
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 26 May 2021
Sec. Schizophrenia
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.631420
This article is part of the Research Topic Insights into the Caregiver Perspective: Involvement, Well-being, and Interventions View all 14 articles
Background: There is a lack of clarity regarding the correlation of caregiving knowledge and skills with caregiving experiences of people living with schizophrenia (PLSs). To address this gap, this comprehensive study examines the relationships of caregiving knowledge and skills to the primary family caregiver's experiences of burden, psychological well-being (stress, anxiety, depression, caregiving rewarding feelings), and coping styles in China.
Methods: A total of 395 primary family caregivers of PLSs were enrolled in a cross-sectional study between May 2019 and September 2019. Each family caregiver was independently assessed on caregiving knowledge and skills, caregiver burden, and psychological well-being, as well as coping styles.
Results: A higher level of caregiving knowledge and skills was positively correlated with less stress (b = −0.48, P < 0.001), anxiety (b = −0.23, P = 0.029), depression (b = −0.29, P = 0.013), and more caregiving rewarding feelings (b = 0.54, P < 0.001). Also, caregivers with more knowledge and skills were more inclined to adopt positive coping strategies (b = 0.44, P < 0.001). Despite these differences, caregivers with different levels of caregiving knowledge and skills reported comparable caregiver burden (b = 0.11, P = 0.705) and the use of a passive coping style (b = 0.10, P = 0.169).
Conclusion: Caregiving knowledge and skills are a reliable predictor of psychological well-being and active coping among the primary family caregivers of PLSs. These findings inform the development of psychoeducational interventions to support family caregivers of PLSs.
With a prevalence of 1–3% worldwide (1), schizophrenia is a psychiatric disorder characterized by profound disturbance in language, perception, thinking, and frequent psychotic experiences (2). People living with schizophrenia (PLSs) are characterized by positive symptoms such as delusions and hallucinations (3). They may also present negative symptoms reflected in alteration of motivation and volition, such as social withdrawal, difficulty in maintaining interpersonal relationships, apathy, and anhedonia (4–6). PLSs may also have other accompanying symptoms, such as cognition impairment and emotional disorder (e.g., mania and depression) (7, 8). Schizophrenia can occur at different stages of life course, while the risk varies across different age groups (9). Reports have shown that the prevalence of schizophrenia changes with age in an inverted U-shape, with the highest value at around 40 years of age. Globally, PLSs aged 25–54 years are estimated to account for 70.8% of total cases. There is no sexual difference in the prevalence (10). PLSs usually have reduced life expectancy in comparison with individuals from the general population (11). This disorder afflicts both PLSs and their family caregivers (12), particularly in countries with insufficient mental health resources and community health service systems (13). In China, more than 90% of PLSs live with their family members and receive family care because of insufficient community health resources (14).
Caring for a family member with schizophrenia requires considerable time, energy, and money from the family caregivers over a prolonged period, which may result in increased caregiver burden and psychological distress (15, 16). Numerous studies have demonstrated a high level of burden among caregivers of PLSs (12, 15, 17, 18) and psychological distress, such as stress, anxiety, and depression (19). For instance, more than half of caregivers report a moderate to severe level of caregiver burden (18), whereas the prevalence of psychological distress is as high as nearly 80% (1, 20). Notably, high levels of caregiver burden and psychological distress among caregivers may also impair the mental health of PLSs (21), who tend to experience physical or verbal domestic violence from their distressed caregivers (22, 23).
Despite significant caregiver burden and distress, there are also reports of positive impacts of caregiving (24, 25). Caring for PLSs may lead to positive transformations among caregivers (26, 27) and promote positive caregiving rewarding feelings, such as enhanced self-satisfaction, self-esteem, self-confidence, and self-affirmation (28, 29). Moreover, caring for PLSs can lead to improvements in stress-coping styles of caregivers (30), which are behavioral coping strategies adopted by individuals to resolve adversities and stressors (31). Evidence has shown that active coping is also associated with better health outcomes (32).
Over the past few decades, various interventions have been developed to support family caregivers of PLSs, of which psychoeducation is the most common and widely shown to be effective (33). Psychoeducation provides PLSs and family caregivers information about strategies and resources to promote the goals of treatment and rehabilitation (33). For caregivers, the key element of psychoeducation lies in improving knowledge and skills in caregiving (34). However, inconsistent findings about the correlations between caregiving knowledge and skills and caregiver burden have been reported by Sefasi et al. (35) and Jagannathan et al. (15). Sefasi et al. found caregivers of PLSs with more knowledge tended to bear greater burden, whereas Jagannathan et al. suggested there was no relationship of caregiving knowledge with burden. To date, no quantitative studies exist that examine the associations of caregiving knowledge and skills with psychological well-being (stress, anxiety, depression, caregiving rewarding feelings) and coping styles (active coping) among the primary family caregivers of PLSs in China.
The theoretical background of this study refers to the stress process model proposed by Pearlin et al. and their assumption that stress results from an interaction of two domains: stressors and mediators (36). Each of these domains can be divided into a series of subparts that have been intensively studied and developed in recent years. According to this model, it can be inferred that stress perceived by caregivers is partially mediated by coping and individual appraisal. Elevated caregiving knowledge and skills help enhance caregivers' ability to cope with adversity and enable them to adopt active coping strategies to address current dilemmas, thus contributing to the reduction of stress (37). Individual appraisal involves subjective assessment on controls of adversity and self-worth. A high level of caregiving knowledge and skills enables caregivers to resolve difficulties in the process of caring for PLSs, thus contributing to increased feelings of personal accomplishment and self-efficacy (38, 39). Furthermore, caregiving knowledge itself is a mediator in the path between stressors and burden (36, 40). Therefore, in the conceptual framework of this study, we assumed that caregiving knowledge and skills may be associated with caregiving experiences (caregiver burden, stress, coping styles, etc.) in a direct or indirect path.
The aim of this study was to evaluate the relationships between caregiving knowledge and skills and a range of caregiving experiences among primary family caregivers of PLSs in China.
This cross-sectional study using one-stage cluster sampling was conducted in 12 community health centers of Changsha City, Hunan Province. The targeted population for this study was the primary family caregivers of PLSs who were registered in the “686 Program,” China's largest demonstration project in mental health services (41, 42). For each person living with schizophrenia, only one primary family caregiver was enrolled in this study based on closeness with PLSs and direct involvement in caregiving. The inclusion criteria were as follows: (1) aged over 18 years; (2) caring for individuals diagnosed with schizophrenia according to the criteria of Chinese Classification of Mental Disorders Version 3 (43) or the International Classification of Diseases, Tenth Revision (44); (3) living with PLSs for over 2 years and taking major responsibility for caregiving; (4) able to understand, read, and communicate with investigators in Chinese. The exclusion criteria included (1) caring for PLSs who received a diagnosis other than schizophrenia; (2) unable to speak Chinese; and (3) lack of literacy, or having serious physical or mental diseases that made them unable to communicate effectively with others.
Data were collected by well-trained researchers from May 2019 to September 2019. First, all participants were informed about the purpose of the study and provided written informed consent before participating. Second, the overall content of questionnaires was introduced to each eligible participant, and they were invited to complete the questionnaires (see assessment below) by face-to-face interviews. Next, a quality-control investigator checked the answers to ensure accuracy, integrity, and consistency. A total of 414 primary family caregivers volunteered to participate in this study, of which 395 participants completed the questionnaire (response rate = 95.41%). No significant difference was detected between individuals who completed and those who did not complete the survey in terms of gender, age, marriage, education, and employment.
The institutional review board of the Xiangya School of Public Health of Central South University approved the protocol of this study. Participants who completed the questionnaire were reimbursed with RMB 20 yuan in cash ($3).
Sociodemographic data of the primary family caregivers were collected by face-to-face interviews, including sex, age, marital status, education, employment status, financial circumstances (annual income per household), length of caregiving, and the relationship between PLSs and the primary caregivers. Besides, whether there were any co-caregivers, additional dependents, and physical illnesses were also recorded.
The understanding of schizophrenia and mastery of caregiving skills were evaluated using the Knowledge and Skills of Caregiving Scale (KSCS). The KSCS is a five-item questionnaire, which was originally designed according to the survey on the demands of mental health knowledge among the Chinese caregivers of PLSs (45–47). Items are scored on a 4-point Likert scale from 0 (do not understand) to 3 (totally understand) to measure the caregiver's understanding of the following aspects: the symptoms of schizophrenia, medication and its side effects, the care of PLSs, and management of symptoms. The total KSCS score ranges from 0 to 15, with a higher score demonstrating higher knowledge of schizophrenia and better skills in caregiving. The detailed contents of the KSCS are illustrated in Supplementary Table 1. The KSCS showed good internal consistency in the current study, with a Cronbach α of 0.87.
Caregiver burden was evaluated using the Zarit Burden Interview (ZBI) (48). The ZBI consists of 22 items, and each item is rated on a 5-point response scale from 0 (never) to 4 (nearly always), except for the final item evaluating global burden from 0 (not at all) to 4 (extremely). The total score ranges from 0 to 88, and higher scores are indicative of higher burden perceived by caregivers. This instrument was first translated into Chinese by Lu et al. (49) in 2009 and found to be reliable and valid in evaluating caregiver burden (50, 51). The ZBI also demonstrated excellent internal consistency in this sample, with a Cronbach α of 0.92.
Perceived stress was assessed using the 10-item Perceived Stress Scale (PSS-10) (52). This instrument covers two domains: perceived helplessness (six items) and perceived self-efficacy (four items) (53, 54). Each item is scored on a 5-point Likert scale from 0 (never) to 4 (often); the total score ranges from 0 to 40, with higher scores indicating greater perceived stress. First translated into Chinese by Yang et al. (55) in 2003, the PSS-10 is reliable in evaluating perceived stress (56, 57). In this study, the PSS-10 exhibited acceptable internal consistency, with a Cronbach α of 0.79.
The seven-item Generalized Anxiety Disorder Scale (GAD-7) (58) was used to reflect the anxiety symptoms of primary family caregivers in the past 2 weeks. Items rated on a 4-point Likert scale from 0 (not at all) to 3 (nearly every day) are summed into a total score, which ranges from 0 to 21, and a cutoff score of 10 has been suggested to differentiate anxiety and non-anxiety (59). The GAD-7 was first translated into Chinese by He et al. (60) in 2010 and is a valid and reliable measure of anxiety among the Chinese population (61). In this study, the GAD-7 demonstrated good internal consistency with a Cronbach α of 0.95.
The depression symptoms of primary family caregivers were screened using the self-reported Patient Health Questionnaire (PHQ-9) (62). The PHQ-9 consists of nine items rated on a 4-point Likert scale from 0 (not at all) to 3 (nearly every day) to evaluate the frequency of depression symptoms in the preceding 2 weeks. The total score ranges from 0 to 27, with higher scores indicative of more depression symptoms. The PHQ-9 was first translated into Chinese by Yeung et al. (63) in 2008 and showed good validity and reliability in Chinese context (64). In the present study, the Cronbach α for the PHQ-9 was 0.93.
The Caregiving Rewarding Feelings (CRF) scale was applied to evaluate positive feelings about caregiving (65). Thirty individuals with schizophrenia and their primary caregivers were qualitatively interviewed for the initial development of the CRF, pretesting, and Delphi method for further revision and then a test with a larger sample to confirm its validity and reliability. The detailed process of development and validation of the CRF has been illustrated elsewhere (65). The CRF is a 12-item questionnaire developed in a Chinese context, and each item is scored on a 4-point Likert scale (0 = “never” to 3 = “nearly always”) to assess whether caring for PLSs makes the primary caregivers “become more loving and patient,” “feels more worthy,” “be more active and optimistic,” “have stronger sense of responsibility,” etc. The total score ranges from 0 to 36, with a higher score suggesting better positive feelings. In this study, the CRF demonstrated excellent internal consistency with a Cronbach α of 0.96.
The Simplified Coping Style Questionnaire (SCSQ) was used to measure a caregiver's coping style (66). This measure is a 4-point Likert questionnaire (0 = “never” to 3 = “nearly always”) that comprises 20 items classified into two dimensions: active coping (12 items) and passive coping (eight items). Active coping mainly reflects one's active coping preference when encountering difficulties, such as “working out several different ways to solve the problem.” Passive coping mainly reflects one's passive coping tendency when encountering difficulties, such as “relying on others to solve the problem.” The total score ranges from 0 to 60, and a higher score for each dimension indicates a higher possibility that the participant would adopt the corresponding coping style. Good reliability and validity of the SCSQ in a Chinese context were reported by Xie (66), and a Cronbach α of 0.88 for the total scale, 0.90 for the subscale of active coping, 0.72 for the subscale of passive coping were detected in the current study.
Sample size was calculated using the correlation power and sample size calculation in G*Power. Assuming a correlation of 0.2 between caregiving knowledge and skill and stress, a Z value of 1.98 at a confidence interval of 95%, and allowable α error of 5%, we needed a sample size of 319. Considering a rejection or loss-to-follow-up rate of 10%, we expanded our final sample size to 350. Our study recruited 395 participants, which satisfies the sample size requirement with a power of 95%.
All statistical analyses were performed using STATA software version 16.0. The categorical variables were presented as counts (percentages), whereas the continuous variables were expressed as mean (SD) or median [interquartile range (IQR)]. Normality of data was determined using frequency distributions (histogram), Kolmogorov–Smirnov test, and skewness and kurtosis statistics. The difference of KSCS scores in different sociodemographic groups was checked using Mann–Whitney U-test or Kruskal–Wallis H test. The correlations between knowledge and skills of caregiving and various types of caregiving experiences (caregiver burden, stress, anxiety, depression, caregiving rewarding feelings, coping styles) were examined by Spearman rank correlation analysis. Adjusted by potential confounders (gender, age, marital status, education, employment, annual income, etc.), several multivariate linear regressions were separately performed to examine the associations between KSCS score and seven types of caregiving experiences among primary family caregivers. Potential multicollinearity between predictor variables was checked by variance inflation factor (VIF), with VIF > 5 indicating collinearity (13). The difference was considered statistically significant at P < 0.05.
The sociodemographic characteristics of the participants are described in Table 1. There were slightly more females (55%) than males (45%). Most of the caregivers were older than 60 years (64%), were married (76%), had a middle school education (60%), and were unemployed (87%), with an annual family income of <10,000 yuan (60%). The largest proportion of caregivers were parents (58%). Most caregivers had been caring for PLSs for over 10 years (81%) and without co-caregivers (56%). Sixty percent of caregivers had no additional dependents and had physical illness such as hypertension, diabetes mellitus, and cardiovascular diseases.
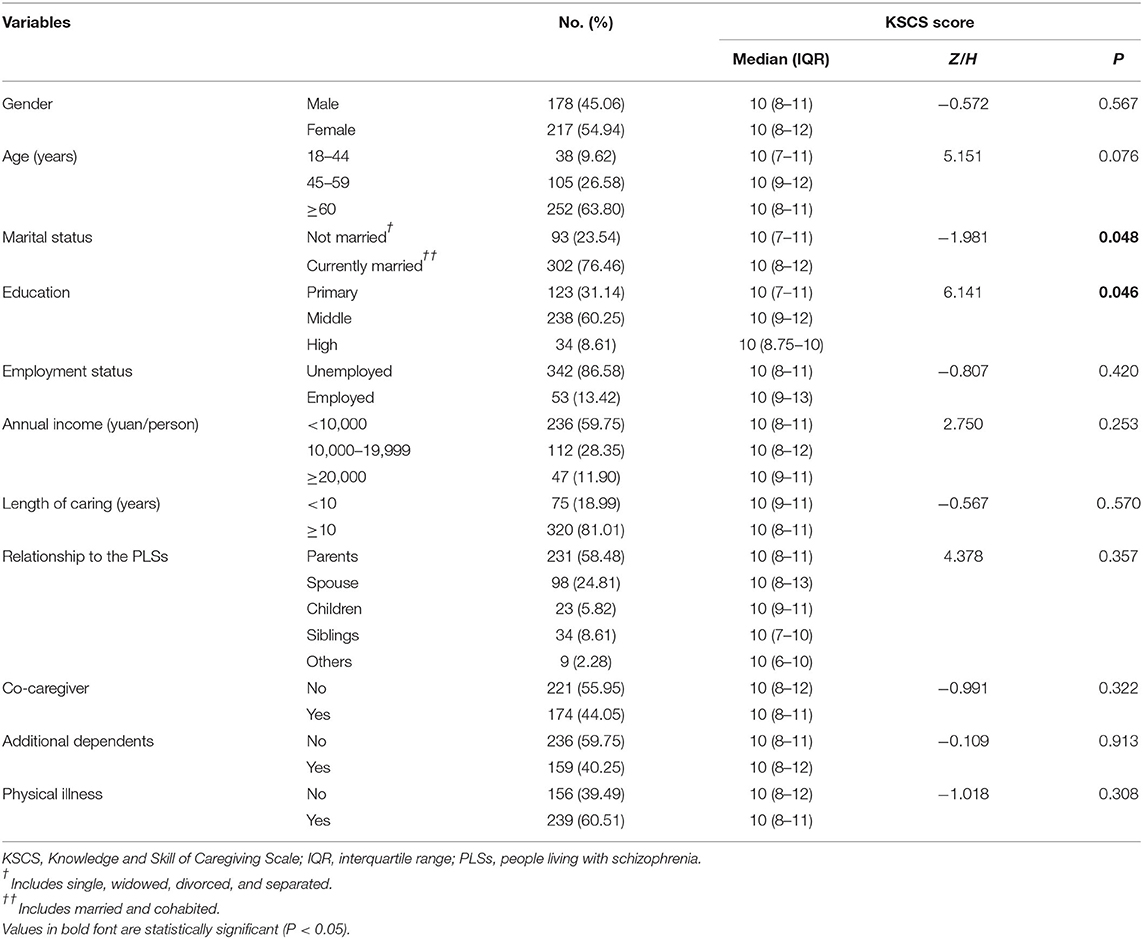
Table 1. Sociodemographic characteristics of the caregivers and comparison of KSCS scores between groups.
The median KSCS score was 10, with an IQR of 8–11. We further compared the KSCS score between groups with different sociodemographic characteristics and found no significant difference except for marital status and education. Caregivers who were married, with higher educational attainment, had better caregiving knowledge and skills (P = 0.048, P = 0.046).
Table 2 summarizes the caregiving experiences concerning caregiver burden, psychological well-being, and coping styles, divided into negative and positive caregiving experiences. Negative caregiving experiences comprised caregiver burden (mean = 43.21), stress (mean = 18.72), anxiety (mean = 7.68), depression (mean = 8.30), and passive coping (mean = 11.80). Positive caregiving experiences consisted of caregiving rewarding feelings (mean = 26.20) and active coping (mean = 20.02).
Caregivers' knowledge and skills about caregiving were negatively correlated with stress (r = −0.210, P < 0.001), anxiety (r = −0.104, P = 0.039), and depression (r = −0.167, P < 0.001), and positively associated with caregiving rewarding feelings (r = 0.208, P < 0.001) and active coping (r = 0.168, P < 0.001). But caregiving knowledge and skills did not correlate with either caregiver burden or passive coping, despite a small trend in favor of a positive correlation.
Table 3 shows the results of several multivariate linear regressions of caregiving knowledge and skills on seven types of caregiving experiences (caregiver burden, stress, anxiety, depression, caregiving rewarding feelings, active coping, passive coping). After controlling for covariates, caregiving knowledge and skills were still significantly negatively associated with stress (b = −0.48, P < 0.001), anxiety (b = −0.23, P = 0.029), and depression (b = −0.29, P = 0.013), as well as positively associated with caregiving rewarding feelings (b = 0.54, P < 0.001). Besides, primary caregivers with more caregiving knowledge and skills were more inclined to adopt positive coping strategies (b = 0.44, P < 0.001). No significant relationship was detected between caregiving knowledge and skills with either caregiver burden (b = 0.11, P = 0.705) or passive coping (b = 0.10, P = 0.169).
To our knowledge, this is the first study that investigates comprehensively the associations of caregiving knowledge and skills with caregiver burden, psychological well-being, and coping styles among primary family caregivers of PLSs in China. Although no relationship was found between caregiving knowledge and skills and caregiver burden, caregiving knowledge and skills were negatively associated with stress, anxiety, and depression and positively associated with caregiving rewarding feelings. In addition, caregivers with more caregiving knowledge and skills were more inclined to adopt positive coping strategies, but not passive coping strategies. These findings add further evidence about the positive associations of caregiving knowledge and skills with a range of health outcomes and inform future psychoeducational interventions for improving caregiver outcomes.
Our study informs the relationship between caregiving knowledge and skills and caregiver burden. Some previous reports indicated that as the level of knowledge about schizophrenia increased, the perceived burden decreased (67, 68), whereas other studies showed the opposite (35). Consistent with previous research reported by Lim et al. (69) and Jagannathan et al. (15), our study showed that primary caregivers' knowledge about schizophrenia did not have any relationship to caregiver burden. Previous research suggested that avoidant coping may lead to increased caregiver burden (70), and the lack of association of caregiving knowledge and skills with caregiver burden in the current study may be due to the null association of caregiving knowledge and skills with passive coping. It is likely that coping style may mediate the relationship between caregiving knowledge and skills and caregiver burden, which warrants further study (71).
The current study also suggests that increased knowledge and skills of caregiving may relieve psychological distress, such as stress, anxiety, and depression. The stress process model argues that stress source, such as family conflicts and financial issues, is an important domain contributing to caregiver burden (36). Wan et al. (1) reported that lack of understanding of psychotic symptoms can lead to conflicts between caregivers and PLSs, which subsequently resulted in a high level of psychological distress among caregivers. Furthermore, caregivers with little knowledge may be more likely to hold false beliefs about schizophrenia, such as thinking that it is the result of bewitchment or drug abuse (72). When bewitchment is viewed as the cause of schizophrenia, caregivers usually hold pessimistic views (73) and lose hope for the recovery of PLSs, leading to psychological distress (35). Thus, increased knowledge and skills of caregiving may help caregivers change their attribution about the cause of schizophrenia so as to better understand the challenges faced by PLSs and take more active steps when crises occur (74). Improved caregiving knowledge and skills may also reduce caregivers' stigma associated with schizophrenia, which is known to be associated with depression and suicidal thoughts (75–77).
Under the framework of the stress process model, individual evaluation on self-worth is considered as a significant moderator of stress and is susceptible to subjective psychological factors. In this study, we demonstrated that improved caregiving knowledge and skills were associated with more caregiving rewarding feelings among the caregivers, an observation that may be explained, in part, by the Chinese culture. Under the influence of Confucianism, the dominant concept of collectivism is deeply rooted in the Chinese culture (13). Family members usually consider care for PLSs as their responsibility, and they may make every effort to facilitate the patient's recovery. A higher level of caregiving knowledge and skills allows them to assume more responsibility and provide better support for their loved one with schizophrenia, which may bring in a higher sense of self-achievement (38). A recent study with primary family caregivers of PLSs showed that improved knowledge and understanding of schizophrenia were effective in increasing their social interactions and promoting greater optimism for the future (74). Also, more knowledge about schizophrenia helps improve the caregiver's ability to monitor symptoms and initiate better collaboration with mental healthcare professionals, thus leading to improved self-efficacy (39).
In the stress process model, the interaction between stressors and psychological outcomes can be mediated by coping strategy (36). Similarly, a heuristic multivariate model proposed by Vitaliano et al. considers that burden results from three domains: stressor, vulnerability, and resource (78). In this model, passive coping is a risk factor for vulnerability. The current results showed that family caregivers with a higher level of caregiving knowledge and skills were more likely to adopt positive coping behaviors, which was related to better mental health (79). This finding also partially explained the phenomenon that a higher level of caregiving knowledge and skills predicted improved psychological well-being. For caregivers, increased knowledge and skills of caregiving may enhance individual confidence and competence in challenging difficulties (80), which is revealed in adopting active coping strategies. As noted above, caregiving knowledge and skills also correlated with hopefulness, which was found to be a predictor of problem-oriented coping (81). Besides, the stress–appraisal–coping paradigm is another theoretical framework for understanding the relationship between caregiving knowledge and stress (82). A better understanding of schizophrenia and caregiving may enable caregivers to reappraise the demands of caregiving, develop more effective strategies to cope with the problems related to caregiving, and better handle maladaptive behaviors of the PLSs, thus leading to reduced stress (74, 83).
The present study has several limitations. First, there was a potential selection bias as the participants in the current study were from the “686 Program,” who may have different caregiving experiences due to the availability of health services compared with those outside the program. A related limitation is that participants who were not willing to participate in the survey were also excluded. Second, as the caregivers in this study were PLSs' family members (informal caregivers), our findings cannot be extrapolated to all caregivers of PLSs. Third, the cross-sectional design of this study did not allow for investigating causal relationships among the variables, which should be further examined using longitudinal data. Fourth, a number of family caregivers in our sample had been caring for their loved one with schizophrenia for a long time, which may be different for caregivers of PLSs after a first episode. Fifth, given that the ZBI is a non-specific scale for the evaluation of caregiver burden, this instrument may not fully reflect the caregiver burden in schizophrenia.
The current study demonstrated that caregiving knowledge and skills were positively related to less stress, anxiety, and depression symptoms. Also, family caregivers with a higher level of caregiving knowledge and skills experienced more caregiving rewarding feelings and were more willing to adopt positive coping strategies in the face of difficulties and challenges. These findings inform future psychoeducational interventions to enhance family caregivers' knowledge and skills of caregiving to improve their psychological well-being and promote active coping.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Institutional review board of Xiangya School of Public Health, Central South University. The patients/participants provided their written informed consent to participate in this study.
All authors have made substantial contributions to the study conception and design, data collection and analysis, as well as to the development and editing of the manuscript. ZZ, RL, and YY contributed to the conception and design of the study. ZZ, YW, PF, TL, and YY contributed to the research conduction and data collection. ZZ and YW contributed to data analyses. PF, TL, JT, RL, and YY contributed to data interpretation. ZZ drafted the article while YW, PF, TL, JT, RL, and YY critically appraised it and revised it. All authors approved the final version of manuscript for submission and publication and agreed to be accountable for all aspects of the work.
This work was funded by a grant from the National Natural Science Foundation of China (Grant Number 71804197) and the China Scholarship Council (CSC) in support of the corresponding author YY.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank all the families of the individuals with schizophrenia for their participation in the WIFI program and for openly sharing their feelings and experiences. We would also like to thank the Changsha Psychiatric Hospital as well as the 12 community health centers for their collaboration and support.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.631420/full#supplementary-material
1. Wan KF, Wong MMC. Stress and burden faced by family caregivers of people with schizophrenia and early psychosis in Hong Kong. Intern Med J. (2019) 49(Suppl 1):9–15. doi: 10.1111/imj.14166
2. World Health Organization. Schizoprenia. Available online at: https://www.who.int/topics/schizophrenia/en/ (accessed June 28, 2020).
3. Zhang Y, You X, Li S, Long Q, Zhu Y, Teng Z, et al. Peripheral blood leukocyte rNA-Seq identifies a set of genes related to abnormal psychomotor behavior characteristics in patients with schizophrenia. Med Sci Monit. (2020) 26:e922426. doi: 10.12659/MSM.922426
5. Bryll A, Krzyściak W, Karcz P, Smierciak N, Kozicz T, Skrzypek J, et al. The relationship between the level of anterior cingulate cortex metabolites, brain-periphery redox imbalance, and the clinical state of patients with schizophrenia and personality disorders. Biomolecules. (2020) 10:1272. doi: 10.3390/biom10091272
6. Müller N, Ackenheil M. Immunoglobulin and albumin content of cerebrospinal fluid in schizophrenic patients: relationship to negative symptomatology. Schizophr Res. (1995) 14:223–8. doi: 10.1016/0920-9964(94)00045-A
7. Kahn RS, Keefe RS. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry. (2013) 70:1107–12. doi: 10.1001/jamapsychiatry.2013.155
8. Musliner KL, Mortensen PB, McGrath JJ, Suppli NP, Hougaard DM, Bybjerg-Grauholm J, et al. Association of polygenic liabilities for major depression, bipolar disorder, and schizophrenia with risk for depression in the danish population. JAMA Psychiatry. (2019) 76:516–25. doi: 10.1001/jamapsychiatry.2018.4166
9. Niu J, Cao Y, Ji Y. Resveratrol, a SIRT1 activator, ameliorates mK-801-Induced cognitive and motor impairments in a neonatal rat model of schizophrenia. Front Psychiatry. (2020) 11:716. doi: 10.3389/fpsyt.2020.00716
10. Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophrenia Bull. (2018) 44:1195–203. doi: 10.1093/schbul/sby058
11. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. (2014) 10:425–48. doi: 10.1146/annurev-clinpsy-032813-153657
12. Parabiaghi A, Lasalvia A, Bonetto C, Cristofalo D, Marrella G, Tansella M, et al. Predictors of changes in caregiving burden in people with schizophrenia: a 3-year follow-up study in a community mental health service. Acta Psychiatr Scand Suppl. (2007) 116:66–76. doi: 10.1111/j.1600-0447.2007.01094.x
13. Yu Y, Li TX, Li YL, Qiu D, Xi SJ, Xiao SY, et al. A cross-sectional study on spouse and parent differences in caregiving experiences of people living with schizophrenia in rural china. BMC Psychiatry. (2020) 20:226. doi: 10.1186/s12888-020-02633-w
14. Phillips MR, West CL, Shen Q, Zheng Y. Comparison of schizophrenic patients' families and normal families in china, using Chinese versions of FACES-II and the family environment scales. Fam Process. (1998) 37:95–106. doi: 10.1111/j.1545-5300.1998.00095.x
15. Jagannathan A, Thirthalli J, Hamza A, Nagendra HR, Gangadhar BN. Predictors of family caregiver burden in schizophrenia: study from an in-patient tertiary care hospital in India. Asian J Psychiatr. (2014) 8:94–8. doi: 10.1016/j.ajp.2013.12.018
16. Nasrallah HA, Harvey PD, Casey D, Csoboth CT, Hudson JI, Julian L, et al. The management of schizophrenia in clinical practice (MOSAIC) registry: a focus on patients, caregivers, illness severity, functional status, disease burden and healthcare utilization. Schizophr Res. (2015) 166:69–79. doi: 10.1016/j.schres.2015.04.031
17. Hsiao CY, Tsai YF. Factors of caregiver burden and family functioning among Taiwanese family caregivers living with schizophrenia. J Clin Nurs. (2015) 24:1546–56. doi: 10.1111/jocn.12745
18. Yu Y, Liu ZW, Tang BW, Zhao M, Liu XG, Xiao SY. Reported family burden of schizophrenia patients in rural china. PLoS ONE. (2017) 12:e0179425. doi: 10.1371/journal.pone.0179425
19. Kate N, Grover S, Kulhara P, Nehra R. Caregiving appraisal in schizophrenia: a study from India. Soc Sci Med. (2013) 98:135–40. doi: 10.1016/j.socscimed.2013.09.005
20. Yusuf AJ, Nuhu FT. Factors associated with emotional distress among caregivers of patients with schizophrenia in Katsina, Nigeria. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:11–6. doi: 10.1007/s00127-009-0166-6
21. Liu C, Wang L, Zhao Q. Factors related to health-related quality of life among chinese psychiatrists: occupational stress and psychological capital. BMC Health Serv Res. (2015) 15:20. doi: 10.1186/s12913-015-0677-7
22. Macneil G, Kosberg JI, Durkin DW, Dooley WK, Decoster J, Williamson GM. Caregiver mental health and potentially harmful caregiving behavior: the central role of caregiver anger. Gerontologist. (2010) 50:76–86. doi: 10.1093/geront/gnp099
23. Smith GR, Williamson GM, Miller LS, Schulz R. Depression and quality of informal care: a longitudinal investigation of caregiving stressors. Psychol Aging. (2011) 26:584–91. doi: 10.1037/a0022263
24. Shiraishi N, Reilly J. Positive and negative impacts of schizophrenia on family caregivers: a systematic review and qualitative meta-summary. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:277–90. doi: 10.1007/s00127-018-1617-8
25. Yu Y, Tang BW, Liu ZW, Chen YM, Zhang XY, Xiao S. Who cares for the schizophrenia individuals in rural china - a profile of primary family caregivers. Compr Psychiatry. (2018) 84:47–53. doi: 10.1016/j.comppsych.2018.04.002
26. Wang A, Bai X, Lou T, Pang J, Tang S. Mitigating distress and promoting positive aspects of caring in caregivers of children and adolescents with schizophrenia: mediation effects of resilience, hope, and social support. Int J Ment Health Nurs. (2020) 29:80–91. doi: 10.1111/inm.12651
27. Chen FP, Greenberg JS. A positive aspect of caregiving: the influence of social support on caregiving gains for family members of relatives with schizophrenia. Community Ment Health J. (2004) 40:423–35. doi: 10.1023/B:COMH.0000040656.89143.82
28. Kulhara P, Kate N, Grover S, Nehra R. Positive aspects of caregiving in schizophrenia: a review. World J Psychiatry. (2012) 2:43–8. doi: 10.5498/wjp.v2.i3.43
29. Kramer BJ. Gain in the caregiving experience: where are we? What next? Gerontologist. (1997) 37:218–32. doi: 10.1093/geront/37.2.218
30. Chiu M, Wesson V, Sadavoy J. Improving caregiving competence, stress coping, and mental well-being in informal dementia carers. World J Psychiatry. (2013) 3:65–73. doi: 10.5498/wjp.v3.i3.65
31. Lazarus RS. The psychology of stress and coping. Issues Ment Health Nurs. (1985) 7:399–418. doi: 10.3109/01612848509009463
32. Hsiao CY, Lu HL, Tsai YF. Caregiver burden and health-related quality of life among primary family caregivers of individuals with schizophrenia: a cross-sectional study. Qual Life Res. (2020) 29:2745–57. doi: 10.1007/s11136-020-02518-1
33. Pekkala E, Merinder L. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. (2002) 2:CD002831. doi: 10.1002/14651858.CD002831
34. Alhadidi MM, Lim Abdullah K, Yoong TL, Al Hadid L, Danaee M. A systematic review of randomized controlled trials of psychoeducation interventions for patients diagnosed with schizophrenia. Int J Soc Psychiatry. (2020) 66:542–52. doi: 10.1177/0020764020919475
35. Sefasi A, Crumlish N, Samalani P, Kinsella A, O'Callaghan E, Chilale H. A little knowledge: caregiver burden in schizophrenia in Malawi. Soc Psychiatry Psychiatr Epidemiol. (2008) 43:160–4. doi: 10.1007/s00127-007-0276-y
36. Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. (1990) 30:583–94. doi: 10.1093/geront/30.5.583
37. Sin J, Norman I. Psychoeducational interventions for family members of people with schizophrenia: a mixed-method systematic review. J Clin Psychiatry. (2013) 74:e1145–62. doi: 10.4088/JCP.12r08308
38. Olawande TI, Ajayi MP, Amoo EO, Iruonagbe CT. Variations in family attitudes towards coping with people living with mental illness. Open Access Maced J Med Sci. (2019) 7:2010–6. doi: 10.3889/oamjms.2019.071
39. Mannion E, Mueser K, Solomon P. Designing psychoeducational services for spouses of persons with serious mental illness. Commun Ment Health J. (1994) 30:177–90. doi: 10.1007/BF02188628
40. Mulud ZA, McCarthy G. Caregiver burden among caregivers of individuals with severe mental illness: testing the moderation and mediation models of resilience. Arch Psychiatr Nurs. (2017) 31:24–30. doi: 10.1016/j.apnu.2016.07.019
41. Good BJ, Good MJD. Significance of the 686 program for china and for global mental health. Shanghai Arch Psychiatry. (2012) 24:175–7. doi: 10.3969/j.issn.1002-0829.2012.03.008
42. Ma H. Integration of hospital and community services-the '686 project'-is a crucial component in the reform of china's mental health services. Shanghai Arch Psychiatry. (2012) 24:172–4. doi: 10.3969/j.issn.1002-0829.2012.03.007
43. Chen YF. Chinese classification of mental disorders (CCMD-3): towards integration in international classification. Psychopathology. (2002) 35:171–5. doi: 10.1159/000065140
44. Anonymous. Implementation of the international statistical classification of diseases and related health problems, tenth revision (ICD-10). Epidemiol Bull. (1997) 18:1–4.
45. Lin J, Zhou Y, Pan S, Zeng G, Lu X, Cai H. [Needs analysis of caregivers of patients with schizophrenia for mental health knowledge]. Mod Clin Nurs. (2015) 14:11–4. doi: 10.3969/j.issn.1671-8283.2015.06.004
46. Lu Z. [Investigation and analysis of the need of mental health knowledge among caregivers of schizophrenics]. Med Forum. (2018) 22:1542–3. doi: 10.19435/j.1672-1721.2018.11.070
47. Feng H, Hu X, Xu C, Zhang J. [Survey of demands of schizophrenic caregivers for knowledge of disease and health education]. Nurs Pract Res. (2016) 13:72–4. doi: 10.3969/j.issn.1672-9676.2016.23.031
48. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. (1980) 20:649–55. doi: 10.1093/geront/20.6.649
49. Lu L, Wang L, Yang X, Feng Q. Zarit caregiver burden interview: development, reliability and validity of the chinese version. Psychiatry Clin Neurosci. (2009) 63:730–4. doi: 10.1111/j.1440-1819.2009.02019.x
50. Tang B, Yu Y, Liu Z, Lin M, Chen Y, Zhao M, et al. Factor analyses of the chinese zarit burden interview among caregivers of patients with schizophrenia in a rural chinese community. BMJ Open. (2017) 7:e015621. doi: 10.1136/bmjopen-2016-015621
51. Yu Y, Liu ZW, Zhou W, Chen XC, Zhang XY, Hu M, et al. Assessment of burden among family caregivers of schizophrenia: psychometric testing for short-form zarit burden interviews. Front Psychol. (2018) 9:2539. doi: 10.3389/fpsyg.2018.02539
52. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
53. Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-Item version of the perceived stress scale. J College Couns. (2006) 9:135–47. doi: 10.1002/j.2161-1882.2006.tb00100.x
54. Barbosa-Leiker C, Kostick M, Lei M, McPherson S, Roper V, Hoekstra T, et al. Measurement invariance of the perceived stress scale and latent mean differences across gender and time. Stress Health. (2013) 29:253–60. doi: 10.1002/smi.2463
55. Yang TZ, Huang HT. [An epidemiological study on stress among urban residents in social transition period]. Zhonghua Liu Xing Bing Xue Za Zhi. (2003) 24:760–4. doi: 10.3760/j.issn:0254-6450.2003.09.004
56. Sun Y, Gao L, Kan Y, Shi BX. The perceived stress scale-10 (PSS-10) is reliable and has construct validity in chinese patients with systemic lupus erythematosus. Lupus. (2019) 28:149–55. doi: 10.1177/0961203318815595
57. Ng SM. Validation of the 10-item chinese perceived stress scale in elderly service workers: one-factor versus two-factor structure. BMC Psychol. (2013) 1:9. doi: 10.1186/2050-7283-1-9
58. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the gAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
59. Schalet BD, Cook KF, Choi SW, Cella D. Establishing a common metric for self-reported anxiety: linking the MASQ, PANAS, and GAD-7 to PROMIS anxiety. J Anxiety Disord. (2014) 28:88–96. doi: 10.1016/j.janxdis.2013.11.006
60. He X, Li C, Qian J, Cui HS, Wu W. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch Psychiatry. (2010) 22:200–3. doi: 10.3969/j.issn.1002-0829.2010.04.002
61. Qing Z. [Reliability and validity of chinese version of the generalized anxiety disorder 7-item (GAD-7) scale in screening anxiety disorders in outpatients from traditional chinese internal department]. Chin Ment Health J. (2013) 27:163–8. doi: 10.3969/j.issn.1000-6729.2013.03.001
62. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
63. Yeung A, Fung F, Yu S-C, Vorono S, Ly M, Wu S, et al. Validation of the patient health questionnaire-9 for depression screening among chinese Americans. Compr Psychiatry. (2008) 49:211–7. doi: 10.1016/j.comppsych.2006.06.002
64. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
65. Yu Y. Study on family burden and experiences of primary caregivers of schizophrenia in community. Central South University Thesis. (2016).
66. Xie Y. [Preliminary study to the reliability and validity of the simple coping style scale]. Chin J of Clin Psychol. (1998) 6:114–5.
67. Fallahi Khoshknab M, Sheikhona M, Rahgouy A, Rahgozar M, Sodagari F. The effects of group psychoeducational programme on family burden in caregivers of Iranian patients with schizophrenia. J Psychiatr Ment Health Nurs. (2014) 21:438–46. doi: 10.1111/jpm.12107
68. Worakul P, Thavichachart N, Lueboonthavatchai P. Effects of psycho-educational program on knowledge and attitude upon schizophrenia of schizophrenic patients' caregivers. J Med Assoc Thai. (2007) 90:1199–204.
69. Lim YM, Ahn YH. Burden of family caregivers with schizophrenic patients in Korea. Appl Nurs Res. (2003) 16:110–7. doi: 10.1016/S0897-1897(03)00007-7
70. Siddiqui S, Khalid J. Determining the caregivers' burden in caregivers of patients with mental illness. Pak J Med Sci. (2019) 35:1329–33. doi: 10.12669/pjms.35.5.720
71. Pakenham KI, Dadds MR. Family care and schizophrenia: the effects of a supportive educational program on relatives' personal and social adjustment. Aust N Z J Psychiatry. (1987) 21:580–90. doi: 10.3109/00048678709158927
72. Gureje O, Lasebikan VO, Ephraim-Oluwanuga O, Olley BO, Kola L. Community study of knowledge of and attitude to mental illness in Nigeria. Br J Psychiatry. (2005) 186:436–41. doi: 10.1192/bjp.186.5.436
73. Amsalem D, Hasson-Ohayon I, Gothelf D, Roe D. Subtle ways of stigmatization among professionals: the subjective experience of consumers and their family members. Psychiatr Rehabil J. (2018) 41:163–8. doi: 10.1037/prj0000310
74. Al-HadiHasan A, Callaghan P, Lymn JS. Qualitative process evaluation of a psycho-educational intervention targeted at people diagnosed with schizophrenia and their primary caregivers in Jordan. BMC Psychiatry. (2017) 17:68. doi: 10.1186/s12888-017-1225-2
75. Guan Z, Huang C, Wiley JA, Sun M, Bai X, Tang S. Internalized stigma and its correlates among family caregivers of patients diagnosed with schizophrenia in Changsha, Hunan, China. J Psychiatr Ment Health Nurs. (2020) 27:224–36. doi: 10.1111/jpm.12571
76. Magaña SM, Ramírez García JI, Hernández MG, Cortez R. Psychological distress among Latino family caregivers of adults with schizophrenia: the roles of burden and stigma. Psychiatr Serv. (2007) 58:378–84. doi: 10.1176/ps.2007.58.3.378
77. Ostman M, Kjellin L. Stigma by association: psychological factors in relatives of people with mental illness. Br J Psychiatry. (2002) 181:494–8. doi: 10.1192/bjp.181.6.494
78. Vitaliano PP, Russo J, Young HM, Teri L, Maiuro RD. Predictors of burden in spouse caregivers of individuals with alzheimer's disease. Psychol Aging. (1991) 6:392–402. doi: 10.1037/0882-7974.6.3.392
79. Chronister J, Chou CC, Liao HY. The role of stigma coping and social support in mediating the effect of societal stigma on internalized stigma, mental health recovery, and quality of life among people with serious mental illness. J Community Psychol. (2013) 41:582–600. doi: 10.1002/jcop.21558
80. Graham C, Ballard C, Sham P. Carers' knowledge of dementia, their coping strategies and morbidity. Int J Geriatr Psychiatry. (1997) 12:931–6. doi: 10.1002/(SICI)1099-1166(199709)12:93.0.CO;2-8
81. Lysaker PH, Campbell K, Johannesen JK. Hope, awareness of illness, and coping in schizophrenia spectrum disorders: evidence of an interaction. J Nerv Ment Dis. (2005) 193:287–92. doi: 10.1097/01.nmd.0000161689.96931.0f
82. Kate N, Grover S, Kulhara P, Nehra R. Relationship of caregiver burden with coping strategies, social support, psychological morbidity, and quality of life in the caregivers of schizophrenia. Asian J Psychiatr. (2013) 6:380–8. doi: 10.1016/j.ajp.2013.03.014
Keywords: schizophrenia, caregiving knowledge and skills, caregiver burden, psychological well-being, coping styles, primary family caregivers
Citation: Zhou Z, Wang Y, Feng P, Li T, Tebes JK, Luan R and Yu Y (2021) Associations of Caregiving Knowledge and Skills With Caregiver Burden, Psychological Well-Being, and Coping Styles Among Primary Family Caregivers of People Living With Schizophrenia in China. Front. Psychiatry 12:631420. doi: 10.3389/fpsyt.2021.631420
Received: 20 November 2020; Accepted: 15 April 2021;
Published: 26 May 2021.
Edited by:
Giuseppe Carrà, University of Milano-Bicocca, ItalyReviewed by:
Raphaelle Richieri, Assistance Publique Hôpitaux de Marseille, FranceCopyright © 2021 Zhou, Wang, Feng, Li, Tebes, Luan and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rongsheng Luan, bHVhbl9yc0BzY3UuZWR1LmNu; Yu Yu, eXV5dTIwMTZAY3N1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.