
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 03 March 2021
Sec. Public Mental Health
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.616016
This article is part of the Research Topic Resilience and Health in the Chinese People during the COVID-19 Outbreak View all 22 articles
Background: Hemodialysis patients not only suffer from somatic disorders but are also at high risks of psychiatric problems. Early this year, the outbreak of coronavirus disease 2019 (COVID-19) has caused great panic and anxiety worldwide. The impact of this acute public health event on the psychological status of hemodialysis patients and its relationship with their quality of life have not been fully investigated.
Methods: This study comprised two parts. The initial study enrolled maintenance hemodialysis patients treated in Ruijin Hospital for more than 3 months from March to May 2020 during the ongoing COVID-19 pandemic. Patients completed three questionnaires including the Impact of Events Scale–Revised (IES-R), General Health Questionnaire-28 (GHQ-28), and Kidney Disease Quality of Life (KDQOL) Short Form (SF). Follow-up study was performed from December 2020 to January 2021, when the pandemic of COVID-19 has been effectively contained in China. Only patients enrolled in the initial study were approached to participate in the follow-up study.
Results: There were 273 maintenance dialysis patients enrolled in the initial study and 247 finished the follow-up study. For the initial study, the estimated prevalence of nonspecific psychiatric morbidity was 45.8% (125/273) by GHQ-28. By IES-R, 53/273 (19.4%) patients presented with total scores above 24 that reflected clinical concerns. We found a significant difference regarding KDQOL scores between patients with different stress response (IES-R) groups (p = 0.026). Our follow-up study showed that KDQOL and SF-36 scores were significantly improved in comparison with those in the initial study (p = 0.006 and p = 0.031, respectively). Though total scores of GHQ-28 and IES-R did not change significantly, some subscales improved with statistical significance. Furthermore, gender, education background, and duration of hemodialysis were three factors that may affect patients' mental health, quality of life, or health status while dialysis duration was the only variable that correlated with those parameters. However, these correlations were combined effects of the COVID-19 pandemic and the dialysis itself.
Conclusions: We found a correlation between changes in the mental health status of dialysis patients and changes in their quality of life. These responses were also mediated by patients' psychosocial parameters. Our results urge the necessity of psychotherapeutic interventions for some patients during this event.
Chronic kidney disease (CKD) is now a global health problem that affects one out of 10 adults worldwide (1, 2). In China, the overall prevalence of CKD was about 10.8% in 2012 (3) and the figure is still increasing. Regardless of the pathogenesis of the disease, the progression of CKD would ultimately lead to end-stage renal disease (ESRD)—a devastating disease that requires dialysis or transplantation in some patients. The impact of ESRD is huge not only in terms of its repercussions on patients but also its burden on the health resources.
In addition to somatic disorders caused by the disease and its complications, ESRD patients also experience high prevalence of psychiatric problems (4, 5). Anxiety or depression occurs in ~10–45% of patients with hemodialysis (6–8). These mental disorders would cause not only non-compliance to treatment but also severe consequences. Consequently, mental health problems in these patients are closely associated with their morbidity and mortality (9, 10). Moreover, psychological variables and aspects of the social environment add much difficulty to the management of their psychological disorders because these factors are intersecting and complex. Given this background, investigating psychosocial factors affecting ESRD patients would provide us with knowledge to identify and manage psychiatric problems in this population.
Psychosocial factors are a vast number of intersecting variables that include individual demographic features, psychologic and behavioral characteristics, social or environmental factors, and patient-level variables. Any factors causing failure of these variables to return to normal would lead to abnormality of the allostatic system and result in psychological disorders in patients. In early 2020, the outbreak of the novel coronavirus disease 2019 (COVID-19) has caused great panic and anxiety worldwide. The pandemic nature of the disease makes vulnerable populations at high risk of infection and causes great stress among patients with hemodialysis. However, the impact of this acute public health event on the psychological status of those patients has not been fully investigated. In this study, we focus on the psychological profiles of patients with hemodialysis in this event to provide a better understanding of the influence of psychosocial factors on the mental health of this population.
The initial study was performed between March and May 2020 in the hemodialysis center of Ruijin Hospital affiliated to Shanghai Jiaotong University School of Medicine to study the psychological profiles of the patients during ongoing COVID-19 pandemic. All patients under hemodialysis therapy for at least 3 months were approached to participate in the initial study. The follow-up study was performed between December 2020 and January 2021 to compare the psychological profiles of the patients after COVID-19 pandemic. Only patients enrolled in the initial study were approached to participate in the follow-up study.
Patients completed three validated questionnaires, including the revised version of Impact of Events Scale, General Health Questionnaire-28, and Kidney Disease Quality of Life Short Form.
The Impact of Events Scale–Revised (IES-R) is a 22-item self-report instrument assessing subjective distress resulting from everyday trauma or acute stress. We adapted IES-R to assess the presence and severity of psychological symptoms experienced by subjects at any time during the current acute public events. Likert rating scale from 0 to 4 was used for each item of IES-R, and the total score was 0 to 88. Total scores of IES-R that exceed 24 reflect clinical concern (11), scores above 33 reflect a probable diagnosis of post-traumatic stress disorder (PTSD) (12), and scores above 37 reflect suppression of immune system function (13). The IES-R has been translated into Chinese and validated in literature (14, 15).
The General Health Questionnaire-28 (GHQ-28) is a 28-item screening tool to detect non-specific psychiatric disorders among individuals in primary care settings (16, 17). GHQ-28 is designed to measure mental health disorders and could be grouped into four subscales: somatization, anxiety, social dysfunction, and depression. Each item is assessed using the 0-0-1-1 scoring method. The total score on the GHQ-28 ranges from 0 to 28 (18). We adopted a cutoff score of 12 out of 28 (those who answered positively to 12 questions would be considered a “case”) (18).
The Kidney Disease Quality of Life Short Form (KDQOL-SF), which has been used in ESRD patients widely, assesses the quality of life of patients with kidney diseases (19). KDQOL-SF comprises 43 disease-specific items (symptoms/problem list, effects of kidney disease, burden of kidney disease, work status, cognitive function, quality of social interaction, sexual function, sleep, social support, dialysis staff encouragement, and patient's satisfaction), 36 generic items (physical functioning, role—physical, pain, general health, emotional well-being, social function, and energy/fatigue), and background information. KDQOL-36 has been translated and validated in Chinese population (20).
Statistical analysis was performed using SPSS 13.0 (SPSS Inc.). Data with normal distribution were summarized as mean ± SD. Data without normal distribution were summarized as median. Comparisons were made using the Student t-test or one-way ANOVA for continuous variables and the χ2-test for categorical variables as required. Pearson correlations were derived, and tests of significance were set at 0.05. Multiple regression analysis was used to analyze association between different variables.
The flow diagram of study is demonstrated in Figure 1. There were 273 maintenance dialysis patients enrolled in the initial study. Male patients composed 58.6% of all the patients, and primary glomerulonephritis was the most common cause (71.8%) of ESRD. Majority of the patients (70.3%, 192/273) received education of secondary or less. At the time of survey, only 16.1% (44/273) of the patients had full or part time job. The baseline characteristics are summarized in Table 1. During follow-up, two patients received renal transplantation and 24 died; the remaining 247 patients finished the follow-up study.
Table 2 summarizes the psychological profiles (GHQ-28, IES-R) and quality of life of the patients (KDQOL and SF-36) during the initial study and follow-up study.
The initial study, which was performed in the ongoing COVID-19 pandemic, showed the total score of GHQ-28 was 13.1 in our patients. A higher score signifies a greater number of symptoms, and details of GHQ subscales are summarized in Table 2. By adopting a cutoff score of 12 out of 28 (18), we found an estimated prevalence of non-specific psychiatric morbidity of 45.8% (125/273). Furthermore, the mean scores for social dysfunction and somatic symptoms were higher compared with the mean scores for anxiety and insomnia and for depression.
Total score and scores of subscales of IES-R are also shown in Table 2. In our study, 53/273 (19.4%) patients presented with total scores above 24, which reflected clinical concerns. Among those patients, 5/273 (1.8%) patients had a probable diagnosis of post-traumatic stress disorder (PTSD) with score >33, and 29/279 (10.6%) patients had scores above 37, which reflected the suppression of immune system functioning.
The follow-up study showed that KDQOL and SF-36 scores significantly improved compared with those in the initial study (p = 0.006 and p = 0.031, respectively), which suggested the improved quality of life after COVID-19 pandemic in our patients. We also compared the total GHQ-28 score and IES-R score. Though total scores of these two scales showed no significant difference, improved somatization symptoms, anxiety and insomnia, and intrusion subscales were found in the follow-up study (p = 0.006, p = 0.005, and p = 0.049, respectively).
We divided the patients into different psychopathology groups according to their IES-R scores or GHQ-28 scores to investigate the interplay between psychiatric diagnosis and quality of life during ongoing COVID-19 pandemic.
By adopting a cutoff of 12 out of 28 by GHQ-28, we did not find any significant difference regarding KDQOL or SF-36 between patients with non-specific psychiatric disorders (GHQ-28 score ≥12) and those without (p > 0.05, data not shown). If we divided patients based on IES-R scores, we found a significant difference regarding KDQOL between different groups (p = 0.026) (Table 3). Furthermore, four subscales of KDQOL (work status, cognitive function, quality of social interaction, and sleep) were found significantly different (p = 0.027, p = 0.022, p = 0.010, and p = 0.039, respectively). However, we did not find a significant difference regarding SF-36 and its subscales between different groups.
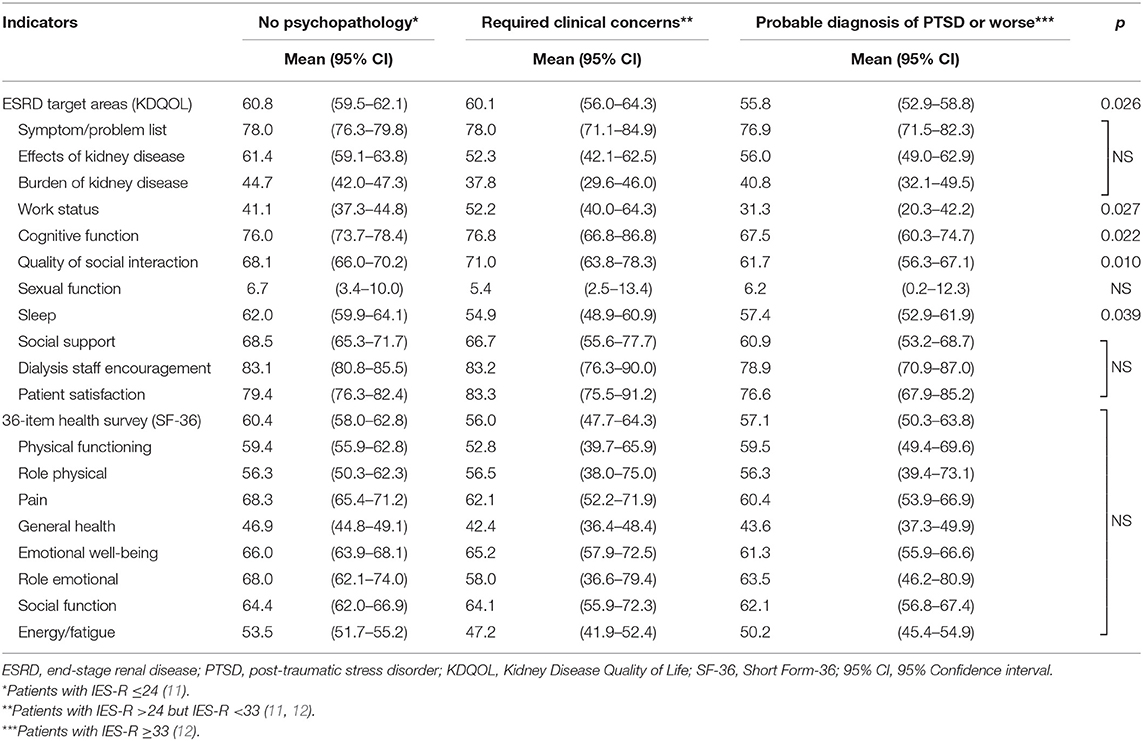
Table 3. Effects of acute stress on quality of life of the patients during ongoing COVID-19 pandemic.
Table 4 summarizes the effects of demographic factors on patients' mental health status and quality of life. We presented the results of GHQ-28, IES-R, KDQOL, and SF-36 total score as measures in relation to various demographic experiences. Our results showed that gender, education background, and duration of hemodialysis were three important factors that may affect patients' mental health, quality of life, or health status.
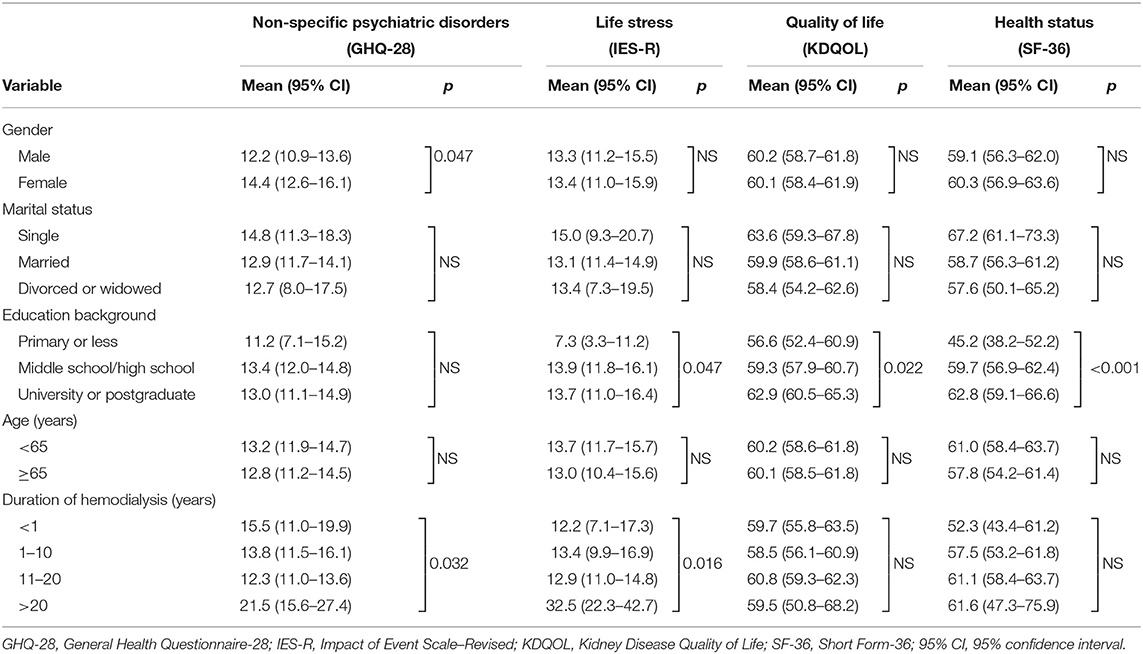
Table 4. Effects of demographic and exposure variables on mental status and quality of life of the patients during ongoing COVID-19 pandemic.
In our study, GHQ-28 was correlated to IES-R, which suggested patients' mental health status was correlated to their stress response (Table 5). Similarly, KDQOL was also correlated to SF-36, suggesting quality of life and health status were both correlated. Furthermore, IES-R was negatively correlated with KDQOL with statistical significance, which suggested patients' quality of life was negatively affected by their distress from acute events.
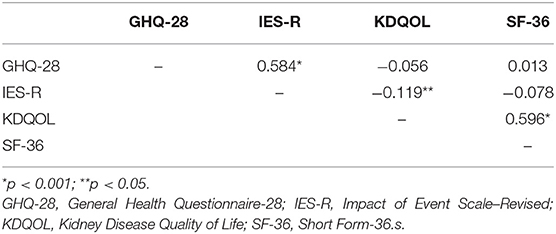
Table 5. Correlation coefficients for the GHQ-28, IES-R, KDQOL, and SF-36 during ongoing COVID-19 pandemic.
We also analyzed the results of total scores of GHQ-28, IES-R, and KDQOL-SF in relation to various demographic variables. Our results showed KDQOL and SF-36 were both intercorrelated. Furthermore, dialysis duration was the only variable that correlated patients' mental health status (GHQ-28), response to stress (IES-R), and health status (SF-36). The correlation of other variables is summarized in Table 6.
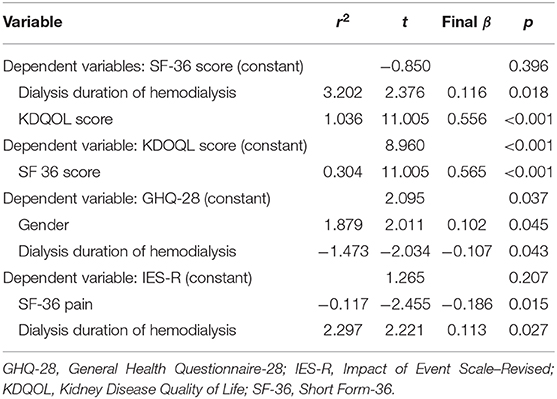
Table 6. Multiple regression of dependent variables and related factors during ongoing COVID-19 pandemic.
Psychological disorders among dialysis patients are not simply a consequence of short-term adjustment reaction to regimens but a long-term concomitant of coping with chronic dialysis and ESRD complications. In a recent cohort study, 22% of patients receiving maintenance hemodialysis had anxiety symptoms and 42% had depressive symptoms. In our study, the estimated prevalence of non-specific psychiatric morbidity was 45.8% by GHQ-28. Furthermore, the psychological disorders are closely associated with all-cause mortality and prolonged hospitalizations (21). Both our results and data from the literatures suggest the mental health disorders among dialysis patients are prevalent, which require timely diagnosis and adequate intervention so as to reduce mortality and improve prognosis.
Many factors contribute to poor mental health status among dialysis patients. Psychosocial parameter is one of such key factors. According to definition, it refers to a group of psychological variables and aspects of social environment that are central to individual's perception of quality of life (9). By adding burden of existing mental health status, psychosocial parameter could worsen patients' psychological status. Meanwhile, patients' perception accompanying the stressor could influence their functional status and eventually affect their prognosis (9). In our study, the average score of KDQOL and SF-36 was higher than those reported by Spain and US (22, 23). Such difference might reflect the influence of current acute public events on patients' quality of life. By further comparison of initial study, our follow-up study demonstrated that KDQOL and SF-36 scores as well as some subscales of GHQ-28 and IES-R were significantly improved after pandemic of COVID-19. Since disease itself and mitigation strategies during COVID-19 pandemic like home isolation, intense health monitoring, and many others would greatly affect dialysis patients' daily lives and access to dialysis therapy, our results thus suggest patients' quality of life and their mental health is greatly influenced by social environmental factors. It was also shown in the current study that gender and education background were two parameters associated with patients' mental health status as well as kidney disease quality of life. Education background determines patients' knowledge and perception to social environmental variables and compliance to renal replacement therapy, while gender is closely associated with other psychosocial factors like employment, income, education, and more; these intersected variables would consequently affect patients' mental health status and their physical well-being. Studies pointed out that psychosocial factors could affect patients' outcome by several mechanisms, which included access to health care, compliance with the dialysis therapy, and their health status (24). Our results thus suggest patient-level psychosocial parameters should receive special attention especially during stressing events as they could affect patients' mental health status as well as their kidney disease quality of life.
Though the prevalence of mental health disorders among dialysis patients is high, they are difficult to identify especially in patients with the backdrop of chronic dialysis. Overlap between uremic symptoms resulted from inadequate dialysis, and depressive symptoms add much difficulty to distinguish and manage dialysis patients with psychological disorders. One possible way to differentiate between psychiatric illness and medical illness is to delineate differences in thinking styles (25). By using professional tools like Diagnostic and Statistical Manual of Mental Disorders (DSM), patient's psychological disorders could be differentiated from mental health problems stemming from medical illness (25, 26). However, these tools are professional and sophisticated, which prevent them from being widely used in clinical practice. An alternative method to evaluate patients' psychological status is to use self-reporting screening tool that does not require professional knowledge to interpret. In our study, we adopted GHQ-28 to detect non-specific psychiatric morbidities among our patients. Results showed scores of social dysfunction and somatic symptoms were higher than anxiety or depression in our patients. Though the subscales of GHQ-28 are not designed to make a psychiatric diagnosis, these scores provide information for somatic, anxiety, social dysfunction and severe depression symptoms. Our results thus imply more attention should be paid to patients' social deficits as they may require more clinical concerns.
We also investigated patients' psychological response to acute stress during the current pandemic event. Stress indicates the change in the physical condition, environment, or psychosocial setting of an organism. It refers to the ability to achieve stability through changes. Failure of levels of stress mediator to return to baseline after challenge would cause abnormality of stress response. Since stressor and functional status of the subjects are two fundamental determinants of stress outcome (9), any changes in patient's status in personal or social contexts could result in depression, anxiety, or development of other mental health problems. By using IES-R, we investigated the psychological symptoms relating to various types of event exposure. Our results indicated that exposure to current acute stress and related events like home isolation, being quarantined, contact tracing, and many others contributed to the psychological symptoms of the patients with dialysis. Similar results were also reported by Wu and colleagues (14) who investigated psychological status of healthcare workers exposed to SARS-related events and found post-traumatic stress (PTS) symptom levels were closely associated with the outbreak of the disease and people's perception levels of the events were related to symptom levels.
We found that IES-R score was negatively correlated to KDQOL score in the current study. IES-R score was adopted for subjective distress from acute stress, and the higher score represented for the more severe psychological symptoms. The way patients respond to the stress would affect their perception and consequently influence their medical outcomes. Therefore, patients with higher IES-R score would have lower level of kidney quality of life. In a recent multicenter study, García-Martínez and colleagues (23) found that patients' resilience to stress was associated with their quality of life. Their results are consistent with our findings, which suggest patients' response to stress would have an impact on different aspects of their quality of life. In light of the important role of patients' response to acute stress, improving their resilience and coping capability with acute stress would help to increase quality of life and decrease the frequency of hospitalization in patients with hemodialysis (27–29).
There are several limitations that must be acknowledged in the current study. First, we did not provide historical profiles of the patients as controls because many patients began their dialysis therapy long before current evaluating tools were introduced in China. We therefore performed the follow-up study when COVID-19 pandemic was effectively contained and made the comparison. Second, our hospital is located in the downtown of the city and most of our patients are from urban areas. Considering social economic status, education background, and some other variables are different between urban and rural areas, data in the current study might not fully represent those from rural areas. Third, the cross-sectional nature of the study made it difficult to establish causal relationship between risk perception and mental health disorders. Last, the subjects' self-reports in the current study were subject to recall bias.
Regardless of the mentioned limitations, our data do provide information regarding psychological impact of acute public events on dialysis patients. Our results urge the necessity of psychotherapeutic interventions for some patients during the current public health event.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Review Board of Ruijin Hospital. The patients/participants provided their written informed consent to participate in this study.
Z-HY wrote the manuscript. X-TP, YC, LW, Q-XC, YZ, and Y-JZ collected the data. Y-XC and Z-HY designed the study and analyzed the data. X-NC and Y-XC reviewed the manuscript and approved the submission. All authors contributed to the article and approved the submitted version.
The authors acknowledge the support from the Research from Shanghai Municipal Key Clinical Specialty (shslczdzk02502).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Li PK, Garcia-Garcia G, Lui SF, Andreoli S, Fung WW, Hradsky A, et al. Kidney health for everyone everywhere: from prevention to detection and equitable access to care. J Nephrol. (2020) 33:201–10. doi: 10.1007/s40620-020-00728-x
2. Eckardt KU, Coresh J, Devuyst O, Johnson RJ, Kottgen A, Levey AS, et al. Evolving importance of kidney disease: from subspecialty to global health burden. Lancet. (2013) 382:158–69. doi: 10.1016/S0140-6736(13)60439-0
3. Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. (2012) 379:815–22. doi: 10.1016/S0140-6736(12)60033-6
4. Berlim MT, Mattevi BS, Duarte AP, Thome FS, Barros EJ, Fleck MP. Quality of life and depressive symptoms in patients with major depression and end-stage renal disease: a matched-pair study. J Psychosom Res. (2006) 61:731–4. doi: 10.1016/j.jpsychores.2006.04.011
5. Alavi NM, Aliakbarzadeh Z, Sharifi K. Depression, anxiety, activities of daily living, and quality of life scores in patients undergoing renal replacement therapies. Transplant Proc. (2009) 41:3693–6. doi: 10.1016/j.transproceed.2009.06.217
6. Cukor D, Peterson RA, Cohen SD, Kimmel PL. Depression in end-stage renal disease hemodialysis patients. Nat Clin Pract Nephrol. (2006) 2:678–87. doi: 10.1038/ncpneph0359
7. Taskapan H, Ates F, Kaya B, Emul M, Kaya M, Taskapan C, et al. Psychiatric disorders and large interdialytic weight gain in patients on chronic haemodialysis. Nephrology. (2005) 10:15–20. doi: 10.1111/j.1440-1797.2005.00321.x
8. Cukor D, Coplan J, Brown C, Friedman S, Newville H, Safier M, et al. Anxiety disorders in adults treated by hemodialysis: a single-center study. Am J Kidney Dis. (2008) 52:128–36. doi: 10.1053/j.ajkd.2008.02.300
9. Kimmel PL. Psychosocial factors in dialysis patients. Kidney Int. (2001) 59:1599–613. doi: 10.1046/j.1523-1755.2001.0590041599.x
10. Kimmel PL, Peterson RA. Depression in end-stage renal disease patients treated with hemodialysis: tools, correlates, outcomes, and needs. Semin Dial. (2005) 18:91–7. doi: 10.1111/j.1525-139X.2005.18209.x
11. Asukai N, Kato H, Kawamura N, Kim Y, Yamamoto K, Kishimoto J, et al. Reliability and validity of the Japanese-language version of the impact of event scale-revised (IES-R-J): four studies of different traumatic events. J Nerv Ment Dis. (2002) 190:175–82. doi: 10.1097/00005053-200203000-00006
12. Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale - revised. Behav Res Ther. (2003) 41:1489–96. doi: 10.1016/j.brat.2003.07.010
13. Kawamura N, Kim Y, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry. (2001) 158:484–6. doi: 10.1176/appi.ajp.158.3.484
14. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. (2009) 54:302–11. doi: 10.1177/070674370905400504
15. Hsu CC, Chong MY, Yang P, Yen CF. Posttraumatic stress disorder among adolescent earthquake victims in Taiwan. J Am Acad Child Adolesc Psychiatry. (2002) 41:875–81. doi: 10.1097/00004583-200207000-00022
16. Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. (1979) 9:139–45. doi: 10.1017/S0033291700021644
17. Goldberg D. The Detection of Psychiatric Illness by Questionnaire: A Technique for the Identification and Assessment of Non-Psychotic Psychiatric Illness. London: Oxford University Press (1972).
18. Lopes Cardozo B, Vergara A, Agani F, Gotway CA. Mental health, social functioning, and attitudes of Kosovar Albanians following the war in Kosovo. JAMA. (2000) 284:569–77. doi: 10.1001/jama.284.5.569
19. Hays RD, Kallich JD, Mapes DL, Coons SJ, Amin N, Carter WB, et al. Kidney Disease Quality of Life Short Form (KDQOL-SF™), Version 1.3: A Manual for Use and Scoring. Santa Monica, CA: RAND (1997).
20. Tao X, Chow SK, Wong FK. Determining the validity and reliability of the Chinese version of the Kidney Disease Quality of Life Questionnaire (KDQOL-36). BMC Nephrol. (2014) 15:115. doi: 10.1186/1471-2369-15-115
21. Schouten RW, Haverkamp GL, Loosman WL, Chandie Shaw PK, van Ittersum FJ, Smets YFC, et al. Anxiety symptoms, mortality, and hospitalization in patients receiving maintenance dialysis: a cohort study. Am J Kidney Dis. (2019) 74:158–66. doi: 10.1053/j.ajkd.2019.02.017
22. Peipert JD, Nair D, Klicko K, Schatell DR, Hays RD. Kidney disease quality of life 36-item short form survey (KDQOL-36) normative values for the united states dialysis population and new single summary score. J Am Soc Nephrol. (2019) 30:654–63. doi: 10.1681/ASN.2018100994
23. Garcia-Martinez P, Temprado-Albalat MD, Ballester-Arnal R, Gandhi-Morar K, Castro-Calvo J, Collado-Boira E. Predictive model of variables associated with health-related quality of life in patients with advanced chronic kidney disease receiving hemodialysis. Qual Life Res. (2020) 29:1817–27. doi: 10.1007/s11136-020-02454-0
24. Kaveh K, Kimmel PL. Compliance in hemodialysis patients: multidimensional measures in search of a gold standard. Am J Kidney Dis. (2001) 37:244–66. doi: 10.1053/ajkd.2001.21286
25. Cukor D, Coplan J, Brown C, Friedman S, Cromwell-Smith A, Peterson RA, et al. Depression and anxiety in urban hemodialysis patients. Clin J Am Soc Nephrol. (2007) 2:484–90. doi: 10.2215/CJN.00040107
26. Michael B, Spitzer RL, Gibbon M, Janet BW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. Washington, DC: American Psychiatric Press (1996).
27. Ahola AJ, Saraheimo M, Forsblom C, Hietala K, Sintonen H, Groop PH, et al. Health-related quality of life in patients with type 1 diabetes–association with diabetic complications (the FinnDiane Study). Nephrol Dial Transplant. (2010) 25:1903–8. doi: 10.1093/ndt/gfp709
28. Mapes DL, Lopes AA, Satayathum S, McCullough KP, Goodkin DA, Locatelli F, et al. Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int. (2003) 64:339–49. doi: 10.1046/j.1523-1755.2003.00072.x
29. Lopes AA, Bragg-Gresham JL, Satayathum S, McCullough K, Pifer T, Goodkin DA, et al. Health-related quality of life and associated outcomes among hemodialysis patients of different ethnicities in the United States: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. (2003) 41:605–15. doi: 10.1053/ajkd.2003.50122
Keywords: hemodialysis, quality of life, mental health, psychological profiles, stress, COVID-19
Citation: Yang Z-H, Pan X-T, Chen Y, Wang L, Chen Q-X, Zhu Y, Zhu Y-J, Chen Y-X and Chen X-N (2021) Psychological Profiles of Chinese Patients With Hemodialysis During the Panic of Coronavirus Disease 2019. Front. Psychiatry 12:616016. doi: 10.3389/fpsyt.2021.616016
Received: 10 October 2020; Accepted: 29 January 2021;
Published: 03 March 2021.
Edited by:
Tina L. Rochelle, City University of Hong Kong, Hong KongReviewed by:
Yuhan Xing, The Chinese University of Hong Kong, ChinaCopyright © 2021 Yang, Pan, Chen, Wang, Chen, Zhu, Zhu, Chen and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong-Xi Chen, cmlja3ljaGVuQHNqdHUuZWR1LmNu; Xiao-Nong Chen, Y3huMTA0MTlAcmpoLmNvbS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.