- 1National Clinical Research Center for Mental Disorders, and Department of Psychiatry, China National Technology Institute on Mental Disorders, Hunan Key Laboratory of Psychiatry and Mental Health, Institute of Mental Health and Hunan Medical Center for Mental Health, The Second Xiangya Hospital of Central South University, Changsha, China
- 2College of Life Sciences and Chemistry, Hunan University of Technology, Zhuzhou, China
- 3Department of Medicine Addiction, Xinjiang Mental Health Center and Urumqi Fourth People’s Hospital, Urumqi, China
- 4Department of Psychiatry, Brains Hospital of Hunan Province, Changsha, China
- 5CAS Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, China
Background: The quality of life (QOL) of patients with methamphetamine use disorder (MAUD) is increasingly recognized as an important outcome. Previous studies have found that impulsivity is negatively associated with QOL in mental disorders, but this relationship is rarely confirmed in patients with MAUD. We hypothesized that impulsivity is negatively correlated with QOL in patients with MAUD based on previous findings. In addition, a variety of drug use characteristics of patients that may potentially affect their QOL need to be further explored. Therefore, the purpose of this study was to explore the relationship between impulsivity, multiple drug use characteristics, and QOL in patients with MAUD.
Methods: A total of 379 patients with MAUD were recruited, and the majority of them were male (85.5%), with an average age of 33.93 ± 7.08 years. Two psychiatrists conducted semi-structured interviews with methamphetamine (MA) users in two compulsory drug rehabilitation centers to obtain their demographics and drug use characteristics. The Barratt Impulsiveness Scale-11 (BIS-11) and Brief WHO Quality of Life Assessment (WHOQOL-BREF) were used to assess patients’ impulsivity and QOL, respectively. Correlation and univariate regression analysis were used to explore the relationships between impulsivity, a series of drug use characteristics and patients’ QOL in different domains. Further multiple linear regression analysis was used to identify what extent the above clinical variables explained the variations in patients’ QOL.
Results: Age, marital status, employment, and various drug use characteristics were significantly associated with at least one QOL domain. Among them, married and full-time job were positively correlated with QOL, while others were negatively correlated with QOL. The total score of BIS-11 was significantly negatively correlated with all four domains of QOL. Impulsivity, a range of drug use characteristics and certain demographic characteristics collectively explained varying degrees of variation in different domains of QOL.
Conclusions: Impulsivity and various drug use characteristics can significantly predict QOL in all fields of MAUD patients. In addition, we have also found differences in the predictors of QOL in different domains. Overall, this study provides clinical guidance for the treatment of MAUD patients, that is, management of impulsivity in patients with MAUD may help improve their QOL and even sustain their drug rehabilitation.
Introduction
Quality of life (QOL) refers to individuals’ subjective perception of their own life status, which involves the domains of physical health, psychological state, social relations and living conditions (1). In the past decade, QOL has been paid more and more attention by psychiatrists because of its importance for outcomes of patients with mental illness (2–4), especially for schizophrenia (5, 6), major depression (7, 8) and bipolar disorder (9, 10). In fact, QOL is not one of the traditional or formal measures of outcomes. Therefore, in contrast to these common psychiatric diseases, a more insidious condition named substance use disorders (SUDs), has received relatively little attention in terms of QOL from both clinicians and researchers (11). Despite the limited number of studies, it does not prevent evidence that QOL has increasingly become a determinant of the outcomes of patients with SUDs (12, 13). More specifically, it has been shown that improved QOL can effectively reduce the use of drugs during treatment seeking (14, 15). In addition, a high QOL contributes to the sustainable withdrawal of patients with SUDs after leaving treatment (16, 17). However, patients with SUDs often reported more impaired QOL than those without SUDs (18, 19), or even poorer than some other chronic disease (20, 21), which may greatly hinder their rehabilitation. Consequently, it is urgent for clinicians to understand the factors leading to the poor QOL in patients with SUDs, so as to improve it in a cost-effective manner.
Previous studies have consistently concluded that impulsivity was significantly associated with QOL, especially in a group of mental disorders characterized by impulsivity, such as bipolar disorder (9, 22), attention deficit hyperactivity disorder (23, 24) and emotional eating (25, 26). In fact, although impulsivity has been shown to be a non-core symptom, in popular diagnostic systems (such as DSM-5 and ICD-11), certain impulsive behaviors can still be used to diagnose SUDs, such as uncontrolled drug seeking (27, 28). Therefore, we hypothesized that the high impulsivity of patients with SUDs may have an impact on their QOL. Unfortunately, there are few studies on the relationship between impulsivity and QOL in patients with SUDs. Although rare, fortunately, we have drawn from this small number of studies that in the SUDs population, patients with higher impulsivity have worse QOL than those with lower impulsivity (29, 30). Furthermore, impulsivity may be a predictor of QOL in patients with SUDs. More specifically, high impulsivity is associated with lower QOL (31, 32). However, there are some shortcomings in the existing studies. On the one hand, they rarely pay attention to the relationships between impulsivity and QOL, and on the other hand, they did not determine whether there is a different relationships between the various domains of QOL (i.e., QOL is basically divided into four domains, namely physical, psychological, social, and environmental, see Method Section). In view of this, our research will focus on solving all these problems ignored by previous studies.
In addition to impulsivity, there are other factors that were consistently associated with the QOL of patients with SUDs, of which the most commonly studied were the characteristics related to drug use, including the frequency of drug use (33, 34), the severity of SUDs (35, 36), comorbidities with mental disorders (37, 38) and polysubstance use (39). In fact, in addition to the above-mentioned drug use characteristics, there are also the age of onset of SUDs, the number of relapse and comorbidities with other SUDs, which seem to have been overlooked in previous studies. Overall, the main purpose of this study was to identify the degree to which impulsivity and some previously less discussed drug use characteristics explain the variations in QOL, especially to clarify the relationships between these clinical variables and QOL in different domains. It is worth emphasizing that most previous studies have used the Addiction Severity Index (ASI) to assess the severity of SUDs (35, 36), which may produce some bias due to the self-reported data. In order to modify this, we obtained the severity of SUDs through the semi-structured interviews in this study, according to the diagnostic criteria of SUDs in DSM-5. In addition, the patients we recruited were recent users of methamphetamine (MA), as MA has increasingly become an illegal drug of abuse worldwide, especially in Asia (40). Currently, methamphetamine use disorder (MAUD) has become an global public health issue (41). Therefore, improving the QOL of MAUD patients is critical to prevent an outbreak.
Method
Participants and Procedures
A total of 379 MA users participated in this study, including of 324 men (85.5%) and 55 women (14.5%), aged from 20 to 54 years old (M =33.93 ± 7.08). They were recruited from two compulsory drug rehabilitation centers in Changsha, Hunan Province. From March to September 2018, two psychiatrists who validated the raters’ consistency conducted semi-structured interviews with MA users who entered drug rehabilitation centers. The inclusion criteria for this study were 1) the core drug used in the last three years was MA; 2) diagnosed as a stimulant use disorder (that is, meeting at least 2 criteria in DSM-5); 3) at least two weeks of detoxification at the time of enrollment. The exclusion criteria were 1) lifetime/current diagnosis of mental illness or personality disorder; 2) alcohol use disorder; 3) intellectual disability or cognitive impairment; 4) presence of any other serious diseases.
This study was approved by the Ethics Committee of The Second Xiangya Hospital of Central South University. The subjects understood the purpose and procedure of the study and signed an informed consent for. They could quit unconditionally and all information was confidential.
Measures
Demographics and Drug Use Characteristics
To ensure data quality, we administrated a semi-structured interview to collect demographics and drug use characteristics of the patients as follows: 1) demographic data included gender, age, education, marital status (whether married), whether they had children, who they lived with (family member or non-family member), employment (full-time or part-time job, unemployment); 2) drug use characteristics included the age of onset of MAUD, the number of relapse (i.e., reused drugs after at least three months of absolute withdrawal), comorbidities with other SUDs [i.e., the patients in this study were classified as simple MAUD, having comorbidities with opioid use disorder (OUD) and comorbid ketamine use disorder (KUD), depending on their diagnosis] and the severity of MAUD (i.e., patients who met six or more criteria were diagnosed as severe MAUD, and those with less than 6 criteria were diagnosed as mild to moderate according to the DSM-5).
Impulsivity
We used the Chinese version of Barratt Impulsiveness Scale-11 (BIS-11) to assess three aspects of impulsivity (42), namely no-planning impulsivity (i.e., the tendency to live an irregular life), motor impulsivity (i.e., act without considering the consequences) and cognitive impulsivity (i.e., defects in thought or difficulty in solving problems). BIS-11 is a self-reported scale of 30 items and is rated on a 5-point Likert scale, ranging from 1 “never” to 5 “always” (43). For the purpose of the current study, the total score was calculated, and a higher score indicates a higher level of trait impulsivity, which was validated in patients with MAUD in our previous studies (44, 45). In this study, the Cronbach’s α of the total scale was 0.909.
Quality of Life
The brief WHO Quality of Life Assessment (WHOQOL-BREF) was used to assess patients’ QOL (1). It has been validated in patients with SUDs (14, 46). WHOQOL-BREF is a self-reported scale composed of 26 items, in which item 3 to 26 constitutes the individual’s four domains of QOL, namely physical QOL (PHYSQOL, seven items), psychological QOL (PSYCHQOL, six items), social QOL (SOCIALQOL, three items) and environmental QOL (ENVIRQOL, eight items). These items are scored with a Likert-5 point scale and all items are positively scored except for item 3, 4, and 26. The sum of each subscale was calculated, and the higher score indicates the higher QOL in corresponding filed. In addition, item 1 and 2 independently assess a person’s overall QOL and physical condition. Since we aimed to examine how clinical variables affect different aspects of QOL, we did not analyze these two overall items. The Cronbach’s α of the four subscales ranged from 0.615 to 0.808 in this study.
Statistical Analysis
Descriptive statistics were used to describe demographic and drug use characteristics. Pearson correlation and univariate regression analysis were used to initially identify the relationship between impulsivity, drug use characteristics and QOL. Multiple linear regression analysis was used to further examine the association of the aforementioned clinical variables. Considering the differences in the four aspects of QOL, we executed four regression models with PHYSQOL, PSYHQOL, SOCIALQOL, and ENVIRQOL as dependent variables, and those measures with p <0.1 in the previous univariate regression analysis together with gender and age as independent variables. All analysis was performed using SPSS software (version 23.0) with a bilateral significance level <0.05.
Results
Description of Demographics and Clinical Variables
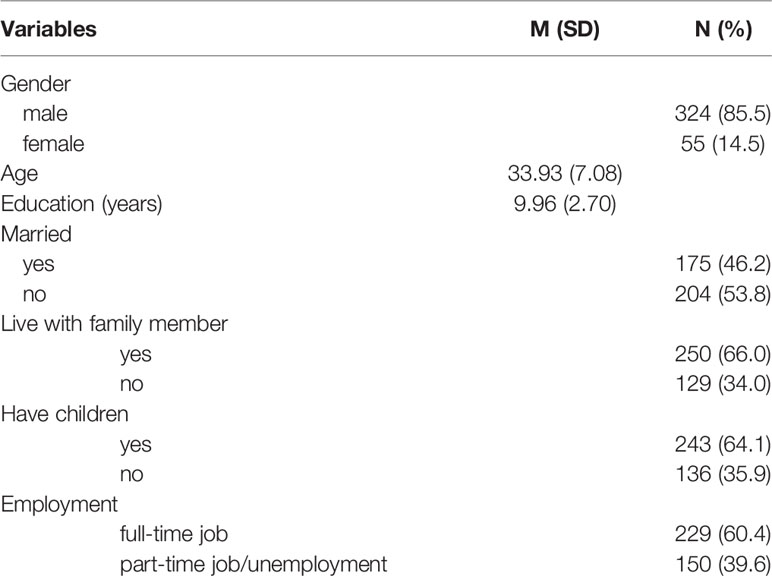
Demographic data is shown in Table 1. The majority (85.5%) of MAUD patients were male. Their average age and years of education were 33.93 (7.08) and 9.96 (2.70) respectively. Regarding their marital status, 175 (46.2%) were married, while others (53.8%) were not. When asked who they usually lived with, 250 (66.0%) reported their family members. In addition, 243 (64.1%) had at least one child. In regard to their employment, 229 (60.4%) had a full-time job, while others were part-time or unemployed.
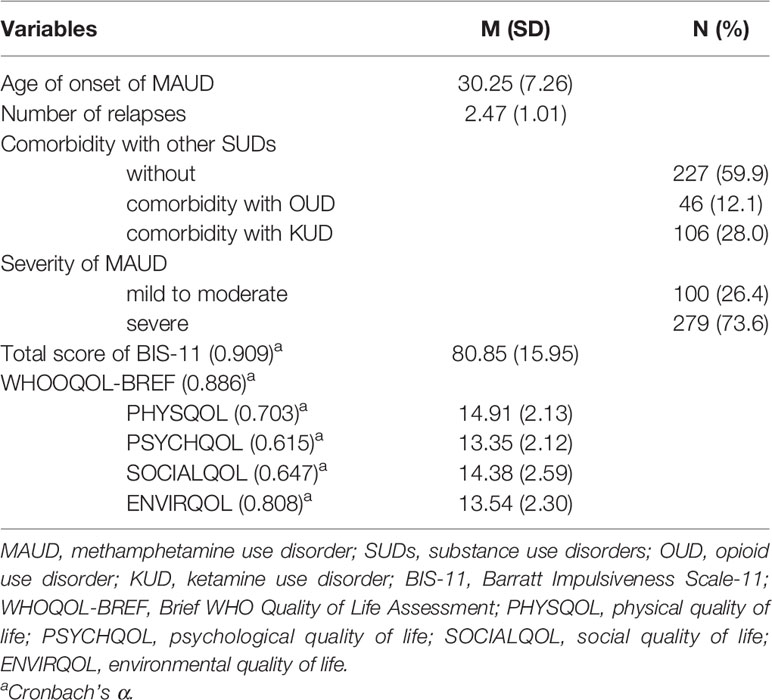
Table 2 shows the drug use characteristics and scores of BIS-11 and WHOQOL-BREF. First, patients reported that their age of onset of MAUD was 30.25 (7.26), with an average of relapse for 2.47 (1.01) times since the onset of MAUD. Regarding comorbidities with other SUDs, 227 cases (59.9%) were diagnosed without comorbidities (that is, simple MAUD), while 46 cases (12.1%) were diagnosed as comorbidities with OUD, and the remaining 106 cases (28.0%) were diagnosed with comorbidities with KUD. In terms of the severity of MAUD, the majority (73.9%) met more than six diagnostic criteria of DSM-5 and they were therefore diagnosed as severe. Then, as we can see in Table 2, the total score of BIS-11 was between 36 and 126, with an average score of 80.85 (15.95). Meanwhile, the sum of four domains of QOL was 14.91 (SD = 2.13, PHYSQOL), 13.35 (SD = 2.12, PSYCHQOL), 14.38 (SD = 2.59, SOCIALQOL), and 13.54 (SD = 2.30, ENVIRQOL), respectively.
Correlations of Drug Use Characteristics, Impulsivity With QOL
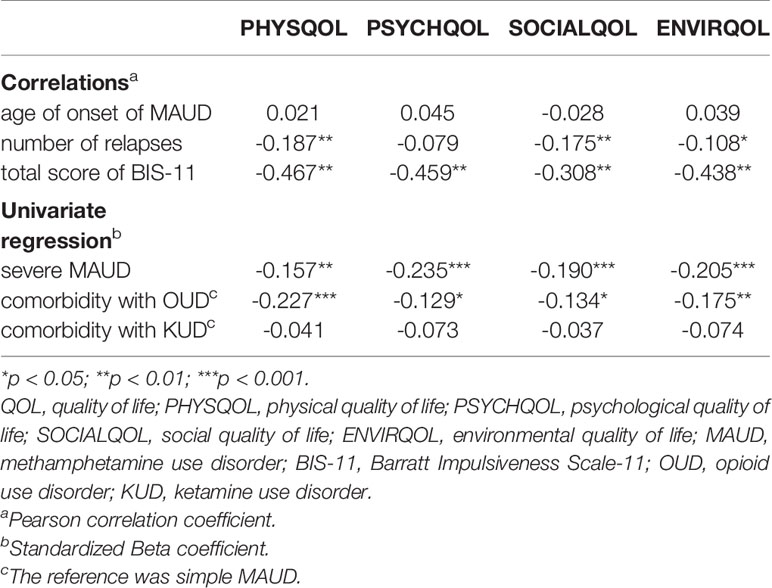
We conducted correlation and univariate regression analysis to initially explore the relationship between multiple clinical variables and QOL. First, Pearson’s correlation results are shown in Table 3. We found that the total score of BIS-11 was negatively correlated with QOL in all four domains, with a correlation coefficient ranging from 0.308 (SOCIALQOL, p < 0.01) to 0.467 (PHYSQOL, p < 0.01). Except for PSYCHQOL, the number of relapses was negatively associated with QOL in other three domains, with correlation coefficients of 0.187 (PHYSQOL, p < 0.01), 0.175 (SOCIALQOL, p < 0.01), and 0.108 (ENVIRQOL, p < 0.05), respectively.
Table 3 also presented the results of univariate regression. We firstly found that severe MAUD was negatively associated with QOL in all four domains, which had the highest correlation with PSYCHQOL (r = -0.235, p < 0.001), and the lowest correlation with PHYSQOL (r = -0.190, p < 0.001). In addition, compared with the simple MAUD, patients comorbid with OUD had significantly lower QOL in all four domains, especially PHYSQOL (β = -0.227, p < 0.001).
Multiple Linear Regression of Drug Use Characteristics, Impulsivity, and QOL
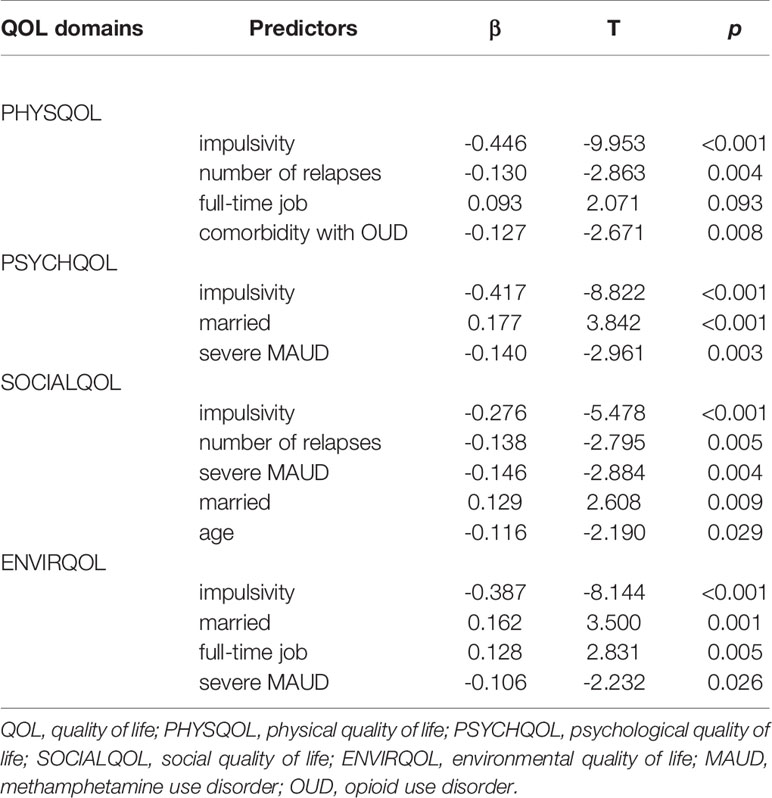
We performed four separate multiple regression models by using Stepwise and Enter methods. First, PHYSQOL was set as the dependent variable, and then gender, age, education, marital status, who lived with, employment, comorbidity with OUD or KUD, number of relapses, severity of MAUD, and impulsivity were set as independent variables. As shown in Table 4, impulsivity (β = -0.446, p < 0.001), number of relapse (β = -0.130, p = 0.004), full-time job (β = 0.093, p = 0.039) and comorbidity with OUD (β = -0.127, p = 0.008) explained 28.1% of the variation in PHYSQOL (F = 24.266, p < 0.001, adjusted R2 = 0.270).
Second, we designated PSYCHQOL as dependent variable, and gender, age, marital status, whether or not have children, employment, comorbidity with OUD or KUD, severity of MA and impulsivity as independent variables. The results showed that 26.4% (F = 22.184, p < 0.001, adjusted R2 = 0.252) of the variation in PSYCHQOL were explained by impulsivity (β = -0.417, p < 0.001), married (β = 0.177, p < 0.001) and severe MAUD (β = -0.140, p = 0.003).
In the next analysis, SOCIALQOL was set as a dependent variable, and gender, age, marital status, having children, who lived with, number of relapses, comorbidity with OUD or KUD, severity of MAUD and impulsivity were included in the regression model. We found that impulsivity (β = -0.276, p < 0.001), number of relapse (β = -0.138, p = 0.005), severe MAUD (β = -0.146, p = 0.004), married (β = 0.129, p = 0.009) and age (β = -0.116, p = 0.029) accounted for 16.3% of the variation in SOCIALQOL (F = 10.344, p < 0.001, adjusted R2 = 0.148).
Finally, ENVIRQOL was set as a dependent variable, while gender, age, marital status, having children, who lived with, employment, number of relapses, comorbidity with or KUD, severity of MAUD, and impulsivity were independent variables. The results showed that 26.2% of variation in ENVIRQOL (F = 18.790, p < 0.001, adjusted R2 = 0.248) was explained by impulsivity (β = -0.387, p < 0.001), married (β = 0.162, p = 0.001), full-time job (β = 0.128, p = 0.005) and severe MAUD (β = -0.106, p = 0.026).
It is worth mentioning that we conducted the Bonferroni test, which tested the deviation caused by multiple comparisons, and the results were still significant.
Discussion
To the best of our knowledge, this is the first study to explore the relationship between impulsivity, drug use characteristics and QOL in the MAUD population. The main findings were as follows. First, certain demographic and a range of drug use characteristics, more specifically, age, marital status, employment, number of relapses, comorbidity with OUD as well as the severity of MAUD were correlated with different QOL. Second, impulsivity was negatively associated with QOL in all four domains among patients with MAUD. Finally, impulsivity, drug use characteristics and some demographics collectively explained the varying degrees of variation in the four domains of QOL.
Regarding demographics, age, married, and having a full-time job can predict one or more QOL domains. Specifically, married positively predicted three domains (ENVIRQOL, SOCIALQOL, and PSYCHQOL), while having a full-time job positively predicted PHYSQOL and ENVIRQOL. These were partially consistent with previous studies in patients with SUDs (39, 47, 48) and other mental disorders (49), indicating that stable social support is more constructive for positive perception of ENVIRQOL. In addition, age was negatively associated with SOCIALQOL which was consistent with one study in patients with depression (50). One of the possible reasons is that SOCIALQOL is involved in the sexual well-being of patients, which is generally reported as unsatisfactory in the elderly (51, 52). In terms of drug use characteristics, number of relapses, severe MAUD, and comorbidity with OUD negatively predicted at least one domain of QOL. First, more relapses predicted poorer PHYSQOL and SOCIALQOL, which was consistent with the findings of some recurrent diseases such as acne (53), depression (54) and SUDs (55). Our findings suggested that relapse was an important risk factor for QOL of SUDs patients, especially in their physical and social domains. Therefore, when treating patients with a higher relapse frequency, special attention should be paid to the recovery of their physical and social functions. Second, compared with simple MAUD, patients comorbid with OUD had significantly lower PHYSQOL. This indirectly supports previous studies that opioid abusers had a particularly poor physical QOL (56–58), even lower than other SUDs (59). In fact, previous studies have also found that comorbidities with alcohol use disorders are a risk factor for QOL (60). Collectively, clinicians should pay special attention to patients with multiple SUDs because their potentially low quality of life may affect the outcomes. Finally, most QOL domains in patients with severe MAUD were worse than those patients with mild to moderate MAUD, confirming the results of previous studies that severity is a stable predictor of poor QOL no matter what assessments was used (35, 61).
In addition to the above results, there were more important findings supporting the previous conclusion that impulsivity was closely related to QOL in patients with impulse-related disorders (10, 22–24, 62), including patients with SUDs in this study. Specifically, impulsivity was significantly negatively correlated with different domains of QOL in patients with MAUD, and even after controlling for demographics and multiple drug use characteristics, impulsivity can still predict each different domain of QOL. This was consistent with our previous hypothesis that impulsivity was a powerful predictor of QOL in patients with SUDs (32, 63), while in the current study, MAUD patients (31, 64). In other words, patients with higher impulsivity have lower QOL. More interestingly, we found that although impulsivity was associated with QOL in all domains, the degree was different. The results of correlation and multiple linear regression showed that impulsivity was most closely related to PHYSQOL and least related to SOCIALQOL. This completely replicated the results of patients with bipolar disorder (22), suggesting that impulsivity was even a stable predictor of cross-domain QOL. Furthermore, impulsivity was the strongest predictor of PHYSQOL which refers to the patients’ physical pain, fatigue, sleep, mobility, daily life, dependence on medical treatment, and ability to work (65). Previous studies have found that patients with SUDs tend to report physical discomfort, such as pain (66, 67) and poor quality of sleep (68, 69), which may interfere with their treatment. Our findings may provide advice to clinicians that reducing impulsivity may improve their perception of PHYSQOL, thereby promoting treatment.
However, this study was not without limitations. First, all patients were recruited from compulsory drug rehabilitation centers, excluding those from voluntary drug rehabilitation centers. In fact, there were some differences in a variety of clinical variables between the two groups, which may lead different results. Second, there were fewer female patients in our sample, resulting an imbalanced sex ratio. Therefore, we did not perform a gender difference analysis when exploring these relationships. We will continue to supply female samples to achieve a balanced sex ratio and explore potential gender differences in our findings. In addition, this study was cross-sectional, and we cannot determine whether impulsivity is a longitudinal predictor of QOL in patients with MAUD. Therefore, additional research is needed to examine whether controlling impulsivity will improve the QOL of patients.
Despite these limitations, this study still has obvious advantages. We have identified that impulsivity can significantly predict all domains of QOL in patients with MAUD, even after controlling for other clinical variables. Our results, combined with previous studies, confirm that higher impulsivity is harmful to QOL of patients with impulsivity-related symptoms. In addition, we have also found that there are some differences between the predictors of different QOL domains. For example, comorbidity with OUD can only predict PHYSQOL. It is worth mentioning that, as the most populous country worldwide, our results are worthy of reference for other regions, especially those with large numbers of drug abusers. Overall, this study provides clinical guideline for treatments, that is, regulating impulsivity in patients with SUDs may help improve their QOL, and even maintain their drug rehabilitation.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: The database can be obtained from the corresponding authors with any reasonable reasons. Requests to access these datasets should be directed to TL, bGl1dGllcWlhbzEyM0Bjc3UuZWR1LmNu.
Ethics Statement
This study was approved by the Ethics Committee of The Second Xiangya Hospital of Central South University. The subjects understood the purpose and procedure of the study and signed an informed consent.
Author Contributions
TL and WH designed the study. HS and XJZ supervised the whole process. QD designed the structure of the interviews and measures. YW, MQL, ZZ and LZ performed the semi-structure interviews and data collection. YZ and MYL participated in data collation. JZ computed statistical analyses and interpreted the results. YW managed the literature search and wrote the manuscript. XYZ designed the framework of the manuscript and revised it. All authors contributed to the article and approved the submitted version.
Funding
The National Key R&D Program of China (2017YFC1310400), the National Natural Science Foundation of China (81371465 and 81671324) and the provincial Natural Science Foundation of Hunan (2020JJ4795) supported this study. The sponsors had no role in the study design, survey process, data analysis, and manuscript preparation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We sincerely thank all the staff in The Compulsory Drug Rehabilitation Center of Public Security Bureau in Changsha, special thanks to Director Xin Shen, Instructor Li Lu and Director Wei Liu for their supports. We would also like to thank all those who participated in the study.
References
1. Group TW. The Development of the World Health Organization Quality of Life Assessment Instrument (the WHOQOL). In: Orley J, Kuyken W, editors. Quality of Life Assessment: International Perspectives. Berlin, Heidelberg: Springer (1994).
2. Berghofer A, Martin L, Hense S, Weinmann S, Roll S. Quality of life in patients with severe mental illness: a cross-sectional survey in an integrated outpatient health care model. Qual Life Res (2020) 29:2073–87. doi: 10.1007/s11136-020-02470-0
3. Picardi A, Rucci P, de Girolamo G, Santone G, Borsetti G, Morosini P. The quality of life of the mentally ill living in residential facilities: findings from a national survey in Italy. Eur Arch Psychiatry Clin Neurosci (2006) 256(6):372–81. doi: 10.1007/s00406-006-0647-5
4. Choo CC, Chew PKH, Ho CS, Ho RC. Quality of Life in Patients With a Major Mental Disorder in Singapore. Front Psychiatry (2018) 9:727. doi: 10.3389/fpsyt.2018.00727
5. Dong M, Lu L, Zhang L, Zhang Y-S, Ng CH, Ungvari GS, et al. Quality of Life in Schizophrenia: A Meta-Analysis of Comparative Studies. Psychiatr Q (2019) 90:519–32. doi: 10.1007/s11126-019-09633-4
6. Xiang Y-T, Weng Y-Z, Leung C-M, Tang W-K, Ungvari GS. Quality of life of Chinese schizophrenia outpatients in Hong Kong: relationship to sociodemographic factors and symptomatology. Aust New Z J Psychiatry (2007) 41(5):442–9. doi: 10.1080/00048670701261228
7. Lex H, Ginsburg Y, Sitzmann AF, Grayhack C, Maixner DF, Mickey BJ. Quality of life across domains among individuals with treatment-resistant depression. J Affect Disord (2019) 243:401–7. doi: 10.1016/j.jad.2018.09.062
8. Guan B, Deng Y, Cohen P, Chen H. Relative impact of Axis I mental disorders on quality of life among adults in the community. J Affect Disord (2011) 131(1–3):293–8. doi: 10.1016/j.jad.2011.01.010
9. Lee D, Cha B, Park CS, Kim BJ, Lee CS, Lee SJ, et al. Effects of resilience on quality of life in patients with bipolar disorder. J Affect Disord (2017) 207:434–41. doi: 10.1016/j.jad.2016.08.075
10. Sylvia LG, Montana RE, Deckersbach T, Thase ME, Tohen M, Reilly-Harrington N, et al. Poor quality of life and functioning in bipolar disorder. Int J Bipolar Disord (2017) 5(1):10. doi: 10.1186/s40345-017-0078-4
11. Laudet AB. The Case for Considering Quality of Life in Addiction Research and Clinical Practice. Addict Sci Clin Pract (2010) 6(1):44–55.
12. Tiffany ST, Friedman L, Greenfield SF, Hasin DS, Jackson R. Beyond drug use: a systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction (2012) 107(4):709–18. doi: 10.1111/j.1360-0443.2011.03581.x
13. Srivastava S, Bhatia MS. Quality of life as an outcome measure in the treatment of alcohol dependence. Ind Psychiatry J (2013) 22(1):41–6. doi: 10.4103/0972-6748.123617
14. Manning V, Garfield JBB, Lam T, Allsop S, Berends L, Best D, et al. Improved Quality of Life Following Addiction Treatment Is Associated with Reductions in Substance Use. J Clin Med (2019) 8(9):1407. doi: 10.3390/jcm8091407
15. Feelemyer JP, Jarlais DCD, Arasteh K, Phillips BW, Hagan H. Changes in quality of life (WHOQOL-BREF) and addiction severity index (ASI) among participants in opioid substitution treatment (OST) in low and middle income countries: an international systematic review. Drug Alcohol Depend (2014) 134:251–8. doi: 10.1016/j.drugalcdep.2013.10.011
16. Best D, Savic M, Beckwith M, Honor S, Karpusheff J, Lubman DI. The role of abstinence and activity in the quality of life of drug users engaged in treatment. J Subst Abuse Treat (2013) 45(3):273–9. doi: 10.1016/j.jsat.2013.02.010
17. Laudet AB, Stanick V. Predictors of motivation for abstinence at the end of outpatient substance abuse treatment. J Subst Abuse Treat (2010) 38(4):317–27. doi: 10.1016/j.jsat.2010.01.007
18. Pasareanu AR, Opsal A, Vederhus JK, Kristensen O, Clausen T. Quality of life improved following in-patient substance use disorder treatment. Health Qual Life Outcomes (2015) 13:35. doi: 10.1186/s12955-015-0231-7
19. Tracy EM, Laudet AB, Min MO, Kim H, Brown S, Jun MK, et al. Prospective patterns and correlates of quality of life among women in substance abuse treatment. Drug Alcohol Depend (2012) 124(3):242–9. doi: 10.1016/j.drugalcdep.2012.01.010
20. Vederhus JK, Pripp AH, Clausen T. Quality of Life in Patients with Substance Use Disorders Admitted to Detoxification Compared with Those Admitted to Hospitals for Medical Disorders: Follow-Up Results. Subst Abuse (2016) 10:31–7. doi: 10.4137/SART.S39192
21. McKetin R, Voce A, Burns R, Shanahan M. Health-related quality of life among people who use methamphetamine. Drug Alcohol Rev (2019) 38(5):503–9. doi: 10.1111/dar.12934
22. Kim YS, Cha B, Lee D, Kim SM, Moon E, Park CS, et al. The Relationship between Impulsivity and Quality of Life in Euthymic Patients with Bipolar Disorder. Psychiatry Invest (2013) 10(3):246–52. doi: 10.4306/pi.2013.10.3.246
23. Quintero J, Morales I, Vera R, Zuluaga P, Fernandez A. The Impact of Adult ADHD in the Quality of Life Profile. J Atten Disord (2019) 23(9):1007–16. doi: 10.1177/1087054717733046
24. Gjervan B, Torgersen T, Rasmussen K, Nordahl HM. ADHD symptoms are differentially related to specific aspects of quality of life. J Atten Disord (2014) 18(7):598–606. doi: 10.1177/1087054712445183
25. Rose MH, Nadler EP, Mackey ER. Impulse Control in Negative Mood States, Emotional Eating, and Food Addiction are Associated with Lower Quality of Life in Adolescents with Severe Obesity. J Pediatr Psychol (2018) 43(4):443–51. doi: 10.1093/jpepsy/jsx127
26. Ferre F, Cambra J, Ovejero M, Basurte-Villamor I. Influence of attention deficit hyperactivity disorder symptoms on quality of life and functionality in adults with eating disorders. Actas Esp Psiquiatr (2017) 45(3):98–107.
27. Lopez AJ, Siciliano CA, Calipari ES. Activity-Dependent Epigenetic Remodeling in Cocaine Use Disorder. Handb Exp Pharmacol (2020) 258:231–63. doi: 10.1007/164_2019_257
28. Chen W, Nong Z, Li Y, Huang J, Chen C, Huang L. Role of Dopamine Signaling in Drug Addiction. Curr Top Med Chem (2017) 17(21):2440–55. doi: 10.2174/1568026617666170504100642
29. Flores-Garcia L, Lensing MB, Ytterstad E, Eisemann M. Quality of life in substance use disorder patients with and without attention deficit hyperactivity disorder 12 months after treatment: a naturalistic follow-up study. Atten Defic Hyperact Disord (2019) 11(3):299–310. doi: 10.1007/s12402-019-00297-5
30. Martínez-González JM, Albein-Urios N, Verdejo-García A, Lozano-Rojas O. Differential Aspects of Treatment Dropout Risk in Cocaine Dependent Patients With and Without Personality Disorders. Adicciones (2014) 26(2):116–25.
31. Rubenis AJ, Fitzpatrick RE, Lubman DI, Verdejo-Garcia A. Impulsivity predicts poorer improvement in quality of life during early treatment for people with methamphetamine dependence. Addiction (2018) 113(4):668–76. doi: 10.1111/add.14058
32. Daigre C, Grau-Lopez L, Rodriguez-Cintas L, Ros-Cucurull E, Sorribes-Puertas M, Esculies O, et al. The role of dual diagnosis in health-related quality of life among treatment-seeking patients in Spain. Qual Life Res (2017) 26(12):3201–9. doi: 10.1007/s11136-017-1668-4
33. Liao J-Y, Mooney LJ, Zhu Y, Valdez J, Yoo C, Hser Y-I. Relationships between marijuana use, severity of marijuana-related problems, and health-related quality of life. Psychiatry Res (2019) 279:237–43. doi: 10.1016/j.psychres.2019.03.010
34. Becker SJ, Curry JF, Yang C. Factors that influence trajectories of change in frequency of substance use and quality of life among adolescents receiving a brief intervention. J Subst Abuse Treat (2011) 41(3):294–304. doi: 10.1016/j.jsat.2011.04.004
35. Campelo SR, Barbosa MA, Dias DR, Caixeta CC, Leles CR, Porto CC. Association between severity of illicit drug dependence and quality of life in a psychosocial care center in BRAZIL: cross-sectional study. Health Qual Life Outcomes (2017) 15(1):223. doi: 10.1186/s12955-017-0795-5
36. Mukherjee A, Dye BA, Clague J, Belin TR, Shetty V. Methamphetamine use and oral health-related quality of life. Qual Life Res (2018) 27(12):3179–90. doi: 10.1007/s11136-018-1957-6
37. Marini M, Schnornberger TM, Brandalise GB, Bergozza M, Heldt E. Quality of Life Determinants in Patients of a Psychosocial Care Center for Alcohol and other Drug Users. Issues Ment Health Nurs (2013) 34(7):524–30. doi: 10.3109/01612840.2013.780118
38. Muller AE, Skurtveit S, Clausen T. Many correlates of poor quality of life among substance users entering treatment are not addiction-specific. Health Qual Life Outcomes (2016) 14(1):39. doi: 10.1186/s12955-016-0439-1
39. Gonzales R, Ang A, Glik DC, Rawson RA, Lee S, Iguchi MY. Quality of Life among Treatment Seeking Methamphetamine-Dependent Individuals. Am J Addictions (2011) 20(4):366–72. doi: 10.1111/j.1521-0391.2011.00142.x
40. Chomchai C, Chomchai S. Global patterns of methamphetamine use. Curr Opin Psychiatry (2015) 28(4):269–74. doi: 10.1097/YCO.0000000000000168
41. Chiang M, Lombardi D, Du J, Makrum U, Sitthichai R, Harrington A, et al. Methamphetamine-associated psychosis: Clinical presentation, biological basis, and treatment options. Hum Psychopharmacol: Clin Exp (2019) 34(5):e2710. doi: 10.1002/hup.2710
42. Li X, Phillips MR, Dong X, Zhang Y, Yang S, Tong Y. Reliability and validity of an adapted Chinese version of Barratt Impulsiveness Scale. Chin Ment Health J (2011) 25(8):610–5. doi: 10.1007/s12583-011-0163-z
43. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol (1995) 51(6):768–74. doi: 10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1
44. Chen S, Huang S, Yang C, Cai W, Chen H, Hao W, et al. Neurofunctional Differences Related to Methamphetamine and Sexual Cues in Men With Shorter and Longer Term Abstinence Methamphetamine Dependence. Int J Neuropsychopharmacol (2020) 23(3):135–45. doi: 10.1093/ijnp/pyz069
45. Huang S, Zhang Z, Dai Y, Zhang C, Yang C, Fan L, et al. Craving Responses to Methamphetamine and Sexual Visual Cues in Individuals With Methamphetamine Use Disorder After Long-Term Drug Rehabilitation. Front Psychiatry (2018) 9:145. doi: 10.3389/fpsyt.2018.00145
46. Muller AE, Skurtveit S, Clausen T. Performance of the WHOQOL-BREF among Norwegian substance use disorder patients. BMC Med Res Methodol (2019) 19(1):44. doi: 10.1186/s12874-019-0690-3
47. Zhang G, Liu H, Xue H, Shan D, Yang YC, Duan S, et al. Analysis of quality of life and its influencing factors of heroin dependent patients with methadone maintenance therapy in Dehong prefecture, Yunnan province. Zhonghua Yu Fang Yi Xue Za Zhi (2011) 45(11):985–9. doi: 10.1631/jzus.B1000278
48. Deng CF, Ma X, Zhou H, Liu QL, Yang Y, Song Z, et al. Quality of life of heroin dependent patients with methadone maintenance therapy. Sichuan Da Xue Xue Bao Yi Xue Ban (2009) 40(3):539–43.
49. Gamage N, Senanayake S, Kumbukage M, Mendis J, Jayasekara A. The prevalence of anxiety and its association with the quality of life and illness severity among bipolar affective disorder patients in a developing country. Asian J Psychiatr (2020) 52:102044. doi: 10.1016/j.ajp.2020.102044
50. Shumye S, Belayneh Z, Mengistu N. Health related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: a cross sectional study. Health Qual Life Outcomes (2019) 17(1):169. doi: 10.1186/s12955-019-1233-7
51. Meyrignac L, Bouati N, Sagne A, Gavazzi G, Zipper AC. Representations of their own sexuality and aging body by old people: phenomenological and psychodynamic approach. Geriatr Psychol Neuropsychiatr Vieil (2017) 15(3):319–28. doi: 10.1684/pnv.2017.0688
52. Mroczek B, Kurpas D, Gronowska M, Kotwas A, Karakiewicz B. Psychosexual needs and sexual behaviors of nursing care home residents. Arch Gerontol Geriatr (2013) 57(1):32–8. doi: 10.1016/j.archger.2013.02.003
53. Dreno B, Bordet C, Seite S, Taieb C, Registre Acne D. Acne relapses: impact on quality of life and productivity. J Eur Acad Dermatol Venereol (2019) 33(5):937–43. doi: 10.1111/jdv.15419
54. Alanazy MH, Binabbad RS, Alromaih NI, Almansour RA, Alanazi SN, Alhamdi MF, et al. Severity and depression can impact quality of life in patients with myasthenia gravis. Muscle Nerve (2020) 61(1):69–73. doi: 10.1002/mus.26719
55. Roncero C, Palma-Alvarez RF, Diaz-Moran S, Grau-Lopez L, Rodriguez-Cintas L, Ros-Cucurull E, et al. Cocaine relapse and health-related quality of life: a 23 weeks study. Actas Esp Psiquiatr (2019) 47(2):37–44.
56. Schepis TS, McCabe SE. Prescription Opioid Misuse in US Older Adults: Associated Comorbidities and Reduced Quality of Life in the National Epidemiologic Survey of Alcohol and Related Conditions-III. J Clin Psychiatry (2019) 80(6):19m12853. doi: 10.4088/JCP.19m12853
57. Bizzarri J, Rucci P, Vallotta A, Girelli M, Scandolari A, Zerbetto E, et al. Dual diagnosis and quality of life in patients in treatment for opioid dependence. Subst Use Misuse (2005) 40(12):1765–76. doi: 10.1080/10826080500260800
58. Dietze P, Stoove M, Miller P, Kinner S, Bruno R, Alati R, et al. The self-reported personal wellbeing of a sample of Australian injecting drug users. Addiction (2010) 105(12):2141–8. doi: 10.1111/j.1360-0443.2010.03090.x
59. Wu LT, Woody GE, Yang C, Blazer DG. How do prescription opioid users differ from users of heroin or other drugs in psychopathology: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Addict Med (2011) 5(1):28–35. doi: 10.1097/ADM.0b013e3181e0364e
60. Colpaert K, De Maeyer J, Broekaert E, Vanderplasschen W. Impact of addiction severity and psychiatric comorbidity on the quality of life of alcohol-, drug- and dual-dependent persons in residential treatment. Eur Addict Res (2013) 19(4):173–83. doi: 10.1159/000343098
61. Pyne JM, French M, McCollister K, Tripathi S, Rapp R, Booth B. Preference-weighted health-related quality of life measures and substance use disorder severity. Addiction (2008) 103(8):1320–9; discussion 30-2. doi: 10.1111/j.1360-0443.2008.02153.x
62. Victor SE, Johnson SL, Gotlib IH. Quality of life and impulsivity in bipolar disorder. Bipolar Disord (2011) 13(3):303–9. doi: 10.1111/j.1399-5618.2011.00919.x
63. Albein-Urios N, Pilatti A, Lozano O, Martinez-Gonzalez JM, Verdejo-Garcia A. The value of impulsivity to define subgroups of addicted individuals differing in personality dysfunction, craving, psychosocial adjustment, and wellbeing: a latent class analysis. Arch Clin Neuropsychol (2014) 29(1):38–46. doi: 10.1093/arclin/act072
64. Mahoney JJ, Thompson-Lake DGY, Cooper K, Verrico CD, Newton TF, De La Garza R. A comparison of impulsivity, depressive symptoms, lifetime stress and sensation seeking in healthy controls versus participants with cocaine or methamphetamine use disorders. J Psychopharmacol (2014) 29(1):50–6. doi: 10.1177/0269881114560182
65. The Whoqol Group. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med (1998) 46(12):1569–85. doi: 10.1016/S0277-9536(98)00009-4
66. Hadinezhad P, Zarghami M, Montazer H, Moosazadeh M, Ghaderi F. Study of Methamphetamine Use in Patients Referred to Emergency Ward of a General Hospital at North of Iran in 2017. Addict Health (2019) 11(1):18–25.
67. Wei GL, Zheng XZ, Chen KQ, Shi YY, Wang LY, Tan XY. Coronary sinus flow is reduced in methamphetamine abusers: a transthoracic echocardiographic study. Int J Cardiovasc Imaging (2018) 34(12):1889–94. doi: 10.1007/s10554-018-1417-y
68. Crouse JJ, Lee RSC, White D, Moustafa AA, Hickie IB, Hermens DF. Distress and sleep quality in young amphetamine-type stimulant users with an affective or psychotic illness. Psychiatry Res (2018) 262:254–61. doi: 10.1016/j.psychres.2018.02.033
Keywords: methamphetamine, quality of life, impulsivity, substance use disorder, drug abuse, drug use
Citation: Wang Y, Zuo J, Hao W, Shen H, Zhang X, Deng Q, Liu M, Zhao Z, Zhang L, Zhou Y, Li M, Liu T and Zhang X (2020) Quality of Life in Patients With Methamphetamine Use Disorder: Relationship to Impulsivity and Drug Use Characteristics. Front. Psychiatry 11:579302. doi: 10.3389/fpsyt.2020.579302
Received: 02 July 2020; Accepted: 31 August 2020;
Published: 30 September 2020.
Edited by:
Yanhui Liao, Sir Run Run Shaw Hospital, ChinaCopyright © 2020 Wang, Zuo, Hao, Shen, Zhang, Deng, Liu, Zhao, Zhang, Zhou, Li, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tieqiao Liu, aXV0aWVxaWFvMTIzQGNzdS5lZHUuY24=; Xiangyang Zhang, emhhbmd4eUBwc3ljaC5hYy5jbg==
 Yingying Wang1
Yingying Wang1 Wei Hao
Wei Hao Hongxian Shen
Hongxian Shen Xiaojie Zhang
Xiaojie Zhang Tieqiao Liu
Tieqiao Liu Xiangyang Zhang
Xiangyang Zhang