
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 08 April 2021
Sec. Schizophrenia
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.640921
This article is part of the Research Topic Thinking through the Schizophrenia Spectrum: Nosological Scenarios and Perspectives beyond Psychosis View all 9 articles
Background: Formal thought disorder was constitutively linked to the original concept of schizophrenia and has since been one of central features supporting its diagnosis. Bleuler considered formal thought disorder as a fundamental symptom of schizophrenia among other fundamental symptoms, including ego disorders. The contemporary concept of self-disorder represents a more developed, nuanced, and systematic approach to disturbances of self-experience than the Bleulerian concept of ego disorders. As fundamental symptoms, on Bleuler's account, are persistently present in every case, an association between these symptoms could be expected. The purpose of this study was to examine the association between self-disorder and formal thought disorder.
Methods: A sample of 94 diagnostically heterogeneous patients was examined for formal thought disorder using clinical rating and a proverb test. The proverb test was analyzed for two different aspects of formal thought disorder: literal responses and bizarre responses. The sample was comprehensively assessed for psychopathology, including self-disorder as measured with the Examination of Anomalous Self-Experience scale.
Results: The patients, who provided bizarre responses, had a higher level of self-disorder, more negative symptoms, lower level of social functioning, and lower level of intelligence. Bizarre answers aggregated in patients diagnosed within the schizophrenia spectrum compared with patients outside the schizophrenia spectrum. We found moderate correlations between the two measures of formal thought disorder (clinically rated and bizarre responses) and self-disorder (0.454 [p < 0.01] and 0.328 [p < 0.01]). Literal responses did not differ between diagnostic groups and also did not correlate with bizarre responses. Specificity of bizarre responses for a diagnosis within schizophrenia spectrum was 86.89%, whereas sensitivity was 40.85%.
Conclusion: The close relation between formal thought disorder and self-disorder further adds to the notion of self-disorder as a unifying psychopathological core beneath the apparently heterogeneous symptoms of schizophrenia.
Formal thought disorder was constitutive for the creation of the concept of schizophrenia. Kraepelin (1) used the term “Zerfahrenheit,” which is sometimes translated into “incoherence,” but which also refers to more subtle distortions of meaning in the patient's speech (2). Bleuler also used this term, but he introduced the general notion of “loosening of associations” as a fundamental symptom of schizophrenia (3). On his account, the fundamental symptoms were specific for the diagnosis of schizophrenia. Formal thought disorder has been subsequently included in most definitions of schizophrenia, although with permutations of its characteristic features and severity. Importantly, the notion of formal thought disorder must be distinguished from the broad Anglo-Saxon concept of “thought disorder.” The latter term is more inclusive and refers to a variety of disturbance of thought, including disorders of thought content such as delusions.
In current literature, it is frequent to use the term “speech disorder.” Obviously, we only have access to the patients' thought processes through their expressions, in speech, writing, or behavior [e.g., “unsinnige Handlungen” (4, 5)]. Formal thought disorder refers to disturbances in the structure (or form) of thinking, e.g., the boundaries of concept formation, semantic disturbances (such as neologisms), or disturbances in the transitions between thought segments (6, 7). Although formal thought disorder is expressed through the patient's speech, it is often difficult to detect disorder of thinking, if the patient's responses are brief or laconic or in interviews with a high degree of structure. It is a well-established clinical observation that the more structured the conversation is, the less prominent the manifestation of the patient's formal thought disorder will be (6). Thus, there are basically two approaches to detect and measure formal thought disorder. One, used in all clinical assessments, is simply the rating of disorder manifest in the patient's speech. Nancy Andreasen has published a detailed scale of “thought, language, and communication disorder” (8) that can be used for this approach. Another approach is based in the tradition of psychological projective tests such as object sorting test or Rorschach (e.g., Holzman's Thought Disorder Index) (9). Another possible test, which is one we also used in the current study, is the proverb test in which the patient is presented with a number of different proverbs, which he then must explain the meaning of (see below) (10).
Studies of formal thought disorder have shown that formal thought disorder may be considered a marker of illness severity. Basic demographics do not seem to be related to the presence of formal thought disorder, whereas the level of intelligence has been related to bizarre thinking. Studies examining the association between social functioning and formal thought disorder have shown ambiguous results (7, 11).
As already mentioned, Bleuler considered formal thought disorder as a fundamental symptom of schizophrenia related to other fundamental symptoms such as ego disorders. However, in modern literature, the relationship between disturbances of self-experience and formal thought disorder has not been probably explored except from theoretical suggestions (12, 13). [For details of self-disorder, see, e.g., (14, 15)]. In the current study, we were interested in the following questions:
1) How is self-disorder as measured by the Examination of Anomalous Self-Experience (EASE) (16) related to clinically rated formal thought disorder and formal thought disorder rated through proverb test?
2) How is formal thought disorder related to other canonical dimensions of schizophrenia (positive and negative symptoms) as well as to social functioning?
The original sample comprised the first 100 admissions, diagnostically heterogeneous patients aged between 18 and 65 years. The sample comprised the consecutive first admissions to the Psychiatric Center Hvidovre (a psychiatric inpatient facility of the University of Copenhagen) that provides psychiatric service to a population of 150,000 in one particular catchment area of the City of Copenhagen (there are no private inpatient psychiatric facilities in Denmark). The patients were included over a period of 18 months independently of their clinical diagnosis at admission. All consecutive first admissions were screened for eligibility. If there were more eligible patients than it was possible to examine within the pragmatic constraints of the project, the youngest patient was always selected. The patients participated on the condition of informed consent, and a relevant medical ethical committee approved the study.
The patients had to be in a condition in which they could tolerate a lengthy interview, because one of the goals of the primary study was to assess the adequacy of different psychopathological interviews (17). This led to exclusion of aggressive, agitated, or severely psychotic patients, who were not able to collaborate. Additional exclusion criteria comprised primary or clinically dominating substance use, history of brain injury, and organic brain disorder. Involuntarily admitted or legal patients were also excluded. Moreover, all participants had to have an intelligence level within the normal range as measured by the Intelligenz-Struktur Test 2000 R (18). All patients were asked to do a proverb test, but four patients declined. After inclusion in the project, two patients later withdrew their consent to the research project. Thus, a total of 94 patients took the proverb test.
Formal thought disorder was assessed using a proverb test consisting of 11 proverbs. The test was chosen as it is easy to administer, not too time consuming, and it is a commonly used test for rating bizarre responses (19, 20). We analyzed the proverbs for (1) literalness and (2) bizarreness, as these are two commonly agreed aspects of formal thought disorder (21). For literalness, we followed the scoring manual by Hertler et al. (22). Based on selected keywords in the proverbs, it was assessed whether these keywords were attributed literalness. We only looked for presence or absence of literalness. To illustrate the test: the proverb “a thief believes everybody steals” means that one ascribes to others one's own flawed or weak mindset or habit. Here are two examples of responses that were rated for literalness: “if you yourself are a thief, you assume that all people are thieves too,” and “people who break the law believe that it is normal.”
For rating bizarreness, we constructed a simple scoring system for bizarre answers inspired by Exner's comprehensive system for scoring the Rorschach (23), more specifically, the DV (Deviant Response) score. Again, we only looked for presence or absence of bizarre response. We rated answers as bizarre; if they were idiosyncratic; if the rater was unable, or found it difficult, to grasp the meaning of the answer; or if there was a private use of terms or expressions in which the meaning may be clear, but the expression itself is unusual. The rating was done jointly and based on clinical judgment in the same way as one would approach the scoring of DV in a Rorschach protocol. Here are a few examples of responses, which we rated bizarre in the present sample: Asked to explain the meaning of the proverb “don't cry over spilt milk,” which means that there is no reason to get upset over something that have already occurred and that cannot be changed, one patient responded, “One should not get upset. To have courage or to get courage.” Another example, asked to explain the meaning the proverb “many a mickle makes a muckle,” which means that lots of small amounts can be accumulated to large amount, one patient responded, “that means that you have to stay young.”
All ratings of formal thought disorder (i.e., literal and bizarre responses to the proverbs) were done by two psychologists (MBP and MGJ), both of which have vast clinical experience and extensive training and experience with the use of the Rorschach test. Both raters were blinded to diagnosis, any kind of psychopathological information, and level of functioning of the patients.
All patients were thoroughly assessed for psychopathology and diagnosed by JN and JP. The interviews were split over two to three sessions, and the total duration of the interviews was 3–6 h. The interview was carried out by an experienced psychiatrist and expert in the use and teaching of the EASE (16) (JN). The interviews were conducted in a semistructured, conversational style, including a thorough psychosocial history, a description of the illness evolution, the Operational Criteria Checklist (OPCRIT) (24) expanded with additional items from the Schedule for Affective Disorders and Schizophrenia (SADS) (25), the Examination of Anomalous Self-Experiences (EASE) (16), the perceptual section from the Bonn Scale for the Assessment of Basic Symptoms (BSABS) (26), and of abnormal expressive features (27). The proverb test was administered after completed interviews. All interviews were videotaped.
The present study used lifetime International Classification of Diseases, 10th Revision (ICD-10) diagnoses based on all available, diagnostically relevant information (interview videos, notes, information from the hospital charts, which also contained second informant descriptions of the illness' symptoms and their evolution). Self-disorder was assessed using the EASE and rated on a lifetime basis as present or absent. We constructed a “positive symptom scale” (including psychotic symptoms) and a “negative symptom scale” (including negative symptoms) by adding items selected from the interview schedule in order to obtain the measures of the canonical dimensions of schizophrenic symptomatology. Table 1 shows the composition and Cronbach α's of the positive and negative symptoms scales in addition to a scale of items targeting clinically rated formal thought disorder.
The variable “social and professional difficulties” was created by summing two items from the interview checklist: “social difficulties” (which covered difficulties in personal relationships as measured by <2 close relations) and “professional difficulties” (which covered difficulties in maintaining jobs or education within the last year); maximal score was 2.
All patients participated upon written consent. The study was approved by the Danish Data Protection Agency. According to Danish legislation, approval from The Danish National Committee on Health Research Ethics is not required for interview studies of this kind. The study adhered to the ethical principles laid down by the Helsinki Declaration.
We analyzed the sample divided into two groups: one group, consisting of patients who provided at least one bizarre response, and another group of patients, who did not provide any bizarre response.
Subsequently, we did some extra analyses with the sample divided into two diagnostic groups: schizophrenia spectrum disorders (i.e., schizophrenia, other non-affective psychoses, and schizotypy) and non-schizophrenia spectrum disorders (including bipolar disorder, major depression, personality disorder, anxiety, and adjustment disorder).
We tested for equality of means by t test when normally distributed and Mann–Whitney U test when not. Correlations were tested with Spearman ρ. For these analyses, we used SPSS version 26. Specificity and sensitivity were calculated using Medcalc's diagnostic test calculator (28).
Table 2 shows that the number of patients with literal responses did not differ between the two groups (bizarre responses vs. no bizarre responses). When dividing the sample into two groups depending on diagnosis, i.e., schizophrenia spectrum disorders vs. all other disorders, we found no significant differences between the groups for literal responses. Looking at the whole sample, we did not find any significant correlation between self-disorder and literal responses to the proverbs.
Table 2 shows significant differences between the group with bizarre responses and the group with no bizarre responses in regard to self-disorder, negative symptoms, clinically rated formal thought disorder, social and professional difficulties, and level of intelligence. We tested if intelligence was a mediating factor for the effect of self-disorder on bizarre responses by linear regression and found that it was not. Self-disorder and level of intelligence were independently contributing to bizarre responses.
The correlations between bizarre responses and other variables are displayed in Table 3. The correlation between self-disorder (mean EASE score) and bizarre responses was moderate (ρ = 0.328, p < 0.01). Bizarre responses significantly aggregated in the schizophrenia spectrum disorders group.
At the bottom of Table 2, it can be seen that 29 of 71 patients within the schizophrenia spectrum gave at least one bizarre response to the proverbs. By contrast, only three patients with a diagnosis outside the schizophrenia spectrum gave a bizarre response.
Finally, we found that the specificity of bizarre responses for schizophrenia spectrum diagnoses was 86.89%, whereas the sensitivity was 40.85% (Table 4).
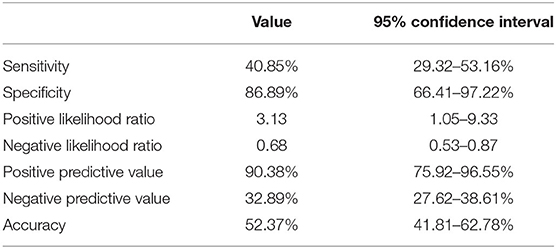
Table 4. Diagnostic sensitivity and specificity of bizarre responses for a schizophrenia spectrum disorder.
This is the first study to systematically examine the relation between formal thought disorder and self-disorder. We found a highly significant, moderate correlation between bizarre responses and self-disorder. The correlation between bizarre answers and negative symptoms as well as clinically rated formal thought disorder was significant, whereas the correlation between bizarre answers and positive symptoms was not. Moreover, we found significantly more difficulties in social and occupational functioning in the group of patients who had given a bizarre response. These findings point to bizarre responses tapping into something central for schizophrenia spectrum disorders (i.e., schizophrenia, other non-affective psychoses, and schizotypy).
Literal responses did not relate significantly with any of the examined variables and did not differ between the diagnostic groups. Literal and bizarre responses did not correlate with each other and appear to reflect different dimensions. These findings are in line with previous studies, which have shown that the formal thought disorder of idiosyncratic verbalizations, autistic logic, and absurd thinking are more characteristic of schizophrenia (9, 29–31).
The specificity of bizarre answers for a diagnosis within schizophrenia spectrum disorders was high, suggesting that the presence of formal thought disorder should prompt clinicians to suspect or at least examine if the patient may fulfill the criteria for a schizophrenia spectrum disorder. Conversely, the absence of formal thought disorder cannot rule out schizophrenia spectrum disorders, as a considerable proportion of these patients did not offer bizarre responses. However, it should be emphasized that these figures should be taken with caution because the confidence intervals in Table 4 vary considerably, and schizophrenia spectrum diagnoses are partly dependent on the presence of formal thought disorder.
From a theoretical point of view, the association between expressive features (formal thought disorder) and subjective experiences (e.g., self-disorder) is perhaps not so surprising. In general, formal thought disorders are typically conceived as a disturbance in the individual's capacity of producing and expressing thoughts in terms of semantics or relations between semantic units. Alternatively, formal thought disorder can be seen as the individual's ability to draw upon the intersubjective resources that help structure our thinking and expression (note that these two views are not mutually exclusive). In the latter view, we have to distinguish, in the terms of Merleau-Ponty, between “le langue” and “la parole” (32). The former is a historically and socially determining intersubjective matrix that dictates or influences our conceptual/cognitive abilities. “Le langue” is this matrix, whereas “la parole” is the individual's thinking and speech. In Merleau-Ponty's view, cognition is therefore heavily dependent on perception and embodied interaction in the social world, in agreement with earlier views of Vygotski (33). In the case of schizophrenia, it has repeatedly been emphasized that consciousness here entails a sort of disintegration. Kraepelin considered the disintegration as a product of weakened center of self-consciousness (Ich-Bewusstsein) (34). Famously, Bleuler introduced the concept of “loosening of associations” as an instance of a general tendency of splitting (Spaltung). Unfortunately, Bleuler's view was often understood as a sort of mechanical deficit in associative mechanisms. Bleuler himself, however, saw this splitting as a lack of hierarchy in the goal-directedness or intentionality. As an example of this intentionality, he mentions a peasant, whose overarching goal is to maximize the productivity of his land. Other activities such as sowing or plowing are subordinate activities to his primary goal. The peasant may do other things such as eating or sleeping, but the overarching goal is always tacitly present in his mind and structures his behavior. Thus, Bleuler saw the splitting and loosening of associations as an expression of diminished intentional directedness of consciousness. He ascribed this deficiency to a disorder of the ego and its activity (3). In the psychoanalytic literature of ego psychology, disorder of thinking was also considered as an expression of the pathology of the self (35).
Viewed from the perspective of the EASE-based self-disorder research, we can point to the following aspects of the link between self-disorder and formal thought disorder. First, self-disorder implies a weakened intersubjective attachment (a disorder of “common sense”), a tendency to solipsistic experiences and generally unstable self-awareness leading to a confusion between modalities of intentionality (14, 16, 36). Self-disorder may also imply a range of preverbal experiences, which may be quite unique and unusual and create a difficulty for conceptualization and verbalization, perhaps prompting the patient to use private or idiosyncratic formulations to articulate prereflectively altered self-experience. Finally, patients with schizophrenia spectrum disorder often seem to exist in different and sometimes competing ontological frameworks, one reflecting our natural attitude and one more private where the laws of causality and non-contradiction do not exist (37–39).
In this study, we approached the issue of self-disorder from a different perspective than that of diagnoses, as the purpose was to explore the association between formal thought disorder and self-disorder. Our findings seem to converge around central phenomena of schizophrenia spectrum disorders, including self-disorder. From our own and others' studies, we know that self-disorder constitutes a trait phenomenon that is present before the full symptomatology of schizophrenia manifests (40–44), suggesting that self-disorder constitutes a basic framework within which the heterogeneous symptoms associated with schizophrenia may be unified and to some extent understood.
In the diagnostic systems of ICD-10 and Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, formal thought disorder is defined at a quite severe level; perhaps leading to more subtle manifestations of formal thought disorder tends to be overlooked. Our findings point to the importance of paying close attention to potential formal thought disorder in the clinical encounter. Additionally, clinicians must be aware that interviews with a high degree of structure can impede formal thought disorder from materializing, and obviously assessments using self-rating scales do not allow for tracking formal thought disorder.
The major limitation to the study is the relatively small sample size. However, studies with such comprehensive assessment of psychopathology are very time consuming, making it difficult to obtain larger samples. Moreover, it should be mentioned that the translation of formally disturbed responses from Danish to English has built-in difficulties, and it is likely that some of the disturbed answers have lost some relevant aspects in the translation.
The datasets generated for this article are not readily available because it contains sensitive personal information. Requests to access the datasets should be directed to SnVsaWVfbm9yZGdhYXJkQGRhZGxuZXQuZGs=.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
JN and JP designed the study and JN collected the data. MG-J and MB-P did the analyses. JN wrote the first draft of the manuscript. All authors contributed to the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
2. Sass H. Phenomenological Aspects on “Zerfahrenheit” and Incohrence. In: Sptitzer M, Uehlein F, Schwartsz M, Mundt C, editors. Phenomenology, Language and Schizophrenia. New York, NY: Springer (1992). p. 147–59. doi: 10.1007/978-1-4613-9329-0_10
3. Bleuler E. Dementia Praecox or the Group of Schizophrenias. New York, NY: International Universities Press (1950).
4. Minkowski E. La schizophrénie. Psychopathologie des schizoïdes et des schizophrenes. Paris: Payot (1927).
5. Conrad K. Die beginnende Schizophrenie. Versuch einer Gestaltanalyse des Wahns. Bonn: Das Narrenschiff im Psychiatrie-Verlag (2002).
6. Jansson L, Nordgaard J. The Psychiatric Interview for Differential Diagnosis. Switzerland: Springer (2016). doi: 10.1007/978-3-319-33249-9
7. Hart M, Lewine RR. Rethinking thought disorder. Schizophr Bull. (2017) 43:514–22. doi: 10.1093/schbul/sbx003
8. Andreasen NC. Scale for the assessment of thought, language, and communication (TLC). Schizophr Bull. (1986) 12:473–82. doi: 10.1093/schbul/12.3.473
9. Holzman PS, Shenton ME, Solovay MR. Quality of thought disorder in differential diagnosis. Schizophr Bull. (1986) 12:360–71. doi: 10.1093/schbul/12.3.360
10. Benjamin JD. A Method for Distinguishing and Evaluationg Formal Thinking Disorders in Schizophrenia. In: Kasanin JS, editor. Language and Thought in Schizophrenia. New York, NY: The Norton Library (1964). p. 65–90.
11. Roche E, Creed L, Macmahon D, Brennan D, Clarke M. The epidemiology and associated phenomenology of formal thought disorder: a systematic review. Schizophr Bull. (2015) 41:951–62. doi: 10.1093/schbul/sbu129
12. Sass LA, Parnas J. Schizophrenia, consciousness, and the self. Schizophr Bull. (2003) 29:427–44. doi: 10.1093/oxfordjournals.schbul.a007017
13. Sass L, Parnas J. Thought disorder, subjectivity, and the self. Schizophr Bull. (2017) 43:497–502. doi: 10.1093/schbul/sbx032
14. Parnas J, Henriksen MG. Disordered self in the schizophrenia spectrum: a clinical and research perspective. Harv Rev Psychiatry. (2014) 22:251–65. doi: 10.1097/HRP.0000000000000040
15. Nordgaard J, Henriksen MG. Phenomenological psychophatology and quantitative research. In: Stanghellini G, Broome M, Fernandez A, Fusar-Poli P, Raballo A, Rosfort R, editors. Oxford Handbook of Phenomenological Psychopathology. Oxford: Oxford University Press (2019).
16. Parnas J, Moller P, Kircher T, Thalbitzer J, Jansson L, Handest P, et al. EASE: examination of anomalous self-experience. Psychopathology. (2005) 38:236–58. doi: 10.1159/000088441
17. Nordgaard J, Revsbech R, Saebye D, Parnas J. Assessing the diagnostic validity of a structured psychiatric interview in a first-admission hospital sample. World Psychiatry. (2012) 11:181–5. doi: 10.1002/j.2051-5545.2012.tb00128.x
18. Von Liepmann D, Beauducek B, Brocke B, Amthauer R. Intelligenz-Struktur-Test 2000 R (I-S-T 2000 R). Göttingen: Hogrefe (2001).
19. Harrow M, Auinlan D. Disordered Thinking and Schizophrenic Psychopathology. New York, NY: Gardner Press (1985).
20. Marengo JT, Harrow M, Lanin-Kettering I, Wilson A. Evaluating bizarre-idiosyncratic thinking: a comprehensive index of positive thought disorder. Schizophr Bull. (1986) 12:497–511. doi: 10.1093/schbul/12.3.497
21. Subotnik KL, Nuechterlein KH, Green MF, Horan WP, Nienow TM, Ventura J, et al. Neurocognitive and social cognitive correlates of formal thought disorder in schizophrenia patients. Schizophr Res. (2006) 85:84–95. doi: 10.1016/j.schres.2006.03.007
22. Hertler CA, Chapman LJ, Chapman JP. A scoring manual for literalness in proverb interpretation. J Consult Clin Psychol. (1978) 46:551–5. doi: 10.1037/0022-006X.46.3.551
23. Exner JE. The Rorschach: A Comprehensive System: Vol 1.. New York, NY: Grune and Stratton (1974).
24. Mcguffin P, Farmer A, Harvey I. A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Arch Gen Psychiatry. (1991) 48:764–70. doi: 10.1001/archpsyc.1991.01810320088015
25. Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry. (1978) 35:837–44. doi: 10.1001/archpsyc.1978.01770310043002
26. Gross G, Huber G, Klosterkötter J, Linz M. Bonner Skala Für die Beurteilung von Basissymptomen. Berlin; Heidelberg: Springer Verlag (1987).
27. Matthysse S, Holzman PS, Gusella JF, Levy DL, Harte CB, Jorgensen A, et al. Linkage of eye movement dysfunction to chromosome 6p in schizophrenia: additional evidence. Am J Med Genet. (2004) 128B:30–6. doi: 10.1002/ajmg.b.30030
28. Medcalc (2020). Available online at: https://www.medcalc.org/calc/diagnostic_test.php (accessed November 1, 2020).
29. Shenton ME, Solovay MR, Holzman P. Comparative studies of thought disorders. II Schizoaffective disorder. Arch Gen Psychiatry. (1987) 44:21–30. doi: 10.1001/archpsyc.1987.01800130023004
30. Solovay MR, Shenton ME, Holzman PS. Comparative studies of thought disorders. I Mania and schizophrenia. Arch Gen Psychiatry. (1987) 44:13–20. doi: 10.1001/archpsyc.1987.01800130015003
31. Vaever MS, Licht DM, Moller L, Perlt D, Jorgensen A, Handest P, et al. Thinking within the spectrum: schizophrenic thought disorder in six Danish pedigrees. Schizophr Res. (2005) 72:137–49. doi: 10.1016/j.schres.2004.04.001
32. Merleau-Ponty M. Indirect language and the voices of silence. In: Merleau-Ponty M, Mccleary D, editors. Signs. Evanston: Northwestern University Press (1964).
34. De Kock L. ‘I think’ (the thought of others). The German tradition of apperceptionism and the intellectual history of schizophrenia. Hist Psychiatry. (2020) 31:387–404. doi: 10.1177/0957154X20933827
35. Erikson EH. The problem of ego identity. J Am Psychoanal Assoc. (1956) 4:56–121. doi: 10.1177/000306515600400104
36. Nordgaard J, Parnas J. Self-disorders and the schizophrenia spectrum: a study of 100 first hospital admissions. Schizophr Bull. (2014) 40:1300–7. doi: 10.1093/schbul/sbt239
37. Henriksen MG, Parnas J. Self-disorders and schizophrenia: a phenomenological reappraisal of poor insight and noncompliance. Schizophr Bull. (2014) 40:542–7. doi: 10.1093/schbul/sbt087
38. Parnas J, Henriksen MG. Mysticism and schizophrenia: a phenomenological exploration of the structure of consciousness in the schizophrenia spectrum disorders. Conscious Cogn. (2016) 43:75–88. doi: 10.1016/j.concog.2016.05.010
39. Parnas J, Urfer-Parnas A, Stephensen H. Double bookkeeping and schizophrenia spectrum: divided unified phenomenal consciousness. Eur Arch Psychiatry Clin Neurosci. (2020). doi: 10.1007/s00406-020-01185-0. [Epub ahead of print].
40. Nelson B, Thompson A, Yung AR. Basic self-disturbance predicts psychosis onset in the ultra high risk for psychosis “prodromal” population. Schizophr Bull. (2012) 38:1277–87. doi: 10.1093/schbul/sbs007
41. Nordgaard J, Handest P, Vollmer-Larsen A, Saebye D, Pedersen JT, Parnas J. Temporal persistence of anomalous self-experience: a 5years follow-up. Schizophr Res. (2017) 179:36–40. doi: 10.1016/j.schres.2016.10.001
42. Nordgaard J, Nilsson LS, Saebye D, Parnas J. Self-disorders in schizophrenia-spectrum disorders: a 5-year follow-up study. Eur Arch Psychiatry Clin Neurosci. (2018) 268:713–8. doi: 10.1007/s00406-017-0837-3
43. Svendsen IH, Oie MG, Moller P, Nelson B, Haug E, Melle I. Basic self-disturbances independently predict recovery in psychotic disorders: a seven year follow-up study. Schizophr Res. (2019) 212:72–8. doi: 10.1016/j.schres.2019.08.009
44. Koren D, Tzivoni Y, Schalit L, Adres M, Reznik N, Apter A, et al. Basic self-disorders in adolescence predict schizophrenia spectrum disorders in young adulthood: a 7-year follow-up study among non-psychotic help-seeking adolescents. Schizophr Res. (2020) 216:97–103. doi: 10.1016/j.schres.2019.12.022
Keywords: schizophrenia, schizotypy, proverb, bizarre, literal, self-disorder, formal thought disorder
Citation: Nordgaard J, Gravesen-Jensen M, Buch-Pedersen M and Parnas J (2021) Formal Thought Disorder and Self-Disorder: An Empirical Study. Front. Psychiatry 12:640921. doi: 10.3389/fpsyt.2021.640921
Received: 12 December 2020; Accepted: 26 February 2021;
Published: 08 April 2021.
Edited by:
Anna Comparelli, Sapienza University of Rome, ItalyReviewed by:
Stefan Jerotic, Clinical Centre of Serbia, SerbiaCopyright © 2021 Nordgaard, Gravesen-Jensen, Buch-Pedersen and Parnas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie Nordgaard, anVsaWVfbm9yZGdhYXJkQGRhZGxuZXQuZGs=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.