- 1Experimental Psychopathology Lab, Institute of Psychology, Polish Academy of Sciences, Warsaw, Poland
- 2Department of Psychiatry, Wroclaw Medical University, Wroclaw, Poland
- 3Department of Community Psychiatry, Chair of Psychiatry, Medical College Jagiellonian University, Krakow, Poland
- 4Orygen, Parkville, VIC, Australia
- 5Centre for Youth Mental Health, The University of Melbourne, Parkville, VIC, Australia
- 6Medical University of Warsaw, Warsaw, Poland
Although self-disturbances (SD) are considered to be a core psychopathological feature of schizophrenia spectrum disorders, there is still insufficient empirical data on the mechanisms underlying these anomalous self-experiences. The aim of the present study was to test a hypothesized model in which cognitive biases and exposure to traumatic life events are related to the frequency of SD which, in turn, contribute to the frequency of psychotic-like experiences (PLEs). Our sample consisted of 193 Polish young adults from the general population (111 females; 18–35 years of age, M = 25.36, SD = 4.69) who experience frequent PLEs. Participants were interviewed for PLEs, SD and social functioning as well as completed self-reported questionnaires and behavioral tasks that measure cognitive biases (e.g., safety behaviors, attention to threat, external attribution, jumping to conclusion, source monitoring, overperceptualization). The model was tested using path analysis with structural equation modeling. All of the hypothesized relationships were statistically significant and our model fit the data well [χ2(23) = 31.201; p = 0.118; RMSEA = 0.043 (90% CI = 0.00–0.078), CFI = 0.985, SRMR = 0.041, TLI = 0.976]. The results revealed a significant indirect effect of traumatic life events on PLEs through SD and self-reported cognitive biases. However, performance-based cognitive biases measured with three behavioral tasks were unrelated to SD and PLEs. The frequency of SD explained a substantial part (43.1%) of the variance in PLEs. Further studies with longitudinal designs and clinical samples are required to verify the predictive value of the model.
Introduction
Phenomenological analyses along with empirical studies suggest that self-disturbances (SD), which are anomalous experiences of basic sense of self, are the core psychopathological feature and phenotypic trait marker of schizophrenia spectrum disorders (1–6). SD refers to the so-called minimal or basic self (“ipseity”), which is conceptualized as the tacit, pre-reflective level of selfhood and the ground of various aspects of conscious awareness (5). It is thought that instability of this minimal self gives rise to anomalous subjective experiences (e.g., a sense that one's thoughts are anonymous and “not mine,” a feeling as if the boundary between self and world is unclear), which may evolve into frank psychotic symptoms (7). In fact, it has been shown that SD precede the development of clinical symptoms of psychosis (8, 9) and may be observed also among patients at risk for psychosis (10–12). Koren et al. (13), in a study of non-psychotic help-seeking adolescents, showed that SD and subclinical psychotic symptoms constitute related but distinct dimensions of potential risk. Furthermore, SD has been found to be related to psychotic-like experiences (PLEs) in non-clinical samples (14–18). These studies, indicating that SD, along with PLEs, are present both in non-clinical and clinal samples, are in line with the hypothesis of a continuous distribution of psychotic symptoms in the general population (19).
Despite SD great importance to the conceptualization of psychosis, there is still insufficient empirical data on the mechanisms underlying these experiences. Recent studies have shown (16, 17) that cognitive biases, that is, dysfunctional information processing patterns leading to maladaptive conclusions and emotional dysregulation, are related to SD. Nelson et al. (20) introduced a theoretical model in which source monitoring deficits are proposed as one of the neurocognitive correlates of SD, especially in the sense of “ownership” of experiences. Source monitoring is a cognitive bias that involves difficulties in making attributions about the origins of experience, for example, whether an event happened to us, whether we just imagined it or someone told us about it. The recent study by Nelson et al. (21) confirmed the relationship between source monitoring, assessed using a variety of neurocognitive and neurophysiological tasks, and SD in patients with early psychosis. The cognitive model of positive symptoms of psychosis (22) emphasizes the importance of cognitive distortions in generating anomalous conscious experiences as well.
Another contributor to SD could be traumatic experiences. Recently, growing evidence suggests that traumatic life events play a significant role in the development of psychosis (23–25). Exposure to trauma is not only significantly more frequent in schizophrenia spectrum disorders than in the general population (25, 26), but also early adverse life events increase the frequency of PLEs in non-clinical individuals (27–29). However, the mechanisms of the relationship between trauma and psychosis still needs further investigation. Sass and Borda (30) proposed that schizophrenia spectrum disorders manifest through SD that could be primary or secondary in nature. Primary SD reflect disturbances in early neurodevelopment, whereas secondary SD appear later as defensive-compensatory reactions to other factors such as childhood adversities, social stress and marginalization. Haug et al. (31) found that traumatic events are indeed significantly associated with higher levels of SD in patients with schizophrenia, but only in women. Recent studies have shown that SD mediate the relationship between traumatic-life events and psychosis proneness in the general population (16, 17). These results suggested that trauma may affect the risk of psychosis through alterations in the basic sense of self.
Based on the above-mentioned literature, the aim of the current study was to test the hypothesized model of cognitive biases and exposure to traumatic life events being related to the frequency of SD which, in turn, contribute to the frequency of PLEs. Therefore, we expected an indirect effect of traumatic experiences and cognitive biases on PLEs through SD. We focused on positive PLEs, since the assumed relationships between variables of interest concern primarily this dimension of psychotic experiences. This model is an extension of one that was previously proposed and tested in a sample of university students (16). The current study was conducted amongst people drawn from the general population (i.e., a non-clinical population) who experience frequent PLEs and therefore are at psychometric risk of developing psychosis. The selected group was evaluated in terms of meeting clinical criteria of ultra-high risk (UHR) of psychosis. The goal of this strategy was to estimate the prevalence of clinical risk of psychosis among people from the general population who are not seeking help. For the measurement of cognitive biases, we used both self-report questionnaires and performance-based behavioral tasks, as they can possibly represent somewhat different constructs (32).
Materials and Methods
Participants
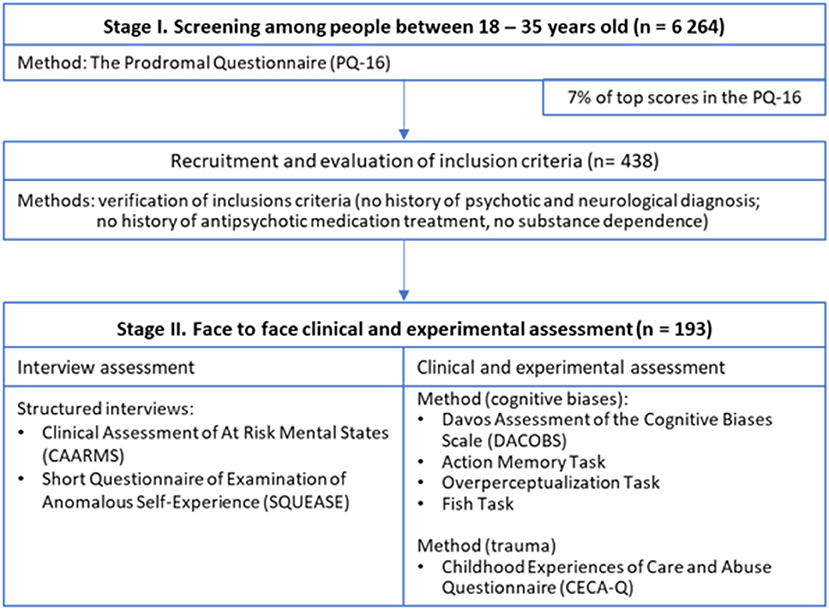
Our study was conducted in two stages (see Figure 1). First, a total sample of 6,264 Polish young adults (3,932 females) aged between 18 and 35 years (M = 26.51, SD = 4.76) were screened for psychometric risk of psychosis using the Prodromal Questionnaire (PQ-16) (33). Screening was carried out via Internet in collaboration with an external company specializing in acquiring for research purposes large population samples and conducting online surveys. Completing the online survey took about 20–30 min. Participants were enrolled from three large Polish cities: Warsaw (1,700,000 inhabitants), Krakow (770,000 inhabitants) and Wroclaw (640,000 inhabitants). Those who scored within 7%1 of top results on the PQ-16 (i.e., had frequent PLEs) and met inclusion criteria were approached to participate in the second stage of the study conducted through face to face assessment. Exclusion criteria for participants were screened with self-report questions which included: a history of any psychotic or neurological diagnosis, history of antipsychotic medication treatment and substance dependence disorder in the previous 6 months. Other psychiatric diagnoses such as major depressive disorder (without psychotic symptoms), bipolar disorder (without psychotic symptoms), personality disorders or anxiety disorders were not considered as exclusion criteria. Four hundred thirty-eight people met inclusion criteria, however 245 respondents could not be contacted or refused to participate in the second stage of the study. The final sample consisted of 193 individuals (111 females, age M = 25.36, SD = 4.69). Face to face assessment in the second stage of the study involved assessment of SD, PLEs, exposure to traumatic life events and cognitive biases. The participants' informed consent was obtained and the ethics committee of the Medical University of Warsaw approved the study.
Measures
Psychotic-Like Experiences
To assess PLEs in the screening stage of the study we used the sixteen-item Prodromal Questionnaire (PQ-16) (33). The PQ-16 is a self-report questionnaire to screen for psychosis risk operationalized as a presence of PLEs. It is a shortened version of the 92-item PQ and consists of items that assess perceptual abnormalities and hallucinations, unusual thought content, delusional ideas, and paranoia as well as negative symptoms on a scale: present vs. non-present –(true vs. false) which we modified to better reflect the frequency of PLEs. Specifically, we used a four-point scale: “never”, “sometimes”, “often”, and “almost always”. The scores range from 0 to 48 points. Most of the items in the PQ-16 refer to attenuated positive psychotic symptoms. The PQ-16 has satisfactory psychometric characteristics in the assessment of PLEs with a specificity and sensitivity of 87% in discriminating patients meeting the criteria of UHR from those who do not meet UHR criteria (33). The scale was validated also in non-help-seeking populations (34, 35). We used a Polish version of the questionnaire (17). Cronbach's alpha for the total score was 0.82.
To evaluate PLEs for their clinical relevance in the second stage of the study we used the Comprehensive Assessment of At-Risk Mental States (CAARMS) (36), for the Polish version see: Jaracz et al. (37). The CAARMS is a semi-structured interview designed to investigate different aspects of attenuated psychopathology and functioning factors over time. The CAARMS consists of seven subscales: positive symptoms (subclinical delusions and hallucinations); negative symptoms (anhedonia, blunted affect, social withdrawal); cognitive changes; behavior changes; motor or physical changes; emotional disturbances; general psychopathology. This instrument allows for assessment of clinical state of UHR of psychosis. Symptoms are evaluated for their severity and frequency on scales ranging from 0 to 6. In our study, we focused on the severity and frequency of the positive symptom subscale that includes: unusual thought content, non-bizarre ideas, perceptual abnormalities, and disorganized speech. The positive symptoms subscale served as an indicator of psychosis proneness (with the combined score for the frequency and the severity subscales from 0 to 48). Cronbach's alpha for this subscale calculated in our sample was 0.82.
Self-Disturbances
To evaluate SD we used the SQUEASE (Møller, private materials). This is a short version of the Examination of Anomalous Self-Experience (EASE), which is a semi-structured phenomenological interview developed by Parnas et al. (38) to examine a wide variety of anomalies considered to be disorders of basic or “minimal” self. The construction of EASE was based on self-descriptions obtained from patients suffering from schizophrenia spectrum disorders. The EASE was used also in non-clinical populations (14, 39). The short version (the SQUEASE) was created by Møller, one of the co-authors of EASE. The SQUEASE consists of 13 items that are grouped into four sections: (1) Cognition and Stream of Consciousness (items include: disorder of short-term memory, attentional disturbances, ruminations-obsessions, thought interference, thought pressure, loss of thought ipseity) (2) Self-Awareness and Presence (items include: distorted first-person perspective, diminished sense of basic self, hyperrefl ectivity, derealization (3) Bodily Experiences (items include: mirror-related phenomena), (4) Existential Reorientation (items include: existential or intellectual change, feeling as if the experienced world is not truly real). These items evaluate SD for their frequency and level of presence on scales ranging from 0 to 4. The possible result for the frequency scale is in the range from 0 to 52. Cronbach's alpha calculated in our sample for the frequency scale was 0.84.
Exposure to Traumatic Life Events
Childhood Experiences of Care and Abuse Questionnaire (CECA.Q) (40) was used to investigate traumatic life events retrospectively such as lack of parental care (neglect and antipathy), parental psychological abuse, role reversal, parental physical abuse, and sexual abuse from an adult before the age of 17. The CECA.Q has been validated among psychotic patients (41) as well as in non-clinical samples (42, 43). It consists of different types of trauma subscales that allow for a wide assessment of traumatic life events. Cronbach's alpha for the total score in our sample was 0.96.
Social Functioning
Social and Occupational Functioning Assessment Scale (SOFAS) (44) is a one-item rating of an individual's functioning scored 0–100. It is intended to assess social and occupational functioning independently of the overall severity of symptoms.
Self-Report Cognitive Biases
The Davos Assessment of Cognitive Biases Scale (DACOBS) (45), for the Polish version, see: Gaweda et al. (46) is a self-report scale that assesses cognitive biases associated with psychosis. The questionnaire contains 42 items to be scored on a 7-point Likert scale, therefore the scores range from 42 to 294 points. All items are grouped into seven subscales and three clusters related to different types of biases: (1) specifically associated with psychosis: jumping to conclusions bias, belief inflexibility bias, attention to threat bias, external attribution bias, (2) associated with cognition: social cognition problems and subjective cognitive problems, and (3) related to coping strategies: safety behaviors. Cronbach's alpha for the total score was 0.89.
Performance-Based Cognitive Biases
Three computer-based tasks were used to assess different cognitive biases:
Overperceptualization bias was measured with a computer-based task of auditory false perceptions—Overperceptualization Task (47). The overperceptualization paradigm assesses the process by which individuals recognize auditory stimuli when in fact they are not present. In this task participants are presented with stimuli in the form of words in three conditions: (1) words can only be heard (audio condition, 60 trials), (2) words can be spoken by a lector who is heard and simultaneously seen on the screen (video condition, 60 trials), (3) before the lector appears on the screen, participants see a board with the word that will be spoken (board condition, 60 trials). Each word is accompanied by background noise making the word difficult to recognize. In 40% of stimuli in each of the three conditions, the lector does not read the word, but only moves his mouth; thus only noise can be heard. Participants have to decide after each word whether they heard a word or not and determine the degree of certainty in their decision. Subjects are instructed to respond as quickly as possible. False auditory perceptions (i.e., hearing a word when it was not spoken) serve as an indicator of overperceptualization bias (ranging from 0 to 72).
Source monitoring deficits were evaluated with Action Memory Task (AMT). The AMT is a computer-based task (48), for Polish version see: Gaweda et al. (49) comprising of 36 actions that are described to participants through text messages (18) or shown through images (18). Each action is imagined or performed by participants. Imagined actions are presented with a red frame, actions that have to be performed have a green frame. Each action is presented for 10 s. The memory retrieval phase starts after a short break. All imagined and performed actions are shown to the participants in random succession, as well as new ones (56 actions in total). In a recognition part of the study, participants are asked to attribute all actions as they were presented. The sum of performed actions recognized as imagined and imagined actions recognized as performed was used as an indicator of source monitoring deficits (ranging from 0 to 36).
Jumping to conclusions bias was measured with Fish Task (50). This task is a revised and computerized version of the beads task (51, 52) which differs from the original task in that a different scenario (lakes with fish instead of jars with beads) is presented. We used two versions of the probabilistic reasoning task which varied in terms of the discrimination ratio. The first version had a high discrimination ratio (80:20) with unambiguous evidence, whereas the second was more difficult with fish in low discriminability (60:40), representing more ambiguous evidence. The instructions were standardized and presented on a computer screen. After each fish was “caught” participants were required to make two judgments: (1) a probability judgment about the likelihood that the fish was caught from either lake A or lake B, and (2) judgment as to whether the available amount of information would justify a decision or not. The number of draws (from 1 to 10) needed to make a decision was an indicator of jumping to conclusion bias (with fewer draws indicating increased jumping to conclusions bias).
Statistical Analysis
All statistical analyses were performed with SPSS version 25.0 and Amos version 25.0.
First, we tested for correlations among the variables of interest by calculating Pearson's correlational coefficients. SD and their relationship with exposure to traumatic life events are at the center of our interest, thus we explored this association in more detail by checking which traumatic events are related to SD. Then, we performed confirmatory factors analysis (CFA) of the latent variable of self-report cognitive biases to verify the original structure of this measure. For performance-based cognitive biases, we aimed to build a factorial model consisting of the results of three tasks: Action Memory, Overperceptualization and Fish Task. PLEs, SD and exposure to traumatic life events were represented in our model by single indicator variables. This decision was dictated by the absence of an established factorial model for positive symptoms in CAARMS, SQUEASE and CECA.Q measures. It also enabled conserving free parameters and increased stability of the parameter estimates for the models.
In the next step, we evaluated hypothesized associations with the structural equation model (SEM) in a series of path analyses to test our theoretical model. Therefore, we tested for the indirect effect of traumatic life events through SD and cognitive biases to PLEs. For this purpose, we used the bootstrap method as recommended by Preacher and Hayes (53). Due to different measurement methods (questionnaire vs. computer-based tasks) we aimed to perform path analyses separately for self-report and performance-based cognitive biases.
The goodness of fit to the data for both analyses (CFA and path analyses) were estimated with the maximum likelihood estimation procedure with the Bollen-Stine bootstrap (n = 2,000) procedure of correction for non-normal distribution. We verified goodness of model fit following the guidelines from literature (54): RMSEA <0.06 (The Root Mean Square Error of Approximation); SRMR <0.08 (The Standardized Root Mean Square Residual); CFI > 0.95 (Confirmatory Fit Index) and TLI > 0.95 (Tucker- Lewis Index).
Results
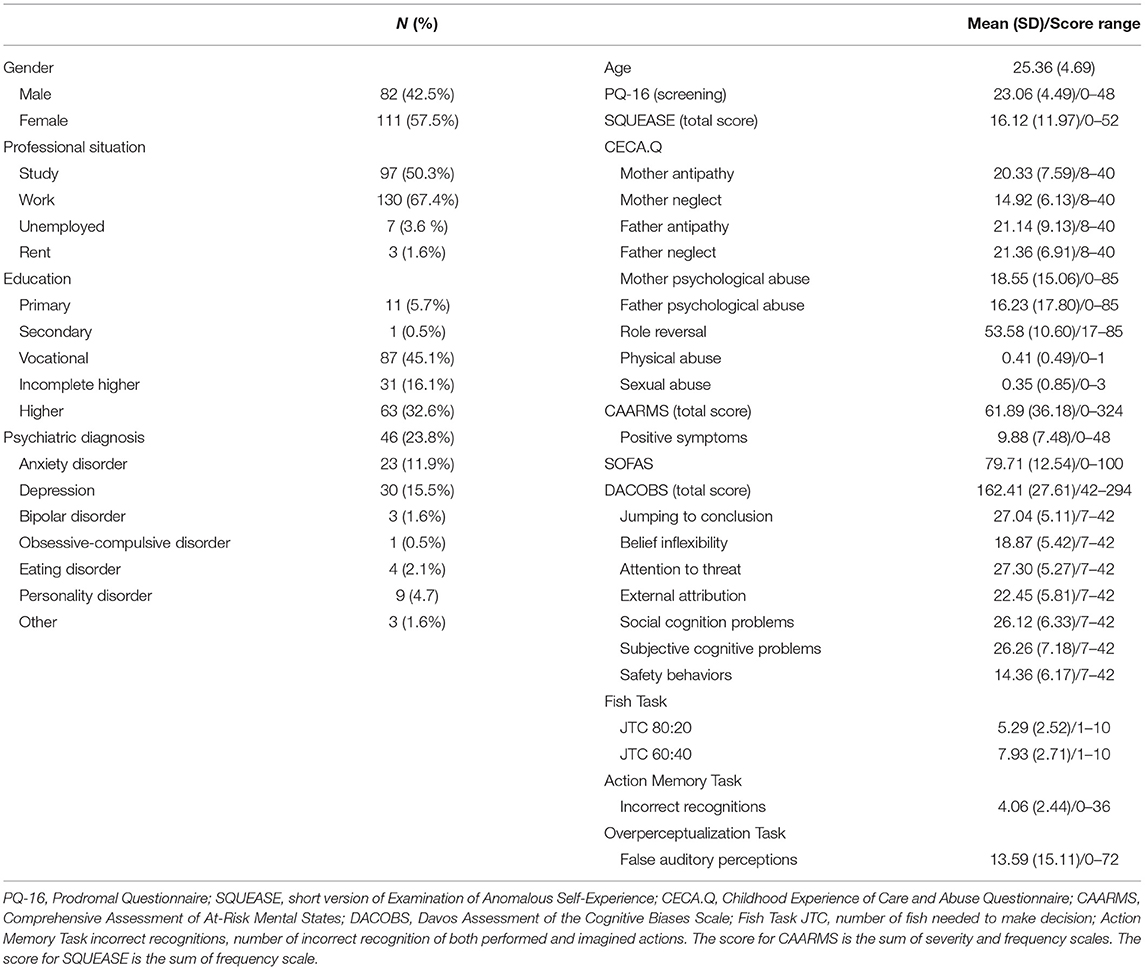
Characteristics of the Sample
The sample characteristics are presented in Table 1. Fifty-one participants from the sample of 193 individuals (26.4%) met the symptom criteria for UHR status after being interviewed with the CAARMS. However, full criteria for UHR status were not met as the group was not help-seeking and their social functioning, as measured using the SOFAS, did not meet UHR functional decline/chronic low functioning requirements.
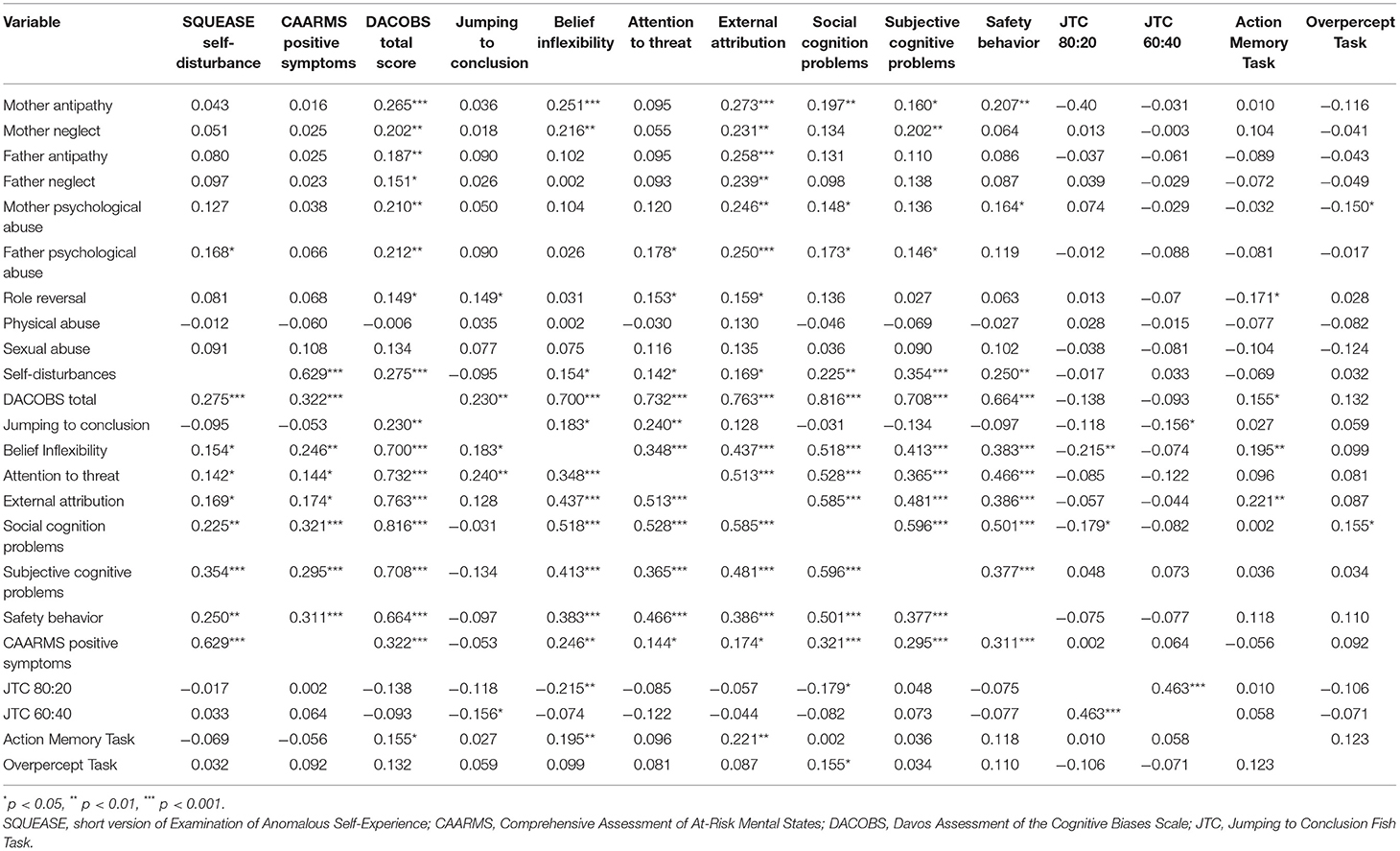
Correlational Analysis
Table 2 presents the results of the correlational analysis. The strongest significant relationship was found between SD and PLEs (r = 0.629, p < 0.001). SD correlated significantly also with self-report cognitive biases and psychological abuse from the father. Except for physical and sexual abuse, all other types of traumatic life events significantly correlated with self-report cognitive biases. It is of note that no subscale of CECA.Q was significantly related to PLEs. These statistically significant relationships among variables of interest allowed for further testing of our hypothesized model with SEM. Surprisingly, no significant relationships were found between performance-based cognitive biases and SD as well as PLEs, thus planned path analysis with these variables was not performed. Furthermore, we found a highly significant correlation between self-report cognitive biases and PLEs. Thus, we decided to investigate an additional model including this path. Gender was not included in path analyses as it was not significantly related to exposure to trauma and other variables of interest. Age significantly correlated with SD (r = −0.176, p < 0.05), PLEs (r = −0.181, p < 0.05) and cognitive biases (r = −0.162, p < 0.05). However, those paths turned out to be insignificant thus we did not include them in the final analyses.
Measurement Model
Due to the inability to confirm the original latent structure of the 42-item DACOBS questionnaire measuring cognitive biases, we decided to use as indicator variables the sum of the points obtained in each subscale instead of all single items. We removed only jumping to conclusion subscale because of its insignificant loading. Thus, the final latent structure for self-report cognitive biases consisted of six indicators (belief inflexibility, attention to threat, external attribution, social cognition problems, subjective cognitive problems, and safety behaviors) and fit the data well [χ2 (7) = 2.791, p > 0.05; RMSEA = 0.00 (90% CI = 0.000–0.037), CFI = 1.00, TLI = 1.023, SRMR = 0.014]. For PLEs, SD and traumatic life events, we used single indicator variables, which was the sum of the frequency and severity scales obtained for all items in the positive symptoms subscale of CAARMS and in father psychological abuse subscale of CECA.Q. In the case of SD we used only the sum of the frequency scale, as the level of presence is a qualitative scale.
Path Analyses
Results of first path analysis suggested a model that fit the data well [χ2 (23) = 33.780, p = 0.068; RMSEA = 0.049 (90% CI = 0.000–0.083), CFI = 0.980, TLI = 0.968, SRMR = 0.044]. However, the path from father psychological abuse to SD turned out to be insignificant. A detailed model is presented in the Supplementary Figure 1. Therefore, we checked for correlations between SD and all single items representing trauma. We selected 12 specific items measuring trauma that were significantly related to SD and used their sum as an indicator variable of exposure to trauma in further path analyses. Those items originally constituted psychological abuse (nine items), role reversal (two items) and parental care (one item) subscales. Detailed correlational analysis between the SQUEASE and CECA.Q items is presented in Supplementary Table 1.
The first model with initially hypothesized relationships is depicted with its standardized path coefficients (standardized regression weights) in Figure 2. The bootstrapping estimate revealed a significant standardized indirect effect of traumatic life events through SD and cognitive biases to PLEs (β = 0.181, 95% CI = 0.102–0.267, p = 0.001). This model explained 39.6% of the variance in PLEs. All of the model fit indices were satisfactory: χ2(24) = 40.847; p = 0.017; RMSEA = 0.060 (90% CI = 0.025–0.091), CFI = 0.968, SRMR = 0.059, TLI = 0.953.
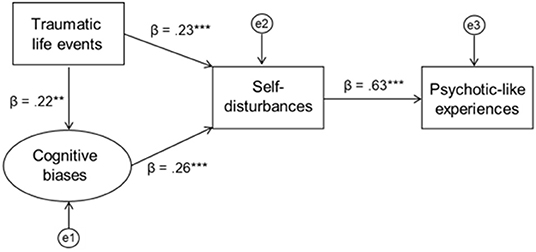
Figure 2. The model of the direct relationship between self-disturbances and psychotic-like experiences with childhood trauma and self-report cognitive biases as the potential contributors to self-disturbances.
The second model includes an additional path from self-report cognitive biases to PLEs and is presented in Figure 3. Standardized indirect effect of traumatic life events through SD and cognitive biases to PLEs was significant (β = 0.207, 95% CI = 0.126–0.293, p = 0.001). The percentage of the variance explained in PLEs was equal to 43.1%. The model has a good fit: χ2(23) = 31.201; p = 0.118; RMSEA = 0.043 (90% CI = 0.00–0.078), CFI = 0.985, SRMR = 0.041, TLI = 0.976.
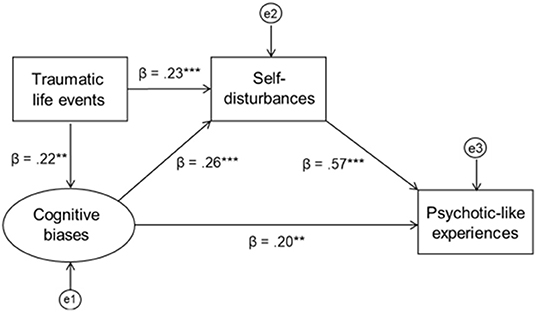
Figure 3. The model of the indirect relationship between childhood trauma and psychotic-like experiences with self-disturbances and cognitive biases as the potential mechanisms underlying this relationship.
Discussion
In the current study, we focused on the relationship between SD and PLEs with exposure to traumatic life events and cognitive biases as potential mechanisms underlying SD. All of the hypothesized associations were found to be statistically significant and the model fit the data well. SD along with its postulated mechanisms explained a substantial part of the variance in PLEs, pointing to the importance of this construct in elucidating and understanding psychosis risk. Results of our study, although obtained in a non-clinical sample, are in line with the basic-self-disorder model of schizophrenia (5, 55).
Several points should be noted regarding the results of our study. First, we found a statistically significant indirect effect of trauma on PLEs, which is consistent with many theoretical and empirical accounts on the role of trauma in shaping psychosis risk (56–59). However, the strength of this relationship was smaller than we expected. One of the possible reasons could lie in the nature of our sample. Although participants in the study reported the highest frequency of PLEs from the screening sample, they functioned well-socially and professionally. In fact, one-quarter of them met the symptomatic criteria for UHR and it was a relatively high level of their functioning that excluded a full diagnosis of this kind. It is likely that individuals with higher social and professional functioning have been less frequently exposed to traumatic-life events (60).
Moreover, we did not find a direct relationship between trauma and PLEs, which contradicts the results obtained in other research (61–63). However, de Vos et al. (64) in their recent study among UHR for psychosis youth acquired similar outcomes, that is, childhood trauma appeared to be unrelated to attenuated psychotic symptoms. In fact, some researchers found the relationship between maltreatment and PLEs to be fully mediated by various mechanisms such as borderline personality features, dissociation, perceived stress, negative-other beliefs or external locus of control (16, 65–67). Those results are consistent with the postulate that trauma alone is not a sufficient factor to cause PLEs (68). The results of our study suggest that to provoke PLEs exposure to trauma first may need to disturb the basic sense of self and trigger dysfunctional changes in information processing from the environment. According to Sass and Borda (30) the relationship between trauma and SD could be explained by dissociative reactions. They introduced the concept of secondary diminished self-presence, one of the aspects of SD, that could be the result of defensive—and in this sense secondary—dissociative reactions to traumatic situations (55). Indeed, the associations between trauma and SD or trauma and dissociation were found in both clinical (31, 69) and non-clinical (16, 17, 66) samples. It has also been shown that dissociative processes are related to childhood adversity in patients with schizophrenia spectrum disorders (69, 70) and in psychosis proneness (71).
The role of the second possible mechanism of SD—cognitive biases—is somewhat more difficult to interpret. Although self-report cognitive distortions showed an association between trauma and PLEs, this was not the case for performance-based cognitive biases. None of the tasks we used in our study was significantly related to neither SD nor PLEs. Moreover, even the correlations between the two distinct measures of cognitive biases turned out to be much smaller and less numerous than we expected. It is possible that self-report and behavioral tasks assess two different aspects of cognitive biases, that is, the first may capture subjective opinion and be a more or less stable, trait-like construct, whereas the second is the objective measure of distortions that are present here and now (i.e., more state like) and in relation to specific perceptual material. Therefore, performance in behavioral tasks may be more influenced by immediate context and affective state for example, whether the person is feeling stressed, relaxed, distracted at the time of testing. This discrepancy between self-report measures and objective neuropsychological results has been observed in previous studies (72, 73). Another possible reason is that behavioral tasks could be less sensitive measures for capturing biased cognitive processes in non-clinical samples. Future studies should investigate the relationship between objective and subjective measures of information- processing biases in more detail and in clinical groups.
It is worth noting that although we hypothesized cognitive biases affect PLEs solely through SD, correlation analysis clearly indicated a highly significant direct relationship between cognitive biases and PLEs. Path analyses suggest that although there is an indirect effect of trauma on PLEs, our results suggest cognitive biases also make a direct and unique contribution to PLEs that goes beyond the presence of SD. This is in line with a cognitive model of psychosis (22, 74) which assumes that biased information processing can directly give rise to psychotic symptoms. Indeed, previous studies have shown that delusions or delusional ideation, for example, are associated with attributional biases (75, 76) or an exaggerated tendency to pay attention to threat (77–79). It has been postulated that exposure to traumatic events in childhood distorts cognitive schemas in a way that people view the world as threatening and attribute negative events and experiences to external factors (17, 29, 66, 80). These distorted cognitive schemas are then used to interpret and explain new experiences in a paranoid framework (56).
Our model may have clinical implications. Different risk factors such as a history of exposure to trauma, cognitive biases and SD should be considered jointly in screening procedures to maximize chances for identifying people who are at the highest risk for psychosis. As SD was the variable that had the highest regression coefficient with PLEs, particular attention should be paid to identify these anomalous self-experiences when detecting individuals at risk and preventing the development of full-blown psychosis (8). Cognitive biases that were found in our study to be both directly and indirectly associated with PLEs can be successfully addressed in cognitive-behavioral therapy (CBT), for example through metacognitive training (81, 82). Furthermore, Škodlar et al. (83) provided a compelling theoretical account of how psychotherapy may be targeted to the amelioration of SD.
The results of the study should be interpreted in light of its strengths and limitations. The strengths of the study lie in the combination of different levels of measures, namely self-report, clinical interviews and behavioral tasks. To the best of our knowledge, this is the first study simultaneously examining trauma exposure and different types of cognitive biases and their relation to SD and PLEs in a non-clinical sample. However, the cross-sectional design of the study precludes causal inference. Therefore, future longitudinal studies in clinical samples are needed to address causality and capture the change in SD and PLEs over time. Further validation of our model should be carried out using the full version for the clinical interview of SD, the EASE (38). This would allow for an examination of relationships between specific aspects of SD and other variables of interest. Moreover, it should be noted that we focused only on positive PLEs, therefore our results do not relate to the entire range of PLEs, such as negative or disorganized PLEs. Lastly, as our model was tested in a specific sample of people with frequent PLEs, thus the results should not be generalized to the clinical risk of psychosis or people with low or medium frequency of PLEs.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committee of the Medical University of Warsaw, Poland. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
ŁG and RP-U: conceptualization and writing. RP-U: data curation, formal analysis, roles/writing—original draft, and visualization. ŁG: funding acquisition. RP-U, AC, DF, and ŁG: investigation. ŁG, DF, and AC: methodology, project administration, resources, and software. LG: supervision. All authors review & editing.
Funding
This study was supported by the OPUS grant from the National Science Center, Poland (ŁG, 2016/21/B/HS6/03210). RP-U was supported by the ETIUDA doctoral scholarship from the National Science Center, Poland (2019/32/T/HS6/00572).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank the following psychiatrists for the clinical assessment of the study participants: Piotr Bładziński, Marta Cichońska, Aneta Kalisz, Kamila Kotowicz, Aldona Krawczyk, Dawid Kruk, Joanna Krzyzanowska-Zbucka, Joanna Leciak, Błazej Misiak, Patryk Piotrowski, Izabela Stefaniak, Filip Stramecki.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.611069/full#supplementary-material
Footnotes
1. ^We planned to recruit approximately 200 participants from approximately 6000 subjects (3.3% of the sample studied) who would achieve scores on the PQ-16 within the top 10%. We chose a wider percentage of the highest scores to recruit from, expecting that not all participants would meet the inclusion criteria and would be willing to take part in the second stage of the study. Finally, we examined 193 people whose results on the PQ-16 against the entire sample turned out to be in the top 7%.
References
1. Nelson B, Yung AR, Bechdolf A, McGorry PD. The phenomenological critique and self-disturbance: implications for ultra-high risk (“prodrome”) research. Schizophrenia Bull. (2008) 34:381–92. doi: 10.1093/schbul/sbm094
2. Parnas J, Handest P. Phenomenology of anomalous self-experience in early schizophrenia. Compr Psychiatry. (2003) 44:121–34. doi: 10.1053/comp.2003.50017
3. Parnas J. Self and Schizophrenia: A Phenomenological Perspective. Kircher T, editor. Cambridge: Cambridge University Press (2003). p. 217–41. doi: 10.1017/CBO9780511543708.012
4. Raballo A, Parnas J. The silent side of the spectrum: schizotypy and the schizotaxic self. Schizophr Bull. (2011) 37:1017–26. doi: 10.1093/schbul/sbq008
5. Sass LA, Parnas J. Schizophrenia, consciousness, and the self. Schizophr Bull. (2003) 29:427–44. doi: 10.1093/oxfordjournals.schbul.a007017
6. Parnas J, Henriksen MG. Disordered self in the schizophrenia spectrum: a clinical and research perspective. Harv Rev Psychiatry. (2014) 22:251–65. doi: 10.1097/HRP.0000000000000040
7. Nelson B, Sass LA, Parnas J. Basicself Disturbance in the Schizophrenia Spectrum: A Review and Future Directions. Kyrios M, editor. Cambridge: Cambridge University Press (2016). p. 158.
8. Nelson B, Thompson A, Yung AR. Basic self-disturbance predicts psychosis onset in the ultra high risk for psychosis “prodromal” population. Schizophrenia Bull. (2012) 38:1277–87. doi: 10.1093/schbul/sbs007
9. Parnas J, Carter J, Nordgaard J. Premorbid self-disorders and lifetime diagnosis in the schizophrenia spectrum: a prospective high-risk study. Early Interv Psychiatry. (2016) 10:45–53. doi: 10.1111/eip.12140
10. Bonoldi I, Allen P, Madeira L, Tognin S, Bossong MG, Azis M, et al. Basic self-disturbances related to reduced anterior cingulate volume in subjects at ultra-high risk for psychosis. Front Psychiatry. (2019) 10:254. doi: 10.3389/fpsyt.2019.00254
11. Davidsen KA. Anomalous self-experience in adolescents at risk of psychosis. Psychopathology. (2009) 42:361–9. doi: 10.1159/000236907
12. Comparelli A, Corigliano V, De Carolis A, Pucci D, Angelone M, Di Pietro S, et al. Anomalous self-experiences and their relationship with symptoms, neuro-cognition, and functioning in at-risk adolescents and young adults. Compr Psychiatry. (2016) 65:44–9. doi: 10.1016/j.comppsych.2015.09.011
13. Koren D, Reznik N, Adres M, Scheyer R, Apter A, Steinberg T, et al. Disturbances of basic self and prodromal symptoms among non-psychotic help-seeking adolescents. Psychol Med. (2013) 43:1365–76. doi: 10.1017/S0033291712002322
14. Torbet G, Schulze D, Fiedler A, Reuter B. Assessment of self-disorders in a non-clinical population: Reliability and association with schizotypy. Psychiatry Res. (2015) 228:857–65. doi: 10.1016/j.psychres.2015.05.011
15. Koren D, Lacoua L, Rothschild-Yakar L, Parnas J. Disturbances of the basic self and prodromal symptoms among young adolescents from the community: a pilot population-based study. Schizophrenia Bull. (2016) 42:1216–24. doi: 10.1093/schbul/sbw010
16. Gaweda L, Prochwicz K, Adamczyk P, Frydecka D, Misiak B, Kotowicz K, et al. The role of self-disturbances and cognitive biases in the relationship between traumatic life events and psychosis proneness in a non-clinical sample. Schizophr Res. (2018) 193:218–24. doi: 10.1016/j.schres.2017.07.023
17. Gaweda L, Pionke R, Krezolek M, Prochwicz K, Klosowska J, Frydecka D, et al. Self-disturbances, cognitive biases and insecure attachment as mechanisms of the relationship between traumatic life events and psychotic-like experiences in non-clinical adults—a path analysis. Psychiatry Res. (2018) 259:571–8. doi: 10.1016/j.psychres.2017.11.009
18. Cicero DC, Neis AM, Klaunig MJ, Trask CL. The inventory of psychotic-like anomalous self-experiences (IPASE): development and validation. Psychol Assess. (2017) 29:13. doi: 10.1037/pas0000304
19. Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. (2009) 39:179–95. doi: 10.1017/S0033291708003814
20. Nelson B, Whitford TJ, Lavoie S, Sass LA. What are the neurocognitive correlates of basic self-disturbance in schizophrenia?: Integrating phenomenology and neurocognition. Part 1 (Source monitoring deficits). Schizophr Res. (2014) 152:12–9. doi: 10.1016/j.schres.2013.06.022
21. Nelson B, Lavoie S, Gaweda L, Li E, Sass LA, Koren D, et al. The neurophenomenology of early psychosis: an integrative empirical study. Conscious Cogn. (2020) 77:102845. doi: 10.1016/j.concog.2019.102845
22. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. (2001) 31:189–95. doi: 10.1017/S0033291701003312
23. Bonoldi I, Simeone E, Rocchetti M, Codjoe L, Rossi G, Gambi F, et al. Prevalence of self-reported childhood abuse in psychosis: a meta-analysis of retrospective studies. Psychiatry Res. (2013) 210:8–15. doi: 10.1016/j.psychres.2013.05.003
24. Isvoranu A-M, van Borkulo CD, Boyette L-L, Wigman JTW, Vinkers CH, Borsboom D. A network approach to psychosis: pathways between childhood trauma and psychotic symptoms. Schizophrenia Bull. (2016) 43:187–96. doi: 10.1093/schbul/sbw055
25. Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. (2012) 38:661–71. doi: 10.1093/schbul/sbs050
26. Fleming MP, Martin CR. Trauma exposure, schizophrenia symptoms, and the stress vulnerability model. In: Martin CR, Preedy VR, Patel VB, editors. Comprehensive Guide to Post-Traumatic Stress Disorders. Cham: Springer International Publishing (2016). p. 205–29.
27. Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. (2008) 193:378–82. doi: 10.1192/bjp.bp.108.049536
28. Saha S, Varghese D, Slade T, Degenhardt L, Mills K, McGrath J, et al. The association between trauma and delusional-like experiences. Psychiatry Res. (2011) 189:259–64. doi: 10.1016/j.psychres.2011.03.019
29. Gaweda L, Pionke R, Krezolek M, Frydecka D, Nelson B, Cechnicki A. The interplay between childhood trauma, cognitive biases, psychotic-like experiences and depression and their additive impact on predicting lifetime suicidal behavior in young adults. Psychol Med. (2020) 50:116–24. doi: 10.1017/S0033291718004026
30. Sass LA, Borda JP. Phenomenology and neurobiology of self disorder in schizophrenia: secondary factors. Schizophr Res. (2015) 169:474–82. doi: 10.1016/j.schres.2015.09.025
31. Haug E, Oie M, Andreassen OA, Bratlien U, Nelson B, Aas M, et al. Anomalous self-experience and childhood trauma in first-episode schizophrenia. Compr Psychiatry. (2015) 56:35–41. doi: 10.1016/j.comppsych.2014.10.005
32. Elliott CS, Fiszdon JM. Comparison of self-report and performance-based measures of everyday functioning in individuals with schizophrenia: implications for measure selection. Cogn Neuropsychiatry. (2014) 19:485–94. doi: 10.1080/13546805.2014.922062
33. Ising HK, Veling W, Loewy RL, Rietveld MW, Rietdijk J, Dragt S, et al. The validity of the 16-item version of the Prodromal Questionnaire (PQ-16) to screen for ultra high risk of developing psychosis in the general help-seeking population. Schizophr Bull. (2012) 38:1288–96. doi: 10.1093/schbul/sbs068
34. Chen F, Wang L, Wang J, Heeramun-Aubeeluck A, Yuan J, Zhao X. Applicability of the Chinese version of the 16-item Prodromal Questionnaire (CPQ-16) for identifying attenuated psychosis syndrome in a college population. Early Interv Psychiatry. (2016) 10:308–15. doi: 10.1111/eip.12173
35. Kim S-W, Chung Y-C, Kang Y-S, Kim J-K, Jang J-E, Jhon M, et al. Validation of the Korean version of the 16-item prodromal questionnaire in a non-help-seeking college population. Psychiatry Investig. (2018) 15:111. doi: 10.30773/pi.2017.04.24
36. Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. (2005) 39:964–71. doi: 10.1080/j.1440-1614.2005.01714.x
37. Jaracz J, Grzechowiak M, Raczkowiak L, Rataj K, Rybakowski J. Polish version of Comprehensive Assessment of At Risk Mental States (CAARMS)–the description of the method. Polish Psychiatry. (2012) 46:95–107. doi: 10.1037/t52049-000
38. Parnas J, Moller P, Kircher T, Thalbitzer J, Jansson L, Handest P, et al. EASE: examination of anomalous self-experience. Psychopathology. (2005) 38:236–58. doi: 10.1159/000088441
39. Koren D, Rothschild-Yakar L, Lacoua L, Brunstein-Klomek A, Zelezniak A, Parnas J, et al. Attenuated psychosis and basic self-disturbance as risk factors for depression and suicidal ideation/behaviour in community-dwelling adolescents. Early Interv Psychiatry. (2019) 13:532–8. doi: 10.1111/eip.12516
40. Smith N, Lam D, Bifulco A, Checkley S. Childhood experience of care and abuse questionnaire (CECA.Q). Validation of a screening instrument for childhood adversity in clinical populations. Soc Psychiatry Psychiatr Epidemiol. (2002) 37:572–9. doi: 10.1007/s00127-002-0589-9
41. Fisher HL, Craig TK, Fearon P, Morgan K, Dazzan P, Lappin J, et al. Reliability and comparability of psychosis patients' retrospective reports of childhood abuse. Schizophrenia Bull. (2011) 37:546–53. doi: 10.1093/schbul/sbp103
42. Carvalho CB, da Motta C, Pinto-Gouveia J, Peixoto E. Influence of family and childhood memories in the development and manifestation of paranoid ideation. Clin Psychol Psychother. (2016) 23:397–406. doi: 10.1002/cpp.1965
43. Fisher HL, Jones PB, Fearon P, Craig TK, Dazzan P, Morgan K, et al. The varying impact of type, timing and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychol Med. (2010) 40:1967. doi: 10.1017/S0033291710000231
44. DSM-IV. Diagnostic and Statistical Manual of Mental Disorders. 4th edition. Association AP, editor. Washington, DC: American Psychiatric Publishing (1994).
45. van der Gaag M, Schutz C, Ten Napel A, Landa Y, Delespaul P, Bak M, et al. Development of the Davos assessment of cognitive biases scale (DACOBS). Schizophr Res. (2013) 144:63–71. doi: 10.1016/j.schres.2012.12.010
46. Gaweda Ł, Prochwicz K, Cella M. Cognitive biases mediate the relationship between temperament and character and psychotic-like experiences in healthy adults. Psychiatry Res. (2015) 225:50–7. doi: 10.1016/j.psychres.2014.10.006
47. Gaweda Ł, Moritz S. The role of expectancies and emotional load in false auditory perceptions among patients with schizophrenia spectrum disorders. European Archives of Psychiatry Clinical Neuroscience. 2019:1–10. doi: 10.1007/s00406-019-01065-2
48. Moritz S, Ruhe C, Jelinek L, Naber D. No deficits in nonverbal memory, metamemory and internal as well as external source memory in obsessive-compulsive disorder (OCD). Behav Res Ther. (2009) 47:308–15. doi: 10.1016/j.brat.2009.01.004
49. Gaweda Ł, Moritz S, Kokoszka A. Impaired discrimination between imagined and performed actions in schizophrenia. Psychiatry Res. (2012) 195:1–8. doi: 10.1016/j.psychres.2011.07.035
50. Moritz S, Thoering T, Kühn S, Willenborg B, Westermann S, Nagel M. Metacognition-augmented cognitive remediation training reduces jumping to conclusions and overconfidence but not neurocognitive deficits in psychosis. Front Psychol. (2015) 6:1048. doi: 10.3389/fpsyg.2015.01048
51. Speechley WJ, Whitman JC, Woodward TS. The contribution of hypersalience to the “jumping to conclusions” bias associated with delusions in schizophrenia. J Psychiatry Neurosci. (2010) 35:7. doi: 10.1503/jpn.090025
52. Moritz S, Veckenstedt R, Randjbar S, Hottenrott B, Woodward TS, Eckstaedt FV, et al. Decision making under uncertainty and mood induction: further evidence for liberal acceptance in schizophrenia. Psychol Med. (2009) 39:1821–9. doi: 10.1017/S0033291709005923
53. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. (2008) 40:879–91. doi: 10.3758/BRM.40.3.879
54. Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Modeling. (1999) 6:1–55.
55. Sass L, Borda JP, Madeira L, Pienkos E, Nelson B. Varieties of Self Disorder: A Bio-Pheno-Social Model of Schizophrenia. Schizophr Bull. (2018) 44:720–7. doi: 10.1093/schbul/sby001
56. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. (2014) 383:1677–87. doi: 10.1016/S0140-6736(13)62036-X
57. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. (2018) 44:1111–22. doi: 10.1093/schbul/sbx161
58. Freeman D, Fowler D. Routes to psychotic symptoms: trauma, anxiety and psychosis-like experiences. Psychiatry Res. (2009) 169:107–12. doi: 10.1016/j.psychres.2008.07.009
59. Heins M, Simons C, Lataster T, Pfeifer S, Versmissen D, Lardinois M, et al. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. (2011) 168:1286–94. doi: 10.1176/appi.ajp.2011.10101531
60. Stain HJ, Brønnick K, Hegelstad WTV, Joa I, Johannessen JO, Langeveld J, et al. Impact of interpersonal trauma on the social functioning of adults with first-episode psychosis. Schizophrenia Bull. (2014) 40:1491–8. doi: 10.1093/schbul/sbt166
61. Soosay I, Silove D, Bateman-Steel C, Steel Z, Bebbington P, Jones PB, et al. Trauma exposure, PTSD and psychotic-like symptoms in post-conflict Timor Leste: an epidemiological survey. BMC Psychiatry. (2012) 12:229. doi: 10.1186/1471-244X-12-229
62. Metel D, Arciszewska A, Daren A, Pionke R, Cechnicki A, Frydecka D, et al. Mediating role of cognitive biases, resilience and depressive symptoms in the relationship between childhood trauma and psychotic-like experiences in young adults. Early Interv Psychiatry. (2020) 14:87–96. doi: 10.1111/eip.12829
63. Appiah-Kusi E, Fisher HL, Petros N, Wilson R, Mondelli V, Garety PA, et al. Do cognitive schema mediate the association between childhood trauma and being at ultra-high risk for psychosis? J Psychiatr Res. (2017) 88:89–96. doi: 10.1016/j.jpsychires.2017.01.003
64. de Vos C, Thompson A, Amminger P, Bendall S, de Haan L, Hartmann J, et al. The relationship between childhood trauma and clinical characteristics in ultra-high risk for psychosis youth. Psychosis. (2019) 11:28–41. doi: 10.1080/17522439.2019.1582686
65. Sengutta M, Gaweda Ł, Moritz S, Karow A. The mediating role of borderline personality features in the relationship between childhood trauma and psychotic-like experiences in a sample of help-seeking non-psychotic adolescents and young adults. Eur Psychiatry. (2019) 56:84–90. doi: 10.1016/j.eurpsy.2018.11.009
66. Gibson LE, Reeves LE, Cooper S, Olino TM, Ellman LM. Traumatic life event exposure and psychotic-like experiences: a multiple mediation model of cognitive-based mechanisms. Schizophr Res. (2019) 205:15–22. doi: 10.1016/j.schres.2018.02.005
67. Hardy A, Emsley R, Freeman D, Bebbington P, Garety PA, Kuipers EE, et al. Psychological mechanisms mediating effects between trauma and psychotic symptoms: the role of affect regulation, intrusive trauma memory, beliefs, and depression. Schizophrenia Bull. (2016) 42(suppl_1):S34-S43. doi: 10.1093/schbul/sbv175
68. Gibson LE, Alloy LB, Ellman LM. Trauma and the psychosis spectrum: a review of symptom specificity and explanatory mechanisms. Clin Psychol Rev. (2016) 49:92–105. doi: 10.1016/j.cpr.2016.08.003
69. Schroeder K, Langeland W, Fisher HL, Huber CG, Schafer I. Dissociation in patients with schizophrenia spectrum disorders: what is the role of different types of childhood adversity? Compr Psychiatry. (2016) 68:201–8. doi: 10.1016/j.comppsych.2016.04.019
70. Schäfer I, Fisher HL, Aderhold V, Huber B, Hoffmann-Langer L, Golks D, et al. Dissociative symptoms in patients with schizophrenia: relationships with childhood trauma and psychotic symptoms. Compr Psychiatry. (2012) 53:364–71. doi: 10.1016/j.comppsych.2011.05.010
71. Cole CL, Newman-Taylor K, Kennedy F. Dissociation mediates the relationship between childhood maltreatment and subclinical psychosis. J Trauma Dissociation. (2016) 17:577–92. doi: 10.1080/15299732.2016.1172537
72. Chang WC, Chan TC, Chiu SS, Hui CL, Chan SK, Lee EH, et al. Self-perceived cognitive functioning and its relationship with objective performance in first-episode schizophrenia: the Subjective Cognitive Impairment Scale. Compr Psychiatry. (2015) 56:42–50. doi: 10.1016/j.comppsych.2014.10.004
73. Moritz S, Balzan RP, Bohn F, Veckenstedt R, Kolbeck K, Bierbrodt J, et al. Subjective versus objective cognition: Evidence for poor metacognitive monitoring in schizophrenia. Schizophr Res. (2016) 178:74–9. doi: 10.1016/j.schres.2016.08.021
74. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. (2002) 41(Pt 4):331–47. doi: 10.1348/014466502760387461
75. Aakre JM, Seghers JP, St-Hilaire A, Docherty N. Attributional style in delusional patients: a comparison of remitted paranoid, remitted nonparanoid, and current paranoid patients with nonpsychiatric controls. Schizophr Bull. (2009) 35:994–1002. doi: 10.1093/schbul/sbn033
76. So SH, Tang V, Leung PW. Dimensions of delusions and attribution biases along the continuum of psychosis. PLoS ONE. (2015) 10:e0144558. doi: 10.1371/journal.pone.0144558
77. Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. (2007) 27:425–57. doi: 10.1016/j.cpr.2006.10.004
78. Gaynor K, Ward T, Garety P, Peters E. The role of safety-seeking behaviours in maintaining threat appraisals in psychosis. Behav Res Ther. (2013) 51:75–81. doi: 10.1016/j.brat.2012.10.008
79. Reininghaus U, Kempton MJ, Valmaggia L, Craig TK, Garety P, Onyejiaka A, et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. (2016) 42:712–22. doi: 10.1093/schbul/sbv190
80. Zinchenko A, Al-Amin MM, Alam MM, Mahmud W, Kabir N, Reza HM, et al. Content specificity of attentional bias to threat in post-traumatic stress disorder. J Anxiety Disord. (2017) 50:33–9. doi: 10.1016/j.janxdis.2017.05.006
81. Moritz S, Andreou C, Schneider BC, Wittekind CE, Menon M, Balzan RP, et al. Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin Psychol Rev. (2014) 34:358–66. doi: 10.1016/j.cpr.2014.04.004
82. Eichner C, Berna F. Acceptance and efficacy of metacognitive training (MCT) on positive symptoms and delusions in patients with schizophrenia: a meta-analysis taking into account important moderators. Schizophrenia Bull. (2016) 42:952–62. doi: 10.1093/schbul/sbv225
Keywords: self-disturbances, psychotic-like experiences, adverse life events, trauma, cognitive biases, psychosis risk
Citation: Pionke-Ubych R, Frydecka D, Cechnicki A, Nelson B and Gawęda Ł (2021) The Indirect Effect of Trauma via Cognitive Biases and Self-Disturbances on Psychotic-Like Experiences. Front. Psychiatry 12:611069. doi: 10.3389/fpsyt.2021.611069
Received: 28 September 2020; Accepted: 08 March 2021;
Published: 29 March 2021.
Edited by:
Giuseppe Carrà, University of Milano-Bicocca, ItalyReviewed by:
David Weiss, Maine Medical Center Research Institute, United StatesSarah Tosato, University of Verona, Italy
Copyright © 2021 Pionke-Ubych, Frydecka, Cechnicki, Nelson and Gawęda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Łukasz Gawęda, bC5nYXdlZGFAcHN5Y2gucGFuLnBs
 Renata Pionke-Ubych
Renata Pionke-Ubych Dorota Frydecka
Dorota Frydecka Andrzej Cechnicki3
Andrzej Cechnicki3 Barnaby Nelson
Barnaby Nelson Łukasz Gawęda
Łukasz Gawęda