- 1Ageing Epidemiology Research Unit, School of Public Health, Imperial College London, London, United Kingdom
- 2Department of Primary Care and Public Health, Imperial College London, London, United Kingdom
- 3Centre for Population Health Sciences, Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
- 4Imperial College Healthcare NHS Trust, Faculty of Medicine, Imperial College London, Public Health Directorate, London, United Kingdom
- 5Department of Infectious Disease Epidemiology, School of Public Health, Imperial College London, London, United Kingdom
The COVID-19 pandemic is imposing a profound negative impact on the health and wellbeing of societies and individuals, worldwide. One concern is the effect of social isolation as a result of social distancing on the mental health of vulnerable populations, including older people. Within six weeks of lockdown, we initiated the CHARIOT COVID-19 Rapid Response Study, a bespoke survey of cognitively healthy older people living in London, to investigate the impact of COVID-19 and associated social isolation on mental and physical wellbeing. The sample was drawn from CHARIOT, a register of people over 50 who have consented to be contacted for aging related research. A total of 7,127 men and women (mean age=70.7 [SD=7.4]) participated in the baseline survey, May–July 2020. Participants were asked about changes to the 14 components of the Hospital Anxiety Depression scale (HADS) after lockdown was introduced in the UK, on 23rd March. A total of 12.8% of participants reported feeling worse on the depression components of HADS (7.8% men and 17.3% women) and 12.3% reported feeling worse on the anxiety components (7.8% men and 16.5% women). Fewer participants reported feeling improved (1.5% for depression and 4.9% for anxiety). Women, younger participants, those single/widowed/divorced, reporting poor sleep, feelings of loneliness and who reported living alone were more likely to indicate feeling worse on both the depression and/or anxiety components of the HADS. There was a significant negative association between subjective loneliness and worsened components of both depression (OR 17.24, 95% CI 13.20, 22.50) and anxiety (OR 10.85, 95% CI 8.39, 14.03). Results may inform targeted interventions and help guide policy recommendations in reducing the effects of social isolation related to the pandemic, and beyond, on the mental health of older people.
Introduction
With unprecedented population aging; the consequences of social isolation on the mental wellbeing of older people is emerging as a significant public health concern, now exacerbated by the COVID-19 pandemic (1, 2). Previous studies have reported that social disconnection puts older people at greater risk of depression and anxiety (3). The impact of severe acute respiratory syndrome (SARS) on mental health, within the general public has previously been reported (4), and recent systematic reviews are beginning to highlight the detrimental impact of COVID-19 on mental health among different populations (5–7). Factors exacerbating this risk are less known but vital in informing appropriate targeted intervention and preventative measures.
The United Kingdom (UK) announced COVID-19 lockdown measures on the 23rd March 2020. Lockdown stipulated a ban on nonessential travel, closure of most shops, offices and public spaces, alongside self-isolation and quarantine for those with possible infection and shielding for those deemed extremely vulnerable due to health conditions. These measures have placed many individuals under conditions of complete isolation, especially those living alone. Long periods of social isolation may have a profound negative effect on mental health conditions including depression, anxiety, stress and insomnia (8), may differ as a function of sex and age (5), and may worsen health inequalities, with poorer and marginalized groups at greatest risk (9). Furthermore, social isolation, loneliness and depression have, in turn, been associated with cognitive decline (10, 11) and incident dementia (12, 13) among older people.
A systematic review, conducted in May 2020, sought to identify the psychiatric symptoms or morbidities associated with COVID-19 among those infected, the general population, psychiatric patients and health-care workers (5). They identified 43 studies, the majority of which were conducted within Chinese populations, investigating the impact of COVID-19 on mental health, but not exclusive to the elderly. One Danish study (n=2,458), conducted within the general public, revealed higher scores in anxiety and depression when compared to pre-lockdown (14), especially among females, while a Chinese study (n=333) reported a moderate-to-severe level of subjective stress, anxiety and depression in an initial survey post-lockdown, with no significant changes one-month later (15). Another systematic review and meta-analysis was conducted on studies relating to the mental health impact of COVID-19 on the general public and health workers, up until the 25th May, including 65 studies, again, predominantly from China (7). They reported the prevalence of anxiety and depression among the general population during the pandemic as 33% (28%–30%) and 28% (23%–32%), respectively. Common risk factors for higher psychological impact included being female, having contracted COVID-19, lower socio-economic status, social isolation and spending longer watching COVID-19 related news. Frontline providers of telephone help services such as Lifeline in Australia, have reported dramatic increases in calls from people experiencing anxiety and loneliness (16). The Australian Bureau of Statistics’ national Household impacts of COVID-19 survey of 1000 adults found that 28% of women and 16% of men reported feeling lonely as a result of the pandemic, and that this was the most common personal stressor identified (17). Finally, a UK study has published findings on the impact of COVID-19 on mental health before and during the pandemic, in participants of the UK Household Longitudinal Study (aged >16 years, n=17,452) (18). A web-based survey administered between April 23–30th 2020, assessed mental health via the 12-item General Health Questionnaire and reported that prevalence of mental health distress rose from 18.9% (17.8, 20.0) in 2018–2019 to 27.3% (26.3, 28.2) in April 2020. Predictors of change were greatest in younger adults, women and people living with children.
Among these studies, the older population is largely underrepresented. We are not aware of any studies in high income countries that have exclusively investigated the impact of social isolation and physical distancing due to COVID-19 restrictions on the mental health of older people. Identifying the key factors that place older people at risk of decline in mental wellbeing is critical in planning appropriate mitigation strategies. Here, we report the effects of social isolation on self-reported changes in levels of depression and anxiety among older people residing within London via an online survey. We investigated the effect of sociodemographic factors, health variables and indicators of loneliness and reduced connectivity as risk factors for change in levels of depression and anxiety. As the literature presents consistent evidence for the effect modification of sex in response to social isolation on mental health (14, 19–23), we also explored whether certain risk factors differentially altered responses to social isolation among men and women. Results may inform interventions to prevent or delay the effects of social isolation on worsening mental health in this susceptible older population.
Materials and Methods
Study Design and Population
To investigate the associations between social isolation measures, implemented due to the COVID-19 pandemic, and the mental and physical health of an older population, we designed and implemented, on April 29th, 2020, the ongoing longitudinal CHARIOT COVID-19 Rapid Response Study (CCRR). Study participants were recruited from the Cognitive Health in Ageing Register for Interventional and Observation Trials (CHARIOT), comprised of ~40,000 volunteers aged 50 years and over, without known dementia diagnosis and who have consented to be contacted for participation in age-related research (24). CHARIOT has been developed by the School of Public Health at Imperial College London, since 2012, in collaboration with primary care practices and community organizations across London. For the CCRR study, data on symptoms and results of COVID-19 tests, demographic and lifestyle factors, mental and physical health are being collected by repeated six-weekly questionnaire online surveys. In the present analysis we report cross-sectional results from the baseline survey, conducted between 30th April – 8th July 2020. All register volunteers were invited via email or post for participation in the CCRR study. Additional adult members of their household, able to provide consent and who wished to take part in the survey, could do so by contacting the study team. Participants were directed via a unique link to the online survey platform, hosted by Qualtrics (Provo, UT, USA), where they were presented with the Participant Information Sheet, then directed to complete an electronic Informed Consent Form. Once the consent form was electronically signed by the participant, the survey was launched. Data collected as a part of this study are anonymized and kept strictly confidential in accordance with the UK General Data Protection Regulations (2016). CCRR was ethically approved by the Imperial College London Joint Research Compliance Office (20IC5942) and by the Health Research Authority (16/EM/0213).
Assessment of Sociodemographic, Health and Lifestyle Factors
Data on general (age, sex, ethnicity, and marital status) demographics, household composition, current occupational status and friend/family contact via technology such as skype/zoom/mobile were extracted. Alcohol and smoking behavior, and height/weight for the calculation of body mass index (BMI) were included. Participants were asked to report any medical history via checking against a list of comorbidities including vascular factors, cancers, neurological and mental health conditions, arthritis and respiratory disease. Loneliness was measured via the following question: “During the period of reduced social contact, have you experienced loneliness (felt isolated, with no companions)”, with the following responses; “never”, “rarely”, “sometimes”, “often”. The variable used to assess sleep was obtained from the question: “During the period of reduced social contact, have you experienced poor sleep (restless and unable to sleep)”, with the following responses; “Not ever”, “Less than once a week”, “Once or twice a week”, “Three or more times a week”. The sleep and loneliness questions were obtained from the Imperial College Sleep Quality questionnaire adapted from the Pittsburgh Sleep Quality Index (25) and Centre for Epidemiologic Studies of Depression Scale, for work-free periods (26).
Depression and Anxiety (Outcome)
Depression and anxiety levels were assessed with the Hospital Anxiety and Depression Scale (HADS) which includes 14 questions on feelings related to anxiety and depression (seven items for each), rated on a 4-level Likert scale from “most of the time” to “not at all” or similar responses (27). The widely used HADS has face validity for use in an older population (28), with questions that are easy to relate to and appropriate to the current circumstances of social isolation. After each item, we added a question as to whether participants were experiencing that feeling “more than”, “less than” or “the same as” before COVID-19 social distancing restrictions. The categorical outcome variable used in this study was overall improvement, worsening or no change in reported items of anxiety and depression (Figure 1). Participants were categorized as either worsened or improved on the depression or anxiety components of HADS if they responded feeling “more than” or “less than” since before lockdown, on four or more of the seven items for depression or anxiety, respectively. All others were categorized as not changed.
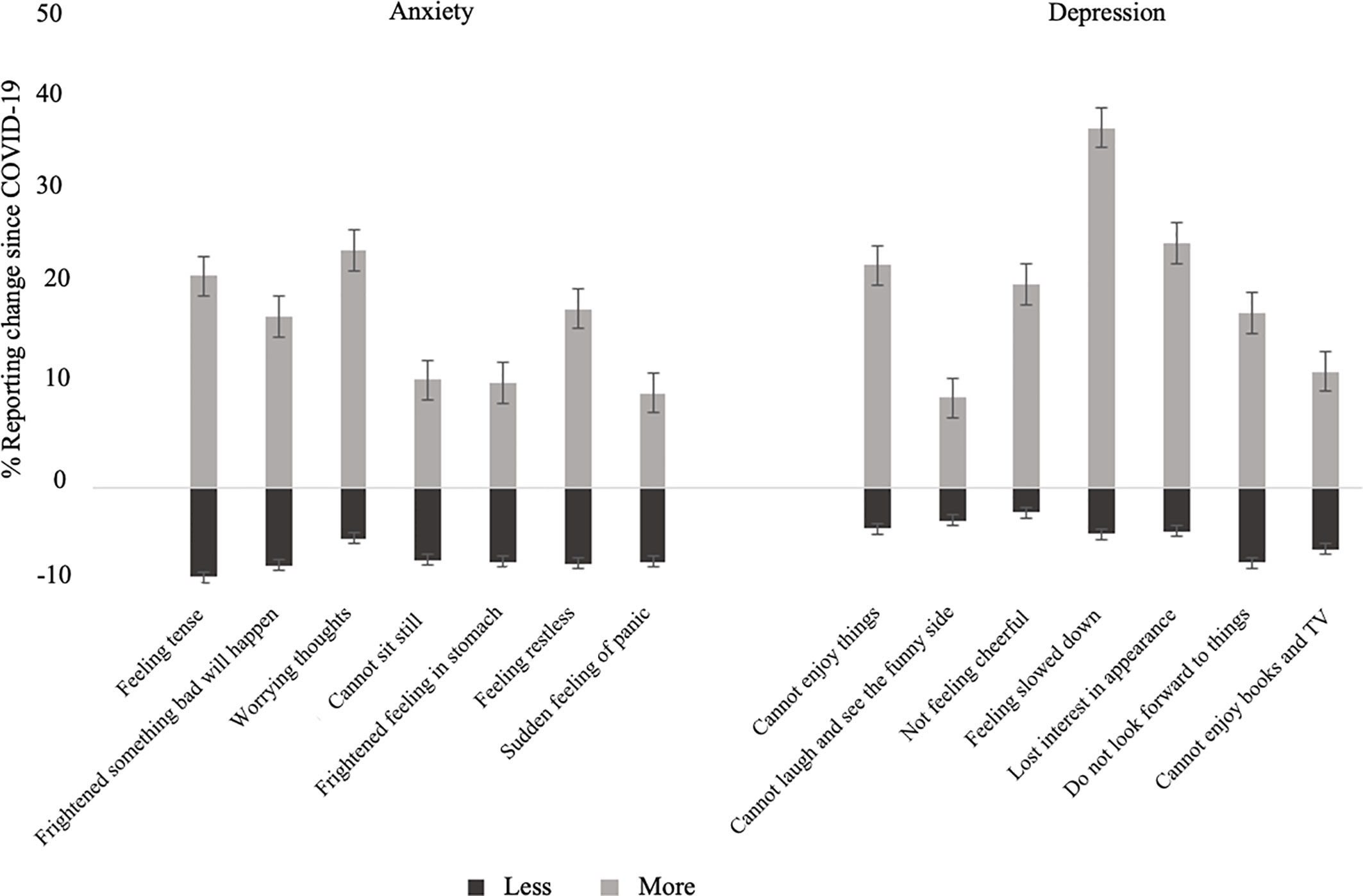
Figure 1 Percent of cohort reporting worsened or improved items of anxiety and depression following COVID-19 social isolation measures. Error bars indicate standard error.
Statistical Analyses
We conducted separate multinomial logistic regression models to assess the association between each of the following factors: sex (men, women), age (continuous, years), marital status (married/partnered, single/widowed/divorced), smoking (no, yes), alcohol consumption (continuous, units per week), sleep quality (not ever, < once per week, 1–2 times per week, ≥3-times per week), feelings of loneliness (never, rarely, sometimes, often), household composition (not living alone, living alone), level of remote friend/family contact via technology (daily, 2–6 times per week, ≤ once per week) and their association with risk of change in components of anxiety and depression since lockdown as separate outcomes (worsened, improved, no change). Analyses was initially conducted in men and women combined, followed by sex-stratification. Interaction terms by sex and exposure were included in each model to determine if the effect of exposure on the outcome measure significantly varied as a function of sex. Models were controlled for confounding effects of age and sex (model 1), and additionally for hypertension, hypercholesterolemia, diabetes, cardiovascular disease, chronic obstructive pulmonary disease (COPD) and any mental health conditions, pre-lockdown (model 2). These common chronic conditions were included as subjectively reported poor health is a known risk factor for depression and anxiety (29–31). Less than 7% of data were missing for any one variable; hence, we did not compute missing values. All variables were included in the model as categorical, with the exceptions of age and alcohol consumption. To enhance interpretation of the logistic regression, alcohol consumption was adjusted to represent risk per increase in 3-units of alcohol per week (approximately one glass of wine), and for age, an increase in risk per 5-years. Results are presented as odds ratios (ORs) and 95% confidence intervals (CI). Statistical two-sided significance level was set at 5% (p<0.05). All analyses were conducted using IBM SPSS 23 for windows.
Results
Cohort Characteristics
At time of data extraction, a total of 9,314 register participants had read the Participant Information Sheet and were directed to complete the consent form. Of this number, 2,187 (24.5%) participants did not complete consent to join CCRR. The remaining 7,127 were included in this study for baseline data analysis. The response rates from 15,000 emailed invitations and 25,000 postal invitations were approximately 35% and 7.5%, respectively.
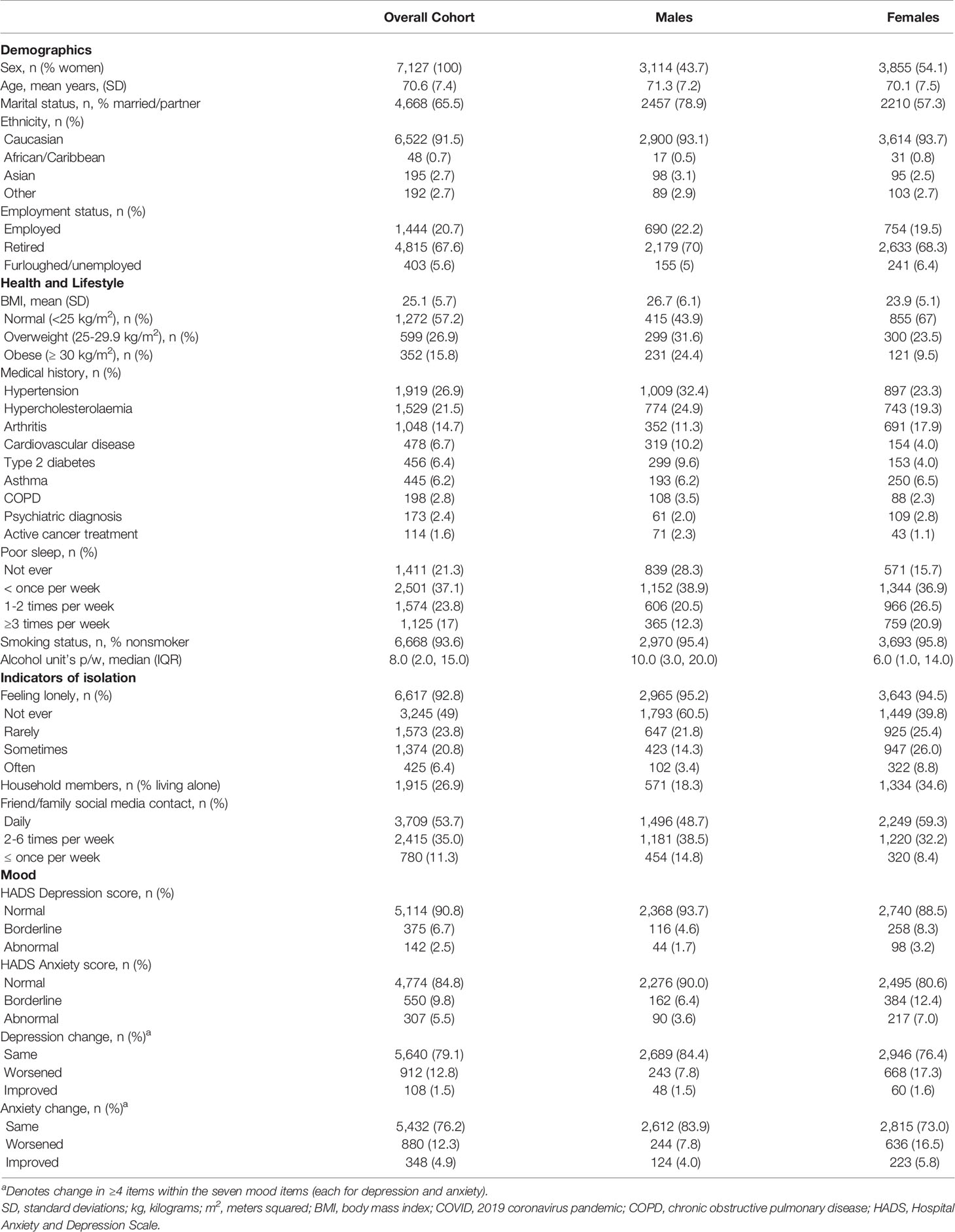
Table 1 presents the cohort characteristics. Of the total sample, majority were Caucasian (91.5%) with a mean age 70.6 (SD 7.4) years (range 50-100). Women represented 54.1% of the cohort, 65.5% were married/partnered, and 20.7% were employed. Mean BMI was 25.1 (SD 5.7), 77.1% of men and 50.6% women reported at least one vascular factor, 2.4% of the overall cohort reported a mental health condition, pre-pandemic. Poor sleep ≥3 times per week was reported by 12.3% of men and 20.9% of women. Majority of the cohort reported that they did not smoke (93.6%), and alcohol consumption was low. A higher proportion of men reported feeling lonely “often” and having contact with friends and family ≥3 times per week compared to women; whereas a higher proportion of women reported living alone. A total of 5.5% of participants fell within the abnormal category for anxiety and 2.5% for depression on the HADS questionnaire, according to population norms. Since lockdown, 12.8% of participants reported feeling worse on components of depression on the HADS and 12.3% reported feeling worse on components of anxiety. On the other hand, fewer participants reported feeling improved on components of depression and anxiety (Figure 1). There was a substantially higher proportion of women scoring abnormal on the HADS depression and anxiety assessment, and who reported feeling worse in components of anxiety and depression post-lockdown, compared to men.
Association of Age and Sex With Change in Anxiety and Depression
After accounting for the confounding effect of covariates, women compared to men were more than twice as likely to report feeling worse on components of depression (OR 2.46, 95% CI 2.10, 2.89) and anxiety (OR 2.42, 95% CI 2.06, 2.85) on the HADS (Tables 2, 3). Conversely, of those reporting improvements (4.9%), women were more likely to report feeling better in components of anxiety (OR 1.7, 95% CI 1.36, 2.16), relative to men. With every five-year increase in age there was a 19% (OR 0.81, 95% CI 0.77, 0.85) and 22% (OR 0.78, 95% CI 0.75, 0.83) lower risk of reporting feeling worse on components of depression and anxiety, respectively.
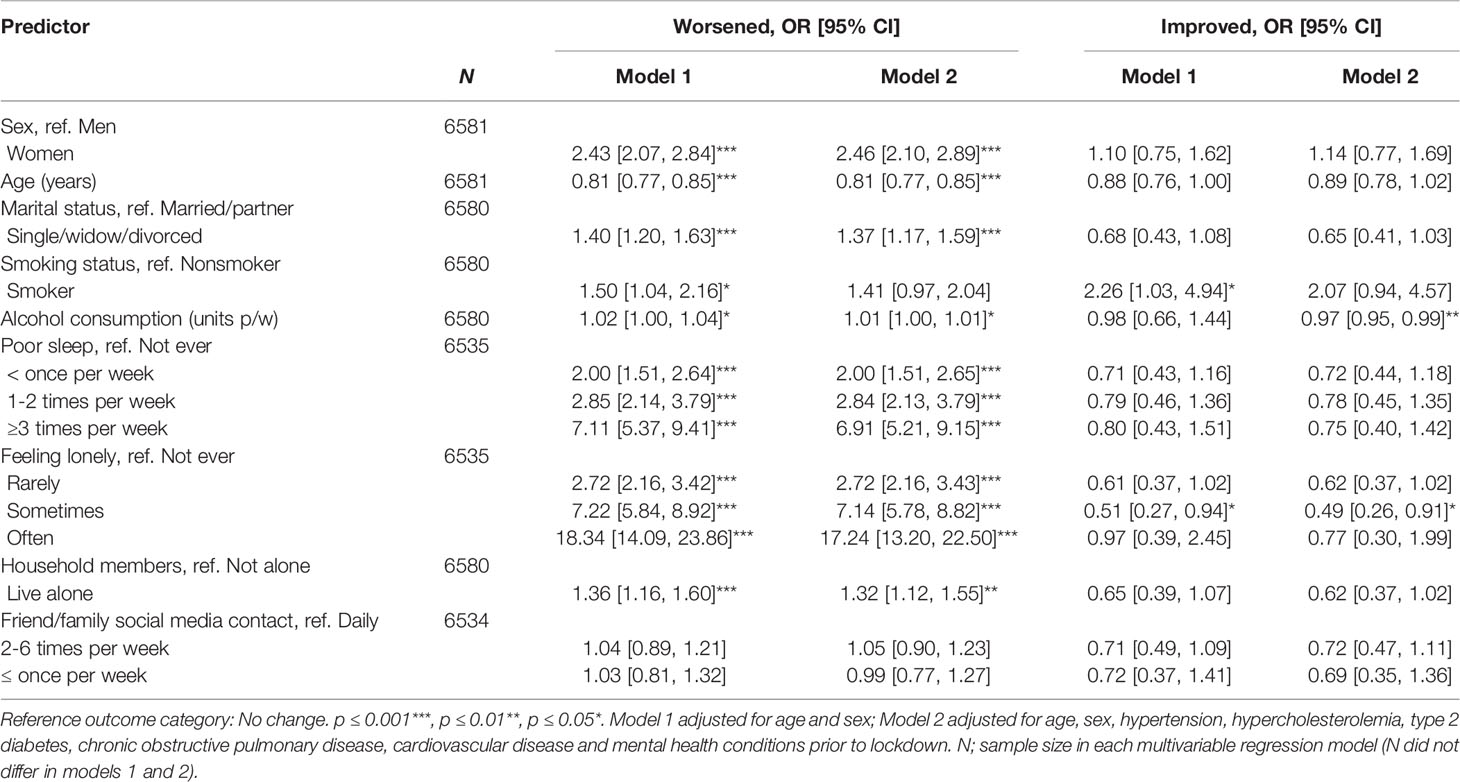
Table 2 Association between sociodemographic factors, health and lifestyle, indicators of isolation and change in components of depression.
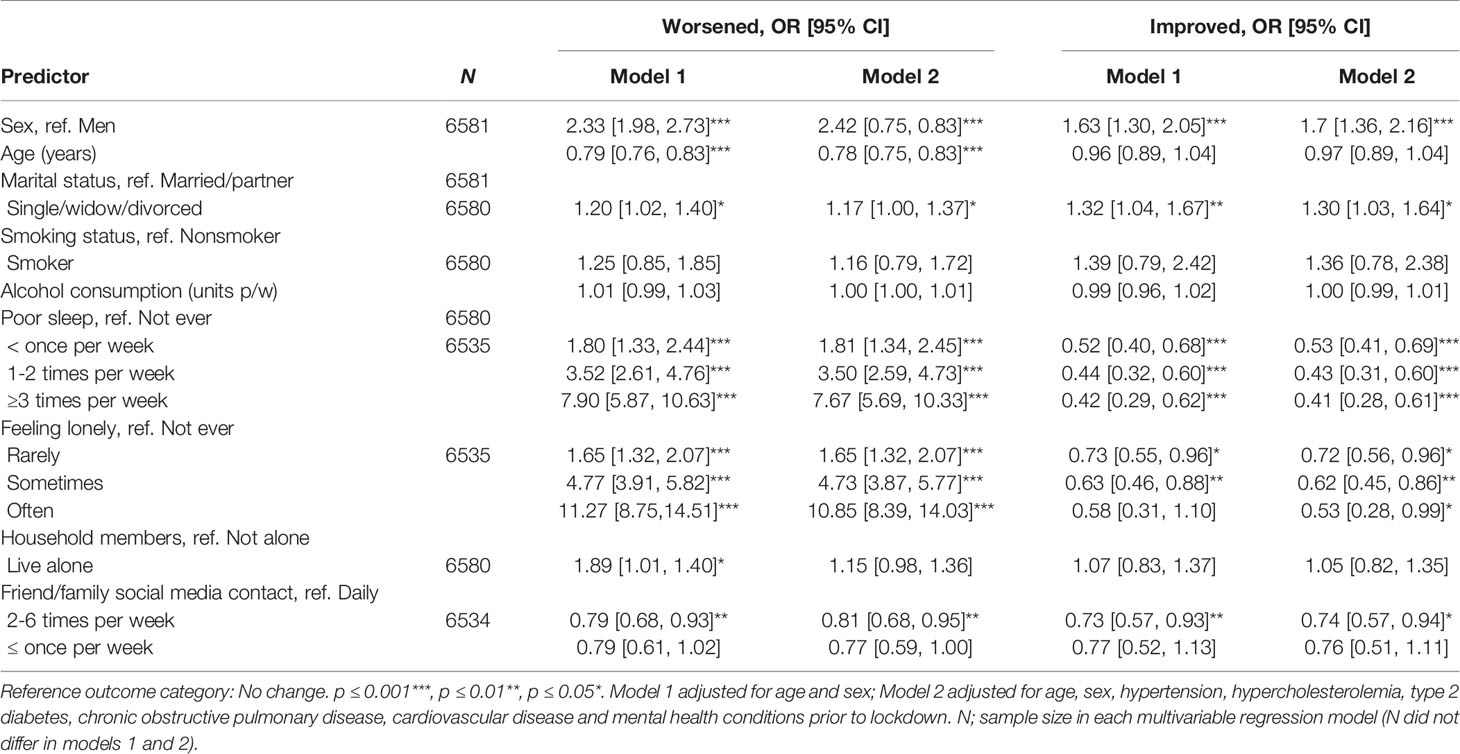
Table 3 Association between sociodemographic factors, health and lifestyle, indicators of isolation and change in components of anxiety.
Loneliness and Reduced Social Connectivity
Overall, 27.2% of the cohort reported that they felt lonely sometimes or often, more in women (34.8%) than men (17.7%). There was a prominent and dose-response association between loneliness and worsened components of anxiety and depression on the HADS. Individuals reporting that they “often” felt lonely had a 17.24 (95% CI 13.20, 22.50) times higher risk of reporting feeling worse in components of depression and 10.85 (95% CI 8.39, 14.03) times higher risk of reporting feeling worse in components of anxiety, compared to those who never felt lonely (Tables 2, 3). Women were twice as likely to report worsened components of depression as a result of loneliness (OR 19.74, 95% CI 14.28, 27.29) compared to men (OR 11.60, 95% CI 6.86, 19.62), and men were more likely to report worsened anxiety (OR 14.79, 95% CI 8.99, 24.32) than women (OR 9.36, 95% CI 6.92, 1.80) (Tables 4, 5).
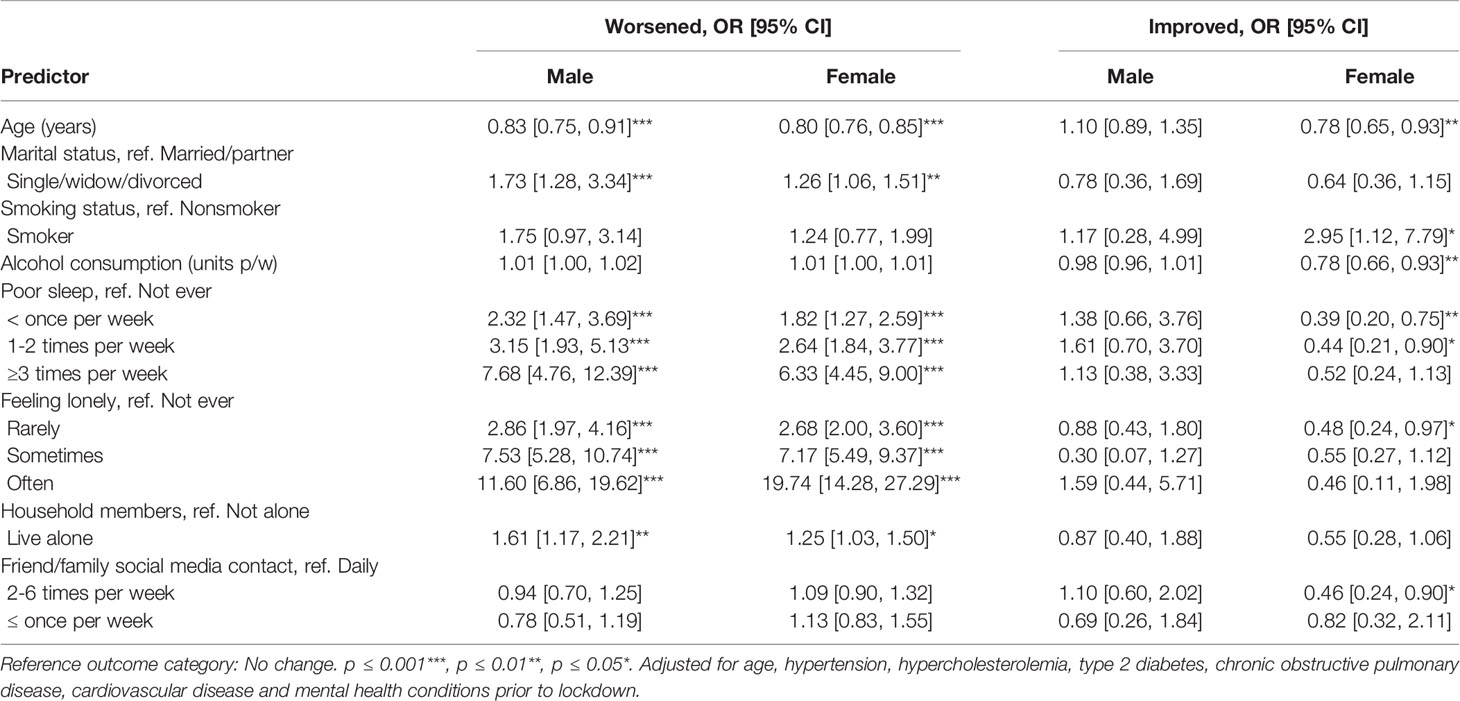
Table 4 Association between sociodemographic factors, health and lifestyle, indicators of isolation and change in components of depression among males and females.
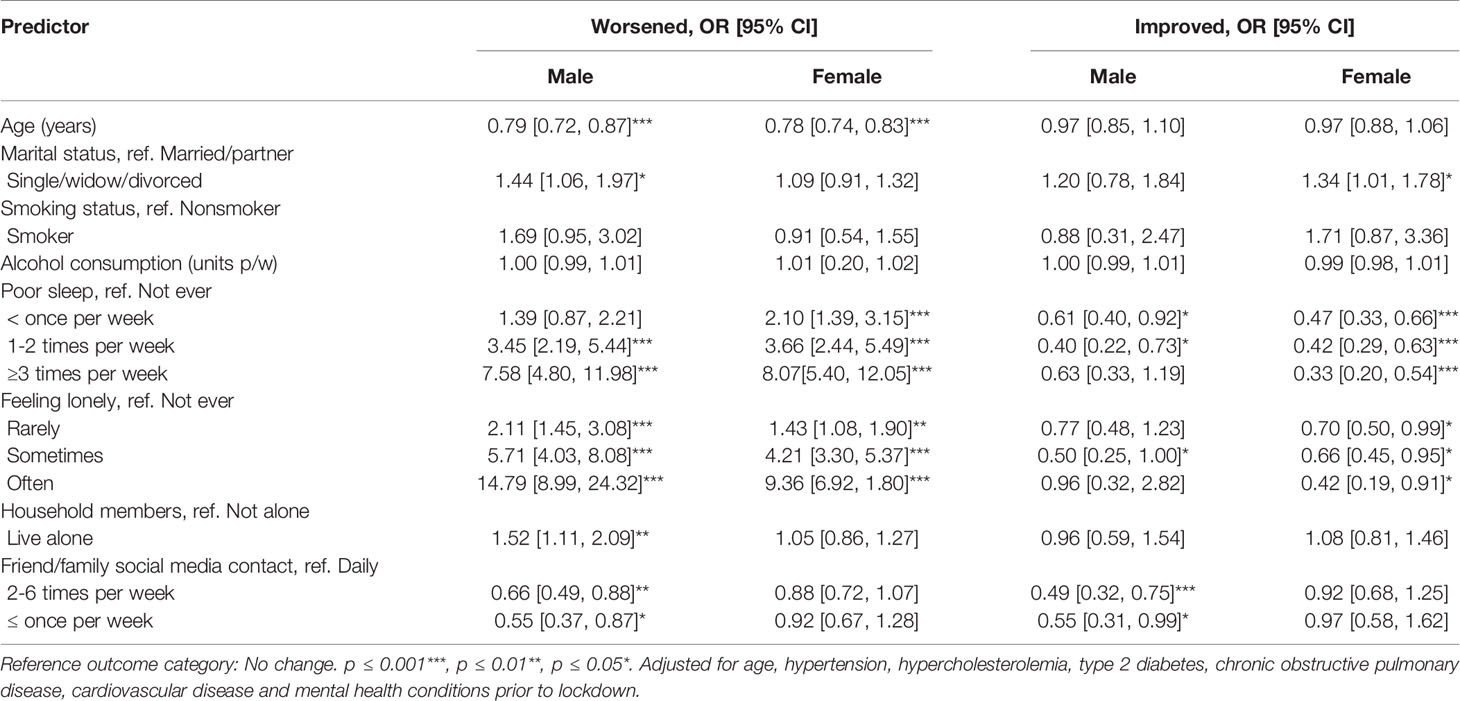
Table 5 Association between sociodemographic factors, health and lifestyle, indicators of isolation and change in components of anxiety among males and females.
Compared to those who reported living with others, those who lived alone were more likely to report feeling worse on components of anxiety (OR 1.89, 95% CI 1.01, 1.40) and depression (OR 1.36, 95% CI 1.16, 1.60) (Tables 2, 3). Findings were augmented among men (Tables 4, 5). The associations were attenuated but remained significant after accounting for the confounding effect of self-reported mental health conditions and vascular factors.
Level of remote contact with friends/family via technology did not significantly alter risk of reporting feeling worse on components of depression (Tables 2, 4). Compared to individuals who reported daily contact, those reporting 2–6 times of online social contact per week had a 19% (OR 0.81, 95% CI 0.68, 0.95) lower risk of reporting feeling worse on components of anxiety, and, conversely, a 26% (OR 0.74, 95% CI 0.57, 0.94) lower likelihood of reporting feeling improved (Table 3). Sex stratified analysis found these results to be augmented and to remain statistically significant among men (Table 5).
Single/widowed/divorced individuals had a 1.37 (95% CI 1.17, 1.59) and 1.17 (95% CI 1.00, 1.37) times higher risk of reporting worsened components of depression and anxiety on the HADS, respectively, compared to those who were married/partnered (Tables 2, 3). These associations were augmented among men (Tables 4, 5). There was also a small proportion more likely to report feeling improvement on components of anxiety, following lockdown (OR 1.30, 95% CI 1.03, 1.64), compared to those who are married/partnered, which were augmented among women (Table 5).
Sleep, Alcohol, and Smoking
Male smokers were more likely to report feeling worse on components of depression (OR 1.75, 95% CI 0.97, 3.14) and anxiety (OR 1.69, 95% CI 0.95, 3.02) on the HADS compared to nonsmokers (Tables 4, 5). This association was not significant for women. However, of those reporting improvements in components of depression, female smokers were more likely to do so than female nonsmokers, while this association was not statistically significant for men. Alcohol consumption was not associated with a remarkable worsening or improvement in components of anxiety or depression in men. However, a three-unit increase in alcohol consumption per week (approximately one glass of wine) was associated with a 22% (OR 0.78, 95% CI 0.66, 0.93) lower likelihood of reporting improvement in components of depression in women.
Cohort participants who subjectively reported experiencing poor sleep were more likely to report worsened components of anxiety and depression and less likely to report improvement, in a dose response manner. Those reporting poor sleep ≥3 times per week had a 6.91 (95% CI 5.21, 9.15) and 7.67 (95% CI 5.69, 10.33) times higher risk for reporting feeling worse in components of depression and anxiety, respectively, compared to those who reported an absence of poor sleep (Tables 2, 3). Differences did not vary significantly by sex.
Discussion
We investigated the effect of sociodemographic, health and lifestyle factors, indicators of loneliness and reduced connectivity on subjective feelings of anxiety and depression among an older population. Most people did not report a change on components of anxiety and depression on the HADS, but for those who did report change, it was more likely worsened than improved (Table 1). Our results indicate that women, younger age, being single/widowed/divorced, living alone, poor sleep and experiencing loneliness are factors linked with higher risk for reporting worsened components of anxiety and/or depression.
Loneliness and Reduced Social Connectivity
This study demonstrated a significant negative association between subjective loneliness and worsened components of both depression and anxiety, following lockdown. These associations had a dose response effect. Levels of anxiety were exacerbated among men, and depression, among women. Furthermore, descriptive statistics indicated a significant change in loneliness before and after lockdown stipulations, whereby those reporting loneliness “often” prior to lockdown increased from 2% to 20% post-lockdown (data not shown). These findings indicate that an increase in loneliness was most likely due to the circumstances surrounding COVID-19 social isolation and was not pre-existing. Our findings corroborate results from a survey on the impact of COVID-19 on mental health (32), as reported in a recent Lancet Psychiatry position paper, indicating a strong association between social isolation and loneliness with symptoms of depression and anxiety (33). Social isolation and loneliness are strongly associated with anxiety, depression, self-harm and suicide attempts across the lifespan (34–36). Older people may be considered prime candidates for risk of loneliness, owing to the higher likelihood of reduced capacity, frailty and comorbidities, and reduced likelihood to engage with others via technology. Our results found that those who were single/widowed/divorced and/or who lived alone were also at increased risk of reporting worsened components of depression and anxiety following COVID-19 lockdown, especially among men. Furthermore, men who engaged in higher levels of friend/family contact via technology, reported feeling worse in components of anxiety, perhaps indicating reverse causality. Being widowed or divorced as a risk factor for worsened mental health has been reported in similar COVID-19 general population cohort studies in Spain (n=3,055) (19) and China (n=1,060) (37), although among younger cohorts and without investigating the effect modification of sex. It may be expected that living alone and without a partner are inherently linked with an increased risk of loneliness, especially under circumstances of social and physical distancing. The frequency and mode of social connectivity via technology, while under social distancing circumstances, and its link with anxiety and depression has not yet been investigated outside the current study, warranting further attention.
The longer-term consequence of such risk factors as loneliness and reduced social connectivity have been reported elsewhere. Social isolation, depression and apathy have been associated with an increased risk of incident dementia in a circular-causal manner (12, 38). Furthermore, data from the English Longitudinal Study of Ageing reported that incident dementia was independently associated with loneliness, a lower number of close relationships and not being married, and that these findings were in fact independent of depression and without reverse causality (13). Our findings and those reported above, only further highlight the need to promptly tackle both the immediate and longer-term consequence of social isolation on the mental and consequential cognitive health of older adults.
Sleep, Alcohol, and Smoking
A total of 40% of our cohort reported sleep disturbances. This figure exceeds worldwide insomnia prevalence, estimated before the pandemic to be between 3.9% and 22% (39). A study conducted in Greece (n=2,427), following COVID-19 lockdown, detected a similar proportion (37.6%) of the general public experiencing some level of sleep disturbance (40). They also reported that women, living in urban areas, stress surrounding risk of COVID-19 infection, loneliness and severe depressive symptoms were all predictive of insomnia. Therefore, it is not unreasonable to suggest that, in such circumstances, sleep disturbances may be an artifact of reverse or bi-directional causality. It may be expected that personal circumstances surrounding the COVID-19 pandemic will increase levels of stress. Worry and ruminating thoughts provoke cognitive arousal and may disturb cortisol homeostasis, resulting in poorer sleep. Such associations have previously been reported under similar circumstances (41). Furthermore, there is existing evidence that loneliness and poor sleep have a bi-directional relationship (42).
We found that men who reported smoking had an increased risk of reporting worsened components of anxiety and depression. Conversely, among the sub-group of those reporting improved components of depression, females with higher alcohol consumption were 22% less likely to report these improvements. Although no study has yet investigated the associations of smoking and alcohol with risk for depression and anxiety during the COVID-19 pandemic, social isolation has been reportedly associated with unhealthy lifestyle factors, including increased smoking and alcohol consumption (35). In our study, of those who smoke, 24.6% reported that they had increased smoking since lockdown, and of drinkers, 14.7% reported an increase in alcohol consumption, both warranting further investigation. Once again, these observations may be a consequence of reverse or bi-directional causality. Nonetheless, majority of participants report no change in smoking and/or drinking behavior post-lockdown, indicating that perceived worsening in components of depression and/or anxiety may also be linked with this pre-existing behavior. Exploration of longitudinal data will elucidate such inferences.
Age and Sex
Women, compared to men, were more likely to report worsened components of anxiety and depression on the HADS. These findings have been replicated, in varying age-groups and from different countries including the UK (18), Demark (14), Spain (19, 23, 43), Italy (21), Turkey (44) and Iran (20, 22). Furthermore, studies conducted on the effects of stress, have consistently reported women to be at increased risk of developing anxiety and depression (45). Notwithstanding, one recent study reported that associations between depression, stress and insomnia was higher among men surveyed during the COVID-19 pandemic (46), while another study reported no differences related to sex (37), both conducted within Chinese populations. To the best of our knowledge, ours is the first to report the effect modification of sex on the association of key risk factors for depression and anxiety, among older people, during the COVID-19 lockdown. Such findings may elucidate causative variations in risk for mental health decline. Factors including loneliness, being single/widowed/divorced, living alone, remote friend/family contact via technology, and alcohol consumption were all contributors to differences between men and women in reported worsening in components of anxiety and depression. These results highlight the importance of investigating specific sociodemographic, health and lifestyle circumstances which augment risk among men and/or women differentially.
In our population of older people, we found that younger age was a risk factor for worsened components of anxiety and depression. To our awareness, only one other study of a much smaller sample (n=236) reported on the associations of COVID-19-related social isolation on mental health among older people exclusively (44), but the authors did not investigate the risk of age. The older age-group is poorly represented within most of reported studies, to date. However, two studies reported lowest risk for anxiety and depression during the earlier stages of COVID-19 lockdown, among a small sub-sample of those >60 years, when compared to younger age-categories, both being within Spanish cohorts (19, 43). Conversely, a Chinese population study, reported that older age increased risk for anxiety and depression (37). Although the effect of COVID-19 on mental health appears to be attenuated by older age, findings within an older sample are scarce and studies have often failed to account for risk factors more commonly affecting older people, such as social isolation and loneliness. Indeed, social disconnection has reportedly put older people at great risk of depression and anxiety (3). Nonetheless, among a healthier older population such as ours, it may also be that with increasing age, older adults are more able to adapt and show higher resilience. To truly understand the relevance of our findings, follow-up data will need to be investigated, and ideally, in comparison with a congruent, younger population.
Limitations
Some study limitations warrant acknowledgment. Firstly, we did not have a measure of anxiety and depression before the COVID-19 social isolation and physical distancing measures were mandated. Thus, we were unable to assess change other than from current and self-reported change. Nonetheless, given the magnitude of observed outcomes, it is not unreasonable to speculate that mental health changes were largely influenced by circumstances surrounding the COVID-19 pandemic and resultant social isolation. Indeed, by comparing the proportion of those reporting worsened components of anxiety and depression against HADS clinical classification (normal, borderline, abnormal), 53% of those who reported worsened depression, and 34% of those who reported worsened anxiety, scored within the normal range on the HADS scale, indicating that lockdown affected mood not only among those with pre-existing disorders, but also in psychologically healthy individuals.
The use of cross-sectional data in this study precludes causal inferences. We are unable to establish the direction of the association between various factors such as changes in alcohol consumption, cigarette smoking, sleep quality, and worsened levels of anxiety or depression. It will be important to investigate repeated measures of modifiable exposures and reported symptoms of depression and anxiety over time. Nonetheless, the CCRR study is ongoing and we endeavor to publish longitudinal findings in due course. Furthermore, we have not yet captured the experiences of those less technologically literate. Wider access to technology may help buffer loneliness and isolation that lead to worsened mental health. Older people, however, are more likely to have limited ability to access technology, most likely representing the more vulnerable of this demographic. We may hypothesize that those who are less able or willing to engage with technology may also present with exacerbated risk factors such as a higher prevalence of comorbidities, and hence, be yet more vulnerable to the effect of social isolation as a result of the pandemic. Similar studies should endeavor to allow administration of surveys via a variety of means, such as phone or post, to capture the experience of those across the so-called digital divide. Indeed, the included cohort is a biased and nonrepresentative sample of the wider London population. The CCRR cohort are healthier with fewer comorbidities than would be expected for this age-group, are predominantly Caucasian and living within the West London region, an area typically associated with higher socioeconomic status (24). Finally, we found a strong and convincing link between subjective loneliness and higher risk for reporting worsened levels of anxiety and depression. However, this variable warrants a more in-depth investigation, with loneliness being gathered via an existing and validated questionnaire designed to assess a wider spectrum of loneliness indicators, such as both emotional and social, believed to be distinct concepts (47). We have, since, optimized our survey questionnaire to capture such additional data.
Conclusion and Perspectives
The negative impact of COVID-19 on mental health among the general population has been identified as a research priority (1, 2, 6, 33, 48). However, few studies to date have specifically addressed the effect of COVID-19 and consequential social and physical distancing measures on mental wellbeing, specifically among an older population. Findings from this study highlight potentially important clinical and public health implications. We have identified, within an older, UK population, risk factors for the development of anxiety and depression as a result of COVID-19 related social isolation. These factors may inform risk stratification and targeted intervention strategies at both a clinical and community level. We highlight the need to track, identify and implement early interventions among individuals at increased risk of developing loneliness as a result of social isolation. Of the interventions used to combat loneliness and social isolation, effective strategies include those that facilitate engagement in meaningful, satisfying group activities, and psychological interventions to address the maladaptive conditions associated with loneliness (16). As in-person intervention strategies during pandemics may be limited or impossible, the use of technologies, such as apps, may remain an important tool, albeit limited by the digital divide, thus potentially excluding significant numbers of particularly vulnerable older people. These and other adaptive strategies to improve knowledge, awareness and self-coping will be vital in mitigating the risk of loneliness, anxiety and depression in older people.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The CCRR study was ethically approved by the Imperial College London Joint Research Compliance Office (20IC5942) and by the East Midlands Derby Health Research Authority (16/EM/0213). The participants provided their written informed consent to participate in the study.
Author Contributions
CR, CdJ, SA-A, CU-M, and LM conceptualized and designed the study. CR performed the data analyses with SA-A, CdJ, and CR conducted the literature review. CR wrote the manuscript with co-authors. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful to all our participants for taking part in this study; for the CHARIOT register and facilitator team: Lesley Williamson, Monica Munoz-Troncoso, Snehal Pandya and Emily Pickering; ICL student volunteers: Mariam Jiwani, Rachel Veeravalli, Islam Saiful, Danielle Rose, Susie Gold, Rachel Nejade and Shehla Shamsuddin; Departmental administrative staff: Stefan McGinn-Summers, Neil Beckford, Inthushaa Indrakumar and Kristina Lakey in AGE for assisting with recruitment to the study and responding to queries about the survey; Kristina Lakey, Stefan McGinn-Summers, Rachel Nejade and Islam Saiful for support with data cleaning; our Departmental Manager: Dinithi Perera, and Project Manager: Heather McLellan-Young, for supporting ethics submissions and advising study document development and our ICL Investigator team, including Alison McGregor, Christina Atchison, David Salman, Thomas Beaney, Nicholas Peters, Aldo Faisal, and Jennifer Quint for contributing to the survey design and ongoing improvements.
References
1. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health (2020) 5(5):e256. doi: 10.1016/S2468-2667(20)30061-X
2. Newman MG, Zainal NH. The value of maintaining social connections for mental health in older people. Lancet Public Health (2020) 5(1):e12–e3. doi: 10.1016/S2468-2667(19)30253-1
3. Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health (2020) 5(1):e62–70. doi: 10.1016/S2468-2667(19)30230-0
4. Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ Can Med Assoc J = J l’Association Med Can (2003) 168(10):1245–51.
5. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun (2020) S0889-1591(20):30954–5. doi: 10.1016/j.bbi.2020.05.048
6. Saltzman LY, Hansel TC, Bordnick PS. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol Trauma (2020) 12(S1):S55–S7. doi: 10.1037/tra0000703
7. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
8. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry (2020) 66(4):317–20. doi: 10.1177/0020764020915212
9. Coronini-Cronberg S, John Maile E, Majeed A. Health inequalities: the hidden cost of COVID-19 in NHS hospital trusts? J R Soc Med (2020) 113(5):179–84. doi: 10.1177/0141076820925230
10. Lara E, Caballero FF, Rico-Uribe LA, Olaya B, Haro JM, Ayuso-Mateos JL, et al. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiatry (2019) 34(11):1613–22. doi: 10.1002/gps.5174
11. Yu B, Steptoe A, Chen Y, Jia X. Social isolation, rather than loneliness, is associated with cognitive decline in older adults: the China Health and Retirement Longitudinal Study. Psychol Med (2020) 1–8. doi: 10.1017/S0033291720001014
12. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (2020) 396(10248):413–46. doi: 10.1016/S0140-6736(20)30367-6
13. Rafnsson SB, Orrell M, d’Orsi E, Hogervorst E, Steptoe A. Loneliness, Social Integration, and Incident Dementia Over 6 Years: Prospective Findings From the English Longitudinal Study of Ageing. J Gerontol B Psychol Sci Soc Sci (2020) 75(1):114–24. doi: 10.1093/geronb/gbx087
14. Sonderskov KM, Dinesen PT, Santini ZI, Ostergaard SD. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr (2020) 32(4):226–8. doi: 10.1017/neu.2020.15
15. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
16. Smith BJ, Lim MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract (2020) 30(2):3022008. doi: 10.17061/phrp3022008
17. Household Impacts of COVID-19 Survey. In: Statistics ABo, editor Australian Bureau of Statistics (2020). Available at: https://www.abs.gov.au/ausstats/abs@.nsf/mf/4940.02020.
18. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry (2020) S2215-0366(20)30308–4. doi: 10.1016/S2215-0366(20)30308-4
19. Rodriguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological Impact and Associated Factors During the Initial Stage of the Coronavirus (COVID-19) Pandemic Among the General Population in Spain. Front Psychol (2020) 11:1540. doi: 10.3389/fpsyg.2020.01540
20. Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr (2020) 51:102076. doi: 10.1016/j.ajp.2020.102076
21. Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, et al. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int J Environ Res Public Health (2020) 17(9):3165–78. doi: 10.3390/ijerph17093165
22. Jahanshahi AA, Dinani MM, Madavani AN, Li J, Zhang SX. The distress of Iranian adults during the Covid-19 pandemic - More distressed than the Chinese and with different predictors. Brain Behav Immun (2020) 87:124–5. doi: 10.1016/j.bbi.2020.04.081
23. Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Lopez-Gomez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun (2020) 87:172–6. doi: 10.1016/j.bbi.2020.05.040
24. Larsen ME, Curry L, Mastellos N, Robb C, Car J, Middleton LT. Development of the CHARIOT Research Register for the Prevention of Alzheimer’s Dementia and Other Late Onset Neurodegenerative Diseases. PloS One (2015) 10(11):e0141806. doi: 10.1371/journal.pone.0141806
25. Buysse DJ, Reynolds CF,3, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res (1989) 28(2):193–213. doi: 10.1016/0165-1781(89)90047-4
26. RL S. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas (1977) 1:385–401. doi: 10.1177/014662167700100306
27. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand (1983) 67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
28. Djukanovic I, Carlsson J, Arestedt K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65-80 years old? A psychometric evaluation study. Health Qual Life Outcomes (2017) 15(1):193. doi: 10.1186/s12955-017-0759-9
29. Livermore N, Sharpe L, McKenzie D. Panic attacks and panic disorder in chronic obstructive pulmonary disease: a cognitive behavioral perspective. Respir Med (2010) 104(9):1246–53. doi: 10.1016/j.rmed.2010.04.011
30. Fenton WS, Stover ES. Mood disorders: cardiovascular and diabetes comorbidity. Curr Opin Psychiatry (2006) 19(4):421–7. doi: 10.1097/01.yco.0000228765.33356.9f
31. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care (2001) 24(6):1069–78. doi: 10.2337/diacare.24.6.1069
32. Survey results. Understanding people's concerns about the mental health impacts of the COVID-19 pandemic. UK: The Academy of Medical Sciences (2020).
33. Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry (2020) 7(6):547–60. doi: 10.1016/S2215-0366(20)30168-1
34. Matthews T, Danese A, Caspi A, Fisher HL, Goldman-Mellor S, Kepa A, et al. Lonely young adults in modern Britain: findings from an epidemiological cohort study. Psychol Med (2019) 49(2):268–77. doi: 10.1017/S0033291718000788
35. Elovainio M, Hakulinen C, Pulkki-Raback L, Virtanen M, Josefsson K, Jokela M, et al. Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lancet Public Health (2017) 2(6):e260–e6. doi: 10.1016/S2468-2667(17)30075-0
36. Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav (2009) 50(1):31–48. doi: 10.1177/002214650905000103
37. Tian F, Li H, Tian S, Yang J, Shao J, Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res (2020) 288:112992. doi: 10.1016/j.psychres.2020.112992
38. Palmer K, Di Iulio F, Varsi AE, Gianni W, Sancesario G, Caltagirone C, et al. Neuropsychiatric predictors of progression from amnestic-mild cognitive impairment to Alzheimer’s disease: the role of depression and apathy. J Alzheimers Dis (2010) 20(1):175–83. doi: 10.3233/JAD-2010-1352
39. Kay-Stacey M, Attarian H. Advances in the management of chronic insomnia. BMJ (2016) 354:i2123. doi: 10.1136/bmj.i2123
40. Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res (2020) 289:113076. doi: 10.1016/j.psychres.2020.113076
41. Lauriola M, Carleton RN, Tempesta D, Calanna P, Socci V, Mosca O, et al. A Correlational Analysis of the Relationships among Intolerance of Uncertainty, Anxiety Sensitivity, Subjective Sleep Quality, and Insomnia Symptoms. Int J Environ Res Public Health (2019) 16(18):3253–68. doi: 10.3390/ijerph16183253
42. Griffin SC, Williams AB, Mladen SN, Perrin PB, Dzierzewski JM, Rybarczyk BD. Reciprocal Effects Between Loneliness and Sleep Disturbance in Older Americans. J Aging Health (2019) 898264319894486. doi: 10.1177/0898264319894486
43. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica (2020) 36(4):e00054020. doi: 10.1590/0102-311x00054020
44. Ozdin S, Bayrak Ozdin S. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry (2020) 66(5):504–11. doi: 10.1177/0020764020927051
45. Malhi GS, Mann JJ. Depression. Lancet (2018) 392(10161):2299–312. doi: 10.1016/S0140-6736(18)31948-2
46. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and Risk Factors Associated With Mental Health Symptoms Among the General Population in China During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open (2020) 3(7):e2014053. doi: 10.1001/jamanetworkopen.2020.14053
47. Dahlberg L, McKee KJ. Correlates of social and emotional loneliness in older people: evidence from an English community study. Aging Ment Health (2014) 18(4):504–14. doi: 10.1080/13607863.2013.856863
Keywords: COVID-19, older adults, anxiety, depression, mental health, social isolation, loneliness
Citation: Robb CE, de Jager CA, Ahmadi-Abhari S, Giannakopoulou P, Udeh-Momoh C, McKeand J, Price G, Car J, Majeed A, Ward H and Middleton L (2020) Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Front. Psychiatry 11:591120. doi: 10.3389/fpsyt.2020.591120
Received: 03 August 2020; Accepted: 31 August 2020;
Published: 17 September 2020.
Edited by:
Gianfranco Spalletta, Santa Lucia Foundation (IRCCS), ItalyReviewed by:
André Hajek, University Medical Center Hamburg-Eppendorf, GermanyFederica Piras, Santa Lucia Foundation (IRCCS), Italy
Copyright © 2020 Robb, de Jager, Ahmadi-Abhari, Giannakopoulou, Udeh-Momoh, McKeand, Price, Car, Majeed, Ward and Middleton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Celeste A. de Jager, Yy5sb290c0BpbXBlcmlhbC5hYy51aw==
 Catherine E. Robb1
Catherine E. Robb1 Celeste A. de Jager
Celeste A. de Jager