- 1School of Health Sciences, Wuhan University, Wuhan, China
- 2Department of Psychiatry, Renmin Hospital of Wuhan University, Wuhan, China
- 3School of Nursing, University of Connecticut, Storrs, CT, United States
Objective: This study aimed to investigate the current status of depression self-management (DSM), and to identify influencing factors of DSM among Chinese community residents.
Methods: Stratified random sampling methodology was adopted in this cross-sectional survey. Respondents completed a collection of self-administered questionnaires
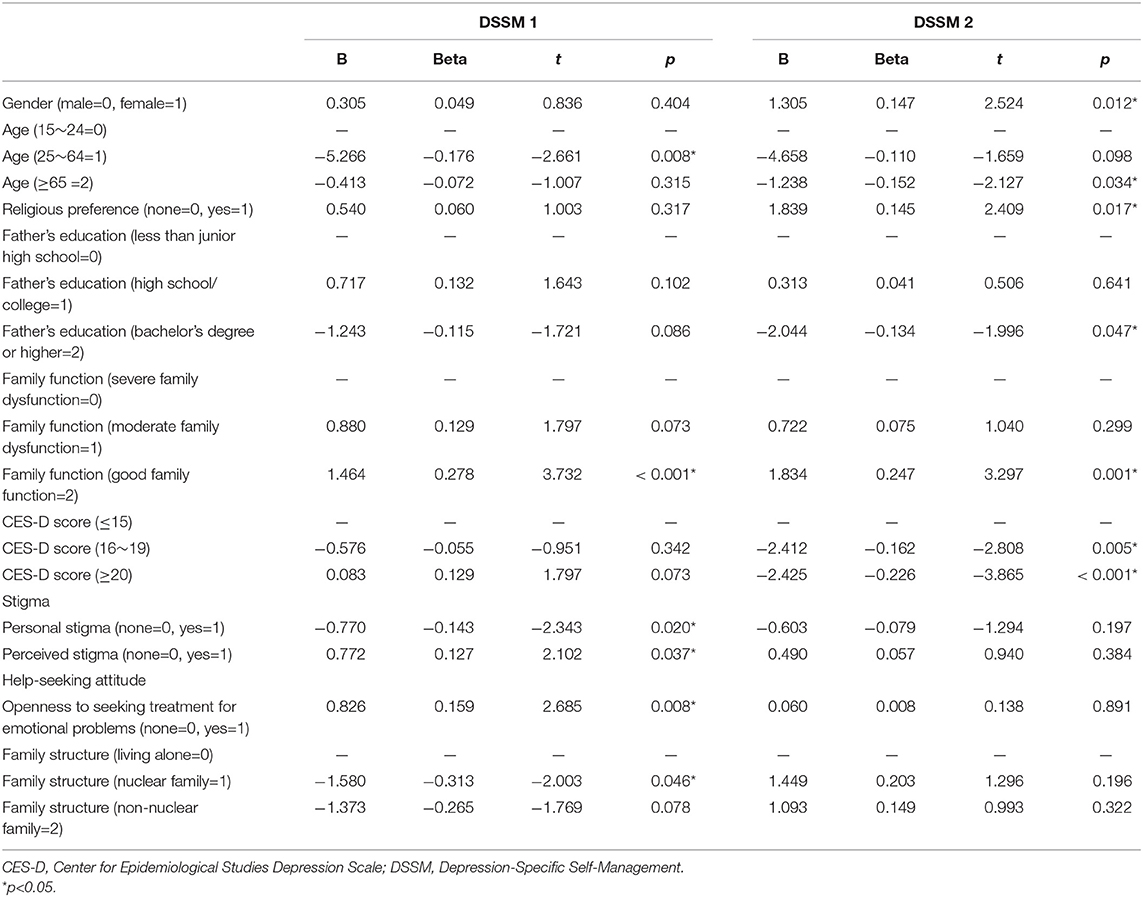
Results: The majority of participants were female (72.2%), having a mean age of 39 years (SD = 17.3). The total mean score on the DSSM was low (31.63 ± 4.69). Using multiple linear regression analysis, age ranging from 25 to 64 years old (Beta = −0.176, p = 0.008), having personal stigma (Beta = −0.143, p = 0.020) and perceived stigma (Beta = 0.127, p = 0.037), and having a nuclear family structure (Beta = −0.313, p = 0.046), good family function (Beta = 0.278, p < 0.001) and good help-seeking attitude (Beta = 0.159, p = 0.008) were associated with DSSM-knowledge. Older age (≥65 years) (Beta = −0.152, p = 0.034), higher CES-D scores (Beta = −0.162, p = 0.005), having a father with a bachelor's degree or higher level of education (Beta = −0.134, p = 0.047), being female (Beta = 0.147, p = 0.012), indicating a religious preference (Beta = 0.145, p = 0.017) and having good family function (Beta = 0.247, p = 0.001) were significantly associated with DSSM-activities.
Conclusions: Reducing stigma related to depression and enhancing help-seeking attitudes may be potential strategies for managing depressive symptoms among Chinese community residents.
Introduction
More than 300 million people world-wide have experienced depression, and close to 0.8 million people die each year due to depression-related suicide (1). The prevalence of depression among Chinese community residents is 6.9% (2), and only a few obtain get timely and effective treatment. The high morbidity, high disability and high suicide rates of depression result in great social burden (3). Considering the recurrent episodes and epidemiology, depression not only requires medication, but also requires self-management to prevent (4) and reduce relapse. Self-management (SM) may be a promising approach (5); it can reduce the cost of health services (6), and offer benefits to the health care system and society (7).
The concept of SM originated with a chronic disease self-management course (CDSMC) (8), and has been applied in a variety of fields related to health. “Self-management is about the methods, skills, and strategies we use to effectively manage our own activities toward achieving certain objectives” (9). It encompasses different dimensions, such as medication management (5, 10), symptom management, informational support, change in lifestyle, social support (10); role management and emotional management (5). It offers people alternatives and helps them to maintain longer-lasting health while reducing the risk of mental health deterioration (11).
Self-management has been shown to be effective among persons with chronic depression (12). Studies reported that SM can result in positive health outcomes (8). SM may relieve or prevent the occurrence of depressive symptoms among elderly adults (13), postpartum women (14) and persons with chronic illness comorbid depression (15–17). In addition to preventing depressive symptoms, SM of depression can increase an individual's self-efficacy and facilitate their quality of life (12).
At present, SM has been increasingly applied to the prevention of depression (18). However, Studies have focused on SM of clients diagnosed with depression (16, 17), whereas very limited studies investigated the level of depression self-management (DSM) among community residents. This results in the need to understand the status of DSM in community residents, such as their level of knowledge and activities being used.
There are a variety of factors that affect DSM, the key ones include stigma (19), family function (20, 21) and help-seeking attitude. As one of the important influencing factors of SM, stigma makes people feel different from others, which becomes a barrier for people to manage themselves (19). In addition, family members play an indispensable role in the achievement of DSM in many ways, such as medication reminders, getting individuals to appointments for medical treatment (20), providing emotional support (21), and improving an individual's self-confidence and actions (22). Another influence on SM is help-seeking attitude. An individual's effective DSM relies on timely and appropriate diagnosis and treatment of depression (23). These factors have a proven impact on DSM. However, there a paucity of research exploring the impact of these variables simultaneously on DSM among Chinese community residents.
This study aimed to investigate the current status of DSM, and to identify the barriers and facilitators to DSM among Chinese community residents. Findings of this study can assist in the development of DSM strategies, and enhance the quality of life of community residents with depressive symptoms. It is anticipated that stigma, family function, help-seeking attitudes and several socio-demographic factors have significant impact on DSM.
Methods
Study Design and Procedure
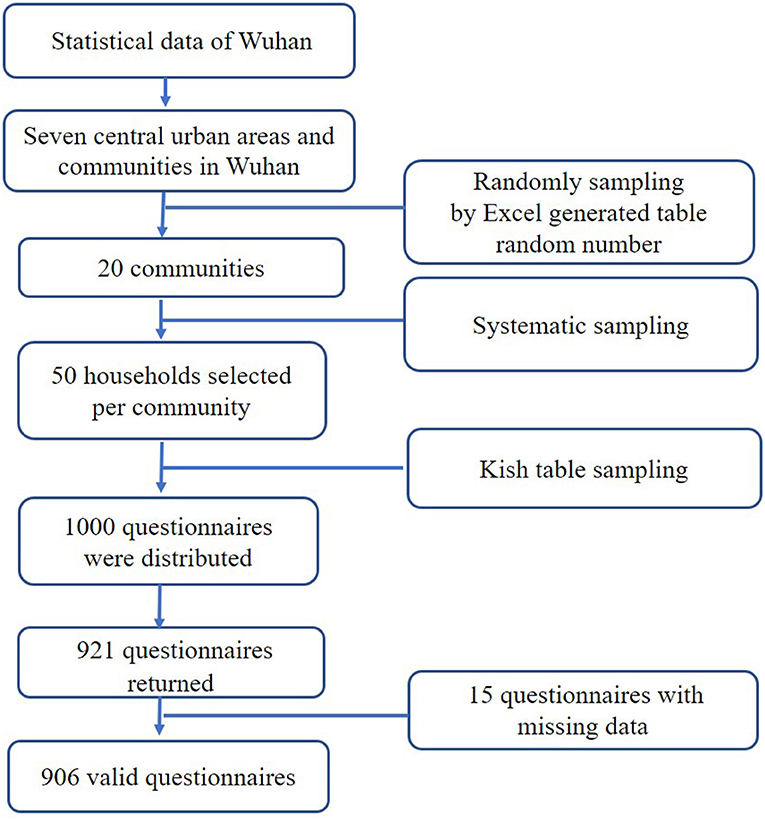
This research was a cross-sectional study which conducted in Wuhan, the capital city of Hubei Province in central China. With a population of about 10.7 million, Wuhan is considered to have an average economic base (24). Data were obtained from seven districts and communities. Stratified random sampling was used throughout the sampling process in the household study to select the target communities, households, and individuals. This sampling method ensured that individuals in the target population who met the requirements were equally likely to be included in the study (see Figure 1). Individuals from each family were selected using Kish table sampling method, and one of eight codes (A, B1, B2, C, D, E1, E2, F) was used to target households; each family member was coded based on the family registration form (including name, age, gender, member number).
Study Sample
The inclusion criteria were: age ≥ 15 years, and a minimum of primary school education and informed consent. Exclusion criteria were: severe physical illness; psychosis and related intellectual disability, dementia and mental disorders caused by abuse of psychoactive substances; and, severe cognitive impairment. These illnesses were screened in a review of medical records and confirmed by treating physicians. This research is part of a large cross-sectional survey (25), which recruited 2,000 samples. Due to limited grant funding, only some core indicators were included in the investigation of all 40 communities. We randomly selected 20 communities and investigated self-management of depression and other indicators. Therefore, the sample size of the current study is 1,000. In this study, G*power 3.1 was used to calculate the sample size based on pretest study results (Effect size = 0.22, α = 0.05, 1-β = 0.90), and the minimal sample size was 844. So, 1,000 participants meet the minimum sample size. A total of 1,000 questionnaires were distributed in this study; 921 questionnaires were returned (response rate: 92.1%) and 906 questionnaires were determined to be valid (effective callback rate: 90.6%).
Measures
Demographic Information
Demographic data was obtained from participants including gender, age, ethnicity, religious preference, education, father's education, mother's education, spouse's education, employment status, occupation, marital status, household income and family structure.
Depression-Specific Self-Management Questionnaire (DSSM)
Depression self-management of participants was self-reported using the Depression-Specific Self-Management Questionnaire (DSSM) which was developed by Ludman et al. (26) and later modified by Gensichen et al. (27). The DSSM consists of nine items with two subscales: the first four items evaluate the respondents' specific knowledge of depression, referred to as depression self-management knowledge (DSSM 1); and the following five items evaluate respondents' specific activities for improving depressive symptoms, referred to as depression self-management activities (DSSM 2). Each subscale uses a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree), or from 1 (never) to 5 (daily) (27). Total scores for DSSM 1 and DSSM 2 are calculated by the sum of each subscale item score, with a higher score representing greater DSSM 1 and DSSM 2. The total score is the sum of all items, ranging from nine to 45, the higher score indicates better self-management of depression. The DSSM, DSSM 1 and DSSM2 utilize 36, 16, and 20 as the critical values, respectively. The Cronbach's alpha coefficient of the DSSM was 0.725.
Center for Epidemiological Studies Depression Scale (CES-D)
The Center for Epidemiological Studies Depression Scale (CES-D) (28), a self-reported instrument, was used to assess participants' weekly depressive symptoms. It includes 20 items, and each item uses a 4-point scale ranging from 0 (no or hardly) to 3 (almost always) (29). The total score is 0 to 60. The higher the score, the more severe the depressive symptoms. A score of 15 or less is classified as no depressive symptoms in the past week; 16–19 indicates there may be depressive symptoms in the past week; and, a score of 20 or above indicates positive depressive symptoms in the last week. The Cronbach's α of the Chinese version was 0.9 (30). In the current study, the Cronbach's alpha coefficient was 0.93.
Family APGAR (Family Function)
Self-reported individual's satisfaction with family functioning was tested by the Family APGAR (31). It uses a 3-point Likert scale ranging from 0 (hardly ever) to 2 (almost always). The total score ranges from 0 to 10. The higher the score, the better the family function. More specifically, 0 to 3 represents severe family dysfunction, 4 to 6 represents moderate family dysfunction and 7 to 10 represents good family function. The Chinese version of the Family APGAR had a Cronbach's α of 0.86 (32). In the current study, Cronbach's α was 0.89.
Depression Stigma Scale (DSS)
The self-reported Depression Stigma Scale (DSS) (33, 34) is mainly used to investigate respondents' stigma toward depression. The DSS has 18 items with two subscales: DSS-Personal (a measure of the respondent's personal attitudes toward depression) and DSS-Perceived (a measure of the respondent's beliefs about the stigmatizing attitudes of others) (33). Each subscale consists of nine items using a 5-point Likert scale, ranging from 4 (strongly agree) to 0 (strongly disagree). In the Chinese version, the retest reliability for the DSS-Personal and DSS-Perceived scales were 0.90 and 0.73. The Cronbach's α for DSS-personal stigma and DSS-perceived stigma were 0.71 and 0.81, respectively.
Attitudes Toward Seeking Professional Psychological Help Scale-Short Form (ATSPPH-SF)
The self-reported ATSPPH-SF (35, 36) is mainly used to identify an individual's attitude toward seeking professional assistance. The scale has a total of 10 items using a 4-point Likert scale. The total score is 0-30 points. The higher the score, the better the help-seeking attitude. The scale has two dimensions: Openness to seeking treatment for emotional problems; Value and need in seeking treatment. The Chinese version had good reliability. Cronbach's alpha for the two dimensions were 0.757 and 0.643.
Data Collection
Permission for this study was obtained from the Institution Review Board of Wuhan University School of Medicine (identifier: 2019YF2032). All participants were provided with informed consent and participation was considered voluntary. Respondents could withdraw at any time without prejudice. Informed consent was obtained from the guardian of participants under the age of 18. Face-to-face interview was used by the investigators who were nursing professionals and uniformly trained. Each participant received a gift after completing the questionnaire. All completed questionnaires were considered confidential and stored in a secure location accessed only by the authors. Data collection occurred from January to December 2017.
Data Analysis
Data analysis was conducted using SPSS21.0 statistical software and a p value of 0.05 was considered statistically significant. Demographic characteristics were described by frequency, mean and standard deviation. The sample are tested by normality and kurtosis, showing a normal distribution. Correlation coefficient was used to analyze the correlation of continuous variables. Multiple linear regression analysis was used for analysis of influencing factors affecting DSM.
Results
Descriptive Data
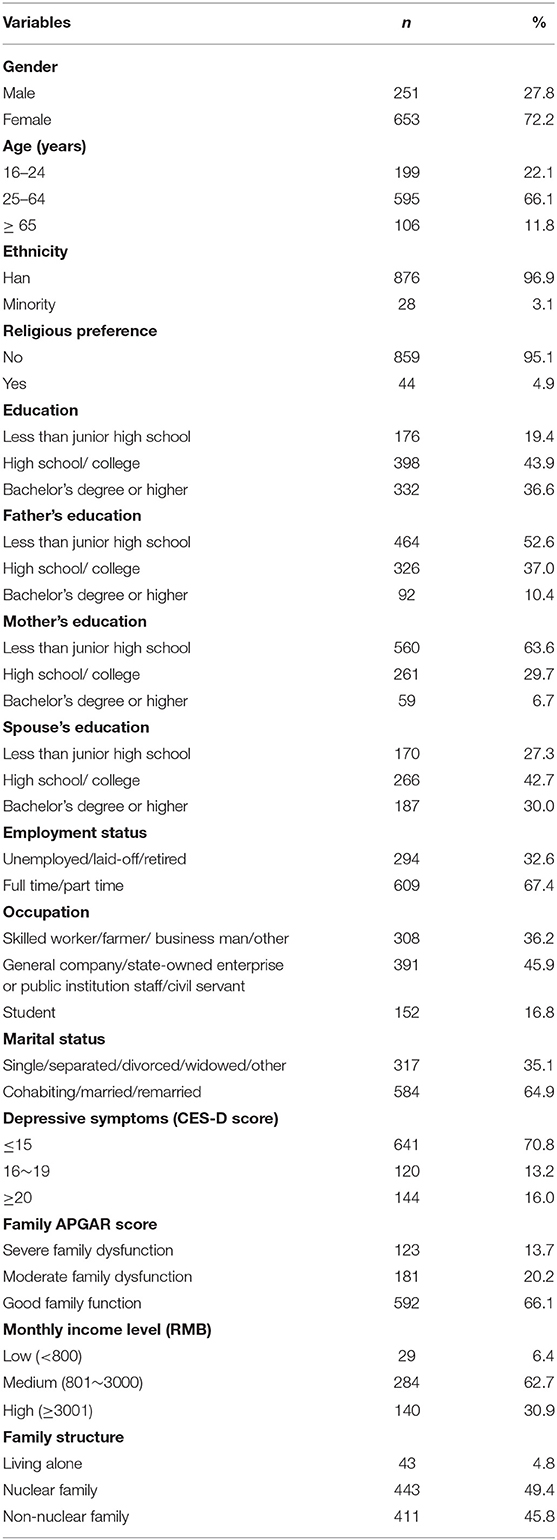
A total of 906 residents participated in the survey and the majority were female (72.2%) having a mean age of 39 years (SD = 17.3). In addition, the mean score of the CES-D was (12.0 ± 7.97). The mean personal stigma score of participants was (19.22 ± 5.05) and the mean perceived stigma score was (21.95 ± 5.03). The average score of help-seeking attitude on “openness” and “value and need” were 10.05 (SD = 3.74), 8.09 (SD = 3.52), respectively. Details of subjects' characteristics are shown in Table 1.
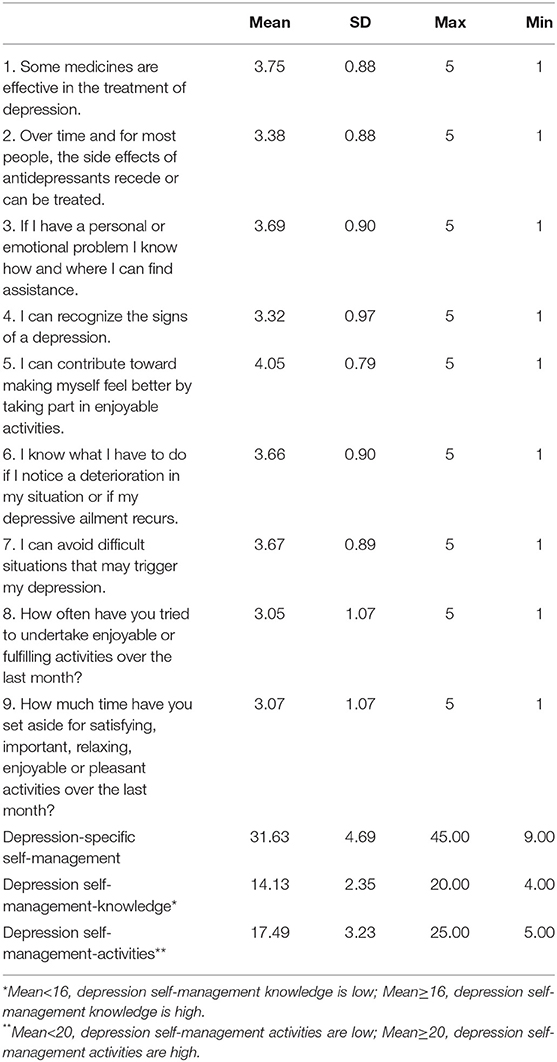
Scores of DSSM
Table 2 shows the current depression management strategies used by participants. The total mean score on the DSSM was <36 (31.63 ± 4.69). The score on DSSM 1 was (14.13 ± 2.35), and the score on DSSM 2 was (17.49 ± 3.23). The highest score (4.05 ± 0.79) was found related to participation in enjoyable activities (item # 5), followed by the use of medications (item # 1, 3.75 ± 0.88). The lowest score (3.05 ± 1.07) was related to item # 8 on the frequency of participation in enjoyable activities, and item # 9 which focused on time set aside for these activities (3.07 ± 1.07).
Correlation Analysis Between DSSM and Stigma, Help-Seeking Attitudes, CES-D and Family APGAR
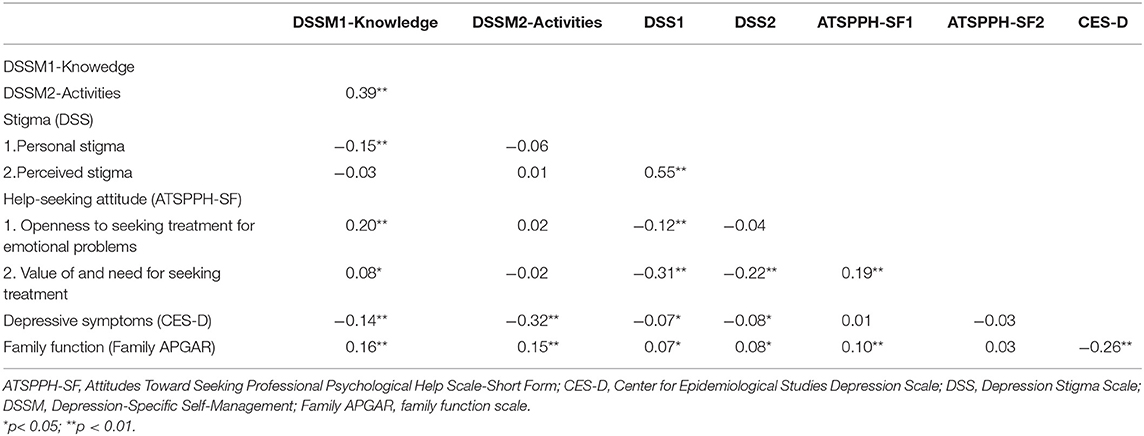
Correlation analysis indicated that both personal stigma and the CES-D score had a negative correlation with DSSM 1 (Pearson r = −0.15, p ≤ 0.001; Pearson r = −0.14, p ≤ 0.001) which is significant (see Table 3). Openness to seeking treatment for emotional problems (r = 0.20) and the value of and need for seeking treatment (r = 0.08) was positively correlated with DSSM 1. Scores on the CES-D (r = −0.32) and Family APGAR (r = 0.15) were significantly correlated with DSSM 2.
Influencing Factors on DSM
Using multiple linear regression analysis, influencing factors of DSM are shown in Table 4. The multiple linear regression models were statistically significant, FDSSM−knowledge = 3.039, p < 0.001, with a R-square value (R2) of 0.505; FDSSM−activities = 2.980, p < 0.001, R2 = 0.251. Findings indicate that age ranging from 25 to 64 years old (Beta = −0.176, p = 0.008), having personal stigma (Beta = −0.143, p = 0.020), and being in a nuclear family structure (Beta = −0.313, p = 0.046) were negatively associated with DSSM 1, while good family function (Beta = 0.278, p < 0.001) and good help-seeking attitude (Beta = 0.159, p = 0.008) were associated in a positive direction with DSSM 1. Older age (≥65 years) (Beta = −0.152, p = 0.034), higher CES-D scores (Beta = −0.162, p = 0.005), and father's bachelor or higher education level (Beta = −0.134, p = 0.047) were negatively associated with DSSM 2, while individuals being female (Beta = 0.147, p = 0.012), having a religious preference (Beta = 0.145, p = 0.017), and having good family function (Beta = 0.247, p = 0.001) were positively associated with DSSM 2.
Discussion
This study found that the level of DSSM was negative in Chinese community residents. Current study results are consistent with previous studies in Rawalpindi (37), Australia (38) with self-management knowledge on depression being negative among community residents in China. Globally, it appears that depression-related knowledge is lacking in the general population. In addition, it also reflects that the general population pays less attention to depression in China. This reinforces the need for healthcare providers to popularize the importance of knowledge about depression. Self-management activities on depression were also negative, which was another interesting finding of this study. Previous study showed that engaging in a variety of activities that suitable for ourselves contribute to better self-management (39). However, it is difficult to choose effective individualized self-management strategies use them consistently. The Internet and other electronic media resources allow for greater access to relevant information, but individuals may lack the initiative to utilize this information. In the face of avoiding complex interpersonal relationships, many people adopt a more solitary lifestyle, and this could contribute to this lack of initiative in engaging in self-management activities.
This study found that good family function was positively associated with DSM knowledge. This finding implied that family function and/or family support played an important role in DSM, which is consistent with a study by Polacsek (23). Family provides a supportive atmosphere for self-management of chronic illness (including depression). For instance, family members were crucial in providing practical support for individuals with mental health problems by offering medication reminders and promoting physical activities (21). Encouraged by their family, members seek diagnosis, receive treatment and take steps to better manage themselves (23). In addition, families provide emotional support for their members, reduce isolation and enhance members' autonomy in self-management (21, 40).
Families can also be a deterrent in promoting a family member's self-management behaviors (19). The results showed that having a father with a bachelor's degree or higher level of education was negatively associated with DSM activities. A family's lack of recognition of a member's illness and their prejudicial viewpoint against individuals with depression can aggravate the member's shame and hinder their SM (41, 42). Having a father with a higher level of education might lead to the father being focused on his occupational and social position, which results in less attention on family life, family members and their mental health. Thus, there may be an unwillingness on the part of the father to accept a family member having depression and helping to promote better strategies for self-management. Moreover, overprotection by the family of their member promotes low confidence in the individual's abilities and thus negatively affects their self-management strategies (43). The health problems of other family members can have competitive demands, and individuals are unable to focus on their own management (20).
Having a positive help-seeking attitude was also an important factor of DSM knowledge. Participants who were more open to seeking help (such as psychotherapy and psychological counseling) during an emotional crisis were noted to have better DSM knowledge. Having access to the health care system can also improve self-management abilities (23). Being willing to seek assistance and receiving practical guidance and feedback on SM from health care professionals promotes better self-management abilities (20).
Positively associated with DSM activities were included being female and having a religious preference. Women are more likely to participate in activities to improve depressive symptoms than men which is consistent with a previous study of persons having depression (44). An interesting finding in this study was that having a religious preference had a significant impact on DSM activities. Similarly, studies by Park (45) showed that individuals who had religious beliefs are more likely to manage depressive symptoms effectively. Religion not only provides spiritual support for individuals, but also offers an opportunity for the individual to have a helpful relationship with others who share their religious beliefs. This form of support plays a solid role in a person's self-management abilities (46).
More depressive symptoms were negatively associated with DSM activities. This is supported by other research that has shown that people were less likely to access self-management information when experiencing severe depressive symptoms (47). A probable explanation is that an individual with major depressive disorder experiences symptoms such as reduced energy (48), lack of interest (49) and motivation (46), which may hinder their effective use of enjoyable activities (50). Cognition may be distorted and the individual can experience a sense of shame that hinders self-management. And, in turn, DSM could improve depressive symptoms (11). Providing support to people with severe depression increases their self-efficacy and enhances self-management behaviors (11, 27).
In the current study, community residents who had higher perceived stigma were more likely to have better knowledge, and people who had higher personal stigma were less likely to have better self-management knowledge. This is supported by another study which found that stigma (perceived stigma) was a motivator of self-management (20). Research has shown that in order to avoid shame, individuals who seek to improve their knowledge of depression and mental health literacy also enhance self-management abilities (20, 23). However, stigma (personal stigma) was also reported to have a negative impact on self-management abilities (23). Stigma prevents respondents from receiving any information about depression, and lack of knowledge of DSM was a barrier to conducting self-management behaviors (19).
Stigma and help-seeking attitude were significantly correlated. Stigma may be one of the barriers to seeking help (51, 52). Participants who had higher stigma were less reluctant to seek help (23), in addition, some non-mental health professionals had higher stigma toward mental disorders and want to keep distance from such people (53), which hindered their ability to meet personal needs. People who are open to seeking help have access to health care resources to develop their health-related literacy, thereby improving their self-management abilities (54) and reducing stigma (52). In addition, both stigma and help-seeking attitude have proven to have a significant impact on DSM. Therefore, these factors should be taken into account when providing effective strategies or interventions to promote self-management and prevent depression.
Study Limitations and Implications
Limitations to this research study have been identified. This was a cross-sectional survey, which could not explain the causal relationship between influencing factors and dependent variables. In addition, the nature of voluntary participation may lead to potential selection bias. This study was done in central China, which limits generalization of findings to other geographic regions. There was a gender imbalance in the sample, the gender imbalance in the sample may influence the representative of the population. While there are limitations, the findings have important implications for future research and practice: it was found that individuals with severe depressive symptoms were less likely to engage in DSM which indicates that greater efforts should be placed on early screening and intervention. In addition, health care providers could be encouraged to address the issue of stigma. This can include educating community residents about depression by providing handouts and educational materials such as videos, flyers and posters at community health centers. To address the issue of improving help-seeking attitude related to DSM, more attention needs to be paid to the use of motivational interviewing to enhance awareness of and the advantages of DSM. Further research could explore the mediating effect between the variables included in this study and the DSSM.
Conclusions
Findings of this study indicate that Chinese community residents had a relative low level of using DSM. Reducing stigma related to depression and enhancing help-seeking attitudes may be potential strategies for managing depressive symptoms and improving the quality of life of Chinese community residents.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institution Review Board of Wuhan University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BXY, SL, XG, and XQW designed the study and wrote the research protocol. SL, BXY, XG, JC, ZCL, JZ, and XQW did the literature review, managed the field survey, quality control, and statistical analysis and prepared the manuscript draft. XQW, JZ, BXY, and JC contributed to the revisions in depth for the manuscript. ZCL, BXY, XQW, and JC supervised the survey and checked the data. All authors contributed to and approved the final manuscript.
Funding
We appreciate the grant support from the National Key R&D Program of China (2018YFC1314600), Hubei Health and Family Planning Commission Research Fund (LHHL2020YB-11), Project of Humanities and Social Sciences of the Ministry of Education in China (20YJCZH204), Wuhan Health and Family Planning Commission Research Fund (WX17B16), Fundamental Research Funds for the Central Universities and the National Natural Science Foundation of China (71503192).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Sincere thanks are given to Dr. Sharon R. Redding (EdD, RN, CNE), Dr. Yingchun Zeng (the Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China) for assistance in editing.
References
1. World Health Organization. Depression-Facet Sheet (2018). Available online at: https://www.who.int/en/news-room/fact-sheets/detail/depression (accessed September 10, 2019).
2. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiat. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
3. Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. (2013) 10:e1001547. doi: 10.1371/journal.pmed.1001547
4. Van Zoonen K, Buntrock C, Ebert DD, Smit F, Reynolds CF, Beekman AT, et al. Preventing the onset of major depressive disorder: a meta-analytic review of psychological interventions. Int J Epidemiol. (2014) 43:318–29. doi: 10.1093/ije/dyt175
5. Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. (2003) 26:1–7. doi: 10.1207/S15324796ABM2601_01
6. Trappenburg J, Jonkman N, Jaarsma T, van Os-Medendorp H, Kort H, de Wit N, et al. Self-management: one size does not fit all. Patient Educ Couns. (2013) 92:134–7. doi: 10.1016/j.pec.2013.02.009
7. Sassen B. Patient Education and Improving Patients' Self-Management. Nursing: Health Education and Improving Patient Self-Management. Cham: Springer International Publishing (2018). p. 141–234.
8. Jones S, Deville M, Mayes D, Lobban F. Self-management in bipolar disorder: the story so far. J Ment Health. (2011) 20:583–92. doi: 10.3109/09638237.2011.600786
9. Mental Health Foundation. Self-Management Of Mental Ill-Health Available online at: https://www.mentalhealth.org.uk/a-to-z/s/self-management-mental-ill-health (accessed September 22, 2019).
10. Barlow J, Wright C, Sheasby J, Turner A, Hanisworth J. Self-management approaches for people with chronic conditions:a review. Patient Educ Couns. (2002) 48:177–87. doi: 10.1016/S0738-3991(02)00032-0
11. Houle J, Gascon-Depatie M, Belanger-Dumontier G, Cardinal C. Depression self-management support: a systematic review. Patient Educ Couns. (2013) 91:271–79. doi: 10.1016/j.pec.2013.01.012
12. Hagerty BM, Bathish MA. Testing the relationship between a self-management intervention for recurrent depression and health outcomes. Appl Nurs Res. (2018) 44:76–81. doi: 10.1016/j.apnr.2018.10.001
13. Cramm JM, Hartgerink JM, de Vreede PL, Bakker TJ, Steyerberg EW, Mackenbach JP, et al. The relationship between older adults' self-management abilities, well-being and depression. Eur J Ageing. (2012) 9:353–60. doi: 10.1007/s10433-012-0237-5
14. Mao HJ, Li HJ, Chiu H, Chan WC, Chen SL. Effectiveness of antenatal emotional self-management training program in prevention of postnatal depression in Chinese women. Perspect Psychiatr Care. (2012) 48:218–24. doi: 10.1111/j.1744-6163.2012.00331.x
15. Kidd T, Carey N, Mold F, Westwood S, Miklaucich M, Konstantara E, et al. A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life. PLoS ONE. (2017) 12:e0185931. doi: 10.1371/journal.pone.0185931
16. Lee MC, Wu SV, Hsieh NC, Tsai JM. Self-management programs on eGFR, depression, and quality of life among patients with chronic kidney disease: a meta-analysis. Asian Nurs Res (Korean Soc Nurs Sci). (2016) 10:255-262. doi: 10.1016/j.anr.2016.04.002
17. Musekamp G, Bengel J, Schuler M, Faller H. Improved self-management skills predict improvements in quality of life and depression in patients with chronic disorders. Patient Educ Couns. (2016) 99:1355–61. doi: 10.1016/j.pec.2016.03.022
18. Driver SJ, Froehlich-Grobe K, Sanches KD. Self-management interventions to prevent depression in people with mobility limitations. Rehabil Process Outcome. (2016) 5:RPO.S39720. doi: 10.4137/RPO.S39720
19. Blixen CE, Kanuch S, Perzynski AT, Thomas C, Dawson NV, Sajatovic M. Barriers to self-management of serious mental illness and diabetes. Am J Health Behav. (2016) 40:194–204. doi: 10.5993/AJHB.40.2.4
20. Schulman-Green D, Jaser SS, Park C, Whittemore R. A metasynthesis of factors affecting self-management of chronic illness. J Adv Nurs. (2016) 72:1469–89. doi: 10.1111/jan.12902
21. Whitehead L, Jacob E, Towell A, Abu-Qamar M, Cole-Heath A. The role of the family in supporting the self-management of chronic conditions: a qualitative systematic review. J Clin Nurs. (2018) 27:22–30. doi: 10.1111/jocn.13775
22. Stamp KD, Dunbar SB, Clark PC, Reilly CM, Gary RA, Higgins M, et al. Family partner intervention influences self-care confidence and treatment self-regulation in patients with heart failure. Eur J Cardiovasc Nurs. (2015) 15:317–27. doi: 10.1177/1474515115572047
23. Polacsek M, Boardman GH, McCann TV. Factors influencing self-management of depression in older adults: a qualitative study. Aging Ment Health. (2019) 24:939–46. doi: 10.1080/13607863.2018.1562538
24. Wuhan Statistic Bureau. Wuhan Statistical Yearbook 2017. Beijing: China Statistics Press (2017).
25. Fang S, Wang XQ, Yang BX, Liu XJ, Morris DL, Yu SH. Survey of Chinese persons managing depressive symptoms: help-seeking behaviours and their influencing factors. Compr Psychiatry. (2019) 95:152127. doi: 10.1016/j.comppsych.2019.152127
26. Ludman E, Katon W, Bush T, Rutter C, Lin E, Simon G, et al. Behavioural factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychol Med. (2003) 33:1061–70. doi: 10.1017/S003329170300816X
27. Gensichen J, Petersen JJ, Karroum T, Rauck S, Ludman E, Konig J, et al. Positive impact of a family practice-based depression case management on patient's self-management. Gen Hosp Psychiatry. (2011) 33:23–8. doi: 10.1016/j.genhosppsych.2010.11.007
28. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
29. Winkensa LHH, Strien Tv, Brouwer IA, Penninx BWJH, Visser M, Lähteenmäki L. Associations of mindful eating domains with depressive symptoms and depression in three european countries. J Affect Disord. (2018) 228:26–32. doi: 10.1016/j.jad.2017.11.069
30. Zhang J, Wu Z, Fang G, LI J, Han BX, Chen ZY, et al. Development of the Chinese age norms of CES-D in urban area. Chin Ment Health J. (2010) 24:139–43. doi: 10.3969/j.issn.1000-6729.2010.02.015
31. Smilkstein G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. (1978) 6:1231.
32. Yang T, Tong Y, Yin X, Lu Z, Gong Y. Evaluation of morisky medication adherence scale and family APGAR applied to patients with tuberculosis. Chin J Soc Med. (2016) 33:580–2. doi: 10.4269/ajtmh.17-0383
33. Griffiths KM. Effect of web-based depression literacy and cognitive–behavioural therapy interventions on stigmatising attitudes to depression randomised controlled trial. Br J Psychiatry. (2004) 185:342–9. doi: 10.1192/bjp.185.4.342
34. Griffiths KM, Christensen H, Jorm AF. Predictors of depression stigma. BMC Psychiatry. (2008) 8:25. doi: 10.1186/1471-244X-8-25
35. Fischer EH, Farina A. Attitudes toward seeking professional psychology help: a shortened form and considerations for research. J Coll Stud Dev. (1995) 36:368–73. doi: 10.1037/t05375-000
36. Komiya N, Good GE, Sherrod NB. Emotional openness as a predictor of college students' attitudes toward seeking psychological help. J Couns Psychol. (2000) 47:138–43. doi: 10.1037/0022-0167.47.1.138
37. Jafri MA, Minhas FA, Tamiz-ud-Din, Slatch MA, Mujeeb F. Knowledge of depression among community members and health care providers in two selected areas of district Rawalpindi. J Col Physicians Surg Pak. (2011) 21:756–9.
38. Reavley NJ, Jorm AF. Recognition of mental disorders and beliefs about treatment and outcome: findings from an Australian national survey of mental health literacy and stigma. Aust N Z J Psychiatry. (2011) 45:947–56. doi: 10.3109/00048674.2011.621060
39. Chambers E, Cook S, Thake A, Foster A, Shaw S, Hutten R, et al. The self-management of longer-term depression: learning from the patient, a qualitative study. BMC Psychiatry. (2015) 15:172. doi: 10.1186/s12888-015-0550-6
40. Martinez I, Interian A, Guarnaccia P. Antidepressant adherence among Latinos: the role of the family. Qual Res Psychology. (2012) 10:63–85. doi: 10.1080/14780887.2011.586102
41. Corrigan PW, Bink AB, Fokuo JK, Schmidt A. The public stigma of mental illness means a difference between you and me. Psychiatry Res. (2015) 226:186–91. doi: 10.1016/j.psychres.2014.12.047
42. Y-Garcia EF, Duberstein P, Paterniti DA, Cipri CS, Kravitz RL, Epstein RM. Feeling labeled, judged, lectured, and rejected by family and friends over depression: cautionary results for primary care clinicians from a multi-centered, qualitative study. BMC Fam Pract. (2012) 13:64. doi: 10.1186/1471-2296-13-64
43. Ahola AJ, Groop PH. Barriers to self-management of diabetes. Diabet Med. (2013) 30:413–20. doi: 10.1111/dme.12105
44. Musil CM, Givens SE, Jeanblanc AB, Zauszniewski JA, Warner CB, Toly VB. Grandmothers and self-management of depressive symptoms. Arch Psychiatr Nurs. (2017) 31:234–40. doi: 10.1016/j.apnu.2016.11.008
45. Park S, Jang H, Furnham A, Jeon M, Park SJ. Beliefs about the causes of and treatments for depression and bipolar disorder among South Koreans. Psychiatry Res. (2018) 260:219–26. doi: 10.1016/j.psychres.2017.11.050
46. Coventry P A, Fisher L, Kenning C, Bee P, Bower P. Capacity, responsibility, and motivation: a critical qualitative evaluation of patient and practitioner views about barriers to self-management in people with multimorbidity. BMC Health Serv Res. (2014) 14:536. doi: 10.1186/s12913-014-0536-y
47. McCusker J, Lambert S D, Haggerty J, Yaffe MJ, Belzile E, Ciampi A. Self-management support in primary care is associated with improvement in patient activation. Patient Educ Couns. (2019) 102:571–77. doi: 10.1016/j.pec.2018.10.026
48. Bell RA, Andrews JS, Arcury TA, Snively BM, Golden SL, Quandt SA. Depressive symptoms and diabetes self-management among rural older adults. Am J Health Behav. (2010) 34:36. doi: 10.5993/AJHB.34.1.5
49. Schinckus L, Dangoisse F, Van den Broucke S, Mikolajczak M. When knowing is not enough: emotional distress and depression reduce the positive effects of health literacy on diabetes self-management. Patient Educ Couns. (2018) 101:324–30. doi: 10.1016/j.pec.2017.08.006
50. Theeke L, Carpenter RD, Mallow J, Theeke E. Gender differences in loneliness, anger, depression, self-management ability and biomarkers of chronic illness in chronically ill mid-life adults in Appalachia. Appl Nurs Res. (2019) 45:55–62. doi: 10.1016/j.apnr.2018.12.001
51. Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry. (2006) 40:51–4. doi: 10.1080/j.1440-1614.2006.01741.x
52. Grant JB, Bruce CP, Batterham PJ. Predictors of personal, perceived and self-stigma towards anxiety and depression. Epidemiol Psychiatr Sci. (2016) 25:247–54. doi: 10.1017/S2045796015000220
53. Wu Q, Luo X, Chen S, Qi C, Yang W, Liao Y, et al. Stigmatizing attitudes towards mental disorders among non-mental health professionals in six general hospitals in Hunan Province. Front Psychiatry. (2020) 10:946. doi: 10.3389/fpsyt.2019.00946
Keywords: depression, self-management, stigma, self-help seeking, Chinese residents
Citation: Liu S, Yang BX, Gong X, Chen J, Liu Z, Zhang J and Wang XQ (2021) Prevalence and Influencing Factors of Depression Self-Management Among Chinese Community Residents: A Cross-Sectional Study. Front. Psychiatry 12:559844. doi: 10.3389/fpsyt.2021.559844
Received: 07 May 2020; Accepted: 06 April 2021;
Published: 07 May 2021.
Edited by:
Ricardo Gusmão, University of Porto, PortugalReviewed by:
Man Ye, Central South University, ChinaPedro Morgado, University of Minho, Portugal
Victoria Soto-Sanz, Miguel Hernández University of Elche, Spain
Copyright © 2021 Liu, Yang, Gong, Chen, Liu, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongchun Liu, emNsaXU2JiN4MDAwNDA7d2h1LmVkdS5jbg==; Jun Zhang, MDAwMzAwNDUmI3gwMDA0MDt3aHUuZWR1LmNu; Xiao Qin Wang, eGlhb3Fpbl93YW5nNzgmI3gwMDA0MDsxNjMuY29t
†These authors share first authorship
 Shuo Liu
Shuo Liu Bing Xiang Yang
Bing Xiang Yang Xuan Gong2†
Xuan Gong2† Jie Chen
Jie Chen Zhongchun Liu
Zhongchun Liu Xiao Qin Wang
Xiao Qin Wang