- 1Department of Psychiatry, Jimma University, Jimma, Ethiopia
- 2School of Nursing and Midwifery, Jimma University, Jimma, Ethiopia
- 3Department of Environmental Health Sciences and Technology, Jimma University, Jimma, Ethiopia
- 4Department of Health, Behavior, and Society, Jimma University, Jimma, Ethiopia
- 5Department of Biostatistics and Epidemiology, Jimma University, Jimma, Ethiopia
- 6Department of Health Policy and Management, Jimma University, Jimma, Ethiopia
Background: The global burden of mental health problems is high and is predicted to rise. At present, mood symptoms are the foremost common psychological problems worldwide, yet little is known regarding their magnitude and associated factors in developing countries. Therefore, this study aimed to assess the magnitude and associated factors of anxiety, depressive, manic symptoms, and suicidal behavior among the rural Jimma community, Ethiopia.
Methods: A community-based quantitative cross-sectional survey was employed on 423 households selected through systematic random sampling. An adapted version of the Mini International Neuropsychiatric Interview tool was used for the structured face-to-face interview. The collected data were checked for completeness, coded, and inserted into Epi Data version 3.1 and exported to SPSS version 23 for analysis. Variables with P < g0.05 and odds ratio (OR) [95% confidence interval (CI)] on multivariate logistic regression analysis were considered as factors associated with the outcome variable.
Results: Overall, 185 (44.0%), 55 (13.1%), 44 (10.5%), and 23 (5.5%) of the respondents had anxiety, depressive, manic symptom, and suicide behavior, respectively. The odds of having anxiety symptoms were nearly 5 times higher among those who had perceived discrimination and racism experience compared to their counterpart [adjusted OR (AOR), 5.02; 95% CI, 1.90–13.26]. Likewise, recently bereaved participants had 4-fold higher odds of reporting depressive symptoms (AOR, 3.9; 95% CI, 1.4–10.4) than the non-bereaved ones. Furthermore, respondents who had depressive symptoms were almost four and a half times more likely to have manic symptoms compared to those who did not (AOR, 4.3; 95% CI, 1.71–11.02).
Conclusion: Anxiety, depressive, manic symptoms, and suicidal behavior were prevalent in the community and positively associated with multiple psychosocial factors. Implementing accessible and affordable community-based mental health services is recommended to mitigate the problems.
Background
Mental health is vital to individual well-being, family bonding, and successful contributions to society. It is associated with the development of societies and countries (1, 2).
The global burden of mental health problems (mood, anxiety disorder, and suicide) is high and predicted to rise. At present, mood symptoms are the foremost common psychological problems worldwide, and it has been forecasted that unipolar depressive disorders will be the second leading cause of the burden of disease in 2030 (3–7).
Mental health problems are known to increase morbidity and mortality and are an important risk factor for adverse health outcomes. The social, economic, and health effects are extensive, where they are related to increased all-cause mortality, occupational disability, poor quality of life, and cardiovascular disease risk (8). Despite this, mental health is often ignored as public health priority (9).
Mental health problems such as mood disorders are associated with multiple factors such as gender, income (10), education level, socioeconomic conditions, medical illness (11, 12), age, substance use (13), stressful life events (14, 15), history of parental substance use (16), residence, marital status (17, 18), perceived racism and discrimination (19, 20), domestic violence (15), death of a close relative (21), birth order (22, 23), violence, migration, sexual abuse experience, life-threatening and physical injuries, difficulties with family relationships, and low emotional support at home during childhood (24, 25).
The World Health Organization (WHO) World Mental Health surveys show clearly that mental disorders are quite common in all the countries (26). However, developing countries, such as Ethiopia, are facing the impact of mental health problems while confronted with limited resources and inequities in access to mental health care (27).
More than three-quarters of people who have mental problems are residing in low- and middle-income countries (LMICs), with mental illness and substance use disorders presenting as an important cause of disease burden (28, 29). In many LMICs, there is typically a shortage of mental health professionals; with little or no multidisciplinary team and few regular drugs available, this can further worsen the impacts and burdens of the problems (30).
In Ethiopia, mental illness is the leading non-communicable disorder in terms of burden. Indeed, in a predominantly rural area of Ethiopia, mental illness comprised 11% of the total burden of disease. Severe mental illness is more often attributed to supernatural causes, rather than as a result of biomedical or psychosocial causes. The number of trained mental health professionals is inadequate for providing services to Ethiopians. There is only one dedicated psychiatric hospital in the entire country for more than 110 million population (31).
Evidence showed that in the rural context living conditions such as limited social and economic resources, stressful life events, poverty, and other demographic disadvantages pose a greater risk for mental health problems (32, 33). Also, various sociocultural factors such as deeply ingrained religious and inherited beliefs that all mental illnesses contribute to the existence and poor modern treatment for mental health problems in the country (34). In Ethiopia, in any ethnic or religious group, supernatural powers are given the attribute of controlling the well-being of the individual's mind. The traditional healing methods are used more by most people (35–37).
In Ethiopia, where undernutrition and preventable communicable diseases are very rampant, mental health problems, which are considered as non-fatal, are not given due consideration (38). Valid and inclusive epidemiological data on the magnitude and associated factor of mental health problems generated from community-based surveys have significant scientific and health policy implications (39). There are some research works documented in the literature regarding the magnitude and associated factors of anxiety, depressive, manic symptoms, and suicidal behavior among Ethiopians. However, in this study, variables such as migration history, perceived discrimination and racism experience, sexual abuse, and domestic violence were included. Furthermore, the studies on mental health problems are scarce in the sub-Saharan countries, and most studies were conducted in the cities. However, this study has tried to reveal the extent of mental health problems and associated factors in the neglected rural area of the country; this might help the local health planners and non-governmental organizations working in the area of mental health to investigate and design effective locally sound mental health interventions to avert the problems. Hence, this study aimed to assess the magnitude and associated factors of anxiety, depressive, manic symptoms, and suicidal behavior among the Jimma zone community, Ethiopia.
Methods
Study Setting
The study was carried in the Jimma zone, Seka Chekorsa district. Jimma zone is administratively divided into 20 districts and one town administration. The total population of the zone was 2,986,957 in 2017 (40). Seka Chekorsa district is located 20 km from Jimma town, and the district has 30 kebeles (the lowest administrative division in the area) with a total population of 208,096 (41). This district has one primary hospital, nine health centers, and 35 health posts. The study was conducted from March 1 to 22, 2020.
Ethiopia is one of the 213 countries that have registered 2019 coronavirus disease (COVID-19) cases since March 13, 2020. In Ethiopia, several cases and deaths are identified (42). The study data were collected in the first couple of weeks of the virus detection in the country.
Sample Size Estimation
Single population proportion formula was used to obtain the desired sample size. We have assumed a 50% proportion of the magnitude of mood symptoms to get the maximum sample size, 95% confidence level, and 5% margin of error. Hence, n = (zα/2)2 P(1–p)/d2; hence, n = (1.96)2 × 0.5 (1–0.5)/(0.05)2 = 384. With the addition of a 10% contingency for non-response, the final sample size was 423.
Study Design, Population, Sampling Technique, and Procedures
A community-based quantitative cross-sectional survey was carried out. First, Seka Chekorsa district was selected from a total of 20 districts in the zone through a simple random sampling lottery technique. Of the 30 kebeles in this district, nine were selected by lottery method based on the WHO sample size calculation guideline for the district health system (43). The number of sampled respondents from each kebele was determined by proportional allocation to the total number of households in each of the sampled kebeles. A systematic random sampling technique was used to select the study units, and periodic interval (K) was calculated using the formula K = N/n, whereby N is the total households in the selected kebeles (1,555), and n is the calculated sample size (423). Accordingly, every four households were included in the study. The first study unit was selected by lottery method between the first and fourth households. Finally, randomly selected household members 18 years or older in the selected household responded to the interview. The study participants were household members 18 years or older in the randomly selected households.
Eligibility Criteria
All the study community members 18 years or older were included in the study. The study community members who were acutely or chronically ill, which makes him/her difficult to participate in the study, were excluded from the study.
Measurements and Procedures
A face-to-face interviewer-administered structured questionnaire was used using an adapted version of the Mini International Neuropsychiatric Interview (M.I.N.I.). M.I.N.I. 5.0.0 was developed by Sheehan et al. and designed for assessing the major Axis I mental health problems in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (researchers and clinicians working in non-profit or publicly owned settings can freely use for clinical and research use) (44). Validation and reliability of the tool have been done with good psychometric properties (45–47). The reliability, Cronbach α score, of the scales in this study was 0.76. This study has assessed the prevalence of DSM-IV criteria A symptoms of panic disorder (lifetime), social anxiety disorder (past month), generalized anxiety disorder (past 6 months), suicide characteristics (such as repeatedly consider hurting self, having a plan to kill self, repeatedly wish dead, and suicide attempt) (past month), a lifetime suicide attempt, major depression (current or 2 weeks), and manic episode (lifetime). The tool has also included questions to measure other family members with such symptom presentations. If the subject answers positive for any of the questions about symptoms included in M.I.N.I.'s anxiety, depressive, manic symptoms, and suicide module, it is considered to have the symptoms. For factors associated with the outcome variable, the questionnaire was developed after a thorough review of the literature that has been done on similar topics (32, 48–50); the presence or absence of these factors was measured using a structured question. Data were collected by 20 health extension workers after receiving training for 2 days on the components of the questionnaire, data recording, and the ethical principles of the data collection process. The English version of the questionnaire was translated into Afaan Oromo and back-translated to English to ensure its uniformity by blinded language experts. The translations were face validated by two independent external experts in the field. Moreover, the data collection tool was pilot tested on 5% of the population in another district to ensure its clarity and consistency. The pretest results showed the questionnaire was easily understandable, and the interview process was clear for the respondents. Afaan Oromo version of the questionnaire was used to obtain the desired data. Appropriate COVID-19 infection containment measures, which WHO recommended (keeping a 2-meter distance, wearing a face mask, and using alcohol-based hand sanitizers), were practiced during the data collection period.
Data Organization and Statistical Analysis
The collected data were checked for completeness, given code, and inserted into Epi Data version 3.1 and exported to SPSS version 23 for analysis. Descriptive statistics were done to summarize the variables. The logistic regression analysis model was used to identify the factor associated with the outcome variable. First, bivariate logistic regression analysis was done, and variables with p < 0.25 were selected as candidate variables for multivariate logistic regression analysis. After the model was tested for multicollinearity and Hosmer–Lemeshow test of model fitness, the final multivariate logistic regression analysis was carried out. Finally, variables with p < 0.05 and 95% confidence interval and odds ratio (OR) were considered as factors associated with the outcome variable.
Ethical Consideration
Ethical approval was obtained from the Institutional Review Board (IRB) of Jimma University (IHRPGD/584/2019). Additionally, a support letter was found from Oromia Regional Health Bureau, Jimma Zone Health Bureau, and a subsequent support letter was obtained from the Seka Chekorsa district health office before the commencement of data collection. Respondents were informed of the study objectives and were assured of the anonymity of their participation. Participation in the study was voluntary, and written informed consent was taken from the respondents. Respondents who had anxiety, depressive and manic symptoms, and suicidal behavior were advised to visit the nearby health facility for further mental health evaluation and management.
Results
Sociodemographic Characteristics
A total of 420 study participants were interviewed successfully, giving a response rate of 99.3%. Three respondents were not willing to participate in the study. The mean age of the respondents was 37.2 years (SD, ±11.9 years) with a range of 18 to 80 years. The majority of the study respondents were females [230 (54.8%)], married [345 (82.1%)], Oromo ethnic group [395 (94%)], Muslim [384 (91.4%)], and unable to read and write [168 (40.0%)]. The mean monthly income was 1,562.5 Ethiopian Birr (ETB) (SD, ±2,769.8) (approximately US $48.00) (Table 1).
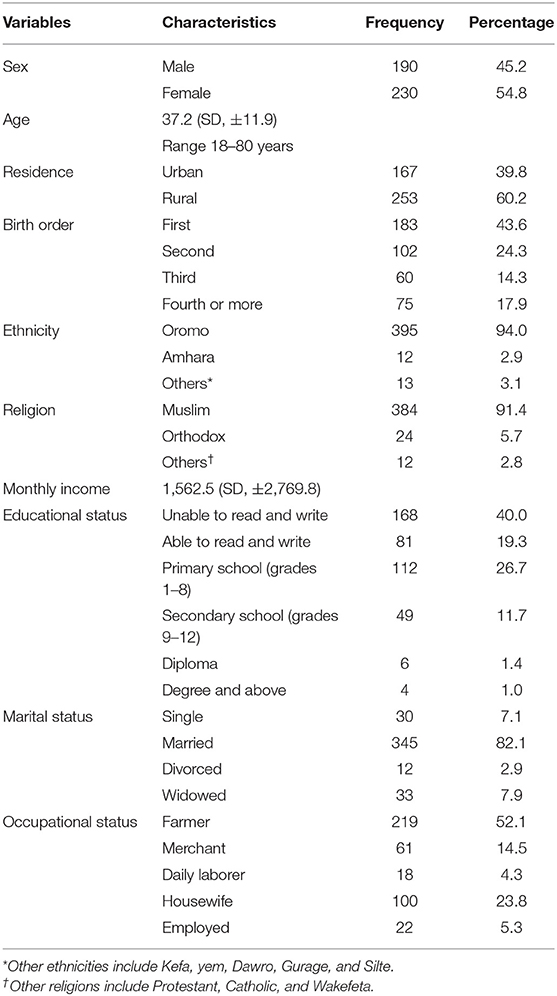
Table 1. Sociodemographic characteristics of respondents at Jimma Zone, Seka Chekorsa district, Southwest Ethiopia, March 2020.
Anxiety Symptoms
Twenty-eight participants (6.7%) had spells or attacks of sudden anxiety, frightened, uncomfortable, or uneasy, even in situations where most people would not feel that way on more than one occasion. Similarly, about 71 (16.9%) respondents were fearful or embarrassed by being watched including things such as speaking in public, eating in public or with others, writing while someone watches, or being in social situations in the past month. Nearly one-quarter [101 (24.0%)] of the participants were worried excessively or had been anxious about several things over the past 6 months. Overall, 185 (44.0%) seemed to have anxiety symptoms (Table 2).
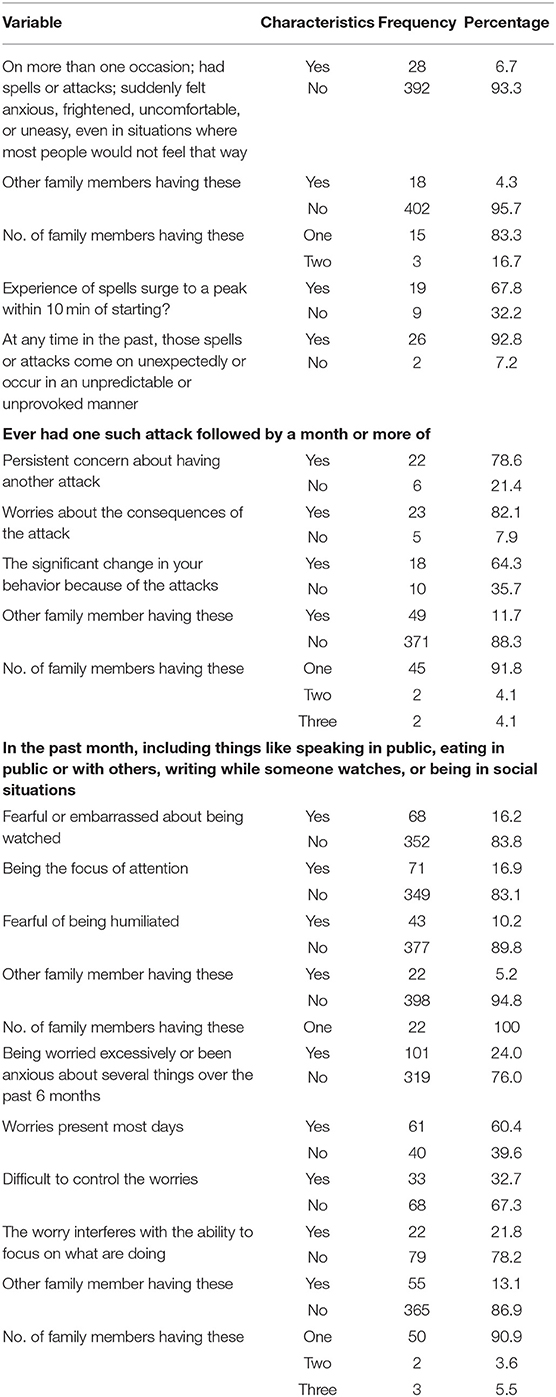
Table 2. Anxiety symptoms characteristics of the respondents and their family at Jimma Zone, Seka Chekorsa district, Southwest Ethiopia, March 2020.
Depressive Symptoms and Suicide Characteristics
Of the total respondents, 39 (9.3%) reported they have been consistently depressed, hopeless most of the day, nearly every day, for the past 2 weeks or more. About 31 (7.4%) participants could identify another family member who was tearful, hopeless, and complaining about emptiness for the past 2 weeks or more. About 40 (9.5%) of the respondents were less interested in most things or much less able to enjoy the things they were used to enjoy most of the time in the past 2 weeks or more. Additionally, 23 (5.5%) of the participants reported repeatedly wishing to be dead, and 5 (1.2%) attempted suicide. Overall, 55 (13.1%) of the respondents had depressive symptoms (Table 3).
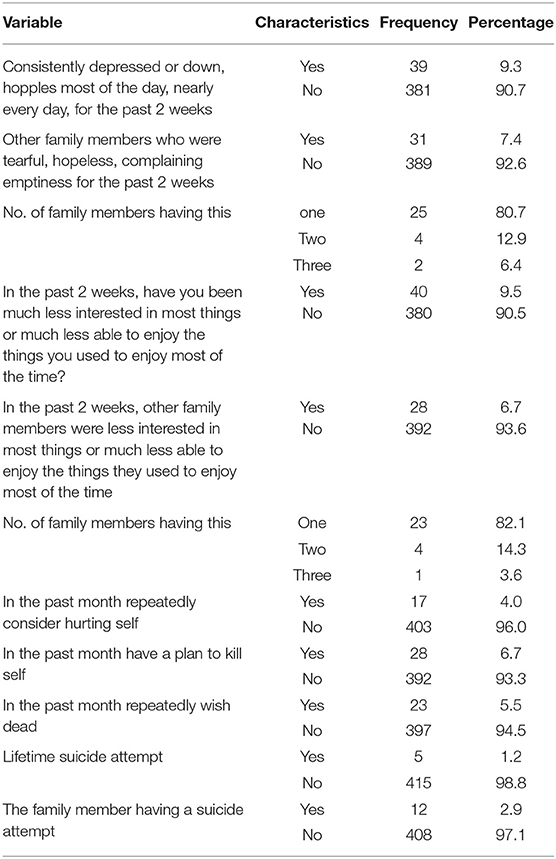
Table 3. Depression and suicidal behavior of the respondents and their family at Jimma Zone, Seka Chekorsa district, Southwest Ethiopia, March 2020.
Manic Symptoms
Among the total respondents, 11 (2.6%) had a lifetime period where they feel “up” or “high” or “hyper” or so full of energy or full of self that got into trouble, or other people thought they were not their usual self for 1 week or more. About 38 (9.0%) of the participants described persistently feeling irritable, had arguments or verbal or physical fights, or shouted at people for several days. Overall, 44 (10.5%) of the respondents were identified to have manic symptoms (Table 4).
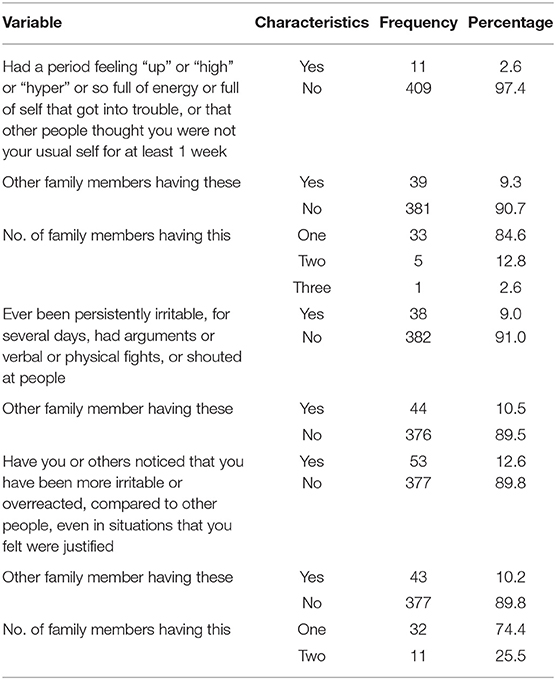
Table 4. Manic symptoms characteristics of the respondents and their family at Jimma Zone, Seka Chekorsa district, Southwest Ethiopia, March 2020.
Respondents' Psychological and Behavioral Characteristics
Among the respondents, 48 (11.4%) had a recent loss of a close family member. About 45 (10.7%) participants were reported being discriminated against. About 12 (2.9%) had confided about being sexually abused, and 118 (28.1%) described financial problems (Table 5).

Table 5. Respondents psychological and behavioral characteristics at Jimma Zone, Seka Chekorsa district Southwest Ethiopia, March 2020.
Factors Associated With Anxiety Symptoms
Male participants had a 50% less risk of developing anxiety symptoms [adjusted OR (AOR), 0.50; 95% CI, 0.29–0.87]. The analysis results also showed rural residents were found to have a 75% less risk of having anxiety (AOR, 0.25; 95% CI, 0.14–0.44). The odds of having anxiety symptoms were ~2 times higher among those who were on the first birth order than those on the third or more birth order. Those employed had 57% less risk of developing anxiety symptoms compared to the housewife counterpart (AOR, 0.43; 95% CI, 0.20–0.90). Respondents whose parents abuse substances had nearly twice increased odds of developing anxiety symptoms (AOR, 2.18; 95% CI, 1.12–4.22). The odds of developing anxiety symptoms were ~5 times higher among those who had perceived discrimination and racism experience (AOR, 5.02; 95% CI, 1.90–13.26). Respondents who had reported stressful event had nearly 4 times' increase of having anxiety symptoms (AOR, 3.96; 95% CI, 1.53–10.24) (Table 6).
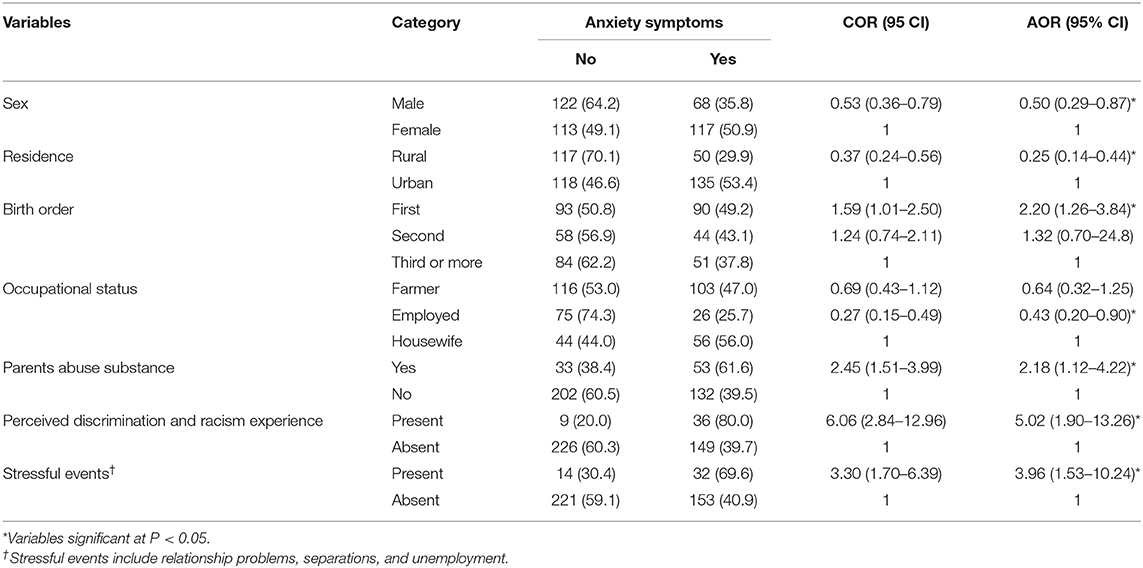
Table 6. Factors associated with anxiety symptoms of the respondents at Jimma Zone, Seka Chekorsa district, Southwest Ethiopia, March 2020.
Factors Associated With Depressive Symptoms
The analysis result has shown depressive symptoms were three and a half times higher among respondents who were unable to read and write compared to primary school and above academic status (AOR, 3.5; 95% CI, 1.3–8.9). Respondents who were on the first birth order were nearly three and a half times more likely to have depressive symptoms compared to those on the third and above birth order (AOR, 3.6; 95% CI, 1.4–8.7). The study participants who had recent bereavement were nearly 4 times more likely to report depressive symptoms (AOR, 3.9; 95% CI, 1.4–10.4). Furthermore, respondents who had depressive symptoms were ~5 times higher to have stressful events compared to their counterparts (AOR, 4.8; 95% CI, 1.7–13.5) (Table 7).
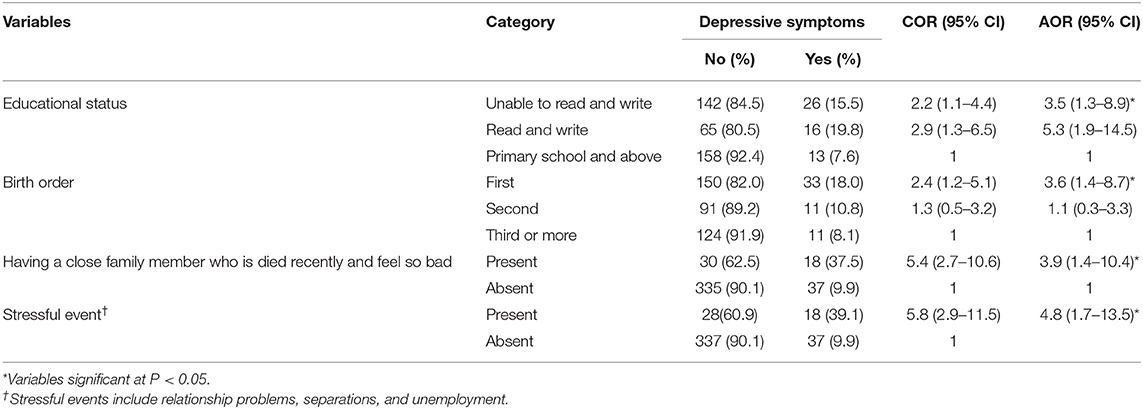
Table 7. Factors associated with depressive symptoms of the respondents at Jimma Zone, Seka Chekorsa district, Southwest Ethiopia, March 2020.
Factors Associated With Manic Symptoms
Respondents who had depressive symptoms were almost four and a half times more likely to have manic symptoms (AOR, 4.3; 95% CI, 1.71–11.02). Study participants with parental substance use history were 3 times more at risk of having manic symptoms (AOR, 2.8; 95% CI, 1.21–6.69). The result of the regression analysis has revealed respondents who had perceived discrimination and racism experience had 5 times more likely to report manic symptoms (AOR, 5.0; 95% CI, 1.96–12.77). Firstborn children had ~4 times higher risk of developing manic symptoms compared to those on the third or more birth order (AOR, 4.1; 95% CI, 1.29–12.98). Study participants who perceived their economic status as a medium were two and a half times more likely to have manic symptoms than those who perceived low economic status (AOR, 2.3; 95% CI, 1.06–5.24) (Table 8).
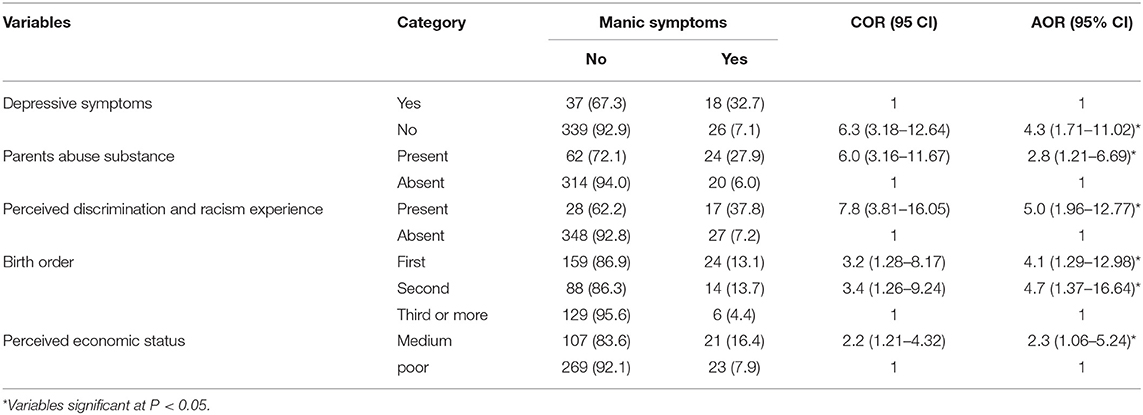
Table 8. Factors associated with manic symptoms of the respondents at Jimma Zone Seka Chekorsa district Southwest Ethiopia, March 2020.
Discussion
The study aimed to assess the magnitude and factors associated with anxiety, depressive, and manic symptoms, and suicidal behavior among the Jimma zone community.
The finding of this study showed 55 (13.1%) of the respondents had depressive symptoms. Consistent findings were reported from the pooled prevalence of depression in Ethiopia (51), rural communities in Malaysia (11.30%) (10), Brazil (14%) (52), northwest Ethiopia (17.5%) (53), and Puerto Rico (17.8%) (54). The findings in all studies have shown that depression is a global problem. However, this study finding is higher than the 4.4% WHO global and regional estimates of the prevalence of depression in 2015 (55). The current study was conducted 5 years later than the WHO study; various changes such as economic inflation, ethnic violence, increased Khat (local stimulant leaf), and other substance use in the area could be the probable contributing factors for the high prevalence of depression in the area. Yet, the result is lower than the studies done among adolescents living in the cities of Kenya (26.4%) (56) and South Brazil (35.4%) (11). The discrepancy could be explained by as follows: this study was conducted in the rural area of the country compared to the Kenya and Brazil studies. Concentrations of low socioeconomic status; low social capital, e.g., social support; and higher rates of pollution [e.g., air, water, and noise pollution in the cities might be the reason for the high prevalence of depression symptoms (57, 58)].
Manic symptoms were noted in 44 (10.5%) of the respondents; similarly, the US National Epidemiologic Catchment Area database showed that the prevalence of subthreshold bipolar symptoms was 5.1% (59). At present, no data exist that indicate how many patients there are with such subthreshold bipolar symptoms in the developing countries and community setting. The high prevalence of substance (Khat) use, socioeconomic pressure, and limited availability of mental health treatment centers in the area might contribute to the symptoms (39, 60).
The finding of this study has shown 185 (44.0%) of the respondents had anxiety symptoms. This finding is higher than those found in the studies done in Malaysia (8.2%) (15), from African cultures (7.3%) to Euro/Anglo cultures (10.4%) (61), rural communities of Northern India (22.7%) (62), and Kashmir valley (26%) (17). The worries and uncertainty resulting from living in poverty seem to be an important driver of mental health problems including anxiety, as do the effects of low income on childhood development and one's living environment (63).
In this study, 5.5 and 1.2% of the participants reported repeatedly wishing dead and attempting suicide, respectively. A consistent finding was reported from the study done in Addis Ababa, Ethiopia, in which the rates of suicidal ideation and attempt were 2.7 and 0.9%, respectively (64). Another population study in Ethiopia has shown 13.5% of the study participants had suicidal ideation, and 1.8% had suicide attempt (65). Additionally, a study was done in Nigeria that revealed 7.28% had suicidal ideation (66). A study done in rural communities in China reported 4.8% and 0.4% had suicidal ideation and attempt, respectively (67). However, our finding was lower than the findings of 17.1% for suicidal ideation and 2.8% for suicide attempts from Brazil (68). The discrepancy could be explained by the differences in the social control networks, extended family ties, religious, cultural practices differences, and different stressors in the study settings (7, 69).
The finding of this study has revealed that respondents with higher educational status had less risk of developing depression. This is consistent with the studies done in Iran (18) and Pakistan (70). This could be because education as a means enables people to gain success in life and may fundamentally contribute to the emotional well-being of the person (71). In the study area, an individual with higher education status usually has better work opportunities, health information, and living standards. This could protect them against developing depression (72). Nevertheless, individuals with higher education backgrounds were comparatively more prone to mood disorders in the study done in the United States (10). This might be explained in that in Western culture highly educated people seek well-paid jobs and may have better socioeconomic expectations. In their race to meet these expectations, they could experience unmanageable stress, which predisposes them to mood disorders (73).
In the current study, respondents with first and second birth order status were more prone to have depression symptoms than those with third and above birth order status. This finding is in line with the study done in Nepal (74). However, no difference was observed in the study done in Egypt (75). Similarly, birth order was found to have an association with anxiety symptoms in this study. This finding was consistent with the study done in Kuwait (69). Birth order is one of the most significant life factors, and it is the best indicator of the kind of personality someone has. In the study area, the oldest child commonly has many responsibilities compared to the youngest child of the family. Studies also have shown that because of much expectations that are placed on the oldest child in a family, the eldest one experiences more emotional disturbance and struggles in coping with the stressful condition (76). In addition, the firstborns were considered as the smaller version of their parents; therefore, they have received much more control and attention from their parents. Hence, they tend to be over responsible, reliable, well-behaved, and careful. This might explain a higher level of emotional disturbances in this group (77).
In our study, respondents with self-perception of their economic status as a medium were at higher risk of having manic symptoms. In many studies, it was usually noted that bipolar disorder was relatively higher among those who have medium socioeconomic status than that of controls or the general population (78, 79). However, many current studies have failed to confirm such assumptions (12). The anticipation of economic shocks may cause mental illness such as mania. People living in poverty face substantial uncertainty and income volatility and complex financial portfolios, often without access to formal insurance; this might increase the risk of developing bipolar symptoms (80, 81).
In the current study, having depressive symptoms was associated with an increased risk of manic symptoms. This might be explained by bipolar disorders beginning with depressive episodes, and a significant proportion of individuals who had initial major depressive disorder will later be reclassified as having a bipolar disorder (82). Various precipitating factors, such as socioeconomic stress, poor control of depressive-manic symptoms through medication, and the nature of the illness by itself, might be the reason for manic-depressive cycle (83, 84).
Perception of prejudice and discrimination based on ethnicity increased the risk of presentation of manic and anxiety symptoms among the respondents. Stress associated with the experiences of perceived racial discrimination and prejudice has substantial negative effects on both physical and mental health and might precipitate mental health problems (85). Discrimination may contribute to psychological problems through numerous possible mechanisms including negative psychological and physical stress response, hypervigilance, and increased involvement in unhealthy behaviors (20, 86, 87). In Ethiopia, ethnicity-related violence in different parts of the country could be the reason for the death, and internal displacement of people from their living area can be considered as a serious stressor for manic symptoms eruption (88, 89).
In this study, respondents whose parents abuse substances were more likely to have anxiety symptoms. This could be because an individual who had parents with abusing substances were having problems including poor attachments, economic difficulties, legal problems, emotional abuses, and violence (90).
Most the studies conducted on depression, anxiety, mania, and suicide behavior in Ethiopia were among prisoners (91), substance users (92), university staffs and students (93, 94), women (95), pregnant women (96, 97), postpartum mothers (98), children (99), medically ill patients (100–103), epileptic patients (104), disorder threshold level (39, 105, 106), and in the context of common mental disorders (13, 107). Our study finding has a unique contribution as it has revealed the rural community mental health problems characteristics.
However, this article has presented psychiatric symptoms, not disorders. Additionally, some of the discussion comparisons were made with many countries that are culturally different from this study setting. So, the generalization and conclusions should be made cautiously. Moreover, as it is cross-sectional by nature, it does not show the cause-and-effect relationship between the outcome and explanatory variables. Ethiopia has registered the first COVID-19 cases on March 13, 2020, the period where this study was conducted. Even though the study was conducted in a rural part of Ethiopia, where the spread of the infection was gradual, this might affect the results of this study. The current study did not assess some of the anxiety symptoms in agoraphobia, posttraumatic stress disorder, and obsessive–compulsive disorder. Furthermore, the study tool to assess the variables of this study was not validated in the local, Afan Oromo, and Amharic languages. Additionally, the latest version of the M.I.N.I. questionnaire was not used because the study tool was restricted by the publisher for free use.
Future Directions
Based on this study's limitations, we recommend interested researchers in the field of mental health and public health to investigate further the magnitude of psychiatric disorders with the latest and validated tools in local languages with a larger sample size. Furthermore, longitudinal studies are recommended to explore the cause-and-effect association of the outcome and explanatory variables.
Clinical Implications of the Study
This study may have an immense contribution in improving the mental health service of the study area by revealing the magnitude of the problems and contributing factors. In the study setting, there were very limited mental health services, which do not match with the rates of mental health problems as found in this study. This study will further motivate the researchers to evaluate the study population's intention to use mental health services, and the presence of stigma on patients with mental health problems and services use that require effective locally sound education programs in the study setting.
Conclusions
The study has revealed that a significant proportion of the community members have anxiety depressive, manic symptoms, and suicidal behavior. Furthermore, various risk factors were identified to have an association with the problems. Therefore, appropriate community-based mental health services should be designed and implemented to address the negative impact of the problems.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the institutional review board of Jimma University, Institute of health. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YT was the principal investigator of the study and was involved from inception to design acquisition of data, analysis, and interpretation, and drafting and editing of the manuscript. LA, SA, GT, ZB, GA, MG, and KY were involved in the reviewing of the proposal, tool evaluation, interpretation, and critical review of the draft manuscript. All authors read and approved the final manuscript.
Funding
Jimma University has funded the study. The funders had no role in the design of the study data collection, analysis, interpretation, and writing of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Jimma University for financial support and the study participants for providing study information.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; CORm, Crude Odds Ratio; OR, Odds Ratio; SD, Standard Deviation; SPSS, Statistical Package for the Social Sciences; US, United State.
References
1. World Health Organization. Mental Health Gap Action Programme - Scaling up Care for Mental, Neurological, and Substance Use Disorders. Geneva: World Health Organization (2008).
2. Becker AE, Kleinman A. Mental health and the global Agenda. N Engl J Med. (2013) 369:66–73. doi: 10.1056/NEJMra1110827
3. Ham L, Van Der, Wright P. Perceptions of mental health and help-seeking behavior in an urban community in Vietnam : an explorative study. Community Ment Heal J. (2011) 47:574–82. doi: 10.1007/s10597-011-9393-x
4. Murray CJL, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet. (1997) 349:1436–42. doi: 10.1016/S0140-6736(96)07495-8
5. Alloy LB, Bender RE, Wagner CA, Abramson LY, Urosevic S. Longitudinal predictors of bipolar spectrum disorders: a behavioral approach system perspective. Clin Psychol Sci Pract. (2009) 16:206–26. doi: 10.1111/j.1468-2850.2009.01160.x
6. Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, Nock MK. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: a meta-analytic review. Clin Psychol Rev. (2016) 43:30–46. doi: 10.1016/j.cpr.2015.11.008
8. Gelaye B, Lemma S, Deyassa N, Bahretibeb Y, Tesfaye M, Berhane Y, et al. Prevalence and correlates of mental distress among working adults in Ethiopia. Clin Pract Epidemiol Ment Health. (2012) 8:126–33. doi: 10.2174/1745017901208010126
9. Jacob N, Coetzee D. Mental illness in the Western Cape Province, South Africa: a review of the burden of disease and healthcare interventions. South African Med J. (2018) 108:176–80. doi: 10.7196/SAMJ.2017.v108i3.12904
10. Wong SY, Lua PL. Anxiety and depressive symptoms among communities in the east coast of Peninsular Malaysia : a rural exploration. MJP Online Early. (2011) 22:22–9.
11. Hirschmann R, Gomes AP, Gonçalves H. Depressive symptomatology among residents of the rural area of a city in Southern Brazil. Rev Saude Publica. (2018) 52 (Suppl. 1):11s. doi: 10.11606/S1518-8787.2018052000266
12. Eid L, Heim K, Doucette S, Mccloskey S, Duffy A, Grof P. Bipolar disorder and socioeconomic status : what is the nature of this relationship? Int J Bipolar Disord. (2013) 1:9. doi: 10.1186/2194-7511-1-9
13. Gari Hunduma, Mulugeta Girma, Digaffe T, Weldegebreal F, Tola A. Prevalence and determinants of common mental illness among adult residents of Harari Regional State, Eastern Ethiopia. Pan Afr Med J. (2017) 28:262. doi: 10.11604/pamj.2017.28.262.12508
14. Sokratous S, Merkouris A, Middleton N, Karanikola M. The association between stressful life events and depressive symptoms among Cypriot university students: a cross-sectional descriptive correlational study. BMC Public Health. (2013) 13:1–16. doi: 10.1186/1471-2458-13-1121
15. Maideen SFK, Sidik SM, Rampal L, Mukhtar F. Prevalence, associated factors and predictors of anxiety: a community survey in Selangor, Malaysia. BMC Psychiatry. (2015) 15:1121. doi: 10.1186/s12888-015-0648-x
16. Maria E Pagano, Richard Rende BFR, Eric L Hargraves ATM, MBK. Impact of parental history of substance use disorders on the clinical course of anxiety disorders. Subst Abus Treat Prev Policy. (2007) 2:35. doi: 10.1186/1747-597X-2-13
17. Housen T, Lenglet A, Ariti C, Shah S, Shah H, Ara S, et al. Prevalence of anxiety, depression, and post-traumatic stress disorder in the Kashmir Valley. BMJ Glob Heal. (2017) 2:e000419. doi: 10.1136/bmjgh-2017-000419
18. Faramarzi M, Cheraghi M, Zamani M, Kheirkhah F, Bijani A, Hosseini SR. Gender-specific predictors of depressive symptoms among community elderly. J Res Health Sci. (2017) 17:377.
19. Karlsen S, Nazroo JY, McKenzie K, Bhui K, Weich S. Racism, psychosis and common mental disorder among ethnic minority groups in England. Psychol Med. (2005) 35:1795–803. doi: 10.1017/S0033291705005830
20. Assari S, Moazen-Zadeh E, Caldwell CH, Zimmerman MA. Racial discrimination during adolescence predicts mental health deterioration in adulthood: gender differences among blacks. Front Public Health. (2017) 5:104. doi: 10.3389/fpubh.2017.00104
21. Sørensen T, Danbolt LJ, Holmen J, Koenig HG, Lien L. Does the death of a family member moderate the relationship between religious attendance and depressive symptoms? The HUNT study, Norway. Depress Res Treat. (2012) 2012:396347. doi: 10.1155/2012/396347
22. Chandola R. A study of birth order, personality & mental health. Int J Adv Res Rev. (2017) 1:26-30. doi: 10.1155/2014/261802
23. Easey KE, Mars B, Pearson R, Heron J, Gunnell D. Association of birth order with adolescent mental health and suicide attempts: a population-based longitudinal study. Eur Child Adolesc Psychiatry. (2019) 28:1079–86. doi: 10.1007/s00787-018-1266-1
24. Pinto ACS, Luna IT, Silva AA, Pinheiro PNC, Braga VAB, e Souza ÂMA. Fatores de risco associados a problemas de saúde mental em adolescentes: revisão integrativa. Rev da Esc Enferm. (2014) 48:555–64. doi: 10.1590/S0080-623420140000300022
25. Tarzia L, Thuraisingam S, Novy K, Valpied J, Quake R, Hegarty K. Exploring the relationships between sexual violence, mental health, and perpetrator identity: a cross-sectional Australian primary care study. BMC Public Health. (2018) 18:1410. doi: 10.1186/s12889-018-6303-y
26. Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, et al. The global burden of mental disorders: an update from the WHO world mental health (WMH) surveys. Epidemiol Psichiatr Soc. (2009) 18:23–33. doi: 10.1017/S1121189X00001421
27. Rojas G, Martínez V, Martínez P, Franco P, Jiménez-Molina Á. Improving mental health care in developing countries through digital technologies: a mini narrative review of the chilean case. Front Public Heal. (2019) 7:391. doi: 10.3389/fpubh.2019.00391
28. Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low- and middle-income countries. Health Serv Insights. (2017) 10:1178632917694350. doi: 10.1177/1178632917694350
29. World Health Organisation. Millions With Mental Disorders Deprived of Treatment and Care. WHO. (2010). Available online at: https://www.who.int/mediacentre/news/releases/2008/pr37/en/%0Ahttp://www.who.int/mediacentre/news/releases/2008/pr37/en/
30. Mckenzie K, Patel V, Araya R. Learning from low-income countries: mental health the pathways to care and prevention. BMJ. (2004) 329:1138–40. doi: 10.1136/bmj.329.7475.1138
31. FMOH. National Mental Health Strategy 2012/13–2015/16. Addis Ababa: Federal Democratic Republic of Ethiopia Ministry of Health (2013).
32. Dias B, Parreira M, Goulart BF, Monteiro S. Common mental disorders and associated factors : a study of women from a rural area. Rev Esc Enferm USP. (2017) 51:e03225. doi: 10.1590/s1980-220x2016033103225
33. Gomes VF, Miguel TLB, Miasso AI. Transtornos mentais comuns: perfil sociodemográfico e farmacoterapêutico. Rev Lat Am Enfermagem. (2013) 21:1203–11. doi: 10.1590/0104-1169.2990.2355
35. Oaks T, Delhi N. Perceptions of mental and physical illnesses in North-western. J Health Psychol. (1999) 4:531–49. doi: 10.1177/135910539900400407
36. Kerebih H. Pattern of help-seeking behavior for common mental disorders among urban residents in Southwest Ethiopia. Qual Prim Care. (2017) 25:208–16.
37. Rijal A. Mental health situation in Nepal and priorities for interventions. Heal Prospect J Public Health. (2018) 17:10–2. doi: 10.3126/hprospect.v17i1.19662
38. Alem A, Desta M, Araya M. Mental health in Ethiopia EPHA expert group report. Ethiop J Heal Dev. (1995) 9:47–62.
39. Negash A, Alem A, Kebede D, Deyessa N, Shibre T, Kullgren G. Prevalence and clinical characteristics of bipolar I disorder in Butajira, Ethiopia : a community-based study. J Affect Disord. (2005) 87:193–201. doi: 10.1016/j.jad.2005.03.011
40. Federal Democratic Republic of Ethiopia Central Statistical Agency. Population Projection of Ethiopia for all Regions at Wereda Level from 2014–2017. Addis Ababa: CSA (2013).
42. Zikargae MH. Covid-19 in Ethiopia: assessment of how the Ethiopian government has executed administrative actions and managed risk communications and community engagement. Risk Manag Healthc Policy. (2020) 13:2803–10. doi: 10.2147/RMHP.S278234
43. Sambo L, Chatora R, Goosen E. Tools for Assessing the Operationality of District Health Systems. Geneva: WHO (2003) 1–112p.
44. Sheehan D, Janavs J, Baker R, Harnett-Sheehan K, Knapp E, Sheehan M, et al. Mini International Neuropsychiatric Interview Version 5.0.0 DSM-IV. (2006).
45. Sheehan DV, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, et al. The validity of the mini international neuropsychiatric interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. (1997) 12:232–41. doi: 10.1016/S0924-9338(97)83297-X
46. De Azevedo Marques JM, Zuardi AW. Validity and applicability of the mini international neuropsychiatric interview administered by family medicine residents in primary health care in Brazil. Gen Hosp Psychiatry. (2008) 30:303–10. doi: 10.1016/j.genhosppsych.2008.02.001
47. Lecrubier Y, Sheehan D V, Weiller E, Amorim P, Bonora I, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. (1997) 12:224–31. doi: 10.1016/S0924-9338(97)83296-8
48. Denur M, Tesfaw G, Yohannis Z. The magnitude and correlates of common mental disorder among outpatient medical patients in Ethiopia : an institution-based cross-sectional study. BMC Res Notes. (2019) 12:360. doi: 10.1186/s13104-019-4394-x
49. Haro JM, Palacín C, Vilagut G, Martínez M, Bernal M, Luque I, et al. Prevalence of mental disorders and associated factors: results from the ESEMeD-Spain study. Med Clin. (2006) 126:445–51. doi: 10.1157/13086324
50. Liu SI, Prince M, Blizard B, Mann A. The prevalence of psychiatric morbidity and its associated factors in general health care in Taiwan. Psychol Med. (2001) 32:629–37. doi: 10.1017/S0033291701005074
51. Bitew T. Prevalence and risk factors of depression in Ethiopia: a review. Ethiop J Health Sci. (2014) 24:161–9. doi: 10.4314/ejhs.v24i2.9
52. Silva MT, Galvao TF, Martins SS, Pereira MG. Prevalence of depression morbidity among Brazilian adults: a systematic review and meta-analysis. Rev Bras Psiquiatr. (2014) 36:262–70. doi: 10.1590/1516-4446-2013-1294
53. Molla GL, Sebhat HM, Hussen ZN, Mekonen AB, Mersha WF, Yimer TM. Depression among Ethiopian adults: cross-sectional study. Psychiatry J. (2016) 2016:1468120. doi: 10.1155/2016/1468120
54. Cheruvu VK, Chiyaka ET. Prevalence of depressive symptoms among older adults who reported medical cost as a barrier to seeking health care: findings from a nationally representative sample. BMC Geriatr. (2019) 19:192. doi: 10.1186/s12877-019-1203-2
55. World Health Organization. Depression and Other Common Mental Disorders Global Health Estimates. Geneva: WHO (2017).
56. Khasakhala LI, Ndetei DM, Mutiso V, Mbwayo AW, Mathai M. The prevalence of depressive symptoms among adolescents in Nairobi public secondary schools: association with perceived maladaptive parental behavior. Afr J Psychiatry. (2012) 15:106–13. doi: 10.4314/ajpsy.v15i2.14
57. Gruebner O, Rapp MA, Adli M, Kluge U, Galea SHA. Cities and mental health. Dtsch Arztebl Int. (2017) 114:121–7. doi: 10.3238/arztebl.2017.0121
58. Galea S, Ahern J, Rudenstine S, Wallace Z, Vlahov D. Urban built environment and depression: a multilevel analysis. J Epidemiol Community Health. (2005) 59:822–7. doi: 10.1136/jech.2005.033084
59. Judd LL, Akiskal HS. The prevalence and disability of bipolar spectrum disorders in the US population : re-analysis of the ECA database taking into account subthreshold cases. J Affect Disord. (2003) 73:123–31. doi: 10.1016/S0165-0327(02)00332-4
60. Teferra S, Hanlon C, Alem A, Jacobsson L. Khat chewing in persons with severe mental illness in Ethiopia: a qualitative study exploring perspectives of patients and caregivers. Transcult Psychiatry. (2011) 48:455–72. doi: 10.1177/1363461511408494
61. Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. (2013) 43:897–910. doi: 10.1017/S003329171200147X
62. Madasu S, Malhotra S, Kant S, Sagar R, Mishra AK, Misra P, et al. Anxiety disorders among adolescents in a rural area of Northern India using screen for child anxiety-related emotional disorders tool: a community-based study. Indian J Community Med. (2019) 44:317–21. doi: 10.4103/ijcm.IJCM_359_18
63. Crick Lunda, Alison Breena, Alan J, Flishera, Ritsuko Kakumab, Joanne Corrigalla, John A, Joskaa LS, et al. Poverty and common mental disorders in low and middle-income countries: a systematic review. Soc Sci Med. (2010) 7:517–28. doi: 10.1016/j.socscimed.2010.04.027
64. Kebede D, Alem A. Suicide attempts and ideation among adults in Addis Ababa, Ethiopia. Acta Psychiatr Scand Suppl. (1999) 397:35–9. doi: 10.1111/j.1600-0447.1999.tb10692.x
65. Fekadu A, Medhin G, Selamu M, Hailemariam M, Alem A, Giorgis TW, et al. Population level mental distress in rural Ethiopia. BMC Psychiatry. (2014) 14:194. doi: 10.1186/1471-244X-14-194
66. Adewuya AO, Ola BA, Coker OA, Atilola O, Zachariah MP, Olugbile O, et al. Prevalence and associated factors for suicidal ideation in the Lagos state mental health survey, Nigeria. BJPsych Open. (2016) 2:385–9. doi: 10.1192/bjpo.bp.116.004333
67. Zhang J, Stewart R, Phillips M, Shi Q, Prince M. Pesticide exposure and suicidal ideation in rural communities in Zhejiang province, China. Bull World Health Organ. (2009) 87:745–53. doi: 10.2471/blt.08.054122
68. Botega NJ, De Azevedo Barros MB, De Oliveira HB, Dalgalarrondo P, Marín-León L. Suicidal behavior in the community: prevalence and factors associated with suicidal ideation. Rev Bras Psiquiatr. (2005) 27:45–53. doi: 10.1590/S1516-44462005000100011
69. Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. National Research Council. Reducing Suicide: A National Imperative. Washingdon, DC: National Academies Press (2002) 516p.
70. Luni FK, Ansari B, Jawad A, Dawson A, Baig SM. Prevalence of depression and anxiety in a village in Sindh. J Ayub Med Coll Abbottabad. (2009) 21:68–72.
71. Mirowsky J, Ross CE. Education, personal control, lifestyle, and health: a human capital hypothesis. Res Aging. (1998) 20:415–49. doi: 10.1177/0164027598204003
72. Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med. (2008) 66:1334–45. doi: 10.1016/j.socscimed.2007.12.019
73. De Vaus J, Hornsey MJ, Kuppens P, Bastian B. Exploring the east-west divide in prevalence of affective disorder: a case for cultural differences in coping with negative emotion. Personal Soc Psychol Rev. (2018) 22:285–304. doi: 10.1177/1088868317736222
74. Risal A, Tharoor H. Birth order, and psychopathology. J Fam Med Prim Care. (2012) 1:137–40. doi: 10.4103/2249-4863.104985
75. Elalky MI, Abed Z, Othman E, Eita LH. The effect of birth order and socio-demographic characteristics on anxiety and depression among adolescents. Int J Nurs Sci. (2015) 5:110–21. doi: 10.5923/j.nursing.20150503.04
76. Zaidi S. Birth Order and Its Effect on Depression in Adults. New Jersey, NJ: Rowan Digital Works (2011).
77. Volling BL. Family transitions following the birth of a sibling: an empirical review of changes in the firstborn's adjustment. Psychol Bull. (2012) 138:497–528. doi: 10.1037/a0026921
78. Malzberg B. Mental disease in relation to economic status. J Nerv Ment Dis. (1956) 123:257–61. doi: 10.1097/00005053-195603000-00006
79. Verdoux H, Bourgeois M. Social class in unipolar and bipolar probands and relatives. J Affect Disord. (1995) 33:181–7. doi: 10.1016/0165-0327(94)00087-P
80. Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. (2020) 370. doi: 10.3386/w27157
81. Mokona H, Yohannes K, Ayano G. Youth unemployment and mental health: prevalence and associated factors of depression among unemployed young adults in Gedeo zone, Southern Ethiopia. Int J Ment Health Syst. (2020) 14:61. doi: 10.1186/s13033-020-00395-2
83. Richardson T, Jansen M, Fitch C. Financial difficulties in bipolar disorder part 1: longitudinal relationships with mental health. J Ment Health. (2018) 27:595–601. doi: 10.1080/09638237.2018.1521920
84. Finseth PI, Morken G, Malt UF, Andreassen OA, Vaaler AE. Risk factors of cycle acceleration in acutely admitted patients with bipolar disorder. Acta Psychiatr Scand. (2014) 130:388–96. doi: 10.1111/acps.12308
85. Klonoff EA, Landrine H, Ullman JB. Racial discrimination and psychiatric symptoms among Blacks. In: Cultural Diversity and Ethnic Minority Psychology. Vol. 5. California: Educational Publishing Foundation (1999). p. 329–39. doi: 10.1037/1099-9809.5.4.329
86. José A. Soto NAD-AB. The relationship between perceived discrimination and generalized anxiety disorder among African Americans, Afro Caribbeans, and non-hispanic whites. J Anxiety Disord. (2011) 25:258–65. doi: 10.1016/j.janxdis.2010.09.011
87. Williams DR, Lawrence JA, Davis BA, Cecilia MPH. Understanding how discrimination can affect health. Heal Serv Res. (2019) 54:1374–88. doi: 10.1111/1475-6773.13222
88. Yusuf S. Drivers of Ethnic Conflict in Contemporary Ethiopia. Addis Ababa: Institue for Security Studies. (2019).
89. Tummala-Narra P, Li Z, Liu T, Wang Y. Violence exposure and mental health among adolescents: the role of ethnic identity and help-seeking. Psychol Trauma Theory, Res Pract Policy. (2014) 6:8–24. doi: 10.1037/a0032213
90. Lander L, Howsare J, Byrne M. The impact of substance use disorders on families and children: from theory to practice. Soc Work Public Health. (2013) 28:194–205. doi: 10.1080/19371918.2013.759005
91. Necho M, Belete A, Tsehay M, Zenebe Y. A meta-analysis of depressive symptoms among Ethiopian prisoners and a narrative description of its associated factors: a country based systematic review and meta-analysis study. BMC Psychiatry. (2020) 20:281. doi: 10.1186/s12888-020-02662-5
92. Atnafie SA, Muluneh NY, Getahun KA, Woredekal AT, Kahaliw W. Depression, anxiety, stress, and associated factors among khat chewers in Amhara region, Northwest Ethiopia. Depress Res Treat. (2020) 2020:7934892. doi: 10.1155/2020/7934892
93. Yeshaw Y, Mossie A. Depression, anxiety, stress, and their associated factors among Jimma university staff, Jimma, Southwest Ethiopia, 2016: a cross-sectional study. Neuropsychiatr Dis Treat. (2017) 13:2803–12. doi: 10.2147/NDT.S150444
94. Kebede MA, Anbessie B, Ayano G. Prevalence and predictors of depression and anxiety among medical students in addis. Int J Ment Health Syst. (2019) 13:30. doi: 10.1186/s13033-019-0287-6
95. Deyessa N, Berhane Y, Alem A, Hogberg U, Kullgren G. Depression among women in rural Ethiopia as related to socioeconomic factors: a community-based study on women in reproductive age groups. Scand J Public Health. (2008) 36:589–97. doi: 10.1177/1403494808086976
96. Tesfaye Y, Agenagnew L. Antenatal depression and associated factors among pregnant women attending antenatal care service in Kochi health center, Jimma town, Ethiopia. J Pregnancy. (2021) 2021:5047432. doi: 10.1155/2021/5047432
97. Bitew T, Hanlon C, Kebede E, Honikman S, Fekadu A. Antenatal depressive symptoms and perinatal complications: a prospective study in rural Ethiopia. BMC Psychiatry. (2017) 17:301. doi: 10.1186/s12888-017-1462-4
98. Fantahun A, Cherie A, Deribe L. Clinical practice & epidemiology in prevalence and factors associated with postpartum depression among mothers attending public health centers of Addis Ababa, Ethiopia, 2016. Clin Pract Epidemiol Ment Health. (2018) 14:196–206. doi: 10.2174/1745017901814010196
99. Ashenafi Y, Kebede D, Desta M, Alem A. Prevalence of mental and behavioral disorders in Ethiopian children. East Afr Med J. (2001) 78:308–11. doi: 10.4314/eamj.v78i6.9024
100. Berihun F. Prevalence and correlates of anxiety and depression among cancer patients in the University of Gondar comprehensive specialized hospital, Northwest Ethiopia. Arch Depress Anxiety. (2017) 3:042–8. doi: 10.17352/2455-5460.000022
101. Duko B, Toma A, Asnake S, Abraham Y. Depression, anxiety and their correlates among patients with HIV in South Ethiopia: an institution-based cross-sectional study. Front Psychiatry. (2019) 10:290. doi: 10.3389/fpsyt.2019.00290
102. Aberha M, Gebeyehu A. Prevalence and factors associated with anxiety among patients with hypertension on follow up at Menelik-II referral hospital, Addis Ababa Ethiopia. J Psychiatry. (2016) 19(4). doi: 10.4172/2378-5756.1000378
103. Mohammedhussein M, Alenko A, Tessema W, Mamaru A. Prevalence and associated factors of depression and anxiety among patients with pulmonary tuberculosis attending treatment at public health facilities in southwest Ethiopia. Neuropsychiatr Dis Treat. (2020) 16:1095–104. doi: 10.2147/NDT.S249431
104. Tegegne MT, Mossie TB, Awoke AA, Assaye AM, Gebrie BT, Eshetu DA. Depression and anxiety disorder among epileptic people at amanuel specialized mental hospital, Addis Ababa, Ethiopia. BMC Psychiatry. (2015) 15:210. doi: 10.1186/s12888-015-0589-4
105. Awas M, Kebede D, Alem A. Major mental disorders in Butajira, southern Ethiopia. Acta Psychiatr Scand Suppl. (1999) 397:56–64. doi: 10.1111/j.1600-0447.1999.tb10695.x
106. Kebede D, Alem A. Major mental disorders in Addis Ababa, Ethiopia. III. Neurotic and somatoform disorders. Acta Psychiatr Scand Suppl. (1999) 397:24–9. doi: 10.1111/j.1600-0447.1999.tb10690.x
Keywords: mood symptoms, anxiety symptoms, suicide, community, Jimma, Ethiopia
Citation: Tesfaye Y, Agenagnew L, Anand S, Tucho GT, Birhanu Z, Ahmed G, Getnet M and Yitbarek K (2021) Mood Symptoms, Suicide, and Associated Factors Among Jimma Community. A Cross-Sectional Study. Front. Psychiatry 12:640575. doi: 10.3389/fpsyt.2021.640575
Received: 11 December 2020; Accepted: 12 February 2021;
Published: 19 March 2021.
Edited by:
Xenia Gonda, Semmelweis University, HungaryReviewed by:
Su-Jeong Seong, Kangdong Sacred Heart Hospital, South KoreaMaayan Shorer, Ruppin Academic Center, Israel
Isabella Berardelli, Sapienza University of Rome, Italy
Copyright © 2021 Tesfaye, Agenagnew, Anand, Tucho, Birhanu, Ahmed, Getnet and Yitbarek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yonas Tesfaye, eW9uYXN0ZXNmYXllNzFAeWFob28uY29t
 Yonas Tesfaye
Yonas Tesfaye Liyew Agenagnew
Liyew Agenagnew Susan Anand2
Susan Anand2 Gudina Terefe Tucho
Gudina Terefe Tucho Masrie Getnet
Masrie Getnet Kiddus Yitbarek
Kiddus Yitbarek