- 1Research Division, Institute of Mental Health, Singapore, Singapore
- 2Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
- 3School of Electrical and Electronic Engineering, Nanyang Technological University, Singapore, Singapore
- 4Department of Occupational Therapy, Institute of Mental Health, Singapore, Singapore
- 5Health and Social Sciences, Singapore Institute of Technology, Singapore, Singapore
- 6Department of Psychosis, Institute of Mental Health, Singapore, Singapore
Neurocognition and functional capacity are commonly reported predictors of real-world functioning in schizophrenia. However, the additional impact of negative symptoms, specifically its subdomains, i.e., diminished expression (DE) and avolition-apathy (AA), on real-world functioning remains unclear. The current study assessed 58 individuals with schizophrenia. Neurocognition was assessed with the Brief Assessment of Cognition in Schizophrenia, functional capacity with the UCSD Performance-based Skills Assessment (UPSA-B), and negative symptoms with the Negative Symptom Assessment-16. Real-world functioning was assessed with the Multnomah Community Ability Scale (MCAS) with employment status as an additional objective outcome. Hierarchical regressions and sequential logistic regressions were used to examine the associations between the variables of interest. The results show that global negative symptoms contribute substantial additional variance in predicting MCAS and employment status above and beyond the variance accounted for by neurocognition and functional capacity. In addition, both AA and DE predict the MCAS after controlling for cognition and functional capacity. Only AA accounts for additional variance in employment status beyond that by UPSA-B. In summary, negative symptoms contribute substantial additional variance in predicting both real-world functioning and employment outcomes after accounting for neurocognition and functional capacity. Our findings emphasize both DE and AA as important treatment targets in functional recovery for people with schizophrenia.
Introduction
Schizophrenia is a potentially debilitating condition that causes functional decline, impeding an individual's ability to live an independent and fulfilling life. Functional recovery has been an important treatment goal (1), and interest in exploring factors influencing functioning has grown (2, 3).
One of the most robust findings is the association between neurocognition and real-world functioning (4–7), which has been supported in both cross-sectional and longitudinal studies (8, 9). Functional capacity, an objective measurement of an individual's ability to perform tasks that are needed in everyday life, has also been found to be associated with real-world functioning (10–13) and at least partially mediate the relationship between neurocognition and real-world functioning (7, 14–19).
A meta-analysis found negative symptoms to be significantly associated with functioning and mediate the relationship between neurocognition and functional outcome (20). Negative symptoms, a core feature of schizophrenia, are also shown to negatively impact real-world functioning in areas such as work performance, everyday living, and social functioning (13, 21, 22). However, the role of negative symptoms in predicting real-world functioning beyond neurocognition and functional capacity remains unclear. Some studies find its unique contribution in predicting real-world functioning, which is independent of neurocognition (23) and functional capacity (15, 19, 24–26), and some studies find no additional influence on real-world functioning (14, 15).
Furthermore, the current conceptualization of negative symptoms comprises two distinct subdomains: diminished expression (DE), consisting of blunted affect and alogia, and avolition-apathy (AA), which includes amotivation, asociality, and anhedonia (27–31). These two subdomains may have different impacts on real-world functioning (32, 33), but their additional contributions to real-world functioning above and beyond neurocognition and functional capacity have not been well-studied.
Therefore, the aim of the present study was to examine the relative contributions of neurocognition, functional capacity, and negative symptoms on real-world functioning. Additionally, we examined employment to provide another perspective of real-world functioning. We hypothesized that negative symptoms, specifically its subdomains of DE and AA, might have unique contributions to real-world functioning and employment in schizophrenia.
Materials and Methods
Participants
Fifty-eight community-dwelling individuals aged between 20 and 51 and diagnosed with schizophrenia were recruited from the outpatient clinics at the Institute of Mental Health, Singapore. The diagnosis was ascertained using the Structured Clinical Interview for DSM-IV (34). The exclusion criteria were as follows: a history of stroke, traumatic brain injury, and neurological disorders such as epilepsy. Ethics approval for the study was granted by the National Healthcare Group's Domain Specific Review Board (Singapore). Written informed consent was obtained from all participants after the study procedures were fully explained.
Assessments
Neurocognition
Neurocognition was assessed using the Brief Assessment of Cognition in Schizophrenia (BACS), a well-established neuropsychological battery used to evaluate cognitive functioning, including verbal memory and learning, working memory, psychomotor function, verbal fluency, and executive function in patients with schizophrenia (35). A composite Z-score was calculated for subsequent analysis (36).
Functional Capacity
The UCSD Performance-Based Skills Assessment-Brief (UPSA-B) (37) was used to assess participants' capacity to perform skills necessary in daily life with tangible props to simulate real-world tasks. The UPSA-B demonstrates adequate psychometric properties, which is close to the full version of the UPSA, and consists of two of the five subscales from the full UPSA (12): (a) financial skills and (b) communication skills.
Negative Symptoms
Negative symptoms were evaluated using the Negative Symptom Assessment-16 (NSA-16), which assesses the negative symptoms of schizophrenia comprising of five factors: communication, emotion/affect, social involvement, motivation, and retardation (38). The AA score was calculated by the sum of motivation and social involvement domain scores; DE score was obtained by the sum of communication and emotion/affect domain scores (39).
Real-World Functioning
Real-world functioning was assessed using the Multnomah Community Ability Scale (MCAS) (40, 41), a 17-item, clinician-rated tool that is used to evaluate broad dimensions of community functioning. The MCAS was the most frequently nominated scale of real-world outcome in the Validation of Everyday Real-World Outcomes (VALERO) in Schizophrenia project and is often used in the evaluation of community mental health interventions (42, 43).
Participant's employment status in the past 1 month was collected via self-report. It was initially recorded in three categories: unemployed, sheltered employment, and non-sheltered employment. Considering that the sheltered employment was non-competitive employment, this category was combined with the unemployed category. A binary variable (employed vs. unemployed) was created for analyses.
Data Analysis
Prior to conducting any analysis, normality assumption was checked and satisfied for all continuous variables. Bivariate correlations between neurocognition, functional capacity, negative symptoms, AA, DE, and real-world functioning were performed using Pearson's correlation.
Demographic variables, including age, gender, and years of education, were individually examined in univariate regressions as a predictor of MCAS; none of them were significant and were excluded in the subsequent analysis as covariates. To test whether negative symptoms would explain additional variance in real-world functioning indexed by MCAS above and beyond the variance explained by neurocognition and functional capacity, hierarchical multiple regression was performed as follows: BACS was entered into the model in step one, followed by UPSA-B in step two. The NSA-16 total was entered in the final step. To examine which negative symptom subdomains influence real-world functioning, AA and DE were entered in the multiple regression model together with BACS and UPSA-B. Collinearity was checked for all multiple regression analysis.
For selecting predictors of employment status, demographic variables (i.e., age, gender, and years of education), neurocognition (BACS), functional capacity (UPSA-B), and negative symptom variables (NSA-16 total, AA and DE) were individually examined in univariate logistic regression. All demographic variables and neurocognition were not significant predictors of employment; hence, they were excluded in the subsequent analysis. Two sequential binary logistic regressions were conducted to assess whether negative symptoms or its subdomains would add unique variance in predicting employment status in addition to the variance explained by functional capacity. In both logistic regressions, functional capacity (UPSA-B) was entered in step 1 and then followed by either negative symptom (NSA-16 total score) or negative symptom subdomains (AA and DE) in step 2.
The p-values reported in this study are not adjusted for multiple comparisons because the analyses were planned and conducted in stages to test the hypothesis that negative symptoms and its subdomains may have unique contributions to real-world functioning and employment in schizophrenia. In addition, corrections might increase the likelihood of type II error (44–46). All analyses were performed with IBM SPSS Statistics for Windows, Version 25.0.
Results
Sample Characteristics
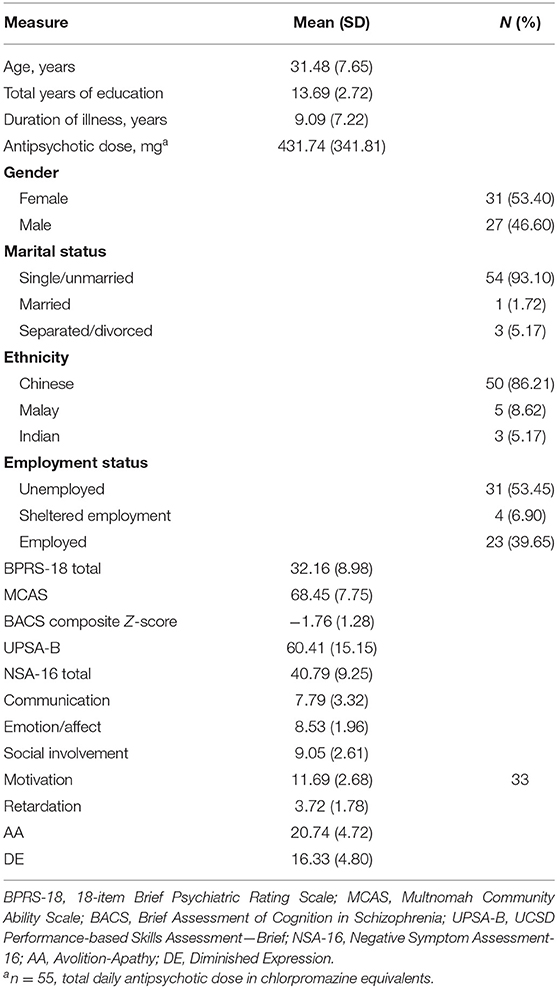
The sample characteristics are reported in Table 1. Three participants were not prescribed an antipsychotic at the time of assessment.
Correlations Among Cognition, Functional Capacity, Negative Symptoms, and Real-World Functioning
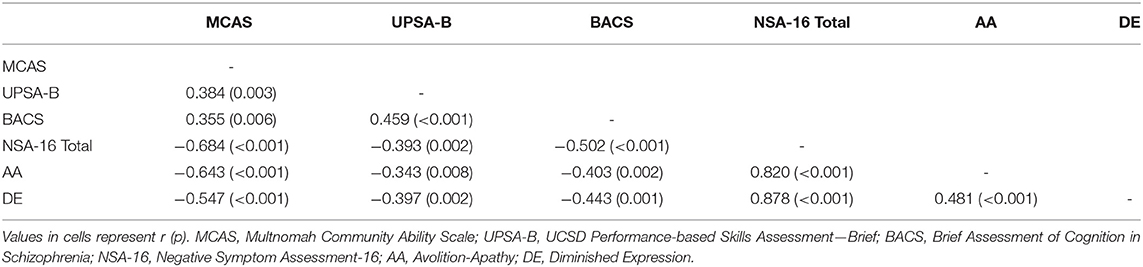
Bivariate intercorrelations among the measures are presented in Table 2. As expected, there was a moderate correlation between BACS and UPSA-B. MCAS was moderately correlated to both BACS and UPSA-B and inversely correlated to NSA-16.
Association With Real-World Functioning
As shown in Table 3, BACS alone significantly predicted MCAS, F(1, 56) = 8.098, p = 0.006, accounting for 11% of the variance. After including UPSA-B in the model, the total variance accounted for significantly increased to 16% (p for F change = 0.045), and UPSA-B became the only significant predictor, F(2, 55) = 6.382, p = 0.003. When the NSA-16 total score was added to the model, it was the only significant predictor and contributed an additional 30% variance in predicting MCAS. With all three predictors in the equation, the total variance accounted for reached 46%, F(3, 54) = 16.916, p < 0.001.
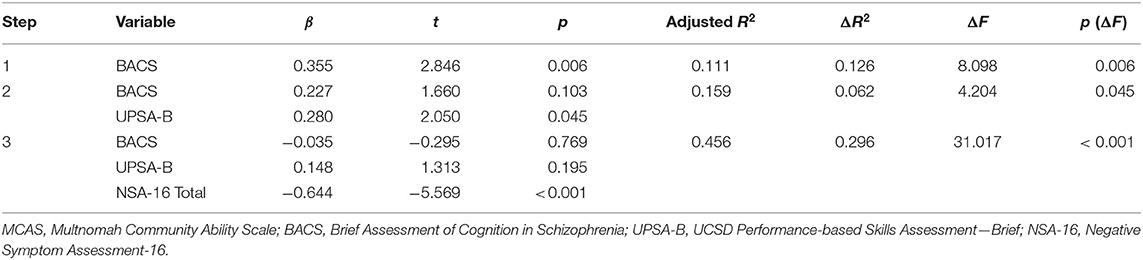
Table 3. Hierarchical regression analysis for variables predicting real-world functioning indexed by MCAS.
When AA and DE were entered into the multiple regression model together with BACS and UPSA-B scores to predict MCAS, a total of 46% of variance was explained, F(4, 53) = 13.140, p < 0.001; R2 = 0.498. Both negative subdomains (i.e., AA and DE) were significant predictors, while BACS and UPSA-B were not (Table 4).
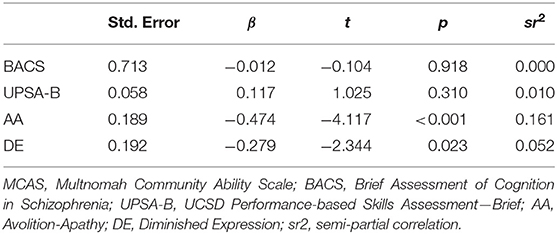
Table 4. Multiple regression analysis for variables predicting real-world functioning indexed by MCAS.
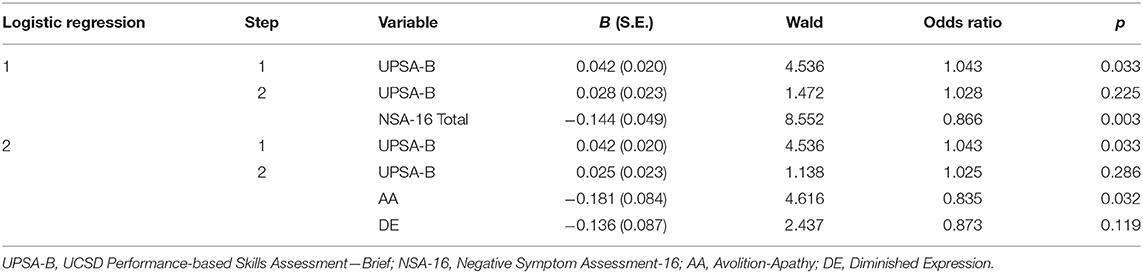
Association With Employment
In the first sequential logistic regression, the likelihood ratio test of block 1 was significant when UPSA-B was the only predictor, χ2 (df = 1) = 5.030, p = 0.025. After adding the NSA-16 total score in step 2, the likelihood ratio test was significant, χ2 (df = 2) = 16.611, p < 0.001, and the deviance in employment accounted for was substantial, Nagelkerke R2 = 0.337. Comparison of likelihood ratios for models with and without the NSA-16 total score showed significant improvement with the addition of the NSA-16 total, χ2 (df = 1) = 11.582, p = 0.001. UPSA-B became a non-significant predictor in step 2, while a significant predictive effect of the negative symptom total score on employment status was observed.
In the second sequential logistic regression, AA and DE were entered into the model in step 2 following UPSA-B in step 1. The likelihood ratio test was significant for the final model, χ2 (df = 3) = 16.399, p = 0.001, with significant improvement made by AA and DE, χ2 (df = 2) = 11.370, p = 0.003. AA was the only significant predictor of employment status (Table 5).
Discussion
In this study, we investigated the additional influence of negative symptoms on real-world functioning indexed by both clinician-rated functioning scale and employment status after controlling for the effect of neuro cognition and functional capacity. We found that negative symptoms contributed a unique and substantial amount of variance to real-world functioning in people with schizophrenia.
In the present study, negative symptoms appear to be a key predictor of real-world functioning. Neurocognition and functional capacity became non-significant predictors of real-world functioning after negative symptoms were added in the model. This result is in contrast to previous studies, which attributed a large proportion of variance of real-world functioning to neurocognition and functional capacity (4, 11). On the other hand, there are studies supporting our findings. Vesterager et al. (47) found that only negative symptoms significantly predicted overall functioning and UPSA-B did not account for additional variance in real-world outcomes beyond that accounted for by negative symptoms. Negative symptoms, not UPSA, were consistently identified as useful predictors in areas of useful activities, self-care, and relationships (26).
Additionally, both AA and DE were significantly associated with real-world functioning after controlling for cognition and functional capacity. This is in contrast to previous reports that DE has no additional predictive value after controlling for AA (32, 48, 49). One recent study found amotivation to mediate the association between neurocognition and social functioning in individuals with psychotic disorder although DE had no such mediating effect (50). Meanwhile, we found that AA had a larger impact compared with DE (AA: SR2 = 0.161; DE SR2 = 0.052). This is congruent with previous reports that AA, especially avolition, has a better predictive ability for functioning than DE (48, 51–54).
The result for employment status was similar to that for MCAS. Functional capacity was significantly associated with employment status; however, when negative symptoms were added, the model improved substantially, and functional capacity was no longer a significant predictor. This result is in part supported by a previous finding that patients who were employed scored significantly higher on the UPSA-B than those who were not employed, but the effect was attenuated after including symptoms of psychosis (55).
In our study, AA was the key negative symptom domain associated with employment. The effects of AA and DE on employment is mixed in previous studies. Liemburg et al. (50) reported amotivation mediated the association between cognition and employment status in patients with recent onset psychotic illness although DE mediated the relationship in a longer illness duration cohort. Strauss et al. (51) reported that patients with AA symptoms were less likely to be gainfully employed and less likely to complete high-quality work than patients with DE symptoms. In line with our result, Ang et al. (56) showed that AA, not DE, was significantly associated with employment status, but the impact of neurocognition or functional capacity was not considered in their study.
Heterogeneity of negative symptoms and functional outcome, various measurement tools adopted, and different sample characteristics may account for the divergent findings regarding the relationship between negative symptoms, cognition, functional capacity, and functional outcome. A majority of past studies used a general psychiatric symptoms scale, such as the Positive and Negative Syndrome Scale (PANSS) (57), to assess negative symptoms, which may not capture all aspects of the construct of negative symptoms. Therefore, the impact of negative symptoms might have been underestimated.
One main strength of this study is that the functional outcomes were indexed by both interviewer-rated functioning level and employment status, an important and pragmatic functional milestone. In some previous studies, employment was indexed by scale ratings on functioning and not objectively collected employment status (16). Functional milestones may not be captured by global scores on everyday functioning scales (58). In addition, the accuracy of the ratings of patients' functioning level might be compromised by patients' poor insight (59), impaired cognitive function, and the presence of psychiatric symptoms (60). In contrast, functional milestones, such as employment status, allow for greater objectivity in assessing an important aspect of real-world functioning.
Some limitations of the study should be mentioned. First, this study had a relatively small sample size with slightly more females than males, which may impact the generalization of the results. Nevertheless, our findings appear consistent with related reports and lend weight to the substantive influence of negative symptoms on real-world functioning. In addition, our study found no effect of gender on real-world functioning and employment status. Second, NSA-16 covers four out of five subdomains of negative symptoms, i.e., blunted affect, alogia, asociality, and avolition, with anhedonia not addressed (39). Although missing the portion on anhedonia, AA still emerged as a strong predictor of real-world functioning in our study. The strong association seen between real-world functioning and AA could be partly due to overlapping behaviors assessed between the measurement scales, a common challenge faced by studies assessing negative symptoms based on behavioral information. However, our study had employment as an alternate outcome, which showed AA's consistent and significant influence across both measures of real-world functioning. Third, the specific impact of negative symptom subdomains on real-world functioning may vary depending on duration of the psychotic illness and the types of functioning, such as independent living, social functioning and occupational functioning (50). The current study evaluated only the overall functioning and employment status in a group of patients with an average 9-year duration of illness. More studies are needed to examine the specific effect of subdomain of negative symptoms on different functioning outcomes with the illness duration considered. Last, this study measured real-world functioning and employment attainment cross-sectionally. Future studies could examine how changes in AA or DE influence real-functioning changes or job tenure (61).
The current study shows a robust influence of both AA and DE on real-world functioning. The results highlight the importance of negative symptoms as unmet treatment needs, especially in the area of functional recovery. Psychiatric rehabilitation programs would do well to go beyond cognitive remediation and skills retraining to address negative symptoms, such as avolition and apathy to maximize an individual's chance at community integration and employment. Future research efforts should focus on addressing and ameliorating negative symptoms in individuals with schizophrenia.
Data Availability Statement
The datasets generated in this article are not readily available because some participants do not allow the data from this study to be used in other research or transferred to other researchers. Requests to access the datasets should be directed to Jimmy Lee, amltbXlfbGVlJiN4MDAwNDA7aW1oLmNvbS5zZw==.
Ethics Statement
The studies involving human participants were reviewed and approved by National Healthcare Group's Domain Specific Review Board, Singapore. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
ZY, JL, BT, and JD designed the study and were responsible for the project management. JL, BT, and JD obtained funding. ZY, SL, and JL performed the statistical analysis and drafted the manuscript. ZY, NA, and YS recruited participants and collected the data. All authors gave feedback on the first draft of the manuscript and approved the submitted manuscript.
Funding
This study was supported by research grants from the Singapore Ministry of Health's National Medical Research Council Center Grant (Grant No. NMRC/CG/004/2013) and Nanyang Institute of Technology in Health and Medicine Seed Fund (Grant No. M4081187.E30).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to express their sincere gratitude to Dr. Gurpreet Rekhi who trained and supervised research psychologists in conducting clinical assessments and all of the participants who participated in this study.
References
1. Kern RS, Glynn SM, Horan WP, Marder SR. Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull. (2009) 35:347–61. doi: 10.1093/schbul/sbn177
2. Lahera G, Galvez JL, Sanchez P, Martinez-Roig M, Perez-Fuster JV, Garcia-Portilla P, et al. Functional recovery in patients with schizophrenia: recommendations from a panel of experts. BMC Psychiatry. (2018) 18:176. doi: 10.1186/s12888-018-1755-2
3. Bechi M, Bosia M, Spangaro M, Buonocore M, Cavedoni S, Agostoni G, et al. Exploring functioning in schizophrenia: predictors of functional capacity and real-world behaviour. Psychiatry Res. (2017) 251:118–24. doi: 10.1016/j.psychres.2017.02.019
4. Bowie CR, Harvey PD. Cognitive deficits and functional outcome in schizophrenia. Neuropsychiatr Dis Treat. (2006) 2:531–6. doi: 10.2147/nedt.2006.2.4.531
5. Fu S, Czajkowski N, Rund BR, Torgalsboen AK. The relationship between level of cognitive impairments and functional outcome trajectories in first-episode schizophrenia. Schizophr Res. (2017) 190:144–9. doi: 10.1016/j.schres.2017.03.002
6. Helldin L, Mohn C, Olsson A-K, Hjärthag F. Neurocognitive variability in schizophrenia spectrum disorders: relationship to real-world functioning. Schizophr Res Cognit. (2020) 20:100172. doi: 10.1016/j.scog.2020.100172
7. Nuechterlein KH, Subotnik KL, Green MF, Ventura J, Asarnow RF, Gitlin MJ, et al. Neurocognitive predictors of work outcome in recent-onset schizophrenia. Schizophr Bull. (2011) 37:S33–40. doi: 10.1093/schbul/sbr084
8. Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. (2000) 26:119–36. doi: 10.1093/oxfordjournals.schbul.a033430
9. Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. (2004) 72:41–51. doi: 10.1016/j.schres.2004.09.009
10. Szabo S, Merikle E, Lozano-Ortega G, Powell L, Macek T, Cline S. Assessing the relationship between performance on the University of California performance skills assessment (UPSA) and outcomes in schizophrenia: a systematic review and evidence synthesis. Schizophr Res Treat. (2018) 2018:9075174. doi: 10.1155/2018/9075174
11. Twamley EW, Doshi RR, Nayak GV, Palmer BW, Golshan S, Heaton RK, et al. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am J Psychiatry. (2002) 159:2013–20. doi: 10.1176/appi.ajp.159.12.2013
12. Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. (2001) 27:235–45. doi: 10.1093/oxfordjournals.schbul.a006870
13. Reichenberg A, Feo C, Prestia D, Bowie CR, Patterson TL, Harvey PD. The course and correlates of everyday functioning in schizophrenia. Schizophr Res Cognit. (2014) 1:e47–52. doi: 10.1016/j.scog.2014.03.001
14. Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, Heaton RK, et al. Predicting schizophrenia patients' real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. (2008) 63:505–11. doi: 10.1016/j.biopsych.2007.05.022
15. Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. (2006) 163:418–25. doi: 10.1176/appi.ajp.163.3.418
16. Fujino H, Sumiyoshi C, Sumiyoshi T, Yasuda Y, Yamamori H, Ohi K, et al. Predicting employment status and subjective quality of life in patients with schizophrenia. Schizophr Res Cognit. (2015) 3:20–5. doi: 10.1016/j.scog.2015.10.005
17. Ho JS, Moore RC, Davine T, Cardenas V, Bowie CR, Patterson TL, et al. Direct and mediated effects of cognitive function with multidimensional outcome measures in schizophrenia: the role of functional capacity. J Clin Exp Neuropsychol. (2013) 35:882–95. doi: 10.1080/13803395.2013.828021
18. Strassnig MT, Raykov T, O'Gorman C, Bowie CR, Sabbag S, Durand D, et al. Determinants of different aspects of everyday outcome in schizophrenia: the roles of negative symptoms, cognition, and functional capacity. Schizophr Res. (2015) 165:76–82. doi: 10.1016/j.schres.2015.03.033
19. Bowie CR, Depp C, McGrath JA, Wolyniec P, Mausbach BT, Thornquist MH, et al. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am J Psychiatry. (2010) 167:1116–24. doi: 10.1176/appi.ajp.2010.09101406
20. Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. (2009) 113:189–99. doi: 10.1016/j.schres.2009.03.035
21. Fulford D, Niendam TA, Floyd EG, Carter CS, Mathalon DH, Vinogradov S, et al. Symptom dimensions and functional impairment in early psychosis: more to the story than just negative symptoms. Schizophr Res. (2013) 147:125–31. doi: 10.1016/j.schres.2013.03.024
22. Erickson M, Jaafari N, Lysaker P. Insight and negative symptoms as predictors of functioning in a work setting in patients with schizophrenia. Psychiatry Res. (2011) 189:161–5. doi: 10.1016/j.psychres.2011.06.019
23. Gonzalez-Blanco L, Garcia-Portilla MP, Dal Santo F, Garcia-Alvarez L, de la Fuente-Tomas L, Menendez-Miranda I, et al. Predicting real-world functioning in outpatients with schizophrenia: role of inflammation and psychopathology. Psychiatry Res. (2019) 280:112509. doi: 10.1016/j.psychres.2019.112509
24. Leifker FR, Bowie CR, Harvey PD. Determinants of everyday outcomes in schizophrenia: the influences of cognitive impairment, functional capacity, and symptoms. Schizophr Res. (2009) 115:82–7. doi: 10.1016/j.schres.2009.09.004
25. Best MW, Gupta M, Bowie CR, Harvey PD. A longitudinal examination of the moderating effects of symptoms on the relationship between functional competence and real world functional performance in Schizophrenia. Schizophr Res Cognit. (2014) 1:90–5. doi: 10.1016/j.scog.2014.03.002
26. Menendez-Miranda I, Garcia-Portilla MP, Garcia-Alvarez L, Arrojo M, Sanchez P, Sarramea F, et al. Predictive factors of functional capacity and real-world functioning in patients with schizophrenia. Eur Psychiatry. (2015) 30:622–7. doi: 10.1016/j.eurpsy.2014.12.011
27. Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. (2006) 32:238–45. doi: 10.1093/schbul/sbj013
28. Liemburg E, Castelein S, Stewart R, van der Gaag M, Aleman A, Knegtering H. Two subdomains of negative symptoms in psychotic disorders: established and confirmed in two large cohorts. J Psychiatr Res. (2013) 47:718–25. doi: 10.1016/j.jpsychires.2013.01.024
29. Strauss GP, Hong LE, Gold JM, Buchanan RW, McMahon RP, Keller WR, et al. Factor structure of the brief negative symptom scale. Schizophr Res. (2012) 142:96–8. doi: 10.1016/j.schres.2012.09.007
30. Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. (2011) 37:300–5. doi: 10.1093/schbul/sbq059
31. Marder SR, Galderisi S. The current conceptualization of negative symptoms in schizophrenia. World Psychiatry. (2017) 16:14–24. doi: 10.1002/wps.20385
32. Rocca P, Montemagni C, Zappia S, Piterà R, Sigaudo M, Bogetto F. Negative symptoms and everyday functioning in schizophrenia: a cross-sectional study in a real world-setting. Psychiatry Res. (2014) 218:284–9. doi: 10.1016/j.psychres.2014.04.018
33. Gur RE, Kohler CG, Ragland JD, Siegel SJ, Lesko K, Bilker WB, et al. Flat affect in schizophrenia: relation to emotion processing and neurocognitive measures. Schizophr Bull. (2006) 32:279–87. doi: 10.1093/schbul/sbj041
34. Association AP. Diagnostic Criteria from DSM-IV-TR. Washington, DC: American Psychiatric Pub (2000).
35. Keefe RSE, Poe M, Walker TM, Harvey PD. The relationship of the brief assessment of cognition in schizophrenia (BACS) to functional capacity and real-world functional outcome. J Clin Exp Neuropsychol. (2006) 28:260–9. doi: 10.1080/13803390500360539
36. Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. (2004) 68:283–97. doi: 10.1037/t38021-000
37. Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull. (2007) 33:1364–72. doi: 10.1093/schbul/sbm014
38. Axelrod BN, Goldman RS, Alphs LD. Validation of the 16-item negative symptom assessment. J Psychiatr Res. (1993) 27:253–8. doi: 10.1016/0022-3956(93)90036-2
39. Daniel DG. Issues in selection of instruments to measure negative symptoms. Schizophr Res. (2013) 150:343–5. doi: 10.1016/j.schres.2013.07.005
40. Barker S, Barron N, McFarland BH, Bigelow DA. A community ability scale for chronically mentally ill consumers: part I. Reliability and validity. Community Ment Health J. (1994) 30:363–83. doi: 10.1007/BF02207489
41. Barker S, Barron N, McFarland BH, Bigelow DA, Carnahan T. A community ability scale for chronically mentally ill consumers: part II. Applications. Community Ment Health J. (1994) 30:459–72. doi: 10.1007/BF02189063
42. Tan BL, Ng WY, Sudhasan J, Chng T, Mok I, Lee J. Factors associated with changes in community ability and recovery after psychiatric rehabilitation: a retrospective study. Community Ment Health J. (2018) 54:1221–7. doi: 10.1007/s10597-018-0249-5
43. Durbin J, Dewa C, Aubry T, Rourke S. The use of multnomah community ability scale as a program evaluation tool. Can J Program Eval. (2004) 19:135–57.
44. Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology (Cambridge, Mass). (1990) 1:43–6. doi: 10.1097/00001648-199001000-00010
45. Perneger TV. What's wrong with Bonferroni adjustments. BMJ. (1998) 316:1236. 10.1136/bmj.316.7139.1236 doi: 10.1136/bmj.316.7139.1236
46. Streiner DL, Norman GR. Correction for multiple testing: is there a resolution? Chest. (2011) 140:16–8. doi: 10.1378/chest.11-0523
47. Vesterager L, Christensen TØ, Olsen BB, Krarup G, Melau M, Forchhammer HB, et al. Cognitive and clinical predictors of functional capacity in patients with first episode schizophrenia. Schizophr Res. (2012) 141:251–6. doi: 10.1016/j.schres.2012.08.023
48. Foussias G, Mann S, Zakzanis KK, van Reekum R, Agid O, Remington G. Prediction of longitudinal functional outcomes in schizophrenia: the impact of baseline motivational deficits. Schizophr Res. (2011) 132:24–7. doi: 10.1016/j.schres.2011.06.026
49. Fervaha G, Foussias G, Agid O, Remington G. Motivational and neurocognitive deficits are central to the prediction of longitudinal functional outcome in schizophrenia. Acta Psychiatr Scand. (2014) 130:290–9. doi: 10.1111/acps.12289
50. Liemburg EJ, Enriquez-Geppert S, Wardenaar KJ, Bruggeman R, Aleman A. Expressive deficits and amotivation as mediators of the associations between cognitive problems and functional outcomes: results from two independent cohorts. Schizophr Res. (2020) 218:283–91. doi: 10.1016/j.schres.2019.12.018
51. Strauss GP, Horan WP, Kirkpatrick B, Fischer BA, Keller WR, Miski P, et al. Deconstructing negative symptoms of schizophrenia: avolition-apathy and diminished expression clusters predict clinical presentation and functional outcome. J Psychiatr Res. (2013) 47:783–90. doi: 10.1016/j.jpsychires.2013.01.015
52. Foussias G, Remington G. Negative symptoms in schizophrenia: avolition and Occam's razor. Schizophr Bull. (2010) 36:359–69. doi: 10.1093/schbul/sbn094
53. Galderisi S, Bucci P, Mucci A, Kirkpatrick B, Pini S, Rossi A, et al. Categorical and dimensional approaches to negative symptoms of schizophrenia: focus on long-term stability and functional outcome. Schizophr Res. (2013) 147:157–62. doi: 10.1016/j.schres.2013.03.020
54. Galderisi S, Rossi A, Rocca P, Bertolino A, Mucci A, Bucci P, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. (2014) 13:275–87. doi: 10.1002/wps.20167
55. Mausbach BT, Harvey PD, Pulver AE, Depp CA, Wolyniec PS, Thornquist MH, et al. Relationship of the brief UCSD Performance-based skills assessment (UPSA-B) to multiple indicators of functioning in people with schizophrenia and bipolar disorder. Bipolar Disord. (2010) 12:45–55. doi: 10.1111/j.1399-5618.2009.00787.x
56. Ang MS, Rekhi G, Lee J. Vocational profile and correlates of employment in people with schizophrenia: the role of avolition. Front Psychiatry. (2020) 11:e00856. doi: 10.3389/fpsyt.2020.00856
57. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
58. Harvey PD, Sabbag S, Prestia D, Durand D, Twamley EW, Patterson TL. Functional milestones and clinician ratings of everyday functioning in people with schizophrenia: overlap between milestones and specificity of ratings. J Psychiatr Res. (2012) 46:1546–52. doi: 10.1016/j.jpsychires.2012.08.018
59. Gould F, Sabbag S, Durand D, Patterson TL, Harvey PD. Self-assessment of functional ability in schizophrenia: milestone achievement and its relationship to accuracy of self-evaluation. Psychiatry Res. (2013) 207:19–24. doi: 10.1016/j.psychres.2013.02.035
60. Sabbag S, Twamley EW, Vella L, Heaton RK, Patterson TL, Harvey PD. Predictors of the accuracy of self assessment of everyday functioning in people with schizophrenia. Schizophr Res. (2012) 137:190–5. doi: 10.1016/j.schres.2012.02.002
Keywords: schizophrenia, real-world functioning, negative symptoms, neurocognition, functional capacity
Citation: Yang Z, Lee SH, Abdul Rashid NA, See YM, Dauwels J, Tan BL and Lee J (2021) Predicting Real-World Functioning in Schizophrenia: The Relative Contributions of Neurocognition, Functional Capacity, and Negative Symptoms. Front. Psychiatry 12:639536. doi: 10.3389/fpsyt.2021.639536
Received: 09 December 2020; Accepted: 08 February 2021;
Published: 19 March 2021.
Edited by:
Ingrid Melle, University of Oslo, NorwayReviewed by:
Anja Vaskinn, Oslo University Hospital, NorwayChristine Mohn, University of Oslo, Norway
Copyright © 2021 Yang, Lee, Abdul Rashid, See, Dauwels, Tan and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jimmy Lee, amltbXlfbGVlJiN4MDAwNDA7aW1oLmNvbS5zZw==
 Zixu Yang
Zixu Yang Soon Hong Lee1,2
Soon Hong Lee1,2 Justin Dauwels
Justin Dauwels Bhing Leet Tan
Bhing Leet Tan Jimmy Lee
Jimmy Lee