
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 01 July 2021
Sec. Mood Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.677136
This article is part of the Research TopicSleep and Psychological Trauma or StressView all 10 articles
 Md Dilshad Manzar1
Md Dilshad Manzar1 Ahmad H. Alghadir2
Ahmad H. Alghadir2 Masood Khan2*
Masood Khan2* Mohammed Salahuddin3,4
Mohammed Salahuddin3,4 Abdulrhman Albougami1
Abdulrhman Albougami1 Jestoni D. Maniago1
Jestoni D. Maniago1 Brian A. Vasquez1
Brian A. Vasquez1 Seithikurippu R. Pandi-Perumal5
Seithikurippu R. Pandi-Perumal5 Ahmed S. Bahammam6,7
Ahmed S. Bahammam6,7Background: Anxiety symptoms, stress, poor sleep, and inadequate sleep hygiene are common in university students and these affect their learning and increase attrition. However, limited knowledge exists about the inter-relationship between these factors among university students in low-middle income countries. Therefore, this study aimed to investigate the prevalence of anxiety symptoms and their relationship with sleep quality, sleep hygiene practices, and psychological stress.
Materials and Methods: A cross-sectional study was conducted with a randomly selected sample of students in Mizan-Aman, Ethiopia. Participants completed a self-administered questionnaire, which included questions about socio-demographics, socio-economic factors, the Leeds Sleep Evaluation Questionnaire-Mizan, Sleep hygiene index, Perceived stress scale-10 (PSS-10), and Generalized anxiety disorder-7 scale (GAD-7).
Results: The prevalence of anxiety symptoms was about 22%. Multivariate regression analysis showed that both anxiety status χ2[(13, N = 480) = 82.68, p < 0.001], and increasing levels of anxiety (model adjusted R2 = 0.204, p < 0.001) were associated with greater psychological stress, inadequate sleep hygiene practices, and poor sleep quality scores after adjusting for age, gender, attendance, substance use, years of university education, time spent in athletic activity every day, and frequency of tea/coffee consumption.
Conclusion: There was a high prevalence of anxiety symptoms in this study population, and this condition was associated with psychological stress, poor sleep, and inadequate sleep hygiene parameters. These results suggest a need to address the various aspects of mental health and its diverse sleep correlates in university students.
Anxiety is one of the common mental health disorders (global prevalence of 3.7%), associated with significant comorbidity and mortality (1). Anxiety is often comorbid with depression or other anxiety disorders, which renders its diagnosis and treatment complicated (2). As a result, anxiety remains undiagnosed and undertreated in most primary care settings (3). Anxiety has added indirect costs to the economic burden of countries owing to significant loss of personnel productivity and increased use of primary health care services (4). As such, it is important to identify anxiety for early diagnosis and treatment. This is more relevant for university students of the present-day world as mental health issues are common and usually associated with pressure to achieve higher academic grades, a transition to a higher level of studies, and pressure to succeed (5). Estimates vary but a large proportion of college-going students show stress (~51–67%), and anxiety symptoms (~34–56%) (6, 7).
Poor sleep quality adversely influences day-to-day activities and may predispose affected individuals to poor health and quality of life outcomes and mental health issues such as anxiety, depression, and other problems (8). There are pieces of evidence showing that anxiety is correlated with poor sleep quality in insomnia (9, 10). Inadequate sleep hygiene practices are correlated with measures of anxiety and stress in Saudi university students (11). However, the association was determined using bivariate analysis, and therefore it is desirable to further investigate this relationship in other populations using multivariate analysis. Sleep quality is associated with psychological distress and inadequate sleep hygiene among Iranian pre-clinical students (12). We recently found that insomnia is highly prevalent among university students and that it is associated with anxiety, and inadequate sleep hygiene practices (13). However, to the best of our knowledge, no study investigated anxiety, and its association with psychological stress, sleep quality and sleep hygiene.
Moreover, two recent studies in the Ethiopian population determined the prevalence and determinants of anxiety in healthcare workers (14) and women attending prenatal care (15). However, there are few reports which determined the prevalence of anxiety in the Ethiopian student population and studied its associated conditions. Therefore, this study was planned to investigate the prevalence of anxiety and its relationship with psychological stress, sleep quality, and sleep hygiene practices among Ethiopian university students.
A total of 17936 students were enrolled in both the campuses located at Mizan city and Tepi city of the Mizan-Tepi University (MTU) in regular and continuous programs in 2017–18 academic year. Haile et al. had reported a prevalence of 63.1% for common mental disorders especially anxiety and depressive symptoms in a similar setting of university students in Ethiopia (16). Therefore, a sample size of 598 was estimated using 5% as margin of error, confidence interval of 99%, population (all students of MTU), and 63.1% as expected response distribution. We randomly selected the Mizan campus for the recruitment of participants in this cross-sectional study. A list of 750 students was initially prepared by a simple random method. Of these students, 189 declined to participate or were absent on the day of the interview, 36 were excluded after screening for the exclusion criteria, and 26 responses were deleted because of person-level missing values, that is, missing responses for most of the items of the four standard questionnaires. Finally, analysis of a dataset of collegiate young adults (n = 499, age: 21.34 ± 2.76 years) is presented. The final sample size was deemed adequate because it was still more than a sample size (351) estimated using 5% as margin of error, confidence interval of 95%, population (all students of MTU), and 63.1% as expected response distribution. Respondents were asked to complete a self-administered questionnaire during in-person meetings with the research team. These meetings were scheduled during the semesters to avoid bias from the examination-related stress. Students who were pursuing higher education from Mizan-Tepi University, Mizan-Aman, Ethiopia were included in the study. Those with an idiosyncratic account of self-reported recollected complaints and those taking neuropsychiatric medications were excluded from the study. Institutional review committee approval from the College of Health Sciences, Mizan-Tepi University, Ethiopia was acquired. Before the collection of data, a precis of the intent and methodology to be implemented was explained to the respondents. The nature of participation was clarified to the respondents as voluntary and their right to terminate participation at any time-point was emphasized. There were no direct benefits for respondents and no risks or chances of harm. It was also communicated to the respondents that they will not receive any fee in exchange for participation. Stringent provisions for privacy and confidentiality were implemented. The study strictly conforms with the Helsinki declaration. Informed written consent for participation and publication were obtained. The study utilized five tools: (i) Generalized anxiety disorder-7 scale (GAD-7), (ii) Leeds Sleep Evaluation Questionnaire-Mizan, (iii) Perceived stress scale-10 (PSS-10), (iv) Sleep hygiene index, and (v) a semi-structured socio-demographics tool. Since the English language is the medium of instruction in all federal universities in Ethiopia, all the tools employed in this study were in English.
GAD-7 scale is a succinct but scrupulously validated inventory to examine anxiety symptoms (17–19). It has been shown to have sufficient diagnostic validity for vetting a wide-array of anxiety-related disorders: “GAD, panic disorder, social phobia, and post-traumatic stress disorder” (18). A cut-point of 10 for GAD-7 is observed in this study to determine anxiety symptoms. A sensitivity of 68% and specificity of 88% were reported by Kroenke et al. at this cut-point. Seven items are scored using an ordinal scale (0–3) to account for the cumulative regularity of anxiety symptoms within the last 7 days (18). The GAD-7 total score, ranging from 0–21, is equal to the linear summation of all the 7-items (17, 18). The severity of the anxiety increases with the increment in the GAD-7 total score (17, 18). The GAD-7 is a valid instrument for screening anxiety in university students in Afro-Asian countries (19, 20).
SHI is a validated 13-item self-report measure of sleep hygiene (21). This study adapted the version with a slightly modified scoring system (dichotomized rating for each of the items: 0 = No; 1 = Yes). SHI total score is the summation of all the items ranging from 0–13, where a lower score infers good sleep hygiene practices and a higher score suggests the otherwise (21). The reliability of this version (dichotomized scoring) is sufficient as indicated by a GLB = 0.85 and Standardized α = 0.66 (22). SHI is valid among university students (11).
Manzar et al. (23) validated the modified version of the LSEQ (i.e., LSEQ-M) (24). The revision was composed to gauge the sleep complaints among the student populace. A 100 mm visual analog scale (VAS) was utilized to rate each of the 10-items (23, 25). Lower scores imply more severe sleep complaints (23). The scores (0–100 range) of each item are transformed into 0–10 range which when summed will yield an LSEQ-M total score ranging from 0–100 (23). LSEQ-M has requisite reliability, adequate internal homogeneity, construct validity, and structural validity in university students (23, 25).
PSS-10 is a succinct (10-items) but scrupulously validated scale of psychological stress (26). PSS-10 is a self-report that appraises the stress experienced by the respondents throughout the month preceding the test. Each item is rated using a 4-point ordinal scale (0 = Never; 4 = Very Often), where higher scores would infer a cumulative regularity of stress-related complaints. The linear summation of all the 10-items will generate the total PSS-10 score (26). The higher the psychological stress level, the higher the PSS-10 total scores. Manzar et al. (27) reported that PSS-10 has adequate psychometric validity when utilized in assessing the psychological stress among Ethiopian university students.
A concise questionnaire was utilized to register the socio-demographic characteristics of the respondents (e.g., age, gender, years of education, attendance (% of classes attended), substance use, daily athletic activity duration, and frequency of daily tea/coffee consumption). Substance use item recorded self-reported habitual consumption of alcohol and/or Khat and/or smoking.
In this study, statistical analysis was performed using SPSS version 26.0. Participants' characteristics were presented using these: mean ± SD (continuous) and percentage and frequency (categorical variables). Chi-square test or Fisher's exact test (categorical variables) and Student's independent t-test (continuous variables) were employed for bivariate analysis.
Multivariate analysis was performed using binary logistic and multiple linear regression. Nineteen multivariate outliers [Mahalanobis distance criteria; X2 (9) = 27.88, p < 0.001] and high leverage points and highly influential points (Cook's distance < 1.0) were removed for performing multivariate analysis. There were few univariate outliers in the attendance and age variables but these were not removed because those values were found to be correct and not arising out of data entry mistakes. Other assumptions for binary logistic regression like (i) independence of observations, (ii) absence of multicollinearity among independent variables as determined by the Spearman's correlation coefficients, and (iii) linear relationship with log odds of all independent variables were satisfied by the dataset. Additional assumptions for the multiple linear regression: (i) linear relation between outcome and independent variable as determined by scatterplot and partial regression plots, (ii) homoscedasticity as determined by studentized residuals plotted against the unstandardized predicted values, and (iii) normal distribution of the residual errors were satisfied by the dataset.
All the covariates and independent variables except gender, attendance, years of education, and frequency of daily tea/coffee consumption were significantly correlated with anxiety. However, gender, attendance, years of education, and frequency of daily tea/coffee consumption were used as covariates or predictors because earlier works have shown them to be associated with anxiety (28–31).
Most of the participants (80.6%) were males (Table 1). Three-fourth of the collegiate young adults (75%) were studying in the first 2 years of university education (Table 1). The average of attendance, PSS-10 total score, LSEQ-M total score, and SHI total score was 95.32 ± 6.87, 18.83 ± 6.43, 60.08 ± 21.19, and 6.44 ± 2.39, respectively (Table 1). The prevalence of anxiety symptoms was 21.6%, and the average GAD-7 total score was 7.2 ± 4.3 in the study sample.
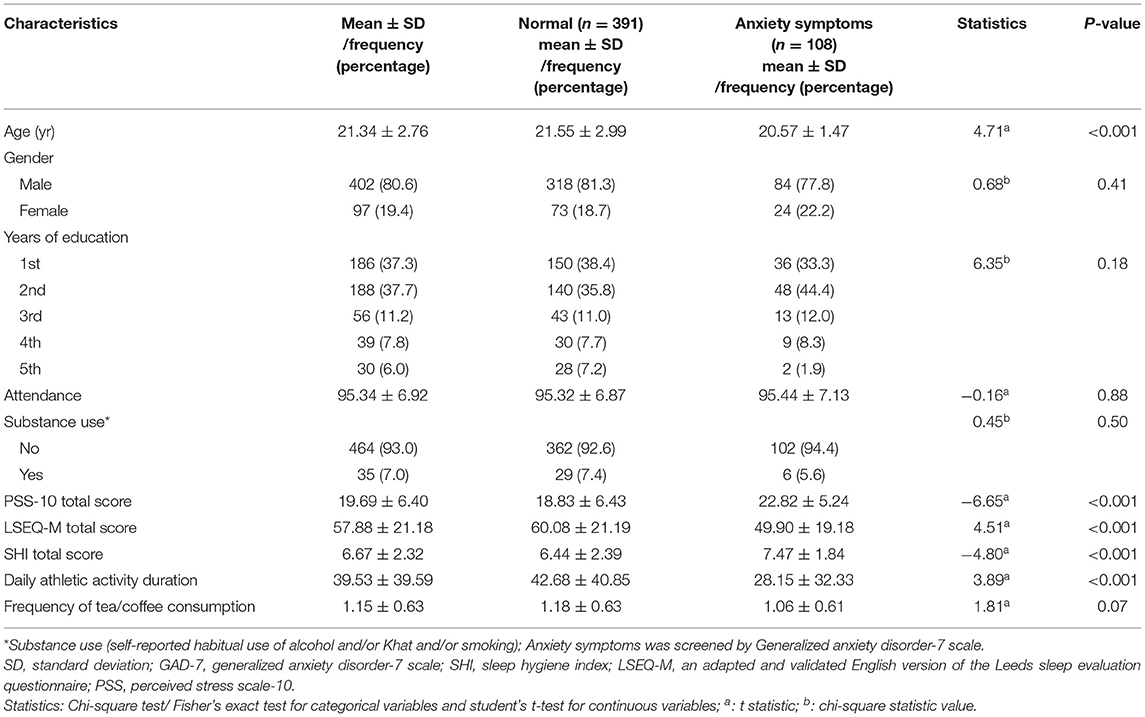
Table 1. Participants' characteristics and their relationship (bivariate) with anxiety in Ethiopian collegiate young adults.
The bivariate analysis predicted that anxiety was more common in students with lower age (20.57 ± 1.47 vs. 21.55 ± 2.99, p < 0.001) and those who spent less time in athletic activities every day (28.15 ± 32.33 vs. 42.68 ± 40.85, p < 0.001) (Table 1). Both PSS-10 total score (22.82 ± 5.24 vs. 18.83 ± 6.43, p < 0.001) and SHI total score (7.47 ± 1.84 vs. 6.44 ± 2.39, p < 0.001) were higher in the anxiety group than normal (Table 1). Similarly, the anxiety group showed lower values for LSEQ-M total score (49.90 ± 19.18 vs. 60.08 ± 21.19, p < 0.001), indicating poorer sleep than the normal young adults (Table 1).
A binary logistic regression was run to predict anxiety; this model was adjusted for age, gender, attendance (percentage of lectures attended), substance use (self-reported habitual use of alcohol and/or Khat and/or smoking), years of university education, time spent in athletic activity every day, and frequency of tea/coffee consumption. The model with three predictors, that is, PSS-10 total score, SHI total score, and LSEQ-M total score were significant in comparison to a model with only intercepts; χ2(13, N = 480) = 82.68, p < 0.001. The model with these predictors explained 24.1% of the variance in the classification of anxiety with an accuracy of 78.8%. Increasing scores of PSS-10 and SHI and the decreasing score of LSEQ-M were associated with anxiety status (Table 2).
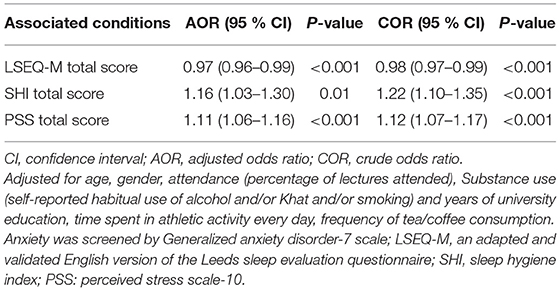
Table 2. Binary logistic regression: association of anxiety with psychological stress, poor sleep, and inadequate sleep hygiene in Ethiopian collegiate young adults.
Further, a multiple linear regression model assessed the extent to which inadequate sleep hygiene, poor sleep, and psychological stress predict changes in anxiety levels. Increasing severity of the anxiety (implied by increasing GAD-7 total score) was predicted by an increasing level of poor sleep (lower LSEQ-M total score), inadequate sleep hygiene (higher SHI total score), and increasing psychological stress (increasing PSS-10 total score) (model adjusted R2 = 0.204, p < 0.001) (Table 3).
In the present study, (i) a high prevalence of anxiety was found in the study population of Ethiopian university students, and (ii) both status of anxiety and an increasing level of anxiety were found to be associated with psychological stress, poor sleep quality, and inadequate sleep hygiene practices. To the best of our knowledge, this is the first study to demonstrate the status of having an anxiety and increasing level of anxiety to be associated with poor sleep, inadequate sleep hygiene practice, and psychological stress. The findings of the present study are strengthened by the fact that all the measures were standard questionnaires that have previously been validated in university students (11, 19, 23, 27). Furthermore, the results are reinforced by the fact that the relationship was significant in the multivariate models after adjusting for many of the known covariates (28–31).
The prevalence of anxiety (~22%) in this study was slightly lower than that reported by a recent systematic review, that is, 24.5% based on a summarized finding of 48 articles from 40 countries (32). Ghrouz et al. (33) found a slightly higher level of anxiety symptoms using the GAD-7 scale (30%) in Indian university students (33). This concordance with the findings of a high prevalence rate of anxiety in Ethiopia and the rest of the world indicates a major global public health problem affecting university attending young adults (32, 33). The anxiety-sleep quality relationship in the present study is supported by previous reports. Poor sleep has been one of the consistent predictors of increased anxiety levels in collegiate young adults (33, 34). Zhang et al. reported that psychological stress mediates the relationship between poor sleep quality and anxiety levels among American nursing students (34). Ghrouz et al. (33) found that poor sleep quality was associated with anxiety in Indian university students (33). A recent systematic review summarized that sleep disturbances may aggravate the severity of anxiety symptoms, and thus, understanding comorbid anxiety and poor sleep may be important for the exploration of treatment strategies (35).
To the best of our knowledge, this is the first study to report a direct association of anxiety status, and anxiety level with inadequate sleep hygiene practices among young adults. However, thematically similar generalizations are entailed in some of the previous reports. Baroni et al. reported that an intervention called sleep course targeted to improve sleep hygiene practices also led to a decrease in anxiety levels in American college students (36). Similarly, Peltz et al. (37) using a moderator-mediator analysis found that (i) sleep hygiene was both directly and indirectly associated with anxiety levels in American adolescents whose school start time is before 8:30 am, and (ii) sleep hygiene was only directly associated with anxiety levels in American adolescents whose school start time was 8:30 am or later (37). A systematic review showed a constellation of poor sleep behaviors like inadequate sleep hygiene, and difficulty in initiating/maintaining sleep are common in children with anxiety disorders (38). Inadequate sleep hygiene practice is common in university students, due to continuous pressure to maintain a higher cumulative grade point average (cGPA), and personal socioeconomic position forcing some of them to work off-campus, all of these adds to their irregular sleeping schedules. Other evidence revealed that an increased co-sleeping tendency in anxious school-going children is found, with one in three children tending to co-sleep 2–4 times a week compared to non-anxious children (39). The use of portable electronic devices by children and adolescents before sleep has been proposed to cause displacement of time to sleep due to increased mental alertness, and psychological stimulation due to light exposure (40). To this end, inadequate sleep hygiene practice is common in university students, thus it is suggested that the universities should have appropriate advisory centers to provide specialized counseling tailored to improve sleep habits, and mental health.
Anxiety and increasing severity of anxiety were associated with psychological stress in the study population. Faravelli and Pallanti reported that distressing events in life lead to the development of anxiety symptoms (41). Perceived exam stress is common in university students with the fear of lower grades. Lower grades may consequently decrease prospects of finding jobs in the future, thoughts about this may increase the level of anxiety. Prolonged stress may impair the ability to perform well-during exams, and in the long-term makes an individual vulnerable to neuropsychiatric complications (42). Other aspects that may potentially increase stress in students are adjustments to the new campus life, fulfilling academic requirements, and simultaneous maintenance of social and academic life.
The study does not have an equal representation of females; nevertheless, the study satisfies the NIH mandate of inclusion of sex as a biological variable for reproducibility and replicability in science (43). Lesser female representation may also be related to the overall lower percentage of female students (about 30%) enrolled at MTU during the academic year. Similar studies involving Ethiopian university students also reported less participation from female students (16). It would be interesting to assess the relationship between courses of study and anxiety symptoms in future studies. Moreover, both regression models used in this study explained 20.4 and 24.1% of the variance. This is most plausibly explained by statistical consideration that some of the covariates associated with anxiety may have not been accounted for in the present study. This aspect should be further explored in future studies. Moreover, a clinical diagnosis of anxiety was not performed. However, it may not be out of place to mention that in the limited resource setting in which this study was performed, a comprehensive clinical neuropsychological assessment was not possible.
The study found a high prevalence of anxiety and psychological anxiety levels in the participating Ethiopian university students. Both the status of anxiety and the increasing severity were associated with higher psychological stress, poor sleep, and inadequate sleep hygiene. Screening of these correlates of anxiety may help in the early identification and management of mental health.
The dataset generated during and/or analyzed during the current study is available in the Supplement File.
The studies involving human participants were reviewed and approved by The Human Institutional Ethics Review Committee, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan. The patients/participants provided their written informed consent to participate in this study.
MM, MS, JM, and BV conceptualized the study, methodology, and were involved in data collection and data curation. MM and MK did the data analysis and wrote and edited the manuscript. AHA, AA, SRP, and AB were involved in supervision. All authors contributed to the article and approved the submitted version.
This research is funded by Vice Deanship of Scientific Research Chairs, King Saud University. The authors extend their appreciation to the Deanship of Scientific Research at Majmaah University for funding this work under Project Number No (R-2021-134).
SRP reports non-financial support from Somnogen Canada Inc. and occasional royalties for the editorial contribution from Springer during the conduct of the study and is an employee of Somnogen Canada Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors are grateful to the Deanship of Scientific Research, King Saud University for funding through Vice Deanship of Scientific Research Chairs. We are grateful to the participants of the study. The authors are grateful to the Deanship of Scientific Research at Majmaah University for funding this work under Project Number No (R-2021-134).
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.677136/full#supplementary-material
GAD, generalized anxiety disorder; PSS-10, perceived stress scale-10; SHI, sleep hygiene index; LSEQ-M, Leeds sleep evaluation questionnaire-Mizan; VAS, visual analog scale.
1. Stein DJ, Scott KM, de Jonge P, Kessler RC. Epidemiology of anxiety disorders: from surveys to nosology and back. Dialogues Clin Neurosci. (2017) 19:127–36. doi: 10.31887/DCNS.2017.19.2/dstein
2. Thibaut F. Anxiety disorders: a review of current literature. Dialogues Clin Neurosci. (2017) 19:87–8. doi: 10.31887/DCNS.2017.19.2/fthibaut
3. Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry. (2002) 63 (Suppl 8):24–34.
4. Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety. (2002) 16:162–71. doi: 10.1002/da.10065
5. Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. (2015) 173:90–6. doi: 10.1016/j.jad.2014.10.054
6. Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. (2019) 16:2735. doi: 10.3390/ijerph16152735
7. Basudan S, Binanzan N, Alhassan A. Depression, anxiety and stress in dental students. Int J Med Educ. (2017) 8:179–86. doi: 10.5116/ijme.5910.b961
8. Mollaoglu M. Trigger factors in migraine patients. J Health Psychol. (2013) 18:984–94. doi: 10.1177/1359105312446773
9. Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
10. Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
11. Anwer S, Alghadir A, Manzar MD, Noohu MM, Salahuddin M, Li H. Psychometric analysis of the sleep hygiene index and correlation with stress and anxiety among saudi university students. Nat Sci Sleep. (2019) 11:325–32. doi: 10.2147/NSS.S222440
12. Rezaei M, Khormali M, Akbarpour S, Sadeghniiat-Hagighi K, Shamsipour M. Sleep quality and its association with psychological distress and sleep hygiene: a cross-sectional study among pre-clinical medical students. Sleep Sci. (2018) 11:274–80. doi: 10.5935/1984-0063.20180043
13. Manzar MD, Noohu MM, Salahuddin M, Nureye D, Albougami A, Spence DW, et al. Insomnia symptoms and their association with anxiety and poor sleep hygiene practices among ethiopian university students. Nat Sci Sleep. (2020) 575–82. doi: 10.2147/NSS.S246994
14. Teshome A, Glagn M, Shegaze M, Tekabe B, Getie A, Assefa G, et al. Generalized anxiety disorder and its associated factors among health care workers fighting COVID-19 in Southern Ethiopia. Psychol Res Behav Manage. (2020) 13:907. doi: 10.2147/PRBM.S282822
15. Kassaw C, Pandey D. The prevalence of general anxiety disorder and its associated factors among women's attending at the perinatal service of Dilla University referral hospital, Dilla town, Ethiopia, April, 2020 in Covid pandemic. Heliyon. (2020) 6:e05593. doi: 10.1016/j.heliyon.2020.e05593
16. Haile YG, Alemu SM, Habtewold TD. Common mental disorder and its association with academic performance among Debre Berhan University students, Ethiopia. Int J Ment Health Syst. (2017) 11:1–1. doi: 10.1186/s13033-017-0142-6
17. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
18. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
19. Alghadir A, Manzar MD, Anwer S, Albougami A, Salahuddin M. Psychometric properties of the generalized anxiety disorder scale among saudi university male students. Neuropsychiatr Dis Treat. (2020) 16:1427–32. doi: 10.2147/NDT.S246526
20. Manzar MD, Alghadir AH, Anwer S, Alqahtani M, Salahuddin M, Addo HA, et al. Psychometric properties of the general anxiety disorders-7 scale using categorical data methods: a study in a sample of university attending ethiopian young adults. Neuropsychiatr Dis Treat. (2021) 17:893. doi: 10.2147/NDT.S295912
21. Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. J Behav Med. (2006) 29:223–7. doi: 10.1007/s10865-006-9047-6
22. Trizano-Hermosilla I, Alvarado JM. Best Alternatives to Cronbach's alpha reliability in realistic conditions: congeneric and asymmetrical measurements. Front Psychol. (2016) 7:769. doi: 10.3389/fpsyg.2016.00769
23. Manzar MD, Salahuddin M, Maru TT, Alghadir A, Anwer S, Bahammam AS, et al. Validation of the adapted Leeds sleep evaluation questionnaire in Ethiopian university students. Health Qual Life Outcomes. (2018) 16:49. doi: 10.1186/s12955-018-0876-0
24. Tarrasch R, Laudon M, Zisapel N. Cross-cultural validation of the Leeds sleep evaluation questionnaire (LSEQ) in insomnia patients. Hum Psychopharmacol. (2003) 18:603–10. doi: 10.1002/hup.534
25. Hameed UA, Al-Jarrah MD, Manzar MD, Nair C, Albougami A, Alrasheadi BA, et al. Leeds sleep evaluation questionnaire in Jordanian university students. A psychometric investigation using comparative confirmatory factor analysis. Saudi Med J. (2020) 41:746–52. doi: 10.15537/smj.2020.7.25146
26. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
27. Manzar MD, Salahuddin M, Peter S, Alghadir A, Anwer S, Bahammam AS, et al. Psychometric properties of the perceived stress scale in Ethiopian university students. BMC Public Health. (2019) 19:41. doi: 10.1186/s12889-018-6310-z
28. Kaczkurkin AN, Moore TM, Ruparel K, Ciric R, Calkins ME, Shinohara RT, et al. Elevated amygdala perfusion mediates developmental sex differences in trait anxiety. Biol Psychiatry. (2016) 80:775–85. doi: 10.1016/j.biopsych.2016.04.021
29. Abu Ruz ME, Al-Akash HY, Jarrah S. Persistent (anxiety and depression) affected academic achievement and absenteeism in nursing students. Open Nurs J. (2018) 12:171–9. doi: 10.2174/1874434601812010171
30. Naz N, Iqbal S, Mahmood A. Stress, anxiety and depression among the dental students of university college of medicine and dentistry Lahore; Pakistan. Pak J Med Health Sci. (2017) 11:1277–81.
31. Nymberg J, Vang Y, Clough N, Masters C. Does daily caffeine intake increase the risk of anxiety? Evid Based Pract. (2018) 21: E2. doi: 10.1097/01.EBP.0000541940.88000.28
32. de Paula W, Breguez GS, Machado EL, Meireles AL. Prevalence of anxiety, depression, and suicidal ideation symptoms among university students: a systematic review. Braz J Health Rev. (2020) 3:8739–56. doi: 10.34119/bjhrv3n4-119
33. Ghrouz AK, Noohu MM, Dilshad Manzar M, Warren Spence D, BaHammam AS, et al. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. (2019) 23:627–34. doi: 10.1007/s11325-019-01780-z
34. Zhang Y, Peters A, Chen G. Perceived stress mediates the associations between sleep quality and symptoms of anxiety and depression among college nursing students. Int J Nurs Educ Scholarsh. (2018) 15:1–9. doi: 10.1515/ijnes-2017-0020
35. Cox RC, Olatunji BO. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. (2016) 37:104–29. doi: 10.1016/j.janxdis.2015.12.001
36. Baroni A, Bruzzese JM, Di Bartolo CA, Ciarleglio A, Shatkin JP. Impact of a sleep course on sleep, mood and anxiety symptoms in college students: a pilot study. J Am Coll Health. (2018) 66:41–50. doi: 10.1080/07448481.2017.1369091
37. Peltz JS, Rogge RD, Connolly H, O'Connor TG. A process-oriented model linking adolescents' sleep hygiene and psychological functioning: the moderating role of school start times. Sleep Health. (2017) 3:465–71. doi: 10.1016/j.sleh.2017.08.003
38. Brown WJ, Wilkerson AK, Boyd SJ, Dewey D, Mesa F, Bunnell BE. A review of sleep disturbance in children and adolescents with anxiety. J Sleep Res. (2018) 27:e12635. doi: 10.1111/jsr.12635
39. Palmer CA, Clementi MA, Meers JM, Alfano CA. Co-sleeping among school-aged anxious and non-anxious children: associations with sleep variability and timing. J Abnorm Child Psychol. (2018) 46:1321–32. doi: 10.1007/s10802-017-0387-1
40. Hale L, Kirschen GW, LeBourgeois MK, Gradisar M, Garrison MM, Montgomery-Downs H, et al. Youth screen media habits and sleep: sleep-friendly screen behavior recommendations for clinicians, educators, and parents. Child Adolesc Psychiatr Clin N Am. (2018) 27:229–45. doi: 10.1016/j.chc.2017.11.014
41. Faravelli C, Pallanti S. Recent life events and panic disorder. Am J Psychiatry. (1989) 146:622–6. doi: 10.1176/ajp.146.5.622
42. Rasheed N. Prolonged stress leads to serious health problems: preventive approaches. Int J Health Sci (Qassim). (2016) 10:V–VI. doi: 10.12816/0031211
43. National Institutes of Health (NIH) (2015). Consideration of Sex as a Biological Variable in NIH-Funded Research. Available online at: https://grants.nih.gov/grants/guide/notice-files/not-od-15-102.html (accessed May 22, 2021).
Keywords: anxiety, perceived stress, sleep quality, sleep hygiene, Leeds sleep evaluation questionnaire
Citation: Manzar MD, Alghadir AH, Khan M, Salahuddin M, Albougami A, Maniago JD, Vasquez BA, Pandi-Perumal SR and Bahammam AS (2021) Anxiety Symptoms Are Associated With Higher Psychological Stress, Poor Sleep, and Inadequate Sleep Hygiene in Collegiate Young Adults—A Cross-Sectional Study. Front. Psychiatry 12:677136. doi: 10.3389/fpsyt.2021.677136
Received: 07 March 2021; Accepted: 05 May 2021;
Published: 01 July 2021.
Edited by:
Rafael Christophe Freire, Queen's University, CanadaReviewed by:
Stephen McNevin, Queens University, CanadaCopyright © 2021 Manzar, Alghadir, Khan, Salahuddin, Albougami, Maniago, Vasquez, Pandi-Perumal and Bahammam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masood Khan, cmFvbWFzb29kMjJAZ21haWwuY29t; bWtoYW40LmNAa3N1LmVkdS5zYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.