
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 25 January 2021
Sec. Child and Adolescent Psychiatry
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.609819
This article is part of the Research Topic Behavioral and Cognitive Impairments Across the Life Span View all 34 articles
 Gisella Baglio1*
Gisella Baglio1*  Michela Zanette1
Michela Zanette1 Monica Di Cesare1
Monica Di Cesare1 Sonia Di Tella1
Sonia Di Tella1 Mario Clerici1,2
Mario Clerici1,2 Francesca Baglio1
Francesca Baglio1 Valeria Blasi1 for the BIF Group†
Valeria Blasi1 for the BIF Group†Adverse Childhood Experiences (ACE) are associated with an increased risk of cerebral, behavioral, and cognitive outcomes, and vulnerability to develop a Borderline Intellectual Functioning (BIF). BIF is characterized by an intelligence quotient (IQ) in the range 70–85, poor executive functioning, difficulties in emotion processing, and motor competencies. All these difficulties can lead to mental and/or neurodevelopmental disorders that require long-term care. Accordingly, we developed an intensive and multidomain rehabilitation program for children with ACE and BIF, termed the Movement Cognition and Narration of emotions Treatment (MCNT1.0). The efficacy of MCNT1.0 on cognitive and social functioning was demonstrated with a previously reported randomized controlled trial (RCT). To extend the impact of the treatment also to the motor domain a new version, called MCNT2.0, was implemented. The present study aims to verify the feasibility of MCNT2.0 and its effects on the motor domain. A quasi-experimental approach was used in which a group of 18 children with ACE and BIF were consecutively recruited and participated in the MCNT 2.0 program. Participants were compared with the MCNT1.0 group as an active comparator, using the dataset of the RCT. The two groups received a full evaluation comprising: the Wechsler Intelligent Scale for Children-IV (WISC-IV), the Movement-ABC (M-ABC), the Test of Gross Motor Development (TGMD), the Social Skills from Vineland Adaptive Behavioral Scale-II (VABS-II) and the Child Behavior Check List 6–18 (CBCL). An ANCOVA was carried out on changes in the scale scores from baseline with age and baseline score as covariates. Results showed a mean adherence to treatment of 0.85 (sd = 0.07), with no differences between groups in IQ, and Social Skills changes, while greater improvements for motor abilities were shown in the MCNT 2.0 group: M-ABC (p = 0.002), and TGMD (p = 0.002). Finally, greater improvement in the CBCL scale was observed in the MCNT 1.0 group (p = 0.002). Results indicate that due to its positive effects on cognitive, social participation and motor domains, MCNT2.0 may represent a protective factor against maladaptive outcomes of children with ACE and BIF.
Adverse environmental conditions are frequently associated with neuropsychiatric consequences during early age. Some studies suggested how the exposure to adverse childhood experience (ACE) contributes to altered structure and function in several neurobiological systems, mostly related to the limbic system, with a consequent “latent vulnerability” to multiple forms of youth and/or adult psychopathology (1–3). ACE can be defined as experiences requiring “significant adaptation by an average child” (4) and include “harms that affect children directly (e.g., abuse and neglect) and indirectly through their living environments (e.g., parental conflict, substance abuse, or mental illness)” (5). Borderline intellectual functioning (BIF) is an important and frequently unrecognized comorbid condition (6–9) with an increased risk of exposure to ACE compared to their peers (10) such as inadequate housing, low parental education, low social class, low income, absence of a parent, parental psychiatric morbidity (10). BIF is defined as a boundary condition between typical development and intellectual disability, characterized by an intelligence quotient (IQ) within the range 70–85, associated with difficulties in social participation and adaptability, and is recognized as a V code in the Diagnostic Statistical Manual-5 (11). Children with BIF exhibit difficulties in several developmental domains such as cognition, affectivity, sociality, and movement: learning disorders, impairment in executive functioning, receptive and expressive language, motor planning, emotional regulation, Theory Of Mind and behavioral difficulties are often detected (7, 12–18). Interestingly, children with BIF also exhibit a peculiar pattern of sleep organization characterized by an alteration of the cyclic alternating pattern, and a positive correlation between sleep duration and intellectual abilities (19, 20). In line with such evidence, several studies found a significant correlation between ACE and sleep disorders (21).
It has been shown that deprived environments negatively impact working memory, inhibitory control, cognitive flexibility (22–27), language (28, 29), and global intelligence (30). Accordingly, a recent study of a large cohort of 14,000 children showed that by the age of 2 years, children belonging to a low socio-economic environment had a 6 point lower IQ compared to their high socio-economic peers. This difference almost tripled when the same subjects were evaluated at the age of 16 (31). Finally, unpredictable and potentially threatening environments negatively impact the development of the emotional response and regulation systems with consequences on behavior and social relationships (4).
Children with ACE and BIF are thus a highly vulnerable population at risk of maladaptive outcomes, such as lifetime cognitive and mental disorders, anxiety, depression, substance abuse, externalizing/internalizing behavioral disorders, drop-out from schooling, and low income if left untreated.
To prevent the psychopathological drift following ACE and to respond to the several special needs of these children, we developed a rehabilitative intervention, termed the Movement Cognition and Narration of emotions Treatment [MCNT; (32)], which aimed at improving global intelligence, movement abilities and adaptive competences. MCNT lasts 9 months and consists in 3 h a day, 5 days a week of 3 laboratories: the Movement Lab, to improve fine and gross motor abilities; the Cognitive Lab, to improve reasoning, mental flexibility and wider executive functioning; and the Emotion Lab, to improve emotion recognition, comprehension and expression [for a detailed description of MCNT see the study protocol published (32)]. Indeed, this method targets the motor, cognitive and affective domains.
The efficacy of this intensive and multidomain experimental approach was investigated with a randomized controlled trial [RCT; (33)]. Results demonstrated that MCNT, which we shall rename here MCNT 1.0, was more effective than Standard Speech therapy (SST, usual care) in improving intellectual, adaptive and behavioral functioning in children with ACE and BIF, whereas no significant improvement was observed in motor abilities.
Moving from our previous results, we have focused on an ad hoc adjustment of the MCNT method, modifying the Movement Lab. We shall rename this new version as MCNT 2.0, in which we have abandoned the game therapy approach in the Movement Lab in lieu of a method focused on movement and body awareness, the Body Minding.
In the light of our previous results, which showed a poor effect of SST on cognitive and adaptive functioning, we preferred not to carry out a RCT with the SST as a control group but to directly compare the two versions of the MCNT intervention. Indeed, a treatment with poor efficacy might prevent the gain of competences relevant for children's development. Moreover, RCTs are expensive and not easy to implement in a routine care setting. For this reasons, we designed a quasi-experimental study (34) in which a group of 18 children with ACE and BIF were consecutively recruited to participate in the MCNT 2.0 program. This group was then compared with the children treated with MCNT 1.0 from the original RCT [(32, 33)].
The aims of the current study were to evaluate the feasibility of MCNT 2.0 intervention and its effect on motor skills in a sample of children with ACE and BIF. Based on our previous experience, we expected MCNT 2.0 to be feasible, and that compared to MCNT 1.0, the newer implementation would reveal a significant positive effect on motor abilities, without any differences between the two interventions on cognitive, social, and behavioral competencies.
The Study was approved by the Ethics Committee of the Don Gnocchi Foundation (DGF) and of the ASST S. Paolo and S. Carlo Hospital. All parents signed a written informed consent at the first meeting.
This was a quasi-experimental study in which a group of children with BIF and exposed to ACE were consecutively recruited and treated with MCNT 2.0, with all the children belonging to the group treated with MCNT 1.0 as an active comparator, consisting of 18 subjects that underwent the rehabilitation intervention in the Years 2016–2017. The MCNT 1.0 group belongs to the dataset of our previous RCT (33).
Participant assignment in the MCNT 2.0 group was not randomized. However, to support internal validity and to reduce sample differences, participants were selected from the same catchment area of the city of Milan and with the same inclusion/exclusion criteria of our previous RCT.
Inclusion criteria were: age range between 6–11 years old and attending primary mainstream school; a Full Scale Intelligence Quotient (FSIQ) score ranging from 70 to 85; presence of an impact on social functioning (school and/or family context) as derived from the clinical history. Since all children participating in the MCNT 1.0 program belonged to a middle, middle-low or low socio-economic status [SES < 39, (35)], we wanted the two groups to be matched for this parameter to control for confounding variables that may threaten the internal validity of the study. For this reason, we verified that none of the children of the MCNT 2.0 were of a high SES background.
Exclusion criteria were: presence of major neuropsychiatric disorders (such as ADHD and autism spectrum disorder); presence of neurological conditions such as epilepsy, traumatic brain injury, brain malformation and infectious disease involving the central nervous system. Other exclusion criteria considered were: the presence of systemic diseases such as diabetes or dysimmune disorders, genetic syndromes such as Down syndrome or Fragile X syndrome. Furthermore, a positive history for psychoactive drugs, particularly referring to current or past use of psychostimulants, neuroleptics, antidepressants, benzodiazepines, and antiepileptic drugs were also considered exclusion criteria.
The MCNT 2.0 group consisted of 18 children with ACE associated with BIF (age: mean = 7.68; sd = 1.25) and attending mainstream primary school in Italy treated with MCNT 2.0 (see methods section) in the years 2018/2019. Initially, 19 participants were enrolled but one child abandoned the study and was excluded from analyses. The MCNT 1.0 group consisted of 18 children with ACE and BIF (mean age = 7.78; sd = 1.31).
Characteristics of two groups at baseline are presented in Table 1.
To detect the presence of ACE we used the Environmental Stress Check-List [ESCL; (2)]. The ESCL consists in a listing of the V-codes from DSM-5, and Z-codes from ICD-10, that explore problems related to relational, neglect, physical, sexual and/or psychological abuse, educational and occupational, housing and economic, social exclusion or rejection, plus the presence of social services intervention, of major psychiatric diagnosis, and of substance abuse within the family members. A 0 (absence) to 1 (presence) score was attributed to each item after careful consideration of its relevance for the clinical manifestations. The ESCL total score ranges from 0 to 24 with higher values indicating a greater number of environmental stressful conditions.
The clinical assessment on motor, cognitive and behavioral domains was carried out at two time points (T0, within 2 months prior to the beginning of the treatment and after 9 months at T1 within 2 months after the end of the treatment).
Motor domain was assessed by a Neuro-Psychomotor in Developmental Age Therapist using:
1. The Movement-ABC [M-ABC; (36)], for the assessment of the motor skills, included manual dexterity, ball skills and static/dynamic balance; the total score was expressed in percentiles and fall into clinical range for scores below 6th percentile, into borderline range from 6th to 15th percentile and into normal range above 15th percentile;
2. The Test of Gross Motor Development [TGMD; (37)] through the assessment of both Locomotor and Object Control abilities give a measure of gross motor skill development, the Gross Motor Quotient (GMQ);
Cognitive domain was assessed by a neuropsychologist using:
1. The Wechsler Intelligence Scale for Children-IV [WISC-IV; (38)] to measure global intellectual functioning as full scale IQ (FSIQ) and the following indices: verbal comprehension index (VCI); perceptual reasoning index (PRI); working memory index (WMI); processing speed index (PSI). Children belonging to the MCNT 1.0 group were evaluated with the previous version of the scale, the WISC-III (39). Despite substantial differences between the two versions in the structure (the later revision of the Scale removed three and introduced five new subtests modifying its structure) and the construct of the indices and of the FSIQ, there is a very high correlation (0.89) in the FSIQ between the two versions, as previously reported (40). Indeed, we decided to use the FSIQ for the between group comparison because it is more stable and reliable when compared to the indices scores across the two versions of the WISC scale. Moreover, to avoid direct comparison of the scores of the two versions, we used delta values (post-pre-treatment scores), a longitudinal single subject change over time approach, to compare the two groups of children.
Behavioral and social skills were assessed by a psychologist using:
1. The Vineland Adaptive Behavioral Scale II [VABS-II; (41)], to assess social functioning, communication abilities, daily living skills, and a full scale quotient (FSQ) of adaptive functioning through a single interview with parents.
2. The Child Behavior Checklist 6–18 [CBCL 6–18; (42, 43)], in the Parent's Report Form, to evaluate emotional and behavioral problems in children and adolescents; data were expressed in Tscore and higher scores indicate greater problems; the total score can be interpreted as falling in the normal (<60 Tscore), borderline (60–63 Tscore), or clinical range (>63 Tscore).
The MCNT2.0 is an adapted version of MCNT1.0, an intensive and multimodal rehabilitation program, whose effectiveness has been demonstrated in our previous study (33). A detailed description of this method is present in the study protocol (32). MCNT consists of three laboratories (Lab), the Movement Lab, the Cognitive Lab and the Emotion Lab, in which children work in small group of seven to eight. Due to the lack of significant results, the Movement Lab was the only one that underwent substantial adjustment from MCNT 1.0–2.0.
Briefly, the first laboratory, the Cognitive Lab, aims at cognitive empowerment working on executive skills, such as fluid reasoning, problem solving, attention, inhibitory control, monitoring, switching, and academic competencies (reading, writing, and calculating) including listening comprehension with the use of the multimedia interactive whiteboard (MIW). The second lab, the Emotion Lab, adopts a relational dynamic approach to improve emotion expression, recognition, comprehension, and autoregulation. Purpose of the Emotion Lab is the “alphabetization” of the emotions (44). Spontaneous play, drawing, stories (invented and/or dramatized) and talking are the preferred tools used by the psychotherapist to achieve these goals. Finally, the third laboratory, the Movement Lab, fostered the improvement of global motor functioning with an game therapy approach using commercial gaming consoles. In the MCNT 2.0 the game therapy was substituted with a method focused on movement and body awareness. The focus was the body as a means through which we move in space and experience feelings. In more details, the Movement Lab 2.0 included two types of activities: (1) bodily movements to work on the “acting self” (45, 46) that is the sense of agency of own body during an action and include feelings and movement controls. This activity included sequences of coordination movements, from the simplest to the most complex, that involved bimanual and interlimbic coordination patterns but also eyes, ears, tongue, breath, and other cross movement designed for stimulating hemispheric brain interconnection and improving balance, stability, coordination and planning, speed, and accuracy in the movements. During the performance, children's attention was usually driven on “feeling the body.” Common games such as jumping rope, hopscotch, target shooting, balance play were performed to increase coordination, speed and accuracy; and (2) bodily awareness/perception to work on the “sensorial self” that is the sense of ownership of body and perceptual experience of all body parts in the external space (45–47). The child was guided toward the representation of his/her body through relaxation techniques guided by imaginative processes.
The MCNT 2.0 treatment was carried out for 9 months in a hospital setting. Children were accompanied from school to our Center with a shuttle service provided by our Institution. Children attended all the three Labs every day for 5 days/week, 3 h/day in the afternoon, working in small groups. For each group two specialized operators were assigned. Moreover, weekly meetings among professionals were carried out to monitor treatment, and to discuss emerging difficulties. Finally, at least two meeting with teachers, and at least 5 meetings with children's parents were provided. The number of the meetings was based on the specificity of each child situation. These meetings had the objective to create a support network and discuss the methodology of the intervention, evaluate the specific needs of each child, and find solutions to problems as they arose.
Adherence to treatment for each participant was calculated as the number of attended sessions divided by the number of total sessions and used as a measure of feasibility.
Since no preliminary data relative to motor abilities from our lab were available, the sample size was calculated according to data from the literature (48). The a priori sample size calculation was performed with G*Power software 3.1, considering a medium effect size (Cohen's f) = 0.25 (49), with an expected power of at least 0.80 and an alpha value 0.05. According to this procedure the estimated sample size a priori was 34.
Statistical analysis was conducted using SPSS software (version 24). Before proceeding to hypothesis testing, we checked the normal distribution for all measures using both the Kolmogorov-Smirnov and Shapiro-Wilk tests. A parametric (one-way ANOVA) or non-parametric (Mann-Whitney) comparison was performed as appropriate to compare baseline demographic and clinical characteristics of the two groups of children, MCNT 1.0 and MCNT 2.0. A chi-squared was used to test differences between groups for sex.
The measures considered in this study were changes in the scale scores from baseline (delta scores). For variables not normally distributed, a Bloom's transformation was applied to normalize scores. An analysis of covariance (ANCOVA), with age and pre intervention evaluation score as covariates, was carried out. Score differences were described using estimated mean, mean difference, and R2 model fitting. An α value of 0.05 was considered statistically significant, and all comparisons were 2-tailed. The false discovery rate (FDR) correction was used to adjust for multiple comparisons between the different measures (50).
The magnitude of effects was calculated and reported with effects size η2 interpreted as follows: 0.01 as a small effect; 0.06 as an intermediate effect; 0.140 and higher as a strong effect (51).
Except for M-ABC and CBCL all data were expressed in standard score.
Data relating to the Communication scale, Daily Living Skills and FSQ of VABS-II and the four indices of WISC-IV were investigated with a paired t-test in the MCNT 2.0 group only.
Table 1 shows baseline comparison between MCNT 1.0 and 2.0 groups. The two groups were matched for sample size, age, sex, SES, ESCL, and FSIQ.
Adherence for MCNT 1.0 was 0.88 (sd = 0.07), for MCNT 2.0 was 0.84 (sd = 0.07) with no statistical difference (Table 1). Both groups showed a very small number of drop-outs: 2 children in the MCNT 1.0 (one child moved to another country before post treatment evaluation, while another child had difficulties in working in a group setting) and 1 child in the MCNT 2.0 group (home to hospital distance was too great for the family to manage).
A detailed listing of the prevalence of each environmental stressor for each group was illustrated in Table 2.
To determine the effects of MCNT 2.0 on motor, cognitive and behavioral/social competencies, an ANCOVA analysis was performed. Delta values (post-pre-treatment) of each scale were compared between groups with age and baseline evaluation as covariates.
Results are reported in Table 3. To summarize, the MCNT 2.0 group showed greater motor ability improvements compared to MCNT 1.0, as detected by both scales: M-ABC (p = 0.002, before Bloom's transformation delta values for MCNT 1.0 mean = 7.85, sd = 15.19; MCNT 2.0 group mean = 40.95, sd = 21.89), and TGMD (p = 0.002). For cognitive abilities detected with the FSIQ, and for Social Skills as detected by the VABS II scale, no significant differences were detected between the two groups. For behavioral competencies, detected with the CBCL scale, a greater improvement was observed in the MCNT 1.0 group (p = 0.002).
To better detail the changes in the intellectual and adaptive functioning of the MNCT 2.0 group only, a paired t-test was performed on pre vs. post treatment scores.
Results are reported in Table 4. Data showed significant difference between pre and post treatment scoring for Perceptual Reasoning Index (PRI, p = 0.04) within the WISC IV evaluation, and for Communication (p = 0.04), Daily Living Skills (p = 0.04), and the Full-Scale Quotient (p = 0.04) within the VABS II.
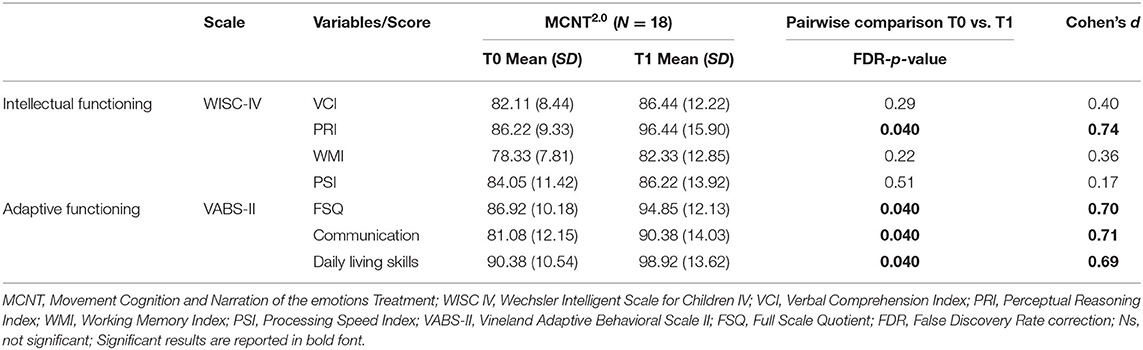
Table 4. Pairwise comparison pre vs. post-MCNT2.0 scores of WISC IV indices and VABS –II sub-scales.
In this work we report data showing the feasibility in term of treatment adherence of the MCNT 2.0 and its greater effects on motor abilities compared to the previous version of the treatment, the MNCT 1.0.
The previous version of the MCNT treatment, MCNT 1.0, was investigated with an RCT study (33) whose results showed a positive effect of the treatment on intellectual, social and behavioral competences in comparison to standard care (i.e., individual speech therapy). Despite MCNT 1.0 having implemented interventions targeting motor competences, significant improvement was not detected in this regard. For this reason, an adjusted version of MCNT was created, in which the movement training component was modified with the introduction of the Body-Minding, a body awareness and interlimbic coordination program; this version was re-named MCNT 2.0. Accordingly, first aim of this study was to evaluate the feasibility and the effects of this modification on the motor competencies. To this purpose, we conducted a quasi-experimental study in which data relative to a non-randomized group of children was compared to a secondary dataset from the previously mentioned RCT (34, 52).
The first result is the feasibility of the MCNT 2.0. Despite the intensity and the long duration of the treatment, we observed a very high adherence coupled with a very low number of drop-outs, demonstrating the feasibility of the MCNT 2.0 program with no differences with the original treatment. In both versions, a shuttle service accompanied children from school to our Institution. Moreover, both versions of the MCNT provided support for the participant's teachers and their families. Having facilitated the access to our Institution and having provided support to the schools enabled the creation of a network supporting children and their families that we believe explains such a high adherence to the rehabilitation treatment.
Another important result of the present study is the confirmation that the MCNT method is effective in the improvement of the intellectual abilities of children with BIF. This is in line with the results of the previous RCT study (33). Specifically, no difference between the two groups was observed in the changes observed after treatment. The two groups showed similar improvement in the full-scale IQ. Moreover, data from the MCNT 2.0 group, showed that this datum was likely due to the increment in the Perceptual Reasoning, as shown by the increment in the PRI. These data are in agreement with the results of our previous study (33) in which an increment in the Performance Quotient was observed in the MCNT 1.0 group. Both indices are measures of Fluid Reasoning (Gf), Comprehension-Knowledge (Gc), and Visual Processing (Gv). The metacognitive strategies used into the Cognitive Lab, which remained unmodified compared to the previous version, facilitated the empowerment of creative thinking through the exploration of new solutions, different perspectives, brainstorming techniques, and semantic association. As a consequence, the participants were able to create conceptual links, improved their long-term memory, and were able to more finely monitor their own cognitive and decision-making processes. This result cannot be imputed to the training of specific abilities that are tested within the IQ evaluation. Indeed, the MCNT approach does not involve any type of targeted cognitive training. The latter approach is controversial because some authors claim that it is effective in improving only the specific cognitive component that is trained. In this respect, some studies highlighted the difficulties in generalizing the trained ability to new learning context, from experimental setting to real life for example (53). In the MCNT, the Cognitive Lab focused on metacognitive strategies that are transversal to several cognitive competences, and more ecological. Our data are relevant in terms of clinical prognosis, because the improvement of global intellectual functioning can have a positive effect also on adaptive skills. Accordingly, a recent study (54) showed poorer emotion processing in adolescents with BIF when compared to healthy controls, and an inverse relationship between intellectual functioning and emotional awareness. The authors interpreted their results as evidence that borderline cognitive functioning affects mentalization processes and thus adaptive skills. For this reason, we consider it important, when working with children with BIF and ACE, to focus the treatment also on the intellectual abilities as defined above.
The main result of the present study is related to the effects of MCNT 2.0 on motor competencies in children with ACE and BIF. Data presented showed a significant increase in fine and gross motor functioning, as assessed with M-ABC and TGMD in children that underwent MCNT 2.0. This result relates to the only difference between the two versions of the MCNT. In the first version of the intervention, a Game Therapy approach was used, based on the use of the Wii and Xbox video game platforms, while the present version applied the Body-Minding, a method focused on both body movements with bimanual and interlimbic coordination exercises and body awareness. The choice of a Game therapy approach in the MCNT 1.0 was based on previous research that demonstrated its good efficacy in promoting engagement, motivation and motor competence in children (55–58) also in case of mental disability (59) and hand-eye coordination in adults (60). The present data, though, showed greater efficacy of the Body-Minding approach. A possible interpretation of this datum is that despite the “Game Therapy” approach is highly motivating and engaging for children, it only allows the choice of the type of game and its level of difficulty but not a finer tuning of the activities due to platform/game limitations. Conversely, the Body-Minding approach, even in a group setting, fostered an intervention on motor coordination and planning, and proprioceptive feeling, that was personalized and tailored on the basis of each child's strengths and difficulties. These data are in agreement with a previous study by Ferguson et al. (48) in which a Nintendo Wii Fit Training was compared to a Neuromotor Task Training (NTT), both carried out in a group setting to evaluate the impact on the performance of children with motor coordination problems. Children that participated in this study, similarly to our sample, attended mainstream primary schools and came from a low-income environment. Results showed that the NTT approach achieved broader and greater success than Wii training in motor proficiency, cardiorespiratory fitness and functional strength. On the contrary, children that underwent the Wii training, improved their anaerobic performance but their motor performance remained within the at-risk range. These data are relevant in light of the poor motor competences typically shown by children with BIF and ACE due to their difficulties in locomotor, object control, and fine motor skills (17, 61, 62).
The herein results on the motor performance of children with ACE and BIF are relevant because the motor difficulties observed in these children are strictly linked with the cognitive processes involving executive functions, such as inhibitory control and planning (63). Moreover, fine motor skills are highly related to the possibility to improve cognitive skills in pre-school children with intellectual disability and learning disorders (64). Indeed, the information arising from within the body, through visual, auditory, olfactive, tactile, and proprioceptive pathway need to be rapidly and efficiently processed and integrated to achieve a body awareness and to produce a goal-directed movement. Thus, intervening on the motor domain, can have an effect also on executive functions and vice-versa. Finally, driving attention on bodily sensation helps to feel, recognize, discriminate and regulate emotions that would otherwise remain confused, unwanted, and unexpressed. Indeed, in addition to cognitive and motor difficulties, children with ACE and BIF show emotional and behavioral difficulties associated (7, 13, 14, 65) with deficits in social competencies (12). Both versions of MCNT rehabilitation program provided specific interventions for emotion narration and recognition, the Emotion Lab, whose efficacy in improving social functioning and behavior was shown by the results of the RCT study (33). The effect of treatment on social functioning was also confirmed in the MCNT 2.0 group. Moreover, significant increment in all indices of the VABS II scale was observed within this group. Unfortunately, the complete profile at the VABS II was available only for the MCNT 2.0 group and thus no comparison with the other group was possible. For this reason, it is not possible to rule out that these results are due to a test-retest effect. Finally, opposite to the results of the RCT, the CBCL score did not show significant changes in the MCNT 2.0 group. A possible interpretation of this result relates to differences in the specific difficulties and/or strengths of the children belonging to the two groups.
To summarize, children attending the MCNT 2.0 intervention improved their performances in all domains, especially in the motor domain whose improvement was more than one standard deviation. Notwithstanding, despite an increment in scores <1 standard deviation in the FSIQ and in the VABS II total score, these data are highly relevant from a clinical perspective for two main reasons. The first relates to the natural history of children with BIF and ACE that is not favorable, but is characterized by a high risk of long-term consequences. Thus, gaining a global improvement is potentially of great relevance. The second relates to the findings of a previous work from our group (33) in which results showed that working only on specific academic abilities produced improvement only in specific areas such as verbal memory and comprehension and did not generalize to adaptive and intellectual abilities. Moreover, this domain specific approach was associated with a paradoxical effect on behavior represented by a worsening on the CBCL scale. Consequently, our data support clinical decisions suggesting the importance of a multi domain therapeutic approach. To determine the long term clinical relevance of the MCNT intervention follow-up studies will be needed.
The present study is not free from limitations. This is a quasi-experimental study whose data from a non-randomized sample of subjects is compared to a secondary dataset from an RCT, according to the “Good Research Practices for Comparative Effectiveness Research” (34, 52, 66, 67). This approach potentially results in a selection bias of the children. To avoid this issue, we used the same inclusion criteria from the previous study and we included the first 20 consecutive children eligible for the study. Moreover, the children belonged to the same socioeconomic environment and from the same area of the children participating in the RCT. Moreover, the small group of participants prevent us from generalizing to the broad population of children with ACE and BIF. Finally, more follow-up is needed to evaluate the long-term effects of the treatment.
Despite these limitations, the herein data are relevant because of the importance to intervene in the developmental course of children experiencing ACE and with a BIF. This population is very vulnerable due to the high risk of school drop-out, poverty, and psychological problems in the adulthood (10, 13, 14, 68). Several data indicate that, in socio-economic disadvantaged contexts, children's IQ, together with the quality of the child/parent relationship, is one of the most important protective factor against maladaptive outcomes (36, 69). Indeed, one of the main goals of MCNT is to support resilience, through the multidomain and integrated approach that promotes the improvement of both the intellectual functioning and the emotional/relational competences of the children. The relational dimension is the real core of MCNT: everyone has an emotional and cognitive potential that can be enriched by the positive interaction with competent figures.
To conclude, our data support the starting hypothesis of the positive effects of our intensive, multidomain approach in children with ACE and BIF, and that a body awareness and interlimbic coordination approach has a greater effect in improving the motor functioning. The treatment of neurodevelopmental disorders is often expensive due to the necessity of a long-term care (70, 71). Is not clear how protective factors and resilience work in modifying the association between ACE and psychopathology. On the basis of our experience, we believe that a multimodal approach intervening on the three major domains, the cognitive, the motor, and the emotion, may positively impact the developmental processes and thus help prevent maladaptive outcomes.
The datasets presented in this article are not readily available and will not be made publicly available because: the informed consent approved by the Ethics committee did not include any statement regarding the possibility to share the data. Requests to access the datasets should be directed to Gisella Baglio, Z2JhZ2xpb0Bkb25nbm9jY2hpLml0.
The studies involving human participants were reviewed and approved by the Ethics Committees of the Don Gnocchi Foundation and of the ASST S. Paolo and S. Carlo Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
GB, MZ, FB, and VB conceived the study and wrote the manuscript. GB, VB, MC, and MZ executed the study. SD helped with statistical analyses. All authors contributed to refinement of the manuscript and approved the final content.
This work was funded by the Charity Fund of the Banca Intesa Foundation and by the Italian Ministry of Health (Ricerca Corrente).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We wish to thank all the children and their families for their participation to the study.
Bergsland Niels, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Bolognesi Elisabetta, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Cabinio Monia, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Canevini Maria Paola, Azienda Socio Sanitaria Territoriale- ASST S. Paolo and S. Carlo Hospital, Milan, Italy, Department of Health Sciences, University of Milan, Milan, Italy; Galbiati Chiara, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Giangiacomo Alice, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Guerini Franca Rosa, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Isernia Sara, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Isola Giulia, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Mancuso Roberta, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Marin Alessandra, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Marcora Elena, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Martino Antonio, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Milone Luana, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Pagliari Chiara, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Don Carlo Gnocchi Foundation Onlus, Milan, Italy; Rumi Viviana, Azienda Socio Sanitaria Territoriale- ASST S. Paolo and S. Carlo Hospital, Milan, Italy; Spada Cinzia, Azienda Socio Sanitaria Territoriale- ASST S. Paolo and S. Carlo Hospital, Milan, Italy; Walder Mauro, Azienda Socio Sanitaria Territoriale- ASST S. Paolo and S. Carlo Hospital, Milan, Italy.
1. McCrory E, Viding E. The theory of latent vulnerability: reconceptualizing the link between childhood maltreatment and psychiatric disorder. Develop Psychopathol. (2015) 27:493–505. doi: 10.1017/S0954579415000115
2. Blasi V, Pirastru A, Cabinio M, Di Tella S, Laganà MM, Giangiacomo A, et al. Early life adversities and borderline intellectual functioning negatively impact limbic system connectivity in childhood: a connectomics-based study. Front Psychiatry. (2020) 11:955. doi: 10.3389/fpsyt.2020.497116
3. Baglio F, Cabinio M, Ricci C, Baglio G, Lipari S, Griffanti L, et al. Abnormal development of sensory-motor, visual temporal and parahippocampal cortex in children with learning disabilities and borderline intellectual functioning. Front Human Neurosci. (2014) 8:806. doi: 10.3389/fnhum.2014.00806
4. McLaughlin KA. Future directions in childhood adversity and youth psychopathology. J Clin Child Adolesc Psychol. (2016) 45:361–82. doi: 10.1080/15374416.2015.1110823
5. Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. (2017) 2:e356–66. doi: 10.1016/S2468-2667(17)30118-4
6. Wieland J, Zitman FG. It is time to bring borderline intellectual functioning back into the main fold of classification systems. BJPsych Bull. (2016) 40:204–6. doi: 10.1192/pb.bp.115.051490
7. Hassiotis A. Borderline intellectual functioning and neurodevelopmental disorders: prevalence, comorbidities and treatment approaches. Adv Mental Health Intellect Disabil. (2015) 9:28. doi: 10.1108/AMHID-06-2015-0028
8. Ninivaggi F. Borderline intellectual functioning in children and adolescents: reexamining an underrecognized yet prevalent clinical comorbidity. Conn Med. (2001) 65:7–11.
9. Fernell E, Ek U. Borderline intellectual functioning in children and adolescents – insufficiently recognized difficulties. Acta Paediatrica. (2010) 99:748–53. doi: 10.1111/j.1651-2227.2010.01707
10. Hassiotis A, Brown E, Harris J, Helm D, Munir K, Salvador-Carulla L, et al. Association of borderline intellectual functioning and adverse childhood experience with adult psychiatric morbidity. Findings from a British birth cohort. BMC Psychiatry. (2019) 19:387. doi: 10.1186/s12888-019-2376-0
11. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Publications (2013).
12. Baglio G, Blasi V, Sangiuliano Intra F, Castelli I, Massaro D, Baglio F, et al. Social competence in children with borderline intellectual functioning: delayed development of theory of mind across all complexity levels. Front Psychol. (2016) 7:1604. doi: 10.3389/fpsyg.2016.01604
13. Peltopuro M, Ahonen T, Kaartinen J, Seppälä H., Närhi V. Borderline intellectual functioning: a systematic literature review. Intellect Dev Disabil. (2014) 52:419–43. doi: 10.1352/1934-9556-52.6.419
14. Salvador-Carulla L, García-Gutiérrez J, Ruiz Gutiérrez-Colosía M, Artigas J, Ibáñez J, Pérez J, et al. Borderline intellectual functioning: consensus and good practice guidelines. Rev Psiquiatr Salud Ment. (2013) 6:109–20. doi: 10.1016/j.rpsmen.2012.12.002
15. Pulina F, Lanfranchi S, Henry L, Vianello R. Intellectual profile in school-aged children with borderline intellectual functioning. Res Dev Disabil. (2019) 95:103498. doi: 10.1016/j.ridd.2019.103498
16. Predescu E, Sipos R, Pop C, Ciocan A, Rus D. Executive functions and emotion regulation in attention-deficit/hyperactivity disorder and borderline intellectual disability. J Clin Med. (2020) 9:986. doi: 10.3390/jcm9040986
17. Alesi M, Battaglia G, Pepi A, Bianco A, Palma A. Gross motor proficiency and intellectual functioning: a comparison among children with Down syndrome, children with borderline intellectual functioning, and typically developing children. Medicine. (2018) 97:e12737. doi: 10.1097/MD.0000000000012737
18. Contena B, Taddei S. Psychological and cognitive aspects of borderline intellectual functioning. Eur Psychol. (2017) 22:159–66. doi: 10.1027/1016-9040/a000293
19. Esposito M, Carotenuto M. Borderline intellectual functioning and sleep: the role of cyclic alternating pattern. Neurosci Lett. (2010) 485:89–93. doi: 10.1016/j.neulet.2010.08.062
20. Esposito M, Carotenuto M. Intellectual disabilities and power spectra analysis during sleep: a new perspective on borderline intellectual functioning. Intellect Dev Disabil. (2014) 58:421–9. doi: 10.1111/jir.12036
21. Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. (2015) 16:320–30. doi: 10.1016/j.sleep.2014.12.013
22. Blair C, Raver CC. Child development in the context of adversity: experiential canalization of brain and behavior. Am Psychol. (2012) 67:309. doi: 10.1037/a0027493
23. Farah MJ, Shera DM, Savage JH, Betancourt L, Giannetta JM, Brodsky NL, et al. Childhood poverty: specific associations with neurocognitive development. Brain Res. (2006) 1110:166–174. doi: 10.1016/j.brainres.2006.06.072
24. Noble KG, McCandliss BD, Farah MJ. Socioeconomic gradients predict individual differences in neurocognitive abilities. Dev Sci. (2007) 10:464–80. doi: 10.1111/j.1467-7687.2007.00600.x
25. Noble KG, Norman MF, Farah MJ. Neurocognitive correlates of socioeconomic status in kindergarten children. Dev Sci. (2005) 8:74–87. doi: 10.1111/j.1467-7687.2005.00394.x
26. Raver C, Blair C, Willoughby M. The family life project key investigators poverty as a predictor of 4-year-olds' executive function: new perspectives on models of differential susceptibility. Dev Psychol. (2013) 49:292–304. doi: 10.1037/a0028343
27. Clearfield MW, Niman LC. SES affects infant cognitive flexibility. Infant Behav Dev. (2012) 35:29–35. doi: 10.1016/j.infbeh.2011.09.007
28. Fernald A, Marchman VA, Weisleder A. SES differences in language processing skill and vocabulary are evident at 18 months. Dev Sci. (2013) 16:234–48. doi: 10.1111/desc.12019
29. Weisleder A, Fernald A. Talking to children matters: early language experience strengthens processing and builds vocabulary. Psychol Sci. (2013) 24:2143–52. doi: 10.1177/0956797613488145
30. O'Connor TG, Rutter M, Beckett C, Keaveney L, Kreppner JM. The effects of global severe privation on cognitive competence: extension and longitudinal follow-up. Child Dev. (2000) 71:376–90. doi: 10.1111/1467-8624.00151
31. Von Stumm S, Plomin R. Socioeconomic status and the growth of intelligence from infancy through adolescence. Intelligence. (2015) 48:30–6. doi: 10.1016/j.intell.2014.10.002
32. Blasi V, Baglio G, Baglio F, Canevini M, Zanette M. Movement cognition and narration of the emotions treatment versus standard speech therapy in the treatment of children with borderline intellectual functioning: a randomized controlled trial. BMC Psychiatry. (2017) 17:146. doi: 10.1186/s12888-017-1309-z
33. Blasi V, Zanette M, Baglio G, Giangiacomo A, Di Tella S, Canevini MP, et al. Intervening on the developmental course of children with borderline intellectual functioning with a multimodal intervention: results from a randomized controlled trial. Front Psychol. (2020) 11:679. doi: 10.3389/fpsyg.2020.00679
34. Berger ML, Mamdani M, Atkins D, Johnson ML. Good research practices for comparative effectiveness research: defining, reporting and interpreting nonrandomized studies of treatment effects using secondary data sources: the ISPOR good research practices for retrospective database analysis task force report—part I. Value Health. (2009) 12:1044–52. doi: 10.1111/j.1524-4733.2009.00600.x
35. Hollingshead AB. Four Factor Index of Social Status. New Haven, Conn: Yale University. (1975). p. 47–55.
36. Henderson S, Sugden D. Movement Assessment Battery for Children. London:The Psychological Corporation (1992).
37. Ulrich DA. Test TGM. Test di valutazione delle abilità grosso-motorie. Trento, Italy: Edizioni Erickson (1992).
38. Orsini A, Pezzuti L, Picone L. WISC-IV: Contributo alla Taratura Italiana [WISC-IV Italian Edition]. Florence: Giunti OS (2012).
39. Orsini A, Picone L. WISC-III: Wechsler Intelligence scale for Children. Adattamento italiano Florence: Giunti OS (2006).
40. Flanagan DP, Kaufman AS. Fondamenti per l'assessment con la WISC-IV. Firenze: Giunti OS Organizzazioni speciali (2012).
41. Sparrow SSP, Cicchetti DV, Balla DA, Balboni G. Vineland-2: Vineland adaptive behavior scales Second Edition-Survey Forms–Manuale. Florence: Giunti OS (2016).
42. Achenbach TM, Rescorla L. Manual for the ASEBA School-Age forms & Profiles: An Integrated System of Multi-Informant Assessment. Burlington, VT: Aseba (2001).
43. Achenbach T, Rescorla L. Multicultural Supplement to the Manual for the ASEBA School-Age forms & Profiles. Burlington VT: University of Vermont Research Center for Children, Youth, & Families (2007).
44. Blasi V, Zanette M, Ferro A. Mentalization as alphabetization of the emotions: oscillation between the opening and closing of possible worlds. Proc Int Forum Psychoanal. (2017) 26:75–84. doi: 10.1080/0803706X.2016.1245440
45. Gallagher S. How the Body Shapes the Mind. Oxford University: Oxford Scholarship Online (2005). doi: 10.1093/0199271941.001.0001
46. Tsakiris M, Prabhu G, Haggard P. Having a body versus moving your body: how agency structures body-ownership. Conscious Cogn. (2006) 15:423–32. doi: 10.1016/j.concog.2005.09.004
47. Roll J-P, Roll R, Velay J-L. Proprioception as a link between body space and extra-personal space. In: Paillard J, editors. Brain and Space. Oxford: Oxford University Press (1991). p. 112–32.
48. Ferguson G, Jelsma D, Jelsma J, Smits-Engelsman B. The efficacy of two task-orientated interventions for children with developmental coordination disorder: neuromotor task training and nintendo Wii fit training. Res Dev Disabil. (2013) 34:2449–61. doi: 10.1016/j.ridd.2013.05.007
49. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press (1969).
50. Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. 29:1165–88. doi: 10.1214/aos/1013699998
51. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York, NY: Routledge (2013).
52. World Health Organization. Monitoring and Evaluating Digital Health Interventions: a Practical Guide to Conducting Research and Assessment. Geneva: World Health Organization (2016).
53. Melby-Lervåg M, Redick TS, Hulme C. Working memory training does not improve performance on measures of intelligence or other measures of “far transfer”: evidence from a meta-analytic review. Perspect Psychol Sci. (2016) 11:512–34. doi: 10.1177/1745691616635612
54. Smirni D, Smirni P, Di Martino G, Operto FF, Carotenuto M. Emotional awareness and cognitive performance in borderline intellectual functioning young adolescents. J Nervous Mental Dis. (2019) 207:365–70. doi: 10.1097/NMD.0000000000000972
55. Sandlund M, McDonough S, Häger-Ross C. Interactive computer play in rehabilitation of children with sensorimotor disorders: a systematic review. Dev Med Child Neurol. (2009) 51:173–9. doi: 10.1111/j.1469-8749.2008.03184.x
56. White K, Schofield G, Kilding AE. Energy expended by boys playing active video games. J Sci Med Sport. (2011) 14:130–4. doi: 10.1016/j.jsams.2010.07.005
57. Jelsma D, Geuze RH, Mombarg R, Smits-Engelsman BCM. The impact of Wii fit intervention on dynamic balance control in children with probable developmental coordination disorder and balance problems. Hum Movement Sci. (2014) 33:404–18. doi: 10.1016/j.humov.2013.12.007
58. Hammond J, Jones V, Hill EL, Green D, Male I. An investigation of the impact of regular use of the W ii F it to improve motor and psychosocial outcomes in children with movement difficulties: a pilot study. Child. (2014) 40:165–75. doi: 10.1111/cch.12029
59. Berg P, Becker T, Martian A, Danielle PK, Wingen J. Motor control outcomes following Nintendo Wii use by a child with down syndrome. Pediatr Phys Ther. (2012) 24:78–84. doi: 10.1097/PEP.0b013e31823e05e6
60. Giannotti D, Patrizi G, Di Rocco G, Vestri AR, Semproni CP, Fiengo L, et al. Play to become a surgeon: impact of Nintendo Wii training on laparoscopic skills. PLoS One. (2013) 8:e57372. doi: 10.1371/journal.pone.0057372
61. Vuijk PJ, Hartman E, Scherder E, Visscher C. Motor performance of children with mild intellectual disability and borderline intellectual functioning. J Intellect Disabil Res. (2010) 54:955–65. doi: 10.1111/j.1365-2788.2010.01318.x
62. Westendorp M, Houwen S, Hartman E, Visscher C. Are gross motor skills and sports participation related in children with intellectual disabilities? J Intellect Disabil Res. (2011) 32:1147–53. doi: 10.1016/j.ridd.2011.01.009
63. Hartman E, Houwen S, Scherder E, Visscher C. On the relationship between motor performance and executive functioning in children with intellectual disabilities. J Intellect Disabil Res. (2010) 54:468–77. doi: 10.1111/j.1365-2788.2010.01284.x
64. Kim H, Carlson AG, Curby TW, Winsler A. Relations among motor, social, and cognitive skills in pre-kindergarten children with developmental disabilities. Res Dev Disabil. (2016) 53:43–60. doi: 10.1016/j.ridd.2016.01.016
65. Dekker MC, Koot HM, Ende, J.vd, Verhulst FC. Emotional and behavioral problems in children and adolescents with and without intellectual disability. J Child Psychol Psychiatry. (2002) 43:1087–98. doi: 10.1111/1469-7610.00235
66. Cox E, Martin BC, Van Staa T, Garbe E, Siebert U, Johnson ML. Good research practices for comparative effectiveness research: approaches to mitigate bias and confounding in the design of nonrandomized studies of treatment effects using secondary data sources: the International society for pharmacoeconomics and outcomes research good research practices for retrospective database analysis task force report—part II. Value Health. (2009) 12:1053–61. doi: 10.1111/j.1524-4733.2009.00601.x
67. Johnson ML, Crown W, Martin BC, Dormuth CR, Siebert U. Good research practices for comparative effectiveness research: analytic methods to improve causal inference from nonrandomized studies of treatment effects using secondary data sources: the ISPOR good research practices for retrospective database analysis task force report—part III. Value in Health. (2009) 12:1062–1073. doi: 10.1111/j.1524-4733.2009.00602.x
68. Emerson E, Einfeld S, Stancliffe RJ. The mental health of young children with intellectual disabilities or borderline intellectual functioning. Soc Psychiatr Psychiatr Epidemiol. (2010) 45:579–87. doi: 10.1007/s00127-009-0100-y
69. Vanderbilt-Adriance E, Shaw DS. Protective factors and the development of resilience in the context of neighborhood disadvantage. J Abnormal Child Psychol. (2008) 36:887–901. doi: 10.1007/s10802-008-9220-1
70. Singh NN. Advances in neurodevelopmental disorders: an editorial. Adv Neurodev Disord. (2017) 1:1–2. doi: 10.1007/s41252-017-0008-6
Keywords: adverse childhood experience, cognitive-behavioral and motor impairment, borderline intellectual functioning, multimodal rehabilitation, stressful environment, emotional deregulation
Citation: Baglio G, Zanette M, Di Cesare M, Di Tella S, Clerici M, Baglio F and Blasi V (2021) Rehabilitation and Disability Spectrum From Adverse Childhood Experience: The Impact of the Movement Cognition and Narration of Emotions Treatment (MCNT) Version 2.0. Front. Psychiatry 11:609819. doi: 10.3389/fpsyt.2020.609819
Received: 05 October 2020; Accepted: 14 December 2020;
Published: 25 January 2021.
Edited by:
Beatrice Arosio, University of Milan, ItalyReviewed by:
Marco Carotenuto, University of Campania Luigi Vanvitelli, ItalyCopyright © 2021 Baglio, Zanette, Di Cesare, Di Tella, Clerici, Baglio and Blasi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gisella Baglio, Z2JhZ2xpb0Bkb25nbm9jY2hpLml0
†Author name and affiliation are discussed in section BIF Group
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.