
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 05 February 2021
Sec. Social Psychiatry and Psychiatric Rehabilitation
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.621259
This article is part of the Research Topic Design and Implementation of Rehabilitation Interventions for People with Complex Psychosis View all 19 articles
Objective: Co-occurrence of chronic psychotic disorders and substance use disorder (SUD) is clinically challenging and increasingly prevalent. In 2000, legislation was passed in Israel to foster rehabilitation and integration in the community of persons with mental health disorders. In 2010, the need to allocate resources for patients with these co-occurring disorders (COD) was officially recognized. Yet, most rehabilitation services were not specifically designed for COD. This study examines the relationship between duration of community rehabilitation and number of psychiatric hospitalization days among persons with/without COD in Israel.
Methods: Data from the National Psychiatric Case Register on 18,684 adults with schizophrenia/schizoaffective disorders hospitalized in 1963–2016, was merged with data from the Israel Mental Rehabilitation Register. Associations and interactions between COD-status (COD/non-COD), time-period (Period1: 2001–2009, Period2: 2010–2016), duration of housing or vocational rehabilitation on hospitalization days per year were analyzed using repeated-measures ANOVA.
Results: The proportion of non-COD chronic psychotic patients who received rehabilitation services increased from 56% in Period1 to 63% in Period2, as it did among COD patients—from 30 to 35%. The proportion of non-COD patients who received longer-duration vocational rehabilitation (≥1 year) was significantly higher (43%) than among COD patients (28%) in both time periods. For housing rehabilitation, these proportions were 79 and 68%, respectively. Persons with COD experienced more hospitalization days annually than non-COD patients. Duration of rehabilitation (less/more than a year) was inversely associated with annual number of hospitalization days (p < 0.0001). This pattern was noted in both COD and non-COD groups and remained significant after controlling for age, sex, COD group, percent of hospitalizations with SUD, and age at first hospitalization.
Conclusions: COD patients with prolonged rehabilitation seemingly achieve long-term clinical improvement similar to non-COD patients, despite most rehabilitation settings in Israel not being designed for COD patients. Yet, COD patients receive overall less rehabilitation services and for shorter periods than non-COD patients. Long-term rehabilitation services should be provided to COD patients, who may need more time to commit to treatment. To achieve better long-term mental health improvements, a continued expansion of community-based integrative treatment and rehabilitation services for COD patients is needed in Israel.
One-fourth to two-thirds of patients with schizophrenia in the US and in Europe have a co-occurring Substance Use Disorder (SUD) (1–6). Analyzing data from the Israel National Psychiatric Case Register (INPCR), we recently reported a co-occurring disorder (COD) rate of 35% among Israeli adults with schizophrenia or schizoaffective disorder (7).
The co-occurrence of schizophrenia/schizoaffective disorder and SUD (also referred to as “dual diagnosis”) is often characterized by a chronic relapsing course of illness. The recurrence or worsening of the SUD can also trigger relapse of a psychotic episode (8). SUD worsens the overall clinical course of schizophrenia—compared to people with schizophrenia only, people with co-occurring SUD tend to be less adherent to treatment, experience more frequent relapses, and have higher rates of violent and life-threatening behavior, suicides and homelessness (9–12). The treatment of persons with COD is particularly challenging and often more complex than treatment of persons without COD (13). In early stage disease (i.e., within 5 years from initial diagnosis), COD patients show fewer brain deficits than non-COD patients, however, over time, the clinical picture is reversed and brain deficits such as volume deficits, shape abnormalities, and abnormalities in default mode network activation are more commonly manifested among COD patients (14, 15). This change is related to the long-term neurotoxic sequelae, but still on average COD patients have more preserved social and emotional functions during the premorbid phase as well as later on. COD patients also have better executive functioning which enables them to maintain their substance using behaviors (14).
The positive effect of community rehabilitation services on patients with severe mental illness, and schizophrenia in particular, has been widely reported (16–19). Community rehabilitation helps improve the functioning, well-being, symptoms severity and self-esteem of schizophrenia patients. There is also worldwide evidence that community rehabilitation is associated with a reduction of hospitalizations and frequency of hospitalization among persons with schizophrenia (20–23). This is likely achieved through positive effects of employment and regular contact and monitoring of the patient which allows for early detection of deterioration in the individual's mental health status and rapid referral for primary care thereby precluding the need for hospitalization.
The Community Rehabilitation of Persons with Mental Disability Law was enacted in Israel in the year 2000 with the aim to foster “the rehabilitation of persons with mental health disorders and their integration in the community, in order to enable them to attain the maximal degree of functional independence and quality of life, while maintaining their dignity.” This law initiated a reform in hospitalization services with the aim of reducing the number of psychiatric hospital beds alongside the establishment of community rehabilitation services, which began operating in 2001.
Of the rehabilitation services offered (vocational, housing, educational, leisure, family support, and treatment coordinator), vocational and housing rehabilitation are the most common, offer the greatest support and are usually the longest in duration. The aim of housing rehabilitation is to enhance social and housekeeping skills for independent-living in the community, by means of finding suitable and dignified housing conditions, with provision of support and on-going contact with community services. Vocational rehabilitation services promote finding and maintaining employment adapted to the wishes and capacities of the individual (24). Rehabilitation programs are generally personalized and accompanied by mental health therapists.
Until recently no rehabilitation services were available for persons with co-occurring disorders of severe mental illness (SMI) and SUD, and those with active drug use were generally denied services. It was only in 2010 that the Israeli parliament officially recognized the need to allocate additional resources for patients with COD (25). These resources included gradual opening of services for COD patients in hospitals and in the community and training of mental professionals about COD.
Enactment of the Community Rehabilitation law lead to the opening of private community-based rehabilitation services regulated and funded by the Ministry of Health (26) and was the precursor of the national insurance mental health reform formally launched in 2015. The reform aimed to integrate mental health services into the general healthcare system (primarily provided by the four HMOs that serve the Israeli population), and reduce the number of psychiatric hospitalizations through the expansion of ambulatory services (27). Overall, these policy shifts have resulted in the reduction of psychiatric hospital beds, number of hospitalization days, and rate of psychiatric hospitalizations (24, 27). People with SMI receiving rehabilitation are being hospitalized for shorter periods and the time between hospitalizations has lengthened (28). This was also true for schizophrenia and schizoaffective disorder patients in particular (22). The re-hospitalization rate decreased among patients with schizophrenia with an in-patient stay longer than 6 months (chronic patients) although not for short-stay patients with schizophrenia or affective disorders (29).
Regrettably, the treatment of addictions and the care of COD patients of SMI and SUD were excluded from the mental health reform of 2015. Patients with COD remained under the responsibility of the Ministry of Health, and are not entitled to receive treatment for their disorders from their HMO (27). Thus, the therapeutic options offered to COD patients, both in hospitals and in the community were, until very recently, limited, and many patients remained without adequate treatment (30–32). This situation existed, despite a growing awareness in recent years among health policy-makers in Israel about the need to allocate additional resources to treat patients with COD (25).
The present study, the first in Israel, examines the relationship between mental rehabilitation in the community and hospitalization characteristics of people with chronic psychotic disorder with and without SUD. We hypothesized that the rate of COD (comorbid chronic psychotic disorders and SUD) patients receiving rehabilitation services will be lower than that of non-COD patients, and that rehabilitation will be associated with a decrease in the number of hospitalization days over time for both groups, with a more substantial decrease among those without SUD.
Data were extracted from Israel's Mental Rehabilitation Register (IMRR) and merged with the National Psychiatric Case Register (NPCR) of the Ministry of Health. The NPCR is the official register of all psychiatric admissions and discharges countrywide since 1950 (33). As described in a previous report (20), we identified all adult patients (aged 18–65) hospitalized in a psychiatric hospital or a psychiatric ward of a general hospital during the period 1963–2016, with an ICD-10 diagnosis (34) of schizophrenia (F20) or schizoaffective disorder (F25) (SZ-SAD) at their last discharge. We restricted the study population to persons hospitalized at least once during the years 2010–2015 in order to ensure that the data and the findings are relevant.
For each hospitalization, a SUD diagnosis is recorded based on an ICD-10 diagnosis of F10–F19 in the categories of dependence and abuse (excluding F17—nicotine dependence) and/or a psychiatrist-documented indication of alcohol and/or drug abuse at admission or discharge. Patients were classified as COD if they had a SUD diagnosis in two or more hospitalizations, or in at least 20% of their hospitalizations.
Each person's hospitalization history was documented from his/her first hospitalization until the end of 2016. A total of 18,684 patients with 168,377 hospitalizations were included in the analysis after exclusion of 29 patients who had an anomalous number of hospitalizations (≥80).
The hospitalization data was merged with data from the IMRR that included: applications to the regional rehabilitation committee, type of rehabilitation service approved (either housing or vocational) and the total length of time the person actually received the service in each of the two time periods 2001–2009 (Period1) and 2010–2016 (Period2). We divided the periods before and after 2010, the year in which the Israeli parliament officially recognized the need to allocate additional resources to treat patients with COD (25). Community rehabilitation services began operating in 2001, and hence this defined the start of the study period.
To assess the impact of rehabilitation duration on hospitalization patterns, we compared hospitalization patterns of people who did not receive any rehabilitation services, people who received rehabilitation services for <1 year and those who received services a year or more. A one-year cutoff was adopted because the likelihood of dropping out of rehab is greatest during the first year (29, 35) and often is the result of the person not fitting in (e.g., not allowing therapeutic contact) or not complying with the service's rules (e.g., harassing or assaulting other service recipients). Completion of the first year often suggests that the person is benefiting from the service in terms of improved quality of life, clinical condition and social functioning, and rehabilitation is likely to be sustained for longer periods of time (28, 35, 36).
This secondary analysis study was conducted in accordance with the Helsinki Declaration and was approved by the IRB of the Israel Ministry of Health. Patients' identification information was anonymized from all datasets prior to being released to the researchers.
Associations between the independent variables [COD-status and length of housing/vocational rehabilitation in Period1 (2001–2009) and in Period2 (2010–2016)] and mean annual number of hospitalization days were assessed using χ2 and t-tests, as appropriate. Repeated measures ANOVA was used to track changes in hospitalization variables across the two time periods. Multivariate ANCOVA modeling for mean hospitalization days per year was performed to identify predictors including rehabilitation length, age, age at first hospitalization, sex, COD-status and percent of hospitalizations with SUD. Statistical significance level was set at p < 0.05 to help guide interpretation of the results. The data were analyzed using IBM® SPSS® Statistics, version 24.0.
Of the 18,684 persons with a psychiatric hospitalization between 2001 and 2016, 28.8% had a co-occurring disorder (Table 1). The COD group was predominantly male (85%) compared with 58% of the non-COD group, and was 3.5 years younger, on average, than the non-COD group. For persons with COD age at first hospitalization was 2.4 years younger than those without COD. The rate of approval by the regional rehabilitation committees for housing rehab services was slightly higher among those with chronic psychotic disorder without COD (90%; SD = 23%) than among persons with COD (85%; SD = 27%) (p < 0.0001). The rate of vocational rehabilitation service approval was identical in both groups (93%).
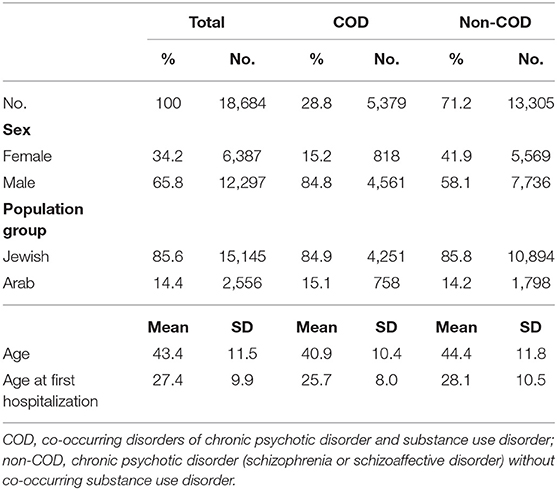
Table 1. Demographic characteristics of people with schizophrenia/schizoaffective disorder (aged 18–65) with a psychiatric hospitalization during the period 1963–2016, by co-occurring SUD status, Israel.
Regarding receipt of rehabilitation services, 63% of non-COD patients and 56% of those with COD received rehabilitation services at some point during 2001 and 2016 (p < 0.0001). In both groups, an increase over time was observed. Among patients without COD, 35% received rehabilitation services in Period1 and this rate increased to 56% in Period2, and among patients with COD the rehabilitation service rate increased from 30 to 48% across the two time periods (Table 2).
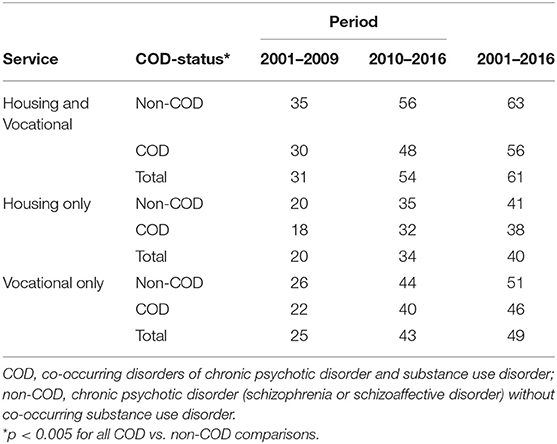
Table 2. Percent of patients who received housing and/or vocational rehabilitation services by period (2001–2009, 2010–2016) and overall, and by COD status.
As seen in Table 3, the average duration of housing and vocational rehabilitation services was shorter for COD patients than non-COD patients. It is worth noting that the mean duration of rehabilitation among those who received services for more than 1 year was 2–6 years (792–2223 days), while among those who received services for <1 year the mean duration was 4–6 months (132–191 days). Duration of rehabilitation was inversely associated with percent of hospitalizations with a SUD diagnosis (p < 0.001).
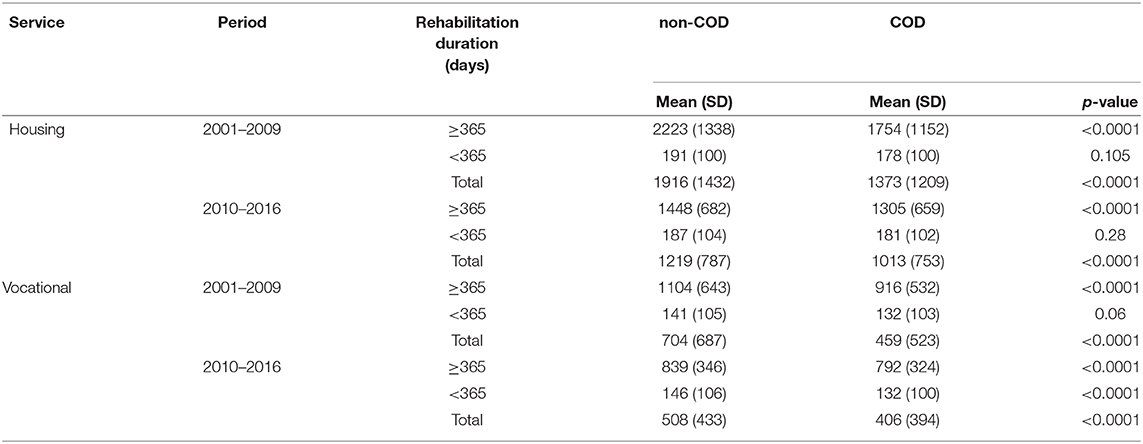
Table 3. Average duration of rehabilitation (in days) by period (2001–2009, 2010–2016) among recipients of housing and vocational rehabilitation services.
Overall, non-COD patients also received vocational rehabilitation for longer duration than COD-patients. 43% of people without COD who received vocational rehabilitation for more than a year in both periods, compared to 28% of people with COD (Table 3). Also, 18% of non-COD people received vocational rehabilitation for less than a year in both periods, compared to 28% of people with COD.
Among persons who received housing-rehabilitation both during Period1 and Period2, duration of rehab was inversely associated with annual number of hospitalization days. As seen in Figures 1, 2, the mean number of hospitalization days was highest for those who received housing or vocational rehabilitation services for <1 year. This was true for those with and without COD. In Period1 the mean number of hospital days was lowest among those who did not receive any rehabilitation, whereas in Period2 those who received more than 1 year of rehab experienced the fewest hospital days per year. COD-status was also significantly associated with hospitalization days—the mean number of hospitalization days/year was consistently higher among those with COD. Comparing Panel A and Panel B, a decrease in hospitalization days from Period1 to Period2 was noted only among those who received rehabilitation over a year. People who received vocational rehabilitation experienced fewer hospitalization days than people with housing rehabilitation (Figures 1, 2).
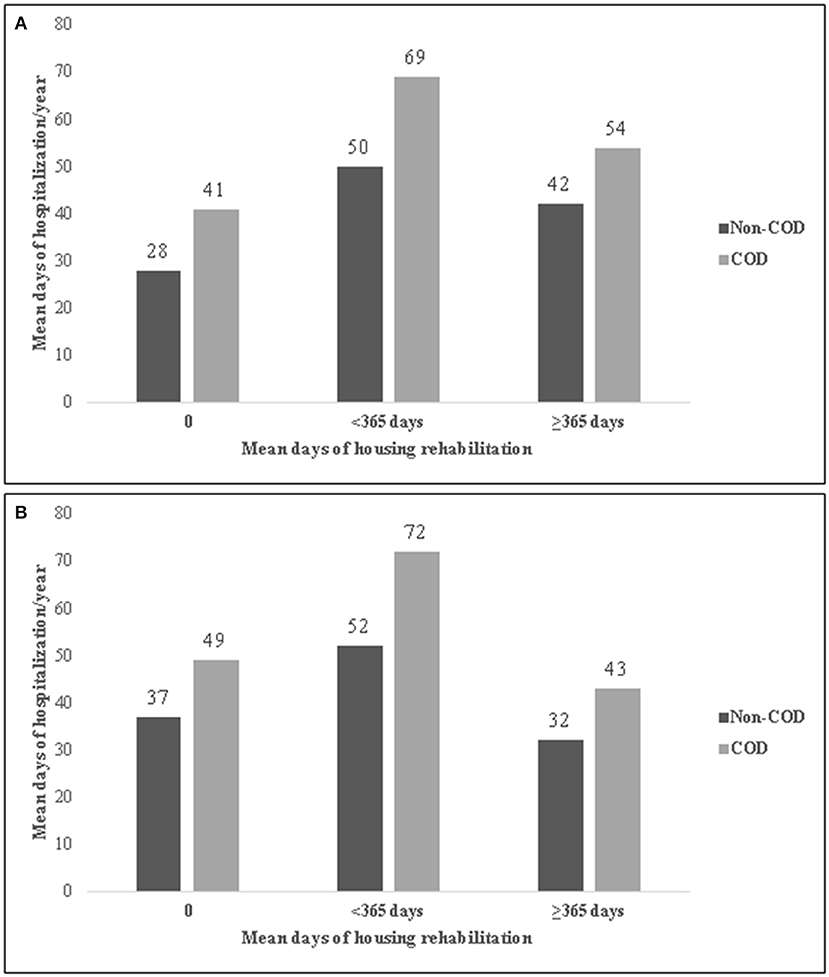
Figure 1. Mean psychiatric hospitalization days per year by duration of housing rehabilitation in Period1 (2001–2009) (A) and Period2 (2010–2016) (B), among hospitalized persons with co-occurring disorders (COD) of chronic psychotic disorder and SUD, Israel, 2010–2016. (A) Period1. (B) Period2.
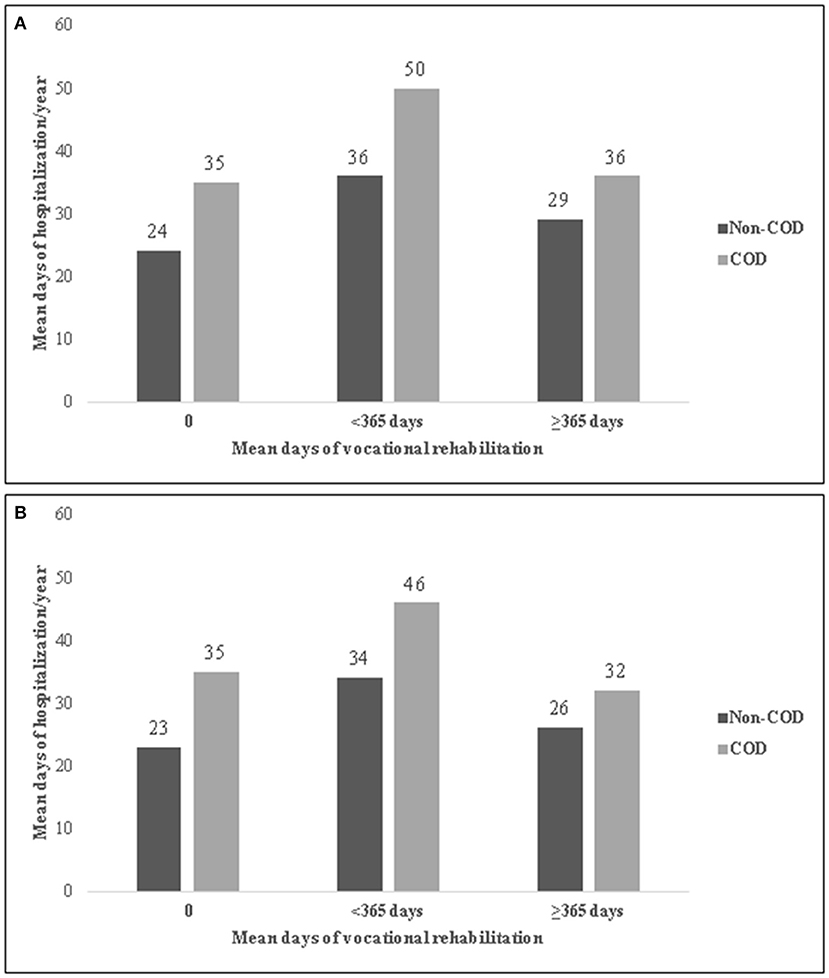
Figure 2. Mean psychiatric hospitalization days per year by duration of vocational rehabilitation in Period1 (2001–2009) (A) and Period2 (2010–2016) (B), among hospitalized persons with co-occurring disorders (COD) of chronic psychotic disorder and SUD, Israel, 2010–2016. (A) Period1. (B) Period2.
As seen in Figure 3, when we restricted the analysis to those who received any housing rehabilitation in both periods, for both groups, longer rehabilitation (more than 1 year) in both periods was associated with the fewest hospitalization days, and short rehab (<1 year) with the most hospitalization days.
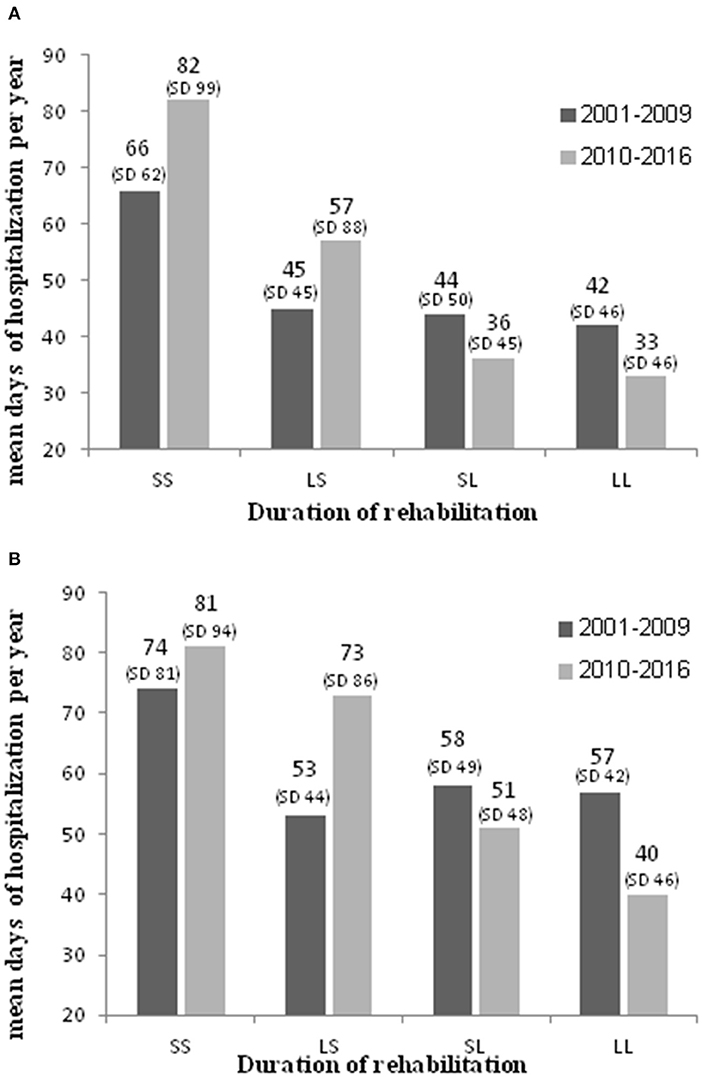
Figure 3. Mean psychiatric hospitalization days per year, by duration of housing rehabilitation in Period1 (2001–2009) and Period2 (2010–2016), among hospitalized persons with chronic psychotic disorder without co-occurring SUD (A) and with SUD (B) who received any housing rehabilitation, Israel, 2010–2016. (A) Hospitalized persons with chronic psychotic disorder without SUD. (B) Hospitalized persons with chronic psychotic disorder with SUD. SS, short rehabilitation in Period1 and Period2; LS, long rehabilitation in Period1 & short in Period2; SL, short rehabilitation in Period1 & long in Period2; LL, long rehabilitation in Period1 and Period2.
People without COD received housing rehabilitation for longer periods−79% of people without COD who received housing rehabilitation, received rehabilitation for more than a year in both periods, compared to 68% of people with COD. Also, 2% of people without COD received housing rehabilitation for less than a year in both periods, compared to 6% of people with COD (p < 0.0001).
As seen with housing rehabilitation, duration of vocational rehabilitation for patients who received any vocational rehabilitation in both periods was also inversely associated with mean days of hospitalization per year (p < 0.0001). Having received vocational rehabilitation for <1 year in either Period1 or Peroid2 was associated with a greater number of hospitalization days per year in 2010–2016 (Figure 4).
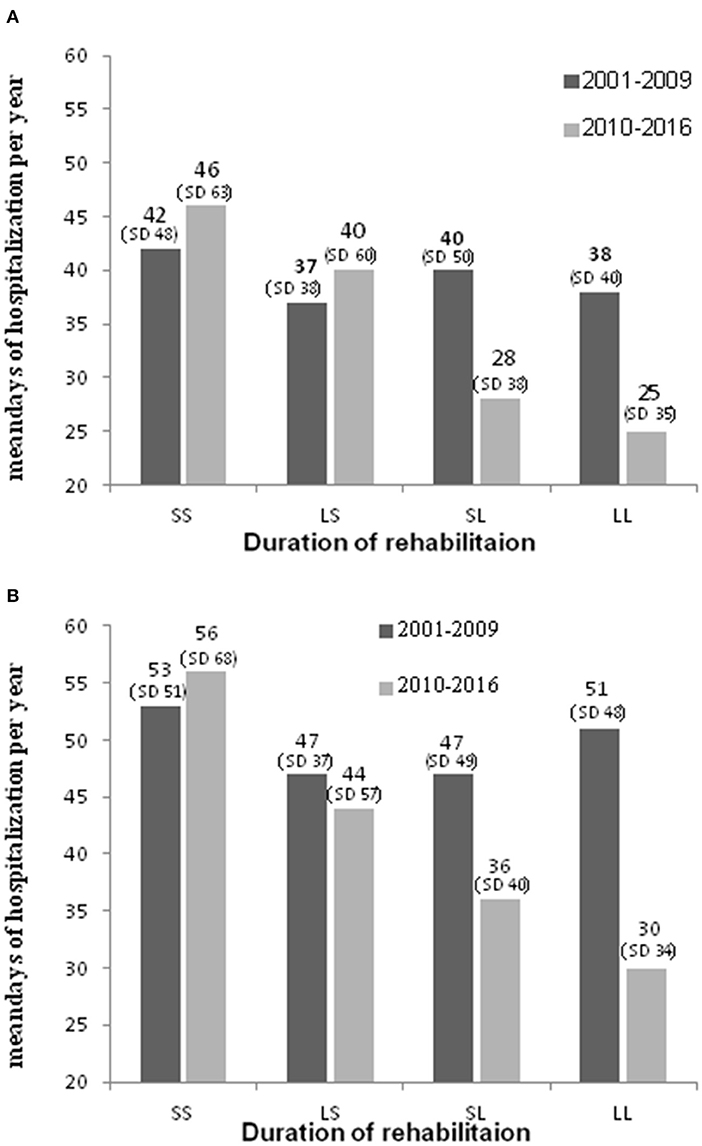
Figure 4. Mean psychiatric hospitalization days per year, by duration of vocational rehabilitation in Period1 (2001–2009) and Period2 (2010–2016), among hospitalized persons with chronic psychotic disorder without co-occurring SUD (A) and with SUD (B) who received any vocational rehabilitation, Israel, 2010–2016. (A) Hospitalized persons with chronic psychotic disorder without SUD. (B) Hospitalized persons with chronic psychotic disorder with SUD. SS, short rehabilitation in Period1 and Period2; LS, long rehabilitation in Period1 & short in Period2; SL, short rehabilitation in Period1 & long in Period; LL, long rehabilitation in Period1 and Period2.
People without COD received vocational rehabilitation for longer periods−43% of people without COD who received vocational rehabilitation received rehabilitation for more than a year in both periods, compared to 28% of people with COD. Also, 18% of non-COD people received vocational rehabilitation for less than a year in both periods, compared to 28% of people with COD (p < 0.0001).
The association between mean number of hospital days and rehabilitation remained significant upon controlling for age, sex, COD group, percent of hospitalizations with SUD, and age at first hospitalization. Multivariate ANCOVA modeling revealed a significant independent association between mean hospitalization days per year during 2010–2016 and COD-status (p < 0.0001). Numer of hospital days was independently associated with percent of hospitalizations with SUD (p = 0.025) and with male sex (p < 0.0001), and inversely associated with age at first hospitalization (p < 0.0001). Age at time of the study was not associated with annual number of hospitalization days.
The results show that from 2001–2009 to 2010–2016 there was an almost 2-fold increase in the proportion of people with chronic psychotic disorder who received rehabilitation. This trend is similar among COD and non-COD patients. In the latter period, two-thirds (63%) of persons without COD and slightly over half (56%) of those with COD received rehabilitation services. The increase in the proportion of people receiving rehabilitation services reflects the development of the rehabilitation system in Israel, which over the years has recognized the need to expand rehabilitative care in the community, thus opening more rehabilitative frameworks. These findings are consistent with previous reports regarding the growth of community rehabilitation services in the country (31, 37).
The percentage of people without COD who qualify for rehabilitation services was significantly greater than those with COD, although the difference is not large. We expected, in light of our clinical experience, a much larger disparity in rehabilitation eligibility in favor of persons without COD. In addition, until recently, and during most years of the current study, there was a declared policy of the Rehabilitation Committees of not providing services to people with active drug use (32). Several explanations for the discrepancy between our hypothesis and the results can be posited. One possible explanation is a cognitive bias which appeared in cases where the Rehabilitation Committee rejected a request for rehabilitation services, due to drug use history. This aroused negative feelings such as disappointment among therapists and patients, and thus such cases might be more recalled than cases where approval was obtained.
Another possibility of the described discrepancy is related to the definition of the COD group in our study (people with at least two hospitalizations, or at least 20% of their hospitalizations with an indication of SUD). We found that people from the COD group who received rehabilitation services, had SUD recorded in less than half of their hospitalizations. Approval for rehabilitation services might have been granted during hospitalizations without active SUD, whereas in other hospitalizations with active drug use, rehabilitation services were refused.
In addition, hospital therapists who submit the patient to the Rehabilitation Committee may not always fully disclose drug use information when the use is not very intense (even in the presence of SUD diagnosis), out of a concern that the information would cause the Committee to reject the request for rehabilitation services.
Our results indicate that persons who received rehabilitation for a longer duration (a year or more) in Period1 and/or Period2, had on average fewer hospitalization days annually in Period2 than those who received rehabilitation for <1 year. This finding corresponds with worldwide studies, including in Israel, which show that community rehabilitation services are associated with fewer hospitalization days and less frequent hospitalizations among people with schizophrenia (20–23).
The finding that people who did not receive rehabilitation services had fewer days of hospitalization than people who received rehabilitation is surprising at first glance. A possible explanation for this could be better underlying clinical condition or stronger support from family or other sources, which enable these persons to manage in the community without rehabilitation services. Indeed, the group who did not receive services includes a small proportion (<10%) whose application for rehabilitation services was refused.
The finding that those who received rehabilitation services for a short duration had, on average, more hospitalization days compared to people with longer rehabilitation, can be easily understood. People who dropped out from the rehabilitation setting may have been discharged from the hospital before a sufficient improvement was achieved and thus were not yet able to adapt to a rehabilitation community setting. It is also possible that joining a new therapeutic framework in the community posed a stressor they could not easily overcome, thus leading to a clinical exacerbation and re-hospitalization. Another explanation could be that some clinical or personality characteristic made it difficult for them to cope with the rehabilitation requirements and to benefit from the rehab services, and these same characteristics had an impact on the higher frequency of hospitalizations and greater number of hospitalization days per year.
The relatively low number of hospitalization days among people receiving longer-duration rehabilitation reinforces the assumption that prolonged rehabilitation is beneficial to patients' mental health and helps prevent re-hospitalization. This assumption is further supported by the finding that persons who received rehabilitation for a short time in Period1 and then received longer rehabilitation in Period2, experienced fewer days of hospitalization. At the same time, the possibility of an underlying confounding clinical or personality characteristic, as mentioned, or higher levels of intrinsic motivation and better family relationship (38) cannot be ruled out.
Duration of vocational rehabilitation, as well as housing rehabilitation, was found to be inversely associated with number of hospitalization days. Although we cannot assume independence between housing rehabilitation and vocational rehabilitation, as some may receive both, those who received vocational rehabilitation experienced fewer hospitalization days per year than those who received housing rehabilitation. Vocational rehabilitation, therefore, may have an even greater effect than housing rehabilitation on the patient's mental condition and on hospitalizations. Employment is especially important for people with COD, because it reduces a sense of emptiness by filling their time with productive activity, improves their quality of life and provides a sense of meaning and self-esteem. This may in turn lessen the emotional need to return to substance abuse and reduce the risk of relapse and re-hospitalizations (39, 40).
We previously reported that from 1991–2016 there was no improvement in the average number of days of hospitalization per year for people with COD, while for those without COD the number of hospitalization days was reduced by half (20). Nonetheless, the most striking results of the present study are that rehabilitation is at least as beneficial for people with COD as for those without COD, and this is also reflected in a decrease in hospitalization days for both groups. This, despite the fact that at the time of the study there were very few rehabilitation frameworks designed for COD patients, and therefore most chronic psychotic people with SUD underwent rehabilitation in settings that did not have COD specialty. However, this interpretation is posited with caution, since it is likely that non-specialized rehabilitation settings are most suitable for persons with lower severity of SUD, such as occasional drug abuse, while those with severe addiction are less likely to manage in a non-specialized setting.
The significantly higher annual number of hospital days, on average, among persons with co-occurring chronic psychotic disorders and SUD, even after controlling for age, sex and percent of hospitalizations with SUD and age at time of study, and the higher frequency of hospitalizations (20), may be a result of more frequent substance-related exacerbations of the clinical condition (8, 41), greater difficulty in cooperating with treatment over time, and longer periods of non-adherence to treatment, as compared with non-COD patients (11, 41–43).
It is also important to note that compared with those without COD, the COD group who received rehabilitation in 2001–2009 and 2010–2016, had a 2–3-fold higher proportion of people who received rehabilitation for less than a year. This might be attributed to personal characteristics of some persons with COD, such as impulsivity (44–46), or directly to drug use that led to the cessation of rehabilitation services, and/or to a shortage of rehabilitation frameworks specifically designed for COD patients.
This study utilized data from the Israel Mental Rehabilitation Register and the National Psychiatric Case Register that captures virtually all psychiatric hospitalizations. Complete hospitalization histories were obtained for all in-patients diagnosed with schizophrenia or schizoaffective disorder in Israel in the period 2010–2015. The retrolective design of the study precluded the analysis of some important demographic and clinical variables, such as severity of the psychotic disorder and SUD, level of functioning, degree of motivation for rehabilitation and level of family support. These factors affect the ability to sustain and benefit from rehabilitation services and on the likelihood of re-hospitalization. Because the severity of patients' SUD was unknown, it was not possible to ascertain whether SUD severity was related to being accepted into and staying in a rehabilitation framework. The relationship between the severity of SUD and the number of hospitalization days is also unknown. It is also possible that for some COD patients, SUD developed subsequent to their first hospitalization, or that SUD was less documented in earlier years. However, we found that for the majority of COD patients, SUD was already documented early in their hospitalization history. Specifically, 85% of patients hospitalized in both periods (2001–2009, 2010–2016) were already diagnosed with SUD in Period1. We believe therefore, that the cross-period comparisons are trustworthy, albeit perhaps with some margin of bias.
In addition, in our study, COD is defined as a SUD diagnosis present in at least two hospitalizations or in at least 20% of each patient's hospitalizations rather than the more commonly used “lifetime” or first-hospitalization SUD definition. We believe this enhances the COD diagnostic validity (specificity) as it describes a chronic comorbid drug use pattern. Indeed, on average, a SUD diagnosis was documented in more than half (54%) of all hospital admissions amongst those classified as COD. We did not adopt stricter COD criteria (i.e., SUD diagnosis appears on a greater proportion of admissions) out of a concern that the secondary SUD diagnosis may be under-recorded, as has been noted in other countries (47). Furthermore, since the standard urine drug tests used in Israel do not detect commonly-used novel psychoactive substances (NPS), suspected drug use cannot always be confirmed in the event that the patient denies use.
Twenty-nine individuals with more than 80 hospitalizations were not included in the analyses. The decision to exclude them stemmed from an impression that the excessive numbers of hospitalizations might have been due to double reporting. Regrettably, the data for these individuals is unavailable and we are unable to rerun the analyses with them included to assess the impact of the exclusion. We believe the impact is negligible given the small number excluded.
Lastly, the unequal duration of Period1 (2001–2009) and Period2 (2010–2016) may introduce some measure of confounding by factors differentially distributed across the two time periods. The periods were defined in accordance with the study objective to assess the government's decision to allocate additional resources toward the treatment and rehabilitation of persons with COD. We are unaware of any substantial temporal changes in treatment or quality of services, beyond the expansion of rehabilitation services. Defining the unit of analysis for number of hospital days as “per year” rather than per period, will have minimized the effect of any such confounding.
In summary, the results of our study show that people with COD appear to have the potential for significant rehabilitation when given the opportunity. Also, it seems that at least some people with COD can go through a prolonged rehabilitation process in the community even in settings that are not specifically designed for people with SUD. However, persons with COD are less likely to remain in rehabilitation for prolonged periods. Findings of this study show that when rehabilitation is prolonged and lasts for at least a year, there is a significant reduction in hospitalization days. These findings reinforce the clinical importance of sustained rehabilitation for people with COD, for whom longer rehabilitation may be required to commit to rehabilitation and to attain clinical stabilization than for persons without COD. It is likely that if rehabilitation frameworks are dedicated for people with COD, those with even more severe SUD may benefit from rehab and will be less likely to drop out early. The process of expanding the rehabilitation services designed for COD patients should be accelerated and more healthcare providers should be trained in evidence-based practices for COD. As this process continues to evolve, we will likely see a significant improvement in the clinical condition of these patients over time and in their ability to manage and re-integrate in the community, and as a result their need for hospitalizations is expected to decline.
The datasets analyzed in this study were obtained from the Ministry of Health of Israel. Access to the data is highly restricted due to the sensitive nature of pyschiatric patient data. Requests to access these datasets should be directed to Mr. Reuven Eliyahu (cmV1dmVuLmVsaWFodUBtb2guZ292Lmls) Data Security Office, Ministry of Health.
All the authors designed the study. SF wrote the first draft of the manuscript. TB-A designed the methods for data analysis. YN and PR proofed and revised the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J. Clin. Psychiatry. (2006) 67(Suppl. 7):5–9. doi: 10.4088/JCP.0706e01
2. Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiatry. (2014) 71:248–54. doi: 10.1001/jamapsychiatry.2013.3726
3. European Monitoring Centre for Drugs and Drug Addiction. Co-morbid Substance Use and Mental Disorders in Europe: A Review of the Data, EMCCODA Papers. Luxembourg: Publications Office of the European Union (2013). Available online at: http://www.emcCODa.europa.eu/attachements.cfm/att_220660_EN_TDAU13002ENN.pdf (accessed January 21, 2021).
4. Nesvåg R, Knudsen GP, Bakken IJ, Høye A, Ystrom E, Surén P, et al. Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: a registry-based study. Soc. Psychiatry Psychiatr. Epidemiol. (2015) 50:1267–76. doi: 10.1007/s00127-015-1025-2
5. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) study. JAMA Psychiatry. (1990) 264:2511–8. doi: 10.1001/jama.264.19.2511
6. Toftdahl NG, Nordentoft M, Hjorthøj C. Prevalence of substance use disorders in psychiatric patients: a nationwide Danish population-based study. Soc. Psychiatry Psychiatr. Epidemiol. (2016) 51:129–40. doi: 10.1007/s00127-015-1104-4
7. Florentin S, Rosca P, Raskin S, Bdolah-Abram T, Neumark Y. Psychiatric hospitalizations of chronic psychotic disorder patients with and without dual diagnosis, Israel, 1963-2016. J. Dual Diagn. (2019) 15:130–9. doi: 10.1080/15504263.2019.1609149
8. Winklbaur B, Ebner N, Sachs G, Thau K, Fischer G. Substance abuse in patients with schizophrenia. Dialogues Clin Neurosci. (2006) 8:37–43. doi: 10.31887/DCNS.2006.8.1/bwinklbaur
9. Janssen B, Gaebel W, Haerter M, Komaharadi F, Lindel B, Weinmann S. Evaluation of factors influencing medication compliance in inpatient treatment of psychotic disorders. Psychopharmacology. (2006) 187:229–36. doi: 10.1007/s00213-006-0413-4
10. Mueser KT, Drake RE, Wallach MA. Dual diagnosis: a review of etiological theories. Addict. Behav. (1998) 23:717–34. doi: 10.1016/S0306-4603(98)00073-2
11. Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia – a 15-year follow-up study: dual diagnosis over 15 years. Schizophr. Res. (2011) 130:228–33. doi: 10.1016/j.schres.2011.04.011
12. Swartz MS, Wagner HR, Swanson JW, Stroup TS, McEvoy JP, Canive JM, et al. Substance use in persons with schizophrenia: baseline prevalence and correlates from the NIMH CATIE study. J. Nerv. Ment. Dis. (2006) 194:164–72. doi: 10.1097/01.nmd.0000202575.79453.6e
13. Lybrand J, Caroff SN. Management of schizophrenia with substance use disorders. Psychiatr. Clin. North Am. (2009) 32:821–33. doi: 10.1016/j.psc.2009.09.002
14. Adan A, Arredondo AY, Capella MD, Prat G, Forero DA, Navarro JF. Neurobiological underpinnings and modulating factors in schizophrenia spectrum disorders with a comorbid substance use disorder: a systematic review. Neurosci. Biobehav. Rev. (2017) 75:361–77 doi: 10.1016/j.neubiorev.2017.01.038
15. Stoychev KR. Neuroimaging studies in patients with mental disorder and co-occurring substance use disorder: summary of findings. Front. Psychiatry. (2019) 10:702. doi: 10.3389/fpsyt.2019.00702
16. Asher L, Patel V, De Silva M. Community-based psychosocial interventions for people with schizophrenia in low and middle-income countries: systematic review and meta-analysis. BMC Psychiatry. (2017) 17:355. doi: 10.1186/s12888-017-1516-7
17. Brekke JS, Long JD. Community-based psychosocial rehabilitation and prospective change in functional, clinical, and subjective experience variables in schizophrenia. Schizophr. Bull. (2000) 26:667–80. doi: 10.1093/oxfordjournals.schbul.a033485
18. Cook J, Pickett S, Razzano L, Fitzgibbon G, Jonikas J, Cohler J. Rehabilitation services for persons with schizophrenia. Psychiatr. Ann. (1996) 26:97–9. doi: 10.3928/0048-5713-19960201-11
19. Roe D, Werbeloff N, Gelkopf M. Do persons with severe mental illness who consume the psychiatric rehabilitation basket of services in Israel have better outcomes than those who do not? Isr. J. Psychiatry Relat. Sci. (2010) 47:166–70.
20. Florentin S, Neumark Y, Raskin S, Bdolah-Abram T, Rosca P. Differential effect of community rehabilitation reform on hospitalizations of patients with chronic psychotic disorders with and without substance use disorder, Israel, 1991–2016. Adm. Policy Ment. Health (2020). doi: 10.1007/s10488-020-01077-4. [Epub ahead of print].
21. Hutchison SL, MacDonald-Wilson KL, Karpov I, Maise AM, Wasilchak D, Schuster JM. Value of psychiatric rehabilitation in a behavioral health medicaid managed care system. Psychiatr. Rehabil. J. (2017) 40:216–24. doi: 10.1037/prj0000271
22. Krieger I, Bitan DT, Sharon-Garty R, Baloush-Kleinman V, Zamir L. The effect of community-based mental health rehabilitation services for schizophrenia: a retrospective cohort study. Psychiatr. Q. (2020) 91:1453–63. doi: 10.1007/s11126-020-09772-z
23. Sytema S, Burgess P, Tansella M. Does community care decrease length of stay and risk of rehospitalization in new patients with schizophrenia disorders? Schizophr. Bull. (2002) 28:273–81. doi: 10.1093/oxfordjournals.schbul.a006937
24. Ministry of Health (2020). Available online at: https://www.health.gov.il/English/Topics/MentalHealth/rehabilitation/Pages/default.aspx (accessed October 12, 2020).
25. Natan G. Treatment of Drug Dependent Persons With Co-morbid Mental Illness. Report to the Israeli Parliament (Knesset), Jerusalem (2010). Available online at: https://fs.knesset.gov.il/globaldocs/MMM/ed566b58-e9f7-e411-80c8-00155d010977/2_ed566b58-e9f7-e411-80c8-00155d010977_11_10107.pdf (accessed January 21, 2021).
26. Aviram U, Ginath Y, Roe D. Mental health reforms in Europe: Israel's rehabilitation in the community of persons with mental disabilities law: challenges and opportunities. Psychiatr. Serv. (2012) 63:110–2. doi: 10.1176/appi.ps.201100009
27. Aviram U, Azary-Viesel S. Mental health reform in Israel: challenge and opportunity. Part I: fundamentals of the reform and the mental health service system on the eve of the reform. Isr. J. Psychiatry Relat. Sci. (2018) 55:45–54.
28. Hornik-Lurie T, Zilber N, Lerner Y. Trends in the use of rehabilitation services in the community by people with mental disabilities in Israel; the factors involved. Isr. J. Health Policy Res. (2012) 1:24. doi: 10.1186/2045-4015-1-24
29. Grinshpoon A, Abramowitz MZ, Lerner Y, Zilber N. Re-hospitalization of first-in-life admitted schizophrenic patients before and after rehabilitation legislation: a comparison of two national cohorts. Soc. Psychiatry Psychiatr. Epidemiol. (2007) 42:355–9. doi: 10.1007/s00127-007-0167-2
30. Roe D, Hasson-Ohayon I, Lachman M, Kravetz S. Selecting and implementing evidence-based practices in psychiatric rehabilitation services in Israel: a worthy and feasible challenge. Isr. J. Psychiatry Relat.Sci. (2007) 44:47–53.
31. Roe D, Lachman M, Mueser KT. Editorial: a decade of the Israeli psychiatric rehabilitation law. Isr. J. Psychiatry Relat. Sci. (2010) 47:164–5.
32. Florentin S, Raskin S. Co-occurring schizophrenia and substance use disorder: etiological theories and challenges in Israel. Harefuah. (2017) 156:715–9.
33. Lichtenberg P, Kaplan Z, Grinshpoon A, Feldman D, Nahon D. The goals and limitations of Israel's psychiatric case register. Psychiatr. Serv. (1999) 50:1043–8. doi: 10.1176/ps.50.8.1043
34. World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics, 11th Revision (2018).
35. Struch N, Shereshevsky Y, Naon D, Daniel N, Fischman N. People With Severe Mental Disorders in Israel: An Integrated View of the Service Systems. Jerusalem: Myers-JDC-Brookdale Institute (2009).
36. Mueser K, Drake RE, Bond GR. Recent advances in psychiatric rehabilitation for patients with severe mental illness. Harvard Rev. Psychiatry. (1997) 5:123–37. doi: 10.3109/10673229709000298
37. Aviram U. Promises and pitfalls on the road to a mental health reform in Israel. Isr. J. Psychiatry Relat. Sci. (2010) 47:171–94.
38. Lim C, Barrio C, Hernandez M, Barragán A, Brekke JS. Recovery from schizophrenia in community-based psychosocial rehabilitation settings: rates and predictors. Res. Soc. Work Pract. (2017) 27:538–51. doi: 10.1177/1049731515588597
39. Petry NM, Andrade LF, Rash CJ, Cherniack MG. Engaging in job-related activities is associated with reductions in employment problems and improvements in quality of life in substance abusing patients. Psychol. Addict. Behav. (2014) 28:268–75. doi: 10.1037/a0032264
40. Manuel JI, Yuan Y, Herman DB, Svikis DS, Nichols O, Palmer E, Deren S. Barriers and facilitators to successful transition from long-term residential substance abuse treatment. J. Subst. Abuse Treat. (2017) 74:16–22. doi: 10.1016/j.jsat.2016.12.001
41. Colizzi M, Carra E, Fraietta S, Lally J, Quattrone D, Bonaccorso S, et al. Substance use, medication adherence and outcome one year following a first episode of psychosis. Schizophr. Res. (2016) 170:311–7. doi: 10.1016/j.schres.2015.11.016
42. Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J. Clin. Psychiatry. (2006) 67:453–60. doi: 10.4088/JCP.v67n0317
43. Phan SV. Medication adherence in patients with schizophrenia. Int. J. Psychiatr. Med. (2016) 51:211–9. doi: 10.1177/0091217416636601
44. Marquez-Arrico JE, López-Vera S, Prat G, Adan A. Temperament and character dimensions in male patients with substance use disorders: differences relating to psychiatric comorbidity. Psychiatry Res. (2016) 237:1–8. doi: 10.1016/j.psychres.2016.01.061
45. Río-Martínez L, Marquez-Arrico JE, Prat G, Adan A. Temperament and character profile and its clinical correlates in male patients with dual schizophrenia. J. Clin. Med. (2020) 9:1876. doi: 10.3390/jcm9061876
46. Richardson GB, Freedlander JM, Katz EC, Dai C-L, Chen C-C. Impulsivity links reward and threat sensitivities to substance use: a functional model. Front. Psychol. (2014) 5:1194. doi: 10.3389/fpsyg.2014.01194
Keywords: schizophrenia, substance use disorder, rehabilitation, co-occurring disorders, hospitalizations, Israel
Citation: Florentin S, Rosca P, Bdolah-Abram T and Neumark Y (2021) Community Rehabilitation and Hospitalizations Among People With Chronic Psychotic Disorder: Is There a Differential Association by Co-occurring Substance Use Disorder? Front. Psychiatry 12:621259. doi: 10.3389/fpsyt.2021.621259
Received: 25 October 2020; Accepted: 13 January 2021;
Published: 05 February 2021.
Edited by:
Frances Louise Dark, Metro South Addiction and Mental Health Services, AustraliaReviewed by:
Giacomo Deste, Civil Hospital of Brescia, ItalyCopyright © 2021 Florentin, Rosca, Bdolah-Abram and Neumark. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yehuda Neumark, eWVodWRhbkBla21kLmh1amkuYWMuaWw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.