- 1Department of Psychology, Catholic University Eichstaett-Ingolstadt, Eichstaett, Germany
- 2Faculty of Applied Healthcare Science, Deggendorf Institute of Technology, Deggendorf, Germany
- 3Department of Psychosomatic Medicine and Psychotherapy, University of Leipzig, Leipzig, Germany
- 4Department of Clinical Psychology and Psychotherapy, Philipps-University of Marburg, Marburg, Germany
- 5Department of Clinical Psychology and Psychotherapy, Institute of Psychology, Goethe University, Frankfurt, Germany
Present-centered therapy (PCT) was originally developed as a strong comparator for the non-specific effects of psychotherapy in the treatment of posttraumatic stress disorder. PCT qualifies as a not strictly supportive treatment as it is structured and homework is assigned between sessions. It does not focus on cognitive restructuring or exposure. A growing body of literature supports its beneficial effects. For example, it demonstrated only slightly inferior effect sizes and lower dropout rates compared to that of trauma-focused cognitive behavioral therapy in several trials with patients suffering from posttraumatic stress disorder. The current study is the first to evaluate the feasibility and the treatment effects of PCT in adults with prolonged grief disorder (PGD). Meta-analyses on psychotherapy for PGD have yielded moderate effect sizes. N = 20 individuals suffering from PGD were treated with PCT by novice therapists as part of a preparation phase for an upcoming RCT in an outpatient setting. Treatment consisted of 20–24 sessions á 50 min. All outcomes were assessed before treatment, at post-treatment, and at the 3-month follow-up. The primary outcome, PGD symptom severity, was assessed using the Interview for Prolonged Grief-13. Secondary outcomes were self-reported PGD severity, depression, general psychological distress, and somatic symptom severity. Furthermore, therapists evaluated their experiences with their first PCT patient and the treatment manual. In intent-to-treat analyses of all patients we found a significant decrease in interview-based PGD symptom severity at post-treatment (d = 1.26). Decreases were maintained up to the 3-month follow-up assessment (d = 1.25). There were also significant decreases in self-reported PGD symptoms, depression, and general psychological distress. No changes were observed for somatic symptoms. The completion rate was 85%. Therapists deemed PCT to be a learnable treatment program that can be adapted to the patient's individual needs. The preliminary results of PCT as a treatment for PGD demonstrate large effects and indicate good feasibility in outpatient settings. The treatment effects were larger than those reported in meta-analyses. Thus, PCT is a promising treatment for PGD. Possible future research directions are discussed.
Introduction
Prolonged grief disorder (PGD) has emerged as a well-defined mental disorder, distinguishable from major depression and posttraumatic stress disorder (PTSD) or other stress-related disorders (1). It has now been included in the ICD-11 (2), with slightly different criteria to those of its counterpart in the DSM-5, the “persistent complex bereavement disorder” (3). Earlier concepts of PGD encompassed complicated or traumatic grief [e.g., (4, 5)]. The core symptoms of all concepts are intense yearning and preoccupation with the deceased; reactive distress symptoms, such as feeling stunned or shocked by the loss; avoidance of reminders of the reality of the loss and emotional numbing, and finally social/identity disruption, for instance feeling detached or finding it difficult to trust others (6). The symptoms and impairment have to persist for more than 6 months after the death of a significant other.
PGD rates have varied considerably across studies due to methodological heterogeneity, sample demographic features, and loss-related characteristics. While a recent meta-analysis has found that 1 in 10 bereaved adults following non-violent death of a loved one suffer from PGD (7), representative studies report lower prevalences [e.g., 7% conditional prevalence in (8)]. Higher prevalences are associated with unnatural losses, with nearly half of the bereaved persons experiencing PGD (9). PGD has been found to be associated with both psychological and physical morbidity, such as impaired quality-of-life (10), increased risk of comorbid disorders with high rates of depression, PTSD, and anxiety disorders (11), increased suicidality (12) and deteriorated health (13). The negative consequences of PGD indicate a need for efficacious treatments. Still, there are relatively few controlled studies examining psychological treatments for PGD. Boelen and Smid (14) list three recommended psychological therapies that have been tested in at least two independent and controlled studies, including “complicated grief treatment” [including elements of exposure, cognitive restructuring, and interpersonal therapy; (15–17)], cognitive behavioral therapy [CBT; combining exposure and cognitive interventions; (18, 19)], and internet-based CBT [encompassing exposure, cognitive interventions, and behavioral activation applied using writing assignments; (20, 21)].
Meta-analyses on the treatment of complicated, traumatic or prolonged grief yielded effect sizes (ESs) for grief outcomes between 0.53 for those with clinically relevant symptoms (22), 0.53 for those undergoing psychotherapy (23), and 0.45 overall, and 0.58, when only considering those treated who were minimally 6 months post-loss (24). The respective ESs for depressive symptoms ranged between 0.16 (22) and 0.35 (24). ESs for general mental distress were reported as small [d = 0.26 in (24)]. In recent reviews (14, 24) on PGD treatment research, it was found that most interventions were grief-specific approaches and used exposure, cognitive restructuring, behavioral activation, and elements of interpersonal therapy. The authors also state that there are too few randomized controlled trials (RCTs) with active controls and that dismantling studies are missing. Consequently, no conclusions can be drawn about the active ingredients of successful treatment manuals.
Present-Centered Therapy [PCT; (25)] was originally developed as a strong comparator for the non-specific effects of psychotherapy in the treatment of PTSD. The goals of PCT are to enhance interpersonal connectedness, improve patients' insight into their current symptoms, and promote a greater sense of mastery via use of effective approaches to solving problems. Therefore, it involves empathic listening and support from the therapist as well as the basic components of behavioral therapy, namely education about the links between symptoms and daily problems, and the fostering of problem-solving skills, including homework exercises. The treatment is provided within the context of intentionally compassionate and helpful acts of the therapist based on client-centered principles like offering empathy, unconditional positive regard and congruence and is led by the individual daily stressors and problems the patient presents. PCT excludes specific trauma-focused components (i.e., exposure, cognitive restructuring of dysfunctional beliefs, stress inoculation training), and therefore seems to choose an alternative approach to address avoidance: by actively dealing with the current problems that may have arisen as a result of the traumatic event, but without engaging emotionally with the traumatic event itself.
In an older meta-analysis based on five RCTs, PCT showed good results in PTSD treatment and lower dropout rates than trauma-focused approaches (26). In a recent Cochrane review (27) based on 12 RCTs, PCT was found to be superior to waitlist (SMD = −0.84). A comparison of PCT to trauma-focused CBT did not support PCT non-inferiority. ESs differed for PCT and trauma-focused CBT with 0.32 in favor of trauma-focused CBT. PCT resulted in 16% lower dropout rates than trauma-focused CBT. Current treatment guidelines suggest that PCT may be offered as a treatment for PTSD when trauma-focused CBT is either not available or not preferred by the patient (28).
Taken together, PCT can be deemed to be what is known as a bona fide therapy, namely a therapy based on psychological principles containing specific factors (i.e., specific techniques like fostering of problem-solving skills and homework exercises, or promoting a theory of the therapeutic change, namely by client-centered principles of offering empathy, unconditional positive regard and congruence) and delivered by trained professionals [cf. (29, 30)]. It is, therefore, a credible intervention for both patients and therapists. Unlike almost all other interventions that have been examined in patients suffering from PGD so far, PCT does not include exposure or cognitive interventions. Given that patients with PGD, as well as those with PTSD, suffer from avoidance (albeit to slightly different degrees), an intervention that takes a different approach to addressing avoidance seems to represent an interesting alternative to previously studied interventions. Furthermore, on a theoretical basis, by focusing on the active mastery of daily problems and functional coping, one might speculate that PCT resembles restoration-orientation according to the Dual Process Model of coping with bereavement (31). This is why we decided to adapt PCT to the needs of patients suffering from PGD. If PCT for PGD would prove feasible and clinical impactful, it might not only serve as an active bona fide treatment with a different treatment focus most PGD interventions had so far, but it also promises to be an ideal active control condition in future PGD trials. Therefore, the aim of this study was to evaluate the feasibility and the treatment effects of PCT in adults with PGD, and to explore therapists' and supervisor's experiences with this new treatment.
Methods
Participants
Participants were treatment-seeking adults aged 18 to 75, whose losses had occurred at least 6 months previously. A primary diagnosis of PGD, as assessed in the Interview for Prolonged Grief-13 [PG-13; (6, 32), see below], was required for inclusion. Because of the ongoing discussion about a multiplicity of different criteria sets for PGD (2, 3, 6, 33, 34), and because the final ICD-11 criteria were not available when we started this trial in 2017, we decided on a compromise between criteria according to Prigerson et al. (6) and the not yet finalized ICD-11 (2). To meet the criteria for PGD in the current study, it was necessary for participants to report at least (a) one separation distress symptom (rated as ≥4 on a 5-point-scale: 1 = never/not at all, 5 = several times a day/extremely), (b) four out of nine cognitive, emotional, and behavioral symptoms (each symptom rated as ≥ 4), and (c) significant impairment in social, occupational or other important domains, for 6 months or longer, after the loss according to the PG-13, see below. Patients had to have sufficient cognitive and German language skills, and give their written informed consent. If patients were on antidepressant medication, the treatment regime needed to be stable for at least 4 weeks prior to joining the trial. The exclusion criteria were: (1) current psychotic or severe substance use disorder, or acute suicidality; (2) ongoing psychotherapy; (3) participation in another treatment trial; and (4) continuous treatment with benzodiazepines, antipsychotics, or opioids. Any change in psychotropic medication during the course of the study was continuously monitored.
Procedure
The current trial was an integral part of a preparation phase for an RCT [(35), German Clinical Trials Register, ID: DRKS00012317]. Treatment was offered at four University outpatient mental health clinics in Germany. The study was approved by the Institutional Review Board of the Catholic University Eichstaett-Ingolstadt (2016/21), and by three Institutional Review Boards of the other study centers (Ethics Committee of the Department of Psychology and Sports of the Goethe University Frankfurt, Ethical Committee at the Medical Faculty of Leipzig University, Local Ethics Committee of the Department of Psychology of the University of Marburg). Recruitment efforts included a study website, advertisements in public and social media, newspaper and radio interviews, flyers in family practices, health and community centers, or churches, and informing general and mental health practitioners via mailings, as well as via talks and publications in the specialized press. The first patient started therapy in June 2017, the last patient finished therapy in May 2019.
The trial included assessments at baseline, post-treatment, and at the 3-month follow-up, each comprising the same clinical interviews and self-ratings described below. All assessments were conducted by trained clinical raters who were blind to the participants' baseline assessment results and treatment progression. Study safety was ensured by monitoring for the incidence of serious adverse events (e.g., suicide attempts, death, occurrence of life-threatening conditions, events that lead to physical disability) using a therapist/rater-administered checklist every treatment session and at post-treatment and follow-up. Participants received a small financial compensation for taking part in the post-treatment and follow-up assessments (€20 for each assessment).
Treatment was administered by 20 study therapists, who were predominantly female (94%), master's level psychologists in advanced postgraduate clinical training (71%) and specialized in CBT (100%). All therapists were novices in PCT and were interested in taking part in an upcoming RCT. They were free in choosing training in PCT or an alternative grief-focused CBT training. All included patients represented each therapist's first training case. All PCT therapists attended a 2-day personal training course in PCT delivered by one of PCT's original authors, Dr. Shea. During the trial, therapists were supervised bi-weekly at the respective study center. In addition, they participated in centralized bi-weekly telephone case consultations to maintain treatment adherence. Therapeutic adherence and competence are currently being evaluated with independent ratings by two raters based on video-documented sessions selected at random.
Outcomes and Measures
The primary outcome was the PGD severity score assessed by the PG-13 in an interview format [(6, 33), German version (36), as published in (37)], which was obtained by calculating the sum of the 11 symptom item scores (range: 11–55). Cutoff scores of 34 and 35 have been suggested for the PG-13 (37, 38). Psychometric evaluation showed good internal consistency [e.g., Cronbach's alphas from 0.83 to 0.93 in (39)]. The PG-13 was also used to assess PGD diagnostic status as defined for the current study (see above) as well as a reliable change in PGD symptoms. In the current sample, the internal consistency of the total severity score (11 items) was 0.71.
Secondary outcomes were assessed that targeted self-reported symptoms of prolonged grief, depression, somatoform symptoms, and general mental distress.
Prolonged grief symptoms were also measured using the self-report measure Inventory of Complicated Grief [ICG; (40), German version ICG-D; (41)]. Participants were asked to rate the extent to which they had experienced 19 grief symptoms during the previous month on a 5-point scale ranging from 0 = never to 4 = all the time. A prolonged grief score was computed (range: 0–76), Cronbach's alpha was 0.70. Prigerson et al. (40) suggested an ICG score >25 as the threshold for distinguishing syndromal from subsyndromal levels of PGD. However, later studies [e.g., (42, 43)] used a cutoff score of ≥ 30 as a more conservative threshold to identify clinically significant cases.
Self-reported depressive symptoms were measured using the German version of the Beck Depression Inventory II [BDI-II; (44)]. The 21 items refer to symptoms of depression during the previous 2 weeks and are rated on a 4-point scale, resulting in a total depression score ranging from 0–63. Cronbach's alpha in the current sample was 0.85.
As we had found a high level of somatoform symptoms in two earlier studies (45, 46), we decided to include a measure to specifically address somatoform complaints. The Screening for Somatoform Disorders [SOMS-7D; (47)] was used to assess self-reported somatoform symptoms. Participants were asked to rate the extent to which they had suffered from 53 somatoform symptoms during the previous 7 days on a 5-point scale (0 = not at all, 4 = very much). A somatization severity index was calculated ranging from 0–208. Cronbach's alpha was 0.89 in the current sample.
Self-reported general mental distress was measured using the Global Severity Index (GSI) from the German version of the Brief Symptom Inventory [BSI; (48)]. The BSI is a widely used 53-item measure of subjective distress caused by psychological and somatic symptoms over the previous seven days. Responses are scored on a 5-point scale (0 = not at all, 4 = extremely). The GSI is calculated using the sums for the nine subscales plus the four additional items, and divided by the total number of items to which the individual responded (score range: 0–4). In the current sample, Cronbach's alpha of the BSI-GSI was 0.94.
To obtain information about the study therapists' evaluations of PCT, we asked all study therapists to fill in an online questionnaire after having completed their first treatment case. We obtained ratings on four subscales: beliefs and attitudes about the intervention (i.e., individuals' attitudes toward and value placed on the intervention); design quality (i.e., perceived excellence in how the intervention is bundled, presented, and assembled); adaptability and trialability (i.e., degree to which an intervention can be adapted, tailored, refined, or reinvented to meet local needs and ability to test the intervention on a small scale in the organization); and resources and access to knowledge (i.e., level of resources dedicated for implementation and on-going operations and ease of access to digestible information and knowledge about the intervention and how to incorporate it into work tasks). For this questionnaire, we used items by Cook et al. (49) or generated items based on the framework model of Damschroder et al. (50). The Consolidated Framework for Implementation Research by Damschroder et al. (50) includes the most common concepts from published implementation theories. The framework is designed to allow researchers to select the concepts most relevant for their particular setting and use them to evaluate the implementation process. As we were primarily concerned with implementing a new intervention, PCT, within the well-established structures of four University outpatient clinics, we selected concepts relating to the characteristics of the intervention, individual characteristics and the inner setting of our clinics to evaluate the implementation process of PCT. Therefore, for the purpose of this study, we created four subscales to evaluate the implementation process of PCT from the viewpoint of therapists. Overall, the questionnaire consisted of 23 items to be rated on a 5-point scale (1 = I do not agree at all, 5 = I agree fully). Mean scores were calculated for each of the four subscales (mean score range: 1–5). One item on barriers to the implementation of PCT also included the option of giving an answer in an open format, if applicable. In the current sample, the internal consistencies of the beliefs and attitudes about the intervention scale (9 items; α = 0.78), the design quality scale (3 items; α = 0.80), and the resources and access to knowledge scale (5 items; α = 0.78) were good. The internal consistency of the adaptability and trialability scale (4 items; α = 0.70) was acceptable. See Supplementary Material 1 for the questionnaire.
The presence of comorbid mental disorders according to DSM-IV criteria at baseline was determined using the Structured Clinical Interview for DSM-IV Axis I [(51), German version: (52)]. DSM-IV criteria were used, because no validated German version for the Structured Clinical Interview for DSM-5 was available in 2017 yet. Interviewer-rated acute suicidality was assessed using the Columbia-Suicide Severity Rating Scale [C-SSRS; (53)]. The five items in the intensity of suicide ideation subscale were used to rate the intensity of current suicide ideation on 5- and 6-point scales (score range: 2–25).
Intervention
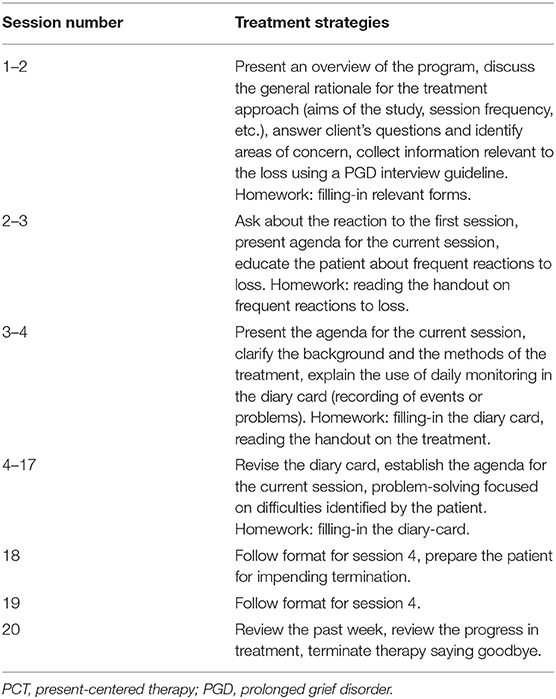
The PCT manual for PTSD (25) was adapted in cooperation with Dr. Shea for its use with PGD patients (54). To adapt PCT for treating PGD in Germany, we made the following modifications: (1). In order to make PCT a credible intervention for both patients and therapists, session length and number were adapted to the standard health insurance coverage for outpatient CBT treatments in Germany, that is, 20 50-min sessions (as compared to 10 100-min sessions). (2). Educating the patient at the beginning of treatment focused on grief-specific topics including grief symptoms and their relation to problems in day-to-day life. Furthermore, therapists were allowed to collect information relevant to the loss in the first sessions in order to establish a therapeutic relationship. (3). Up to four additional optional sessions were possible to handle special occasions or needs (e.g., suicidality, dealing with anniversaries). Altogether, a maximum of 24 therapy sessions was possible according to the protocol, see Table 1 for an overview. Besides educating the patients on grief symptoms, PCT did not include any grief-specific cognitive-behavioral components (e.g., exposure, cognitive restructuring of dysfunctional beliefs, instructions to do specific homework). Its focus was on the daily monitoring of stressors and problems in their relation to PGD and on their active mastery. The therapists provided support and established an empathic relationship. This encouraged the expression of thoughts or feelings and explicitly focused on factors of client-centered therapy. Therefore, PCT has elements of supportive therapy, but is a more structured approach that follows a manual and includes the use of a diary to record problems throughout the week. It did not, however, use any active interventions except for giving information, pointing out themes, or other ways of fostering functional coping and the patient's problem-solving skills. If the patient brought up problems regarding the loss, discussions on the loss itself were avoided in favor of focusing on how to better cope with symptoms in daily life resulting from the loss. The aim was to achieve greater insight and support regarding the consequences of the loss. When patients were emotionally distressed during sessions, therapists acted in an empathic, compassionate and helpful manner and promoted functional problem-solving when appropriate.
Data Analyses
All primary and secondary outcome analyses were performed as intent-to-treat (ITT) analyses. We used the last observation carried forward (LOCF) procedure to replace missing values due to participants dropping out of the study. To examine the effects of PCT on primary and secondary outcomes, we conducted a repeated-measures multivariate analysis of variance (MANOVA) with measurement time points (pretreatment, post-treatment, follow-up) as a within-subject factor. To assess the effects on each of the outcome measures, repeated measures analyses of variance (ANOVAs) were performed with three measurement time points post hoc. The significance level for all analyses was set to α = 0.05 (2-tailed). As analyses were considered in an exploratory manner, the significance level was not adjusted for multiple tests. Cohen's d ES was calculated for within group pre-post comparisons. Cochran's Q test, which is a generalization of the McNemar test for more than two measurement time points, was applied to investigate the change in diagnostic status with respect to PGD (55). Statistics were calculated using IBM SPSS Statistics 25 for Windows. The criterion for a clinically reliable change in the PG-13 severity score according to Jacobson and Truax (56) was calculated on the basis of Cronbach's α of the PG-13 severity score in the current study, as proposed by Martinovich et al. (57). Thus, clinically reliable improvement was defined as a reduction of more than 6.88 points in the PG-13 severity score.
The open format answers regarding barriers to implementation of the PCT survey were analyzed and summarized by creating condensed meaning units according to Bengtsson (58).
Results
Participant Flow
We screened 32 individuals for eligibility; 12 of them did not meet the study criteria. Six of them had not been clinically diagnosed as having PGD. See Figure 1 for participant flow. One eligible candidate for treatment declined. As a result, 20 participants began treatment with PCT. Their ages ranged from 37 to 74, with n = 3 aged under 50.
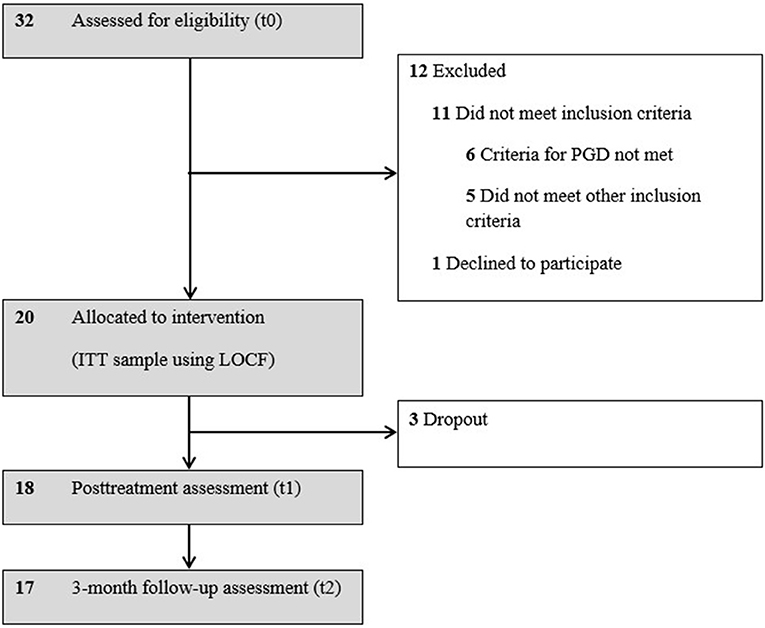
Figure 1. Flow diagram of study participants. ITT, intent-to-treat; LOCF, last observation carried forward; PGD, prolonged grief disorder.
Most participants were women (80%) and currently employed (50%). Fifteen participants had completed secondary education only (≤ 12 years), and five had been to college (>12 years). The majority of participants had lost a partner (45%), or child (35%). The deaths were mostly natural (75%) but unexpected (50%). The mean time since loss was 48.8 months (Mdn = 27.0; range: 6–337). All patients met the criteria for PGD diagnostic status as defined for the current study.
At baseline, 16 participants (80%) met the criteria of at least one comorbid psychiatric disorder with an average of M = 1.00 (SD = 0.65) in addition to PGD. For further details, see Table 2.
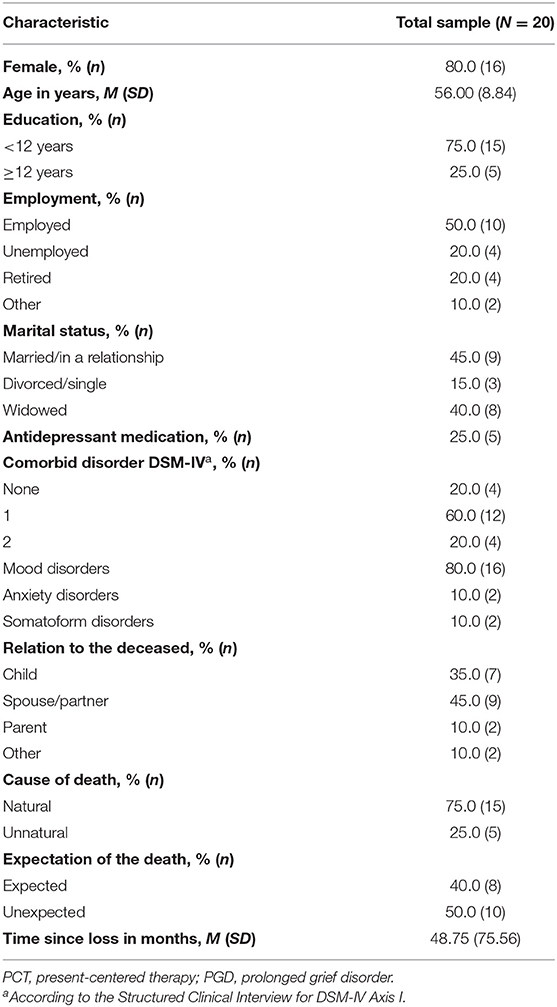
Table 2. Sociodemographic and loss-related characteristics of study participants in the feasibility trial of PCT adapted for PGD.
Of all the participants who began treatment with PCT, three participants (15%) discontinued treatment prematurely after session 5, session 7, and session 12, respectively. In all of these cases, treatment was terminated because of a lack of treatment motivation. In two of these cases the reasons for dropout reported by the respective therapists were relatively long travel distances coupled with low motivation for change. In the third case a very low motivation to attend therapy sessions was mentioned. We were able to obtain further data from one of the participants who dropped out at post-treatment. Another participant did not complete the post-treatment self-report ratings, and data of the SOMS-7D of one further participant at the follow-up assessment was missing.
The mean duration of treatment was 23.65 weeks (SD = 7.10), with an average of M = 18.70 (SD = 4.99) sessions provided. Neither suicidal crises nor other serious adverse events occurred during the intervention or up to the 3-month follow-up.
Treatment Outcome
The repeated measures MANOVA of the primary (PG-13) and secondary outcome measures (ICG, BDI-II, BSI-GSI, SOMS-7D) calculated on the basis of the ITT sample (N = 20), demonstrated a significant effect of time, F(10, 108) = 2.08, p = 0.032.
Repeated measures ANOVA revealed a significant large effect for the total severity score of interview-rated PGD symptoms (PG-13) from pre- to posttreatment with d = 1.26. Improvements remained stable at the 3-month follow-up, d = 1.25. See Table 3 for the results of respective ANOVAs and effect sizes.
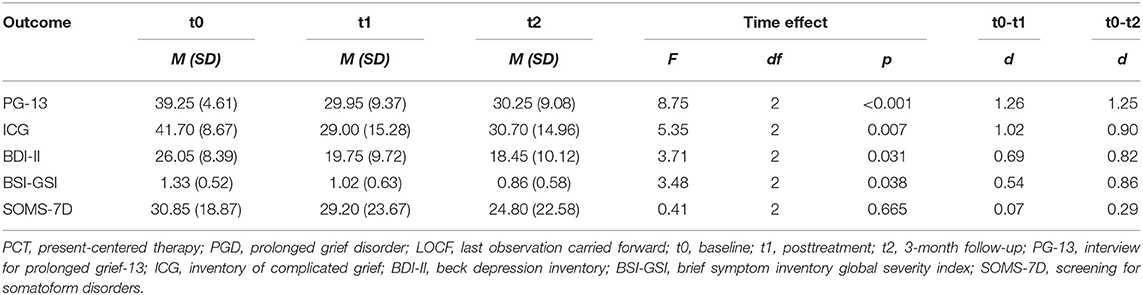
Table 3. Primary and secondary outcomes of study participants in the feasibility trial of PCT adapted for PGD adults based on intent-to-treat analyses with LOCF, N = 20.
At post-treatment, 15 participants (75%) no longer met the PGD criteria according to the PG-13, and 13 participants (65%) at the 3-month follow-up. Three of the five cases who still met the PGD criteria after treatment, were the participants who had dropped out. The change in PGD diagnostic status over time was significant, Cochran's Q(2) = 24.57, p < 0.001. At post-treatment, 10 participants (50%) met the criteria for reliable change according to the PG-13 score, whereas 11 participants (55%) met the criteria for reliable change at the 3-month follow-up. No clinically relevant worsening of symptoms was observed. Throughout the trial, no serious adverse event was reported.
The results regarding self-reported PGD symptoms (ICG) revealed a significant large effect from pre- to post-treatment with d = 1.02, see Table 3. The ES remained large at the 3-month follow-up, d = 0.90. However, total sum scores at posttreatment as well as 3-month follow up remained at or above more conservative cutoff scores used in other studies [e.g., (43)].
Participants improved significantly from pre- to post-treatment and up to the 3-month follow-up with regard to BDI-II and BSI-GSI. ESs for improvements of depressive symptoms and general mental distress were medium to large, ranging from 0.54 to 0.86. There were no significant improvements with regard to somatoform symptoms as assessed by the SOMS-7D.
Evaluation of the Study Therapists' Perspective
Of all the PCT study therapists, 17 (85%) responded to our online questionnaire after having completed their first treatment case, including the three therapists whose patients discontinued treatment prematurely. Their demographic characteristics are given in Table 4.
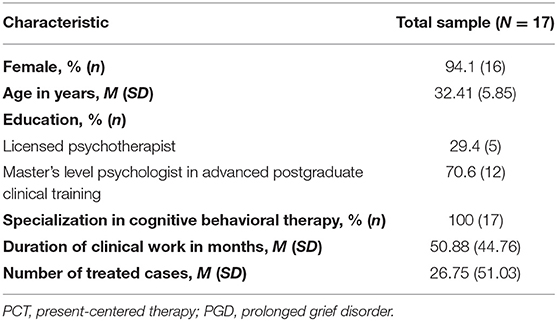
Table 4. Demographic characteristic of study therapists in the feasibility trial of PCT adapted for PGD.
The mean scores of the four subscales of the evaluation of PCT can be considered as medium to high, with M = 3.65 (SD = 0.54) regarding beliefs and attitudes about the intervention, M = 3.94 (SD = 0.64) regarding design quality, M = 3.94 (SD = 0.64) regarding adaptability and trialability, and M = 3.95 (SD = 0.74) regarding resources and access to knowledge. Therefore, PCT adapted for PGD as evaluated by the study therapists seems to be an adaptable and learnable intervention of good design quality that was evaluated positively by CBT therapists.
Only nine therapists (53%) reported at least one barrier to administering PCT with their pilot cases. The reported barriers were grouped into five categories. In three cases (17.6%), therapists reported that features of a personality disorder or rigid behavior patterns complicated implementing the manual with their patient. Three categories were each mentioned by two therapists (11.8%) as a barrier: patient's lack of motivation for change or reactance, lack of permission to use typical CBT methods (like cognitive restructuring, exposition), and problems during treatment because the patient would have needed clearly defined goals. One therapist (5.9%) reported the PCT manual as being not specific enough as a further problem when administering PCT. Two of these categories (personality features and rigid behavior patterns, reactance from the patient and lack of motivation for change) seem to be associated with the individual patient's characteristics and might not, therefore, be a problem specific to PCT. The other three categories (lack of target definition with the patient, unspecific manual, no permission to use typical CBT methods) seem to constitute specific problems associated with differences between the nature of the PCT program and the prior CBT-training of the therapists.
Experiences With PCT From the Supervisor's Perspective
Multicenter case consultations were put in place to monitor treatment adherence throughout the study. Study therapists became easily engaged in PCT, reported generally positive relationships with their patients and no important problems with regard to treatment adherence. They also reported that most patients engaged very well in PCT. Some therapists expressed doubts about the effectiveness of the PCT treatment and were reminded of the body of evidence that had been published up to then. All therapists had a CBT qualification, including mastery of a minimal amount of client-centered techniques. The group repeatedly discussed appropriate and inappropriate therapist behaviors to stay within the limits of the treatment manual. Another challenging question was how important problem solving and filling in the diary card were. Some therapists, for example, reported, that patients did not fill in the diary cards or carry out specific homework assignments. During case consultations therapists were motivated to focus more on the therapeutic relationship as mode of action rather than following a CBT-typical perspective when dealing with homework assignments undone. In most cases a decision was taken to focus on behaviors that enhance a positive relationship and promote factors of client-centered therapy. With respect to problem-solving, therapists were reminded to first help the patient to identify their emotions, and only thereafter to work on problem-solving, thus avoiding the risk of talking about solutions that were trivial and not specific enough.
Discussion
Outcomes and Safety of PCT for PGD
This study is the first to investigate the feasibility of PCT in patients suffering from PGD. While PCT previously had been evaluated in samples with PTSD (27), we were interested in the feasibility and treatment effects of PCT in a sample of bereaved adults. We found significant pre- to post-treatment reductions in PGD symptoms as assessed by the PG-13 and the ICG indices with large ESs. However, PCT did not yield ICG total sum scores substantially below clinical cutoffs at post-treatment or follow-up. According to the PG-13 severity score, 50% of participants showed clinically meaningful improvement, and 75% of the participants achieved remission from PGD. Improvements remained nearly stable at the 3-month follow-up. Regarding secondary outcome measures, significant improvements from pre- to post-treatment were observed with respect to depressive symptoms and general mental distress as assessed in self-report, with medium pre-post ESs and large ESs at follow-up.
The ESs regarding PGD symptoms were higher than those reported in meta-analyses for PGD treatments in adults (22–24). These results are encouraging as the self-reported baseline severity of PGD symptoms, MICG = 41.70, in our sample was comparable to several RCTs evaluating grief-focused treatments [e.g., MICG = 42.6 in (18), MICG = 47.5 in (19), MICG = 45.8 in (15), MICG = 46.1 in (59)]. Compared to small ESs for depressive symptoms and general mental distress reported in the literature (22, 24), our results with medium pre-post ESs and large ESs at follow-up seem to be promising. However, because of the small sample size and the uncontrolled design of the study, interpretation of these ESs should only be made with caution (60). Furthermore, compared to ICD-11 criteria, the more strict criteria set used in this study (6) might also have affected ESs, as including participants with lower symptom scores might have yielded in lower ESs.
The severity of somatoform symptoms at baseline was high in the current sample, as the mean score of the SOMS-7D corresponded to percentile rank = 93 according to the German norm sample (47). This is in line with results from other bereaved samples (46, 61, 62). The non-significant differences with regard to somatoform symptoms, as assessed by the SOMS-7D, might be explained by the fact that PCT does not contain any components that are assumed to be specific mechanisms of change for the treatment of somatoform disorders (63, 64).
To adapt the treatment protocol to the standard health insurance coverage for outpatient CBT treatments in Germany, we allowed 20 to 24 50-min sessions to be administered, with a mean of 18.70 sessions conducted. Therefore, the mean number of treatment sessions was considerably higher than the number reported by meta-analyses evaluating grief-focused treatments [10 in (24), 10 to 16 in (23)]. This higher number of treatment sessions might, in part, explain the large ESs we found with respect to PTG symptoms.
Acceptability in Patients and Therapists
We did not observe any exacerbation of PGD symptoms from pretreatment to any later assessment point, nor did any adverse event occur during the trial. These results indicate that the intervention was well-received by the participants and was safe. PCT was a new treatment for all of the study therapists as PCT was previously unknown in Germany. In particular, the strong focus on client-centered techniques (following the core conditions sensu Rogers) while dispensing with almost all CBT methods, constituted an unusual approach for many of the therapists. They were all trained in CBT but had not undergone training with the focus on client-centered techniques prior to the current trial. In line with this, the lack of target definition with the patient, the unspecific manual, and the withholding of permission to use typical CBT methods seemed to be specific problems associated with the nature of the PCT program. Some study therapists reported them as barriers. However, these problems might decrease with an increasing number of cases treated with PCT and with growing expertise in emphasizing client-centered techniques in the therapeutic process. It is also questionable whether these problems occur at all with non-CBT therapists. Therefore, implementing PCT with therapists with other theoretical backgrounds than CBT in future studies would be very informative.
Three participants dropped out of treatment (15%). In two of these cases, the respective patients had to travel very long distances to the treatment site combined with a reported low motivation for change, as indicated by their therapists. In the third case very low motivation to attend therapy sessions was mentioned from the start. All dropouts may also be associated with the participants' high pretreatment PG-13 severity (all above the median of 39) and ICG scores (all above the median of 40). However, in terms of completion rates, the results in our study are good, with 85% completion in PCT vs. 82% in the study by Shear et al. (59), 73% in the study by Shear et al. (15), 79% in the study by Rosner et al. (46) and 71% in the study by Boelen et al. (10).
Overall, the promising results of PCT in patients suffering from PGD as studied in this trial, but also in previous trials with PTSD patients, raise questions about possible psychological mechanisms that are responsible for change in PCT. Unlike many effective interventions for PTSD and PGD, PCT clearly does not include any exposure or cognitive restructuring. It can be assumed that exposure and cognitive restructuring cause direct symptom reductions in patients via facilitating emotional processing, minimizing avoidance, and modifying negative cognitions—mechanisms that seem to be crucial for recovering from PTSD (65) as well as PGD (66). In contrast, patients treated with PCT seem to experience enhanced psychosocial functioning through the application and practice of more effective solutions to daily stressors, and this might indirectly lead to a symptom reduction. PCT's focus on problem-solving in the present might be especially attractive for bereaved patients, as they often have to deal with new problems after the loss (e.g., inheritance issues, problems in everyday life as a result of secondary losses). Furthermore, they might be afraid of interventions that foster emotional engagement with the loss because of avoidance or unbearable emotional pain. This might be also the case in patients suffering from PTSD, for whom PCT achieved lower dropout rates than trauma-focused CBT (26, 27). Additional mechanisms underlying PCT may rely on the therapeutic benefits that emerge from a caring relationship, including mobilization of hope and optimism, and increased positive self-regard (67). These are non-specific elements every psychotherapy contains, but they might be activated to a special degree in PCT. However, these assumptions regarding mechanisms underlying PCT and how they affect long-term effects of treatment success require precise evaluation in future process-outcome studies.
Limitations and Strengths
The generalizability of our study results is limited by the small sample size and the predominantly female (80%) sample. A more general limitation is the lack of a control group, which reduces the strength of the conclusions that can be drawn from the findings. Therefore, natural remission of symptoms or non-specific effects of supportive study attention cannot be excluded. In addition, the non-randomized design may have influenced participants' motivation for taking part in the trial and their retention other than an RCT design. Hence, an RCT with a solid sample size is necessary to test the specific efficacy of PCT for PGD. Furthermore, follow-up assessments for a longer period than 3 months after treatment would have been advisable. Since the ratings of treatment adherence by independent trained raters are not completed yet, we are unable to report on the results of a formalized adherence rating. Yet, specific focus in supervision and case consultations was given to treatment adherence and specifically to the omission of CBT interventions. Finally, using a qualitative methodological approach would have provided further insight regarding therapists' acceptability of PCT. Despite these limitations, which are primarily due to the study design, feasibility trials are of high interest, especially to foster research when there is a lack of controlled studies as for PGD (14). Feasibility trials allow to examine the safety and acceptability of a new or adapted intervention for a new target group before administering it in larger trials. They are also crucial to examine treatment and training protocols. When developing a psychological treatment, it is important to consider how easily and successfully health professionals new to grief treatment can learn to administer it. If a high amount of training is needed to teach the new treatment, dissemination and implementation might prove difficult. Finally, feasibility trials allow for developing adherence/competence measures and recruitment procedures that are crucial for subsequent RCTs, if the treatment demonstrates clinical impact. To address these goals, the current trial served as an important first step in evaluating PCT for PGD and is in line with sample sizes of other pilot and feasibility trials with bereaved patients [e.g., (68–70)].
Implications
In conclusion, our study furnishes preliminary evidence of the feasibility, efficacy, and safety of PCT with PGD. PCT adapted for PGD was deemed to be an adaptable and easy-to-learn intervention of good design quality by our relatively young CBT therapists. Future studies are needed to address the question of the efficacy of PCT adapted to PGD compared to adequate control conditions. Based on our results, it seems reasonable to choose and evaluate PCT as an active control condition compared to a grief-focused CBT, including exposure and cognitive structuring, in a current RCT (35). Furthermore, the need for specific treatment components, such as exposure, cognitive restructuring techniques, or behavioral activation, should be addressed in dismantling studies targeting patients suffering from PGD. PCT might be a viable alternative for patients unable or unwilling to participate in grief-focused treatments. Further evaluation of PCT in RCTs may help determine which treatment components are beneficial and necessary for the individual PGD patient and might allow formulation of individualized treatment recommendations and different treatment selection [see (71)]. Therefore, further research regarding the efficacy of PCT but also regarding individual predictors of treatment success in PCT is of high interest.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of the Catholic University Eichstaett-Ingolstadt, Ethics Committee of the Department of Psychology and Sports of the Goethe University Frankfurt, Ethical Committee at the Medical Faculty of Leipzig University, Local Ethics Committee of the Department of Psychology of the University of Marburg. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AV and RR contributed to the design of the study. RR was the principal investigator. AK, WR, and RS were leaders of the collaborating study centers. HC organized the database. AV performed the statistical analyses and wrote the first draft of the manuscript. AN and RR wrote sections of the manuscript. All authors contributed to the manuscript revision, read and approved the submitted version.
Funding
Some parts of the study were funded by proFOR+, a funding program run by the Catholic University of Eichstaett-Ingolstadt. The open access publication of this article was supported by the Open Access Fund of the Catholic University Eichstaett-Ingolstadt. The associated RCT following this study was funded by a grant from the German Research Foundation (DFG RO 2042/7-1).
Conflict of Interest
AN was paid fees for supervising PCT. RR was paid fees for workshops and presentations on PGD treatment.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all the patients who participated in this trial, and all therapists and raters who administered the interventions and assessments.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.534664/full#supplementary-material
References
1. Jordan AH, Litz BT. Prolonged grief disorder: diagnostic, assessment, and treatment considerations. Prof Psychol Res Pract. (2014) 45:180–7. doi: 10.1037/a0036836
2. World Health Organization (2018). ICD-11 international classification of diseases for mortality and morbidity statistics. 11th revision. World Health Organization (2018). Available online at: https://icd.who.int/browse11/l-m/en
3. American Psychiatric Association ed. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, DC: American Psychiatric Association (2013).
4. Horowitz M, Siegel B, Holen A, Bonanno G, Milbrath C, Stinson C. Diagnostic criteria for complicated grief disorder. Am J Psychiatry. (1997) 154:904–10.
5. Prigerson H, Shear MK, Jacobs SC, Reynolds CF, Maciejewski PK, Davidson JRT, et al. Consensus criteria for traumatic grief: a preliminary empirical test. Br J Psychiatry. (1999) 174:67–73.
6. Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. (2009) 6:e1000121. doi: 10.1371/journal.pmed.1000121
7. Lundorff M, Holmgren H, Zachariae R, Farver-Vestergaard I, O'Connor M. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J Affect Disord. (2017) 212:138–49. doi: 10.1016/j.jad.2017.01.030
8. Kersting A, Brähler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. (2011) 131:339–43. doi: 10.1016/j.jad.2010.11.032
9. Djelantik AAAMJ, Smid GE, Mroz A, Kleber RJ, Boelen PA. The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: systematic review and meta regression analysis. J Affect Disord. (2020) 265:146–56. doi: 10.1016/j.jad.2020.01.034
10. Boelen PA, Prigerson HG. The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults. Eur Arch Psychiatry Clin Neurosci. (2007) 257:444–52. doi: 10.1007/s00406-007-0744-0
11. Simon NM, Shear MK, Thompson EH, Zalta AK, Perlman C, Reynolds CF, et al. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Compr Psychiatry. (2007) 48:395–9. doi: 10.1016/j.comppsych.2007.05.002
12. Latham AE, Prigerson HG. Suicidality and bereavement: complicated grief as psychiatric disorder presenting greatest risk for suicidality. Suicide Life Threat Behav. (2004) 34:350–62. doi: 10.1521/suli.34.4.350.53737
13. Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. (2007) 370:1960–73. doi: 10.1016/S0140-6736(07)61816-9
14. Boelen PA, Smid GE. Disturbed grief. Prolonged grief disorder and persistent complex bereavement disorder. BMJ. (2017) 357:j2016. doi: 10.1136/bmj.j2016
15. Shear MK, Frank E, Houck PR, Reynolds CF. Treatment of complicated grief: a randomized controlled trial. JAMA. (2005) 293:2601–8. doi: 10.1001/jama.293.21.2601
16. Shear MK, Reynolds CF, Simon NM, Zisook S, Wang Y, Mauro C, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. (2016) 73:685–94. doi: 10.1001/jamapsychiatry.2016.0892
17. Supiano KP, Luptak M. Complicated grief in older adults: a randomized controlled trial of complicated grief group therapy. Gerontologist. (2014) 54:840–56. doi: 10.1093/geront/gnt076
18. Boelen PA, de Keijser J, van den Hout MA, van den Bout J. Treatment of complicated grief. A comparison between cognitive-behavioral therapy and supportive counseling. J Consult Clin Psychol. (2007) 75:277–84. doi: 10.1037/0022-006X.75.2.277
19. Bryant RA, Kenny L, Joscelyne A, Rawson N, Maccallum F, Cahill C, et al. Treating prolonged grief disorder: a randomized clinical trial. JAMA Psychiatry. (2014) 71:1332–9. doi: 10.1001/jamapsychiatry.2014.1600
20. Eisma MC, Boelen PA, van den Bout J, Stroebe W, Schut HAW, Lancee J, et al. Internet-based exposure and behavioral activation for complicated grief and rumination: a randomized controlled trial. Behav Ther. (2015) 46:729–48. doi: 10.1016/j.beth.2015.05.007
21. Wagner B, Knaevelsrud C, Maercker A. Internet-based cognitive-behavioral therapy for complicated grief: a randomized controlled trial. Death Stud. (2006) 30:429–53. doi: 10.1080/07481180600614385
22. Currier JM, Neimeyer RA, Berman JS. The effectiveness of psychotherapeutic interventions for bereaved persons: a comprehensive quantitative review. Psychol Bull. (2008) 134:648–61. doi: 10.1037/0033-2909.134.5.648
23. Wittouck C, Van Autreve S, Jaegere E, de Portzky G, van Heeringen K. The prevention and treatment of complicated grief: a meta-analysis. Clin Psychol Rev. (2011) 31:69–78. doi: 10.1016/j.cpr.2010.09.005
24. Johannsen M, Damholdt MF, Zachariae R, Lundorff M, Farver-Vestergaard I, O'Connor M. Psychological interventions for grief in adults. A systematic review and meta-analysis of randomized controlled trials. J Affect Disord. (2019) 253:69–86. doi: 10.1016/j.jad.2019.04.065
25. Shea MT, Davis N, Howard J, Key F, Lambert J. Present-Centered Therapy (PCT) Manual. Unpublished Manual Developed for Cooperative Studies: Treatment of Posttraumatic Stress Disorders in Women (2003).
26. Frost ND, Laska KM, Wampold BE. The evidence for present-centered therapy as a treatment for posttraumatic stress disorder. J Trauma Stress. (2014) 27:1–8. doi: 10.1002/jts.21881
27. Belsher BE, Beech E, Evatt D, Smolenski DJ, Shea MT, Otto JL, et al. Present-centered therapy (PCT) for post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. (2019) 2019:CD012898. doi: 10.1002/14651858.CD012898.pub2
28. International Society for Traumatic Stress Studies. ISTSS prevention and treatment guidelines (2018). Available online at: https://www.istss.org/treating-trauma/new-istss-prevention-and-treatment-guidelines.aspx (accessed February 6, 2019).
29. Lambert MJ. The efficacy and effectiveness of psychotherapy. In: Lambert MJ, editor. Bergin and Garfield's Handbook of Psychotherapy and Behaviour Change. Hoboken, NJ: Wiley (2013). p. 169–218.
30. Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn H-N. A meta-analysis of outcome studies comparing bona fide psychotherapies: empiricially, “all must have prizes. Psychol Bull. (1997) 122:203–15. doi: 10.1037/0033-2909.122.3.203
31. Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. (1999) 23:197–224. doi: 10.1080/074811899201046
32. Prigerson HG, Maciejewski PK. Prolonged Grief Disorder (PG-13) Scale. Boston, MA: Dana-Farber Cancer Institute (2008).
33. Comtesse H, Vogel A, Kersting A, Rief W, Steil R, Rosner R. When does grief become pathological? Evaluation of the ICD-11 diagnostic proposal for prolonged grief in a treatment-seeking sample. Eur J Psychotraumatol. (2020) 11:1694348. doi: 10.1080/20008198.2019.1694348
34. Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, et al. Complicated grief and related bereavement issues for DSM-5. Depression Anxiety. (2011) 28:103–17. doi: 10.1002/da.20780
35. Rosner R, Rimane E, Vogel A, Rau J, Hagl M. Treating prolonged grief disorder with prolonged grief-specific cognitive behavioral therapy: study protocol for a randomized controlled trial. Trials. (2018) 19:241. doi: 10.1186/s13063-018-2618-3
36. Vogel A, Pfoh G, Rosner R. PG-13+9: Interview for Prolonged Grief – Revised and Extended Translation of the PG-13. Eichstaett: Catholic University of Eichstaett-Ingolstadt (2017).
37. Lichtenthal WG, Corner GW, Sweeney CR, Wiener L, Roberts KE, Baser RE, et al. Mental health services for parents who lost a child to cancer: if we build them, will they come? J Clin Oncol. (2015) 33:2246–53. doi: 10.1200/JCO.2014.59.0406
38. Pohlkamp L, Kreicbergs U, Prigerson HG, Sveen J. Psychometric properties of the prolonged grief disorder-13 (PG-13) in bereaved Swedish parents. Psychiatry Res. (2018) 267:560–5. doi: 10.1016/j.psychres.2018.06.004
39. Litz BT, Schorr Y, Delaney E, Au T, Papa A, Fox AB, et al. A randomized controlled trial of an internet-based therapist-assisted indicated preventive intervention for prolonged grief disorder. Behav Res Ther. (2014) 61:23–34. doi: 10.1016/j.brat.2014.07.005
40. Prigerson HG, Maciejewski PK, Reynolds CFIII, Bierhals AJ, Newsom JT, Fasiczka A, et al. Inventory of complicated grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res. (1995) 59:65–79. doi: 10.1016/0165-1781(95)02757-2
41. Lumbeck G, Brandstätter M, Geissner E. Erstvalidierung der deutschen Version des Inventory of Complicated Grief“ (ICG-D). Zeitschrift für Klinische Psychologie und Psychotherapie. (2012) 41:243–8. doi: 10.1026/1616-3443/a000172
42. Cozza SJ, Fisher JE, Mauro C, Zhou J, Ortiz CD, Skritskaya N, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. (2016) 173:919–29. doi: 10.1176/appi.ajp.2016.15111442
43. Cozza SJ, Shear MK, Reynolds CF, Fisher JE, Zhou J, Maercker A, et al. Optimizing the clinical utility of four proposed criteria for a persistent and impairing grief disorder by emphasizing core, rather than associated symptoms. Psychol Med. (2019) 50:1–8. doi: 10.1017/S0033291719000254
44. Hautzinger M, Keller F, Kühner C. BDI-II. Beck Depressions-Inventar Revision. 2nd ed. Frankfurt: Harcourt Test Services (2009).
45. Rosner R, Lumbeck G, Geissner E. Effectiveness of an inpatient group therapy for comorbid complicated grief disorder. Psychother Res. (2011) 21:210–8. doi: 10.1080/10503307.2010.545839
46. Rosner R, Pfoh G, Kotoučová M, Hagl M. Efficacy of an outpatient treatment for prolonged grief disorder: a randomized controlled clinical trial. J Affect Disord. (2014) 167:56–63. doi: 10.1016/j.jad.2014.05.035
48. Franke GH. Brief symptom inventory von L. R. Derogatis (Kurzform der SCL-90-R). Deutsche Version. Göttingen: Beltz (2000).
49. Cook JM, O'Donnell C, Dinnen S, Coyne JC, Ruzek JI, Schnurr PP. Measurement of a model of implementation for health care: toward a testable theory. Implementation Sci. (2012) 7:59. doi: 10.1186/1748-5908-7-59
50. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
51. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). New York, NY: Biometric Research Department (1997).
52. Wittchen H-U, Zaudig M, Fydrich T. SKID-I. Strukturiertes Klinisches Interview für DSM-IV Achse I: Psychische Störungen. Göttingen: Hogrefe (1997).
53. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. (2011) 168:1266–77. doi: 10.1176/appi.ajp.2011.10111704
54. Nocon A, Shea MT, Rosner R. Gegenwartsakzentuierte Therapie (GAT) bei Anhaltender Trauerstörung: Manual [Present-centered therapy adapted for prolonged grief disorder]. Eichstaett: Catholic University of Eichstaett-Ingolstadt (2017).
56. Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. (1991) 59:12–9.
57. Martinovich Z, Saunders S, Howard K. Some comments on “Assessing clinical significance”. Psychother Res. (1996) 6:124–32.
58. Bengtsson M. How to plan and perform a qualitative study using content analysis. NursPlus Open. (2016) 2:8–14. doi: 10.1016/j.npls.2016.01.001
59. Shear MK, Wang Y, Skritskaya N, Duan N, Mauro C, Ghesquiere A. Treatment of complicated grief in elderly persons: a randomized clinical trial. JAMA Psychiatry. (2014) 71:1287–95. doi: 10.1001/jamapsychiatry.2014.1242
60. Lipsey MW, Wilson DB. The efficacy of psychological, educational, and behavioral treatment: confirmation from meta-analysis. Am Psychol. (1993) 48:1181–209. doi: 10.1037//0003-066X.48.12.1181
61. Huh HJ, Huh S, Lee SH, Chae J-H. Unresolved bereavement and other mental health problems in parents of the sewol ferry accident after 18 months. Psychiatry Invest. (2017) 14:231–9. doi: 10.4306/pi.2017.14.3.231
62. Rosner R, Bartl H, Pfoh G, Kotoučová M, Hagl M. Efficacy of an integrative CBT for prolonged grief disorder: a long-term follow-up. J Affect Disord. (2015) 183:106–12. doi: 10.1016/j.jad.2015.04.051
63. Kleinstäuber M, Witthöft M, Hiller W. Efficacy of short-term psychotherapy for multiple medically unexplained physical symptoms: a meta-analysis. Clin Psychol Rev. (2011) 31:146–60. doi: 10.1016/j.cpr.2010.09.001
64. Koelen JA, Houtveen JH, Abbass A, Luyten P, Eurelings-Bontekoe EHM, van Broeckhuysen-Kloth SAM, et al. Effectiveness of psychotherapy for severe somatoform disorder: meta-analysis. Br J Psychiatry. (2014) 204:12–9. doi: 10.1192/bjp.bp.112.121830
65. Sripada RK, Rauch Sheila AM, Liberzon I. Psychological mechanisms of PTSD and its treatment. Curr Psychiatry Rep. (2016) 18:99. doi: 10.1007/s11920-016-0735-9
66. Boelen PA, de Keijser J, de van den Hout MA, van den Bout J. Factors associated with outcome of cognitive-behavioural therapy for complicated grief: a preliminary study. Clin Psychol Psychother. (2011) 18:284–91. doi: 10.1002/cpp.720
67. Schnurr PP, Shea MT, Friedman MJ, Engel CC. Posttraumatic stress disorder and cognitive behavioral therapy—reply. JAMA. (2007) 297:2694–5. doi: 10.1001/jama.297.24.2694
68. Iliya YA. Music therapy as grief therapy for adults with mental illness and complicated grief: a pilot study. Death Stud. (2015) 39:173–84. doi: 10.1080/07481187.2014.946623
69. O'Connor M, Piet J, Hougaard E. The effects of mindfulness-based cognitive therapy on depressive symptoms in elderly bereaved people with loss-related distress: a controlled pilot study. Mindfulness. (2014) 5:400–9. doi: 10.1007/s12671-013-0194-x
70. Papa A, Sewell MT, Garrison-Diehn C, Rummel C. A randomized open trial assessing the feasibility of behavioral activation for pathological grief responding. Behav Ther. (2013) 44:639–50. doi: 10.1016/j.beth.2013.04.009
Keywords: prolonged grief disorder, loss, psychotherapy, bereavement, present-centered therapy
Citation: Vogel A, Comtesse H, Nocon A, Kersting A, Rief W, Steil R and Rosner R (2021) Feasibility of Present-Centered Therapy for Prolonged Grief Disorder: Results of a Pilot Study. Front. Psychiatry 12:534664. doi: 10.3389/fpsyt.2021.534664
Received: 13 February 2020; Accepted: 15 March 2021;
Published: 15 April 2021.
Edited by:
Clare Killikelly, University of Zurich, SwitzerlandReviewed by:
Rolf J. Kleber, Utrecht University, NetherlandsLene Larsen, Independent Researcher, Copenhagen, Denmark
Copyright © 2021 Vogel, Comtesse, Nocon, Kersting, Rief, Steil and Rosner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Vogel, anna.vogel@ku.de
 Anna Vogel
Anna Vogel