- 1Department of Biomedical Engineering, The Chinese University of Hong Kong, Hong Kong SAR, China
- 2School of Biomedical Engineering, University of Technology Sydney, Ultimo, NSW, Australia
- 3School of Science, Edith Cowan University, Perth, WA, Australia
- 4Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China
- 5Department of Rehabilitation Sciences, Jamia Hamdard University, New Delhi, India
- 6Department of Occupational Therapy, Mahatma Gandhi Occupational Therapy College, Jaipur, India
The novel coronavirus disease (COVID-19) pandemic has made a huge impact on people's physical and mental health, and it remains a cause of death for many all over the world. To prevent the spread of coronavirus infection, different types of public health measures (social isolation, quarantine, lockdowns, and curfews) have been imposed by governments. However, mental health experts warn that the prolonged lockdown, quarantine, or isolation will create a “second pandemic” with severe mental health issues and suicides. The quarantined or isolated people may suffer from various issues such as physical inactivity, mental health, economic and social problems. As with the SARS outbreak in 2003, many suicide cases have been reported in connection with this current COVID-19 pandemic lockdown due to various factors such as social stigma, alcohol withdrawal syndrome, fear of COVID infection, loneliness, and other mental health issues. This paper provides an overview of risk factors that can cause suicide and outlines possible solutions to prevent suicide in this current COVID-19 pandemic.
Introduction
The novel coronavirus disease (COVID-19) is a recently discovered infectious disease that is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 was first identified in Wuhan, China in December 2019 (1), and it has since spread rapidly to the entire world. On January 30, 2020, the World Health Organization (WHO) declared it a Public Health Emergency of International Concern (PHEIC) based on the International Health Regulations (2005), and they declared it a pandemic on March 11, 2020 (2). The following clinical symptoms present in COVID-19 patients: fever, cough, fatigue, muscle soreness, headache, diarrhea, and dyspnea. However, on April 1, 2020, China's National Health Commission (NHC) reported that 78% of cases were asymptomatic (3). COVID-19 mainly spreads through the respiratory droplets. Besides, people can also be infected by touching contaminated surfaces where the is virus present and then touching their own mouth, eyes, and nose (4). As of May 20, 2020, 4,761,559 confirmed cases and 317,529 confirmed deaths have been reported from 216 countries (WHO, 2020). The United States of America (USA) is in the number one place among a list of countries most affected by coronavirus. For example, according to a report from the WHO Coronavirus Disease (COVID-19) Dashboard, as of May 20, 2020, 1,477,459 confirmed cases and 89,271 deaths were reported in the USA. In India, the second-most populated country in the world, as of May 20, 2020, a total of 101,139 confirmed cases and 3,163 deaths were reported by the WHO (5). At present, there is no vaccination or any other therapeutic method for COVID-19. Therefore, a number of preventive measures have been taken around the world to prevent the spread of infection, such as quarantine, social isolation, lockdowns, and curfews. In this COVID-19 pandemic, ~2.6 billion people have been quarantined or are in under lockdown around the world (6). Although public health preventive measures have been taken to control the spread of COVID-19 infection, it has still had a huge impact on mental health around the world due to various psychological, social, and economical factors, such as loneliness, social isolation, anxiety, stress, depression, fear of COVID-19 infection, loss of loved ones, alcohol withdrawal syndrome or substance misuse, and loss of employment (7–9). Several studies reported that these above-mentioned factors will or have already increased suicide rates during COVID-19 (8, 10–12). A nationwide survey study reported that 34.1% of the quarantined or isolated people had experienced at least one of the following mental health issues: acute stress, anxiety, depression, and sleep disorders (13), and their study also stated that this likelihood was higher in frontline workers, people with pre-existing mental health issues, and people with chronic physical health disorders. Specifically, a previous study found that suicidal ideation behavior was significantly higher among people with pre-existing mental health disorders than in healthy controls in the COVID-19 pandemic (14). Furthermore, previous literature has stated that COVID-19 pandemic-related suicide rates will in the future range from 1 to 145% based on various prediction modeling studies (12). However, limited studies have been carried out on COVID-19 infection prevention measures (isolation, social isolation, locking, and curfew order) and their impact on mental health. Likewise, as soon as these lockdown policies are implemented, there is no updated and functional suicide monitoring system data on the effect of COVID-19 lockdown and other social distancing measures on mental health and suicide. Therefore, in this study, we briefly reviewed the different types of infectious-preventive measures for better understanding and the psychological impact of infection-preventive measures and risk factors for COVID-19-related suicides (up to May 2020). This study also tried to suggest possible solutions to prevent risk factors for the psychological effects of quarantine or lockdown procedures.
Types of COVID-19 Preventive Measures
These kinds of preventive measures are not unfamiliar; for example, 40 days of quarantine were imposed in Italy during the 14th century to prevent plague epidemics (15, 16), and, more recently, a quarantine was put in place for severe acute respiratory syndrome (SARS) in 2003 (17). Quarantine is one of the oldest and most effective methods to reduce the spread of communicable diseases, and it separates and restricts people who have been exposed to a contagious disease or who have traveled to an affected region; people may not, however, be infected or might be asymptomatic. For instance, more than 150,000 persons were quarantined at their homes in Taiwan to control the SARS outbreak in 2003. Out of 150,000 quarantined people, only 24 people were infected by SARS-coronavirus (SARS-CoV) infection (18). In the COVID-19 outbreak, most of the countries in the world enforced a compulsory 14 days home quarantine or in a designated place (hotel) for people who have traveled to other countries. Under the policies of quarantine, people are not allowed to move from their home or designated place to meet others or invite visitors to their place of residence. If quarantine measures are implemented by the governments, people need to strictly follow the guidelines of the governments or public health authorities. It can be either voluntary or mandatory and implemented at individual groups or community level (19).
On the other hand, isolation has been imposed on the infected people to protect the non-infected people from those people with a confirmed diagnosis of contagious disease. Isolation and quarantine have been considered extreme forms of social distancing. The infected persons will usually be admitted and isolated in the hospital settings under medical supervision (20). In case of infection with mild symptoms, the infected person will be isolated at home.
Another form of public health measure to prevent the spread of infectious disease from person to person is “social distancing.” The “social distancing” measures are implemented to reduce people's physical interactions with other people in the community. Since COVID-19 transfers from human to human (21), the following guidelines are practiced in the social distancing methods: wearing face masks, maintaining at least 6 feet distance from the other persons, avoiding social gatherings, avoiding handshakes, avoiding crowds at the parks, beaches, restaurants, shops, or any other public or private places, and work from home if possible.
The most extreme type of public health measure is “lockdown.” Lockdown restricts the moment of people from one place to another place, and it can be imposed when enough people have fallen sick due to contagious diseases in specific regions or countries (22, 23). The government may order the shut down of schools, universities, public transports, taxis, railways, domestic and international flights, restaurants, temples, churches, mosques, and movie theatres, but hospitals remain an exception (24, 25).
Impact of Isolation, Quarantine, and Lockdown on Mental Health and Risk of Suicide
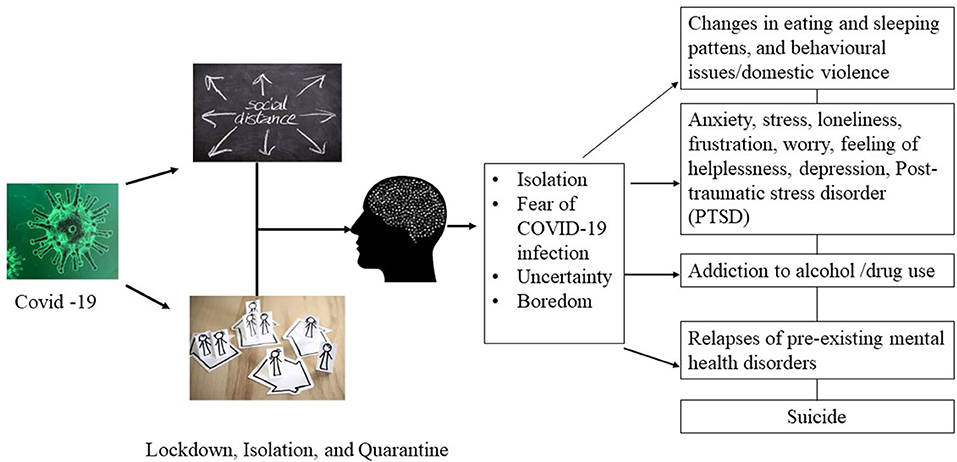
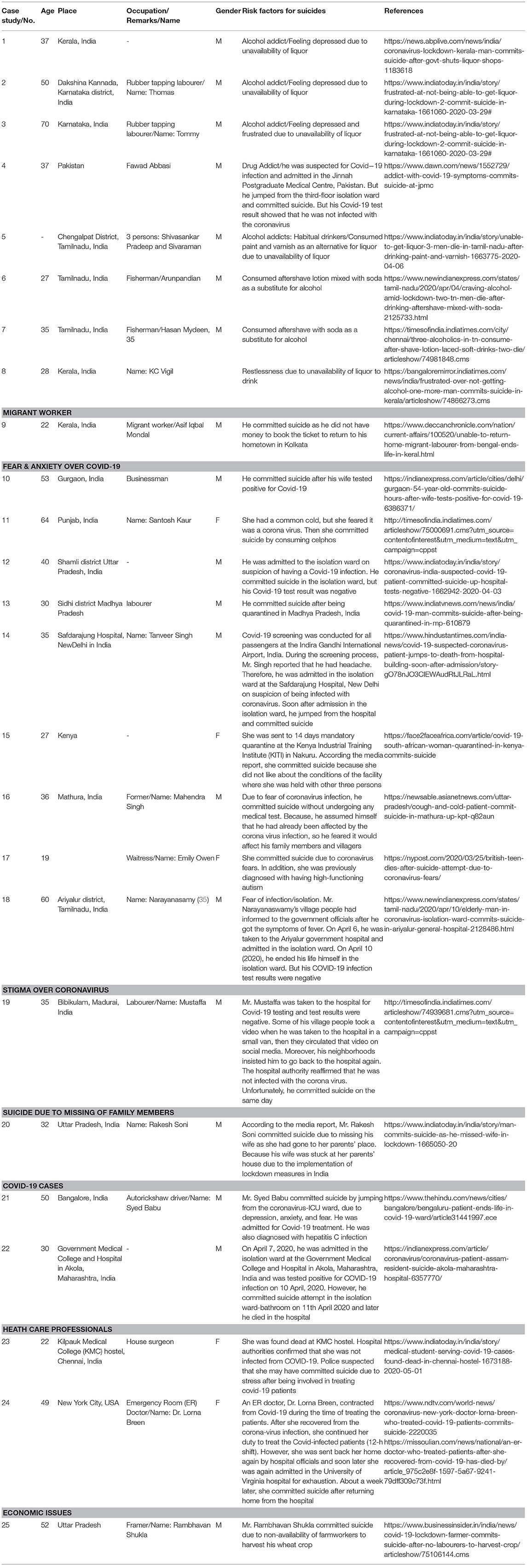
Around the world, the COVID-19 pandemic and lockdown have brought a huge burden to the public, governments, and the economy of the countries. Although quarantines or lockdowns are implemented for a good reason, to prevent the spread of COVID-19, they may cause various adverse effects in the form of physical, psychological, social, and economic consequences. In particular, with social distancing, isolation, and lockdown, people may suffer from very serious psychological issues, such as anxiety, stress, fear, fear-induced overreactive behavior, frustration, guilt, anger, boredom, sadness, worry, nervousness, helplessness, loneliness, insomnia, and depression (26, 27) (Figure 1). A previous study investigated the psychological effects of SARS-quarantined persons in Toronto, Canada, and it was reported that 28.9% of people had a symptom of posttraumatic stress disorder (PTSD), and 31.2% suffered from depressive disorder (28). In extreme cases, social distancing or social isolation may increase the risk of suicide (29), and the following risk factors may trigger suicidal thoughts and ideas: social isolation due to prolonged lockdown, stress, fears of contracting the infection from others, isolated or quarantined individuals with pre-existing mental health issues, loss of employment, financial instability (7, 30, 31), fear of staying in the isolation ward in the hospital, loss of a loved one or missing family members, and feelings of insecurity for the future. At the SARS outbreak in 2003, a higher suicide rate (18.6 per 100,000) was recorded in Hong Kong (32) and most of them were older adults aged 65 or above (37.46/100,000) (33). Loneliness, isolation, anxiety, fear of contracting the virus, and fear of being a burden to their families were thought to be associated with higher suicide rates among older adults during the time of the SARS epidemic in Hong Kong (32, 34). Like the SARS outbreak in 2003, COVID-19 has instilled an uncertainty in people throughout the world, and it has led people to commit suicide, especially, more cases of suicide have been reported in developing countries than in other parts of the world in the early days of lockdown, isolation, and social distance practices (Table 1).
COVID-19 and Alcohol Addiction
Alcohol dependence is a significant risk factor for suicide. It also has high comorbidity with a variety of psychiatric issues such as depression, violent behavior, mood, and anxiety disorders (36). A previous study reported that people with alcohol addiction are 60–120 times more likely to commit suicide than people with no alcohol use disorders (37). On the other hand, after the announcement of a lockdown in India, there have been a number of suicide cases that have reportedly been due to the current unavailability of alcohol in the market. People with alcohol addictions suffer from alcohol withdrawal syndrome when they suddenly stop drinking or significantly reduce their alcohol intake (38). Alcohol withdrawal syndrome is characterized by tremors, insomnia, anxiety, and other physical and mental symptoms (alcohol hallucinosis, alcohol withdrawal seizures, and delirium tremens). According to the India Today newspaper (March 2020), two alcohol-related suicides were reported in the state of Karnataka, India. The first instance was of a 50-year-old man who desperately moved around for few days to acquire liquor before he ended his life due to frustration and alcohol withdrawal syndrome (39). Another person, a 70-year-old man, committed suicide by hanging himself in a tree in the same district of Karnataka due to the non-availability of alcohol. According to News18, seven people committed suicide due to alcohol withdrawal syndromes in the districts of Thrissur, Kochi, Kannur, Kollam, and Thiruvananthapuram, Kerala, India (40, 41), and most of them were younger than 40 years old (42). In contrast, some people with alcohol addiction took to after-shave lotion or paint and varnish as alternative drinks to liquor after liquor shops closed due to lockdown in Tamilnadu, India. Furthermore, it has been reported that three people died by drinking paint and varnish (43), and two people died after consuming after-shave lotion (44).
COVID- 19 and Social Stigma
Social stigma in the context of health is the extreme social disapproval of a person or group based on a specific disease and its characteristics. Likewise, the COVID-19 outbreak has not only spread fear and anxiety worldwide, it has also fostered various kinds of social stigma, such as discrimination, and racism, and judgmental attitudes toward quarantined or isolated people and people who have traveled to the virus-affected regions or countries. In addition, stigmatized people may be experiencing social rejection or avoidance by others, physical violence, and denial of healthcare services, housing, education, and employment opportunities (45). These types of social stigma not only affect those with the disease, but it also affects their family members, friends, and communities. It can make people afraid to get screened for COVID-19 or any other contagious diseases, and some even take extreme steps, such as suicide or displaying anti-social behavioral issues.
COVID- 19 and Unemployment: An Economic Issue
Although we save thousands of people from the COVID-19 infection by implementing prolonged lockdown measures, there will be a huge micro-, meso-, and macroeconomic loss to individuals, organizations, and countries. The prolonged lockdown can cause an increasing unemployment rate, and it may drive stress, mental health issues, family issues, intake of more alcohol or substance use, an increase in crime or suicide rates. A recent report from the United Nation Labor Agency stated that this COVID-19 pandemic will have a worse effect on the labor market and may lead to a risk of a 50% loss of the global workforce (46). Furthermore, UN news reported that the lockdown measures will affect almost 2.7 billion workers globally (47). Currently, there are millions of workers who suffer from uncertainties related to food, security, and future life. According to the press release of the International Labor Organization (ILO), on April 29, 2020, the second quarter (Q2/2020) of the global showed that working hours from this year (2020) are expected to be 10.5% lower than the last quarter of 2019 (Q4/2019) due to pandemic lockdown measures. This global working hours damage is estimated to be equivalent to 305 million full-time jobs (48). Specifically, in developing countries such as in India, about 27 million people (age group 20–30 years) lost their jobs in April 2020 (49), and the Centre for Monitoring Indian Economy (CMIE) reported that 84% of the household will be affected by decreased monthly income. Similarly, ~1 million people lost their jobs in Australia (50) and 5.5 million in Canada, which was an increase in the unemployment rate of up to 13%, putting it closer to the unemployment rate in the USA (14%) (51).
A recent report predicts that the worldwide unemployment rate is estimated to be at a maximum of 5.6%, and it will increase the suicide rate to 9,570 per year (52). For example, more than 1,500 were made to the Los Angeles suicide crisis hotline crisis in March 2020 after few weeks of lockdown, and one in five calls were related to suicide (53). All over the world, government officials are also stressed over dealing with the economic fallout of the coronavirus. For example, Mr. Thomas Schaefer, Minister of Finance of Hesse, Germany, recently committed suicide on March 28, 2020, due the COVID-19 crisis (54). Likewise, according to Aman et al. (2020) until now, more than 300 deaths have been reported as non-COVID-19 infection-related deaths following the lockdown in India. Among those deaths, 34 deaths were recorded due to financial hardship and starvation (55), however, these reports have not confirmed how many deaths were suicide related.
COVID-19 Non-pharmaceutical Interventions and Psychopathological Factors
It is important to identify which factors modulate the mechanism and changes in psychopathology symptoms among the public in the period of the COVID-19 pandemic. A recent Norwegian population-based study reported that people with pre-existing mental health disorders and those who were living alone are affected by loneliness in the period of implementation of social distancing measures, and loneliness was very closely associated with depression and anxiety (56). Another study found that people with pre-existing anxiety-related and mood disorders had more negative impact than those with no mental disorders; anxiety-related disorder groups, in particular, expressed more fears of the socioeconomic impact, xenophobia, fear of danger and contamination, and traumatic stress-related symptoms (57) based on COVID Stress Scales (58). In addition, a psychopathological cross-sectional study found that some specific fear factors (neuroticism, corona phobia, and hypochondriasis) played a role to elevate pandemic-related psychopathology, such as depressive symptoms and generalized anxiety, in the period of lockdown/other preventive measures (59). These prolonged lockdown/other preventive measure factors and the uncertainty of when the COVID-19 crisis is over would also increase the prevalence of post-traumatic stress disorder (PTSD). Recent literature reported that the prevalence of post-traumatic stress disorder (PTSD) during the COVID-19 in Saudi Arabia was 22.63% (PTSD cut-off score), 24.8% (criteria), and 19.6% (combined). In addition, their study reported that the PTSD prevalence was similar or higher to USA (31.8%), Spain (15.8%,), and Italy (29.5%) than China (2.7–12.8%) (60).
On the other hand, a recent study reported that 37 adolescents and youths, including 14 school-age students, committed suicide in the period of lockdown, based on the report of media news between February 15 to July 6, 2020 (35). The COVID-19 prevention strategies related distress, online class/remote schooling, and examination-related stress to tendencies toward depression, loneliness, and psychological distress. Also, a suicide pact (son and mother) was reported in Bangladesh due to an argument between family members regarding online class (61). Likewise, the elderly population has been the most affected age group due to COVID-19 lockdown in terms of isolation or difficulty in obtaining medical and rehabilitation services for aging-related complications. In this COVID-19 pandemic, older adults have a high risk of infection and death (62). Therefore, the elderly population is more prone to fear, stress, depression, loneliness, and other mental issues.
The COVID-19 social restrictive preventive measures related psychopathological factors, such as stress and anxiety, to an increase in alcohol consumption as a coping mechanism. Regarding the COVID-19 and use of substance or alcohol consumption, previous literature estimated that 75,000 “deaths of despair” may result from COVID-19 pandemic related (stress, isolation, and unemployment) drug and alcohol addiction, and suicide (63, 64).
Suicide Prevention During and After the COVID-19 Outbreak
Across the globe, there is a huge uncertainty is seen among the public due to the coronavirus pandemic. People are facing difficulties in accessing their basic needs (e.g., food and medical services) as well as employment, their futures, and well-being due to the current scenario of the prolonged restrictions on movement, social distancing, and isolation. Besides, social isolation and loneliness can cause serious public health issues among people whether young, middle-aged, or old, and there is a strong association between these and the development of neurocognitive and mental health disorders as well as heart and autoimmune diseases (65); social isolation and loneliness could create negative health outcomes, such as high blood pressure, heart diseases, disability, a decline of cognitive function, and depression (66).
For example, the National Public Health Group-Well Being Trust and Robert Graham Center for Policy Studies in Family Medicine and Primary Care (US) have estimated that around 75,000 Americans could die because of suicide, alcohol and drug misuse, and as a result of the COVID-19 pandemic (67). Another report from the Brain and Mind Centre at Sydney University, Australia, predicted that the suicide rates will double due to the social and economic consequences of the national lockdown measures, and about 1,500 extra deaths will occur in Australia (68). Therefore, worldwide, mental health and suicide experts warn governments to take immediate action to intervene in mental health issues among the public in the COVID-19 pandemic to avoid suicide-related deaths (69). In this paper, the following possible solutions and public health awareness methods have been discussed to prevent suicide among the public and healthcare workers, and Table 2 shows the impact of quarantine, isolation, lockdown, and social distancing (SWOT analysis).
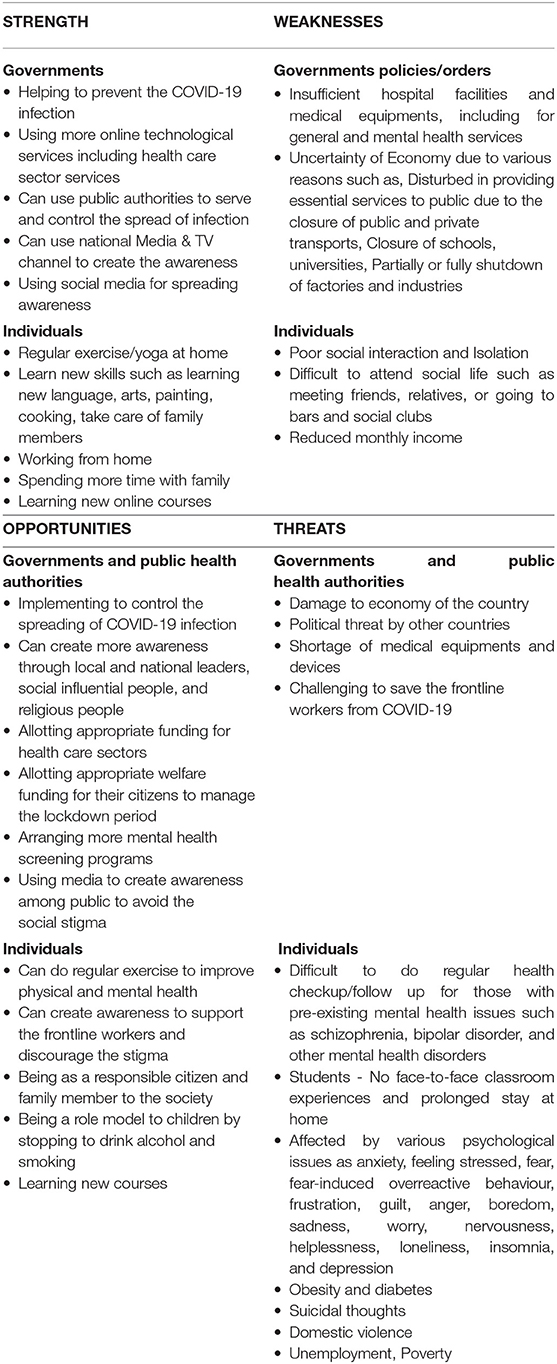
Table 2. SWOT: COVID-19 preventive measures (quarantine, isolation, lockdown, and social distancing) and mental health.
Recommendations and Suggestions for Social Stigma
Governments, media, the public, and individuals have an essential role to play to prevent the COVID-19-social stigma against ethnicities, religions, and specific countries. Media in particular should carefully select their topics when covering COVID-19 topics. Topics must be factual and respectful to avoid stigmatization, fear, and anxiety among the public. For example, certain words can be replaced by other words “people who have COVID-19” instead of “COVID-19 cases” and “people who may have COVID-19” instead of “COVID-19 suspects” and “suspected cases” (70). In addition, governments and public authority officials can request that celebrities, religious leaders, and leaders of specific regions spread facts about COVID-19 through social media platforms and TV channels. It would be helpful to reach out to the greatest number of people to reduce stress and anxiety among the public. Unfortunately, most healthcare workers have experienced social stigmatization from working with patients with COVID-19. To prevent the social stigmatization of healthcare professionals, showing support and making statements of gratitude on social media aimed at doctors and healthcare workers would increase recognition of their vital role in the community and reduce stigma.
Recommendations and Suggestions for Social Distancing, Quarantine, and Isolation
Prolonged social distancing and isolation, can impact both the physical and mental well-being of individuals, including healthy people. To avoid the stress, anxiety, depression, and other serious mental health issues, including suicidal ideas, individuals can attempt activity scheduling, such as reading, listening to music, learning, watching interesting TV programs, regular exercise (e.g., stretching and yoga), and learning a new language, instead of continuously watching live coverage of coronavirus-related news. For example, One World: Together At Home is a special broadcast curated by Lady Gaga in support of healthcare workers on the frontlines of the COVID-19 crisis, and this event also raised $128 million to support vaccine development and local and regional charities (71). Although social distancing requires the maintenance of physical space between people, people can contact their family members and friends by using various social apps like WhatsApp, FaceTime, Viber, Skype, Zoom, and Facebook messenger. In addition, this study suggests providing more online telehealth counseling services to the quarantined and isolated people as well as people who are recovering from coronavirus infection.
Recommendations for Preventing Alcohol-Addiction-Related Suicides
In this study, we have discussed the number of alcohol-dependence-related deaths during the lockdown period. Most individuals try to consume more alcohol to overcome social isolation, assuming that alcohol consumption will reduce their anxiety and stress during the lockdown period. However, alcohol consumption leads to many physical and mental health problems, including liver- and lung-related diseases, depression, anxiety, suicidal thoughts, and social and behavioral problems. In India, most alcohol-related deaths were associated with substance withdrawal syndrome. Therefore, not only quarantined people but also the individuals who have been admitted for COVID-19 care need to be screened for substance use withdrawal syndrome along with COVID-19 care. Also, there are a number of myths about consuming alcohol and COVID-19. Therefore, we suggest educating individuals and raise their awareness of the effect of alcohol consumption and circulate guidelines for avoiding suicide. We list the following topics as suggestions for content for governments policymakers and media to raise awareness among the public:
a. Drinking alcohol will not kill the virus and it will not help you develop immunity/resistance to coronavirus
b. Drinking alcohol will not help you cope with stress; in fact, it is likely to cause anxiety, depression, and other mental health disorders and vulnerable behaviors
c. Contact the local or national mental health counseling hotlines if you have any signs of alcohol use withdrawal syndrome
d. Local governments can support the individuals by providing food, medicine, subsidies, and more telehealth-hotline-based psychological intervention services to protect people from alcohol-related suicide deaths
e. Local governments should advertise telehealth-hotline-based psychological intervention services phone numbers through social media, television programs, and social influencers
f. Local governments should encourage individuals and family members to do regular yoga and exercises at home in this lockdown period
g. Avoid drinking alcohol in front of children to be a role model for the child
h. Provide more online telehealth services for alcohol-dependent people with pre-existing mental health issues
Recommendations and Suggestions for Unemployment, Economic Issues, and Suicide
Current worldwide suicide rates high compared to the previous economic recession of 2008. Recession triggers various kinds of stress and mental health issues among individuals due to unemployment, job loss, loan defaults, and government cuts to welfare and healthcare budgets. These financial difficulties will cause more recession-related mental health issues and suicide. To prevent pandemic-recession-related suicide, mental health experts and researchers have to raise awareness toward the governments and societies about an increasing unemployment rate being a risk factor for suicide. The pandemic is expected to bring about miserable outcomes; therefore, governments should implement programs to secure the basic needs of living for their citizens, waiving or extending loan payments, the healthcare and educational costs, and providing more online mental health services, including for inpatients in hospitals. In addition, the provision of more funding for mental health services and setting up more mental telehealth services in every hospital is necessary to control pandemic-related suicides. A previous study reported that two-thirds of suicides occurred among people who have lost their job within the year, and 50% of people committed suicide while they were employed (72). Therefore, early mental health intervention is essential to prevent suicide among both the working and non-working population now and in the future.
Recommendations and Suggestions for Supporting Healthcare Professionals
In this pandemic, healthcare professionals are more prone to stress and trauma due to dealing with COVID-19. There are a number of factors that cause this: long working hours, less sleep, isolatiton from one's family for long periods of time and worry about one's family's safety, lack of protective equipment, lack of testing kits, less-experienced new staffs, and facing discrimination and harassment from the public from fears due to working with COVID-19. Therefore, the national and local governments should ensure the safety of their healthcare workers by providing enough personal protective equipment and medical testing kits, issuing ordinances for harassment and discrimination, creating awareness among the public about the COVID-19 infection and the importance of healthcare workers, ensuring appropriate working hours with enough resting hours, and providing mental health services to the healthcare workers. Moreover, governments can ensure adequate compensation and healthcare services for healthcare professionals if they contracted COVID-19.
Physical Activity for Overall Physical and Mental Health
Physical activities will not only improve physical health but will also improve the psychological well-being of individuals (73–75). Previously, several studies have reported that physical activity can reduce sadness and suicidal intention (76, 77). The World Health Organization has recommended a required amount of physical activity per day or week for all age groups for people to stay healthy at home during the time of COVID-19. For example, adults aged over 18 years should do at least 150 min of physical activity per week (moderate intensity), and at least 60 min of moderate to vigorous physical activities per day has been recommended for children/adolescents between the age of 5 and 17 years. For children aged 1–5 years, should do at least 180 min/day of various types of physical activity (any intensity) (78). Therefore, we suggest that doing regular exercise or yoga at home is essential during this lockdown period to overcome mental health diseases, including suicide, depression, and anxiety disorders, and other chronic physical diseases, such as cerebrovascular diseases, obesity, and diabetes.
Prevention of Psychopathology During and After Lockdown
Early identification and prevention of causative factors for psychopathology is very essential to avoiding “second-pandemic”-related deaths. COVID-19 pandemic lockdown has been a psychopathological burden and has had a negative impact on the quality of life of the public, including school students and children, various kinds of frontline workers, people with pre-existing mental health issues, and the elderly population. Based on the previous literature, fear of COVID-19 is associated with anxiety, stress, and depression (79, 80). In a severe condition, psychopathological factors can lead to suicidal thoughts and attempts among those with pre-existing mental disorders.
The management of coronavirus fear and other factors is essential to prevent mental health issues, including suicide. The prevention strategies for fear are not only related to infection of COVID-19, the mental health intervention strategies and government policies should also be focused on various other factors, such as fear of contamination or loss of employment, pre-existing mental health issues, awareness of COVID-19 infection, awareness of social distancing and lockdown policies, social media news about the COVID-19, arrangement of online counseling sessions for students through their schools, telepsychiatry for isolated patients to alleviate their fear, anxiety, stress, and depression. In addition, government and mental health officers/hospital/service providers should closely work and monitor the services for people with pre-existing mental health issues. Otherwise, recurrence is more likely to occur in people with bipolar disorder and schizophrenia.
Strengths and Limitations
In our paper, we provide an overview of risk factors causing suicide and possible solutions to prevent suicide in this current COVID-19 pandemic. However, our study has several limitations. Firstly, our review study was conducted during the period of lockdown, i.e., up to May 2020. Secondly, there was no updated and functional suicide monitoring system data on the subject of implementing the lockdown, quarantine, and other social distancing procedures and their impact on mental health and suicide. Therefore, this study mostly used the search engine “Google” as an electronic database to search and analyze relevant information from the online and other media news.
Conclusion
The COVID-19 pandemic has traumatized the entire world physically, psychologically, emotionally, socially, and economically following the implementation of forced lockdown measures to prevent the spread of infection. Therefore, the local, regional, and national governments need to act quickly along with mental health providers to make new mental health policies and improve the availability of mental health services for everyone (people with COVID-19 infection, frontline workers, those in quarantine/isolation, people with preexisting mental health issues, students, and older adults) to prevent suicide due to the COVID-19 pandemic.
Author Contributions
BG and RT conceptualized and designed the study. BG, RT, AA-J, KF, PP, and SM analyzed the literature and wrote, revised, and approved the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARSCoV- 2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. doi: 10.1016/j.ijantimicag.2020.105924
2. World Health Organization. Director-General's Opening Remarks at the Media Briefing on COVID-19. World Health Organization (2020). Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 (accessed at: May 20, 2020).
3. Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. (2020) 369:m1375. doi: 10.1136/bmj.m1375
4. CDC. How COVID-19 Spreads. Centers for Disease Control and Prevention. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html (accessed at April 18, 2020).
5. WHO. Coronavirus Disease (COVID-19) Dashboard. World Health Organization. (2020). Available online at: https://covid19.who.int/ (accessed at: May 20, 2020).
6. Hoof EV. Lockdown is the World's Biggest Psychological Experiment - and We Will Pay the Price. (2020). Available online at: https://www.weforum.org/agenda/2020/04/this-is-the-psychological-side-of-the-covid-19-pandemic-that-were-ignoring/ (accessed at: April 20, 2020).
7. Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. COVID-19 suicide prevention research collaboration. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatr. (2020) 7:468–71. doi: 10.1016/S2215-0366(20)30171-1
8. Zortea TC, Brenna CT, Joyce M, McClelland H, Tippett M, Tran MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts: a systematic review. Crisis. (2020) 2020:1–14. doi: 10.1027/0227-5910/a000753
9. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. (2020) 113:707–12. doi: 10.1093/qjmed/hcaa202
10. John A, Okolie C, Eyles E, Webb RT, Schmidt L, McGuiness, et al. The impact of the COVID-19 pandemic on self-harm and suicidal behavior: a living systematic review. F1000Research. (2020) 9:1–25. doi: 10.12688/f1000research.25522.1
11. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. (2021) 5:229–38. doi: 10.1101/2020.08.30.20184168
12. John A, Pirkis J, Gunnell D, Appleby L, Morrissey J. Trends in suicide during the covid-19 pandemic. BMJ. (2020) 371:m4352. doi: 10.1136/bmj.m4352
13. Wang Y, Shi L, Que J, Lu Q, Liu L, Lu Z, et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatr. (2021) 22:1–10. doi: 10.1038/s41380-021-01019-y
14. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
15. Tognotti E. Lessons from the history of quarantine, from plague to influenza A. Emerg Infect Dis. (2013) 19:254–59. doi: 10.3201/eid1902.120312
16. Cetron M, Simone P. Battling 21st-century scourges with a 14th-century toolbox. Emerg Infect Dis. (2004) 10:2053–54. doi: 10.3201/eid1011.040797_12
17. Goh KT, Cutter J, Heng BH, Ma S, Koh BK, Kwok C. Epidemiology and control of SARS in Singapore. Ann Acad Med Singap. (2006) 35:301–16.
18. Hsieh YH, King CC, Chen CW, Ho M-S, Lee J-Y, Liu F-C, et al. Quarantine for SARS, Taiwan. Emerg Infect Dis. (2005) 11:278–82. doi: 10.3201/eid1102.040190
19. Cetron M, Landwirth J. Public health and ethical considerations in planning for quarantine. Yale J Biol Med. (2005) 78:325–30.
20. Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. (2020) 20:e102–7. doi: 10.1016/S1473-3099(20)30129-8
21. Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J Adv Res. (2020) 24:91–8. doi: 10.1016/j.jare.2020.03.005
22. Public Health Agency of Sweden: Quarantine and Lockdown. Available online at: https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/communicable-disease-control/COVID-19/quarantine-and-lockdown/ (accessed at: April 18, 2020).
23. Ramaprasad H. India has closed its railways for the first time in 167 years. Now trains are being turned into hospitals. CNN News. (2020). Available online at: https://edition.cnn.com/2020/04/05/asia/indian-railways-coronavirus-hospitals-intl-hnk/index.html (Accessed at: April 18, 2020).
24. Punemirrior. Maharashtra Goes Into Lockdown: Here's What You Can and Can't Do During This Time. (2020). Available online at: https://punemirror.indiatimes.com/maharashtra-goes-into-lockdown-heres-what-you-can-and-cant-do-during-this%20time/articleshow/74770654.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst (accessed at: April 18, 2020).
25. Times of India. Tamil Nadu police Book 39,000 for Section 144 Violation. (2020). Available online at: http://timesofindia.indiatimes.com/articleshow/74940489.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst (accessed at: April 18, 2020).
26. Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol infect. (2008) 136:997–1007. doi: 10.1017/S0950268807009156
27. Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J Psychiatr. (2020) 51:102073. doi: 10.1016/j.ajp.2020.102073
28. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. (2004) 10:1206–12. doi: 10.3201/eid1007.030703
29. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-A Perfect Storm? JAMA Psychiatr. (2020) 77:1093–4. doi: 10.1001/jamapsychiatry.2020.1060
30. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
31. Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. (2009) 374:315–23. doi: 10.1016/S0140-6736(09)61124-7
32. Cheung YT, Chau PH, Yip PS. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int J Geriatr Psychiatr. (2008) 23:1231–38. doi: 10.1002/gps.2056
33. Chan SM, Chiu FK, Lam CW, Leung PY, Conwell Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatr. (2006) 21:113–18. doi: 10.1002/gps.1432
34. Yip PS, Cheung YT, Chau PH, Law YW. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. (2010) 31:86–92. doi: 10.1027/0227-5910/a000015
35. Manzar MD, Albougami A, Usman N, Mamun MA. COVID-19 suicide among adolescents and youths during the lockdown: an exploratory study based on media reports. Preprints. (2020) 2020:2020080709. doi: 10.20944/preprints202008.0709.v1
36. Wiener CD, Moreira FP, Zago A, Souza LM, Branco JC, Oliveira JF, et al. Mood disorder, anxiety, and suicide risk among subjects with alcohol abuse and/or dependence: a population-based study. Braz J Psychiatry. (2018) 40:1–5. doi: 10.1590/1516-4446-2016-2170
37. Sher L, Cooper TB, Mann J, Oquendo MA. Modified dexamethasone suppression-corticotropin-releasing hormone stimulation test: a pilot study of young healthy volunteers and implications for alcoholism research in adolescents and young adults. Int J Adolesc Med Health. (2006) 18:133–8. doi: 10.1515/IJAMH.2006.18.1.133
38. Bayard M, Mcintyre J, Hill K, Woodside J. Alcohol withdrawal syndrome. Am. Family Physic. (2004) 69:1443–50.
39. India Today. Frustrated at Not Being Able to Get Liquor During Lockdown, 2 Commit Suicide in Karnataka. (2020). Available online at: https://www.indiatoday.in/india/story/frustrated-at-not-being-able-to-get-liquor-during-lockdown-2-commit-suicide-in-karnataka-1661060-2020-03-29# (accessed at: April 18, 2020).
40. Amid Coronavirus Lockdown States Across India Witness Surge in Suicide Cases Due to Alcohol Withdrawal Symptoms. (2020). Available online at: https://www.news18.com/news/india/amid-coronavirus-lockdown-states-across-india-witness-surge-in-deaths-due-to-alcohol-withdrawal-symptoms-2561191.html (accessed at: April 20, 2020).
41. In God's Own Country 1 Died of Covid-19 but 7 Commit Suicide After Alcohol Ban. (2020). Available online at: https://www.livemint.com/news/india/in-god-s-own-country-1-died-of-covid-19-but-7-commit-suicide-after-alcohol-ban-11585483376504.html (accessed at: April 20, 2020).
42. Jayakumar PB. Alcohol Non-Availability Kills More Than Coronavirus in Kerala; Foreign Liquor Served as 'Medicine'. (2020). Available online at: https://www.businesstoday.in/current/economy-politics/alcohol-non-availability-kills-more-than-coronavirus-in-kerala-foreign-liquor-served-as-medicine/story/399716.html (accessed April 20, 2020).
43. Lobo S. Unable to Get Liquor, 3 Men Die in Tamil Nadu After Drinking Paint and Varnish. (2020). Available online at: https://www.indiatoday.in/india/story/unable-to-get-liquor-3-men-die-in-tamil-nadu-after-drinking-paint-and-varnish-1663775-2020-04-06 (accessed at: April 20, 2020).
44. Gokul R. Three Alcoholics in TN Consume After Shave Lotion-Laced Soft Drinks, Two Die. (2020). Available online at: http://timesofindia.indiatimes.com/articleshow/74981848.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst (accessed at: April 20, 2020).
45. CDC. Reducing Stigma. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/reducing-stigma.html#t1 (accessed at: April 22, 2020).
46. UN News. Nearly Half of Global Workforce at Risk as Job Losses Increase Due to COVID-19: UN Labor Agency. (2020). Available online at: https://news.un.org/en/story/2020/04/1062792 (accessed at: May 10, 2020).
47. UN News. COVID-19: Impact Could Cause Equivalent of 195 Million Job Losses, Says ILO Chief. (2020). Available online at: https://news.un.org/en/story/2020/04/1061322 (accessed at: May 10, 2020).
48. ILO. COVID-19: Stimulating the Economy and Employment. ILO: As Job Losses Escalate, Nearly Half of Global Workforce at Risk of Losing Livelihoods. (2020). Available online at: https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_743036/lang--en/index.htm (accessed at: May 10, 2020).
49. Sharma YS. 27 Million Youth in Age Group of 20-30 Years Lost Jobs in April: CMIE. Economic Times (2020). Available online at: https://economictimes.indiatimes.com/news/economy/indicators/unemployment-rate-dips-to-23-97-data-from-cmie-shows/articleshow/75689370.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst (accessed at: May 15, 2020).
50. Janda M. Almost a Million Australians Out of Work Due to Coronavirus; RBA Tips Economy to Take 10pc Hit. ABC News. (2020). Available online at: https://www.abc.net.au/news/2020-05-05/almost-one-million-australians-lose-jobs-due-to-coronavirus/12215494 (accessed at: May 10, 2020).
51. Willms J. Coronavirus Update: Canada Unemployment Rate Jumps to 13%, But Numbers Even Worse Across the Border. The Globe and Mail: Canada (2020). Available online at: https://www.theglobeandmail.com/canada/article-coronavirus-update-canada-unemployment-rate-jumps-to-13-but-numbers (accessed at: May 10, 2020).
52. Kawohl W, Nordt C. (2020). COVID-19, unemployment, and suicide. Lancet Psychiatr. (2020) 7:389–90. doi: 10.1016/S2215-0366(20)30141-3
53. Boswell J. Los Angeles Suicide Hotline has Received Upwards of 1,500 Calls in March - 75 Times the Previous Month - Over Fears of Getting Coronavirus and Related Anxiety About Eviction, Inability to Pay Bills and Losing Loved Ones. Mailonline. (2020). Available online at: https://www.dailymail.co.uk/news/article-8169429/Los-Angeles-suicide-hotline-received-upwards-1-500-calls-coronavirus-fears.html (accessed at: May 10, 2020).
54. Ridler F. German State Finance Minister 'kills himself' 'in despair' Over Economic Effects of Coronavirus Crisis. (2020). Available online at: https://www.dailymail.co.uk/news/article-8164881/Death-German-finance-official-linked-virus-crisis.html. (accessed at: May 10, 2020).
55. Hindu News. Coronavirus Lockdown/Activists Say Over 300 Deaths Related to Lockdown Troubles. (2020). Available online at: https://www.thehindu.com/news/national/activists-say-over-300-deaths-related-to-lockdown-troubles/article31491525.ece. (accessed at: May 10, 2020).
56. Hoffart A, Johnson SU, Ebrahimi OV. Loneliness and social distancing during the COVID-19 pandemic: risk factors and associations with psychopathology. Front. Psychiatr. (2020) 11:589127. doi: 10.3389/fpsyt.2020.589127
57. Asmundson GJ, Paluszek MM, Landry CA, Rachor GS, McKay D, Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J Anxiety Disord. (2020) 74:102271. doi: 10.1016/j.janxdis.2020.102271
58. Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJG. Development and initial validation of the COVID stress scales. J Anxiety Disord. (2020) 72:102232. doi: 10.1016/j.janxdis.2020.102232
59. Lee SA, Crunk EA. Fear and psychopathology during the COVID-19 crisis: neuroticism, hypochondriasis, reassurance-seeking, and coronaphobia as fear factors. OMEGA-J Death Dying. (2020). doi: 10.1177/0030222820949350. [Epub ahead of print].
60. Alshehri FS, Alatawi Y, Alghamdi BS, Alhifany AA, Alharbi A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi Pharmaceutical J. (2020) 28:1666–73. doi: 10.1016/j.jsps.2020.10.013
61. Mamun MA, Chandrima RM, Griffiths MD. Mother and son suicide pact due to COVID-19-related online learning issues in Bangladesh: an unusual case report. Int J Ment Health Addict. (2020) 7:1–4. doi: 10.1007/s11469-020-00362-5
62. Petretto DR, Pili R. Ageing and COVID-19: what is the role for elderly people? Geriatrics. (2020) 5:25. doi: 10.3390/geriatrics5020025
63. Petterson S, Westfall J, Miller BF. Projected deaths of despair during the coronavirus recession. Well Being Trust. (2020) 8:2020. WellBeingTrust.org
64. Chiappini S, Guirguis A, John A, Corkery JM, Schifano F. COVID-19: The hidden impact on mental health and drug addiction. Front Psychiatr. (2020) 11:767. doi: 10.3389/fpsyt.2020.00767
65. Newman MG, Zainal NH. The value of maintaining social connections for mental health in older people. Lancet Public Health. (2020) 5:e12–3. doi: 10.1016/S2468-2667(19)30253-1
66. Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. (2015) 105:1013–9. doi: 10.2105/AJPH.2014.302427
67. Simon M. 75,000 Americans at Risk of Dying From Overdose or Suicide Due to Coronavirus Despair, Group Warns. CNN News (2020). Available online at: https://edition.cnn.com/2020/05/08/health/coronavirus-deaths-of-despair/index.html. (accessed at: May 10, 2020).
68. Ayling L. The Silent COVID-19 Death Toll: Far More Australians Will Kill Themselves Because of Coronavirus Lockdown Than Those Who Die of the Virus, Experts Say. (2020). Available online at: https://www.dailymail.co.uk/news/article-8293233/Far-people-Australia-predicted-die-suicide-coronavirus-lockdown.html (accessed at: May 10, 2020).
69. Ting V. Coronavirus: Suicide Experts Warn of Pandemic's Impact on Mental Health, With Hong Kong's Jobless, Poor, and Elderly Most at Risk. South China Morning Post (2020). Available online at: https://www.scmp.com/news/hong-kong/health-environment/article/3081582/coronavirus-suicide-experts-warn-pandemics-impact (accessed at: May 10, 2020).
70. UNICEF. Social Stigma Associated With the Coronavirus Disease (COVID-19). UNICEF. Available online at: https://www.unicef.org/documents/social-stigma-associated-coronavirus-disease-COVID-19 (accessed May 11, 2020).
71. Savage M. Coronavirus: Stars Take Part in One World: Together at Home Concert. (2020). Available online at: https://www.bbc.com/news/entertainment-arts-52333890 (accessed at: May 10, 2020).
72. Coope C, Donovan J, Wilson C, Barnes M, Metcalfe C, Hollingworth W, et al. Characteristics of people dying by suicide after job loss, financial difficulties and other economic stressors during a period of recession (2010–2011): a review of coroners? records. J Affect Disord. (2015) 183:98–105. doi: 10.1016/j.jad.2015.04.045
73. Asztalos M, Wijndaele K, De Bourdeaudhuij I, Philippaerts R, Matton L, Duvigneaud N, et al. Specific associations between types of physical activity and components of mental health. J Sci Med Sport. (2008) 12:468–74. doi: 10.1016/j.jsams.2008.06.009
74. Peluso MA, Andrade LH. Physical activity and mental health: the association between exercise and mood. Clinics. (2005) 60:61–70. doi: 10.1590/S1807-59322005000100012
75. Cho KO. Physical activity and suicide attempt of south Korean adolescents-evidence from the eight Korea youth risk behaviors web-based survey. J Sport Sci Med. (2014) 13:888–93.
76. Brosnahan J, Steffen LM, Lytle L, Patterson J, Boostrom A. The relation between physical activity and mental health among Hispanic and non-Hispanic white adolescents. Arch Pediatr Adolesc Med. (2004) 158:818–23. doi: 10.1001/archpedi.158.8.818
77. Vancampfort D, Hallgren M, Firth J, Rosenbaum S, Schuch FB, Mugisha J, et al. Physical activity and suicidal ideation: a systematic review and meta-analysis. J Affect Disord. (2018) 225:438–48. doi: 10.1016/j.jad.2017.08.070
78. WHO. Connecting the World to Combat Coronavirus: Healthy at Home. (2020). Available online at: https://www.who.int/news-room/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---physical-activity (accessed at: May 18, 2020).
79. Chen B, Sun J, Feng Y. How have COVID-19 isolation policies affected young people's mental health? –evidence from Chinese college students. Front Psychol. (2020) 11:1529. doi: 10.3389/fpsyg.2020.01529
Keywords: COVID-19, mental health, suicide, quarantine, lockdown, social distancing, isolation
Citation: Ganesan B, Al-Jumaily A, Fong KNK, Prasad P, Meena SK and Tong RKY (2021) Impact of Coronavirus Disease 2019 (COVID-19) Outbreak Quarantine, Isolation, and Lockdown Policies on Mental Health and Suicide. Front. Psychiatry 12:565190. doi: 10.3389/fpsyt.2021.565190
Received: 24 May 2020; Accepted: 17 March 2021;
Published: 16 April 2021.
Edited by:
Antonio Ventriglio, University of Foggia, ItalyReviewed by:
Junxiang Chen, University of Pittsburgh, United StatesHoang-Long Vo, Hanoi Medical University, Vietnam
Copyright © 2021 Ganesan, Al-Jumaily, Fong, Prasad, Meena and Tong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Raymond Kai-Yu Tong, kytong@cuhk.edu.hk; Adel Al-Jumaily, adel.al-jumaily@ieee.org; Balasankar Ganesan, balasankarganesan@cuhk.edu.hk
 Balasankar Ganesan
Balasankar Ganesan