- 1Neurology Department of Shenzhen Second People's Hospital, First Affiliated Hospital of Shenzhen University Health Science Center, Shenzhen, China
- 2Spine Department of Shenzhen Second People's Hospital, First Affiliated Hospital of Shenzhen University Health Science Center, Shenzhen, China
Objective: Previous studies suggested that insomnia was associated with an increased risk of cardiocerebral vascular diseases (CVDs) but not clear in different insomnia symptoms. We performed a meta-analysis to investigate the association of individual insomnia symptoms and risk of CVDs.
Methods: In this meta-analysis, we systematically searched published articles by using electronic databases including PubMed, Cochrane Library, MedLine, and Google Scholar. Studies were enrolled if they indicated clear insomnia symptoms, prospective, and evaluated the association of insomnia symptoms and CVD outcome in adults free of CVDs at baseline.
Results: There were seven prospective cohort studies with sample sizes ranging from 2,960 to 487,200 included in this meta-analysis. Mean follow-up duration was 10.6 years. Insomnia symptoms of having difficulty initiating or maintaining sleep (DIS or DMS), non-restorative sleep (NRS), and early morning awakening (EMA) were analyzed in this study. All studies were compared under a random-effects model. NRS, DIS, and DMS were, respectively, related to 16% [hazard ratio (HR) 1.16, 95% CI 1.07–1.24], 22% (HR 1.22, 95% CI 1.06–1.40), and 14% (HR 1.14, 95% CI 1.02–1.27) higher risk of first-ever CVD incidence during the follow-up. Based on our analysis, EMA was not a risk factor of CVDs (HR 1.06, 95% CI 0.99–1.13).
Conclusion: This study suggested that symptoms of DIS, DIM, or NRS were associated with a higher risk of CVD incidence in insomnia patients free of CVDs at baseline. But this association was not significant in insomnia patients complaining about EMA.
Introduction
Insomnia, defined as a person feeling of having difficulty initiating (DIS) or maintaining sleep (DMS) or feeling of non-restorative sleep (NRS), is the most common sleep disorder throughout the world, with an average prevalence of 33% (1–3). As a disease with high prevalence, insomnia could cause a health burden of an annual expenditure of 92.5–107.5 billion dollars years ago (4), which is a critical issue that needs to be solved.
There were about 35.7% of Chinese residents who complained about poor sleep quality in the research of China Chronic Disease and Risk Factor Surveillance (5). Even worse, insomnia has been proven to be associated with several ill health conditions, including hypertension, depression, diabetes, as well as neurological disorders (6–8). In recent years, some prospective studies indicated that insomnia disorder was associated with increased risks of cardiocerebral vascular diseases (CVDs) (9–12). However, the relationship of individual insomnia symptoms and risk of CVDs is still controversial because the inclusion criteria of insomnia patients in the published studies were not consistent.
DIS and DMS were identified as risk factors of CVDs, while early morning awakening (EMA) was associated with an increased risk in the study of Zheng et al. but insignificant in a Swedish cohort (13, 14).
Therefore, the aim of this study was to systematically review related prospective cohort studies and conduct a meta-analysis of all the available studies in order to investigate the association between different insomnia symptoms and the risk of first-ever CVDs.
Methods
Selection of Studies
We systematically searched published articles (through February 24, 2020) by using electronic databases including PubMed, Cochrane Library, MedLine, and Google Scholar. The keywords relating to insomnia as MeSH terms and text words (“Disorders of Initiating and Maintaining Sleep” or “Early Awakening” or “Insomnia” or “Insomnia Disorder” or “sleep complaints” or “sleep disturbance” or “Sleeplessness” or “poor sleep quality”) were used in combination with keywords relating to CVD (“myocardial infarction” or “myocardial ischemia” or “coronary artery disease” or “coronary heart disease” or “Cerebrovascular Accidents” or “stroke” or “cardiovascular disease” or “cardiocerebral vascular disease”). We limited our search to prospective cohort studies, supplemented by manually reviewing the reference of all retrieved papers. There was no language restriction of the studies. The inclusion criteria for the eligible articles were as follows: (1) the study should be prospective cohort or longitudinal cohort with follow-up; (2) patients with age >18 years, free of CVDs at baseline; (3) report specific insomnia symptoms and clear methods of sleep disorder assessment; (4) primary or secondary outcome should be the association of sleep disorder and CVDs; (5) the quantitative estimates of the univariate or multivariate adjusted hazard ratio (HR) and 95% confidence intervals (CIs) for CVD outcomes associated with insomnia symptoms should be provided. Relative risks (RRs) were considered equivalent to HR in the prospective cohort study; (6) the follow-up duration of each study should be longer than 2 years. Any study that did not meet the inclusion criteria was excluded. The articles were initially included or excluded based on title, abstract, and finally based on the complete article, decided by two independent interviewers.
Data Extraction
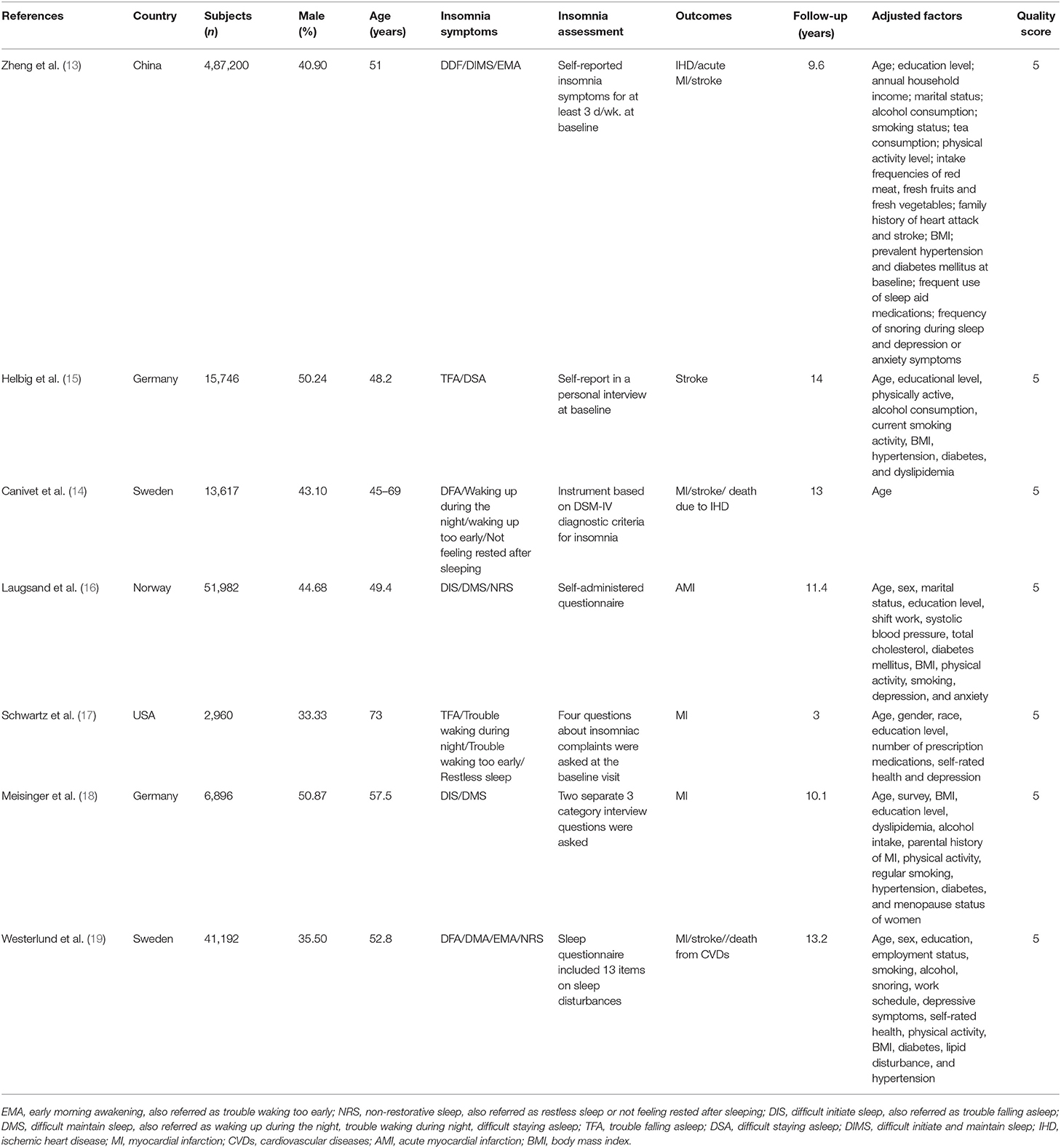
The following data were extracted from the final included studies as the baseline characteristics: first author's name, year of publication, country, number of subjects at baseline, male gender proportion, mean age at baseline, insomnia symptoms of subjects, methods of insomnia disorder assessment, study outcome, follow-up duration, variables adjusted for confounding factors at the univariate or multivariate model. We also extracted HR and 95% CIs for CVD outcomes associated with insomnia symptoms for the statistical analysis.
Statistical Analysis
The HR we used for analysis was from the most complete adjustment for confounders in the original study (adjusted confounders were shown in Table 1). All analyses used random-effects models, with heterogeneity assessed using the I2 statistic. Heterogeneity across studies was considered substantial if I2 > 50%. In order to identify the source of heterogeneity, we performed sensitivity analyses by eliminating each included study step by step and a subgroup analysis according to gender. Publication bias was evaluated by means of the Egger's test. We performed the statistical analysis by STATA version 15 (StataCorp LLC, College Station, Texas, USA), and statistical significance was considered when a two-tailed p < 0.05.
Results
Study Identification and Selection
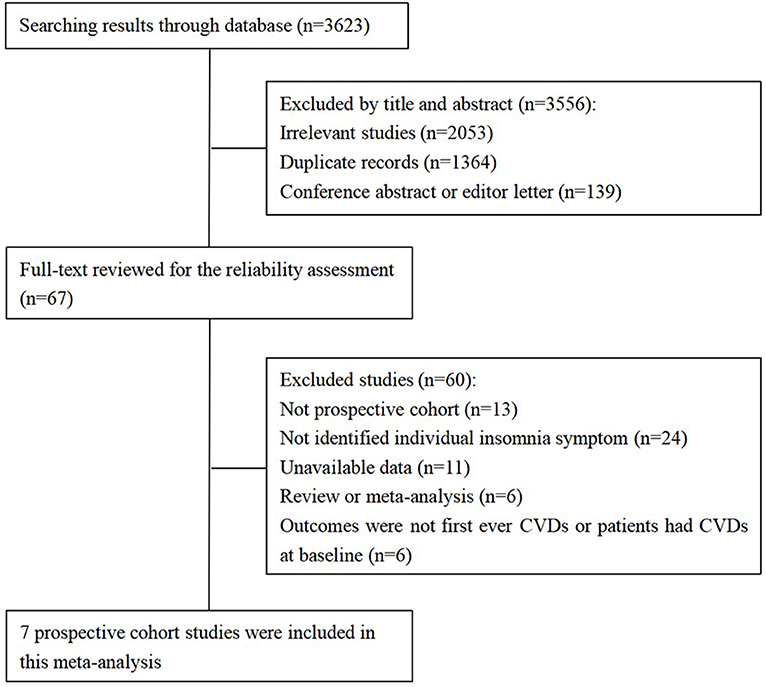
Based on our search strategy, there were a total of 3,623 records identified through the databases. We excluded 3,556 articles by title and abstract and then reviewed the full text to further exclude 60 studies according to the inclusion criteria of our study (follow chart shown in Figure 1).
Finally, there were seven prospective cohort studies included in this meta-analysis (13–19). Of these, there were three studies that separately analyzed the association between CVD outcome and different insomnia symptoms according to males and females, which means that they analyzed two outcomes in the same study. Therefore, we entered each of them as a single paper for the statistical analysis; as a result, there were 10 studies enrolled in the final analysis.
The entered articles included studies from China, USA, Germany, Norway, and Sweden, with sample sizes ranging from 2,960 to 487,200. The mean follow-up duration of this cohort was 10.6 years. As for the assessment of insomnia symptoms, two of the studies used the dichotomous variable (yes or no) (13, 15) while others used three to four category choices [(14, 16–19); e.g., never, occasionally, often, almost every night], in which cases we used the most serious category as the presence of insomnia symptoms based on the same criteria of the original articles. We evaluated the quality of these cohort studies by Newcastle–Ottawa Scale (NOS) (details shown in Table 1).
Insomnia Symptoms and Cardiocerebral Vascular Outcomes
After pooling all 10 studies' comparisons under a random-effects model, which were divided by different insomnia symptoms, the meta-analysis showed patients with NRS was in 16% higher risk of CVDs compared to those without corresponding symptoms (HR 1.16, 95% CI 1.07–1.24). Subjects who complained DIS and DMS had 22 and 14% increased risk of suffering CVDs, respectively, with respect to those without these two complaints (DIS: HR 1.22, 95% CI 1.06–1.40; DMS: HR 1.14, 95% CI 1.02–1.27). The association of EMA symptom and CVD incidence risk was not significant in data analysis (Figure 2). Overall, different insomnia symptoms were significantly associated with a 13% higher risk of suffering CVDs compared to subjects without any insomnia complaint (HR 1.13, 95% CI 1.08–1.19). There was no significant heterogeneity across the study of EMA and NRS, but a borderline heterogeneity was shown across the study of DIS and DMS. The overall heterogeneity was also significant with I2 = 56.8% (p < 0.001).
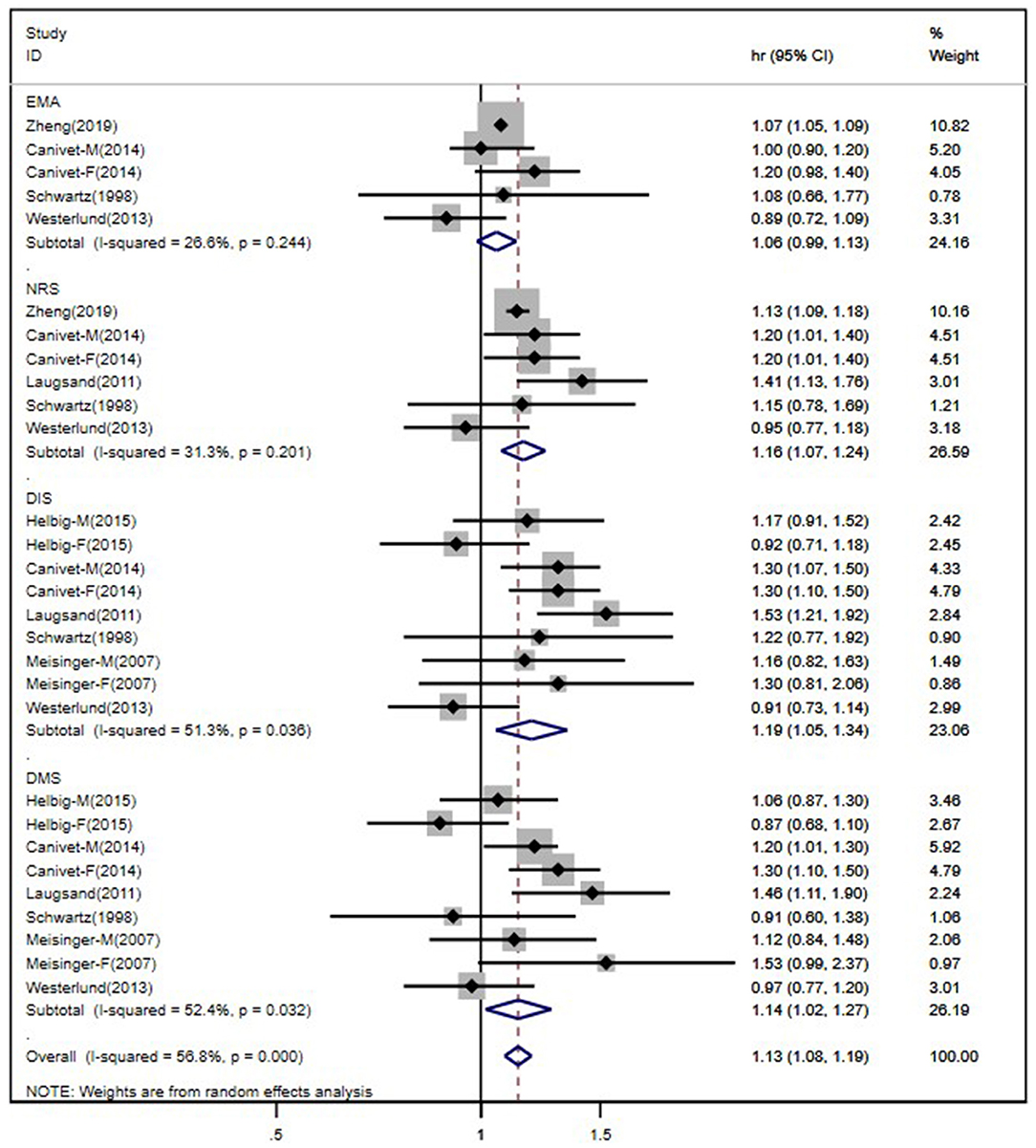
Figure 2. Forest plot of studies evaluating the association of individual insomnia symptoms and risk of cardiocerebral vascular disease.
Sensitivity Analyses and Publication Bias
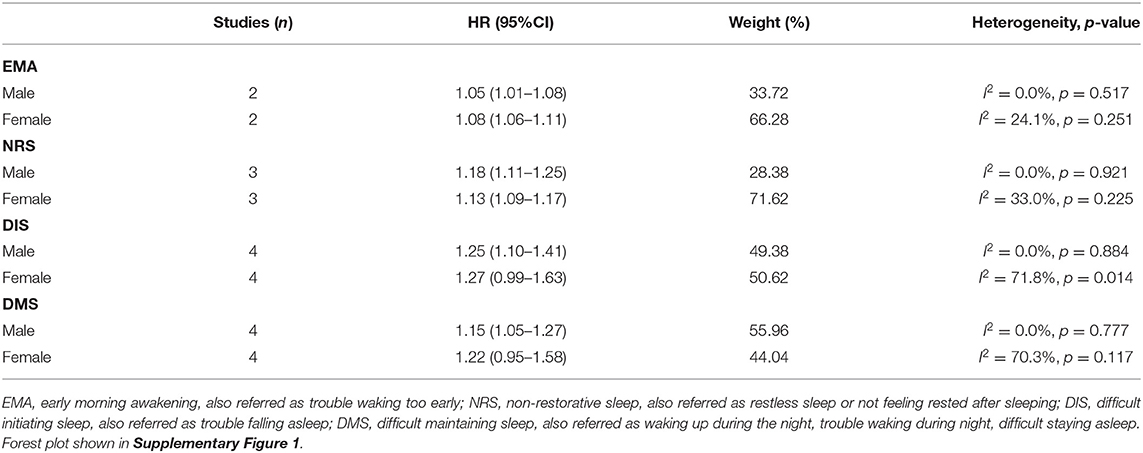
As we had mentioned above, studies of patients with DIS and DMS symptoms reported borderline significant heterogeneity. Actually, according to our search strategy, the study of Eaker et al. (20) was also included at the beginning, but in our primary data analysis, the heterogeneity was much higher in the DIS studies (I2 = 62.5%, p = 0.04; after being excluded, I2 = 51.3%, p = 0.036). Therefore, we did not include this study in our final analysis. In order to figure out other possible difference across the studies, we performed a subgroup study based on gender for the sensitivity analysis. Since not all included studies had separate HR and 95% CI for CVDs and insomnia symptoms according to male and female, we only use the available data. The subgroup analysis based on the available studies showed that females with DIS and DMS symptoms reported much higher heterogeneity compared to males (Table 2). Egger's test was used to assess the publication bias of this study, which showed no significant results (p = 0.097).
Discussion
Insomnia is the most common sleep disturbance globally, which can cause both mental and physical illness. Previous studies have indicated insomnia disorder as a new risk factor of CVDs, other than the traditional atherosclerotic risk factors. However, insomnia patients may complain about different symptoms, including difficulty falling asleep, difficulty maintaining asleep, waking up too early in the morning, and feeling restless after one-night sleep. Patients might have all or just some of these symptoms. It is not clear if all these symptoms had the same association with CVD incidence risk. As a result, this meta-analysis aimed to investigate the relationship between each insomnia symptom and the risk of first-ever CVDs.
Our meta-analysis showed an overall increased risk of CVDs in patients with insomnia symptoms, which was consistent with findings of previous studies. Patients with complaints of DIS (HR 1.22, 95% CI 1.06–1.40), DIM (HR 1.14, 95% CI 1.02–1.27), or NRS (HR 1.16, 95% CI 1.07–1.24) were in higher risk of CVDs individually in this study. Our data indicated that insomnia patients complaining of DIS had much higher risk of CVD than other insomnia symptoms, which was consistent with previous literature. Zheng et al. (13) combined DIS and DMS as one insomnia symptom (DIMS) in a prospective cohort study of 487,200 Chinese adults. The results showed that DIMS was associated with both ischemic heart disease and ischemic stroke but not hemorrhagic stroke (13). Moreover, DIS or NRS was found to be related to 55 or 32% increased risk of CVD mortality, respectively, among 23,447 US men (21). DIS and DMS were related to a higher risk of total strokes (fatal and non-fatal) at first, but this relationship became insignificant after adjusting for age and other risk factors of stroke in the population-based MONICA/KORA Augsburg Cohort Study (15). Our study did not detect a significantly increased risk of CVDs in insomnia patients with EMA symptom. EMA was related to a slight increase in CVD incidence in the study of China Kadoorie Biobank (HR 1.07, 95% CI 1.05–1.09) (13), while the relationship was remarkable neither in male nor female within a Swedish cohort, which consisted of 13,617 subjects ages 45–64 without CVDs at baseline (14).
The mechanisms of increased risk of CVDs in patients with insomnia symptoms are still unclear. The elevated sympathetic and hypothalamic–pituitary–adrenal axis activity is one of the possible mechanisms (22). DIS and DMS in insomnia patients could induce overall short sleep duration, which was proven to be associated with hypercortisolemia and increased catecholaminergic and autonomic activity, resulting in increased blood pressure and impaired glucose metabolism (23–26). High risk of genotype might be another contributing mechanism (27). Furthermore, an experimental study indicated that insomnia disorder could cause abnormal circulating levels of growth hormone, leptin, and ghrelin in younger adults, aggravating the risk of obesity in this population (28). All these factors can lead to an increased risk of CVD incidence.
Limitations
There were several limitations in the present meta-analysis. Firstly, the insomnia symptoms of enrolled studies were assessed by self-reported questionnaires or interviews. This may lead to a possible higher risk of selection bias due to the interviewers as well as recall and report bias caused by the participants. Some objective instrument (e.g., polysomnography) could be used in future investigations, but the medical expense is still an unsolved problem. Secondly, since we only included studies with clear insomnia symptoms instead of a general conception, this led to the limited number of entered articles compared to previous reviews. However, with the acceptable quality score and large scale of each cohort study and the result of different associations between individual insomnia symptom and CVD risk, our meta-analysis still provided a remarkable reference for future research. Additionally, we could not enter all the included studies in the sensitivity analysis because not all studies provided the separate HR and 95% CI according to male and female. But the primary results showed that there were much more higher heterogeneity across the female subgroup in all insomnia symptoms, especially for DIS and DMS, which showed borderline heterogeneity in the overall analysis. Therefore, female was accepted as the possible origin of heterogeneity and needs to be further investigated in a future study of CVD incidence risk in insomnia patients with different symptoms.
Conclusions
In conclusion, this meta-analysis indicated that symptoms of DIS, DIM, or NRS were associated with a higher risk of CVD incidence in insomnia patients free of CVDs at baseline. But this association was not significant in insomnia patients complaining of EMA.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
LR and YW conceived and designed the study. TL and SH independently extracted data from the eligible studies and any argument was resolved either by discussion or by involving YW when necessary. SH performed the paper writing with the assistance of TL. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Scientific Research Items of Shenzhen Science and Technology Innovation Committee (Nos. SGLH20180628161804465 and KJYY20180703165202011) and clinical research projects of Shenzhen Second People's Hospital (No. 20203357015).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.654719/full#supplementary-material
References
1. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. (2014) 146:1387–94. doi: 10.1378/chest.14-0970
2. Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: classification and criteria changes. World Psychiatry. (2013) 12:92–8. doi: 10.1002/wps.20050
3. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. (2002) 6:97–111. doi: 10.1053/smrv.2002.0186
5. Yin ZMP, Li Y, Jiang Y, Wang L, Zhao W. A study on risk factors for poor sleep quality among Chinese residents aged 15-69 years [in Chinese]. Hin J Prev Contr Chron Dis. (2011) 19:2.
6. Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. (2012) 21:427–33. doi: 10.1111/j.1365-2869.2011.00990.x
7. Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. (2007) 3:6.
8. Troxel WM, Buysse DJ, Matthews KA, Kip KE, Strollo PJ, Hall M, et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep. (2010) 33:1633–40. doi: 10.1093/sleep/33.12.1633
9. Ramar K, Surani S. The relationship between sleep disorders and stroke. Postgrad Med. (2015) 122:145–53. doi: 10.3810/pgm.2010.11.2232
10. Hsu C-Y, Chen Y-T, Chen M-H, Huang C-C, Chiang C-H, Huang P-H, et al. The association between insomnia and increased future cardiovascular events. Psychosomatic Med. (2015) 77:743–51. doi: 10.1097/PSY.0000000000000199
11. Elwood P. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Commun Health. (2006) 60:69–73. doi: 10.1136/jech.2005.039057
12. Tikhomirova OV, Kozhevnikova VV, Zybina NN, Startseva ON, Bobko OV. A role of insomnia in the development of silent cerebral infarctions. Zhurnal nevrologii i psikhiatrii im. S.S. Korsakova. (2018) 118:3. doi: 10.17116/jnevro20181180923
13. Zheng B, Yu C, Lv J, Guo Y, Bian Z, Zhou M, et al. Insomnia symptoms and risk of cardiovascular diseases among 0.5 million adults: a 10-year cohort. Neurology. (2019) 93:e2110–20. doi: 10.1212/WNL.0000000000008581
14. Canivet C, Nilsson PM, Lindeberg SI, Karasek R, Östergren PO. Insomnia increases risk for cardiovascular events in women and in men with low socioeconomic status: a longitudinal, register-based study. J Psychosomatic Res. (2014) 76:292–9. doi: 10.1016/j.jpsychores.2014.02.001
15. Helbig AK, Stöckl D, Heier M, Ladwig KH, Meisinger C. Symptoms of insomnia and sleep duration and their association with incident strokes: findings from the population-based MONICA KORA Augsburg Cohort Study. PLoS ONE. (2015) 10:e0134480. doi: 10.1371/journal.pone.0134480
16. Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. (2011) 124:2073–81. doi: 10.1161/CIRCULATIONAHA.111.025858
17. Schwartz SW, Cornoni-Huntley J, Cole SR, Hays JC, Blazer DG, Schocken DD. Are sleep complaints an independent risk factor for myocardial infarction? AEP. (1998) 8:9. doi: 10.1016/S1047-2797(97)00238-X
18. Meisinger C, Heier M, Löwel H, Schneider A, Döring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA KORA Augsburg Cohort Study. Sleep. (2007) 30:7. doi: 10.1093/sleep/30.9.1121
19. Westerlund A, Bellocco R, Sundström J, Adami H-O, Åkerstedt T, Trolle Lagerros Y. Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur J Epidemiol. (2013) 28:463–73. doi: 10.1007/s10654-013-9802-2
20. Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol. (1992) 135:854–64. doi: 10.1093/oxfordjournals.aje.a116381
21. Li Y, Zhang X, Winkelman JW, Redline S, Hu FB, Stampfer M, et al. Association between insomnia symptoms and mortality: a prospective study of U.S. men. Circulation. (2014) 129:737–46. doi: 10.1161/CIRCULATIONAHA.113.004500
22. Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. (2009) 32:491–7. doi: 10.1093/sleep/32.4.491
23. Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci USA. (2008) 105:1044–9. doi: 10.1073/pnas.0706446105
24. Silvani A. Sleep disorders, nocturnal blood pressure, and cardiovascular risk: A translational perspective. Auton Neurosci. (2019) 218:31–42. doi: 10.1016/j.autneu.2019.02.006
25. Sivertsen B, Lallukka T, Salo P, Pallesen S, Hysing M, Krokstad S, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. (2014) 23:124–32. doi: 10.1111/jsr.12102
26. Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. (2008) 1129:287–304. doi: 10.1196/annals.1417.033
27. Said MA, Verweij N, van der Harst P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank Study. JAMA Cardiol. (2018) 3:693–702. doi: 10.1001/jamacardio.2018.1717
Keywords: insomnia, symptom, cardiovascular disease, stroke, meta-analysis
Citation: Hu S, Lan T, Wang Y and Ren L (2021) Individual Insomnia Symptom and Increased Hazard Risk of Cardiocerebral Vascular Diseases: A Meta-Analysis. Front. Psychiatry 12:654719. doi: 10.3389/fpsyt.2021.654719
Received: 17 January 2021; Accepted: 25 March 2021;
Published: 14 May 2021.
Edited by:
Masoud Tahmasian, Shahid Beheshti University, IranReviewed by:
Nader Salari, Kermanshah University of Medical Sciences, IranNava Zisapel, Tel Aviv University, Israel
Copyright © 2021 Hu, Lan, Wang and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lijie Ren, MTM2MzE2MDU5NjZAMTI2LmNvbQ==; Yang Wang, aGVsZW53eTE5NzhAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Shiyu Hu1†
Shiyu Hu1† Tao Lan
Tao Lan Lijie Ren
Lijie Ren