- 1Department of Social Welfare and Counseling, Chodang University, Muan, South Korea
- 2Clinical Emotion and Cognition Research Laboratory, Inje University, Goyang, South Korea
- 3Department of Psychiatry, Inje University, Ilsan-Paik Hospital, Goyang, South Korea
Objective: This study examined the relationship of childhood physical abuse, posttraumatic stress disorder (PTSD), depression, and suicide in patients with PTSD through path analysis.
Materials and Methods: A total of 114 patients with PTSD (36 men and 78 women) were recruited and completed psychological assessments including the Childhood Trauma Questionnaire, the scale for suicidal ideation, the clinician-administered PTSD scale for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, the PTSD checklist, and the Hospital Anxiety and Depression Scale. Structural equation modeling was used to evaluate the results. We developed a model including childhood physical abuse experience as the causal variable, suicidal ideation as a result variable, and PTSD and depression as mediation variables. PTSD symptoms were divided into four clusters [intrusion, avoidance, negative cognition and mood, and altered arousal and reactivity (hyperarousal)] to determine predictive power for suicide.
Results: PTSD symptoms fully mediated the relationship between childhood physical abuse and suicidal ideation. Furthermore, PTSD symptoms fully mediated the relationship between childhood physical abuse and depression. Among the PTSD symptoms, hyperarousal was the only symptom cluster that mediated the relationship between childhood physical abuse and suicidal ideation. The symptom clusters of negative cognition and mood as well as hyperarousal mediated the relationship between childhood physical abuse and depression.
Conclusions: This study presents a link between childhood physical abuse and current symptoms in patients with PTSD, and highlights specific PTSD symptom clusters (i.e., hyperarousal, negative cognition and mood) that may increase the risk for psychopathology later in life.
Introduction
There are high rates of suicidal behavior among individuals diagnosed with posttraumatic stress disorder (PTSD) after being exposed to trauma (1, 2). According to several existing studies, the suicide attempt rates of patients with PTSD is between 24 and 40% (3–7). In patients with chronic PTSD, 56.4% experience suicidal behaviors, including suicidal ideation and suicide attempts (8).
Complex trauma in response to repeated and perpetuating experiences of interpersonal trauma usually shows more severe symptoms than simple trauma related to a single event, such as a car accident, natural disaster, or robbery (9–12). Childhood physical abuse is a leading example of complex trauma (13–15), and it has been reported that the influence of childhood physical abuse on suicidal behavior is serious (1, 16–18). In a study of 6,642 Canadians, a group that has experienced childhood physical abuse had a five-fold higher suicidal ideation when the group that did not experience such trauma (19). According to a national epidemiological survey of 43,093 individuals, the group that had experienced childhood physical abuse experienced higher levels of substance abuse disorders, ADHD, PTSD, and mood disorders, with higher rates of suicidal attempts compared to the group that had not experienced childhood physical abuse (17). Furthermore, PTSD diagnosis is one of the strongest predictors of recent and lifetime suicide attempts in adults who have experienced childhood abuse (20–22).
The number and severity of PTSD symptoms have been reported as key predictors of suicidal behavior in patients (5, 8, 23). According to a 15-year study that tracked the relationship between childhood trauma, PTSD occurrence, and suicide attempts with 1,698 adolescents, participants with a PTSD diagnosis had a significantly higher risk of suicide attempts compared to those exposed to trauma but not diagnosed with PTSD, and those not exposed to trauma (24).
Studies have examined the relationship between specific PTSD symptoms and suicidal behaviors. Most of these studies have utilized the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria (25) dividing the symptoms into three clusters of reexperience, avoidance/numbing, and hyperarousal, to confirm their relationships with suicide. Some studies involving firefighters and soldiers reported that re-experiencing symptoms had a positive correlations with suicidal behavior (4, 6, 26, 27). Hyperarousal symptoms had a positive correlation with the risk of suicide in a community sample (6, 26, 28, 29). While there have been studies dividing PTSD symptoms into four clusters of intrusion, avoidance, negative cognition and mood, and altered arousal and reactivity based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria (28, 30–32), there are a limited number of studies related to suicidal behavior. In addition, studies based on the DSM-5 criteria do not control for demographic information and only measured the frequency of experiences of suicidal ideation and suicide attempts.
The main criticism of previous studies on PTSD and suicidality is that they overlook depression (23). Depression may mediate the relationship between PTSD and suicidal behaviors (33, 34), and the co-occurrence of PTSD and depression may exacerbate the effects of PTSD, leading to suicidal behavior (34).
Our study examined the relationship of childhood physical abuse, PTSD, and depression and suicide in patients with PTSD through path analysis. We developed a model for patients with PTSD that included childhood physical abuse, PTSD symptoms (including four PTSD symptom clusters), depression, and suicide, and tested its validity (Figure 1). Confirming the relationship between the variables influencing suicidal behavior in patients with PTSD will present important implications in preventing suicide in patients with PTSD.
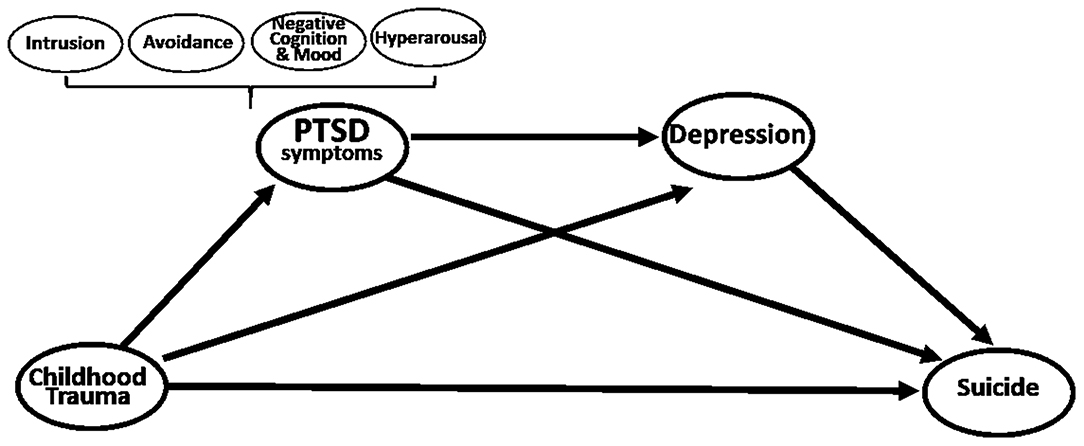
Figure 1. Hypothetical model: Multiple mediation model for effect of childhood trauma on suicide via PTSD symptoms and depression.
Materials and Methods
Participants
Patients with PTSD were recruited from the Psychiatry Department of the Inje University Ilsan Paik Hospital in Goyang, Korea. The diagnosis of PTSD made by a psychiatrist was based on the DSM-5 full criteria. We excluded participants with a history or suffering from any psychiatric and/or neurological illness other than PTSD, such as schizophrenia, bipolar disorder, anorexia nervosa, intellectual disability, epilepsy, etc. A total of 146 patients with PTSD were registered for the study. Data sets from 32 individuals were excluded from the study [including 9 individuals who did not attempt or complete the psychological scale, 10 individuals who had high scores for denial on the Childhood Trauma Questionnaire (CTQ), and 13 individuals with severe brain damage]. Ultimately, data from 114 patients with PTSD were included in the analysis. The patients with PTSD included in the analysis were composed of 36 men (31.60%) and 78 women (68.40%), with an average age of 44.36 years (SD = 12.77) and an average education of 12.78 years (SD = 3.21). Each participant signed an informed consent form approved by the Institutional Review Board at Inje University Ilsan Paik Hospital before participating (IRB No. 2015-07-025).
Psychological Measures
Childhood Trauma Questionnaire
The Korean validated version of the CTQ was used to evaluate childhood physical abuse (35). It is known as a useful self-report questionnaire in eliciting retrospective reports of childhood trauma (36). It consists of five subscales of various childhood trauma, including emotional, physical, and sexual abuse, and emotional and physical neglect as well as another scale for detecting minimization and denial. The CTQ consists of 28 items and is assessed with a 5-point Likert scale ranging from 1 (“never true”) to 5 (“very often true”). The coefficient alpha of the K-CTQ was 0.79 in this study, and the coefficient alphas of the 5 subscales were 0.89 (emotional abuse), 0.85 (sexual abuse), 0.90 (physical abuse), 0.61 (emotional neglect), and 0.95 (physical neglect).
Scale for Suicidal Ideation (SSI)
SSI a self-reported questionnaire for measuring suicidality (37). This study utilized the Korean validated version of the SSI (38). The scale consists of 19 items and is assessed using a 3-point Likert scale ranging from 0 to 2. The coefficient alpha of this scale was 0.91.
Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)
CAPS-5 is a structured diagnostic interview that corresponds with the DSM-5 diagnosis for PTSD, administered by a psychiatrist (39). It consists of 30 items and assesses information about the frequency and severity of PTSD symptoms. This was assessed by standardizing and simplifying the conversion of symptom frequency and intensity ratings into dichotomous scores (“Yes” or “No”) and symptom severity (from 0 [“Absent”] to 4 [“Extreme/incapacitating”]). The coefficient alpha of the CAPS-5 severity score was 0.80.
Posttraumatic Stress Disorder Checklist-5 (PCL-5)
The PCL-50 is a self-reported questionnaire for measuring PTSD symptoms based on the DSM-5 and consists of a total of 20 questions (40). This study utilized the Korean validated version of the PCL-5 (41). The PCL-5 helps in the screening and diagnostic evaluation of PTSD and is used for the purpose of observing changes in PTSD symptoms. The results are measured using a Likert scale, ranging from 0 (“not at all”) to 4 (“extremely”), measuring the degree of pain one has experienced within the last month or since the previous stressful event. In addition, this study divided PTSD symptoms into four clusters based on the DSM-5. The four symptom clusters (intrusion, avoidance, negative cognition and mood, and altered arousal and reactivity) were individually included in the hypothetical model. In the text, altered arousal and reactivity are referred to as hyperarousal for convenience. The coefficient alpha of the PCL-5 score was 0.93 in this study.
Hospital Anxiety and Depression Scale (HADS)
HADS was used to evaluate symptoms of depression and anxiety (42). This study utilized the Korean validated version of HADS (43). It is a self-reported questionnaire with 7 items for describing anxiety and 7 items for describing depression. It is assessed with a 4-point Likert scale ranging from 0 (“no problems”) to 3 (“maximum distress”). The coefficient alphas for the subscales of HADS were 0.92 (anxiety) and 0.83 (depression) in this study.
Statistical Analysis
Partial correlation analysis with bootstrapping at a 1,000-sampling rate was performed to examine the correlations among the variables. Sex, age, years of education, and type of trauma were controlled.
To utilize the maximum likelihood estimation method in the structured equation model, this study confirmed the skewness and kurtosis of the variables. Skewness over 3 and kurtosis over 7 are considered to be a moderately non-normal distribution (44).
Exploratory factor analysis was performed to establish the latent variables. The scale was parceled using the Factor-Parceling Approach based on the size of the factor loads (45, 46). SSI and PCL-5 were each grouped into a total of three factors, with six to seven items per parcel. As for the childhood physical abuse and the HADS-depression scale, all individual items were used without any parceling.
To analyze the convergent validity and discriminant validity of the latent variables, this study conducted a confirmatory factor analysis and utilized the maximum likelihood estimation method. Values of 0.50 or higher for standardized factor load are reported to indicate satisfactory convergent validity (47), in accordance with the criteria of discriminant validity, which states that a correlation of 0.80 or higher between latent variables indicates the measurement of the same concept. To test reliability, Cronbach's α values were calculated.
To evaluate the fit of the measurement model, this study calculated χ2, χ2/df, comparative fit index (CFI), normed fit index (NFI), incremental fit index (IFI), Tucker Lewis Index (TLI), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), root mean squared error of approximation (RMSEA), root mean-square residual (RMR), and standardized root mean squared residual (SRMR). A good model is defined as when χ2/df is <3, the CFI, NFI, IFI, TLI, GFI, and AGFI are >0.90, and the RMSEA and SRMR are <0.08 (44).
To test whether PTSD symptoms and depression mediate the relationship between childhood physical abuse and suicidal ideation, this study used the serial multiple mediation model as the structural model. Furthermore, the four structural models including the 4 PTSD symptom clusters were set to specifically investigate the effect of PTSD symptoms on suicidal ideation in patients with PTSD. The fit of the structural model was calculated, and the validity of the structural model was confirmed by using the maximum likelihood estimation to analyze the validity of the parameters. Next, this study identified the total, direct, and indirect effects of the model. To evaluate the significance of the indirect effects, this study used a bootstrapping method to generate 1,000 samples (48). Phantom variables were used to confirm the size and significance of the specific indirect effects (49).
This study examined the hypothetical model using AMOS 20 for testing the structural equation model (SPSS, Inc., Chicago, IL, USA). Statistical analyses were performed using SPSS 18 (SPSS, Inc., Chicago, IL, USA).
Results
Descriptive Statistics
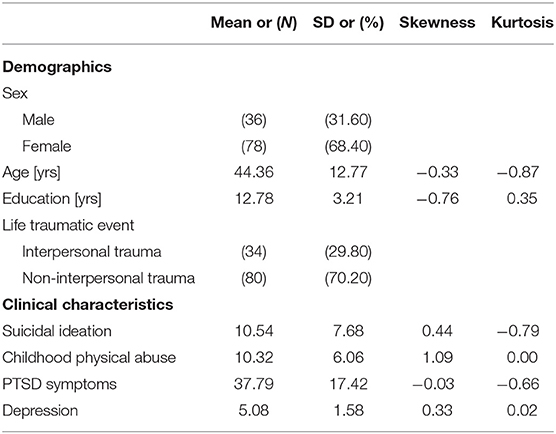
Among 114 patients with PTSD, 34 experienced trauma from interpersonal relationships such as sexual abuse or domestic abuse (29.6%), and 80 (70.2%) experienced non-relationship trauma, such as automobile accidents, falls, and kidnappings. The frequency, mean, standard deviation, skewness, and kurtosis of the variables are shown in Table 1.
Significant positive correlations were identified between suicidal ideation and childhood physical abuse (r = 0.198, p < 0.05), suicidal ideation and PTSD symptoms (r = 0.440, p < 0.001), suicidal ideation and depression (r = 0.362, p < 0.001), childhood physical abuse, and PTSD symptoms (r = 0.263, p < 0.01), and PTSD symptoms and depression (r = 0.534, p < 0.001). In contrast, the correlations between childhood physical abuse and depression was not statistically significant.
Tests of the Measurement Model
This study found that the standardized factor loading value was higher than 0.50, indicating no issues with convergent validity in the measurement model (47). The correlations between latent variables ranged between 0.184 and 0.643, meeting the criteria of 0.80 or below, indicating that the measurement model has discriminant validity. The Cronbach's α values of the latent variables ranged from 0.717 to 0.924, which indicates reliability. The fit of the measurement model was found to be acceptable, with χ2 = 97.822 (p = 0.144), IFI = 0.987, TLI = 0.984, CFI = 0.987, RMSEA = 0.038, and SRMR = 0.043 (44).
Test of the Structural Model
The results indicated that the fit of the structural model including four major variables (i.e., childhood physical abuse, PTSD symptoms, depression, and suicidal ideation) was acceptable, with χ2/df = 144.034/127 = 1.134, IFI = 0.985, TLI = 0.979, CFI = 0.984, and RMSEA = 0.034.
The results of the effect test indicated that PTSD symptoms fully mediate the relationship between childhood physical abuse and suicidal ideation in patients with PTSD (Figure 2A). More specifically, the total effect of childhood physical abuse on suicidal ideation was significant (β = 0.222, p = 0.040). The direct effect of childhood physical abuse on suicidal ideation was not significant (β = 0.103, p = 0.304). The indirect effect of PTSD symptoms between childhood physical abuse and suicidal ideation was significant (β = 0.119, p = 0.039). The specific indirect effect of PTSD symptoms between childhood physical abuse and suicidal ideation was significant (B = 0.009, p = 0.010) (Table 2).
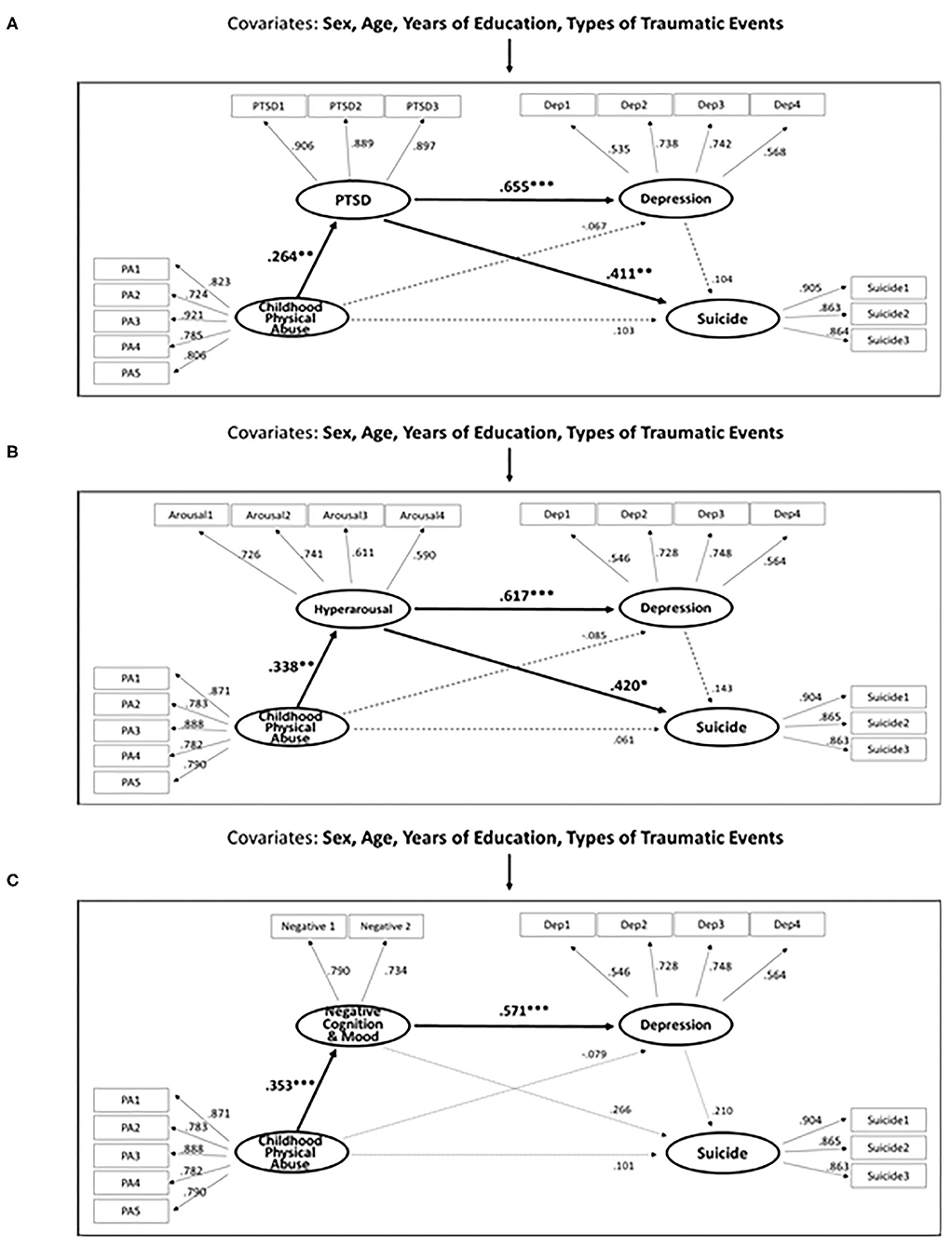
Figure 2. (A) Structural equation model of the effects of childhood physical abuse, PTSD and depression on suicide in patients with PTSD (N = 114). (B,C) Structural equation model of the effects of childhood physical abuse, specific PTSD symptom cluster and depression on suicide in patients with PTSD (N = 114).
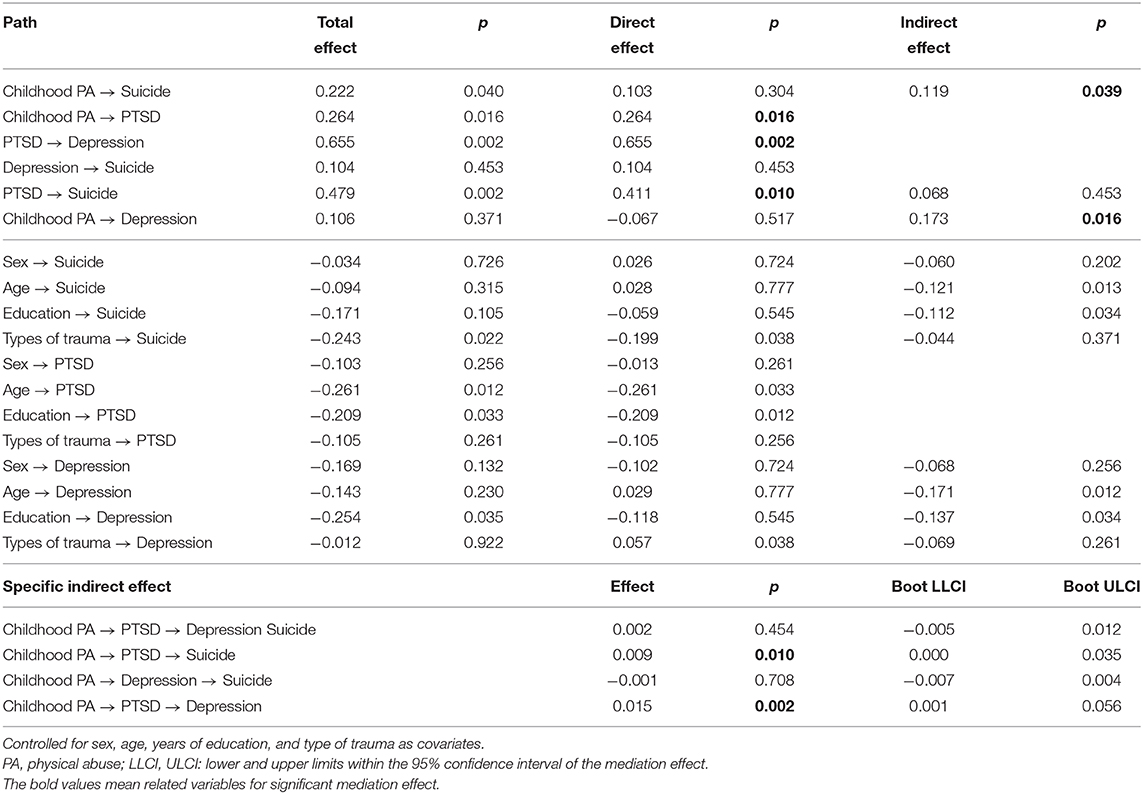
Table 2. Standardized total, direct, indirect, and specific indirect effects of structural model in patients with PTSD (N = 114).
Furthermore, PTSD symptoms fully mediated the relationship between childhood physical abuse and depression (Figure 2A). More specifically, the total effect of childhood physical abuse on depression was not significant (β = 0.106, p = 0.371). The direct effect of childhood physical abuse on depression was not significant (β = −0.067, p = 0.517). The indirect effect of PTSD symptoms between childhood physical abuse and depression was significant (β = 0.173, p = 0.016). The specific indirect effect of PTSD symptoms between childhood physical abuse and depression was significant (B = 0.015, p = 0.002) (Table 2). The results show that PTSD symptoms act as important mediators in the relationship where childhood physical abuse, possibly leading to the development of depression or suicide among patients with PTSD.
However, the specific indirect effect of PTSD symptoms and depression between childhood physical abuse and suicidal ideation (B = 0.002, p = 0.454), and the specific indirect effect of depression between childhood physical abuse and suicidal ideation (B = −0.001, p = 0.708) were not statistically significant.
Test of the Structural Model for Specific PTSD Symptom Clusters
The fit of the four structural models for specific PTSD symptom clusters were all acceptable as follows: χ2/df <3, CFI, NFI, IFI, TLI, GFI, and AGFI are more than 0.90, and RMSEA and SRMR are <0.08 (Supplementary Table 1) (44).
The results of the effect test indicated that the hyperarousal cluster was the only cluster that fully mediated the relationship between childhood physical abuse and suicidal ideation (Figure 2B). More specifically, the direct effect of childhood physical abuse on hyperarousal (β = 0.338, p = 0.002) and the direct effect of hyperarousal on suicidal ideation (β = 0.420, p = 0.038) were significant. The indirect effect of childhood physical abuse on suicidal ideation through hyperarousal (B = 0.042, p = 0.041) was significant. Furthermore, the hyperarousal cluster fully mediated the relationship between childhood physical abuse and depression (Figure 2B). In other words, the direct effect of hyperarousal on depression (β = 0.617, p = 0.002) and the indirect effect of childhood physical abuse on depression through hyperarousal (B = 0.068, p = 0.003) were significant. Finally, the negative alterations in cognition and mood fully mediated the relationship between childhood physical abuse and depression (Figure 2C). In other words, the direct effect of childhood physical abuse on negative alterations in cognition and mood (β = 0.353, p = 0.004), the direct effect of negative alterations in cognition and mood on depression (β = 0.571, p = 0.002), and the indirect effect of childhood physical abuse on depression through negative alterations in cognition and mood (B = 0.063, p = 0.001) were significant. The direct effects, indirect effects, and specific indirect effects using bootstrapping of the four structural models are presented in Supplementary Table 2.
Discussion
The purpose of this study was to explore the relationship between childhood physical abuse, PTSD symptoms, depression, and suicidal ideation in patients with PTSD. The results indicated that PTSD symptoms fully mediated the relationship between childhood physical abuse and suicidal ideation. Furthermore, PTSD symptoms fully mediated the relationship between childhood physical abuse and depression. Among the symptom clusters, hyperarousal fully mediated the relationship between childhood physical abuse and suicidal ideation. The negative alterations in cognition and mood and hyperarousal fully mediated the relationship between childhood physical abuse and depression.
PTSD symptoms fully mediated the relationship between childhood physical abuse and suicidal ideation. These results are similar with previous studies which pinpointed PTSD symptom as one of the major factors related to suicide among PTSD patients (26, 34, 50, 51). This study is also in line with existing studies showing that people who have experienced childhood physical abuse were more likely to be diagnosed with PTSD (52–56). PTSD symptoms can be understood as the internal state of fear, experienced through childhood physical abuse, that persists in current lives (57). PTSD symptoms was reported to appear when a traumatic experience in childhood have not been fully integrated or assimilated into memory, and individuals have difficulty processing the experience as a past event that can no longer bring harm (58). In addition, people who have experienced childhood physical abuse are vulnerable to different types of trauma in adulthood (59), which can lead to more serious and a higher frequency of suicide behaviors (60). In summary, our current results provide a link between childhood physical abuse and later life psychopathology in patients with PTSD.
PTSD symptoms fully mediate the relationship between childhood physical abuse and depression in patients with PTSD. Previous studies have shown that PTSD is a major predictor of the co-occurrence of depression (61–68). Our results support that patients with a primary diagnosis of PTSD had identified depressive symptoms as being one of the most frequent co-occurrence.
Among the PTSD symptom clusters, only hyperarousal mediated the relationship between childhood physical abuse and suicidal ideation. Hyperarousal refers to symptoms of anxiety, hypervigilance, difficulty concentrating, and irritability (69) and includes deficits in emotion regulation, impulsivity, and aggressive and self-destructive behavior (70, 71). The association between hyperarousal and suicidal behavior may reflect the tendency of severely traumatized patients with PTSD to crave a way out of their emotional pain, and do so through ending their lives (72). Studies reporting an association between anxiety sensitivity and suicidal behavior support this interpretation (73–75). Anxiety sensitivity is referred to as the fear of arousal sensation, and bodily sensations associated with autonomic arousal as a sign of imminent personal harm. Trauma survivors suffering from persistent hyperarousal showed extreme levels of fear over losing cognitive control (76). Patients with PTSD are thought to perceive suicidal behavior as a strategy to avoid an agonizing internal state (76). In short, suicidal ideation in patients with PTSD might be related to one of the PTSD patients' responses to try and extinguish intense pain in the midst of post-traumatic hyperarousal. Therefore, our findings can help identify those who are at a higher risk for suicidal ideation and provide early therapeutic interventions.
The hyperarousal PTSD symptom cluster fully mediated the relationship between childhood physical abuse and depression. As mentioned above, those with serious hyperarousal symptoms demonstrate violent, aggressive, and self-destructive behaviors, damaging themselves and others (77). Furthermore, they have difficulties in social relationships, as they are often blamed or shunned by people around them and find adaptation difficult (78), which can ultimately increase depression. This is in line with existing studies that aggressive and impulsive behaviors possibly leading to the development of depression (78, 79).
The negative alterations in cognition and mood fully mediated the relationship between childhood physical abuse and depression. A higher number of adults and adolescents who have experienced childhood abuse were currently suffering from depressive disorders compared to those who did not have the same experience (80). A longitudinal study also found that people who have experienced childhood physical abuse were more likely to have later depressive disorder (81). The depression of those who suffered from childhood physical abuse has been shown to be related to helplessness, guilt, and loss of attachment experienced through childhood physical abuse (82, 83). Our result is consistent with prior findings in the sense that childhood physical abuse indirectly predicted depression through mediating of the negative alterations in cognition and mood cluster. Because this cluster emphasizes negative cognition and mood related to trauma, it significantly overlaps with depression (84). The negative alterations in cognition and mood cluster could be used to identify those with PTSD symptoms, which later develop into co-occurrence of depression.
There are some limitations to this study. First, this study examined mediation effects based on cross-sectional data of patients with PTSD. Therefore, it is difficult to find causality in the relationships between the variables. Although the CTQ is regarded as a reliable tool for measuring childhood trauma in many studies (85–90), additional longitudinal studies would be helpful to support the findings from this study. Second, although the minimum sample size was 114, given an effect size (f 2) of 0.15, significance criterion of 0.05, power at 0.80, and 9 for the number of predictor variables (91), a replication study is needed to generalize the current findings. Third, although the type of trauma was controlled as a covariate, a further investigation separating PTSD patients with relational trauma from those with non-relational trauma is needed.
In conclusion, this study is meaningful as it was to our knowledge the first attempt to examine the mediation effect of PTSD symptoms in the relationship between childhood physical abuse and suicidal ideation in patients with PTSD. Although the relationship between PTSD and suicidality has been previously established, the current findings offer progress of this knowledge, as it sheds light on the importance of specific PTSD symptoms (i.e., hyperarousal, negative cognition and mood). It also provides a link between childhood physical abuse and current symptoms, and highlight hyperarousal symptoms that may increase the risk of suicidal ideation in later life. Therefore, treatment that focuses on alleviating hyperarousal symptoms would be helpful to prevent suicidal ideation in patients with PTSD who have experienced childhood physical abuse.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board at Inje University Ilsan Paik Hospital (IRB No. 2015-07-025). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AK performed study conception, design, methodology, formal analysis, and writing-original draft. HSL performed data collection and writing-editing. S-HL performed funding acquisition, investigation, review, and supervision. All authors discussed the results and commented on the manuscript at all stages, and approved the final manuscript.
Funding
This work was partially supported by the Brain Research Program through the National Research Foundation of Korea from the Ministry of Science, ICT & Future Planning (NRF-2015M3C7A1028252) and the Korea Medical Device Development Fund grant funded by the Korea Government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (Project Number: 202013B10) to Seung Hwan Lee.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English language editing.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.613735/full#supplementary-material
References
1. Thompson MP, Kaslow NJ, Lane DB, Kingree J. Childhood maltreatment, PTSD, and suicidal behavior among African American females. J Interpers Violence. (2000) 15:3–15. doi: 10.1177/088626000015001001
2. Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, et al. Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS ONE. (2010) 5:e10574 doi: 10.1371/journal.pone.0010574
3. Davidson JR, Hughes D, Blazer DG, George LK. Post-traumatic stress disorder in the community: an epidemiological study. Psychol Med. (1991) 21:713–21. doi: 10.1017/S0033291700022352
4. Amir M, Kaplan Z, Efroni R, Kotler M. Suicide risk and coping styles in posttraumatic stress disorder patients. Psychother Psychosom. (1999) 68:76–81. doi: 10.1159/000012316
5. Freeman TW, Roca V, Moore WM. A comparison of chronic combat-related posttraumatic stress disorder (PTSD) patients with and without a history of suicide attempt. J Nerv Ment Dis. (2000) 188:460–3. doi: 10.1097/00005053-200007000-00011
6. Kotler M, Iancu I, Efroni R, Amir M. Anger, impulsivity, social support, and suicide risk in patients with posttraumatic stress disorder. J Nerv Ment Dis. (2001) 189:162–7. doi: 10.1097/00005053-200103000-00004
7. Nad S, Marcinko D, Vuksan-Æusa B, Jakovljevic M, Jakovljevic G. Spiritual well-being, intrinsic religiosity, and suicidal behavior in predominantly Catholic Croatian war veterans with chronic posttraumatic stress disorder: a case control study. J Nerv Ment Dis. (2008) 196:79–83. doi: 10.1097/NMD.0b013e31815faa5f
8. Tarrier N, Gregg L. Suicide risk in civilian PTSD patients. Social psychiatry psychiatric epidemiology. (2004) 39:655–61. doi: 10.1007/s00127-004-0799-4
9. Herman JL. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J Trauma Stress. (1992) 5:377–91. doi: 10.1002/jts.2490050305
10. van der Kolk BA, Courtois CA. Editorial comments: complex developmental trauma. J Trauma Stress. (2005) 18:385–8. doi: 10.1002/jts.20046
11. Cloitre M, Stolbach BC, Herman JL, van der Kolk B, Pynoos R, Wang J, et al. A developmental approach to complex PTSD: childhood and adult cumulative trauma as predictors of symptom complexity. J Trauma Stress. (2009) 22:399–8. doi: 10.1002/jts.20444
12. Cloitre M, Garvert DW, Weiss B, Carlson EB, Bryant RA. Distinguishing PTSD, complex PTSD, and borderline personality disorder: a latent class analysis. Eur J Psychotraumatol. (2014) 5:25097. doi: 10.3402/ejpt.v5.25097
13. Allen JG. Coping With Trauma: Hope Through Understanding. Washington, DC: American Psychiatric Pub (2008).
14. Cook A, Spinazzola J, Ford J, Lanktree C, Blaustein M, Cloitre M, et al. Complex trauma in children and adolescents. Psychiatr Ann. (2017) 35:390–8. doi: 10.3928/00485713-20050501-05
15. Spinazzola J, Ford JD, Zucker M, van der Kolk BA, Silva S, Smith SF, et al. Survey evaluates: complex trauma exposure, outcome, and intervention among children and adolescents. Psychiatr Ann. (2017) 35:433–9. doi: 10.3928/00485713-20050501-09
16. Braquehais MD, Oquendo MA, Baca-García E, Sher L. Is impulsivity a link between childhood abuse and suicide? Compr Psychiatry. (2010) 51:121–9. doi: 10.1016/j.comppsych.2009.05.003
17. Sugaya L, Hasin DS, Olfson M, Lin KH, Grant BF, Blanco C. Child physical abuse and adult mental health: a national study. J Trauma Stress. (2012) 25:384–92. doi: 10.1002/jts.21719
18. Liu J, Fang Y, Gong J, Cui X, Meng T, Xiao B, et al. Associations between suicidal behavior and childhood abuse and neglect: a meta-analysis. J Affect Disord. (2017) 220:147–55. doi: 10.1016/j.jad.2017.03.060
19. Fuller-Thomson E, Baker TM, Brennenstuhl S. Evidence supporting an independent association between childhood physical abuse and lifetime suicidal ideation. Suicide Life Threat Behav. (2012) 42:279–91. doi: 10.1111/j.1943-278X.2012.00089.x
20. Evren C, Kural S, Cakmak D. Clinical correlates of childhood abuse and neglect in substance dependents. Addict Behav. (2006) 31:475–85. doi: 10.1016/j.addbeh.2005.05.030
21. Joiner TE Jr, Sachs-Ericsson NJ, Wingate LR, Brown JS, Anestis MD, Selby EA. Childhood physical and sexual abuse and lifetime number of suicide attempts: a persistent and theoretically important relationship. Behav Res Ther. (2007) 45:539–47. doi: 10.1016/j.brat.2006.04.007
22. Sarchiapone M, Carli V, Cuomo C, Marchetti M, Roy A. Association between childhood trauma and aggression in male prisoners. Psychiatry Res. (2009) 165:187–92. doi: 10.1016/j.psychres.2008.04.026
23. Panagioti M, Gooding PA, Dunn G, Tarrier N. Pathways to suicidal behavior in posttraumatic stress disorder. J Trauma Stress. (2011) 24:137–45. doi: 10.1002/jts.20627
24. Wilcox HC, Storr CL, Breslau N. Posttraumatic stress disorder and suicide attempts in a community sample of urban American young adults. Arch Gen Psychiatry. (2009) 66:305–11. doi: 10.1001/archgenpsychiatry.2008.557
25. American Psychiatric Association. Diagnostic Criteria from DSM-IV-TR. Washington, DC: American Psychiatric Association (2000).
26. Bell JB, Nye EC. Specific symptoms predict suicidal ideation in Vietnam combat veterans with chronic post-traumatic stress disorder. Mil Med. (2007) 172:1144–7. doi: 10.7205/MILMED.172.11.1144
27. Jurišić B, Marušič A. Suicidal ideation and behavior and some psychological correlates in physically disabled motor-vehicle accident survivors. Crisis. (2009) 30:34–8. doi: 10.1027/0227-5910.30.1.34
28. Ben-Ya'acov Y, Amir M. Posttraumatic symptoms and suicide risk. Pers Individ Differ. (2004) 36:1257–64. doi: 10.1016/S0191-8869(03)00003-5
29. Steyn R, Vawda N, Wyatt GE, Williams J, Madu S. Posttraumatic stress disorder diagnostic criteria and suicidal ideation in a South African Police sample. Afr J Psychiatry. (2013) 16:19–22. doi: 10.4314/ajpsy.v16i1.3
30. Selaman ZM, Chartrand HK, Bolton JM, Sareen J. Which symptoms of post-traumatic stress disorder are associated with suicide attempts? J Anxiety Disord. (2014) 28:246–51. doi: 10.1016/j.janxdis.2013.12.005
31. Boffa JW, Stanley IH, Hom MA, Norr AM, Joiner TE, Schmidt NB. PTSD symptoms and suicidal thoughts and behaviors among firefighters. J Psychiatr Res. (2017) 84:277–83. doi: 10.1016/j.jpsychires.2016.10.014
32. Able ML, Benedek DM. Severity and symptom trajectory in combat-related PTSD: a review of the literature. Curr Psychiatry Rep. (2019) 21:58. doi: 10.1007/s11920-019-1042-z
33. Leiner AS, Compton MT, Houry D, Kaslow NJ. Intimate partner violence, psychological distress, and suicidality: a path model using data from African American women seeking care in an urban emergency department. J Fam Violence. (2008) 23:473–81. doi: 10.1007/s10896-008-9174-7
34. Panagioti M, Gooding P, Tarrier N. Post-traumatic stress disorder and suicidal behavior: a narrative review. Clin Psychol Rev. (2009) 29:471–82. doi: 10.1016/j.cpr.2009.05.001
35. Yu J, Park J, Park D, Ryu S, Ha J. Validation of the Korean childhood trauma questionnaire: the practical use in counselling and therapeutic intervention. Korean J Health Psychol. (2009) 14:563–78. doi: 10.17315/kjhp.2009.14.3.006
36. Everson MD, Smith JB, Hussey JM, English D, Litrownik AJ, Dubowitz H, et al. Concordance between adolescent reports of childhood abuse and child protective service determinations in an at-risk sample of young adolescents. Child Maltreat. (2008) 13:14–26. doi: 10.1177/1077559507307837
37. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. (1979) 47:343. doi: 10.1037/0022-006X.47.2.343
38. Shin MS, Park KB, Oh KJ, Kim ZS. A study of suicidal ideation among high school students: the structural relation among depression, hopelessness, and suicidal ideation. Korean J Clin Psychol. (1990) 9:1–19.
39. Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol Assess. (2018) 30:383–95. doi: 10.1037/pas0000486
40. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. (2015) 28:489–98. doi: 10.1002/jts.22059
41. Kim J-W, Chung H-G, Choi J-H, So H-S, Kang S-H, Kim D-S, et al. Psychometric Properties of the Korean version of the PTSD Checklist-5 in Elderly Korean Veterans of the Vietnam War. Korean Academy of Anxiety Disorder. (2017) 13:123–31. doi: 10.24986/anxmod.2017.13.2.123
42. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
43. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. Journal of Korean Neuropsychiatric Association. (1999) 38:289–96.
44. Kline RB. Principles and practice of structural equation modeling. (2015). Guilford publications.
45. Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: exploring the question, weighing the merits. Structural equation modeling. (2002) 9:151–73. doi: 10.1207/S15328007SEM0902_1
46. Rogers WM, Schmitt N. Parameter recovery and model fit using multidimensional composites: a comparison of four empirical parceling algorithms. Multivariate Behav Res. (2004) 39:379–412. doi: 10.1207/S15327906MBR3903_1
47. Gefen D, Straub D, Boudreau M-C. Structural equation modeling and regression: guidelines for research practice. J Commun Assoc Inf Syst. (2000) 4:7. doi: 10.17705/1CAIS.00407
48. Preacher KJ, Selig JP. Advantages of Monte Carlo confidence intervals for indirect effects. Communication Methods Measures. (2012) 6:77–98. doi: 10.1080/19312458.2012.679848
49. Perera HN. A novel approach to estimating and testing specific mediation effects in educational research: explication and application of Macho and Ledermann's. (2011) phantom model approach. Int J Quant Res Educ. (2013) 1:39–60. doi: 10.1504/IJQRE.2013.055640
50. Thoresen S, Mehlum L. Traumatic stress and suicidal ideation in Norwegian male peacekeepers. J Nerv Ment Dis. (2008) 196:814–21. doi: 10.1097/NMD.0b013e31818b6a92
51. Panagioti M, Gooding P, Taylor PJ, Tarrier N. A model of suicidal behavior in posttraumatic stress disorder (PTSD): the mediating role of defeat and entrapment. Psychiatry Res. (2013) 209:55–9. doi: 10.1016/j.psychres.2013.02.018
52. Cloitre M, Scarvalone P, Difede J. Posttraumatic stress disorder, self-and interpersonal dysfunction among sexually retraumatized women. J Trauma Stress. (1997) 10:437–52. doi: 10.1002/jts.2490100309
53. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. (2000) 68:748. doi: 10.1037/0022-006X.68.5.748
54. Nishith P, Mechanic MB, Resick PA. Prior interpersonal trauma: the contribution to current PTSD symptoms in female rape victims. J Abnorm Psychol. (2000) 109:20. doi: 10.1037/0021-843X.109.1.20
55. Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: a review of the empirical literature. Trauma Violence Abuse. (2005) 6:103–29. doi: 10.1177/1524838005275087
56. Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, et al. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. J Natl Med Assoc. (2006) 98:1630.
57. Stovall-McClough KC, Cloitre M. Unresolved attachment, PTSD, and dissociation in women with childhood abuse histories. J Consul Clin Psychol Rev. (2006) 74:219. doi: 10.1037/0022-006X.74.2.219
58. Horowitz MJ. Stress-response syndromes: A review of posttraumatic stress and adjustment disorders. In: Wilson JP, Raphael B, editors. The Plenum Series on Stress and Coping. International Handbook of Traumatic Stress Syndromes. Plenum Press. (1993). p. 49-60. doi: 10.1007/978-1-4615-2820-3_4
59. Cyr K, Chamberland C, Clément M-È, Lessard G, Wemmers J-A, Collin-Vézina D, et al. Polyvictimization and victimization of children and youth: results from a populational survey. Child Abuse Neglect. (2013) 37:814–20. doi: 10.1016/j.chiabu.2013.03.009
60. Lopez-Castroman J, Jaussent I, Beziat S, Guillaume S, Baca-Garcia E, Olié E, et al. Posttraumatic stress disorder following childhood abuse increases the severity of suicide attempts. J Affect Disord. (2015) 170:7–14. doi: 10.1016/j.jad.2014.08.010
61. Erickson DJ, Wolfe J, King DW, King LA, Sharkansky EJ. Posttraumatic stress disorder and depression symptomatology in a sample of Gulf War veterans: a prospective analysis. J Consult Clin Psychol. (2001) 69:41. doi: 10.1037/0022-006X.69.1.41
62. Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC, et al. Posttraumatic stress disorder and depression in battle-injured soldiers. Am J Psychiatry. (2006) 163:1777–83. doi: 10.1176/ajp.2006.163.10.1777
63. O'Toole BI, Catts SV, Outram S, Pierse KR, Cockburn J. The physical and mental health of Australian Vietnam veterans 3 decades after the war and its relation to military service, combat, and post-traumatic stress disorder. Am J Epidemiol. (2009) 170:318–30. doi: 10.1093/aje/kwp146
64. Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J Affect Disord. (2010) 123:249–57. doi: 10.1016/j.jad.2009.08.006
65. Wells TS, LeardMann CA, Fortuna SO, Smith B, Smith TC, Ryan MA, et al. A prospective study of depression following combat deployment in support of the wars in Iraq and Afghanistan. Am J Public Health. (2010) 100:90–9. doi: 10.2105/AJPH.2008.155432
66. Borsboom D, Cramer AO, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS ONE. (2011) 6:e27407. doi: 10.1371/journal.pone.0027407
67. Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. (2011) 67:1240–58. doi: 10.1002/jclp.20845
68. Park CL, Pless Kaiser A, Spiro A III, King DW, King LA. Does wartime captivity affect late-life mental health? A study of Vietnam-era repatriated prisoners of war. Res Hum Dev. (2012) 9:191–209. doi: 10.1080/15427609.2012.705554
69. APA. Diagnostic and statistical manual of mental disorders, Text Revision (DSM-IV-TR). Washington, DC: APA (2000).
70. APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub (2013).
71. Friedman MJJJ. Finalizing PTSD in DSM-5: getting here from there and where to go next. J Trauma Stress. (2013) 26:548–56. doi: 10.1002/jts.21840
72. Briere J, Godbout N, Dias C. Cumulative trauma, hyperarousal, and suicidality in the general population: a path analysis. J Trauma Dissociation. (2015) 16:153–69. doi: 10.1080/15299732.2014.970265
73. Schmidt NB, Woolaway-Bickel K, Bates M. Evaluating panic-specific factors in the relationship between suicide and panic disorder. Behav Res Ther. (2001) 39:635–49. doi: 10.1016/S0005-7967(00)00034-6
74. Katz C, Yaseen ZS, Mojtabai R, Cohen LJ, Galynker II. Panic as an independent risk factor for suicide attempt in depressive illness: findings from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. (2011) 72:1628–35. doi: 10.4088/JCP.10m06186blu
75. Capron DW, Cougle JR, Ribeiro JD, Joiner TE, Schmidt NB. An interactive model of anxiety sensitivity relevant to suicide attempt history and future suicidal ideation. J Psychiatr Res. (2012) 46:174–80. doi: 10.1016/j.jpsychires.2011.10.009
76. Price RK, Risk NK, Haden AH, Lewis CE, Spitznagel EL. Post-traumatic stress disorder, drug dependence, and suicidality among male Vietnam veterans with a history of heavy drug use. Drug Alcohol Depend. (2004) 76:S31–43. doi: 10.1016/j.drugalcdep.2004.08.005
77. Berkowitz L. Frustration-aggression hypothesis: examination and reformulation. Psychol Bull. (1989) 106:59–73. doi: 10.1037/0033-2909.106.1.59
78. Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment Dev Psychopathol. (1999) 11:59–84. doi: 10.1017/S0954579499001959
79. Weiss B, Catron T. Specificity of the comorbidity of aggression and depression in children. J Abnorm Child Psychol. (1994) 22:389–401. doi: 10.1007/BF02168081
80. Afifi TO, Boman J, Fleisher W, Sareen J. The relationship between child abuse, parental divorce, and lifetime mental disorders and suicidality in a nationally representative adult sample. Child Abuse Neglect. (2009) 33:139–47. doi: 10.1016/j.chiabu.2008.12.009
81. Fergusson DM, Lynskey MT. Physical punishment/maltreatment during childhood and adjustment in young adulthood. Child Abuse Neglect. (1997) 21:617–30. doi: 10.1016/S0145-2134(97)00021-5
82. Herman DB, Susser ES, Struening EL, Link BL. Adverse childhood experiences: are they risk factors for adult homelessness? Am J Public Health. (1997) 87:249–55. doi: 10.2105/AJPH.87.2.249
83. Cho MK, Cho H-I. The relationship between child abuse and school violence: the mediating effects of aggression and depression. Korean J Sch Psychol. (2019) 16:17–38.
84. Biehn TL, Elhai JD, Seligman LD, Tamburrino M, Armour C, Forbes D. Underlying dimensions of DSM-5 posttraumatic stress disorder and major depressive disorder symptoms. Psychol Inj Law. (2013) 6:290–8. doi: 10.1007/s12207-013-9177-4
85. Paivio SC. Stability of retrospective self-reports of child abuse and neglect before and after therapy for child abuse issues. Child Abuse Negl. (2001) 25:1053–68. doi: 10.1016/S0145-2134(01)00256-3
86. Kim JS, Jin MJ, Jung W, Hahn SW, Lee S-H. Rumination as a mediator between childhood trauma and adulthood depression/anxiety in non-clinical participants. Front Psychol. (2017) 8:1597. doi: 10.3389/fpsyg.2017.01597
87. Lee SH, Park Y, Jin MJ, Lee YJ, Hahn SW. Childhood trauma associated with enhanced high frequency band powers and induced subjective inattention of adults. Front Behav Neurosci. (2017) 11:148. doi: 10.3389/fnbeh.2017.00148
88. Kim S, Kim JS, Jin MJ, Im CH, Lee SH. Dysfunctional frontal lobe activity during inhibitory tasks in individuals with childhood trauma: an event-related potential study. Neuroimage Clin. (2018) 17:935–42. doi: 10.1016/j.nicl.2017.12.034
89. Jin MJ, Jeon H, Hyun MH, Lee S-H. Influence of childhood trauma and brain-derived neurotrophic factor Val66Met polymorphism on posttraumatic stress symptoms and cortical thickness. Sci Rep. (2019) 9:1–12. doi: 10.1038/s41598-019-42563-6
90. Kwon A, Min D, Kim Y, Jin MJ, Lee SH. Interaction between catechol-O-methyltransferase polymorphism and childhood trauma in suicidal ideation of patients with post-traumatic stress disorder. Brain Behav. (2020) 10:e01733. doi: 10.1002/brb3.1733
Keywords: PTSD, suicide, childhood physical abuse, depression, hyperarousal
Citation: Kwon A, Lee HS and Lee S-H (2021) The Mediation Effect of Hyperarousal Symptoms on the Relationship Between Childhood Physical Abuse and Suicidal Ideation of Patients With PTSD. Front. Psychiatry 12:613735. doi: 10.3389/fpsyt.2021.613735
Received: 29 October 2020; Accepted: 03 March 2021;
Published: 26 March 2021.
Edited by:
Liliana Dell'Osso, University of Pisa, ItalyReviewed by:
Maayan Shorer, Ruppin Academic Center, IsraelSebastian Trautmann, Medical School Hamburg, Germany
Copyright © 2021 Kwon, Lee and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seung-Hwan Lee, lshpss@paik.ac.kr; lshpss@hanmail.net
 Aeran Kwon1
Aeran Kwon1