
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 23 December 2021
Sec. Public Mental Health
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.567446
This article is part of the Research Topic Coronavirus Disease (COVID-19): Psychological, Behavioral, Interpersonal Effects, and Clinical Implications for Health Systems View all 204 articles
 Xiaoxiao Sun1†
Xiaoxiao Sun1† Fei Xie1†
Fei Xie1† Beijing Chen1
Beijing Chen1 Peixia Shi1
Peixia Shi1 Sitong Shen1
Sitong Shen1 Zhaohua Chen1
Zhaohua Chen1 Yuan Yuan2
Yuan Yuan2 Mengjia Zhang1
Mengjia Zhang1 Xuemei Qin1
Xuemei Qin1 Yingzhe Liu3
Yingzhe Liu3 Yuan Wang4
Yuan Wang4 Qin Dai1*
Qin Dai1*Objective: The outbreak of coronavirus disease 2019 (COVID-19), declared as a major public health emergency, has had profound effects on public mental health especially emotional status. Due to professional requirements, medical staff are at a higher risk of infection, which might induce stronger negative emotions. This study aims to reveal the emotional status of Chinese frontline medical staff in the early epidemic period to better maintain their mental health, and provide adequate psychological support for them.
Methods: A national online survey was carried out in China at the early stage of the COVID-19 epidemic. In total, 3025 Chinese frontline medical staff took part in this investigation which utilized a general information questionnaire, the Emotion Regulation Questionnaire (ERQ), and the Berkeley Expressivity Questionnaire (BEQ).
Results: At the early stage of COVID-19, anxiety was the most common negative emotion of Chinese medical staff, followed by sadness, fear, and anger, mainly at a mild degree, which declined gradually over time. Nurses had the highest level of negative emotions compared with doctors and other healthcare workers. Women experienced more fear than men, younger and unmarried medical staff had more anxiety and fear compared with elders and married ones. Risk perception and emotional expressivity increased negative emotions, cognitive reappraisal reduced negative emotions, while negative emotions led to more avoidant behavior and more physical health disturbances, in which negative emotions mediated the effect of risk perception on avoidant behavior tendency in the model test.
Conclusion: Chinese frontline medical staff experienced a mild level of negative emotions at the early stage of COVID-19, which decreased gradually over time. The findings suggest that during the epidemic, nurses' mental health should be extensively attended to, as well as women, younger, and unmarried medical staff. To better ensure their mental health, reducing risk perception and improving cognitive reappraisal might be important, which are potentially valuable to form targeted psychological interventions and emotional guidance under crisis in the future.
Coronavirus disease 2019 (COVID-19), similar to SARS in 2003, has been declared as a major public health emergency (1), and has had a profound influence on personal mental health (2, 3). Up to May 4, 2020, there were 3,349,786 confirmed cases and 238,628 deaths because of COVID-19 worldwide (4). Millions of medical staff worked on the frontline to fight against the disease, making them face a high risk of infection (5, 6) and huge mental pressure (7, 8). Thousands of Chinese medical personnel combated with COVID-19 on the frontline, of whom over 3,000 medical staff were infected with the virus as of February 20, 2020 (8). Therefore, the COVID-19 epidemic can be regarded as a crisis event for the general population especially for those frontline medical staff.
According to Myer and Conte's (9) triage assessment system (TAS) for crisis intervention, reactions to crisis events are divided into three domains: affective or emotional, behavioral, and cognitive. The TAS model offers us an understanding about the type of reactions people experience as well as the intensity of these reactions in crisis. TAS can also provide a quick, accurate, and easy-to-use method that is directly usable in the intervention process and can monitor individuals' progress during the crisis intervention process. Thus, the TAS model is not only a valuable tool in the assessment of individual reactions in crisis but also a guide in the identification of the complex interaction among the three domains (9).
The first and most significant response under crisis is emotional response. Fear, anxiety, anger, and sadness are universal negative emotions among medical staff when facing sudden and arduous public health issues (10, 11). Studies revealed (10) that fear was a prominent emotional response among healthcare workers, and 1.4 times that compared with non-clinical staff (12). Taking the SARS epidemic as an example, frontline medical personnel were more likely to experience stronger negative emotions, such as the fear of being infected themselves or infecting their family members and anxiety of uncertainty (10, 13, 14). Additionally, anxiety was another common negative emotion among medical personnel (15). Medical staff working in emergency, ICU, and respiratory departments were two times more likely to suffer from anxiety (12). As to the gender difference, women had more anxiety compared with men (16). Being female, having frequent contact with patients, inadequate protective supplies, and being overloaded work were all related to the high level of anxiety (17, 18), which might contribute to emotional exhaustion (19). Besides, healthcare workers also experienced anger and sadness during SARS (13). A variety of factors might increase substantial psychological stress on medical staff (11, 13), such as shortage of protective supplies, direct contact with patients, and overloaded work, which might increase the infection rate of medical staff consequently (17, 20, 21). Although there exist studies on the negative emotions of medical staff during past epidemics, previous studies did not observe the status and sources of negative emotions of medical staff in detail, which is guaranteed to better maintain their mental health, as well as to provide adequate psychological support for them.
Nevertheless, different medical professionals may have different negative emotional responses. Studies reported (22) that nurses were more worried compared with doctors during the A/H1N1 influenza pandemic. The overall level of distress of nurses was significantly higher than that of other medical staff (23). During the COVID-19 epidemic, nurses reported experiencing more severe mental health symptoms than those of physicians (16). However, the emotional status and trend of negative emotions at the early stage of the epidemic were not systematically investigated, which was potentially important to develop more targeted psychological support toward different types of medical staff, since they were equally treated in the current psychological intervention (23).
In terms of emotional states, personal emotions fluctuate instead of sustaining (24). As Gross (24) pointed out, an individual's emotions unfold over seconds to minutes, which suggests the dynamic changes of emotions as time goes by. The latest cross-sectional survey (12) on the COVID-19 epidemic investigating 2042 medical staff from Fujian Provincial Hospital in China revealed that about 70.6% of the medical staff suffered from a moderate to severe level of fear, and 22.6% had a mild to moderate level of anxiety. However, this investigation was carried out at very early stage of this epidemic (January 24, 2020), and did not continue to monitor the emotion change of medical staff. The trend of negative emotions of Chinese medical staff is needed to explore timely and targeted psychological support in different periods of COVID-19. In previous epidemics, studies found (19, 25) that the fear and anxiety of medical staff appeared immediately and then decreased at the early stage of the epidemic, indicating that the early epidemic stage would be a critical period to monitor the negative emotional responses of frontline medical staff, as well as to provide timely psychological assistance. We thus supposed that negative emotions might be continuously decreasing from the initial phase of the epidemic.
So far, only the negative emotion reaction under crisis has been discussed, while according to Myer's TAS model, cognitive and behavioral reactions of frontline medical staff also need to be paid attention to. Facing the COVID-19 crisis event, a full understanding of the negative emotional responses and its influential factors from cognitive and behavioral domains might help to provide comprehensive information to formulate effective psychological interventions in future.
Studies reported (26) that risk perception in the cognitive domain might induce negative emotion. One study showed (27) that the level of fear elevated when people perceived a higher risk perception of SARS. Kushnir et al. (28) also reported that people tended to overestimate the risk of events that rarely happened while eliciting intense fears. Moreover, irrational risk perception would bring unnecessary anxiety and panic in turn (26). According to the Health Belief Model (29), risk perception could also influence individual behaviors. The high risk perception could affect medical staff's willingness to care for patients, especially when they were afraid of infecting their family members (30). Therefore, it could be assumed that the risk perception might influence the negative emotions and behavior of frontline medical staff under this epidemic.
Emotions might change behavior pattern. In terms of the relationship between negative emotion and behavioral reaction, studies revealed that fear was linked with avoidant behavior for protecting individuals from dangers (31, 32). For example, some medical staff were reluctant to work or determined to resign due to the fear of being infected or infecting their family members during the SARS epidemic (17, 33). The results suggested that negative emotions might promote the avoidant behavior tendency of medical personnel in the present epidemic, which need further evidence.
Stress would not only induce negative emotions, but also activate physical response. As mentioned above, the high level of negative emotion might cause physical function disturbance of frontline medical staff during an epidemic, such as headaches (7), anorexia (10), sleep disorders (34), and pain (35). Indeed, medical staff experienced more physical symptoms such as burnout, insomnia, and anorexia (10, 11, 13). However, the influence of negative emotions on the physical health of medical staff remains unknown under COVID-19, and we supposed that focusing on the physical response of frontline medical staff could broaden Myer's TAS theoretical system and reflect individual response toward COVID-19 more systematically.
Moreover, emotion regulation defined as the attempt to affect the way that one experiences or expresses emotions (24), can be used to help frontline medical staff deal with emotion reactions under the COVID-19 crisis. Gross and John (36) proposed that cognitive reappraisal and expressive suppression were two common emotion regulation strategies. Cognitive reappraisal, defined as the attempt to reinterpret the situation eliciting the emotion in the manner of changing its emotional impact (37, 38), could reduce negative emotions as reported (37, 39). While expressive suppression is defined as the attempt to hide, suppress, or reduce the ongoing emotion-expressive behavior (40). Cognitive reappraisal is related to healthier emotion and better wellbeing compared with expressive suppression (41). Additionally, emotional expressivity, which means expressing emotion through verbal, non-verbal, and physiological channels (42), also has an influence on negative emotions besides cognitive reappraisal and expressive suppression. Gross also pointed out that emotional expressivity as an opposite regulation strategy of expressivity suppression, might have a unique influence on emotions, correlating with negative emotion and mental health problems (43). Importantly, a study showed (44) that only expressive suppression significantly modulated fear under an epidemic, while other emotional regulation strategies did not, which suggested that different types of emotional regulation had different effects on fear emotion. However, previous research usually observe the effect of emotion regulation strategies on emotion in total, while the effect of different types of emotional regulation strategies on different types of emotions under crisis was not systematically revealed.
In summary, our present study aims to investigate the emotional status of Chinese frontline medical staff at the early period of the COVID- 19 epidemic, and further explore its trend and influential pathway. Our hypotheses were:
1) Chinese frontline medical staff might have a certain degree of negative emotions at the early stage of the COVID- 19 epidemic;
2) Nurses might have a higher level of negative emotions compared with other medical professionals;
3) At the early stage of the COVID- 19 epidemic, negative emotions of the Chinese frontline medical staff might decrease significantly;
4) Risk perception and emotion regulation might influence negative emotion;
5) Negative emotion might have a potential effect on avoidant behavior tendency and physical health;
6) Negative emotion might have a mediation effect between risk perception and avoidant behavior tendency and physical health.
A cross-sectional online survey was used to assess the emotional responses of Chinese frontline medical staff with a convenience sampling method. Doctors, nurses, and other medical staff, who cared for COVID-19 patients in the designated hospitals during this epidemic were eligible for this online national investigation from January 27 to February 11, 2020. Participants answered the questionnaire through an online link based on their personal will. A total of 4,100 medical staff responded, and 3,025 questionnaires were completed, which were from all provinces in China. Incomplete and halfheartedly filled in questionnaires were excluded from formal analysis. As depicted in Supplementary Table 1, there were 1,916 (63.3%) women and 1,109 (36.7%) men, aged between 20 and 65 years old. Among them, 1,237 (40.9%) were doctors, 1,371 (45.3%) were nurses, and 417 (13.8%) were other medical staff. In addition, 1,852 (61.2%) were married, 1,067 (35.3%) were unmarried, and 106 (3.5%) were divorced or widowed. Over 96.6% of the participants had college and postgraduate or higher educational levels. The participants covered all provincial administrative regions in China, which were divided into six groups of provinces according to the number of confirmed cases (above 10,000, 1,000–9,999, 500–999, 100–499, 10–99, and 1–9).
General information: Basic information about demographic characteristics, including gender, age, degree of education, marital status, and city (number of confirmed cases above 10,000, 1,000–9,999, 500–999, 100–499, 10–99, and 1–9) were collected.
Negative emotions: To collect the degree of negative emotions, four questions were designed with five options (none, mild, moderate, severe, extremely severe/unbearable): How fearful (anxious, angry, sad) do you feel today? Exploratory factor analysis (EFA, principal axis factoring (PAF)) and reliability analysis were carried out and found that the KMO of this scale was 0.797, which accounted for as much as 64.931% of the total variance; the Cronbach's alpha was 0.82. Cognitive sources for negative emotions are listed in the Supplementary Materials.
Risk perception: To observe people's risk perception during the epidemic, three questions were designed (yes or no): “This is a severe outbreak,” “Epidemic is close to me,” “I am in danger.” Exploratory factor analysis [EFA, principal axis factoring (PAF)] and reliability analysis were carried out and found that the KMO of this scale was 0.622, which accounted for as much as 57.94% of the total variance; the Cronbach's alpha was 0.635.
Cognitive sources of public anxiety: To explore possible sources of public anxiety, 12 questions were investigated (yes or no): Do you feel anxious about the new confirmed cases, possible infection without isolation, death number, shortage of protective supplies, new suspected cases, possible infection without protection, new foci, insufficient cooperation of patients, insufficient protection, being isolated due to the epidemic, insufficient duty of medical staff, and others?
Cognitive sources of public anger: To explore possible sources of public anger, 10 questions were surveyed (yes or no): Do you feel anger about irresponsible rumors, possible infection without isolation, possible infection without protection, insufficient cooperation of patients, shortage of protective supplies, insufficient attention of unit, insufficient duty of medical staff, unsupported by families, being isolated due to the epidemic, and others?
Cognitive sources of public sadness: To explore possible sources of public sadness, eight questions were investigated (yes or no): Do you feel sadness about innocent people, shortage of protective supplies, helpless patients, exhausted medical staff, being infected by the virus, being isolated due to the epidemic, unsupported by families, and others?
Cognitive sources of public fear: To explore possible sources of public fear, 14 questions were investigated (yes or no): Do you fear being infected by the virus, infection of families, possible infection without isolation, new confirmed cases, death after infection, shortage of protective supplies, possible infection without protection, death number, disrupted work or study after the epidemic, new foci, new suspected cases, insufficient cooperation of patients, being isolated due to the epidemic, and others?
Avoidant behavior tendency: To observe potential avoidant behavior tendency during the epidemic, three questions were designed (yes or no): “I am intending to run away if possible,” “To escape isolation, I might not go to hospital if I am a suspected case,” “To protect myself and families, I might quit the job if I am a medical staff member.” The KMO of this scale was 0.687, which accounted for as much as 77.88% of the total variance; the Cronbach's alpha was 0.857.
Disturbed physical function: To observe potential disturbed physical health during the epidemic, three questions were designed (yes or no): “Within the past week, I cannot keep my regular schedule as usual,” “Within the past week, I cannot eat as well as usual,” “Within the past week, I cannot sleep as well as usual.” The KMO of this scale was 0.602, which accounted for as much as 56.20% of the total variance; the Cronbach's alpha was 0.607.
Emotional regulation strategies: The Emotion Regulation Questionnaire (ERQ) with 10 items was used in this investigation, which was designed by Gross and John (36) and translated into Chinese in 2007 (45). High scores indicate higher cognitive reappraisal and expressive suppression, respectively. The Cronbach's alpha coefficient was 0.827 for cognitive reappraisal and 0.714 for expressive suppression in this study.
The Berkeley Expressivity Questionnaire (BEQ) (43) was also used to observe personal emotional expression, which is comprised of 16 items and 3 subscales: impulse strength, negative expressivity, and positive expressivity. The Cronbach's alpha coefficient was 0.834 in this study.
Questions were designed and edited as an online questionnaire, which was approved by the Human Research Ethics Committee of the Army Medical University of China and Wenjuanxing online platform (www.wjx.top), a platform providing functions equivalent to Amazon Mechanical Turk. From January 27 to February 11, 2020,participants answered the questionnaire through an online link with their personal cellphone or computer based on his/her individual will; there was no adverse consequence if they refused or did not have time to fill in the online questionnaire. Each person took about 10–15 min to complete the questionnaire after they signed the electronic version of the informed consent form. All participants could get a professional psychological consultation and aid via the hotline at the bottom of the electronic questionnaire.
An independent t-test and one way ANOVA were conducted to observe the demographic characteristics of negative emotions. Independent t-test analysis was also carried out to observe the influence of risk perception on negative emotions. The Chi-squared test was carried out to observe the effect of negative emotions on avoidant behavior tendency and disturbed physical function. Pearson correlation was carried out to observe the correlation between negative emotions, risk perception, emotional regulation, avoidant behavior, and disturbed physical function. A structural equation model was carried out with AMOS 24.0 to test the interaction between variables based on the TAS theory model.
To observe the negative emotional features of frontline medical staff, an independent two-sample t-test and one-way ANOVA analysis were conducted, which indicated (Supplementary Table 1) that women had a higher level of fear compared with men [t(3,023) = −3.288, p = 0.001, Cohen's d = 0. 12]. Medical staff aged 40–49 years old had lower levels of anxiety [F(3,3,021) = 5.026, p = 0.002, partial-eta2 = 0.005, and fear F(3,3,021) = 3.417, p = 0.017, partial-eta2 = 0.003]. Medical staff with postgraduate degrees or higher reported lower fear levels [F(3,3,021) = 2.763, p = 0.041, partial-eta2 = 0.003]. Unmarried medical staff reported higher levels of anxiety [F(3,3,021) = 3.200, p = 0.022, partial-eta2 = 0.003] and fear [F(3,3,021) = 3.564, p = 0.014,partial-eta2 = 0.004]. As expected, medical staff from the city (over 10,000 confirmed cases) had higher levels of anxiety [F(3,3,021) = 2.440, p = 0.004, partial-eta2 = 0.032] and anger [F(3,3,021) = 3.412, p = 0.004, partial-eta2 = 0.006].
One way ANOVA (Figure 1A) showed that among the negative emotions, anxiety was the most prominent emotion in medical staff, followed by sadness, fear, and anger [F(3,12,096) = 174.075, p < 0.001, partial-eta2 = 0.041]. The response selection rates of anxiety, sadness, fear, and anger were 78.3 67.5 68, and 45.8%. And 32.8–55.2% of medical staff rated their emotion at a mild degree. Further analysis (Supplementary Table 2) showed that compared with doctors and other medical staff, nurses had higher selection rates of anxiety [χ2(2,3,025) = 16.776, p < 0.001], sadness [χ2(2,3,025) = 11.908, p < 0.001], fear [χ2(2,3,025) = 49.976, p < 0.001], and anger [χ2(2,3,025) = 21.270, p < 0.001].
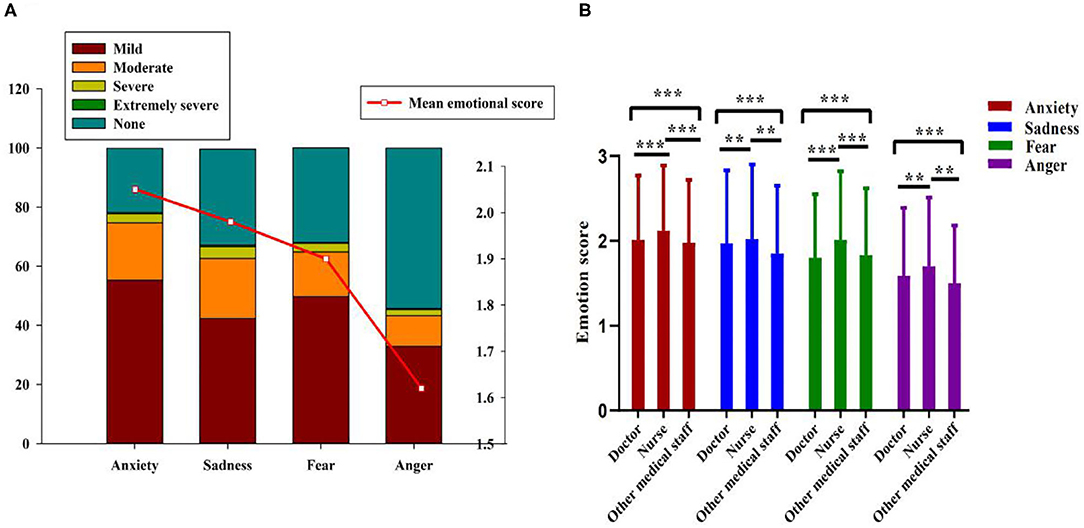
Figure 1. The negative emotional levels of different medical staff. (A) The overall negative emotional levels and response rates. (B) The negative emotional levels between different professionals. **p < 0.01, ***p < 0.001.
Figure 1B shows that nurses also reported higher levels of anxiety [F(2,3,022) = 8.347, p < 0.001, partial-eta2= 0.005], sadness [F(2,3,022) = 7.732, p < 0.001, partial-eta2 = 0.005], fear [F(2,3,022) = 34.630, p < 0.001, partial-eta2 = 0.022], and anger [F(2,3,021) = 9.719, p < 0.001, partial-eta2 = 0.006]. The results indicated that nurses experienced stronger negative emotions compared with other medical staff.
Figure 2A shows that the levels of negative emotions gradually declined over time during the early stage of the epidemic [anxiety: F(15,3,009) = 3. 199, p < 0.001, partial-eta2 = 0.016, sadness: F(15,3,009) = 2.016, p = 0.011, partial-eta2 = 0.010, fear: F(15,3,009) = 2.577, p = 0.001, partial-eta2 = 0.013, and anger: F(15,3,009) = 2.067, p = 0.009, partial-eta2 = 0.010]. Further analysis indicated (Figure 2B) that different medical professionals had a similar downward trend of sadness, fear, and anger over time without significant difference.
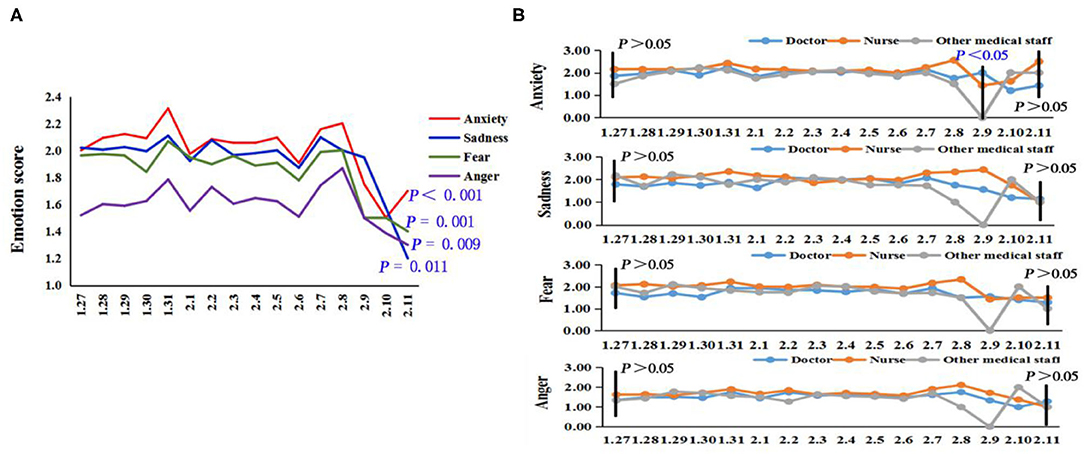
Figure 2. The trend of negative emotions over time. (A) The overall emotional trend of frontline medical staff. (B) The emotional trend of different medical professionals.
Supplementary Figure 1 shows that the shortage of protective supplies was the leading cause for all negative emotions. Specifically, the main sources for anxiety were possible infection without isolation, new confirmed cases, and possible infection without protection. The main sources for sadness were exhausted medical staff, helpless patients, and innocent people. The main sources for fear were possible infection without isolation, possible infection without protection, and being infected by the virus. The main sources for anger were possible infection without isolation, possible infection without protection, and irresponsible rumors.
The Chi-squared test was conducted to compare the percentage of sources between different medical professionals, which (Supplementary Table 3) indicated that compared with doctors, nurses had higher rates of “shortage of protective supplies” [χ2(2,3025) =10.121, p = 0.006] and “new confirmed cases” [χ2(2,3025) = 39.266, p < 0.001], which were sources of anxiety, as well as a higher percentage of “being infected by the virus” [χ2(2,3025) =17.980, p < 0.001], which was a main source of fear.
Figure 3 shows that medical staff answered “yes” for “this is a severe outbreak,” and had higher levels of anxiety [t(3,023) = 2.980, p = 0.003, Cohen's d = 0.46], sadness [t(3,023) = 2.677, p = 0.007, Cohen's d = 0.42], and fear [t(3,023) = 4.455, p < 0.001, Cohen's d = 0.73] compared with those medical staff who had no risk perception. Similarly, medical staff answered “yes” for “the epidemic is close to me,” and reported higher levels of anxiety [t(3,023) = 2.945, p = 0.003, Cohen's d = 0.31], sadness [t(3,023) = 2.375, p = 0.018, Cohen's d = 0.26], and fear [t(3,023) = 4.073, p < 0.001, Cohen's d = 0.47]. Moreover, medical staff answered “yes” for “I am in danger,” and reported higher levels of anxiety [t(3,023) = 12.602, p < 0.001, Cohen's d = 0.70], sadness [t(3,023) = 8.536, p < 0.001, Cohen's d = 0.47], fear [t(3,023) = 13.567, p < 0.001, Cohen's d = 0.77], and anger [t(3,023) = 7.061, p < 0.001, Cohen's d = 0.41].
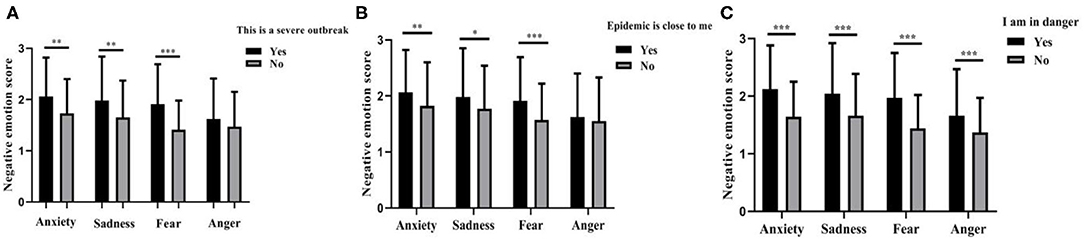
Figure 3. The impact of risk perception on negative emotions. (A) This is a severe outbreak. (B) The epidemic is close to me. (C) I am in danger. *p < 0.05, **p < 0.01, ***p < 0.001.
Pearson correlation showed that (Table 1) cognitive reappraisal and expression suppression were negatively related to the levels of anxiety, fear, anger, and sadness (r = −0.049 ~ −0. 137, p < 0.01), while positive emotion expression, negative emotion expression, and impulse strength were positively correlated with negative emotions (r = 0.041 ~ 0. 166, p < 0.05).
Figure 4 indicates that negative emotions increased avoidant behavior tendency [χ2(4,3,025) = 12.530 ~ 145.929, all p < 0.01] and disturbed physical function [χ2(4,3,025) = 46.331 ~ 319.721, all p < 0.001] with increasing tendency as the enhancement of negative emotions (Supplementary Table 4).
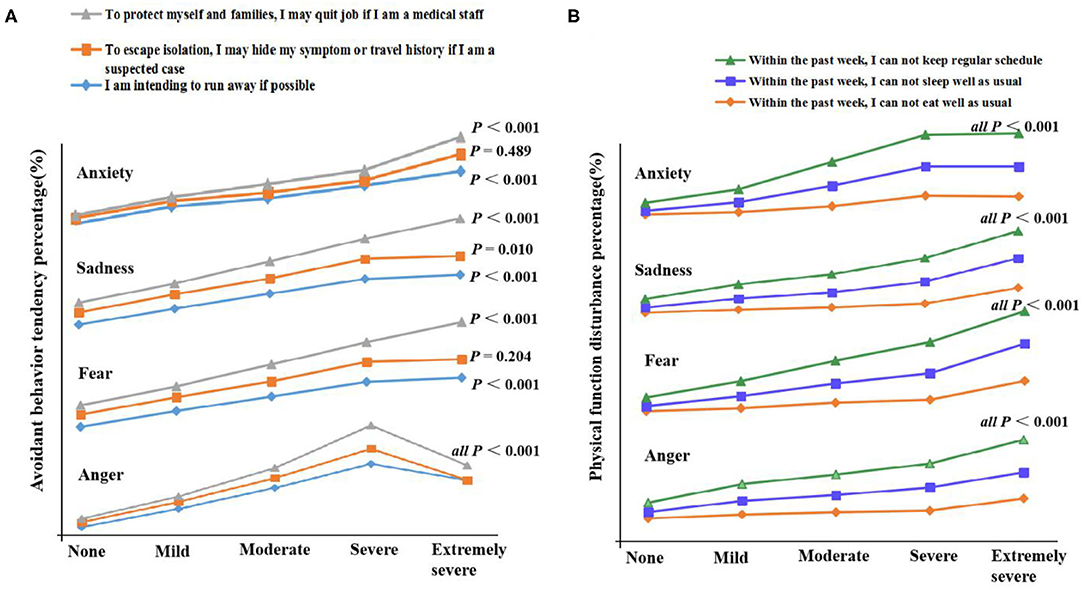
Figure 4. The effects of negative emotions on avoidant behavior tendency and disturbed physical function. (A) Avoidant behavior tendency. (B) Disturbed physical function.
Supplementary Figure 2 shows that the CFA analysis on risk perception, disturbed physical function, and avoidant behavior tendency indicated an ideal model fit (46) (χ2 = 0, df = 0, NFI = 1.000, IFI = 1.000, CFI = 1.000, RMSEA = 0.012 ~ 0.052), whereas the CFA coefficients of negative emotions also showed a satisfied model fit (χ2 = 4.998, df = 1, χ2 /df = 4.998, NFI = 0.999, IFI = 0.999, CFI = 0.999, RMSEA = 0.005).
To further explore the interaction between negative emotions and risk perception, emotional regulation, avoidant behavior tendency, and disturbed physical function, a hypothesis-driven model test was carried out (χ2 = 57.986, df = 9, χ2/df = 6.443, RMSEA = 0.042, GFI = 0.995, AGFI = 0.983, NFI = 0.973, IFI = 0.977, TLI = 0.946, CFI = 0.977).
Figure 5 indicates that risk perception had a positive direct effect on negative emotion and avoidant behavior tendency, and an indirect effect on avoidant behavior tendency (0.029–0.048). Cognitive reappraisal had a negative effect while emotional expressivity had a positive effect on negative emotion. Negative emotion had a positive direct effect on avoidant behavior tendency and disturbed physical function, and an indirect effect on disturbed physical function (0.005–0.02). The results indicated a positive effect between negative emotion and risk perception, avoidant behavior tendency, and disturbed physical function, in which negative emotion and avoidant behavior tendency played a mediation role.
Moreover, cognitive reappraisal reduced negative emotion (β = −0.15, p < 0.001), and avoidant behavior tendency (β = −0.08, p < 0.001), while impulse strength and negative expressivity increased negative emotion (β = 0.11, 0.12, p < 0.001).
Multi-group analysis was conducted to verify the differences of models in three groups (doctors, nurses, and other medical staff). The result showed that there was no statistical difference in group comparisons (p = 0.367), which indicated that the different roles of medical staff did not affect this model.
In the current study, we explored the status, trend, and influential pattern of negative emotions in the Chinese frontline medical staff at the early stage of the COVID-19 epidemic via a nationwide investigation. Overall, we found that Chinese frontline medical staff experienced a mild level of negative emotions (i.e., fear, anxiety, anger, and sadness) in the early period of COVID-19, the trend of which decreased gradually over time. Additionally, nurses experienced a higher level of negative emotions, as well as women, younger, and unmarried medical staff. Risk perception and emotional expressivity increased negative emotions, cognitive reappraisal and expressive suppression reduced negative emotion, while negative emotions led to more avoidant behavior and more physical health disturbances, in which negative emotions mediated the effect of risk perception on avoidant behavior tendency and physical health disturbance of Chinese frontline medical staff.
The study revealed that Chinese frontline medical staff did experience different negative emotions, such as anxiety, sadness, fear, and anger. Among all the negative emotions, anxiety was the most common one for Chinese medical staff at the early stage of COVID-19. At the initial stage of COVID-19, it was normal for the public including frontline medical staff to experience negative emotions with the increasing number of confirmed cases and deaths. Our finding was consistent with other studies (48, 49), which also revealed that medical staff experienced a higher level of anxiety during epidemics. For example, a multicenter survey (50) reported that the prevalence of anxiety was 44.7% in 1,563 Chinese medical workers fighting against COVID-19. Another study (20) also showed that frontline health professionals were highly vulnerable to experiencing physical exhaustion, fear, and emotion disturbance. Notably, in this study, four negative emotions were measured based on the TAS theory, while previous studies (5, 47) rarely investigated all the four negative emotions in one research. Thus, the findings suggested that psychological interventions and support should focus on relieving these primary negative emotions under crisis for frontline medical staff.
As to the degree of those negative emotions, medical staff only suffered from a mild degree even in the toughest period of fighting COVID-19, while the degree of negative emotions was rarely reported in other research. This might be due to the fact that Chinese medical staff had experienced the SARS epidemic in 2003 and they had been well prepared for the challenge of future epidemics ever since.
Among all the frontline medical staff, nurses reported the highest level of negative emotions compared with other medical professionals in our investigation, which was consistent with previous studies (22, 23). Nurses were more worried than doctors during the A/H1N1 influenza pandemic (22), and the overall level of distress was significantly higher than that of other medical staff during SARS (23). Nurses were regarded as the most vulnerable group among frontline medical staff due to their high exposure risk to the novel coronavirus compared with other medical professionals. For example, nurses were always at the frontline to screen suspected patients (51) and had close contacts with patients (52). Besides nurses, women, younger, and unmarried frontline medical staff also reported a higher level of negative emotions. Therefore, more attention should be paid to maintain their psychological health under the current epidemic, and it is essential to support different kinds of medical staff differently.
The trend of negative emotions of Chinese frontline medical staff declined gradually as time went by, which was consistent with our hypothesis and previous findings (19, 25). However, according to one study conducted in Hong Kong in June 2003, researchers reported a relatively low level of distress in medical staff at the first stage of the epidemic, and they assumed that the level would be higher at the peak of the epidemic (23). Our result was inconsistent with their assumption. Two possible explanations for this finding: Firstly, the Chinese government played an active and productive role in the response to fighting against the epidemic, which enhanced medical staff's confidence toward the epidemic, and reduced their negative emotions effectively. Secondly, Chinese mental healthcare professionals provided psychological support for frontline medical staff in a timely and convenient manner (23), which guaranteed their mood effectively. The results suggested that along with the powerful executions of the government and epidemic control in China, medical staff's negative emotion decreased in a sense, which confirmed the effect of national epidemic control on public emotion. The finding also showed that psychological experts could provide psychological support at the beginning of an epidemic, which would be an important preventive measure to deal with the mental health problems of frontline medical staff.
In this study, we found that the shortage of personal protective equipment (PPE) was the leading source of all negative emotions (i.e., fear, anxiety, anger, and sadness) of frontline medical staff at the early stage of the COVID-19 epidemic, which was also consistent with previous findings (13). Without standardized PPE, frontline medical staff were exposed to the higher risk of being infected with the virus. Besides, the potential infected individuals without quarantine and the suspected cases without protection were the main causes of anxiety, fear, and anger of frontline medical staff in this study, which was not previously reported. The results indicated that the quarantine and protection of suspected patients should be implemented strictly and effectively to reduce medical staff's psychological stress. Moreover, being infected by COVID-19 was also a primary source of fear among frontline medical staff. Thus, self-protection is of vital significance and much attention should be paid to train medical staff on how to use PPE before contacting patients (50). Our findings also showed that frontline medical staff felt sad about the existence of exhausted medical staff and severely infected patients. Together, results suggested that to reduce negative emotions of medical staff effectively, strategies should ensure PPE and implement protective procedures strictly and enhance therapeutic efficacy so that it might be most effective, which offers valuable evidence for the government.
The findings confirmed that risk perception induced negative emotions of frontline medical staff significantly, which was consistent with the study (27) conducted during SARS. It showed that the level of fear elevated when people perceived a higher risk perception of the infectious disease (27). Therefore, reducing the risk perception of the epidemic may help healthcare workers reduce negative emotions. One systematic review of healthcare workers' perceptions of risk suggests that institutions need to ensure that appropriate infection control safeguards are in place to protect workers and their families (30). By doing so, negative emotions of medical staff are reduced effectively with lower risk perception.
Additionally, our findings showed the potential effect of negative emotion on personal avoidant behavior tendency, with the evidence of higher avoidant behavior tendency in medical staff with stronger negative emotion. Previous studies also found that some medical staff were reluctant to work or wanted to resign due to the fear of being infected or infecting their family members during the SARS epidemic (17, 33). The results suggested that reducing negative emotions may decrease the avoidant behavior tendency accordingly.
Besides, the findings also revealed the effect of negative emotion on personal disturbed physical function, with the evidence that a higher level of disturbed physical function in medical staff was related with a stronger level of negative emotion. The findings filled in the blank of previous empirical research between negative emotion and personal disturbed physical function, which also suggested that reducing negative emotions might decrease the physical function disturbance of frontline medical staff accordingly.
Moreover, the study innovatively verified the effect of emotion regulation strategy on negative emotion in the group of frontline medical staff during the early period of the COVID-19 epidemic. The findings showed that higher cognitive reappraisal and expressive suppression reduced the degree of negative emotions, while emotional expressivity increased negative emotions. The results indicate that the application of cognitive reappraisal and expressive suppression and less utilization of emotional expressivity may reduce negative emotions of frontline medical staff.
Together, risk perception induced negative emotions of frontline medical staff, emotion regulation strategies modulated negative emotions, and negative emotion had an effect on avoidant behavior tendency and disturbed physical function. The findings confirmed the TAS theory and further suggested the interaction between cognition, emotion, and behavior.
The model test confirmed that risk perception increased negative emotion, which has been illustrated in a previous study (27). Moreover, emotional expressivity increased negative emotion, cognitive reappraisal and expressive suppression decreased negative emotion, and negative emotion increased disturbed physical health, which were first verified in this study. Among which, negative emotion played an important mediation role between risk perception and avoidant behavior and disturbed physical function. Therefore, measures to reduce risk perception of frontline medical staff should be taken in a timely manner to decrease negative emotion and avoidant behavior at the early period of the COVID-19 epidemic. For example, training courses about the disease and treatment might be an effective way to minimize risk perception (53, 54). Meanwhile, to better maintain normal psychological and physical function under crisis, intervention and guidance on fear emotion are critical. We also found that avoidant behavior could directly influence disturbed physical function, filling the gap of existing knowledge. Thus, we can reduce negative emotions and avoidant behavior of frontline medical staff to promote their physical function by adopting interventions like cognitive-behavioral therapy (CBT) (55, 56). This knowledge helps to reveal an influential pattern between negative emotion and risk perception, emotion regulation strategy, avoidant behavior tendency, and physical function.
Importantly, negative emotions could be reduced through cognitive reappraisal and reduced risk perception, followed by decreased avoidance behavior and physical impairment. The findings provide a guide for psychologists to promote crisis intervention in the group of frontline medical staff during the COVID-19 epidemic, which further broadens the application of the TAS model.
The strengths of our study are as follows: firstly, the current study was one of the earliest nationwide and large population-based online surveys targeted at Chinese frontline medical staff fighting against COVID-19 from January 27 to February 11, 2020, which covered all 32 provincial administrative regions of China. Secondly, our study was a continuous trend survey of negative emotions of frontline medical staff at the early COVID-19 stage. We also explored the emotion status of different medical professionals, which might be potentially important to draw up psychological interventions for the targeted population under a public health crisis. Thirdly, we also explored the influential effects between negative emotions and risk perception, avoidant behavior, physical dysfunction, and emotion regulation among Chinese frontline medical staff, which could help provide emotion support more precisely and scientifically in the future.
Several limitations also exist in the study. First, only one question was designed to evaluate each kind of the four common negative emotions, and the study lacked more details about negative emotions of Chinese frontline medical staff fighting. Second, the data of other influential factors of emotions, such as coping styles and resilience, were not collected in the present study, and thus future research can explore more variables interacting with the emotions of frontline medical staff during epidemics. Moreover, despite the fact that numerous statistically significant results were found in the study, the effect sizes were rather weak. Some bias might exist due to the online data collection though it was a very convenient and effective way to do the online survey during COVID-19.
In conclusion, Chinese frontline medical staff experience a mild level of negative emotions (i.e., fear, anxiety, anger, and sadness) at the early stage of COVID-19, which decreases gradually over time. Nurses report a higher level of negative emotions, as well as women, younger, and unmarried healthcare professionals. To better ensure the mental health of medical staff, reducing risk perception and improving cognitive reappraisal might be important, which would be potentially valuable to form targeted psychological intervention and emotional guidance under crisis in the future.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of the Army Medical University of China. The patients/participants provided their written informed consent to participate in this study.
QD: research design, review, and supervision. XS: making questionnaires, data analysis, and writing original draft preparation. FX: review and editing. BC, PS, SS, ZC, YY, MZ, XQ, YL, and YW: data collection. All authors have read and agreed to the published version of the manuscript.
QD claims that this study was supported by the Key Project of Natural Science Foundation of Chongqing (cstc2020jcyj-zdxmX0009), the Medical Innovation Project of Army Medical University (2019ZLX003), and the Key Project and Innovation Project of People's Liberation Army of China (18CXZ005).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors thank the Wenjuanxing platform and Mr. Li of Weirenren psychological consultation center for their support and endeavor on questionnaire investigation. We also thank all participants who took part in this online investigation. We appreciate the hard work of all graduate students who took part in this study as research assistants.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.567446/full#supplementary-material
1. Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. (2020) 368:m408. doi: 10.1136/bmj.m408
2. Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I. COVID- 19 Pandemia and Public and Global Mental Health from the Perspective of Global Health Securit. Psychiatr Danub. (2020) 32:6–4. doi: 10.24869/psyd.2020.6
3. Zhang Y, Ma ZF. Impact of the COVID- 19 pandemic on mental health and quality of life among local residents in Liaoning province, china: a cross-sectional study. Int J Environ Res Public Health. (2020) 17:2381. doi: 10.3390/ijerph17072381
4. World Health Organization. 2019 Coronavirus Outbreak Notification. (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on May 4, 2020).
5. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID- 19) epidemic among the general population in china. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
6. Zhou P, Huang Z, Xiao Y, Huang X, Fan XG. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect Control Hosp Epidemiol. (2020) 41:745–6. doi: 10.1017/ice.2020.60
7. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID- 19 outbreak. Brain Behav Immunity. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
8. Huang J, Liu F, Teng Z, Chen J, Zhao J, Wang X, et al. Care for the psychological status of frontline medical staff fighting against COVID- 19. Clin Infect Dis. (2020) 71:3268–9. doi: 10.1093/cid/ciaa385
9. Myer RA, Conte C. Assessment for crisis intervention. J Clin Psychol. (2006) 62:959–70. doi: 10.1002/jclp.20282
10. Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. (2006) 43:215–25. doi: 10.1016/j.ijnurstu.2005.03.006
11. Ho SM, Kwong-Lo RS, Mak CW, Wong JS. Fear of severe acute respiratory syndrome (SARS) among health care workers. J Consult Clin Psychol. (2005) 73:344–9. doi: 10.1037/0022-006X.73.2.344
12. Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID- 19 pandemic: a cross-sectional study. Psychiatry Res. (2020) 288:112936. doi: 10.1016/j.psychres.2020.112936
13. Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. (2003) 168:1245–51. doi: 10.1001/jama.289.18.2432
14. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. (2007) 52:233–40. doi: 10.1177/070674370705200405
15. Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan for fighting against the COVID- 19 epidemic. J Nurs Manag. (2020) 28:1002–9. doi: 10.1111/jonm.13014
16. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
17. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID- 19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
18. Schwartz J, King CC, Yen MY. Protecting health care workers during the COVID- 19 coronavirus outbreak-lessons from Taiwan's SARS response. Clin Infect Dis. (2020) 71:858–60. doi: 10.1093/cid/ciaa255
19. Choi BS, Kim JS, Lee DW, Paik JW, Lee BC, Lee JW, et al. Factors Associated with emotional exhaustion in south korean nurses: a cross-sectional study. Psychiatry Invest. (2018) 15:670–6. doi: 10.30773/pi.2017.12.31
20. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
21. Xiang YT, Jin Y, Wang Y, Zhang Q, Zhang L, Cheung T. Tribute to health workers in China: a group of respectable population during the outbreak of the COVID-19. Int J Biol Sci. (2020) 16:1739–40. doi: 10.7150/ijbs.45135
22. Goulia P, Mantas C, Dimitroula D, Mantis D, Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. (2010) 10:322. doi: 10.1186/1471-2334-10-322
23. Wong TW, Yau JK, Chan CL, Kwong RS, Ho SM, Lau CC, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. (2005) 12:13. doi: 10.1097/00063110-200502000-00005
24. Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. (1998) 2:271–99. doi: 10.1037/1089-2680.2.3.271
25. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immunity. (2020) 87:11–17. doi: 10.1016/j.bbi.2020.03.028
26. Shi K, Lu J, Fan H, Jia J, Song Z, Li W, et al. Rationality of 17 cities' public perception of SARS and predictive model of psychological behavior. Chin Sci Bull. (2003) 48:1297–303. doi: 10.1007/BF03184166
27. Rosoff H, John RS, Prager F. Flu, risks, and videotape: escalating fear and avoidance. Risk Anal. (2012) 32:729–43. doi: 10.1111/j.1539-6924.2012.01769.x
28. Kushnir H, Packer C. Perceptions of risk from man-eating lions in southeastern Tanzania. Front Ecol Evolut. (2019) 7:47. doi: 10.3389/fevo.2019.00047
29. Leppin A, Aro AR. Risk perceptions related to SARS and avian influenza: theoretical foundations of current empirical research. Int J Behav Med. (2009) 16:7–29. doi: 10.1007/s12529-008-9002-8
30. Koh Y, Hegney DG, Drury V. Comprehensive systematic review of healthcare workers' perceptions of risk and use of coping strategies towards emerging respiratory infectious diseases. Int J Evidence Based Healthcare. (2011) 9:403–19. doi: 10.1111/j.1744-1609.2011.00242.x
31. Shultz JM, Cooper JL, Baingana F, Oquendo MA, Espinel Z, Althouse BM, et al. The Role of fear-related behaviors in the 2013-2016 West Africa Ebola virus disease outbreak. Curr Psychiatry Rep. (2016) 18:104. doi: 10.1007/s11920-016-0741-y
32. Yeung DY, Fung HH. Age differences in coping and emotional responses toward SARS: a longitudinal study of Hong Kong Chinese. Aging Mental Health. (2007) 11:579–87. doi: 10.1080/13607860601086355
33. Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM, Yeh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. (2004) 185:127–33. doi: 10.1192/bjp.185.2.127
34. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID- 19) in January and February 2020 in China. Med Sci Monit. (2020) 26:e923549. doi: 10.12659/MSM.923549
35. Lam MH, Wing YK, Yu MW, Leung CM, Ma RC, Kong AP, et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med. (2009) 169:2142–7. doi: 10.1001/archinternmed.2009.384
36. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
37. Kobayashi R, Shigematsu J, Miyatani M, Nakao T. Cognitive reappraisal facilitates decentering: a longitudinal cross-lagged analysis study. Front Psychol. (2020) 11:103. doi: 10.3389/fpsyg.2020.00103
38. Sai L, Luo S, Ward A, Sang B. Development of the tendency to use emotion regulation strategies and their relation to depressive symptoms in chinese adolescents. Front Psychol. (2016) 7:1222. doi: 10.3389/fpsyg.2016.01222
39. Liu W, Liu F, Chen L, Jiang Z, Shang J. Cognitive reappraisal in children: neuropsychological evidence of up-regulating positive emotion from an ERP Study. Front Psychol. (2019) 10:147. doi: 10.3389/fpsyg.2019.00147
40. Chen S, Deng Z, Xu Y, Long Q, Yang J, Yuan J. Individual differences in spontaneous expressive suppression predict amygdala responses to fearful stimuli: the role of suppression priming. Front Psychol. (2017) 8:1. doi: 10.3389/fpsyg.2017.00001
41. Cutuli D. Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: an overview on their modulatory effects and neural correlates. Front Syst Neurosci. (2014) 8:175. doi: 10.3389/fnsys.2014.00175
42. Trierweiler LI, Eid M, Lischetzke T. The structure of emotional expressivity: each emotion counts. J Pers Soc Psychol. (2002) 82:1023–40. doi: 10.1037/0022-3514.82.6.1023
43. Gross JJ, John OP. Facets of emotional expressivity: three self-report factors and their correlates. Pers Individ Differ. (1995) 19:555–68. doi: 10.1016/0191-8869(95)00055-B
44. Dillard JP, Yang C, Li R. Self-regulation of emotional responses to Zika: spiral of fear. PloS ONE. (2018) 13:e0199828. doi: 10.1371/journal.pone.0199828
45. Wang L, Liu HC, Li ZQ, Du W. Reliability and validity of emotion regulation questionnaire Chinese revised version. China J Health Psychol. (2007) 15:503–5. doi: 10.13342/j.cnki.cjhp.2007.06.012
46. Birmaher B. Emotional and behavioral problems of Chinese left-behind children: a preliminary study. Soc Psychiatry Psychiatr Epidemiol. (2010) 45:655–64. doi: 10.1007/s00127-009-0107-4
47. Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosomatic Res. (2020) 133:110102. doi: 10.1016/j.jpsychores.2020.110102
48. Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Progr Neuropsychopharmacol Biol Psychiatry. (2021) 107:110247. doi: 10.1016/j.pnpbp.2021.110247
49. Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
50. Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID- 19 outbreak. Lancet Psychiatry. (2020) 7:e17–e8. doi: 10.1016/S2215-0366(20)30077-8
51. Chen CS, Wu HY, Yang P, Yen CF. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr Serv. (2005) 56:76–9. doi: 10.1176/appi.ps.56.1.76
52. Catton H. Global challenges in health and health care for nurses and midwives everywhere. Int Nurs Rev. (2020) 67:4–6. doi: 10.1111/inr.12578
53. Zhang Z, Liu S, Xiang M, Li S, Zhao D, Huang C, et al. Protecting healthcare personnel from 2019-nCoV infection risks:lessons and suggestions. Front Med. (2020) 14:229–31. doi: 10.1007/s11684-020-0765-x
54. Manabe T, Tran TH, Doan ML, Do TH, Pham TP, Dinh TT, et al. Knowledge, attitudes, practices and emotional reactions among residents of avian influenza (H5N1) hit communities in Vietnam. PLoS ONE. (2012) 7:e47560. doi: 10.1371/journal.pone.0047560
55. Ford T, Richardson J, Wilkinson K, Smith P, Berry V, Barnhofer T, et al. Could mindfulness-based cognitive therapy prevent a lifelong recurrent course of depression or anxiety by addressing key mechanisms of vulnerability in high-risk adolescents? Br J Psychiatry. (2020) 216:175–7. doi: 10.1192/bjp.2019.183
Keywords: COVID-19, negative emotion, status, trend, influential pathway, Chinese frontline medical staff
Citation: Sun X, Xie F, Chen B, Shi P, Shen S, Chen Z, Yuan Y, Zhang M, Qin X, Liu Y, Wang Y and Dai Q (2021) Negative Emotions in Chinese Frontline Medical Staff During the Early Stage of the COVID-19 Epidemic: Status, Trend, and Influential Pathways Based on a National Investigation. Front. Psychiatry 12:567446. doi: 10.3389/fpsyt.2021.567446
Received: 29 May 2020; Accepted: 16 November 2021;
Published: 23 December 2021.
Edited by:
Andrea De Giorgio, eCampus University, ItalyReviewed by:
Miloš Stankovic, Ludwig Maximilian University of Munich, GermanyCopyright © 2021 Sun, Xie, Chen, Shi, Shen, Chen, Yuan, Zhang, Qin, Liu, Wang and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qin Dai, ZGFpcWluMTAxQGhvdG1haWwuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.