- 1College of Physical Education and Sports Science, HengYang Normal University, Hengyang, China
- 2Department of Neuroscience and Regenerative Medicine, Augusta University, Augusta, GA, United States
- 3Laboratory of Laser Sports Medicine, College of Physical Education and Sports Science, South China Normal University, Guangzhou, China
First reported in Dec 2019, the on-going COVID-19 pandemic has become a public health emergency of international concern (PHEIC). The isolation and quarantine during the COVID-19 pandemic limited the physical and social activities of the population, which contributed to the increased prevalence of mental disorder. Depression and anxiety are the most common mental illnesses conferring a serious impact on individuals' life quality. This review summarizes the mental health consequences of COVID-19, especially for depression and anxiety. Exercise as an intervention for anxiety and depression has been demonstrated in both of the animal studies and human clinical trials. The underlying mechanism including the regulation on the production of brain-derived neurotrophic factor (BDNF), D-β-hydroxybutyrate, synaptic transmission, hypothalamic pituitary adrenal (HPA) axis, tryptophan hydroxylase, GSK3β/β-catenin pathway, neuroinflammation, oxidative stress and PGC-1α1-PPAR axis. In addition, we summarized the exercise strategies to fight against anxiety and depression according to the information from American College of Sports Medicine (ACSM), World Health Organization and recent literatures about physical exercise during COVID-19.
Introduction
Since the first coronavirus infection (COVID-19) case reported in Dec 2019, the COVID-19 continue to emerge and represent a serious issue to public health (1). In the past several months, increased number of confirmed coronavirus cases and deaths, stay-at-home restriction and tons of information about COVID-19 inevitably conferred impact on people's mental health, especially for people already living with mental disorder (2). According to a perspective article published in the New England Journal of Medicine, depression and anxiety may develop to be side effects of COVID-19 after the Covid-19 Pandemic (3). However, the medical care required to large number of COVID-19 cases induced the currently ignorance regarding public mental health during the coronavirus pandemic (1, 3).
According to previous studies, more than 50% of patients with severe acute respiratory syndrome (SARS) and middle east respiratory syndrome (MERS) experienced varying degrees of mental disorder after the outbreak of SARS in 2003 and MERS in 2015 (1, 4), indicating widespread outbreaks of infectious diseases were usually closely related to the increased prevalence of mental disorders (5). Among these disorders, anxiety and depression are the most common mental illnesses conferring a serious impact on individuals' life quality (6). Researchers in China investigated the psychological impact of the COVID-19 during the initial stage of coronavirus and found a high percent of the respondents with moderate to severe depressive (16.5%) and anxiety (28.8%) symptoms (7). Although emergency psychological crisis interventions has been performed to reduce the mental impact induced by COVID-19, changings to the public mental health still exist (8).
The beneficial effect of exercise on improving physical health and fighting disease has be widely studied (9, 10). A large body of evidence suggested regular exercise could significantly reduce the risk of depression, anxiety and considered to be beneficial in the prevention of about 25 conditions (11–14). Furthermore, physical inactivity has been considered as a modifiable risk factor for numerous diseases including depression and anxiety (15). Here, we reviewed the recent studies concerning mental health related to COVID-19 coronavirus and the beneficial role of exercise against anxiety and depression. Exercise type, exercise frequency, exercise intensity and the underlying mechanism will be discussed.
Method
We conducted a narrative review of recent studies concerning mental health related to COVID-19 coronavirus and the beneficial role of exercise against anxiety and depression.
A literature search within the PubMed and Web of Science databases was conducted. Literatures with clear description of exercise type, exercise frequency, exercise intensity and effect of exercise on anxiety and depression were included.
Increased Risk of Mental Disorders During The Covid-19 Pandemic
As a “public health emergency of international concern (PHEIC)” for the entire world, COVID-19 has caused a rapid growth in the number of confirmed and suspected cases in the past several months (16). Isolation and quarantine were proven as effective measures contributing to the successful containment of the COVID-19 in China and other regions (17). Isolation was defined as the separation and activity restriction of ill persons with infectious disease to prevent its transmission to others. The definition of quarantine differs from isolation referring to the activity restriction of healthy persons who have been exposed to an infectious disease and may suffer with this disease in the future (18). Although the isolation and quarantine were two of the effective disease-control methods according to previous experience including SARS in 2003 (18), people in quarantine or isolation reported a high prevalence of symptoms of mental disorders (18). For the confirmed and suspected patients, they underwent the fear of the severe consequences and quarantine (19, 20). For the medical service provider, especially those working on the Covid-19 battlefront, they are at both high risk of Covid-19 infection and mental health problems, as they experience the fear and worry about their own health, and the spreading the virus to their relatives and friends (20). For other people, stressors during quarantine, including fears of infection, boredom and frustration, inadequate supplies, inadequate information and financial loss, contributed to poorer mental health (21). In addition, due to the mandatory quarantine procedures in most of the countries suffering the virus, people, especially for people already living with mental disorder, may experience depression, despair and anxiety (2). According to a previous study including 1,210 participants in China during the period January to February, 54% of respondent reported they suffered moderate to severe psychological impacts from the virus. About one-third of them reported moderate to severe anxiety symptoms, and 17% of them reported obvious depressive symptoms (7). The increased level of anxiety and depression in patients and healthy persons were detected after the stay-at-home order in several countries (22–24). As we do not know how long coronavirus disruptions will last, finding an intervention to prevent or alleviate the psychological impacts is urgently needed.
Exercise as an Intervention for Anxiety and Depression During The COVID-19 Pandemic
The effect of exercise in treating or preventing anxiety and depression has been demonstrated in numerous studies (25–27), and widely accepted as an affordable, non-invasive, and easily accessible measures for individual with mental disorders (28, 29). Recently, a study reported that, as people were rarely able to get access to exercise facilities during the Covid-19 pandemic, exergames based on the combination of exercise with appealing digital games was a potential method to cope with anxiety (30). A 20 min single session exergame at moderate intensity were able to significantly reduce the levels of anxiety in healthy person and 8 week exergames performed 2 days per week (60 min per session) was demonstrated to alleviate the anxiety levels in patients (30–32). For Covid-19 patients, relaxation techniques and breathing exercises were recommend as one of the interventions to improve acute anxiety, although more evidence is needed (33). Furthermore, a study on college students demonstrated daily physical activity confers beneficial effects in reducing Covid-19-induced stress and anxiety (34).
Effects and Mechanisms of Exercise on Depression
Depression is one of the most prevalent mental disease affecting around 340 million people all over the world (35), and exert a significant financial and emotional burden to both families and society (36). Patients with depression presented low levels of mood, feelings of guilt, decreased appetite, poor sleep quality, helplessness, low self-worth, fatigue, psychomotor retardation, low interest in social interaction and sexual activity (37). Stressful events from work place and school or abnormal endocrine function such as hypercortisolism are the common risk factors contributing to depression (38), and about 50% of the depression is determined by gene (37).
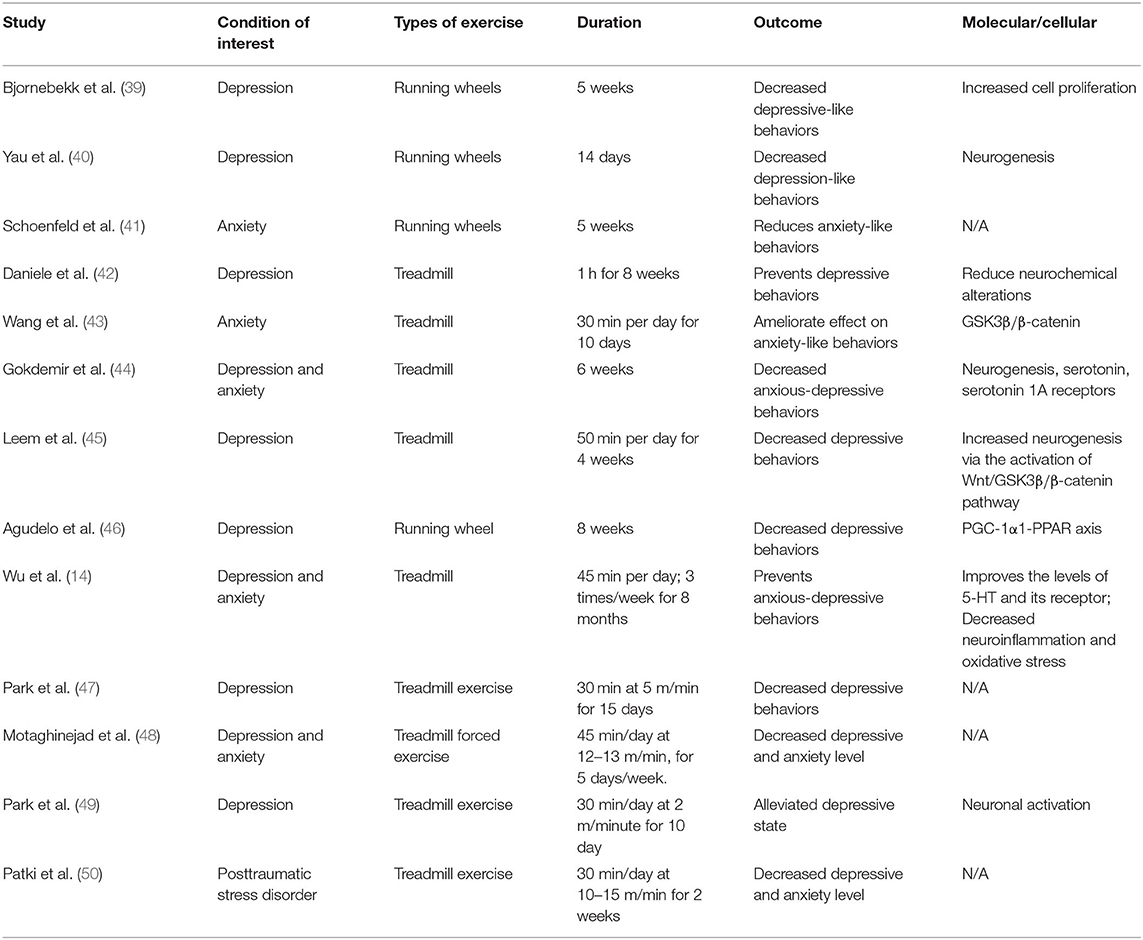
Studies on animals demonstrated the beneficial role of exercise on depression depends on the regulation of neurotransmitter, neurogenesis, neurotrophic factors, and cerebral blood flow (Table 1) (51). As reported, exercise could induced the increased level of brain-derived neurotrophic factor (BDNF), which contributed the increased ability against anxiety and depression in mice (52). One of the possible mechanisms was due to the accumulation of an endogenous molecule, D-β-hydroxybutyrate (DBHB), in the hippocampus. The increased DBHB level after long-term exercise could cross the blood brain barriers (BBB) and inhibit class I histone deacetylases, which will specifically improve the expression of BDNF and affect synaptic transmission (52). In a sleep deprivation-induced depression mouse model, exercise was also found to normalize the decreased levels of BDNF, and therefore exert neuroprotective effect and neurotrophic effect (52). In addition, study demonstrated exercise pretreatment could prevent depressive behavior and neurochemical alterations, such as increased levels of norepinephrine (NE), serotonin and its metabolite in the mouse brain, associated with sleep deprivation (42, 44). Furthermore, in a maternal separation-induced depression animal model, the level of 5-hydroxytryptamine (5-HT) and tryptophan hydroxylase (TPH) were decreased in the dorsal raphe. However, treadmill exercise was able to alleviate depression-like behavior through increasing 5-HT and TPH expression (43), and GSK3β/β-catenin pathway were also believed involved in this process (43). In AD patients, depression is a first sign of cognitive decline at the early stages of AD progression (53). In our previous study, long-term exercise training has been demonstrated as an effective approach to prevent depression in transgenic AD rats, involving the important role of neuroinflammation, oxidative stress, 5-HT and its receptor regulated by exercise training (14). In addition, a well-designed study found transgenic mice with overexpression of muscle PGC-1α are resilient to stress-induced depression and control plasma and brain kynurenine/kynurenic acid balance, suggesting PGC-1α1-PPAR axis in skeletal muscle as a novel target of exercise in the prevention of depression (14).
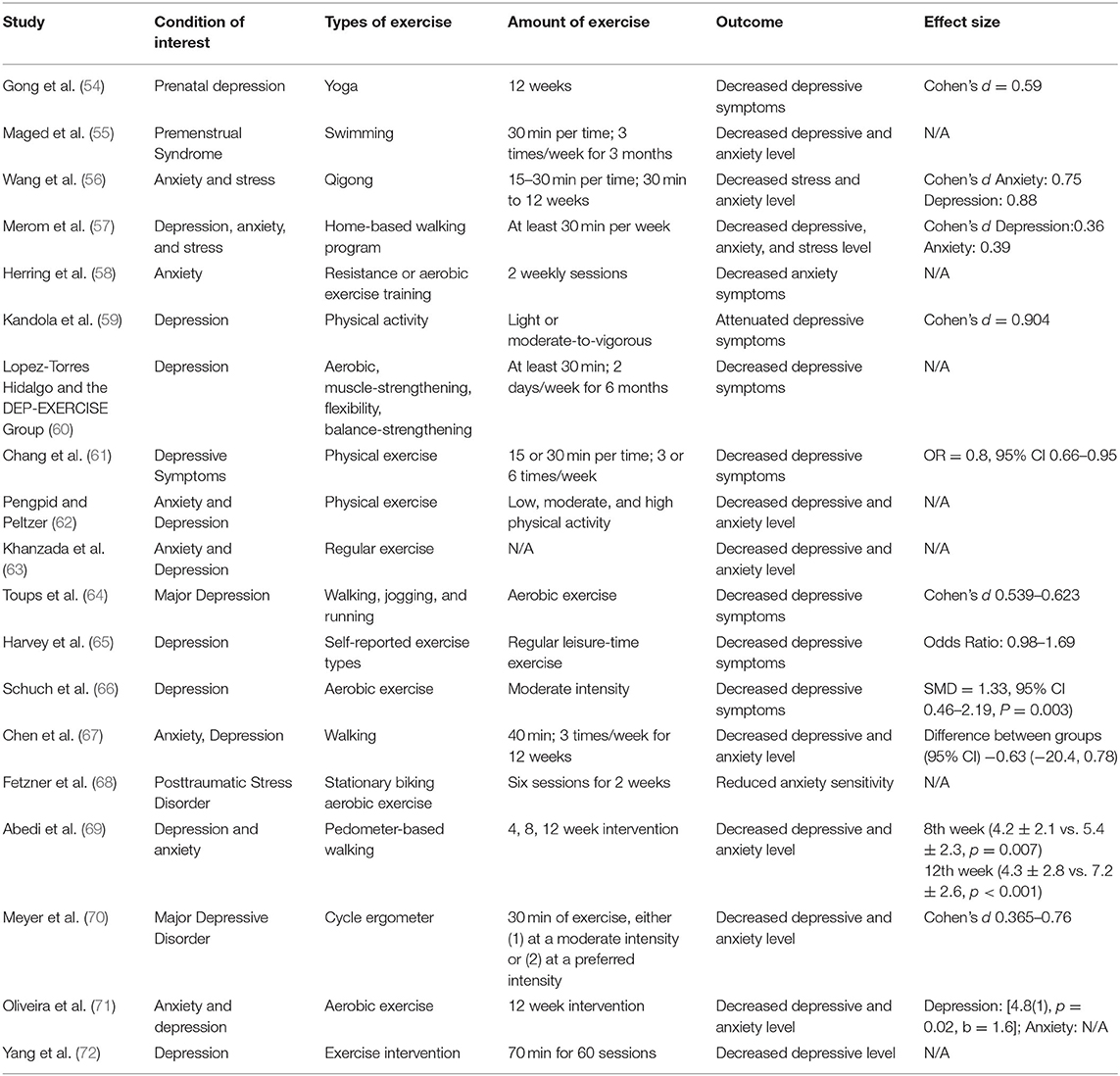
Studies on human also provided tons of evidence on the beneficial role of exercise on depression (Table 2) (63–66). In a prospective cohort study, sedentary behavior was positively associated with a higher depression scores at different ages. In contrast, moderate-to-vigorous physical activity were negatively related to symptoms of depression. Therefore, this study suggested that increased light activity and reduced sedentary behavior might contribute to the decreased prevalence of depression (59). Although in another study, there were only small effect in favor of exercise in the inhibition of depression, the small sample size, a high heterogeneity in the participants, interventions and methods of measurement may limit the ability to draw positive results (73). In addition, studies from different countries and regions supported the beneficial of regular exercise on depression. A study including 312 Spanish patients with clinically significant depression over 65 years old reported that at least 60 min daily moderate-intensity regular exercise (muscle strengthening, aerobic exercise, flexibility and balance exercises) could significantly alleviate depression symptoms (60). An 8 year follow-up study in Finland found persons with dyskinesia and a sedentary lifestyle were at higher risk for depression compared with physically active individuals with intact mobility (74). A prospective cohort study from Taiwan reported that three times a week of moderate intensity (at least 15 min per time) continuous exercise could significantly decrease the risk of depressive symptoms, suggesting moderate-intensity regular exercise was beneficial way to improve mental health (61). Furthermore, a study in Myanmar and Vietnam found participant with less sedentary behavior and high physical activity were at lower risk of having depression (62). Depression is also one of the most common complications associated with physical diseases and symptoms (75). For cancer patients, routine care with 40 min per time, three time a week home exercise for 12 weeks significantly reduced the level of depression compared with usual-care group without home-based walking exercise (67). For patients with post-traumatic stress disorder (PTSD), depression is one of the common symptoms (76, 77). Two week fixed bicycle aerobic exercise was able to attenuate PTSD severity and depression symptom (68). According to previous study, depression are very common among the elderly woman, and postmenopausal individuals are vulnerable to depression (78). However, 12 week pedometer-based walking significantly decreased the levels of depression (69). The dysfunction of hypothalamic–pituitary–adrenal (HPA) axis, the increased secretion of corticotropin-releasing hormone (CRH), the impaired responsiveness to glucocorticoids, the increased size and activity of the pituitary were found in patients in depression patients. The ability of exercise on regulating hypothalamo-pituitary adrenal (HPA) axis supported physical exercise may one of the method to improve depression symptoms (79, 80).
Effects and Mechanisms of Exercise on Anxiety
According to previous studies, nearly one-half of people diagnosed with depression will also experience comorbid anxiety (81). Anxiety is one of the most common mental health diseases contributing to poor concentration, emotional changes, impaired sleep quality and difficulties in performing daily tasks (82, 83). Due to the typical symptoms, including sweating, shaking, chills, rapid heartbeat, poor mental state and hyperventilation, anxiety was defined as a specific psychiatric disorder (37). As reported by previous studies, 25% of the population reported at least one episode of anxiety disorder during their lifetime, and 6% of men and 13% of women suffer from anxiety disorders in the United States (84). Compared with drug therapy, exercise is considered as an alternative therapy for anxiety disorders, which has lower cost and fewer side effects.
Although compared with human studies, preclinical animal anxiety research was limited by animal models and effective anxiety tests (85, 86), previous studies suggests that exercise can significantly improve anxiety symptoms (14, 26, 37, 87). The possible underlying possible mechanism may rely on the regulation of hypothalamic-pituitary-adrenal (HPA) axis (88), the upregulation of BDNF (52), the improvement of neurogenesis and angiogenesis (89, 90), and the regulation of inflammatory systems (91). HPA axis dysfunction plays an important role in the onset of anxiety (92). The unexpected or/and long-term stress response along HPA axis is able to induce fear, sympathetic disorder and excessive vigilance, which are closely associated with anxiety (88). However, resistance exercise training was able to regulate cortisol levels, which is one of the functional production of the HPA axis (93, 94). In addition to learning and memory, the hippocampus is also an important brain region involved in social cognition and emotion processing (95). According to previous studies, exercise exerted anti-anxiety effects by improving hippocampal neurogenesis and normalizing the neurotransmission of neuropeptide Y (NPY) (96). However, more studies on this mechanism are still needed, as other studies found although exercise can improve adult neurogenesis, the new neurons are not involved in the decreased anxiety-like behavior (41). Similar to depression, the decreased BDNF level is a vulnerability factor for anxiety (97). Numerous studies have found that physical exercise can increase the expression of BDNF in the dentate gyrus (98, 99). Although stress-induced increased was able to down-regulate BDNF levels, interestingly, the physical exercise was found to be able to restore BDNF to pre-stress levels, suggesting that exercise protects against stress-induced decreased level of BDNF (93). The regulation of the inflammatory system by exercise is another possible mechanism against anxiety. As reported in previous study, elevated levels of pro-inflammatory cytokine C-reactive protein (CRP) was associated with anxiety disorders (100, 101). Intriguingly, exercise conferred its beneficial effect on anxiety by regulating inflammatory systems (91, 102).
Similar to depression, studies on human from different countries showed that exercise could attenuate anxiety behaviors. A study from the United States showed that regular physical activity could significantly reduce the risk of anxiety compared to their sedentary counterparts (103). A study including individuals in the Netherlands reported that moderate exercise has a negative association with anxiety symptoms compared with non-exercisers (104). For healthy people, individuals with a single bouts of physical exercise have reported less state anxiety, although they did not investigate the effect of accumulated bouts of exercise on anxiety levels (105–107). However, in other interventional studies, researchers found multiple bouts of exercise for 12 months was associated with significant anxiety reduction compared to control group (108). Additionally, different types of exercise on the anxiety reduction were also reported in numerous studies (109). Yoga, an ancient Eastern practice consisting of breath control, physical postures, and meditation, has shown its beneficial effect on patients with severe anxiety symptoms, although the effect was relatively mild (109). Another study investigating the effect of Tai Chi, a traditional Chinese martial art, on anxiety found that older adults with anxiety receiving medical therapy could benefit from Tai Chi exercise compared with those who only receiving medical therapy (110).
Exercise Strategies to Fight Against Anxiety and Depression in Covid-19 Pandemic
The beneficial role of physical exercise has been proved in numerous chronic diseases, including heart disease (111), diabetes (112), asthma (113), back pain (114), arthritis (115), cancer (116), and Alzheimer's disease (13). In addition, as mentioned above, tons of evidence has demonstrated the beneficial role of regular physical exercise on the reduction of anxiety and depression (14, 26, 37, 63–66, 87, 117). Although outdoor physical exercise is unavailable during the outbreak of Covid-19, indoor exercise is recommended in view of the positive effect of exercise on boosting immune system (118–120) and alleviating anxiety and depression (14, 26, 37, 63–66, 87, 117).
According to the information from American College of Sports Medicine (ACSM) (121), World Health Organization (122) and recent literatures about physical exercise during COVID-19 (117), the following exercise strategies were summarized: (1) 150 min moderate-intensity or 75 min vigorous-intensity exercise per week, or perform both of them (or modify according to personal or individual specifications). (2) Home-based exercises including knee-to-elbows, plank, back extensions, squats, side knee lifts, “superman,” “Bridge,” chair dips, chest opener, seated meditation, legs up the wall were recommended. (3) For the outdoor activities allowed by the local government, be active in a local park and keep at least 6 feet distance between you and others. (4) The multi-faceted exercise program is recommended, including aerobic, balance, resistance, coordination and activity training are recommended. (5) Do not use public exercise equipment to avoid virus transmission. Notably, these exercise strategies are recommended for healthy individuals in self-quarantine and cannot replace medical guidance.
Although we believe that home-based exercise best avoids viral transmission, a healthy balance between outdoor and indoor physical activities is optimal when possible. The judgement of where to engage in physical activities should be determined according to individual's living environment, economic status, health status, and local restrictions.
Approaches To Increase Physical Activity Behavior
Although increasing physical activity has demonstrated a beneficial role in fighting anxiety and depression, changing an inactive lifestyle and beginning an exercise regimen is achallenging endeavor for many individuals. According to previous studies, various strategies have been reported as possible approaches to increase physical activity. These include focusing on small quantities of physical activity (e.g., doing exercise during leisure time) (123), improving self-regulation (e.g., learning the benefits of exercise, use of activity trackers to get behavior feedback) (124, 125), strengthening non-conscious processes (e.g., using an enjoyable workout to form an exercise habit) (126), using internet and smartphone apps (127), and increasing accessibility to facilities and environments (e.g., purchasing a treadmill for home use to perform exercise with and compare one's performance with other family members) (125, 128). Also, research suggests a combination of approaches mentioned were better able to lead to improved outcomes (129, 130).
Taken together, the COVID-19 pandemic not only affects physical health, but also mental health (131) Regular physical exercise is for mental health, and able to alleviate the levels of depression and anxiety during COVID-19 pandemic. Staying physically active during the COVID-19 pandemic would contribute to the attenuation of the side effects of COVID-19 on mental health after the pandemic.
Author Contributions
SH and LY drafted the manuscript. SH and CW prepared the tables. LY and LT edited and revised the manuscript. All authors approved the final version of the manuscript.
Funding
This study was supported by Research Grant 19C0276 from Provincial education department of Hunan, startup funding (18D22) from HengYang Normal University, and Innovation Project of Graduate School of South China Normal University (2018LKXM010).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Kim SW, Su KP. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. (2020) 87:4–5. doi: 10.1016/j.bbi.2020.03.025
2. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
3. Pfefferbaum B, North CS. Mental health and the covid-19 pandemic. N Engl J Med. (2020) 383:510–12. doi: 10.1056/NEJMp2008017
4. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. (2009) 31:318–26. doi: 10.1016/j.genhosppsych.2009.03.001
5. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
6. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. (2011) 12:160–74. doi: 10.1016/S1470-2045(11)70002-X
7. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
8. Dong L, Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis. (2020) 26:1616–18. doi: 10.3201/eid2607.200407
9. Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. (2006) 174:801–9. doi: 10.1503/cmaj.051351
10. Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. (2019) 107:525–39. doi: 10.1016/j.neubiorev.2019.09.040
11. Rhodes RE, Warburton DE, Murray H. Characteristics of physical activity guidelines and their effect on adherence: a review of randomized trials. Sports Med. (2009) 39:355–75. doi: 10.2165/00007256-200939050-00003
12. Alford L. What men should know about the impact of physical activity on their health. Int J Clin Pract. (2010) 64:1731–4. doi: 10.1111/j.1742-1241.2010.02478.x
13. Wu C, Yang L, Tucker D, Dong Y, Zhu L, Duan R, et al. Beneficial effects of exercise pretreatment in a sporadic Alzheimer's rat model. Med Sci Sports Exerc. (2018) 50:945–56. doi: 10.1249/MSS.0000000000001519
14. Wu C, Yang L, Li Y, Dong Y, Yang B, Tucker LD, et al. Effects of exercise training on anxious-depressive-like behavior in alzheimer rat. Med Sci Sports Exerc. (2020) 52:1456–69. doi: 10.1249/MSS.0000000000002294
15. Yates BE, DeLetter MC, Parrish EM. Prescribed exercise for the treatment of depression in a college population: an interprofessional approach. Perspect Psychiatr Care. (2020) 56:894–9. doi: 10.1111/ppc.12508
16. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM. (2020) 113:311–2. doi: 10.1093/qjmed/hcaa110
17. Sjodin H, Wilder-Smith A, Osman S, Farooq Z, Rocklov J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Euro Surveill. (2020) 25:2000280. doi: 10.2807/1560-7917.ES.2020.25.13.2000280
18. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
19. Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. (2020) 16:1732–8. doi: 10.7150/ijbs.45120
20. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
21. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
22. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. (2020) 288:112954. doi: 10.1016/j.psychres.2020.112954
23. Li X, Dai T, Wang H, Shi J, Yuan W, Li J, et al. [Clinical analysis of suspected COVID-19 patients with anxiety and depression]. Zhejiang Da Xue Xue Bao Yi Xue Ban. (2020) 49:203–8. doi: 10.3785/j.issn.1008-9292.2020.03.02
24. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. (2020) 36:e00054020. doi: 10.1590/0102-311x00054020
25. Strohle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. (2009) 116:777–84. doi: 10.1007/s00702-008-0092-x
26. Stonerock GL, Hoffman BM, Smith PJ, Blumenthal JA. Exercise as treatment for anxiety: systematic review and analysis. Ann Behav Med. (2015) 49:542–56. doi: 10.1007/s12160-014-9685-9
27. Stubbs B, Vancampfort D, Rosenbaum S, Firth J, Cosco T, Veronese N, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: a meta-analysis. Psychiatry Res. (2017) 249:102–8. doi: 10.1016/j.psychres.2016.12.020
28. Rimes RR, de Souza Moura AM, Lamego MK, de Sa Filho AS, Manochio J, Paes F, et al. Effects of exercise on physical and mental health, and cognitive and brain functions in schizophrenia: clinical and experimental evidence. CNS Neurol Disord Drug Targets. (2015) 14:1244–54. doi: 10.2174/1871527315666151111130659
29. Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V. Exercise and mental health. Maturitas. (2017) 106:48–56. doi: 10.1016/j.maturitas.2017.09.003
30. Viana RB, de Lira CAB. Exergames as coping strategies for anxiety disorders during the COVID-19 quarantine period. Games Health J. (2020) 9:147–9. doi: 10.1089/g4h.2020.0060
31. Collado-Mateo D, Dominguez-Munoz FJ, Adsuar JC, Garcia-Gordillo MA, Gusi N. Effects of exergames on quality of life, pain, and disease effect in women with fibromyalgia: a randomized controlled trial. Arch Phys Med Rehabil. (2017) 98:1725–31. doi: 10.1016/j.apmr.2017.02.011
32. Viana RB, Alves CL, Vieira CA, Vancini RL, Campos MH, Gentil P, et al. Anxiolytic effects of a single session of the exergame zumba((R)) fitness on healthy young women. Games Health J. (2017) 6:365–70. doi: 10.1089/g4h.2017.0085
33. Khawam E, Khouli H, Pozuelo L. Treating acute anxiety in patients with COVID-19. Cleve Clin J Med. (2020) doi: 10.3949/ccjm.87a.ccc016. [Epub ahead of print].
34. Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int J Environ Res Public Health. (2020) 17:3722. doi: 10.3390/ijerph17103722
35. Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. (2016) 202:67–86. doi: 10.1016/j.jad.2016.03.063
36. Cooney G, Dwan K, Mead G. Exercise for depression. JAMA. (2014) 311:2432–3. doi: 10.1001/jama.2014.4930
37. Wegner M, Helmich I, Machado S, Nardi AE, Arias-Carrion O, Budde H. Effects of exercise on anxiety and depression disorders: review of meta- analyses and neurobiological mechanisms. CNS Neurol Disord Drug Targets. (2014) 13:1002–14. doi: 10.2174/1871527313666140612102841
38. Stephens MA, Wand G. Stress and the HPA axis: role of glucocorticoids in alcohol dependence. Alcohol Res. (2012) 34:468–83.
39. Bjornebekk A, Mathe AA, Brene S. Running has differential effects on NPY, opiates, and cell proliferation in an animal model of depression and controls. Neuropsychopharmacology. (2006) 31:256–64. doi: 10.1038/sj.npp.1300820
40. Yau SY, Li A, Hoo RL, Ching YP, Christie BR, Lee TM, et al. Physical exercise-induced hippocampal neurogenesis and antidepressant effects are mediated by the adipocyte hormone adiponectin. Proc Natl Acad Sci USA. (2014) 111:15810–5. doi: 10.1073/pnas.1415219111
41. Schoenfeld TJ, McCausland HC, Sonti AN, Cameron HA. Anxiolytic actions of exercise in absence of new neurons. Hippocampus. (2016) 26:1373–8. doi: 10.1002/hipo.22649
42. Daniele T, de Bruin PFC, Rios ERV, de Bruin VMS. Effects of exercise on depressive behavior and striatal levels of norepinephrine, serotonin and their metabolites in sleep-deprived mice. Behav Brain Res. (2017) 332:16–22. doi: 10.1016/j.bbr.2017.05.062
43. Wang LR, Kim SH, Baek SS. Effects of treadmill exercise on the anxiety-like behavior through modulation of GSK3beta/beta-catenin signaling in the maternal separation rat pup. J Exerc Rehabil. (2019) 15:206–12. doi: 10.12965/jer.1938094.047
44. Gokdemir O, Cetinkaya C, Gumus H, Aksu I, Kiray M, Ates M, et al. The effect of exercise on anxiety- and depression-like behavior of aged rats. Biotech Histochem. (2020) 95:8–17. doi: 10.1080/10520295.2019.1624825
45. Leem YH, Kato M, Chang H. Regular exercise and creatine supplementation prevent chronic mild stress-induced decrease in hippocampal neurogenesis via Wnt/GSK3beta/beta-catenin pathway. J Exerc Nutr Biochem. (2018) 22:1–6. doi: 10.20463/jenb.2018.0009
46. Agudelo LZ, Femenia T, Orhan F, Porsmyr-Palmertz M, Goiny M, Martinez-Redondo V, et al. Skeletal muscle PGC-1alpha1 modulates kynurenine metabolism and mediates resilience to stress-induced depression. Cell. (2014) 159:33–45. doi: 10.1016/j.cell.2014.07.051
47. Park SS, Kim TW, Park HS, Seo TB, Kim YP. Effects of treadmill exercise on activity, short-term memory, vascular dysfunction in maternal separation rats. J Exerc Rehabil. (2020) 16:118–23. doi: 10.12965/jer.2040234.117
48. Motaghinejad M, Motevalian M, Larijani SF, Khajehamedi Z. Protective effects of forced exercise against methylphenidate-induced anxiety, depression and cognition impairment in rat. Adv Biomed Res. (2015) 4:134. doi: 10.4103/2277-9175.161528
49. Park JK, Lee SJ, Oh CS. Treadmill exercise exerts ameliorating effect on isolation-induced depression via neuronal activation. J Exerc Rehabil. (2013) 9:234–42. doi: 10.12965/jer.130005
50. Patki G, Li L, Allam F, Solanki N, Dao AT, Alkadhi K, et al. Moderate treadmill exercise rescues anxiety and depression-like behavior as well as memory impairment in a rat model of posttraumatic stress disorder. Physiol Behav. (2014) 130:47–53. doi: 10.1016/j.physbeh.2014.03.016
51. Deslandes A, Moraes H, Ferreira C, Veiga H, Silveira H, Mouta R, et al. Exercise and mental health: many reasons to move. Neuropsychobiology. (2009) 59:191–8. doi: 10.1159/000223730
52. Sleiman SF, Henry J, Al-Haddad R, El Hayek L, Abou Haidar E, Stringer T, et al. Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body beta-hydroxybutyrate. Elife. (2016) 5:e15092. doi: 10.7554/eLife.15092.012
53. Visser PJ, Verhey FR, Ponds RW, Kester A, Jolles J. Distinction between preclinical Alzheimer's disease and depression. J Am Geriatr Soc. (2000) 48:479–84. doi: 10.1111/j.1532-5415.2000.tb04992.x
54. Gong H, Ni C, Shen X, Wu T, Jiang C. Yoga for prenatal depression: a systematic review and meta-analysis. BMC Psychiatry. (2015) 15:14. doi: 10.1186/s12888-015-0393-1
55. Maged AM, Abbassy AH, Sakr HRS, Elsawah H, Wagih H, Ogila AI, et al. Effect of swimming exercise on premenstrual syndrome. Arch Gynecol Obstet. (2018) 297:951–9. doi: 10.1007/s00404-018-4664-1
56. Wang CW, Chan CH, Ho RT, Chan JS, Ng SM, Chan CL. Managing stress and anxiety through qigong exercise in healthy adults: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Altern Med. (2014) 14:8. doi: 10.1186/1472-6882-14-8
57. Merom D, Phongsavan P, Wagner R, Chey T, Marnane C, Steel Z, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders–a pilot group randomized trial. J Anxiety Disord. (2008) 22:959–68. doi: 10.1016/j.janxdis.2007.09.010
58. Herring MP, Jacob ML, Suveg C, Dishman RK, O'Connor PJ. Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. (2012) 81:21–8. doi: 10.1159/000327898
59. Kandola A, Lewis G, Osborn DPJ, Stubbs B, Hayes JF. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: a prospective cohort study. Lancet Psychiatry. (2020) 7:262–71. doi: 10.1016/S2215-0366(20)30034-1
60. Lopez-Torres Hidalgo J, DEP-EXERCISE Group. Effectiveness of physical exercise in the treatment of depression in older adults as an alternative to antidepressant drugs in primary care. BMC Psychiatry. (2019) 19:21. doi: 10.1186/s12888-018-1982-6
61. Chang YC, Lu MC, Hu IH, Wu WI, Hu SC. Effects of different amounts of exercise on preventing depressive symptoms in community-dwelling older adults: a prospective cohort study in Taiwan. BMJ Open. (2017) 7:e014256. doi: 10.1136/bmjopen-2016-014256
62. Pengpid S, Peltzer K. High sedentary behaviour and low physical activity are associated with anxiety and depression in Myanmar and Vietnam. Int J Environ Res Public Health. (2019) 16:1251. doi: 10.3390/ijerph16071251
63. Khanzada FJ, Soomro N, Khan SZ. Association of physical exercise on anxiety and depression amongst adults. J Coll Phys Surg Pak. (2015) 25:546–8.
64. Toups M, Carmody T, Greer T, Rethorst C, Grannemann B, Trivedi MH. Exercise is an effective treatment for positive valence symptoms in major depression. J Affect Disord. (2017) 209:188–94. doi: 10.1016/j.jad.2016.08.058
65. Harvey SB, Overland S, Hatch SL, Wessely S, Mykletun A, Hotopf M. Exercise and the prevention of depression: results of the HUNT cohort study. Am J Psychiatry. (2018) 175:28–36. doi: 10.1176/appi.ajp.2017.16111223
66. Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. (2016) 77:42–51. doi: 10.1016/j.jpsychires.2016.02.023
67. Chen HM, Tsai CM, Wu YC, Lin KC, Lin CC. Randomised controlled trial on the effectiveness of home-based walking exercise on anxiety, depression and cancer-related symptoms in patients with lung cancer. Br J Cancer. (2015) 112:438–45. doi: 10.1038/bjc.2014.612
68. Fetzner MG, Asmundson GJ. Aerobic exercise reduces symptoms of posttraumatic stress disorder: a randomized controlled trial. Cogn Behav Ther. (2015) 44:301–13. doi: 10.1080/16506073.2014.916745
69. Abedi P, Nikkhah P, Najar S. Effect of pedometer-based walking on depression, anxiety and insomnia among postmenopausal women. Climacteric. (2015) 18:841–5. doi: 10.3109/13697137.2015.1065246
70. Meyer JD, Crombie KM, Cook DB, Hillard CJ, Koltyn KF. Serum endocannabinoid and mood changes after exercise in major depressive disorder. Med Sci Sports Exerc. (2019) 51:1909–17. doi: 10.1249/MSS.0000000000002006
71. Oliveira AB, Ribeiro RT, Mello MT, Tufik S, Peres MFP. Anandamide is related to clinical and cardiorespiratory benefits of aerobic exercise training in migraine patients: a randomized controlled clinical trial. Cannabis Cannabinoid Res. (2019) 4:275–84. doi: 10.1089/can.2018.0057
72. Yang J, Tan J, Zheng L, Lu CX, Hou WQ, Liu Y, et al. Plasma BDNF and TrkB mRNA in PBMCs are correlated with anti-depressive effects of 12-weeks supervised exercise during protracted methamphetamine abstinence. Front Mol Neurosci. (2020) 13:20. doi: 10.3389/fnmol.2020.00020
73. Larun L, Nordheim LV, Ekeland E, Hagen KB, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. (2006) 3:CD004691. doi: 10.1002/14651858.CD004691.pub2
74. Lampinen P, Heikkinen E. Reduced mobility and physical activity as predictors of depressive symptoms among community-dwelling older adults: an eight-year follow-up study. Aging Clin Exp Res. (2003) 15:205–11. doi: 10.1007/BF03324501
75. Goodwin GM. Depression and associated physical diseases and symptoms. Dialogues Clin Neurosci. (2006) 8:259–65.
76. Gros DF, Price M, Magruder KM, Frueh BC. Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Res. (2012) 196:267–70. doi: 10.1016/j.psychres.2011.10.022
77. Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand. (2015) 131:350–9. doi: 10.1111/acps.12371
78. Clayton AH, Ninan PT. Depression or menopause? Presentation and management of major depressive disorder in perimenopausal and postmenopausal women. Prim Care Companion J Clin Psychiatry. (2010) 12:PCC08r00747. doi: 10.4088/PCC.08r00747blu
79. Stranahan AM, Lee K, Mattson MP. Central mechanisms of HPA axis regulation by voluntary exercise. Neuromol Med. (2008) 10:118–27. doi: 10.1007/s12017-008-8027-0
80. Duclos M, Tabarin A. Exercise and the hypothalamo-pituitary-adrenal axis. Front Horm Res. (2016) 47:12–26. doi: 10.1159/000445149
81. Hirschfeld RM. The comorbidity of major depression and anxiety disorders: recognition and management in primary care. Prim Care Companion J Clin Psychiatry. (2001) 3:244–54. doi: 10.4088/PCC.v03n0609
82. Mogg K, Bradley BP. Anxiety and threat-related attention: cognitive-motivational framework and treatment. Trends Cogn Sci. (2018) 22:225–40. doi: 10.1016/j.tics.2018.01.001
83. Yu Q, Zhuang Q, Wang B, Liu X, Zhao G, Zhang M. The effect of anxiety on emotional recognition: evidence from an ERP study. Sci Rep. (2018) 8:16146. doi: 10.1038/s41598-018-34289-8
84. Lepine JP. The epidemiology of anxiety disorders: prevalence and societal costs. J Clin Psychiatry. (2002) 63(Suppl. 14):4–8.
85. Steimer T. Animal models of anxiety disorders in rats and mice: some conceptual issues. Dialogues Clin Neurosci. (2011) 13:495–506.
86. Ennaceur A, Chazot PL. Preclinical animal anxiety research - flaws and prejudices. Pharmacol Res Perspect. (2016) 4:e00223. doi: 10.1002/prp2.223
87. Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. (2011) 41:15–28. doi: 10.2190/PM.41.1.c
88. Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J Affect Disord. (2013) 148:12–27. doi: 10.1016/j.jad.2013.01.014
89. Morland C, Andersson KA, Haugen OP, Hadzic A, Kleppa L, Gille A, et al. Exercise induces cerebral VEGF and angiogenesis via the lactate receptor HCAR1. Nat Commun. (2017) 8:15557. doi: 10.1038/ncomms15557
90. Morgan JA, Singhal G, Corrigan F, Jaehne EJ, Jawahar MC, Breen J, et al. Ceasing exercise induces depression-like, anxiety-like, and impaired cognitive-like behaviours and altered hippocampal gene expression. Brain Res Bull. (2019) 148:118–30. doi: 10.1016/j.brainresbull.2019.02.014
91. Moylan S, Eyre HA, Maes M, Baune BT, Jacka FN, Berk M. Exercising the worry away: how inflammation, oxidative and nitrogen stress mediates the beneficial effect of physical activity on anxiety disorder symptoms and behaviours. Neurosci Biobehav Rev. (2013) 37:573–84. doi: 10.1016/j.neubiorev.2013.02.003
92. Faravelli C, Lo Sauro C, Godini L, Lelli L, Benni L, Pietrini F, et al. Childhood stressful events, HPA axis and anxiety disorders. World J Psychiatry. (2012) 2:13–25. doi: 10.5498/wjp.v2.i1.13
93. Adlard PA, Cotman CW. Voluntary exercise protects against stress-induced decreases in brain-derived neurotrophic factor protein expression. Neuroscience. (2004) 124:985–92. doi: 10.1016/j.neuroscience.2003.12.039
94. Crewther BT, Cook C, Cardinale M, Weatherby RP, Lowe T. Two emerging concepts for elite athletes: the short-term effects of testosterone and cortisol on the neuromuscular system and the dose-response training role of these endogenous hormones. Sports Med. (2011) 41:103–23. doi: 10.2165/11539170-000000000-00000
95. Zhu Y, Gao H, Tong L, Li Z, Wang L, Zhang C, et al. Emotion regulation of hippocampus using real-time fMRI neurofeedback in healthy human. Front Hum Neurosci. (2019) 13:242. doi: 10.3389/fnhum.2019.00242
96. Liu PZ, Nusslock R. Exercise-mediated neurogenesis in the hippocampus via BDNF. Front Neurosci. (2018) 12:52. doi: 10.3389/fnins.2018.00052
97. Janke KL, Cominski TP, Kuzhikandathil EV, Servatius RJ, Pang KC. Investigating the role of hippocampal BDNF in anxiety vulnerability using classical eyeblink conditioning. Front Psychiatry. (2015) 6:106. doi: 10.3389/fpsyt.2015.00106
98. Alomari MA, Khabour OF, Alzoubi KH, Alzubi MA. Forced and voluntary exercises equally improve spatial learning and memory and hippocampal BDNF levels. Behav Brain Res. (2013) 247:34–9. doi: 10.1016/j.bbr.2013.03.007
99. Firth J, Stubbs B, Vancampfort D, Schuch F, Lagopoulos J, Rosenbaum S, et al. Effect of aerobic exercise on hippocampal volume in humans: a systematic review and meta-analysis. Neuroimage. (2018) 166:230–8. doi: 10.1016/j.neuroimage.2017.11.007
100. Vogelzangs N, Beekman AT, de Jonge P, Penninx BW. Anxiety disorders and inflammation in a large adult cohort. Transl Psychiatry. (2013) 3:e249. doi: 10.1038/tp.2013.27
101. Michopoulos V, Powers A, Gillespie CF, Ressler KJ, Jovanovic T. Inflammation in fear- and anxiety-based disorders: PTSD, GAD, and beyond. Neuropsychopharmacology. (2017) 42:254–70. doi: 10.1038/npp.2016.146
102. Flynn MG, McFarlin BK, Markofski MM. The anti-inflammatory actions of exercise training. Am J Lifestyle Med. (2007) 1:220–35. doi: 10.1177/1559827607300283
103. Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. (2003) 36:698–703. doi: 10.1016/S0091-7435(03)00042-2
104. De Moor MH, Beem AL, Stubbe JH, Boomsma DI, De Geus EJ. Regular exercise, anxiety, depression and personality: a population-based study. Prev Med. (2006) 42:273–9. doi: 10.1016/j.ypmed.2005.12.002
105. Yeung RR. The acute effects of exercise on mood state. J Psychosom Res. (1996) 40:123–41. doi: 10.1016/0022-3999(95)00554-4
106. Esquivel G, Diaz-Galvis J, Schruers K, Berlanga C, Lara-Munoz C, Griez E. Acute exercise reduces the effects of a 35% CO2 challenge in patients with panic disorder. J Affect Disord. (2008) 107:217–20. doi: 10.1016/j.jad.2007.07.022
107. Strickland JC, Smith MA. The anxiolytic effects of resistance exercise. Front Psychol. (2014) 5:753. doi: 10.3389/fpsyg.2014.00753
108. King AC, Taylor CB, Haskell WL. Effects of differing intensities and formats of 12 months of exercise training on psychological outcomes in older adults. Health Psychol. (1993) 12:292–300. doi: 10.1037/0278-6133.12.4.292
109. Saeed SA, Cunningham K, Bloch RM. Depression and anxiety disorders: benefits of exercise, yoga, and meditation. Am Fam Phys. (2019) 99:620–7.
110. Song QH, Shen GQ, Xu RM, Zhang QH, Ma M, Guo YH, et al. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder. Int J Physiol Pathophysiol Pharmacol. (2014) 6:55–60.
111. Bove AA. Exercise and heart disease. Methodist Debakey Cardiovasc J. (2016) 12:74–5. doi: 10.14797/mdcj-12-2-74
112. Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Cleve Clin J Med. (2017) 84(Suppl. 1):S15–21. doi: 10.3949/ccjm.84.s1.03
113. Lang JE. The impact of exercise on asthma. Curr Opin Allergy Clin Immunol. (2019) 19:118–25. doi: 10.1097/ACI.0000000000000510
114. Alanazi MH, Parent EC, Dennett E. Effect of stabilization exercise on back pain, disability and quality of life in adults with scoliosis: a systematic review. Eur J Phys Rehabil Med. (2018) 54:647–53. doi: 10.23736/S1973-9087.17.05062-6
115. Metsios GS, Kitas GD. Physical activity, exercise and rheumatoid arthritis: effectiveness, mechanisms and implementation. Best Pract Res Clin Rheumatol. (2018) 32:669–82. doi: 10.1016/j.berh.2019.03.013
116. Idorn M, Thor Straten P. Exercise and cancer: from “healthy” to “therapeutic?” Cancer Immunol Immunother. (2017) 66:667–71. doi: 10.1007/s00262-017-1985-z
117. Jurak G, Morrison SA, Leskosek B, Kovac M, Hadzic V, Vodicar J, et al. Physical activity recommendations during the COVID-19 virus outbreak. J Sport Health Sci. (2020) 9:325–7. doi: 10.1016/j.jshs.2020.05.003
118. Gleeson M. Immune function in sport and exercise. J Appl Physiol. (2007) 103:693–9. doi: 10.1152/japplphysiol.00008.2007
119. Simpson RJ, Kunz H, Agha N, Graff R. Exercise and the regulation of immune functions. Prog Mol Biol Transl Sci. (2015) 135:355–80. doi: 10.1016/bs.pmbts.2015.08.001
120. Song M, Chan AT. The potential role of exercise and nutrition in harnessing the immune system to improve colorectal cancer survival. Gastroenterology. (2018) 155:596–600. doi: 10.1053/j.gastro.2018.07.038
121. American College of Sports Medicine (2020). Staying Physically Active During the COVID-19 Pandemic.
122. World Health Organization. Stay Physically Active During Self-Quarantine. (2020). Available online at: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/technical-guidance/stay-physically-active-during-self-quarantine (accessed May 10, 2020).
123. Goenka S, Lee IM. Physical activity lowers mortality and heart disease risks. Lancet. (2017) 390:2609–10. doi: 10.1016/S0140-6736(17)32104-9
124. Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. (2009) 28:690–701. doi: 10.1037/a0016136
125. Schwartz J, Rhodes R, Bredin SSD, Oh P, Warburton DER. Effectiveness of approaches to increase physical activity behavior to prevent chronic disease in adults: a brief commentary. J Clin Med. (2019) 8:295. doi: 10.3390/jcm8030295
126. Kaushal N, Rhodes RE. Exercise habit formation in new gym members: a longitudinal study. J Behav Med. (2015) 38:652–63. doi: 10.1007/s10865-015-9640-7
127. Vandelanotte C, Muller AM, Short CE, Hingle M, Nathan N, Williams SL, et al. Past, present, and future of ehealth and mhealth research to improve physical activity and dietary behaviors. J Nutr Educ Behav. (2016) 48:219–28.e211. doi: 10.1016/j.jneb.2015.12.006
128. Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW, et al. Correlates of physical activity: why are some people physically active and others not? Lancet. (2012) 380:258–71. doi: 10.1016/S0140-6736(12)60735-1
129. Geller K, Lippke S, Nigg CR. Future directions of multiple behavior change research. J Behav Med. (2017) 40:194–202. doi: 10.1007/s10865-016-9809-8
130. Rhodes RE, Janssen I, Bredin SSD, Warburton DER, Bauman A. Physical activity: health impact, prevalence, correlates and interventions. Psychol Health. (2017) 32:942–75. doi: 10.1080/08870446.2017.1325486
Keywords: physical exercise, depression, anxiety, COVID-19, isolation, quarantine
Citation: Hu S, Tucker L, Wu C and Yang L (2020) Beneficial Effects of Exercise on Depression and Anxiety During the Covid-19 Pandemic: A Narrative Review. Front. Psychiatry 11:587557. doi: 10.3389/fpsyt.2020.587557
Received: 26 July 2020; Accepted: 14 October 2020;
Published: 04 November 2020.
Edited by:
Andreas Maercker, University of Zurich, SwitzerlandReviewed by:
Walter Bierbauer, Zurich University of Applied Sciences, SwitzerlandFederica Sancassiani, University of Cagliari, Italy
Copyright © 2020 Hu, Tucker, Wu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luodan Yang, bG95YW5nQGF1Z3VzdGEuZWR1; Chongyun Wu, MjAxMzAyMDg1NkBtLnNjbnUuZWR1LmNu
 Shaojuan Hu
Shaojuan Hu Lorelei Tucker
Lorelei Tucker Chongyun Wu
Chongyun Wu Luodan Yang
Luodan Yang