
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 12 November 2020
Sec. Aging Psychiatry
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.586686
This article is part of the Research TopicCognitive, Psychological, and Psychiatric Consequences of the Coronavirus (COVID-19) Pandemic in the Population of Older Persons with Cognitive Impairment, Dementia, and/or Neuropsychiatric DisordersView all 45 articles
 Renzo Rozzini1,2*
Renzo Rozzini1,2* Angelo Bianchetti2,3
Angelo Bianchetti2,3 Francesca Mazzeo1
Francesca Mazzeo1 Giulia Cesaroni1
Giulia Cesaroni1 Luca Bianchetti4
Luca Bianchetti4 Marco Trabucchi2
Marco Trabucchi2The aim of the study is to describe the clinical characteristics and outcomes of a series of older patients consecutively admitted into a non-ICU ward due to SARS-CoV-2 infection (14, males 11), developing delirium. Hypokinetic delirium with lethargy and confusion was observed in 43% of cases (6/14 patients). A total of eight patients exhibited hyperkinetic delirium and 50% of these patients (4/8) died. The overall mortality rate was 71% (10/14 patients). Among the four survivors we observed two different clinical patterns: two patients exhibited dementia and no ARDS (acute respiratory distress syndrome), while the remaining two patients exhibited ARDS and no dementia. The observed different clinical patterns of delirium (hypokinetic delirium; hyperkinetic delirium with or without dementia; hyperkinetic delirium with or without ARDS) identified patients with different prognosis: we believe these observations may have an impact on the management of older subjects with delirium due to COVID-19.
Although the most frequent and life-threatening complications of coronavirus disease 19 (COVID-19) are respiratory, there are increasing reports of neurological and psychiatric involvement (1).
It is known that delirium can be the symptom of the presentation of many diseases, particularly in frail and older patients, and is recognized as an independent risk factor for mortality (2). The overall prevalence of delirium in the hospital setting is about 14–24%; its prevalence is higher, about 30%, in emergency, surgical, or medical wards (3, 4). To date, the clinical presentation of delirium in older patients with COVID-19 infection have rarely been described; in fact, although some studies focus on epidemiological data and outcome, few studies analyze the clinical aspects of delirium in COVID-19 (5–8). The aim of this study is to describe clinical characteristics and outcomes of a series of elderly patients presenting delirium as the main symptom of COVID-19.
The study was carried out in the COVID ward in an Acute Care Hospital located in Brescia, one of the hardest hit cities by SARS-CoV-2 infection in northern Italy (9). We collected the characteristics of 14 older patients (age range 70–90, mean age 78.2; 11 males) consecutively admitted developing prevalent or incident delirium (respectively 10 and 4 cases). All the patients were admitted with a diagnosis of COVID-19, confirmed by a real-time reverse-transcriptase-polymerase chain reaction (rRT-PCR); three patients came from nursing homes, the remainder from home.
Medical information collected were age, sex, PaO2/FiO2, chest x-ray or CT, comorbidities [ischemic heart disease, chronic obstructive pulmonary disease (COPD), hypertension, diabetes, malignancies, neurodegenerative diseases], blood tests [hemoglobin, platelets count, neutrophils, lymphocytes, C-reactive protein (CRP), urea, and creatinine], and oxygen therapy (i.e., from nasal cannula to high flow cannula oxygen therapy to non-invasive ventilation). To assess the severity of COVID-19 pneumonia the SIAARTI criteria were followed, i.e., mild ARDS (acute respiratory distress syndrome): PaO2/FiO ratio 201–300; moderate ARDS: 101–200, and severe ARDS: ≤ 100 (10). The diagnosis of dementia was made on the basis of the data collected from clinical records, while the severity of dementia was assessed by CDR (11) and functional status by the Barthel Index (12). CDR was estimated based on information collected from family members and the records of patients. Delirium was detected through 4At (assessment test for delirium and cognitive impairment) (13).
Clinical criteria were used to characterize delirium subtypes: hypoactive or hyperactive. The presence of a disturbance of consciousness was retrospectively defined by altered arousal.
Hyperactive delirium with aggression and agitation was observed in eight patients, while the remaining six patients exhibited hypoactive delirium with lethargy and confusion.
Moreover, dementia was diagnosed in six out of 14 patients; among these, four developed hypokinetic delirium, while the remaining two developed hyperkinetic delirium. Patients without dementia were younger, with a mean age of 74.1 years (see Table 1).
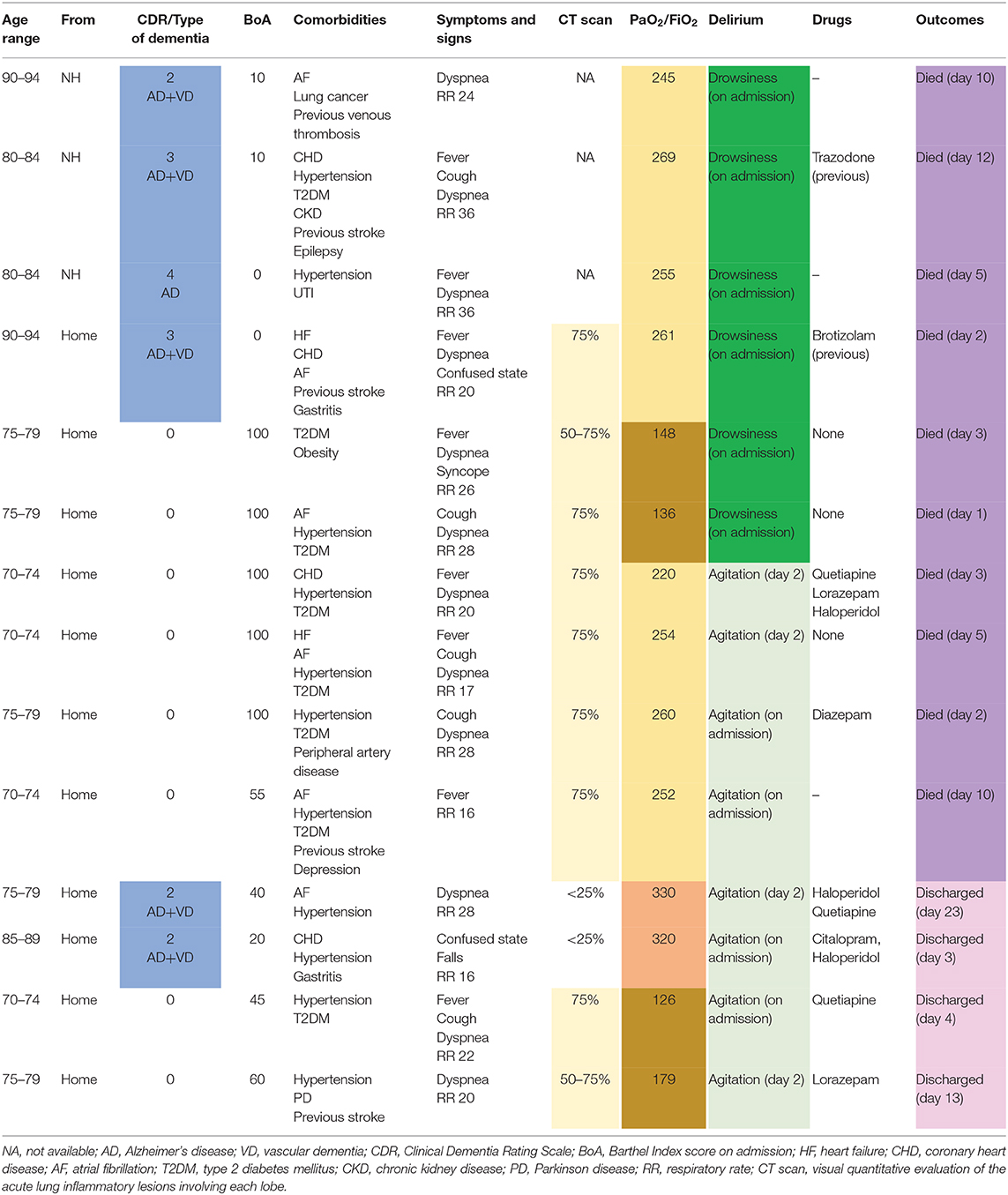
Table 1. Characteristics and outcomes of 14 older patients with confirmed diagnosis of COVID-19 and delirium.
The drugs used to treat patients with hyperkinetic delirium were: lorazepam (2 cases), diazepam (1 cases), quetiapine (3 cases), and haloperidol (3 cases). Two patients with hypokinetic prevalent delirium were treated before hospitalization with brotizolam (1 case) and trazodone (1 case).
Two of the patients were hospitalized for stage III pneumonia (PaO2/FiO2 ratio >300), eight patients were hospitalized for stage IV pneumonia-mild ARDS (200<PaO2/FiO2 <3008), and four patients were hospitalized with stage IV pneumonia-moderate ARDS (100<PaO2/FiO2 <200).
Upon admission, the patients presented the following symptoms: fever (7 cases), dyspnea (12 cases), cough (4 cases), fall and syncope (one case).
Almost all the patients (12/14) had a respiratory rate greater than 19.
The overall mortality rate was 71% (10/14 patients). All 6 of the patients exhibiting hypokinetic delirium and the 50% of patients (4/8) with hyperkinetic delirium died. Patients with hypokinetic delirium exhibited dementia and mild ARDS in four cases and no dementia and moderate ARDS in two cases.
Among the four survivors we observed two different clinical patterns: two patients exhibited dementia and no ARDS, while the remaining two patients exhibited ARDS and no dementia.
All patients living in a nursing home developed hypokinetic delirium and died.
A chest CT scan was taken for 11 of the patients: in two cases the lung involvement was less than 25%, in two cases it was from 50 to 75%, and in seven cases it was greater than 75%. The two cases with lower lung involvement survived; one patient with intermediate (50–75%) and one with greater involvement (>75%) also survived.
Each patient showed a high number of comorbidities: nine patients were affected by cardiovascular diseases (mainly coronary heart disease, atrial fibrillation, and heart failure), 12 by hypertension, and eight by diabetes. In particular, only four patients had no more than two comorbid conditions. In detail: survivors with hyperkinetic delirium had two or three comorbidities; deceased patients with hyperkinetic delirium had three or more comorbidities; deceased patients with hypokinetic delirium had two comorbidities in two cases and three or more in four cases.
With increasing frequency, delirium is reported as a symptom of the presentation of COVID-19 in older patients, although clinical aspects are rarely characterized (14). In a French series of elderly patients with COVID-19, delirium was present in 26.7% of patients, in two thirds of the cases in the hypokinetic form (15). In a series of hospitalized older patients with COVID-19 in the UK, delirium was observed in 25.2% of the sample (16). In older patients with dementia, delirium was a clinical manifestation of COVID-19 in 67% of cases, in 75% of these cases in the hypokinetic form (17). Mortality rates in these case series related to COVID-19 disease are still inconclusive and so comparison with other literature is uncertain.
In our patients with delirium, mortality was higher (71%) than previously reported for cases of hospitalized older people with delirium (ranging from 9 to 25%) (4). All subjects who developed hypokinetic delirium died. According to the literature, this form of delirium is associated with worse outcomes, particularly among patients affected by dementia (18). Multimorbidity is a condition associated with higher mortality, especially among patients who developed hypokinetic delirium: thus, hypokinetic delirium needs to be considered a marker of poor prognosis even in previously fit patients (3).
The onset of delirium is due to a complex interaction between the baseline vulnerability of the patient or predisposing factors and noxious insults or precipitating factors; recent observations lead us to believe that frailty and immunosenescence constitute factors that explain the excess mortality in elderly subjects with COVID-19 (19).
In our study, hyperkinetic delirium in cognitively unimpaired patients with mild ARDS had a better prognostic value than hypokinetic delirium in those with the same lung impairment. Hyperkinetic delirium in patients with dementia was observed in non-ARDS pneumonia (PaO2/FiO2 > 300). Patients with hyperkinetic delirium who died had a higher noxious insult (i.e., 200 < PaO2/FiO2 < 300) or dementia, and high level of comorbidities.
The high mortality rate of subjects developing delirium as an onset symptom of COVID-19, particularly in its hypokinetic form, could suggest brain involvement rather than the worsening effect of a pre-existing condition of frailty. Taking cognizance of the emergency due to the outbreak of COVID-19 and the consequent necessity of brief and easy-to-use tools and the involvement of non-expert doctors and nurses in COVID wards, to diagnose delirium we decided to use the 4AT test, a reliable tool designed for delirium detection in clinical practice (13).
Based on our observations, we hypothesize that delirium subtypes may be markers of biological severity of precipitating disease in COVID-19 patients. Specifically, patients suffering from a higher involvement of brain function and thus manifesting hypokinetic delirium, have a worse prognosis, while those who develop hyperkinetic delirium with a lower degree of dysregulation induced by the disease have a better chance of survival. Data on the ARDS stage confirm this interpretation since deceased patients with hypokinetic delirium and dementia were the most biologically compromised (with the most severe form of ARDS).
These different clinical patterns (hypokinetic delirium; hyperkinetic delirium with or without dementia; hyperkinetic delirium with or without ARDS) identify patients with different prognosis. Although the data were collected in a relatively limited number of cases, these observations may have an impact on the management of older subjects with delirium due to COVID-19.
In conclusion, our study indicates that delirium, particularly in the hypokinetic form, is related to a high risk of mortality in patients with COVID-19, especially in the presence of dementia. Therefore, a systematic recognition of this syndrome in COVID-19 patients is crucial for establishing a reliable prognosis.
All datasets presented in this study are included in the article/Supplementary Material.
The studies involving human participants were reviewed and approved by Comitato Etico di Brescia. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
RR, FM, and GC contribute to evaluation of cases, data management and discussion. AB, LB, and MT reviewed and discussed the manuscript. AB and RR wrote the first draft. All authors carefully reviewed, discussed and contributed to various draft of the manuscript. All authors approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Leonardi M, Padovani A, McArthur JC. Neurological manifestations associated with COVID-19: a review and a call for action. J Neurol. (2020) 267:1573–6. doi: 10.1007/s00415-020-09896-z
2. Persico I, Cesari M, Morandi A, Haas J, Mazzola P, Zambon A, et al. Frailty and delirium in older adults: a systematic review and meta-analysis of the literature. J Am Geriatr Soc. (2018) 66:2022–30. doi: 10.1111/jgs.15503
3. Bellelli G, Morandi A, Di Santo SG, Mazzone A, Cherubini A, Mossello E, et al. “Delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. (2016) 14:106. doi: 10.1186/s12916-016-0649-8
4. Morandi A, Di Santo SG, Zambon A, Mazzone A, Cherubini A, Mossello E, et al. Delirium, dementia, and in-hospital mortality: the results from the italian delirium day 2016, A National Multicenter Study. J Gerontol Ser A Biol Sci Med Sci. (2019) 74:910–6. doi: 10.1093/gerona/gly154
5. Tay HS, Harwood R. Atypical presentation of COVID-19 in a frail older person. Age Ageing. (2020) 49:523–4. doi: 10.1093/ageing/afaa068
6. Alkeridy WA, Almaghlouth I, Alrashed R, Alayed K, Binkhamis K, Alsharidi A, et al. A Unique presentation of delirium in a patient with otherwise asymptomatic COVID-19. J Am Geriatr Soc. (2020) 68:1382–4. doi: 10.1111/jgs.16536
7. Kotfis K, Williams Roberson S, Wilson JE, Dabrowski W, Pun BT, Ely EW. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit Care. (2020) 24:176. doi: 10.1186/s13054-020-02882-x
8. Marengoni A, Zucchelli A, Grande G, Fratiglioni L, Rizzuto D. The impact of delirium on outcomes for older adults hospitalised with COVID-19. Age Ageing. (2020) 49:923–6. doi: 10.1093/ageing/afaa189
9. Rozzini R, Bianchetti A. COVID Towers: low- and medium-intensity care for patients not in the ICU. CMAJ. (2020) 192:E463–4. doi: 10.1503/cmaj.75334
10. SIAARTI. Percorso Assistenziale per il Paziente Affetto da COVID-19. Sezione 1 - Procedure area critica - versione 02 (2020).
11. Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. (1982) 140:566–72.
13. Bellelli G, Morandi A, Davis DH, Mazzola P, Turco R, Gentile S, et al. Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing. (2014) 43:496–502. doi: 10.1093/ageing/afu021
14. Bianchetti A, Rozzini R, Guerini F, Boffelli S, Ranieri P, Minelli G, et al. Clinical presentation of COVID19 in dementia patients. J Nutr. Health Aging. (2020) 24:560–2. doi: 10.1007/s12603-020-1389-1
15. Annweiler C, Sacco G, Salles N, Aquino JP, Gautier J, Berrut G, et al. National French survey of COVID-19 symptoms in people aged 70 and over. Clin Infect Dis. (2020) ciaa792. doi: 10.1093/cid/ciaa792
16. Zazzara MB, Penfold RS, Roberts AL, Lee K, Dooley H, Sudre CH, et al. Delirium is a presenting symptom of COVID-19 in frail, older adults: a cohort study of 322 hospitalised and 535 community-based older adults. medRxiv. (2020) 2020.06.15.20131722. doi: 10.1101/2020.06.15.20131722
17. Bianchetti A, Bellelli G, Guerini F, Marengoni A, Padovani A, Rozzini R, et al. Improving the care of older patients during the COVID-19 pandemic. Aging Clin Exp Res. (2020) 32:1883–8. doi: 10.1007/s40520-020-01641-w
18. Rosgen BK, Krewulak KD, Stelfox HT, Ely EW, Davidson JE, Fiest KM. The association of delirium severity with patient and health system outcomes in hospitalised patients: a systematic review. Age Ageing. (2020) 49:549–57. doi: 10.1093/ageing/afaa053
Keywords: COVID 19, delirium, elderly, frailty, mortality
Citation: Rozzini R, Bianchetti A, Mazzeo F, Cesaroni G, Bianchetti L and Trabucchi M (2020) Delirium: Clinical Presentation and Outcomes in Older COVID-19 Patients. Front. Psychiatry 11:586686. doi: 10.3389/fpsyt.2020.586686
Received: 23 July 2020; Accepted: 22 September 2020;
Published: 12 November 2020.
Edited by:
Gianfranco Spalletta, Santa Lucia Foundation (IRCCS), ItalyReviewed by:
Elizabeta Blagoja Mukaetova-Ladinska, University of Leicester, United KingdomCopyright © 2020 Rozzini, Bianchetti, Mazzeo, Cesaroni, Bianchetti and Trabucchi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renzo Rozzini, cmVuem8ucm96emluaUBwb2xpYW1idWxhbnphLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.