
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 16 April 2021
Sec. Psychological Therapies
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.602648
This article is part of the Research Topic Contemporary Issues in Defining the Mechanisms of Cognitive Behavior Therapy View all 13 articles
 Esther T. Beierl1*†
Esther T. Beierl1*† Hannah Murray1,2*†
Hannah Murray1,2*† Milan Wiedemann1,2
Milan Wiedemann1,2 Emma Warnock-Parkes1,3
Emma Warnock-Parkes1,3 Jennifer Wild1,2
Jennifer Wild1,2 Richard Stott3,4
Richard Stott3,4 Nick Grey3,4,5
Nick Grey3,4,5 David M. Clark1,2,3
David M. Clark1,2,3 Anke Ehlers1,2,3*
Anke Ehlers1,2,3*Background: Working alliance has been shown to predict outcome of psychological treatments in multiple studies. Conversely, changes in outcome scores have also been found to predict working alliance ratings.
Objective: To assess the temporal relationships between working alliance and outcome in 230 patients receiving trauma-focused cognitive behavioral treatment for posttraumatic stress disorder (PTSD).
Methods: Ratings of working alliance were made by both the patient and therapist after sessions 1, 3, and 5 of a course of Cognitive Therapy for PTSD (CT-PTSD). Autoregressive, cross-lagged panel models were used to examine whether working alliance predicted PTSD symptom severity at the next assessment point and vice versa. Linear regressions tested the relationship between alliance and treatment outcome.
Results: Both patients' and therapists' working alliance ratings after session 1 predicted PTSD symptom scores at the end of treatment, controlling for baseline scores. At each assessment point, higher therapist working alliance was associated with lower PTSD symptoms. Crossed-lagged associations were found for therapist-rated alliance, but not for patient-rated alliance: higher therapists' alliance ratings predicted lower PTSD symptom scores at the next assessment point. Similarly, lower PTSD symptoms predicted higher therapist working alliance ratings at the next assessment point. Ruminative thinking was negatively related to therapists' alliance ratings.
Conclusions: Working alliance at the start of treatment predicted treatment outcome in patients receiving CT-PTSD and may be an important factor in setting the necessary conditions for effective treatment. For therapists, there was a reciprocal relationship between working alliance and PTSD symptom change in their patients during treatment, suggesting that their alliance ratings predicted symptom change, but were also influenced by patients' symptom change.
The working alliance, an important aspect of the therapeutic relationship, defined broadly as the “collaborative and affective bond between the therapist and patient” (1), has long been considered an essential component in the successful delivery of psychological therapy (2). Research findings have generally supported this assumption, with moderate but consistent associations found between alliance ratings and treatment outcome across different therapeutic approaches and disorders (1, 3). However, effect sizes are often in the small to moderate range; Horvath et al. (4) estimated an effect of r = 0.28 based on 190 alliance-outcome relationships reported in 201 studies. This is similar to results reported in previous meta-analyses with estimates of r = 0.26 [24 studies (3)] and r = 0.22 [79 studies (1)]. These associations are found whether the alliance rating is made by the patient, therapist or an observer. Some, but not all, studies have found that patients' alliance ratings are better predictors of outcome than therapists' or observers' (1, 3). Similarly, patients' ratings tend to be more consistent across therapy sessions than therapists' (1), suggesting that patients view the alliance as more stable. This finding requires replication, as few studies include ratings taken from both patient and therapist at multiple time points.
Studies investigating the predictive power of the working alliance have found differing effects depending on the time point at which the alliance is recorded. DeRubeis and Feeley (5) found that observer-rated working alliance measured in an early session of treatment for depression did not predict subsequent symptom change. However, symptom reduction during treatment predicted alliance later in therapy, raising the intriguing possibility that it is improvement in therapy which predicts how positively the alliance is viewed, rather than the other way around. Many studies have averaged alliance ratings taken across therapy (4) obscuring the temporal order, and therefore the causation relationship between alliance and outcome.
Studies which have investigated the temporal relationship between alliance ratings and outcome have produced mixed findings, with some reporting a relationship between alliance and treatment outcome (6–9), while others did not find evidence for a significant association (10, 11). The possibility that symptom change predicts later alliance ratings has also been replicated in several studies (7, 9, 12). A reciprocal relationship, whereby alliance is found to predict symptom improvement and vice versa has also been demonstrated (13, 14).
A number of studies have shown that a good working alliance predicts better treatment outcome in patients with PTSD [see (15) for a review]. However, most of these studies have used a pooled or single point measure of working alliance and have not examined the relationship in the opposite direction (i.e., symptom change influencing alliance). This study aims to assess both directions of the relationship by taking ratings of working alliance at three time points (after sessions 1, 3, and 5) within the treatment arc. This allows a more rigorous examination of the longitudinal relationships between the working alliance and treatment outcome in the early phase of treatment where the greatest changes in symptoms are observed (Ehlers et al., 2021)1. Ratings taken by both patients and therapists will be analyzed in a cohort of patients being treated for posttraumatic stress disorder (PTSD) using Cognitive Therapy for PTSD [CT-PTSD (16)], which is based on (17) cognitive model of PTSD. Working alliance has only been assessed in CT-PTSD in one previous study, where Brady et al. (18) compared high and low treatment responders on an observer-rated version of the Working Alliance Inventory (WAI) and found that the alliance/agreement component of the scale (comprising items on the task and goals of therapy), but not the relationship (or bond) component predicted better outcome. Brady et al. (18) also found that a perseverative thinking style (ruminative thinking) was related to lower working alliance and poorer outcomes. This study will explore these findings with a larger cohort and with patient and therapist ratings, including analysis of sub-scales of the WAI. Given the importance of ruminative thinking identified in Brady et al.'s study, we will also explore its association with working alliance and outcome, by analyzing whether rumination correlates with ratings of working alliance.
There may be reason to argue that the working alliance is particularly important in treatment for PTSD [e.g., (15)]. CT-PTSD, and most other evidence-based treatments, are trauma-focused, relying on the disclosure of intensely personal and painful experiences. Furthermore, avoidance of reminders of the trauma, as well as cognitive and emotional avoidance, are symptoms of PTSD, so a strong therapeutic alliance is needed to encourage patients to overcome their avoidance of talking about or thinking about their trauma. Lastly, many people with PTSD have experiences of interpersonal trauma, interpersonal difficulties and poor trauma-related social support, which have been shown to impede the development of a trusting alliance (19, 20). In this study, the effect on working alliance of interpersonal vs. non-interpersonal traumas will be assessed, and entered as a potential moderator in the relationship between working alliance and outcome.
The study investigated three questions:
1. Prediction of treatment outcome: In line with previous research, we predicted that higher working alliance rated by patients and therapists at the end of session 1 of CT-PTSD would predict better treatment outcome, measured by PTSD symptom severity at the end of treatment, controlled for baseline PTSD severity.
2. Does working alliance drive symptom improvement during treatment or vice versa: As previous research has yielded inconsistent results about the direction of changes in symptoms and working alliance, we investigated whether working alliance predicts symptom improvement a later session and/or vice versa (see Figure 1).
3. Relationship of alliance with ruminative thinking: In addition, we explored the relationship between patients' ruminative thinking style and patient and therapist ratings of working alliance, building on Brady et al.'s (18) results that ruminative thinking is associated with lower agreement/confidence, a component of alliance.
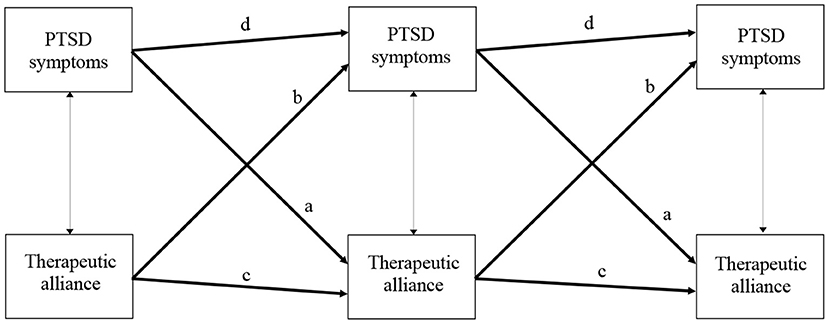
Figure 1. Schematic figure of the hypothesized autoregressive, cross-lagged models. Thick paths with arrows in one direction, such as a (PDSt → WAIt+1; t refers to the respective treatment session and t+1 to 2 sessions later) and b (WAIt → PDSt+1) indicate cross-lagged effects, paths c (WAIt → WAIt+1) and d (PDSt → PDSt+1), indicate autoregressive effects; thin paths with arrows in both directions represent correlations at the same session (PDSt ↔ WAIt).
The current study is a secondary analysis of an effectiveness study of a cohort of 343 consecutive patients treated in routine clinical care (Ehlers et al., 2021)1 with CT-PTSD (16). Patients had experienced a range of traumas, including various forms of interpersonal violence, accidents, and death of others.
Treatment was delivered by clinical psychologists, trainee clinical psychologists, and CBT therapists and trainees with other professional backgrounds (i.e., psychiatry, nursing) with a range of clinical experience. Patients completed PTSD symptom measures weekly before every treatment session (assessing their symptoms over the preceding week) and patients and therapists both completed working alliance measures at the end of sessions 1, 3, and 5. The measure was given to the patient by a research assistant, and not seen by the therapist.
Working alliance scores and the corresponding PTSD symptom severity for the week following sessions 1, 3, and 5 were used for the analysis of the bidirectional relationships, and the interval between assessments was thus two treatment sessions. Data were available for 230 patients for whom at least one patient or one therapist alliance measure and one PTSD symptom measure was available at the respective sessions. Demographics for the study sample of N = 230 are presented in Table 1 and descriptive statistics are presented in Table 2.
Posttraumatic stress disorder symptom data at their final treatment session and at baseline was available for all patients. Exploration of any possible patterns of missing data for the other measures is reported in the preliminary analyses. Patients received on average M = 9.95 (SD = 4.57) treatment sessions in total.
Patients completed the Posttraumatic Diagnostic Scale [PDS (21)], which assesses the severity of the 17 PTSD symptoms specified in the Diagnostic and Statistical Manual of Mental Disorders, Fourth edition [DSM-IV (22)]. Patients rated the extent to which they were bothered by each of the 17 symptoms during the last week (4-point Likert scale) before each treatment session. Cronbach's α at session 1 was 0.88.
Therapeutic working alliance was assessed by the patients and therapists using the short version (23) of the WAI at the end of sessions 1, 3, and 5. The original version of the WAI was developed by Horvath and Greenberg (24) according to Bordin's (25) three components of alliance (tasks, goals, and bond). The short version consists of 12 items (7-point Likert scale), Cronbach's α at session 1 was 0.95 for the patient ratings and 0.96 for the therapist ratings. For the prediction of treatment outcome, sub-scores of the WAI (Task, Goal, Bond) were also calculated to aid interpretation.
Ruminative thinking was measured at session 1 with the 6-item rumination subscale of the Response to Intrusions Scale (26, 27). Cronbach's α for this subscale was 0.86.
Cognitive Therapy for PTSD (CT-PTSD) aims to reduce the patient's sense of current threat by changing problematic meanings of the trauma and its consequences, elaborating and updating the memories of the trauma with information that gives them a less threatening meaning at present, discriminating triggers of intrusive memories, and changing behaviors and cognitive processes that maintain PTSD, such as rumination and safety behaviors.
Core interventions in CT-PTSD are: the collaborative development of an individualized case formulation; reclaiming/rebuilding your life assignments to address the clients' perceived permanent change after trauma by re-engagement with activities and relationships; changing problematic appraisals of the traumas and their sequelae via information, guided discovery and behavioral experiments; updating trauma memories by elaborating and updating the worst moments of the memory; discrimination training with triggers of reexperiencing; a site visit (returning to the scene of the trauma); dropping unhelpful behaviors and cognitive processes; a blueprint summarizing what the client has learned in treatment and planning for any setbacks. Throughout treatment, the work on appraisals is closely interwoven with memory work and is tailored to the case formulation. The specific cognitive therapy techniques depend on the client's pattern of emotions and underlying cognitive themes. For further details of treatment procedures and measures see https://oxcadatresources.com.
Preliminary analyses investigated any effects of PTSD symptom severity or degree of working alliance on the occurrence of missing data (coded as “1”) vs. not missing (coded as “0”) using logistic regressions; unstandardized parameter estimates are reported for these analyses. Welch tests were used to investigate any potential differences between patients who experienced interpersonal (coded as “−0.5”) compared to non-interpersonal traumas (coded as “0.5”) with regards to therapeutic alliance at the beginning of treatment and PTSD symptom severity at baseline and at the end of treatment. Moderation and simple slope analyses using multiple linear regressions investigated any effects between trauma type and alliance ratings on treatment outcome, controlled for baseline severity.
The first research question (prediction of treatment outcome by initial working alliance, controlled for baseline PTSD symptom severity) was tested using multiple linear regressions and we report unstandardized and standardized coefficients.
To investigate the second research question (whether working alliance drives symptom improvement during treatment or vice versa), autoregressive, cross-lagged panel models (28) were specified. As shown in Figure 1, these models tested effects of time for each of the variables (i.e., symptom improvements over time) and any causal effects between both variables (i.e., if working alliance drives improvement in symptoms, we would observe effects of the WAI on symptom scores at two sessions later, i.e., WAI at session 1 on symptoms at session 3, and from WAI in session 3 on symptoms at session 5, paths b in Figure 1; and vice versa if symptom change drives alliance change, paths a in Figure 1). Autoregressions (paths c and d) and cross-lag effects across sessions (paths a and b), and correlations within the same sessions were each set to be equal and freely estimated. In addition to reporting standardized (β) parameter estimates for the main research questions, unstandardized parameter estimates (b) are reported for these panel models (see Table 3). Model fit was evaluated based on the χ2-test statistic (29, 30) and the fit indices CFI (31), RMSEA (32), and SRMR (33). We set the criterion that at least one patient alliance score and one PTSD symptom score at the relevant sessions (either after session 1, 3, or 5) should be available for a patient to be included in the respective panel analysis (n = 185 patients). Similarly, at least one therapist alliance rating and one PTSD symptom score had to be available at the relevant sessions for a patient to be included in the panel model investigating therapist alliance (n = 213 patients). In order to include all patients within those two sub-samples (symptom or alliance data only available at one or two of the three respective sessions) into the respective panel analyses, Robust Maximum Likelihood estimation (34) was used together with Full Information Maximum Likelihood (35).
The third research question (association between working alliance and ruminative thinking) was assessed with Pearson correlations (r).
Data were analyzed using RStudio (36) and the packages lavaan (37), psych (38), sjmisc (39), skimr (40), emmeans (41), and the tidyverse set of packages (42). R code for data analysis can be accessed at ETB's Open Science Framework repository (https://osf.io/4dqyx/).
Whether PTSD symptom data after session 5 were missing or not did not depend on: PTSD symptom severity after session 1, b = −0.01, SE = 0.01, bp = −0.16, p = 0.352; the degree of patients' alliance after session 1, b = −0.01, SE = 0.02, bp = 0.06, p = 0.779; or therapists' alliance after session 1, b = −0.03, SE = 0.02, bp = −0.31, p = 0.091.
Patients who experienced interpersonal traumas rated their therapeutic alliance after session 1 lower than patients who experienced other types of trauma, t(130.04) = −2.80, p = 0.006, whereas there was no significant difference for therapist ratings, t(154.46) = −1.74, p = 0.084. Patients who experienced interpersonal compared to non-interpersonal traumas did not differ in their PTSD symptom severity at baseline, t(170.74) = −1.17, p = 0.243, or at the end of treatment, t(181.70) = 1.95, p = 0.053.
Trauma type (interpersonal vs. non-interpersonal) did not significantly moderate any influence of patients' alliance ratings after session 1 on PTSD symptom severity at the end of treatment, controlled for baseline PTSD symptom severity, b = 0.37, SE = 0.21, β = −0.29, p = 0.077, R2adj = 0.15. However, a simple slope analysis revealed that, for patients who experienced interpersonal traumas, patients' therapeutic alliance after session 1 had a significant effect on reduction of PTSD symptom severity at the end of treatment, controlled for baseline severity, b = −0.31, 95% CI [−0.51, −0.11]. This relationship was not significantly different from zero for patients who experienced non-interpersonal traumas, b = −0.06, 95% CI [−0.29, 0.42].
Trauma type (interpersonal vs. non-interpersonal) also did not significantly moderate any effect of therapist' alliance ratings after session 1 on PTSD symptom severity at the end of treatment, controlled for baseline PTSD symptom severity, therapists' WAI: b = −0.13, SE = 0.17, β = 0.10, p = 0.460, R2adj = 0.27. For both patients with interpersonal and non-interpersonal traumas, the relationship between therapists' working alliance after session 1 had a significant effect on treatment outcome, controlled for baseline severity, interpersonal trauma: b = −0.32, 95% CI [−0.51, 0.14]; non-interpersonal trauma: b = −0.45, 95% CI [−0.74, 0.16].
Both higher patient-reported and therapist-reported working alliance after the first treatment session predicted better outcome, i.e., lower PTSD symptom severity at the final treatment session (controlled for symptom severity at baseline); patients' WAI: b = −0.23, SE = 0.09, β = −0.19, p = 0.008, R2adj = 0.13; therapists' WAI : b = −0.36, SE = 0.08, β = −0.29, p < 0.001, R2adj = 0.28. The results were the same if the three WAI sub-scales were considered independently (patients: Task sub-scale p = 0.018, Goal sub-scale p = 0.004, Bond sub-scale p = 0.018; therapists: Task p < 0.001, Goal p < 0.001, Bond p < 0.001).
Both cross-lagged, autoregressive panel models for the patients' and therapists' alliance ratings fit the data well; model for patients' WAI: = 12.61, p = 0.247, CFI = 0.99, RMSEA [95% CI] = 0.04 [0.00, 0.10], SRMR = 0.05; model for therapists' WAI: = 22.16, p = 0.014, CFI = 0.97, RMSEA [95% CI] = 0.08 [0.04, 0.13], SRMR = 0.06. In the patients' alliance model, 64% of variance was explained in PTSD symptom severity and 60% of variance in patient-reported working alliance after session 5. In the therapists' alliance model, 70% of variance was explained in PTSD symptom severity and 67% of variance in therapist-reported working alliance after session 5.
Patient-reported working alliance and PTSD symptom severity. A higher working alliance reported by patients (see Table 3 and Figure 1) was not associated with lower PTSD symptom severity at the same session, r = −0.08, p = 0.122. Higher alliance scores after sessions 1 or 3 predicted higher alliance at the next assessment (i.e., alliance ratings after the session 1 predicted higher alliance ratings after the session 3 and alliance ratings after the session 3 predicted higher alliance ratings after the session 5; paths c in Figure 1), β = 0.79, p < 0.001. Lower PTSD symptom severity in the week after sessions 1 or 3 predicted lower PTSD symptom severity at the next assessment (i.e., PTSD symptom severity after the session 1 predicted PTSD symptom severity after the session 3 and PTSD symptom severity after the session 3 predicted PTSD symptom severity after the session 5; paths d in Figure 1), β = 0.76, p < 0.001. Thus, preceding levels of patient-reported therapeutic alliance predicted subsequent levels of patients' alliance and preceding levels of PTSD symptom severity predicted subsequent levels of symptom severity.
Taking into account these autoregressive coefficients, patients' self-reported PTSD symptom severity in the week after sessions 1 or 3 did not significantly predict a higher patient-reported alliance at the next assessment (i.e., PTSD symptom severity after the session 1 did not predict alliance after the session 3 and PTSD symptom severity after the session 3 did not predict alliance after the session 5; paths a in Figure 1), β = −0.05, p = 0.173. A higher patient-reported alliance after sessions 1 or 3 also did not predict lower PTSD symptom severity at the next assessment (i.e., alliance after the session 1 did not predict PTSD symptom severity after the session 3 and alliance after the session 3 did not predict symptom severity after the session 5; paths b in Figure 1), β = −0.06, p = 0.142. Thus, preceding levels of patient-reported therapeutic alliance did neither drive subsequent improvement in PTSD symptom severity, nor vice versa.
Therapist-reported working alliance and PTSD symptom severity. A higher working alliance reported by therapists (see Table 3 and Figure 1) was associated with lower PTSD symptom severity after the same session, r = −0.16, p < 0.001. Higher therapist-reported alliance after sessions 1 or 3 predicted higher therapist-reported alliance at the subsequent assessment (i.e., after the session 3 or 5; paths c in Figure 1), β = 0.75, p < 0.001, and lower PTSD symptom severity in the week after session 1 or 3 predicted lower PTSD symptom severity at the successive assessment (i.e., after the session 3 or 5; paths d in Figure 1), β = 0.77, p < 0.001. Thus, similar to the results from the auto-regressions in the patients' alliance model, preceding levels of therapist-reported alliance predicted subsequent levels of therapist-reported alliance and preceding levels of PTSD symptom severity predicted subsequent levels of symptom severity.
Taking into account these auto-regressions, lower PTSD symptom severity in the week after session 1 or 3 significantly predicted higher therapist-reported working alliance at the subsequent assessment (i.e., after the session 3 or 5; paths a in Figure 1), β = −0.12, p = 0.001, and higher therapist-reported alliance after session 1 or 3 predicted significantly lower PTSD symptoms at the subsequent assessment (i.e., after the session 3 or 5; paths b in Figure 1), β = −0.13, p = 0.001. Thus, unlike to the results from the cross-lagged parameters in the patients' alliance model, preceding levels of therapist-reported alliance did drive subsequent PTSD symptom improvement and vice versa.
Therapist alliance ratings in the first session showed a negative relationship with patients' ruminative thinking about the trauma in the same session, r = −0.19, p = 0.015, whereas patient alliance ratings showed a non-significant positive relationship with rumination, r = 0.13, p = 0.131.
This study aimed to assess whether higher working alliance predicted better treatment outcomes in patients receiving CT-PTSD. Higher working alliance at the start of treatment, as rated by both patients and therapists after session 1, was associated with greater symptom improvement, measured by symptom scores at the end of treatment, controlled for baseline scores. This extends the earlier findings of Brady et al. (18), who found that patients reporting a stronger working alliance were more likely to respond well to CT-PTSD, and replicates the findings of numerous other studies which have found a positive association between working alliance and therapy outcome, including in PTSD treatment (15). Although the effect sizes in our study were of small to medium size, they are in line with those of other studies in a range of different disorders (1, 3, 15). These results support the importance of establishing a good working relationship with patients in trauma-focused psychological therapies for PTSD, which is associated with treatment outcomes, although other processes such as reduction of negative appraisals also play a role (43). Higher ratings in the total score and all the three subscales Bond, Goal, and Task were predictive of better outcomes, suggesting that a positive relationship and agreement on mutual goals as well as agreement on concrete steps to be taken in therapy may be important in facilitating change. The alliance ratings were consistently high for both patients and therapists. The collaborative therapeutic style of CT-PTSD may have facilitated a positive working alliance.
Secondly, we aimed to find whether working alliance led to improved symptom scores or vice versa. The results from autoregressive, cross-lagged panel models in this study provided support for a bidirectional relationship between the patients' symptom improvements and working alliance rated by therapists during treatment. A measure of working alliance completed by therapists after sessions 1 and 3 of treatment predicted subsequent symptom severity (i.e., after session 3 and 5; see Figure 1), with a better alliance predicting lower symptoms scores, taking into account the preceding symptom scores. During treatment, therapist-rated alliance after session 3 and 5 was predicted by symptom scores at the preceding time point (i.e., after session 1 and 3; see Figure 1), as well as by preceding alliance ratings. This fits with other studies suggesting a reciprocal relationship between alliance and outcome (13, 14); a positive alliance leads to better therapy outcomes, and better outcomes encourage therapists to view the alliance more positively. The reciprocal relationship found for working alliance contrasts with studies showing a unidirectional relationship between changes in negative cognitions about the trauma and symptom change in the treatment of PTSD. Cognitive change preceded symptom change in studies of CT-PTSD (43) and other trauma-focused cognitive behavioral treatments (44), and a reverse relationship was found in only a small minority of studies. Taken together, these findings suggest that cognitive change drives symptom change, but a good working alliance both facilitates, and is a result of, symptom change.
However, despite the overall relationship between patient-rated working alliance at the session 1 and improvement of PTSD symptoms during therapy, no significant cross-lagged associations between patients' alliance and symptoms were found in the early sessions of therapy when taking into account the significant effects of preceding symptom scores on subsequent symptom levels, and preceding alliance scores on subsequent alliance levels. Preceding levels of patients' alliance (i.e., after sessions 1 or 3; see Figure 1) did neither predict subsequent levels of PTSD symptom severity (i.e., after session 3 or 5; see Figure 1), nor vice versa (PTSD symptom scores in the week after session 1 or 3 did not predict the working alliance at the subsequent assessment, i.e., after session 3 or 5; see Figure 1), controlled for the respective auto-correlations of symptoms scores and alliance scores over time. Thus, the results for patient-rated alliance were mixed, which is in line with the literature. Some studies have shown that working alliance rated by PTSD patients is predictive of treatment outcomes [e.g., (45, 46)], but Forbes et al. (47) and van Minnen et al. (48) reported no association between working alliance and outcome in their PTSD samples.
One potential reason for this discrepancy is methodological. In contrast to earlier studies, the cross-lagged analyses used in this study controlled for autocorrelations within each measure, which were high. The sample that provided patient alliance ratings was somewhat smaller than that for therapist ratings, restricting power. There was also some indication of restricted variance in patient alliance ratings in the later sessions and ceiling effects, and is in keeping with previous studies which have found that patient ratings of alliance tend to be fairly stable during treatment (1). Indeed, the patients' ratings of alliance in this study were consistently fairly high after all the three sessions 1, 3, and 5. It may be that their early first impressions of the therapeutic alliance, based on a first session of therapy that was engaging and collaborative, changed very little as treatment progressed and did not affect, nor was affected by, changes in their symptoms. Beck (49) wrote that a good therapeutic alliance is “necessary but not sufficient” to effect change in cognitive therapy. It may be that the “good enough” working alliance for most of the patients in this study was sufficient for engagement with treatment, but that the major influence on symptom change did not lie in their perception of the therapeutic relationship, but in the tasks and techniques used in treatment to produce cognitive change. This could suggest that therapists should prioritize establishing a solid working alliance in early sessions as a foundation for other aspects of treatment.
The reason for the discrepancy between the cross-lagged associations of PTSD symptoms of therapist and patient alliance ratings is unclear. Therapists do have more experience in the process of therapy than patients, and may be more likely to pick up on aspects of the alliance that will prove beneficial for future outcomes. Other studies, however, have found the opposite effect, with patients' ratings of alliance more predictive of outcome than therapists' [e.g., (1, 3, 50)]. Due to the methodological properties of the autoregressive, cross-lagged panel models (51) it cannot be ruled out that the alliance ratings partly reflected some trait-like stability. This might have led to the lagged parameters not only representing within-person relationships over time, but also between-person processes. This methodological problem may have been more pronounced for patients, some of whom had PTSD-related problems trusting other people in general which may have influenced their ratings. Indeed, a history of interpersonal trauma was related to lower initial ratings of the therapeutic alliance, which is in keeping with other studies that have suggested that people with a history of interpersonal trauma may particularly struggle to form a strong therapeutic alliance [e.g., (52)], but trauma type did not moderate the relationship between the working alliance and treatment outcome. However, the finding from the simple slopes analysis did indicate a potential effect of interpersonal trauma on the alliance-outcome relationship. This relationship requires further investigation.
Finally, the study aimed to explore the relationship between ruminative thinking and working alliance, following Brady et al.'s (18) finding that observer-rated ruminative thinking was associated with lower working alliance and predicted poorer outcomes in CT-PTSD. In this study, negative correlations between patient-rated ruminative thinking and therapist ratings of working alliance were found, but a non-significant positive correlation was found when patients rated the alliance. This indicates that therapists, but not patients, see rumination as an unhelpful strategy and thus rate alliance lower when this happens. The differential effect of ruminative thinking on patients' and therapists' rating may thus have contributed to the different pattern of results for the cross-lagged relationship with symptom reduction, as therapists are more effectively spotting that rumination is an unhelpful strategy, linked to poorer treatment outcome. Potential clinical implications of this finding are that therapists should address ruminative thinking in a manner which preserves the working alliance, such as collaboratively establishing the effect it has on the maintenance of PTSD symptoms.
A strength of this study was that it was drawn from a consecutive cohort of PTSD patients with a wide range of traumas and ethnic backgrounds who received an evidence-based psychological treatment in routine care and that the direction of the relationship between working alliance and symptom change during treatment could be investigated by repeated assessments.
Methodological limitations of the study include ceiling effects in the alliance measure that may have potentially masked effects, as a possible restriction in variance restricts magnitude of correlations and correlation-based parameters. The sample was of a similar size to other studies in this area, but would benefit from replication with a larger sample due to more complex analysis and estimation methods used in this study compared to previous studies. Another possible limitation is that the time lag between the therapy sessions was not always exactly 1 week, which may have led to some noise in the parameter estimates (53).
Despite these limitations, the study provides further insight into the relationship between working alliance and treatment outcome amongst patients receiving treatment for PTSD. It highlights the importance of a strong working alliance at the very start of treatment, possibly particularly with patients who have experienced interpersonal trauma and in addressing rumination. The mixed findings also indicate the importance of using ratings from multiple raters (therapist and patient) at multiple time points in treatment to fully understand the relationship between alliance and outcome in future studies.
The datasets presented in this article are not readily available because, we did not obtain consent to share patient data at the time of data collection but share the data analysis code and details of results. Requests to access the datasets should be directed to YW5rZS5laGxlcnNAcHN5Lm94LmFjLnVr.
The studies involving human participants were reviewed and approved by King's College and South London and Maudsley Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
EB wrote and revised manuscript, designed statistical analysis plan, and conducted statistical data analysis. HM wrote and revised manuscript, involved in literature review, contributed to treatment, data collection, and data analysis plan. MW involved in data management, contributed to data analysis plan, and critical revision of write-up. EW-P, JW, and RS contributed to treatment and clinical supervision, data collection, and critical revision of write-up. NG was the co-director of clinical treatment and clinical supervision, contributed to data collection, and critical revision of write-up. DC was the co-grant holder and contributed to critical revision of write-up. AE was the primary investigator of study and grant holder, designed and supervised data collection, clinical supervision, contributed to write-up, and critical revision. All authors contributed to the article and approved the submitted version.
This study was funded by Wellcome Trust grants 069777 and to 200796 to AE and DC, the Oxford Health NIHR Biomedical Research Centre and a Mental Health Research UK studentship awarded to AE and MW. It was supported by the NIHR South London and Maudsley Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The funders were not involved in planning or analyzing the study. Open access fees are funded through a block grant to Oxford University.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would like to thank Dr. David Veale for his support and Kelly Archer, Anna Bevan, Inga Böllinghaus, Georgina Bremner, Linda Horrell, Judith Kalthoff, Birgit Kleim, Ruth Morgan, Jennifer Readings, Catherine Seaman, Elizabeth Woodward, and Yvette Yeboah for their help with data collection and entry. We would also like to thank Margaret Dakin, Sue Helen, and Julie Twomey for their administrative support.
1. ^Ehlers A, Wild J, Warnock-Parkes E, Stott R, Grey N, Cullen D, et al. Effectiveness of cognitive therapy in routine clinical care: Second phase implementation. (2021).
1. Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J Consult Clin Psychol. (2000) 68:438–50. doi: 10.1037/0022-006X.68.3.438
3. Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: a meta-analysis. J Couns Psychol. (1991) 38:139–49. doi: 10.1037/0022-0167.38.2.139
4. Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. (2011) 48:9–16. doi: 10.1037/a0022186
5. DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognit Ther Res. (1990) 14:469–82. doi: 10.1007/BF01172968
6. Anker MG, Owen J, Duncan BL, Sparks JA. The alliance in couple therapy: partner influence, early change, and alliance patterns in a naturalistic sample. J Consult Clin Psychol. (2010) 78:635–45. doi: 10.1037/a0020051
7. Crits-Christoph P, Gibbons MBC, Hamilton J, Ring-Kurtz S, Gallop R. The dependability of alliance assessments: the alliance–outcome correlation is larger than you might think. J Consult Clin Psychol. (2011) 79:267–78. doi: 10.1037/a0023668
8. Schwartz C, Hilbert S, Schlegl S, Diedrich A, Voderholzer U. Common change factors and mediation of the alliance–outcome link during treatment of depression. J Consult Clin Psychol. (2018) 86:584–92. doi: 10.1037/ccp0000302
9. Webb CA, DeRubeis RJ, Amsterdam JD, Shelton RC, Hollon SD, Dimidjian S. Two aspects of the therapeutic alliance: differential relations with depressive symptom change. J Consult Clin Psychol. (2011) 79:279–83. doi: 10.1037/a0023252
10. Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. J Consult Clin Psychol. (1999) 67:578–82. doi: 10.1037/0022-006X.67.4.578
11. Strunk DR, Brotman MA, DeRubeis RJ. The process of change in cognitive therapy for depression: predictors of early inter-session symptom gains. Behav Res Ther. (2010) 48:599–606. doi: 10.1016/j.brat.2010.03.011
12. Barber JP, Connolly MB, Crits-Christoph P, Gladis L, Siqueland L. Alliance predicts patients' outcome beyond in-treatment change in symptoms. J Consult Clin Psychol. (2000) 68:1027. doi: 10.1037/0022-006X.68.6.1027
13. Marker CD, Comer JS, Abramova V, Kendall PC. The reciprocal relationship between alliance and symptom improvement across the treatment of childhood anxiety. J Clin Child Adolesc Psychol. (2013) 42:22–33. doi: 10.1080/15374416.2012.723261
14. Xu H, Tracey TJ. Reciprocal influence model of working alliance and therapeutic outcome over individual therapy course. J Couns Psychol. (2015) 62:351–9. doi: 10.1037/cou0000089
15. Ellis AE, Simiola V, Brown L, Courtois C, Cook JM. The role of evidence-based therapy relationships on treatment outcome for adults with trauma: a systematic review. J Trauma Dissociation. (2018) 19:185–213. doi: 10.1080/15299732.2017.1329771
16. Ehlers A, Clark DM, Hackmann A, McManus F, Fennell MJV. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behav Res Ther. (2005) 43:413–31. doi: 10.1016/j.brat.2004.03.006
17. Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. (2000) 38:319–45. doi: 10.1016/S0005-7967(99)00123-0
18. Brady F, Warnock-Parkes E, Barker C, Ehlers A. Early in-session predictors of response to trauma-focused cognitive therapy for posttraumatic stress disorder. Behav Res Ther. (2015) 75:40–7. doi: 10.1016/j.brat.2015.10.001
19. Keller SM, Zoellner LA, Feeny NC. Understanding factors associated with early therapeutic alliance in PTSD treatment: adherence, childhood sexual abuse history, and social support. J Consult Clin Psychol. (2010) 78:974–9. doi: 10.1037/a0020758
20. Lawson DM, Skidmore ST, Akay-Sullivan S. The influence of trauma symptoms on the therapeutic alliance across treatment. J Counsel Dev. (2020) 98:29–40. doi: 10.1002/jcad.12297
21. Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychol Assess. (1997) 9:445–51. doi: 10.1037/1040-3590.9.4.445
22. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth edition, DSM-IV. Washington, DC: American Psychiatric Association (2000).
23. Tracey TJ, Kokotovic AM. Factor structure of the working alliance inventory. Psychol Assess. (1989) 1:207–10. doi: 10.1037/1040-3590.1.3.207
24. Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. J Couns Psychol. (1989) 36:223–33. doi: 10.1037/0022-0167.36.2.223
25. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory Res Pract. (1979) 16:252–60. doi: 10.1037/h0085885
26. Clohessy S, Ehlers A. PTSD symptoms, response to intrusive memories, and coping in ambulance service workers. Br J Clin Psychol. (1999) 38:251–65. doi: 10.1348/014466599162836
27. Murray J, Ehlers A, Mayou RA. Dissociation and posttraumatic stress disorder: two prospective studies of road traffic accident victims. Br J Psychiatry. (2002) 180:363–8. doi: 10.1192/bjp.180.4.363
28. Bollen KA, Curran PJ. Latent curve models: A structural equation approach. Hoboken, NJ: Wiley (2006). doi: 10.1002/0471746096
29. Bollen KA. Structural Equations with Latent Variables. New York, NY: Wiley. doi: 10.1002/9781118619179
30. Jöreskog KG. A general approach to confirmatory maximum likelihood factor analysis. Psychometrika. (1969) 34:183–202. doi: 10.1007/BF02289343
31. Bentler PM. Comparative fit indexes in structural models. Psychol Bull. (1990) 107:238–46. doi: 10.1037/0033-2909.107.2.238
32. Steiger JH, Lind JC. Statistically based tests for the number of common factors. Paper presented at the Annual Meeting of the Psychometric Society. Iowa City, IA. (1980).
33. Jöreskog KG, Sörbom D. Analysis of Linear Structural Relationships by Maximum Likelihood and Least Squares Methods (Report No. 81-88). Sweden: Department of Statistics, University of Uppsala (1981).
35. Arbuckle LL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced Structural Equation Modeling. Mahwah, NJ: Lawrence Erlbaum. (1996). p. 243–77.
36. RStudio Team. RStudio: Integrated development for R. Boston, MA: RStudio, Inc. RStudio version 1.4.1103 (2021). doi: 10.1007/978-3-662-62518-7_1
37. Rosseel Y. lavaan: An R package for structural equation modeling. J Stat Software. (2012) 48:1–36. R package version 0.6-7. doi: 10.18637/jss.v048.i02
38. Revelle W. psych: Procedures for Personality and Psychological Research. Northwestern University, Evanston, IL. (2020). R package version 2.0.12. Available online at: https://CRAN.R-project.org/package=psych
39. Lüdecke D. sjmisc: Data and variable transformation functions. J Open Source Software. (2018) 3:754. R package version 2.8.6. doi: 10.21105/joss.00754
40. Waring E, Quinn M, McNamara A, Arino de la Rubia E, Zhu H, Ellis S. skimr: Compact and Flexible Summaries of Data. (2020). R package version 2.1.2. Available online at: https://CRAN.R-project.org/package=skimr
41. Lenth RV. emmeans: Estimated Marginal Means, aka Least-Squares Means. (2021). R package version 1.5.4. Available online at: https://CRAN.R-project.org/package=emmeans.
42. Wickham H, Averick M, Bryan J, Chang W, D'Agostino McGowan L, Francois R, et al. Welcome to the tidyverse. J Open Source Software(2019) 4:1686. R package version 1.3.0. doi: 10.21105/joss.01686
43. Kleim B, Grey N, Hackmann A, Nussbeck F, Wild J, Stott R, et al. Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. J Consult Clin Psychol. (2013) 81:383–93. doi: 10.1037/a0031290
44. Brown LA, Belli GM, Asnaani A, Foa EB. A review of the role of negative cognitions about oneself, others, and the world in the treatment of PTSD. Cognit Ther Res. (2019) 43:143–73. doi: 10.1007/s10608-018-9938-1
45. Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. J Consult Clin Psychol. (2002) 70:1067–74. doi: 10.1037/0022-006X.70.5.1067
46. Ruglass LM, Miele GM, Hien DA, Campbell AN, Hu MC, Caldeira N, et al. Helping alliance, retention, and treatment outcomes: a secondary analysis from the NIDA clinical trials network women and trauma study. Subst Use Misuse. (2012) 47:695–707. doi: 10.3109/10826084.2012.659789
47. Forbes D, Parslow R, Creamer M, Allen N, McHugh T, Hopwood M. Mechanisms of anger and treatment outcome in combat veterans with posttraumatic stress disorder. J Trauma Stress. (2008) 21:142–9 doi: 10.1002/jts.20315
48. Van Minnen A, Arntz A, Keijsers GPJ. Prolonged exposure in patients with chronic PTSD: predictors of treatment outcome and dropout. Behav Res Ther. (2002) 40:439–57. doi: 10.1016/S0005-7967(01)00024-9
50. Cronin E, Brand BL, Mattanah JF. The impact of the therapeutic alliance on treatment outcome in patients with dissociative disorders. Eur J Psychotraumatol. (2014) 5:22676. doi: 10.3402/ejpt.v5.22676
51. Hamaker EL, Kuiper RM, Grasman RP. A critique of the cross-lagged panel model. Psychol Methods. (2015) 20:102–16. doi: 10.1037/a0038889
52. Doukas A, D'Andrea W, Doran J, Pole N. Psychophysiological predictors of working alliance among treatment-seeking women with complex trauma exposure. J Trauma Stress. (2014) 27:672–9. doi: 10.1002/jts.21968
Keywords: posttraumatic stress disorder, cognitive therapy, working alliance, cross-lagged associations, treatment outcome
Citation: Beierl ET, Murray H, Wiedemann M, Warnock-Parkes E, Wild J, Stott R, Grey N, Clark DM and Ehlers A (2021) The Relationship Between Working Alliance and Symptom Improvement in Cognitive Therapy for Posttraumatic Stress Disorder. Front. Psychiatry 12:602648. doi: 10.3389/fpsyt.2021.602648
Received: 03 September 2020; Accepted: 18 March 2021;
Published: 16 April 2021.
Edited by:
Nikolaos Kazantzis, Cognitive Behavior Therapy Research Unit, AustraliaReviewed by:
Jonaimontas, Vilnius University, LithuaniaCopyright © 2021 Beierl, Murray, Wiedemann, Warnock-Parkes, Wild, Stott, Grey, Clark and Ehlers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Esther T. Beierl, ZXN0aGVyLmJlaWVybEBwc3kub3guYWMudWs=; Hannah Murray, aGFubmFoLm11cnJheUBwc3kub3guYWMudWs=; Anke Ehlers, YW5rZS5laGxlcnNAcHN5Lm94LmFjLnVr
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.