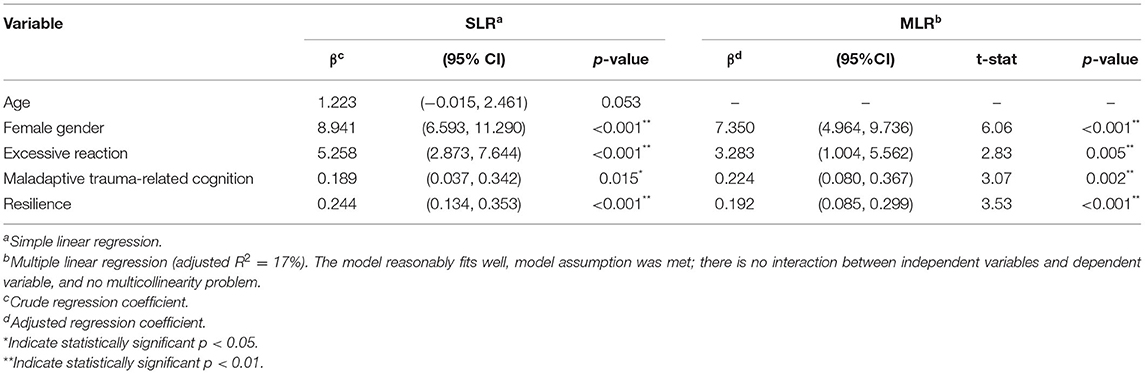
Results: The prevalence of PTS symptoms was 69.9%. Among the respondents, 61.37% were female and 56.48% had mothers with lower educational levels. Using multiple linear regression, the final predictors of PTS symptoms were excessive reactions (e.g., wailing loudly, miserable shrieking) of proxy during earthquake (β = 3.283, p = 0.005), maladaptive trauma-related cognition (β = 0.224, p = 0.002), and resilience (β = 0.192, p < 0.001) with female gender (β = 7.350, p < 0.001) as a control variable. Through simple linear regression, victims who witnessed injury or death during the earthquake (p = 0.003), had a proxy died during the earthquake (p = 0.01), and trapped victims or those who had difficulty escaping (p = 0.01) were identified to potentially predict the occurrence of PTS symptoms, warranting further study.
Conclusion: The presence of excessive proxy reactions during the earthquake, maladaptive trauma-related cognition, and resilience in adolescents exposed to a natural disaster are worth targeting and prioritizing in future post-disaster interventions.
Introduction
Natural disasters have physical and psychological impacts on individuals and their surrounding community. The psychological effects of such catastrophes on a person include depression, anxiety, and stress-related illnesses (1). Post-traumatic stress disorder (PTSD) is one of the stress-related disorders that may develop following exposure to a major traumatic event. PTSD sufferers experience episodes of recurrent intrusion symptoms such as distressing memories of traumatic events, nightmares, and dissociative reactions, as well as avoidance, negative changes in cognition and mood, and hyperarousal (2).
The risk factors for the development of PTSD include extreme age (children, adolescents, and elderly), female gender, low socioeconomic status, low level of education, and aspects of trauma severity (direct and indirect exposure to disaster, witnessing destruction of property, worry about others, witnessing death and injuries of others and physical injury to self during an event of a natural disaster) (3, 4). A study in Indonesia by Marthoenis et al. (5) found that 58.3% of adolescents showed clinical symptoms of PTSD 6 months after the 2016 Aceh Earthquake. The high prevalence of post-traumatic stress (PTS) symptoms in adolescents is worrying as this may affect their daily functioning and cognition. The worse scenario was PTS symptoms that persisted until adulthood resulting in the need for PTSD treatment secondary to childhood trauma (6). Maladaptive cognitive processes experienced during traumatic events may contribute to the long-lasting PTS symptoms. Meiser-Stedman et al. (7) observed that cognitive processes play crucial in the development and persistence of PTS symptoms in both children and adolescents. In the study, all the perceived threats, overwhelming feelings, and confusion during the traumatic event contributed to the onset of acute PTS symptoms. Poorly elaborated, sensory-based memories, dissociation, rumination, and negative appraisals were closely associated with persistent PTS symptoms.
A recent cohort study conducted by Altamore et al. (8) postulated that repeated exposure to earthquakes increased the prevalence of developing psychological distress and PTSD, in which 0.5% prevalence of probable PTSD assessed in 2015 spiked to 16.9% in 2017 after the second earthquake. Although the cohort samples experienced a low level of distress for 8 years after the first earthquake, a second exposure to the earthquake had led to a higher level of psychological and PTS symptoms. Even after the natural disaster has subsided, visiting or being at the place of incidence may still trigger trauma and negative memories that can affect a person's mental and physical health (9). Therefore, the frequency of exposure to earthquakes may influence the development of PTSD and the resilience of adolescents exposed to natural disasters.
Also, resilience is fundamental for people to positively function after a disaster. Resilience was strongly associated with reduced PTS symptoms 3 months after a hurricane (10) and improved quality of life after earthquake exposure (11). Moreover, Smith et al. (12) revealed that a high level of resilience was associated with lower probabilities of developing mental health issues such as depression, anxiety, and stress. Adolescents who experienced the 2016 Fort McMurray wildfire also showed that those who had high resilience showed higher self-esteem and quality of life scores (13).
Several factors that increased resilience in the post-disaster population included self-efficacy, having coping strategies, and good social support (14). Positive thinking and self-motivation were among the strategies used in self-efficacy by the population. Coping strategies such as turning to God and religious activities had helped them to remain hopeful in adversities. Social support given by government and non-government organizations also proved to be helpful in building resilience in the population (14).
Developing countries have started integrating mental health and psychosocial support in their disaster preparedness and response (15–17). However, recent studies showed that mental health problems especially PTSD, depression, and anxiety were still relatively high in these countries (18, 19). Adolescents are vulnerable to their surroundings and may not have adequate knowledge of how to cope with mental health issues and what to do in response to natural disasters. There are limited studies on the effects of repeated trauma exposures on adolescents' mental health. If no prompt identification and treatment, PTSD may persist for a long period of time and impair the children's or adolescents' function and development (20, 21). Therefore, this study aimed to determine the relationship between PTS symptoms, maladaptive trauma-related cognition, and resilience in adolescents exposed to the earthquakes in Lombok, Indonesia.
Materials and Methods
This cross-sectional study was part of an intervention under a student mobility program conducted by the Student Council of the National University of Malaysia in a state high school located at Lombok, Indonesia from July 15 to 21, 2019. The aim of the program was to provide humanitarian aid and psychosocial support, including interventions such as relaxation and coping techniques, for the local adolescents exposed to multiple earthquakes. Lombok is well known as a disaster-prone area due to the island's location in the Pacific Ring of Fire characterized by active movement of tectonic plates resulting in frequent natural disasters. Multiple earthquakes occurred within 9 months: a strong magnitude earthquake (6.4) on July 29, 2018, followed by a major earthquake of 7.0 magnitude on August 5, 2018, and a moderate magnitude earthquake (5.8) on March 17, 2019. The current study involved a group of adolescents in Lombok who survived the earthquakes.
Description of Primary Data
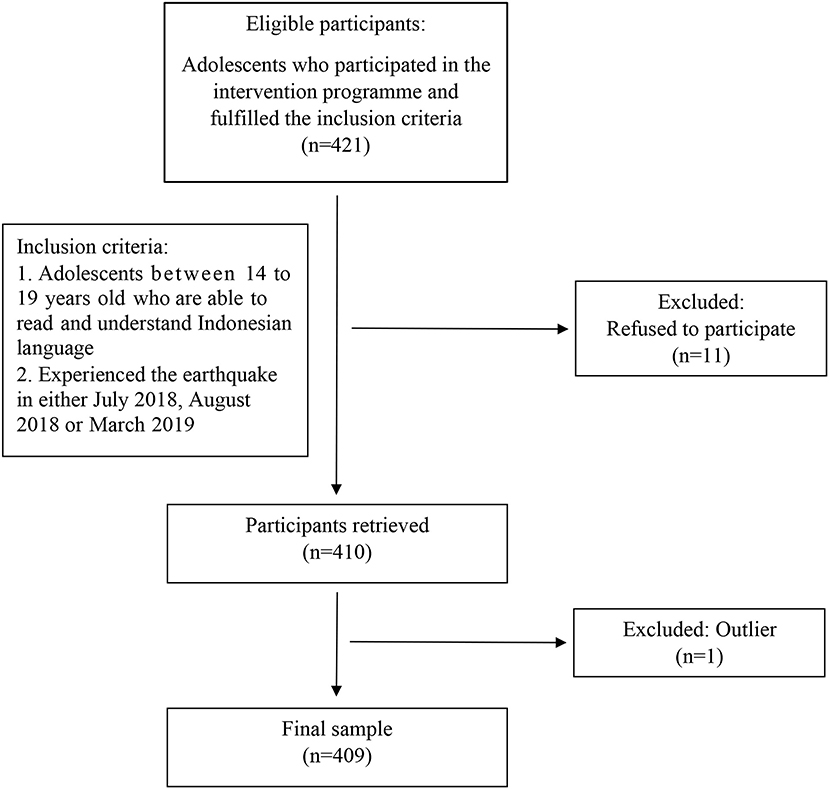
Researchers collected data from secondary school students who participated in the intervention program by purposive sampling method. The inclusion criteria were adolescents ranging from 14 to 19 years old with the ability to read and understand Indonesian language and had experienced at least one of the earthquakes in the 9 months. The study used the WHO definition of adolescents as those who fall within the age range of 10–19 years (22). Exclusion criteria applied to adolescents whose parents did not give consent or those who were unable to understand the questionnaire even under the guidance of the facilitators. The WHO sample size formula (23) yielded a calculated sample size of 246 with the absolute precision of 5% and the level of significance of 95%. The study obtained 421 participants who fulfilled the inclusion criteria and were enrolled for survey completion before the intervention program. However, 11 adolescents refused to participate in the study which resulted in a total sample of 410 participants (Figure 1). The assembly point of the school was the data collection location. Thirty facilitators divided the participants into small groups of 15, and participants were given self-rated questionnaires to be answered. Indonesian facilitators were readily available to assist with further inquiries on any of the questions.
Instruments
The back-translated questionnaires in Indonesian language were used in this study, including socio-demographic and disaster correlates, Child Revised Impact of Events Scale-13 (CRIES-13) (24), Child's Post-Traumatic Cognitions Inventory (CPTCI) (25), and Child and Youth Resilience Measure-Revised (CYRM-R) (26).
Sociodemographic and Disaster Correlates
The sociodemographic questionnaire measured age, gender, household numbers, and educational level of participants and parents. We reviewed disaster correlates, including the reaction of parents during the incident, frequency of exposure to the earthquake, destruction of property or residence, recent move to a new school or place, trapped or separated from proxy during the event, and experienced or witnessed injury and death during the incidents. This questionnaire described the background of the study population.
CRIES-13
CRIES-13 is a screening instrument to assess children at risk of PTSD. It consists of 13 items measuring intrusion (4 items), avoidance (4 items), and arousal (5 items) with a cut-off point of 30. A score of 30 and above indicates the positive screening of PTSD. The scoring for each item uses 0 (Not at all), 1 (Rarely), 3 (Sometimes), and 5 (Often), making the total score ranges from 0 to 65. Cronbach's alpha (27) was found to be 0.80 for the total scale and was 0.70, 0.73, and 0.60 for intrusion, avoidance, and arousal subscales, respectively. Perrin et al. (28) had examined the specificity and sensitivity of the scale in two different samples which included 1) clinical samples comprising children and adolescents (7–18 years old) in Child Traumatic Stress Clinic who were being referred for PTSD assessment, and 2) accident and emergency room samples that included victims of road traffic accidents or assault cases aged from 10 to 16 years. Both samples showed good sensitivity and specificity with a cut-off point of 30 given that the clinical sample reported sensitivity of 0.91 and specificity of 0.65 while the accident and emergency sample reported sensitivity of 0.86 and specificity of 0.73.
CPTCI
Maladaptive trauma-related cognition is assessed using CPTCI consisting of 25 items with two sub-scales: 1) permanent and disturbing change (13 items), and 2) fragile person in a scary world (12 items). A 4-point range of responses from do not agree at all (1) to agree a lot (4) is used to rate each item. The total possible score ranges from 25 to 100, with higher scores corresponding to more negative trauma-related cognition. The reported Cronbach's alpha for this scale ranged from 0.86 to 0.93 (25).
CYRM-R
CYRM-R consists of 17 items that measure personal resilience (10 items) and caregiver resilience (7 items). A 5-point Likert scale, ranging from not at all (1) to a lot (5), rates each item. The total score ranges from 17 to 85. Cronbach's alpha was 0.902 for both personal and caregiver resilience (26, 29).
Ethical Issues
The study obtained approval from the institution's ethics committee. Written consent was obtained from the parents of the participants prior to study enrollment. Participants who showed high post-traumatic stress symptoms were advised to seek psychological treatment at the nearby hospital.
Statistical Analysis
Multiple imputations replaced the missing values in the data. We used descriptive analysis to describe the basic demographic data and earthquake exposure among the participants. Student t-test and ANOVA were both used to outline the relationship between significant demographic data shown in previous studies, trauma experience prior to or preceding the incidents and frequency of earthquake exposure to the development of PTS symptoms, resilience, and trauma-related cognition of the participants. Pearson's correlation described the strength of the relationship between an interval variable with another interval variable, while point biserial correlation was used for the relationship between an interval variable with another nominal variable. Multiple linear regression determined the predictors of post-traumatic stress symptoms.
Results
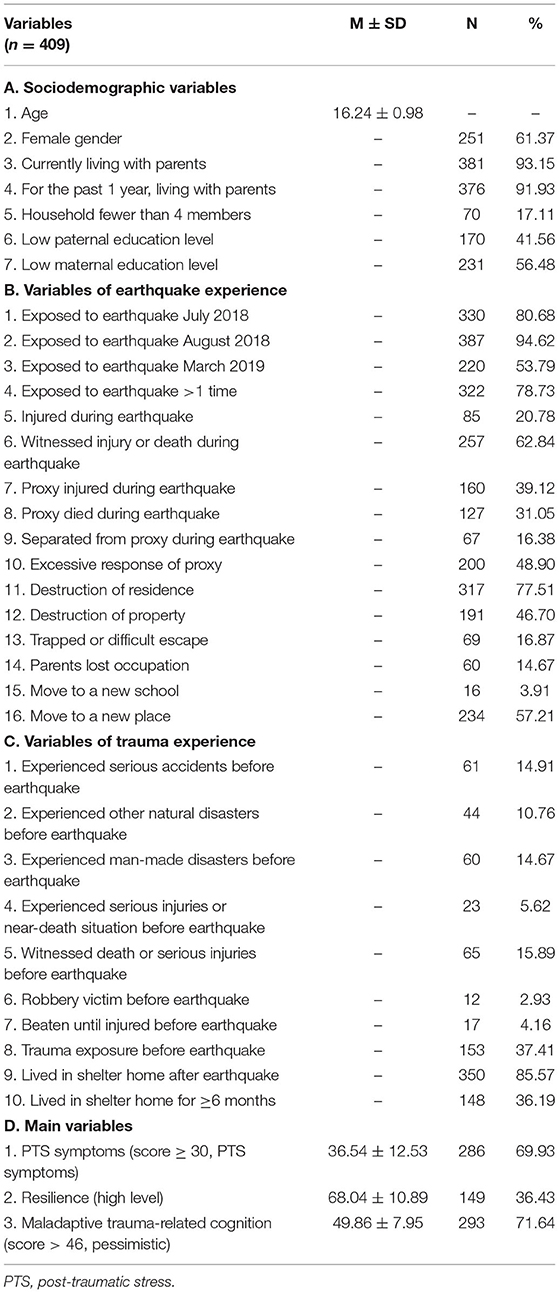
The final participants included were 409 with 158 (38.6%) males and 251 (61.4%) females. One subject was removed from the study as it was an outlier for the CPTCI questionnaire, identified with scatter plot and interquartile range method. A suggested cut-off of 30 was used and the prevalence of probable PTSD was 69.9% for the CRIES questionnaire. The proportion of exposure to the earthquake at least once, twice, and three times were 21.3, 28.4, and 50.4%, respectively. Table 1 presents the questionnaire responses.
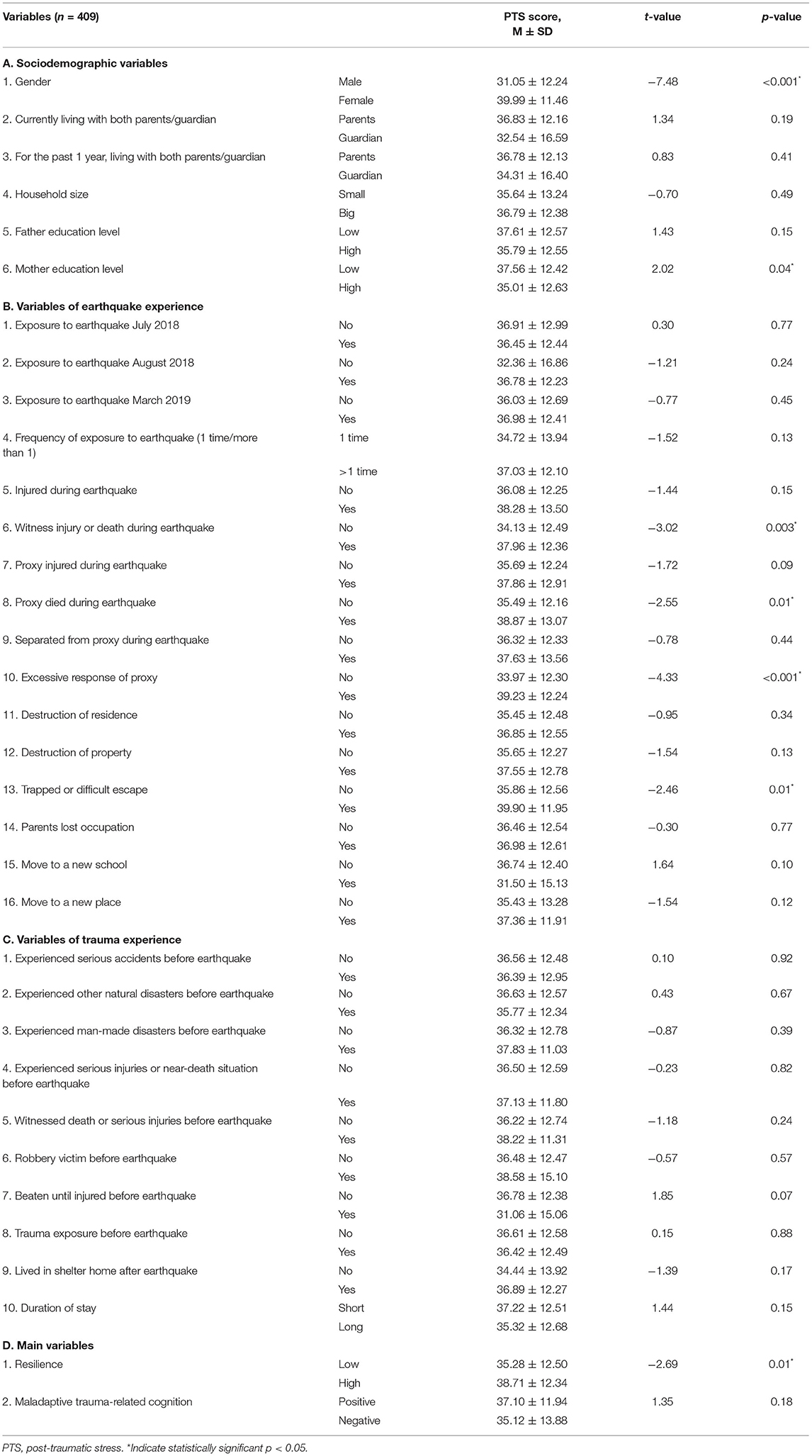
As predicted, results of independent t-test showed a significant difference in the PTS symptoms across gender, in which females [M = 39.99, SD = 11.46, t(407) = −7.48, p < 0.001] had higher PTSD scores than males. Besides, adolescents with mothers of lower educational level [M = 37.56, SD = 12.42, t(399) = 2.02, p = 0.04] scored significantly higher in PTS symptoms; in comparison with adolescents whose mother had education of at least secondary level. There were also significantly higher PTS scores among adolescents who had witnessed injury or death [M = 37.96, SD = 12.36, t(407) = −3.02, p = 0.003] compared with those who did not; and among adolescents who had family, guardian, or acquaintance who died during earthquake [M = 38.87, SD = 13.07, t(407) = −2.55, p = 0.01] in comparison with those who did not have deceased proxy during earthquake. In addition, PTS scores were significantly higher among adolescents whose parents reacted excessively during earthquake (e.g., loud wailing, loud prayers) [M = 39.23, SD = 12.24, t(407) = −4.33, p ≤ 0.001], in contrast to those whose parents did not react this way. In comparison with the differences in PTS scores, adolescents who were trapped or experienced difficult escape during earthquake [M = 39.90, SD = 11.95, t(407) = −2.46, p = 0.01] scored significantly higher than those who did not experience this. The adolescents who have higher level of resilience were found to have higher PTS scores [M = 38.71, SD = 12.34, t(407) = −2.69, p = 0.01] than those with lower level of resilience. Details are tabulated in Table 2.
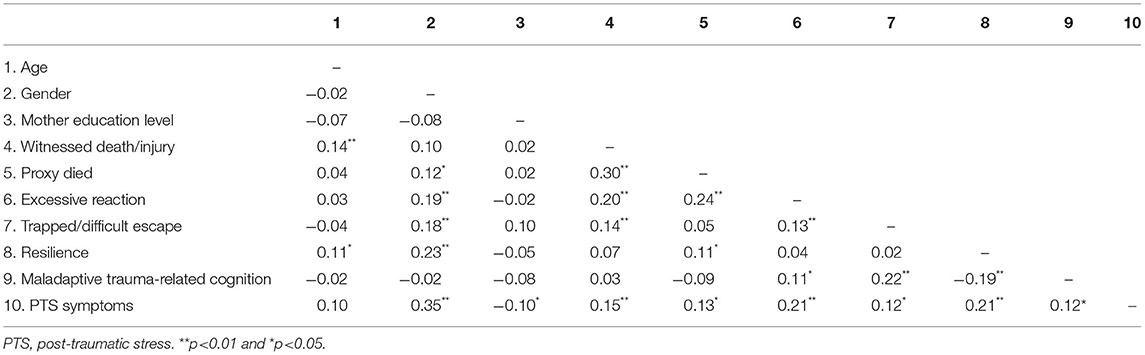
The results of zero-order correlation are shown in Table 3. This bivariate analysis was primarily used to guide the selection of variables into the regression model. Findings show that when compared with males, females had a positive but weak PTS score (rpb = 0.35). Maternal education level had a negative but negligible correlation with PTS symptoms (rpb = −0.10). In contrast, maladaptive trauma-related cognition (higher score indicating more negative trauma-related cognition) and resilience had statistically significant weak, positive correlation with PTS symptoms (r = 0.12 and r = 0.21). In addition, the variables of trauma exposure listed in Table 3 also correlated positively and significantly with PTS symptoms (r = 0.12–0.21), indicating weak relationships.
According to the regression analysis results (Table 4), the model explained 17% of the variance and was a significant predictor of PTS symptoms [F(4,404) = 22.06, p ≤ 0.001]. The female gender contributed most significantly to the model (β = 7.350, p < 0.001), followed by excessive reaction of parents during earthquake (β = 3.283, p = 0.005), maladaptive trauma-related cognition (β = 0.224, p = 0.002), and resilience (β = 0.192, p < 0.001). Simple linear regression demonstrated that the statistical significance of adolescents who witnessed injury or death during earthquake (p = 0.003), had a proxy died during earthquake (p = 0.01), and those who were trapped or had a difficult escape (p = 0.01) may potentially predict the occurrence of PTS symptoms.
Discussion
The prevalence of PTS symptoms among adolescents post-earthquake was 69.9% in this study, which was higher compared with other studies. The prevalence of PTSD among adolescents 6 months after Aceh earthquake and 12 months post-Wenchuan earthquake were 47 and 17.5%, respectively (5, 30). Furthermore, Rahmadian et al. (31) reported that 19.9% of children and adolescents who were survivors of natural disasters in Indonesia fulfilled the criteria of PTSD diagnosis. The prevalence may be affected by differences in the study population, method of assessments, time-lapse after earthquake, and the severity of the event. A few factors may contribute to the high prevalence of PTS symptoms in this study. Older children were found to be more susceptible to the development of PTSD compared with younger children (32). Other than that, recurrent exposures to disasters can potentially bring a negative additive effect on mental health (33). Moreover, the purposive sampling method of this study may also contribute to the high prevalence.
This study found a significant difference between gender with regards to severity of PTS symptoms. According to the study results, female adolescents had higher PTS symptoms score compared with males. This result is consistent with the meta-analysis by Furr et al. (34) that suggested females are more vulnerable to the development of PTS symptoms. Derivois et al. (35) and Cadichon et al. (36) also concluded that female gender is an important PTSD risk factor among the study's population. Several explanations including stronger apprehension of threat, higher extent of peritraumatic dissociation, poor social support, and gender differences in acute subjective responses to trauma were suggested by a research review (37). Witnessing injury or death during earthquakes and excessive response from parents during and after earthquakes were significantly associated with higher PTS symptoms scores. Kilic et al. (38) reported that negative effect on children was more significant when fathers became more irritable and detached. Ekşi et al. (39) and Ma et al. (40) also reported that witnessing death and suffering as well as extreme reactions from parents or other adults during and following earthquake are significant risk factors for the development of PTS symptoms. These reactions include wailing, crying, and praying loudly, which may raise children's fright, insecurity, and helplessness. As parents or adults are coping models, the children may perceive the event as frightening or even threatening after observing the adults' reactions. This finding suggests that the subjective element of disaster experience contributes to an adolescent's post-trauma response, which should be made aware and recognized in psychological interventions.
In addition, maladaptive trauma-related cognitions measured by CPTCI was found to be one of the predictors that was positively associated with PTS symptoms. A meta-analysis showed cognitive deficits regarding working memory, executive function, verbal learning and memory, visual learning and memory, information processing speed, and visuospatial function play important roles in PTS symptoms and are associated with the disorder (41). Stallard et al. (42) supported that negative trauma appraisal and cognitive coping style lead to permanent PTS symptoms. This is because the ongoing negative trauma appraisal contributes as a factor that causes the traumatic event to be experienced as a current threat even though the traumatic event happened in the past. A significant difference in cognitive style between adolescents with high risk of PTSD and low risk of PTSD was also reported in research conducted following the Wenchuan earthquake in China (40). Thus, adolescents with negative and maladaptive trauma-related cognitions require careful screening and monitoring for PTSD development.
The findings of the study revealed that resilience was significantly and positively associated with PTS symptoms among adolescents exposed to Lombok earthquakes. A study done among street children in Haiti showed that those with severe PTS symptoms possessed higher level of resilience (43). On the contrary, other studies showed adolescents with higher resilience level had lower risk of developing PTS symptoms (4, 44–46). Resilience was also shown to be a predictor of PTSD in a recent study (47). While resilience has been an established protective factor that modulates response toward trauma, the study results showed that adolescents with higher resilience level were significantly associated with higher PTS scores. We postulated that the high scoring of PTS symptoms in these participants may be contributed by repeated exposures to earthquakes within a 9-month period. In this study, as high as 50.4% of participants experienced earthquakes three times in Lombok, Indonesia. Previous studies have observed dose gradients of trauma, in which more intense, more prolonged, and more cumulative traumas were associated with more symptoms (48, 49). Adolescents who experienced additional trauma after an earthquake exposure were also shown to be more likely to develop delayed or chronic PTS symptoms (50). Moreover, a longitudinal study over 17 years among child survivors of dam collapse found that PTSD remained present at a higher-than-normal rate; however, resilience and recovery were observed in most exposed individuals (51).
Also, resilience is not merely a personality trait, but it has been broadening to a more ecological context that can be developed at any age based on individual relationships and environments (52–54). It is conceivable that in the study, the measure of current resilience level captured both effects of existing resilience and growth following trauma exposures. The high level of resilience in this population may be contributed by various external resources including good social support from caregivers and community, religion, spirituality, and cultural resources, not solely associated with the experiences from repeated earthquakes. Different dimensions of social support from family members, peers, teachers, and community were identified as resources of resilience in previous studies (55–57). The study participants scored high with regards to relational resilience, which also suggested that family members and peers were important resources for adolescents to show resilience. Besides, our participants are all Muslims. While religion and spirituality were shown to promote resilience (58–60), a study conducted in Islamic population pointed out that religion was a key factor in facing the tragedy of tsunami in their communities and reinforcing social ties (61).
Several potential predictors of PTS symptoms were ascertained in this study, including adolescents who witnessed injury or death during earthquake, had a proxy died during earthquake, and those who were trapped or had a difficult escape. These exposures to traumatic events during earthquake were significantly associated with higher PTS scores, which were consistent with other studies (62–64). The results may imply that adolescents who had higher degree of physical exposure to a disaster portrayed a larger impact on their reactions or coping in post-trauma adjustment. However, these findings must be cautiously interpreted due to the weak association in the study results. The potential of these exposure indicators as predictors of PTS symptoms warrants future research to gain further insight.
More importantly, the study results demonstrated that there was a negative correlation between maladaptive trauma-related cognitions and resilience. Limited studies have adequately answered the relationship between these two salient indicators of PTS symptoms. This finding will add value to and consolidate the holistic interventions among adolescents exposed to disasters as cognitive functioning is one of many aspects that is often disregarded in post-traumatic psychopathology. Our growing understanding of negative trauma-related appraisals and resilience will hopefully help with the development of more strategies for PTSD management. The psychological therapy of PTSD is deemed to focus on the key role of various predictors in overcoming the adversity and trauma response among adolescents, for instance, avoidance, intrusion, and arousal. Intervention designs should be based on the unique gender differences in responding to traumatic events as females exhibited higher PTS scores compared with males. Also, it is necessary to be aware that proxy's reaction in adverse situations may influence children's stress responses. Thus, family-based therapy is recommended as the importance of proxy's response in preventing stress reactions of adolescents needs to be emphasized. Moreover, in the situation of family members who were affected during earthquakes, the vulnerable adolescents should be screened vigorously and provided intervention, if necessary, even though they appeared physically or mentally well.
This study has some limitations. A cross-sectional study design was used and hence, the relationship between the exposures and outcomes could not be well explained. Thus, further longitudinal studies on the same population may produce more valuable results. Besides, the collection of data took place a year after the earthquake incidents. The results may not explain the direct acute effects of the earthquakes and may not be applicable to other time frames after earthquakes. The cognition and resilience of the samples might be affected by other confounding variables such as social support in this period. Furthermore, the back-translated questionnaires in Indonesian language have not been validated in the local population. The questionnaires were administered by self-reporting method, which carried the risk of information bias and led to less accuracy. Future studies may employ other information sources such as caregivers' and teachers' reports, as well as clinical interviews to enhance the accuracy and reliability of the findings.
Conclusions
The findings of this study revealed that the natural disaster, namely earthquakes, brought notable psychological impacts on adolescents in Lombok, Indonesia. This was discernible by the high prevalence of PTS symptoms in the participants. Several predictors of PTS symptoms among adolescents post-earthquakes were identified in this study, including maladaptive trauma-related cognitions, resilience, and excessive reactions of proxy during earthquakes. These are worth targeting and prioritizing in future post-disaster interventions. Adolescents who witnessed injury or death, had a proxy died, and had difficulty in escaping or being trapped during earthquakes were identified as the potential predictors of PTS symptoms, which warrant further studies. Early identification of vulnerable adolescents is essential to offer preventive measures and to provide effective psychological support if necessary. The negative association between maladaptive trauma-related cognition and resilience further emphasized the role of cognition in post-traumatic psychopathology and should be further investigated in future studies.
Data Availability Statement
The datasets presented in this article are not readily available because data cannot be shared due to confidentiality issues. Requests to access the datasets should be directed to Suzaily Wahab, c3V6YWlseXdoYkB5YWhvby5jb20=.
Ethics Statement
The study involving human participants was reviewed and approved by Secretariat of Research and Innovation, Faculty of Medicine, The National University of Malaysia and Ethical Committee of Medical Research, Faculty of Medicine, The University of Mataram. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
SW and HD conceptualized and contributed to the study design. LY, WC, MY, NS, NA, CM, and SMW collected the data. RI, HD, WC, LY, and AO performed the data analysis and interpretation. SW, LY, WC, MY, NS, and HD wrote the draft of the article. Finally, SW, RI, and HD critically revised the article. All authors have made substantive intellectual contributions to the manuscript, read, and approved the final article.
Funding
This is an independent research funded and supported by the Ministry of Higher Education, Malaysia and Universiti Kebangsaan Malaysia Medical Centre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer CN declared a shared affiliation, with no collaboration, with the authors SW, LY, WC, MY, NS, RI, AO, and HD at the time of the review.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank all participants of this study. We would also like to acknowledge the collateral support from Faculty of Health Science, Universitas Muhammadiyah Mataram, Indonesia.
References
1. de Terte I, Gardner D, Hudson-doyle E, Bethell F. Adversity in the Asia Pacific region: challenges facing health and society. J Loss Trauma. (2018) 23:347–50. doi: 10.1080/15325024.2018.1479153
2. American Psychiatric Association. Trauma- and stressor-related disorders. In: Diagnostic and Statistical Manual of Mental Disorders (5th ed), DSM-5. Arlington, VA: American Psychiatric Association (2013).
3. Asim M, Mekkodathil A, Sathian B, Elayedath R, N RK, Simkhada P, et al. Post-traumatic stress disorder among the flood affected population in Indian subcontinent. Nepal J Epidemiol. (2019) 9:755–8. doi: 10.3126/nje.v9i1.24003
4. Ying L, Wu X, Lin C, Jiang L. Traumatic severity and trait resilience as predictors of posttraumatic stress disorder and depressive symptoms among adolescent survivors of the Wenchuan earthquake. PLoS ONE. (2014) 9:e89401. doi: 10.1371/journal.pone.0089401
5. Marthoenis M, Ilyas A, Sofyan H, Schouler-Ocak M. Prevalence, comorbidity and predictors of post-traumatic stress disorder, depression, and anxiety in adolescents following an earthquake. Asian J Psychiatr. (2019) 43:154–9. doi: 10.1016/j.ajp.2019.05.030
6. Boterhoven de Haan KL, Lee CW, Fassbinder E, Voncken MJ, Meewisse M, van Es SM, et al. Imagery rescripting and eye movement desensitisation and reprocessing for treatment of adults with childhood trauma-related post-traumatic stress disorder: IREM study design. BMC Psychiatry. (2017) 17:165. doi: 10.1186/s12888-017-1330-2
7. Meiser-Stedman R, McKinnon A, Dixon C, Boyle A, Smith P, Dalgleish T. A core role for cognitive processes in the acute onset and maintenance of post-traumatic stress in children and adolescents. J Child Psychol Psychiatry. (2019) 60:875–84. doi: 10.1111/jcpp.13054
8. Altamore F, Grappasonni I, Laxhman N, Scuri S, Petrelli F, Grifantini G, et al. Psychological symptoms and quality of life after repeated exposure to earthquake: a cohort study in Italy. PLoS ONE. (2020) 15:e0233172. doi: 10.1371/journal.pone.0233172
9. Md Akhir NH, Azman A, Md Akhir N. Kesan bencana banjir di Kelantan terhadap kesejahteraan psikologi sukarelawan (An impact of flood disaster in Kelantan towards psychological well-being among volunteers). Jurnal Psikologi Malaysia. (2018) 32:102–11. Available online at: http://spaj.ukm.my/ppppm/jpm/article/view/433 (accessed August 8, 2021).
10. Long LJ, Bistricky SL, Phillips CA, D'Souza JM, Richardson AL, Lai BS, et al. The potential unique impacts of hope and resilience on mental health and well-being in the wake of Hurricane Harvey. J Trauma Stress. (2020) 33:962–72. doi: 10.1002/jts.22555
11. Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: the mediating role of social support. Public Health. (2014) 128:430–7. doi: 10.1016/j.puhe.2014.03.002
12. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
13. Brown M, Agyapong V, Greenshaw A, Cribben I, Brett-MacLean P, Drolet J, et al. Significant PTSD and other mental health effects present 18 months after the Fort McMurray wildfire: findings from 3,070 grades 7–12 students. Front Psychiatry. (2019) 10:623. doi: 10.3389/fpsyt.2019.00623
14. Md Akhir N, Soh OK, Md Akhir NH. Faktor pengaruh resiliensi mangsa banjir: Kajian kes di Kelantan (Factors influencing resilience of flood victims: a case study in Kelantan). Jurnal Psikologi Malaysia. (2020) 34:105–18. Available online at: http://spaj.ukm.my/ppppm/jpm/article/view/565 (accessed August 8, 2021).
15. Setiawan GP, Viora E. Disaster mental health preparedness plan in Indonesia. Int Rev Psychiatry. (2006) 18:563–6. doi: 10.1080/09540260601037920
16. Acharya L, Upadhya KD, Kortmann F. Mental health and psychosocial support aspects in disaster preparedness: Nepal. Int Rev Psychiatry. (2006) 18:587–92. doi: 10.1080/09540260601038407
17. Htay H. Mental health and psychosocial aspects of disaster preparedness in Myanmar. Int Rev Psychiatry. (2006) 18:579–85. doi: 10.1080/09540260601108952
18. Powell T, Li SJ, Hsiao Y, Ettari C, Bhandari A, Peterson A, et al. Investigating the aftershock of a disaster: a study of health service utilization and mental health symptoms in post-earthquake Nepal. Int J Environ Res Public Health. (2019) 16:1369. doi: 10.3390/ijerph16081369
19. Rasido I, Patodo M. Post disaster: earthquake, tsunami, liquefaction mental health prevalence of Tadulako University students. Enferm Clin. (2020) 30:214–8. doi: 10.1016/j.enfcli.2019.10.071
20. Liu M, Wang L, Shi Z, Zhang Z, Zhang K, Shen J. Mental health problems among children one-year after Sichuan earthquake in China: a follow-up study. PLoS ONE. (2011) 6:e14706. doi: 10.1371/journal.pone.0014706
21. Schwind JS, Formby CB, Santangelo SL, Norman SA, Brown R, Frances RH, et al. Earthquake exposures and mental health outcomes in children and adolescents from Phulpingdanda village, Nepal: a cross-sectional study. Child Adolesc Psychiatry Ment Health. (2018) 12:1–9. doi: 10.1186/s13034-018-0257-9
22. World Health Organization. Recognizing Adolescence. (2014). Available online at: https://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html (accessed August 8, 2021).
23. Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies: A Practical Manual. Geneva: World Health Organization. (1991). Available online at: https://whqlibdoc.who.int/publications/9241544058_(p1-p22).pdf (accessed August 8, 2021).
24. Children's Revised Impact of Event Scale (CRIES-13). Children and War Foundation. (2005). Available online at: https://emdrfoundation.org/toolkit/cries-13.pdf
25. Meiser-Stedman R, Smith P, Bryant R, Salmon K, Yule W, Dalgleish T, et al. Development and validation of the Child Post-Traumatic Cognitions Inventory (CPTCI). J Child Psychol Psychiatry. (2009) 50:432–40. doi: 10.1111/j.1469-7610.2008.01995.x
26. Jefferies P, McGarrigle L, Ungar M. The CYRM-R: a rasch-validated revision of the child and youth resilience measure. J Evidence-Based Soc Work. (2019) 16:70–92. doi: 10.1080/23761407.2018.1548403
27. Smith P, Perrin S, Dyregrov A, Yule W. Principal components analysis of the impact of event scale with children in war. Pers Individ Dif. (2003) 34:315–22. doi: 10.1016/S0191-8869(02)00047-8
28. Perrin S, Meiser-Stedman R, Smith P. The Children's Revised Impact of Event Scale (CRIES): validity as a screening instrument for PTSD. Behav Cogn Psychother. (2005) 33:487–98. doi: 10.1017/S1352465805002419
29. Borualogo IS, Jefferies P. Adapting the child and youth resilience measure-revised for Indonesian contexts. J Educ Health Community Psychol. (2019) 8:480–98. doi: 10.12928/jehcp.v8i4.12962
30. Ying LH, Wu XC, Lin CD. Longitudinal linkages between depressive and posttraumatic stress symptoms in adolescent survivors following the Wenchuan earthquake in China: a three-wave, cross-lagged study. Sch Psychol Int. (2012) 33:416–32. doi: 10.1177/0143034311421271
31. Rahmadian AA, Furqon, LN SY, Rusmana N. Prevalensi PTSD dan karakteristik gejala stres pascatrauma pada anak dan remaja korban bencana alam. Edusentris, Jurnal Ilmu Pendidikan dan Pengajaran. (2016) 3:1–17. doi: 10.17509/edusentris.v3i1.184
32. Tang B, Deng Q, Glik D, Dong J, Zhang L. A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. Int J Environ Res. (2017) 14:1537. doi: 10.3390/ijerph14121537
33. Geng F, Zhou Y, Liang Y, Fan F. A longitudinal study of recurrent experience of earthquake and mental health problems among Chinese adolescents. Front Psychol. (2018) 9:1259. doi: 10.3389/fpsyg.2018.01259
34. Furr JM, Comer JS, Edmunds JM, Kendall PC. Disasters and youth: a meta-analytic examination of posttraumatic stress. J Consult Clin Psychol. (2010) 78:765–80. doi: 10.1037/a0021482
35. Derivois D, Mérisier GG, Cénat JM, Castelot V. Symptoms of posttraumatic stress disorder and social support among children and adolescents after the 2010 Haitian earthquake. J Loss Trauma. (2014) 19:202–12. doi: 10.1080/15325024.2013.789759
36. Cadichon JM, Lignier B, Cénat JM, Derivois D. Symptoms of PTSD among adolescents and young adult survivors six years after the 2010 Haiti earthquake. J Loss Trauma. (2017) 22:646–59. doi: 10.1080/15325024.2017.1360585
37. Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychol Bull. (2007) 133:183–204. doi: 10.1037/0033-2909.133.2.183
38. Kilic EZ, Ozguven HD, Sayil I. The psychological effects of parental mental health on children experiencing disaster: the experience of Bolu earthquake in Turkey. Fam Process. (2003) 42:485–95. doi: 10.1111/j.1545-5300.2003.00485.x
39. Ekşi A, Braun KL, Ertem-Vehid H, Peykerli G, Saydam R, Toparlak D, et al. Risk factors for the development of PTSD and depression among child and adolescent victims following a 7.4 magnitude earthquake. Int J Psychiatry Clin Pract. (2007) 11:190–9. doi: 10.1080/13651500601017548
40. Ma X, Liu X, Hu X, Qiu C, Wang Y, Huang Y, et al. Risk indicators for post-traumatic stress disorder in adolescents exposed to the 5.12 Wenchuan earthquake in China. Psychiatry Res. (2011) 189:385–91. doi: 10.1016/j.psychres.2010.12.016
41. Scott JC, Matt GE, Wrocklage KM, Crnich C, Jordan J, Southwick SM, et al. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. (2015) 141:105–40. doi: 10.1037/a0038039
42. Stallard P, Smith E. Appraisals and cognitive coping styles associated with chronic post-traumatic symptoms in child road traffic accident survivors. J Child Psychol Psychiatry. (2007) 48:194–201. doi: 10.1111/j.1469-7610.2006.01692.x
43. Cénat JM, Derivois D, Hébert M, Amédée LM, Karray A. Multiple traumas and resilience among street children in Haiti: psychopathology of survival. Child Abuse Negl. (2018) 79:85–97. doi: 10.1016/j.chiabu.2018.01.024
44. Wrenn GL, Wingo AP, Moore R, Pelletier T, Gutman AR, Bradley B, et al. The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients. J Natl Med Assoc. (2011) 103:560–6. doi: 10.1016/S0027-9684(15)30381-3
45. Bensimon M. Elaboration on the association between trauma, PTSD and posttraumatic growth: the role of trait resilience. Pers Individ Dif. (2012) 52:782–7. doi: 10.1016/j.paid.2012.01.011
46. Heetkamp T, de Terte I. PTSD and resilience in adolescents after New Zealand earthquakes. New Zealand J Psychol. (2015) 44:31–8. Available online at: https://www.psychology.org.nz/journal-archive/NZJP-Volume-44-No-1-2015.pdf#page=31 (accessed August 8, 2021).
47. Mat Salleh MN, Ismail H, Mohd Yusoff H. Prevalence and predictors of post-traumatic stress disorder (PTSD) among firefighters: a scoping review. Int J Public Health Res. (2020) 10:1183–94. Available online at: http://spaj.ukm.my/ijphr/index.php/ijphr/article/view/259 (accessed August 8, 2021).
48. Masten AS. Resilience of children in disasters: a multisystem perspective. Int J Psychol. (2021) 56:1–11. doi: 10.1002/ijop.12737
49. Bornstein MH, Leventhal TE, Lerner RM. Handbook of Child Psychology and Developmental Science: Ecological Settings and Processes. Hoboken, NJ: John Wiley & Sons, Inc. (2015).
50. Silwal S, Chudal R, Dybdahl R, Sillanmäki L, Lien L, Sourander A. Post-traumatic stress and depressive symptoms among adolescents after the 2015 earthquake in Nepal: a longitudinal study. Child Psychiatry Hum Dev. (2021) 19:1. doi: 10.1007/s10578-021-01136-3
51. Green BL, Grace MC, Vary MG, Kramer TL, Gleser GC, Leonard AC. Children of disaster in the second decade: a 17-year follow-up of Buffalo Creek survivors. J Am Acad Child Adolesc Psychiatry. (1994) 33:71–9. doi: 10.1097/00004583-199401000-00011
52. Rutter M. Resilience as a dynamic concept. Dev. Psychopathol. (2012) 24:335–44. doi: 10.1017/S0954579412000028
53. Gillespie BM, Chaboyer W, Wallis M. Development of a theoretically derived model of resilience through concept analysis. Contemp. Nurse. (2007) 25:124–35. doi: 10.5172/conu.2007.25.1-2.124
54. Fleming J, Ledogar RJ. Resilience, an evolving concept: a review of literature relevant to Aboriginal research. Pimatisiwin. (2008) 6:7–23. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2956753/
55. Lerner RM, Liben LS, Mueller U. Handbook of Child Psychology and Developmental Science, Cognitive Processes. Hoboken, NJ: John Wiley & Sons (2015).
56. Ungar M, Connelly G, Liebenberg L, Theron L. How schools enhance the development of young people's resilience. Soc Indic Res. (2019) 145:615–27. doi: 10.1007/s11205-017-1728-8
57. Husni Rahiem MD, Krauss SE, Rahim H. The child victims of the Aceh tsunami: stories of resilience, coping and moving on with life. Procedia Eng. (2018) 212:1303–10. doi: 10.1016/j.proeng.2018.01.168
58. Milstein G. Disasters, psychological traumas, and religions: resiliencies examined. Psychol Trauma. (2019) 11:559–62. doi: 10.1037/tra0000510
59. Gunnestad A, Thwala S. Resilience and religion in children and youth in Southern Africa. Int J Child Spiritual. (2011) 16:169–85. doi: 10.1080/1364436X.2011.580726
60. Kim S, Esquivel GB. Adolescent spirituality and resilience: theory, research, and educational practices. Psychol Sch. (2011) 48:755–65. doi: 10.1002/pits.20582
61. Guarnacci U. Joining the dots: social networks and community resilience in post-conflict, post-disaster Indonesia. Int Disaster Risk Reduct. (2016) 16:180–91. doi: 10.1016/j.ijdrr.2016.03.001
62. Marthoenis M, Nirwana A, Fathiariani L. Prevalence and determinants of posttraumatic stress in adolescents following an earthquake. Indian J Psychiatry. (2019) 61:526–8. doi: 10.4103/psychiatry.IndianJPsychiatry_35_19
63. Zhou X, Kang L, Sun X, Song H, Mao W, Huang X, et al. Prevalence and risk factors of post-traumatic stress disorder among adult survivors six months after the Wenchuan earthquake. Compr Psychiatry. (2013) 54:493–9. doi: 10.1016/j.comppsych.2012.12.010
Keywords: natural disasters, post-traumatic stress, cognition, resilience, adolescent
Citation: Wahab S, Yong LL, Chieng WK, Yamil M, Sawal NA, Abdullah NQ, Muhdisin Noor CR, Wd Wiredarma SM, Ismail R, Othman AH and Damanhuri HA (2021) Post-traumatic Stress Symptoms in Adolescents Exposed to the Earthquake in Lombok, Indonesia: Prevalence and Association With Maladaptive Trauma-Related Cognition and Resilience. Front. Psychiatry 12:680393. doi: 10.3389/fpsyt.2021.680393
Received: 14 March 2021; Accepted: 27 September 2021;
Published: 08 November 2021.
Edited by:
Alexis Revet, Centre Hospitalier Universitaire de Toulouse, FranceReviewed by:
Asilay Seker, Cambridgeshire and Peterborough NHS Foundation Trust, United KingdomChong Guan Ng, University of Malaya, Malaysia
Copyright © 2021 Wahab, Yong, Chieng, Yamil, Sawal, Abdullah, Muhdisin Noor, Wd Wiredarma, Ismail, Othman and Damanhuri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suzaily Wahab, c3V6YWlseXdoYkB5YWhvby5jb20=
 Suzaily Wahab
Suzaily Wahab Li Ling Yong
Li Ling Yong Wei Keong Chieng
Wei Keong Chieng Myristica Yamil
Myristica Yamil Noor Azah Sawal
Noor Azah Sawal Nurul Qiyaam Abdullah2
Nurul Qiyaam Abdullah2 Hanafi Ahmad Damanhuri
Hanafi Ahmad Damanhuri