- 1Department of Psychiatry, Second Xiangya Hospital, Central South University, Changsha, China
- 2Department of Psychiatry, The First Affiliated Hospital of Nanchang University, Nanchang, China
- 3Department of Psychology, Jiangxi Mental Hospital, Nanchang, China
- 4Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Changsha, China
Background: Even though methadone maintenance treatment (MMT) is effective and widely recommended, it is widely misunderstood and stigmatized. This study aimed to explore people's attitudes and beliefs toward MMT, and stigmatization of MMT patients in China.
Methods: This randomized, vignette-based study enrolled 1,066 household respondents (552 males and 514 females, response rate is 88.83%, 86.00% in vignette 1 and 91.66% in vignette 2) from two communities in China. Respondents initially completed questionnaires on sociodemographic characteristics and their knowledge about methadone and MMT. They were then randomly assigned to vignette 1 (described a patient receiving MMT) or vignette 2 (described a patient receiving amlodipine treatment). The labeling, stereotyping, and social distance toward the individual described in the vignettes were evaluated.
Results: In these two vignettes, respondents showed a significantly higher level of stigma and discrimination toward the patient receiving MMT than the patient receiving amlodipine treatment. Approximately 60% of respondents believed that methadone is a type of addictive drug and that participating in MMT is a way to get high. Over 60% of respondents labeled the heroin-dependent patient who is receiving MMT as an addict even though the patient has not used heroin for several years; about 80% of them believed that the patient has undesirable characteristics and expressed a strong desire for social distance.
Conclusions: People's misunderstanding of MMT, and stigmatization of MMT patients were very common among populations in the communities in China. To maximize MMT patients benefiting from MMT programs, more efforts are needed to minimize the impact of MMT-related stigma.
Introduction
Methadone Maintenance Treatment in China
In China, opioids remain one of the most widely used illegal drugs (1), and illicit opioid use continues to drive the human immunodeficiency virus (HIV) epidemics and increase crime (2, 3). To address the severe social and medical problems associated with illicit opioid use, China initiated the methadone maintenance treatment (MMT) program with just eight sites in 2004. By the end of 2016, the program has been extended to 789 sites, with 162,000 heroin users under treatment, as stated by the annual report on drug control in China in 2017 (from the Office of China National Narcotics Control Commission, http://jhak.com/grwz/20170125.pdf). MMT has a long-established efficacy in preventing illicit opioid use, reducing crime, and decreasing the risk of HIV and hepatitis C virus (HCV) transmission (4–6).
Even though MMT is effective and widely recommended, it is still largely misunderstood and stigmatized (7–10). Negative attitudes and beliefs toward MMT are widespread, such as taking methadone is a way to get high, and patients receiving MMT are characterized as incompetent, untrustworthy, irresponsible, and has a weak willpower (11). Due to these prejudice, stereotypes, and discrimination, MMT patients have been stigmatized widely in the community (12). Research indicates that stigma against MMT gives rise to many negative consequences, including increased involvement in risky behavior, non-participation, treatment withdrawal, delayed recovery, and reintegration process (13–16).
Stigmatization Toward MMT Patients
A previous study reported that MMT service providers had a high-level stigma toward MMT patients (17). Community-based social support may play a more crucial role in improving and continuing the treatment of individuals under MMT (18). Exploring the community population's attitudes and beliefs toward MMT and stigmatization of MMT patients in China will help us develop better MMT. Thus, the present study aimed to assess public stigmatizing attitudes toward the patients receiving MMT in China, based on Link and Phelan's conception of the stigma process. According to Link and Phelan's (19) view of stigma [stigma occurs when the following interrelated components converge: “(1) labeling: people distinguish and label human differences; (2) stereotyping: the labeled is linked to undesirable characteristics; (3) separating: the labeled is separated as an out-group; (4) the labeled experience status loss and discrimination; and (5) a power situation is necessary to allow these process to unfold]”, we hypothesize that misunderstanding of MMT and stigmatization of MMT patients would also be very common among populations in the communities in China.
Methods
Research Procedure and Respondents
The data was collected between December 2018 and March 2019. Participants were enrolled from an urban community in the Tianxin district of Changsha city and a rural community in the Junshan district of Yueyang city, Hunan province. Participants were randomly selected from the household-based sample in these communities by Excel worksheet. In total, 800 households were selected from the urban community with 3,363 households, and 400 households were selected from the rural community with 1,046 households. One person at least 16 years old was randomly chosen in each family. A total of 1,200 individuals were included in this study. A local organizer in each community brought interviewers into each house and gave a brief account of the survey. Respondents were provided with 10 CNY to compensate for their participation. Ethical approval was obtained from the Ethics Committee of Jiangxi Mental Hospital (No. 20180204).
Research Instruments
In this community-based, randomized case vignette study, we developed a survey booklet, including the respondents' demography and knowledge about MMT, as well as two vignettes to assess stigmatization of MMT. Respondents in the study group received vignette 1, describing a patient receiving MMT, while respondents in the control group received vignette 2, illustrating a patient receiving amlodipine treatment. Each participant was randomly given one of the vignettes.
Public Knowledge About MMT
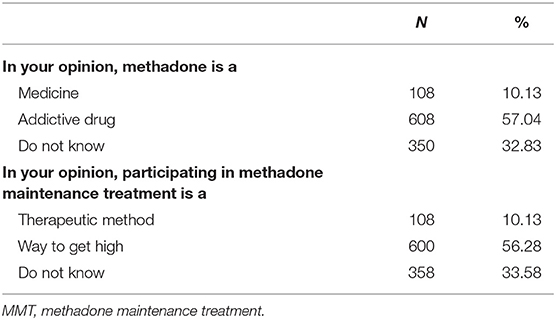
A set of questions were asked to examine the participants' knowledge about MMT, such as “In your opinion, methadone is a—(1) medicine, (2) addictive drug, (3) do not know? In your opinion, participating in MMT is a—(1) therapeutic method, (2) means of drug addiction, (3) do not know?”
Labeling
Participants were asked to define the person depicted in the vignette (1) normal person, (2) patient, and (3) addict with the question “In your opinion, Zhangsan is a ______.”
Stereotyping
The semantic differential scale was used to assess the measure of stereotyping (20). The scale comprises seven pairs of polar adjectives on seven 7-point rating scales. Scores ranged from 1 to 7, lower values indicating a more negative stereotype. Participants were categorized as having a negative stereotype about the person depicted in the vignette if they scored below 4 points.
Social Distance
The social distance scale (21–23) was used to assess participants' desire for social distance. Participants were asked about their willingness to engage in five forms of social contact with the person depicted in the vignette including (1) “become a neighbor,” (2) “spend an evening socializing,” (3) “make friends,” (4) “start working closely,” and (5) “become related as a family.” These items were rated on a 4-point scale from 1 (definitely) to 4 (definitely not). The mean score ranged from 1 to 4 points, with a higher score reflecting a stronger desire for social distance. Participants were viewed as unwilling to engage in these forms of interaction if they scored above the point of 2.5.
Vignettes
We constructed one vignette depicting a patient receiving MMT and the other describing a patient receiving amlodipine treatment. Patients in the two vignettes met ICD-10 criteria for opioids dependent, currently abstinent, but receiving treatment with methadone, and hypertension, respectively.
Vignette 1: Patient Receiving MMT
Zhang San is a 38-year-old male. His first ingestion of heroin was at his friend's house approximately 10 years ago. In the subsequent months, the intake dosage gradually increased. He gradually lost interest in other activities in life. Because of heroin use, he lost his job. Three years ago, he initiated an attempt to stop heroin use and went to an MMT clinic to receive MMT. In the past 3 years, he has taken his medication on time and has not used heroin. He has found a job and has been working continuously since then.
Vignette 2: Patient Receiving Amlodipine Treatment
Zhang San is a 38-year-old male. Three years ago, he received an examination at the hospital due to occasional dizziness and lack of strength. His blood pressure was repeatedly measured over 170/100 mmHg. Zhang San was prescribed with amlodipine. In the past 3 years, he has taken his medication on time and keep his blood pressure in the normal range. He has been working continuously.
Statistical Analysis
All statistical analyses were conducted in SPSS version 20.0 software package. The t-tests (for continuous variables) and χ2 analysis (for categorical variables) were performed to compare the differences in public stigma toward the MMT patient and the hypertension patient. Moreover, correlation analysis was performed to examine the correlation between stigmatization and the age, sex, marital status, education, resident, and monthly income of the community residents.
Results
Of the 1,200 individuals identified in the survey, 134 (11.17%) lost contact. Thus, 1,066 (88.83%) participants were (86.00% in vignette 1 and 91.66% in vignette 2) included in this study. The demographic information is shown in Table 1. There are no differences in the sociodemographic characteristics between participants who responded to the vignette of the patient receiving amlodipine treatment and those who responded to the vignette of the patient receiving MMT.
Community Residents' Understanding of MMT
Approximately 60% of respondents believed that methadone is a type of addictive drug and that participating in MMT is a way to get high. Over 30% of the respondents expressed that they did not know what methadone is or what MMT entails. Only 10.13% of the respondents acknowledged methadone as medicine and perceived participating in MMT as a treatment method (Table 2).
Community Residents' Stigmatization of MMT Patients
Labeling
More than half (64.00%) of the respondents labeled the patient receiving MMT as addicts, 18.18% identified a patient's label. Only 17.82% identified a normal label for the MMT patient, whereas 67.83% labeled the hypertension patient receiving amlodipine treatment as normal (Table 3).

Table 3. Community residents' stigmatization toward the patient receiving AT and the patient receiving MMT.
Stereotyping
The stereotypes about the patient receiving MMT were generally negative. Compared with the hypertension patient (5.35 ± 1.12), the heroin-dependent patient receiving MMT (3.47 ± 1.75) was rated far more negatively. The majority (76.46%) of respondents had a negative stereotype about the MMT patient, whereas only 10.47% had a negative stereotype about the patient receiving amlodipine treatment (Table 3).
Social Distance
Most of the respondents expressed a high-level desire for social distance from the patient receiving MMT. Approximately 90% of respondents were unwilling to make friends with the heroin-dependent patient receiving MMT and have the person marry into the family. Most (78.54%) were unwilling to start working closely with the person; more than half of them were unwilling to move next door to and spend an evening socializing with the person. Respondents showed a higher level of desire for social distance from the patient receiving MMT (3.33 ± 0.79) than the patient receiving amlodipine treatment (1.72 ± 0.31). More details are shown in Table 3.
Correlation analysis did not find any associations between sociodemographic with the views about MMT, negative stereotype, or social intolerance toward the patient receiving MMT (as shown in the Supplementary Material).
Discussion
As far as we know, this is the first study to evaluate the misunderstanding of MMT and stigmatization toward MMT patients in China. Findings of this study reveal that misunderstanding of MMT is widely spread in the community in Hunan, China. Although MMT effectively reduces opioids use, criminality, and adverse health effects, only 10.13% of the respondents acknowledged methadone as medicine and perceived MMT as a treatment method. Consistent with reports that MMT continues to be largely misunderstood (7, 11, 12), many respondents perceived methadone as a type of addictive drug and that participating in MMT is a way to get high.
High Level of Stigma and Discrimination Toward MMT Patients
In these two vignettes, respondents showed a significantly higher level of stigma and discrimination toward patients receiving MMT than patients receiving amlodipine treatment. Approximately 60% of respondents believed that methadone is a type of addictive drug and that individuals participate in MMT to get high. Over 60% of respondents labeled the heroin-dependent patient who is receiving MMT as an addict. About 80% believed the patient has undesirable characteristics and expressed a strong desire for social distance.
These findings also show stigmatization of MMT patients compared with patients with other chronic conditions that require treatment such as hypertension. The majority of the community respondents in the community labeled the methadone patient as an addict, believing the patient receiving MMT is bad, insincere, dangerous, unpredictable, unreliable, weak, and selfish. Since negative stereotype could evoke community rejection (24), it is no surprise that the respondents expressed a strong desire for social distance across different domains of social interaction with patients receiving MMT. Participants expressed that the more intimate the interaction, the stronger the desire to keep a distance. Thus, the vast majority were unwilling to make friends with the patient receiving MMT or have the person marry into the family.
These findings in our study suggest that widespread misunderstanding of MMT and stigmatization of the patients in the community should be taken into account in the community-based MMT program. China has established the largest MMT network in the world to address the serious social and medical problems associated with illicit opioid use. However, the present study indicates that community residents are far from being well-prepared to accept methadone patients. The continuing stigmatization of methadone patients may undermine the government's efforts to help them tackle their condition. Interventions to resolve misunderstandings and reduce stigmatization are necessary for all sections of the community.
Many studies have demonstrated that the MMT stigma is an extension of substance use stigma (8, 11, 25–28). Therefore, interventions that reduce MMT stigma may need to co-address substance use stigma (27). Keeping a reasonable balance between raising public awareness of drugs while avoiding discrimination and rejection against drug users is an important issue in public media communication. Previous evidence demonstrated that communicating with the public using sympathetic stories or narratives that humanize the experiences of individuals with substance use disorder is a promising technique for reducing stigma (29–31). In contrast, messages blaming individuals with substance use disorder will increase public negative emotions and desire for social distance toward them (32, 33). Furthermore, information about the therapeutic quality of MMT is especially needed to address stigma. Stories or narratives portraying individuals with successful treatment recovery would reduce MMT stigma (34–36).
Limitations
There are several limitations to the study. First, this study is based on self-report data which may induce self-report bias. Second, information was obtained through closed-ended questions, which may guide participants to provide socially desirable responses. Third, other factors other than MMT depicted in the vignette, such as heroin dependence, may impact responses, thus leading to overestimated stigma levels. Fourth, participants were recruited from two communities in Hunan, which may not fully represent all community members in this province or in China. Despite this, participants were randomly selected from these two communities, which reduced bias and increase the representation of findings. Fifth, as 11.17% of the identified individuals could not be contacted, it is unknown if their views and attitudes toward MMT patients are different from the respondents. Sixth, the vignette response rate described that patient receiving MMT (86.00%) was much lower than the patient receiving amlodipine treatment (91.66%). These non-responders who received MMT vignette may have more negative attitudes toward patients receiving MMT, which may lead to underestimation of the stigmatization toward MMT. Yet, the present result still reflects a high level of stigmatization attitudes toward MMT and patients receiving MMT in community residents. Last but not least, we did not evaluate participants' personal experience, such as having encountered such patients in the past, which may influence results and could provide some information about prevention and intervention.
Conclusions
Our findings demonstrate that misunderstanding of MMT and stigmatization of MMT patients are very common among populations in the communities in China. Educating community residents regarding MMT's therapeutic quality and the patient identity of the person receiving MMT is recommended.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethic Committee of Jiangxi Mental Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
TL and QW performed the statistical analysis. QD, QW, and TL prepared the first draft of the manuscript. QD, MH, FY, and QL assisted in the collection of data and implementation. QD, TL, and QW have contributed to the interpretation of data and writing. WH commented on the manuscript. All authors participated in the research, study design, manuscript preparation, and have approved the final manuscript.
Funding
This study was supported by the Natural Science Foundation of Jiangxi Province of China (No. 20192BAB205037 to TL).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank all participants. We also thank Winson Fu Zun Yang, a Ph.D. student of Texas Tech University, for English language editing of this paper.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.601266/full#supplementary-material
References
1. Office of China National Narcotics Control Commission. Drug Situation in China (2019). (2020). Available online at: http://www.nncc626.com/2020-06/25/c_1210675877.htm (accessed September 28, 2020)
2. Winkelman TNA, Chang VW, Binswanger IA. Health, polysubstance use, and criminal justice involvement among adults with varying levels of opioid use. JAMA Netw Open. (2018) 1:e180558. doi: 10.1001/jamanetworkopen.2018.0558
3. Alpren C, Dawson EL, John B, Cranston K, Panneer N, Dawn Fukuda H, et al. Opioid use fueling HIV transmission in an urban setting: an outbreak of HIV infection among people who inject drugs—Massachusetts, 2015–2018. Am J Public Health. (2020) 110:37–44. doi: 10.2105/AJPH.2019.305366
4. Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat. (2005) 28:321–9. doi: 10.1016/j.jsat.2005.02.007
5. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. (2014) 2014: CD002207. doi: 10.1002/14651858.CD002207.pub4
6. Fullerton CA, Kim M, Thomas CP, Lyman DR, Montejano LB, Dougherty RH, et al. Medication-assisted treatment with methadone: assessing the evidence. Psychiatr Serv. (2014) 65:146–57. doi: 10.1176/appi.ps.201300235
7. Matheson C, Jaffray M, Ryan M, Bond CM, Fraser K, Kirk M, et al. Public opinion of drug treatment policy: exploring the public's attitudes, knowledge, experience and willingness to pay for drug treatment strategies. Int J Drug Policy. (2014) 25:407–15. doi: 10.1016/j.drugpo.2013.11.001
8. Anstice S, Strike CJ, Brands B. Supervised methadone consumption: client issues and stigma. Subst Use Misuse. (2009) 44:794–808. doi: 10.1080/10826080802483936
9. Harris J, McElrath K. Methadone as social control: institutionalized stigma and the prospect of recovery. Qual Health Res. (2012) 22:810–24. doi: 10.1177/1049732311432718
10. Etesam F, Assarian F, Hosseini H, Ghoreishi FS. Stigma and its determinants among male drug dependents receiving methadone maintenance treatment. Arch Iran Med. (2014) 17:108–14. doi: 10.14172/AIM.005
11. Woo J, Bhalerao A, Bawor M, Bhatt M, Dennis B, Mouravska N, et al. “Dont judge a book by its cover”: a qualitative study of methadone patients' experiences of stigma. Subst Abus Res Treat. (2017) 11:1178221816685087. doi: 10.1177/1178221816685087
12. Conner KO, Rosen D. You're nothing but a junkie: multiple experiences of stigma in an aging methadone maintenance population. J Soc Work Pract Addict. (2008) 8:244–64. doi: 10.1080/15332560802157065
13. Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, et al. An investigation of stigma in individuals receiving treatment for substance abuse. Addict Behav. (2007) 32:1331–46. doi: 10.1016/j.addbeh.2006.09.008
14. Latkin C, Srikrishnan AK, Yang C, Johnson S, Solomon SS, Kumar S, et al. The relationship between drug use stigma and HIV injection risk behaviors among injection drug users in Chennai, India. Drug Alcohol Depend. (2010) 110:221–7. doi: 10.1016/j.drugalcdep.2010.03.004
15. Stancliff S, Myers JE, Steiner S, Drucker E. Beliefs about methadone in an inner-city methadone clinic. J Urban Heal. (2002) 79:571–8. doi: 10.1093/jurban/79.4.571
16. Peterson JA, Schwartz RP, Mitchell SG, Reisinger HS, Kelly SM, O'Grady KE, et al. Why don't out-of-treatment individuals enter methadone treatment programmes? Int J Drug Policy. (2010) 21:36–42. doi: 10.1016/j.drugpo.2008.07.004
17. Luo S, Lin C, Feng N, Wu Z, Li L. Stigma towards people who use drugs: a case vignette study in methadone maintenance treatment clinics in China. Int J Drug Policy. (2019) 71:73–7. doi: 10.1016/j.drugpo.2019.06.005
18. Raheimi S, Jalali A, Jalali R. Social support among women undergoing methadone maintenance treatment in Iran. J Addict Nurs. (2018) 29:179–87. doi: 10.1097/JAN.0000000000000234
19. Link BG, Phelan JC. Stigma and its public health implications. Lancet. (2006) 367:528–9. doi: 10.1016/S0140-6736(06)68184-1
20. Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull. (2004) 30:511–41. doi: 10.1093/oxfordjournals.schbul.a007098
21. Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. (1999) 89:1328–33. doi: 10.2105/AJPH.89.9.1328
22. Brown SA. Standardized measures for substance use stigma. Drug Alcohol Depend. (2011) 116:137–41. doi: 10.1016/j.drugalcdep.2010.12.005
23. Luo T, Wang J, Li Y, Wang X, Tan L, Deng Q, et al. Stigmatization of people with drug dependence in China: a community-based study in Hunan province. Drug Alcohol Depend. (2014) 134:285–9. doi: 10.1016/j.drugalcdep.2013.10.015
24. Angermeyer MC, Matschinger H. Labeling—stereotype— discrimination: an investigation of the stigma process. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:391–5. doi: 10.1007/s00127-005-0903-4
25. Earnshaw V, Smith L, Copenhaver M. Drug addiction stigma in the context of methadone maintenance therapy: an investigation into understudied sources of stigma. Int J Ment Health Addict. (2013) 11:110–22. doi: 10.1007/s11469-012-9402-5
26. Gourlay J, Ricciardelli L, Ridge D. Users' experiences of heroin and methadone treatment. Subst Use Misuse. (2005) 40:1875–82. doi: 10.1080/10826080500259497
27. Smith LR, Mittal ML, Wagner K, Copenhaver MM, Cunningham CO, Earnshaw VA. Factor structure, internal reliability and construct validity of the Methadone Maintenance Treatment Stigma Mechanisms Scale (MMT-SMS). Addiction. (2020) 115:354–67. doi: 10.1111/add.14799
28. Tran BX, Vu PB, Nguyen LH, Latkin SK, Nguyen CT, Phan HTT, et al. Drug addiction stigma in relation to methadone maintenance treatment by different service delivery models in Vietnam. BMC Public Health. (2016) 16:238. doi: 10.1186/s12889-016-2897-0
29. Frank LB, Murphy ST, Chatterjee JS, Moran MB, Baezconde-Garbanati L. Telling stories, saving lives: creating narrative health messages. Health Commun. (2015) 30:154–63. doi: 10.1080/10410236.2014.974126
30. Kennedy-Hendricks A, McGinty EE, Barry CL. Effects of competing narratives on public perceptions of opioid pain reliever addiction during pregnancy. J Health Polit Policy Law. (2016) 41:873–916. doi: 10.1215/03616878-3632230
31. Bachhuber MA, McGinty EE, Kennedy-Hendricks A, Niederdeppe J, Barry CL. Messaging to increase public support for naloxone distribution policies in the United States: results from a randomized survey experiment. PLoS ONE. (2015) 10:e0130050. doi: 10.1371/journal.pone.0130050
32. Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social stigma toward persons with prescription opioid use disorder: associations with public support for punitive and public health-oriented policies. Psychiatr Serv. (2017) 68:462–9. doi: 10.1176/appi.ps.201600056
33. Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. J Pers Soc Psychol. (1988) 55:738–48. doi: 10.1037/0022-3514.55.5.738
34. McGinty E, Pescosolido B, Kennedy-Hendricks A, Barry CL. Communication strategies to counter stigma and improve mental illness and substance use disorder policy. Psychiatr Serv. (2018) 69:136–46. doi: 10.1176/appi.ps.201700076
35. Romer D, Bock M. Reducing the stigma of mental illness among adolescents and young adults: the effects of treatment information. J Health Commun. (2008) 13:742–58. doi: 10.1080/10810730802487406
Keywords: stigma, methadone maintenance treatment, MMT, China, public attitudes
Citation: Deng Q, Hu M, Yu F, Liu Q, Hao W, Wu Q and Luo T (2020) A Community-Based Investigation of Stigma Toward Individuals Receiving Methadone Maintenance Treatment in China: A Randomized Case Vignette Study. Front. Psychiatry 11:601266. doi: 10.3389/fpsyt.2020.601266
Received: 31 August 2020; Accepted: 23 October 2020;
Published: 25 November 2020.
Edited by:
Jianhua Chen, Shanghai Jiao Tong University, ChinaReviewed by:
Min Zhao, Shanghai Changning Mental Health Center, ChinaWan-jun Guo, Sichuan University, China
Yilang Tang, Emory University, United States
Copyright © 2020 Deng, Hu, Yu, Liu, Hao, Wu and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiuxia Wu, d3VxaXV4aWFAY3N1LmVkdS5jbg==; Tao Luo, bHVvdGFvMDlAaG90bWFpbC5jb20=
 Qijian Deng
Qijian Deng Maorong Hu
Maorong Hu Fang Yu3
Fang Yu3 Wei Hao
Wei Hao Qiuxia Wu
Qiuxia Wu Tao Luo
Tao Luo