
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 29 October 2020
Sec. Mood Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.563761
This article is part of the Research TopicPerinatal Mental Health: Expanding the Focus to the Family ContextView all 30 articles
 Susan Garthus-Niegel1,2,3*
Susan Garthus-Niegel1,2,3* Andreas Staudt3
Andreas Staudt3 Patricia Kinser4
Patricia Kinser4 Silje Marie Haga5
Silje Marie Haga5 Filip Drozd5
Filip Drozd5 Sophie Baumann3
Sophie Baumann3In contrast to the large body of research on maternal perinatal depression, paternal perinatal mental health has received little attention; and longitudinal studies on paternal perinatal depression, following (expectant) fathers over time, are exceedingly rare. This population-based study aimed to (1) estimate prevalence rates of perinatal depression symptoms among German (expectant) fathers, (2) identify differential profiles of perinatal depression in (expectant) fathers, (3) determine modifiable predictors of latent depression profiles, and (4) estimate how membership in subgroups changes during the perinatal period. Data were derived from the longitudinal cohort study DREAM (Dresden Study on Parenting, Work, and Mental Health), including 1,027 (expectant) fathers responding to the Edinburgh Postnatal Depression Scale (EPDS) during pregnancy and 8 weeks postpartum. Unobserved profiles of paternal perinatal depression and movement between profiles were investigated using latent transition analysis. A number of potential predictors with regard to lifestyle and current life situation were included as covariates. We found that rates of paternal depression symptoms decreased with 9% during pregnancy to 5% at 8 weeks postpartum. Further, four latent depression profiles emerged: most (expectant) fathers did not exhibit any depression symptoms (not depressed), whereas some reported mainly the absence of joy (anhedonic) and some experienced mainly self-blame and worries (anxious-worried). The depressive profile was characterized by endorsement to most symptoms of perinatal depression. Perceived social support and relationship satisfaction appeared to be protective against paternal depression symptoms. Differential transitioning or stability patterns in profile membership during the perinatal period were found, whereas the depressive profile showed to be the least stable. This prospective population-based cohort study is the first study to identify paternal perinatal depression profiles together with their predictors and changes during the perinatal period. Future research is warranted to examine whether the identified paternal depression profiles have differential outcomes, particularly in the context of person-centered prevention and intervention strategies. Further, longitudinal trajectories of paternal depression ought to be studied, taking into account additional measurement points as well as modifiable risk factors.
The perinatal period is a time involving much emotional turmoil for (expectant) parents. Regarding (expectant) mothers, studies suggest that women are at increased risk for mental health concerns during this life period (1) and report that 10–15% of women experience clinically significant depression symptoms during pregnancy or the postpartum period (2, 3). Recent studies highlight that women are at equal risk of developing depression during pregnancy as after birth (4), and one of the greatest risks factors for the onset of postpartum depression is depression symptoms in pregnancy (5–8). Core symptoms of maternal perinatal depression comprise tearfulness, feelings of hopelessness, inadequacy, guilt, inability to cope with and feel joy over the new baby, agitation and anxiety, loss of appetite, poor concentration and memory, sleep disturbances, fatigue, social isolation, and suicidal ideation (9). Perinatal depression symptoms are a major cause for concern as they directly or indirectly increase maternal morbidity and mortality (10). Indeed, clinically significant depression symptoms are projected to be a leading cause of illness and disability in the world by 2030; further, suicide is currently a major cause of maternal death in developed countries (10, 11). Children of affected women are at increased risk of being born preterm or with low birth weight (12) and are less frequently breastfed (13). Also, women who suffer from perinatal depression are less capable of interacting with their infant in an appropriate and warm manner, such as engaging in important developmental activities with the baby (e.g., playing and talking) which may negatively influence the child's cognitive and socioemotional development (14–16) and the infant's attachment style (17).
In contrast to the large body of research on maternal perinatal depression, paternal perinatal mental health has received little attention from researchers and clinicians, and very little is known about paternal perinatal depression (18–21). However, as with their maternal counterparts, fathers appear to be at increased risk of depression in the perinatal period (22–26). While the prevalence rate of depression in men in the general population is ~4.8% (27), a meta-analysis found that the rate of paternal depression between the first trimester and 1 year postpartum was 10.4% (19). This suggests that paternal perinatal depression also represents a significant public health concern (19). As gender roles shift and paternal involvement in childcare is becoming the norm in western societies, fathers' mental health becomes increasingly important for their children (19, 28). Indeed, there is mounting evidence that early paternal depression may have substantial emotional, behavioral, and developmental effects on children (19, 29–31). For instance, longitudinal cohort studies from the United Kingdom have shown that depression symptoms in the father at 2 months postpartum could predict a higher risk of behavioral problems in children at 3.5 years of age (32) and an increased risk of behavioral and conduct disorders, including peer relationship difficulties, by 7 years of age (29, 33). Paternal depression during the perinatal period may resemble maternal perinatal depression (19), although some evidence suggests that depression in men is characterized more often by a high level of general distress (33, 34). Thus far, data on paternal perinatal depression are based on an emerging and inconsistent literature, and longitudinal studies on paternal perinatal depression, following (expectant) fathers over time, are exceedingly rare (19).
Given the clear need for longitudinal studies on paternal perinatal depression, this population-based study aimed to (1) estimate prevalence rates of perinatal depression symptoms among German (expectant) fathers, (2) identify differential profiles of perinatal depression in (expectant) fathers, (3) determine modifiable predictors of latent depression profiles, and (4) estimate how membership in subgroups changes during the perinatal period.
This investigation is part of the longitudinal cohort Dresden Study on Parenting, Work, and Mental Health (DREAM; DResdner Studie zu Elternschaft, Arbeit, und Mentaler Gesundheit), which prospectively examines the relationship between parental work participation, role distribution, stress factors, and their effects on perinatal outcomes and long-term family mental and somatic health (35). Expectant mothers and their partners were recruited during pregnancy, predominately at information sessions in hospitals and birth preparation courses in and around Dresden, Germany. The DREAM study consists of currently four measurement points, during which questionnaires covering a comprehensive field of physical and mental health outcomes are completed by participants. The measurement points encompass time point one (T1; during pregnancy), and three postpartum assessment waves: time point two (T2) at 8 weeks after the anticipated birth, time point three (T3) at 14 months, and time point four (T4) at 2 years after birth [postpartum follow-up data collection is still ongoing and prolongation into middle childhood planned; for a detailed description of the study see (35)]. The DREAM study has been reviewed and approved by the Ethics Committee of the Faculty of Medicine of the Technische Universität Dresden (No: EK 278062015), and all participants provided their written informed consent to participate in this study. Study data were collected and managed using Research Electronic Data Capture (REDCap), hosted at the “Koordinierungszentrum für Klinische Studien” at the Faculty of Medicine of the Technische Universität Dresden (36, 37). For the purpose of the present study, T1 (during pregnancy) and T2 (8 weeks postpartum) data from 1,027 (expectant) fathers were analyzed.
Paternal perinatal depression symptoms were measured by the German version of the Edinburgh Postnatal Depression Scale [EPDS; (38)], which was administered at T1 and T2. The EPDS is the most common scale to screen for symptoms of maternal perinatal depression (39) and has been validated in numerous studies. It has been shown to be a valid instrument for identifying probable major depression in postnatal fathers (21, 34). The EPDS is a 10-item self-report instrument, scored on a four-point scale [0–3; (38, 40)], with scores ranging from 0 to 30 whereby higher scores suggest higher levels of depression symptoms.
The 10 EPDS items were used as manifest indicators of latent paternal depression profiles. The items were dichotomized in order to represent approval or refusal of each symptom. Dichotomized items were chosen over the original scale and a three-categorical solution because very few individuals scored in the two highest categories of the four-point EPDS scale. Moreover, using the original scale would add substantial complexity to the identification and distinction of latent profiles, not least because the response options do not seem to be equidistant. Due to the item-specific labels of the EPDS, the cut-off, above which a symptom was regarded as endorsed, had to be chosen for each item individually. The dichotomization was either carried out between response options 0–1 and 2–3 (EPDS items 3–8) or between 0 and 1–3 (EPDS items 1, 2, 9, and 10).
For the purpose of sample description, the sum score of the EPDS was used. The prevalence of paternal perinatal depression is reported using the most common cut-off scores of ≥10 to indicate minor depression and ≥12 to indicate major depression (34, 38, 40). For all latent variable models, single dichotomized EPDS items were used (see section Statistical Analysis).
Socio-demographic characteristics, relationship factors, and health behaviors were assessed at T1. Current paternal age was calculated from (expectant) fathers' date of birth and the date they answered the T1 questionnaire. (Expectant) fathers were asked to indicate the number of children below the age of 14 living in the same household and their highest general educational degree, which was condensed into two categories (<12 years/12 or more years of school education).
Perceived social support was measured with the short version of the Social Support Questionnaire [F-SozU-14; (41)]. The short version of the Partnership Questionnaire [PFB-K; (42)] was used to assess relationship satisfaction. For both questionnaires, the sum score was calculated, with higher scores indicating higher levels of perceived social support and relationship satisfaction, respectively. One item was used to assess the distribution of housework between the two partners. The original scale ranged from 0 (“I do everything”) to 10 (“My partner does everything”) and was recoded so that 0 represents an equal distribution of household duties (five on the original scale) and higher values (deviations from 5) indicate an inequitable distribution to either side.
(Expectant) fathers' Body Mass Index (BMI) was calculated from their indicated height and weight. Self-reported alcohol consumption was measured with a quantity-frequency index, resulting in four categories: 0, 1–2, 3–7, or 8 or more alcoholic standard drinks consumed per week. Smoking was assessed with three categories: never smoked, former smokers or current smokers. Expectant fathers were asked to indicate how often they engage in physical activity per week (e.g., brisk walking, going to work by bicycle, sports): less than once per week, 1–2 times per week, or 3 times or more per week.
Three variables from the respective expectant mothers' T1 questionnaire were included as covariates: the expectant mothers' age, her highest educational degree, and her EPDS sum score.
To identify paternal perinatal depression profiles, and to estimate predictors and changes in subgroup membership, mixture modeling was used. Descriptive statistics and dropout analyses were done in Stata 14 (43). Logistic regression was used to test if T1 variables predicted non-participation at T2. Latent variable modeling was performed using Mplus version 7.4 (44). All latent variable models were analyzed with a full-information maximum likelihood estimator with robust standard errors, which uses all available data under the assumption of missing at random.
Data were analyzed in consecutive steps following the framework proposed by Ryoo et al. (45). At first, latent paternal perinatal depression profiles were identified using Latent Class Analysis (LCA). In LCA, manifest indicators (i.e., the 10 dichotomized EPDS items) are used to extract unobserved subgroups (latent classes) represented by a categorical latent variable. The aim is to find the number of latent classes that adequately represents the heterogeneity in a study population. The identification of the number of latent paternal depression profile classes was based on T1 data without adjusting for any covariates.
Models with different numbers of latent classes were compared using the Bayesian Information Criterion [BIC; (46)], the Akaike Information Criterion [AIC; (47)], the bootstrapped likelihood ratio test [BLRT; (48)], the class sizes as well as the conceptual meaning and distinctiveness of each latent class. BIC and AIC balance fit and parsimony of latent models, whereas models with smaller values are superior. The BLRT compares a model with k latent classes to a model with k-1 latent classes, whereas statistical significance favors the k-class-model. To evaluate clarity in classification, entropy (49) was obtained, with values ≥ 0.80 indicating adequate classification (50). Each model was rerun with a higher number of starting values (1,000 instead of 20) to ensure that the solutions are replicated and not caused by local maxima.
Then, data from T2 were analyzed in a similar manner to determine if the same number of latent classes were found for T1. Changes in latent class membership during the perinatal period from T1 to T2 were estimated using Latent Transition Analysis (LTA). In LTA, latent transition probabilities are estimated that represent the probabilities of changing the latent class from T1 to T2. The prerequisite for LTA is measurement invariance over time which allows to interpret changes in latent class membership as actual changes in paternal depression profiles because the latent classes have the same meaning over time. Measurement invariance was tested by comparing a measurement invariant LTA model in which the thresholds of class indicators were held equal over time with a measurement variant LTA model in which thresholds were allowed to vary over time using BIC values. To evaluate whether the LTA model-implied data fit to the empirical data, bivariate standardized residuals (BSRs) were used, with values below |1.96| indicating good fit. For the final LTA model (Figure 1), covariates were included to predict latent class membership at T1 in a multinomial logistic regression. Results were given as Odds Ratios (OR) with 95% confidence intervals (95%-CI).
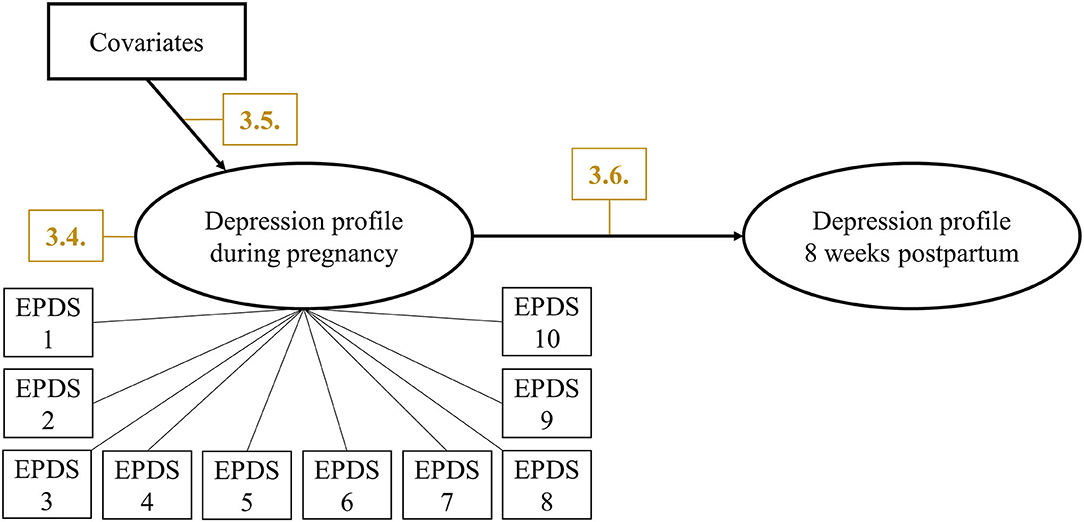
Figure 1. Final LTA modeling predictors and changes in paternal perinatal depression profiles. Manifest indicators for depression profile at 8 weeks postpartum were omitted for clarity. Yellow numbers indicate corresponding sections in Results.
By January 2020, n = 1,194 expectant fathers returned the first questionnaire (T1). Those expecting more than one child (n = 21), those who returned the questionnaire after birth (n = 21), and those who had incomplete data on the covariates (n = 125) were excluded. Thus, 1,027 expectant fathers were included into the analysis.
Of the n = 1,008 fathers, who had already received the second questionnaire (T2), n = 860 (85 %) fathers had returned the completed questionnaire on time. Those who were not reached for T2 (n = 145) were less likely to have children below the age of 14 in the household prior to the index baby (OR = 0.52, 95% CI: 0.30–0.90) and were more likely to report former (OR = 1.79, 95% CI: 1.16–2.76) or current smoking (OR = 2.23, 95% CI: 1.36–3.64).
Baseline sample characteristics are shown in Table 1. The final sample was composed of 1,027 men with a mean age of 32.4 years (SD = 4.9). The majority of participants (n = 675, 65.7%) had 12 or more years of school education. During pregnancy (T1), the mean EPDS score was 3.9 (SD = 3.6). According to the standard EDPS cut-off scores, 50 expectant fathers (5%) screened positive for minor depression (≥10) and 40 (4%) for major depression (≥12). At the postpartum (T2) assessment, the mean EPDS score was 3.5 (SD = 3.3). Of those participating in the T1 assessment, 20 (2%) screened positive for minor depression and 22 (3%) for major depression.
Table 2 shows fit indices, entropy values, and class sizes for separate LCA models specifying one to six classes. While AIC decreased with increasing number of classes, BIC and BLRT p-values indicated preferred fit for the four-class models. Therefore, we selected the four-class solution for LTA. BIC values indicated preferred fit for the measurement invariant LTA model (BIC = 10,802) over the measurement variant LTA model (BIC = 10,987). Of the 760 BSRs from the measurement invariant LTA, 738 values (97%) were below |1.96|. The largest residual value was 3.86. Entropy for the final LTA model with covariates was 0.84.
The estimated class-specific probabilities of scoring high on the EDPS items for the four-class model are depicted in Figure 2. (Expectant) fathers in the largest class (n = 677, 66%) were characterized by near-zero probabilities of scoring high on the EPDS items. This class was labeled not depressed. About 17% of the (expectant) fathers (n = 178) were allocated to an anhedonic class characterized by high probabilities of scoring high on EPDS items 1 (“I have not been able to laugh and see the funny side of things”) and 2 (“I have not looked forward with enjoyment to things”). (Expectant) fathers in the anxious-worried class (n = 142, 14%) were characterized by high probabilities of scoring high on EPDS items 3 (“I have blamed myself unnecessarily when things went wrong”) and 4 (“I have been anxious or worried for no good reason”). The smallest class (n = 30, 3%) consisted of (expectant) fathers with high probabilities of agreeing with all EPDS items. This class was labeled depressive.
As shown in Table 3, (expectant) fathers in the anhedonic class were less likely to engage in physical activity three or more times vs. once a week (OR = 0.48, 95% CI: 0.27–0.85), reported lower social support (OR = 0.94, 95% CI: 0.92–0.97), were less satisfied with their relationship (OR = 0.93, 95% CI: 0.88–0.98), were less likely to have a partner with 12 or more years of education (OR = 0.57, 95% CI: 0.34–0.96), and were more likely to have a partner scoring high on the EPDS (OR = 1.08, 95% CI: 1.02–1.13) compared to (expectant) fathers in the not depressed class.
(Expectant) fathers in the anxious-worried class were younger (OR = 0.91, 95% CI: 0.85–0.98), were less likely to have 12 or more years of school education (OR = 0.51, 95% CI: 0.31–0.84), were more likely to have a higher BMI (OR = 1.07, 95% CI: 1.01–1.13), reported lower social support (OR = 0.94, 95% CI: 0.91–0.97), and were more likely to have a partner of older age (OR = 1.11, 95% CI: 1.02–1.21) and to have a partner scoring high on the EPDS (OR = 1.07, 95% CI: 1.01–1.14) compared to (expectant) fathers in the not depressed class.
(Expectant) fathers in the depressive class were more likely to have children below age 14 in the household (OR = 2.67, 95% CI: 1.08–6.59), reported lower social support (OR = 0.93, 95% CI: 0.89–0.99), and were less satisfied with their relationship (OR = 0.87, 95% CI: 0.77–0.98) compared to (expectant) fathers in the not depressed class.
Table 4 shows the probabilities of transitioning from a particular latent depression profile class during pregnancy to another class at 8 weeks postpartum (T2). Stability in the depression profile was highest in the not depressed class. (Expectant) fathers allocated to this class during pregnancy had a probability of 0.884 of still being classified as not depressed at 8 weeks postpartum. For the other classes, probabilities that an (expectant) father would transition to the not depressed class ranged between 0.265 (depressive) and 0.549 (anhedonic). Stability in the depression profile was lowest in the depressive class. (Expectant) fathers allocated to this class during pregnancy had a probability of 0.337 of remaining depressive at 8 weeks postpartum (T2). For the other classes, probabilities of transitioning to the depressive class ranged between 0.004 (not depressed) and 0.027 (anxious-worried).
This prospective population-based cohort study estimated prevalence rates of paternal perinatal depression symptoms, identified paternal perinatal depression profiles as well as predictors of those latent depression profiles, and estimated latent transition probabilities in the identified subgroups during the perinatal period. Our data revealed four main findings. First, about one in 10 expectant fathers reported depression symptoms; lower rates were reported at 8 weeks postpartum. Second, four qualitatively different depression profiles exist within the study population, with two-thirds of the (expectant) fathers experiencing no or few depression symptoms. Third, perceived social support and relationship satisfaction may be protective against paternal depression symptoms. Fourth, expectant fathers with absence of depression are very unlikely to develop symptoms at postpartum; those with symptomatology during pregnancy are likely to experience improvement or even remission from depression symptoms.
We found that rates of paternal depression symptoms decreased from T1 to T2, with 9% during pregnancy (i.e., 5% likely minor and 4% likely major depression) and 5% at 8 weeks postpartum (i.e., 2% likely minor and 3% likely major depression). These prevalence rates are slightly lower than what was found as an overall rate in a previous meta-analysis (19). However, the meta-analysis found that national origin of the study accounted for considerable variability in depression rates of fathers. While (expectant) fathers in the United States reported somewhat higher depression rates (14.1% on average), the average rate of the international studies was 8.2%, and thus rather similar to our results. Further, a more recent meta-analysis found an overall prevalence rate of paternal perinatal depression of 8% (51). Likewise, in line with these meta-analyses' results suggesting that the first 3 months postpartum are characterized by especially low depression rates (19, 51), we found lower prevalence rates at 8 weeks postpartum compared to the prior assessment during pregnancy. Still, a recent study among first-time fathers identified a subgroup of fathers whose depressive symptoms were highest at 1 year postpartum (52). Therefore, data from a longer follow-up period are needed before more definite conclusions can be drawn.
Further, four latent depression profiles emerged: most (expectant) fathers did not exhibit any depression symptoms (not depressed), whereas some reported mainly the absence of joy (anhedonic) and some experienced mainly self-blame and worries (anxious-worried). The depressive profile was characterized by endorsement to most symptoms of perinatal depression. Tuohy and McVey conducted a principal component analysis of the EPDS in recent mothers and found that the scale encompasses three dimensions: depression, anhedonia, and anxiety (53). Our own findings add and complement these prior findings gained from a traditional variable-centered approach with a person-centered approach proposing that the EPDS appears to reflect important dimensionality both toward symptomatology as well as toward inherent latent subgroups.
Even though we found some differential predictors of the respective depression profiles, several of the potentially modifiable predictors displayed similar patterns. All three depression profiles with at least some depression symptomatology (i.e., the anhedonic, anxious-worried, and depressive class) reported lower social support and individuals in the anhedonic and the depressive class were less satisfied with their relationships. Hence, perceived social support and relationship satisfaction served as protective factors; this finding is similar to a previous study on emotional distress in couples during pregnancy (54). Maternal depression, on the other hand, served as a risk factor for both the anhedonic and anxious-worried class, corresponding to results of a meta-analysis estimating moderate maternal-paternal depression symptom correlation (19). Interestingly, (expectant) fathers with an anhedonic profile were less likely to engage in physical activity three or more times a week compared to those with absence of depression symptoms, whereas this association was not found in those with an anxious-worried or depressive profile. Moreover, having children below the age of 14 in the same household prior to the index baby increased the risk for being categorized into the depressive profile, but not into the anhedonic or anxious-worried profile. Although our data do not allow causal inferences to be made, this may have implications for the development of future mental health interventions tailored to the respective paternal depression profile.
Our results showed differential transitioning or stability patterns in profile membership during the perinatal period. The depressive profile was the least stable (as underlined by the fact that fewer fathers scored above the EPDS major and minor cut-offs during the postpartum period): the probability to be classified as depressive at 8 weeks postpartum, if one was already classified as depressive during pregnancy was 34%. In contrast, the probability of remaining not depressed was 88%. Transitioning into the depressive profile at 8 weeks postpartum was very unlikely. This is entirely in line with findings from studies on maternal perinatal depression showing that one of the most important risks factors for postpartum depression is depressive symptomatology during pregnancy (6, 7). Interestingly, the anhedonic and anxious-worried profile exhibited somewhat parallel courses and there were practically no transitions between these two profiles. Rather, members of these two profiles either stayed in the same profile or changed to the not depressed profile, suggesting that they indeed represent qualitatively different depression profile patterns.
These findings suggest that the ideal time to initiate prevention measures is during the prenatal period, even in individuals who have sub-clinical symptom levels. Furthermore, it may be speculated that the anhedonic and anxious-worried profiles are mildly symptomatic precursors of depression, and thus may represent target groups for prevention with low threshold symptomatology. However, we are unable to validate the clinical significance of depression symptoms in these groups.
To our knowledge, this prospective population-based cohort study is the first study to identify paternal perinatal depression profiles together with their predictors and changes during the perinatal period. We used state-of-the-art categorical latent variable modeling; this technique allowed us to use all available data of a large sample of (expectant) fathers, to classify them into meaningful (a priori unknown) subgroups representing unobserved heterogeneity in the larger population, and to identify underlying covariates or mechanisms which cause the heterogeneity. Despite our large sample size, some potentially important predictors (e.g., socio-economic status) could not be taken into account because of very small cell sizes in the joint distribution. Further, transition probabilities could not be predicted due to the same reason. As a result, parameter estimates would not have been trustworthy. Another limitation is the lack of measurements after 8 weeks postpartum, as previous literature suggests that paternal depression could have a late onset (19). Also, the assessment of depression symptoms was based on self-report and depression symptoms may be under-reported due to social desirability. Even though the EPDS has been validated in numerous studies, this has been done primarily in women; further, it is well-established that EPDS is a screening instrument rather than a clinical diagnostic tool. Finally, selection bias may have limited the generalizability for the whole population of (expectant) fathers. The high proportion of higher-educated participants may also be explained by characteristics of the recruitment setting. The Dresden population includes a large number of university students and employees. Further, persons with higher rather than lower socioeconomic status may be more likely to take part in hospital information sessions and birth preparation courses.
This prospective population-based cohort study is the first study to identify paternal perinatal depression profiles together with their predictors and changes during the perinatal period. To this end we used state-of-the-art categorical latent variable modeling to classify our large sample of (expectant) fathers into meaningful subgroups. The findings from this study suggest that future research is warranted to examine whether the identified paternal depression profiles have differential outcomes, particularly in the context of person-centered prevention and intervention strategies. In a similar vein, it would be of great relevance to determine whether the depressive profile in fact represents a group in need of clinical treatment. Finally, future studies ought to investigate longitudinal trajectories of paternal depression, taking into account additional measurement points as well as modifiable risk factors. Following up the study's participants, we will be eventually able to do so with the DREAM study applying growth mixture modeling (GMM).
The datasets presented in this article are not readily available because of legal and ethical constraints. Public sharing of participant data was not included in the informed consent of the study. Requests to access the datasets should be directed to Susan Garthus-Niegel, c3VzYW4uZ2FydGh1cy1uaWVnZWxAdW5pa2xpbmlrdW0tZHJlc2Rlbi5kZQ==.
The DREAM study has been reviewed and approved by the Ethics Committee of the Faculty of Medicine of the Technische Universität Dresden (No: EK 278062015), and all Participants provided their written informed consent to participate in this study.
This study was conceived and research questions developed by SG-N and SB. AS and SB performed the statistical analysis. Data were interpreted by SG-N, AS, PK, SH, FD, and SB. SG-N, AS, and SB wrote the manuscript. SG-N has acquired the funding and been responsible for conception and design of the DREAM study as well as the coordination and supervision of the (ongoing) data collection. All authors contributed to the article and approved the submitted version.
The DREAM study received funding by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation; GA 2287/4-1 and GA 2287/4-2). Also, SG-N is a management committee member of COST action CA18211.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We want to thank all (expectant) fathers and their partners for supporting our project. Furthermore, we want to thank all cooperating clinics and midwives for having provided access to the potential participants as well as all students having performed the recruitment. We wish to extend many thanks to all institutions supporting our lottery. We are further grateful to Marie Kopp and Victoria Kress for their helpful assistance in data preparation.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.563761/full#supplementary-material
1. Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. (2006) 296:2582–9. doi: 10.1001/jama.296.21.2582
2. Goecke TW, Voigt F, Faschingbauer F, Spangler G, Beckmann MW, Beetz A. The association of prenatal attachment and perinatal factors with pre- and postpartum depression in first-time mothers. Arch Gynecol Obstet. (2012) 286:309–16. doi: 10.1007/s00404-012-2286-6
3. Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. (2005) 106:1071–83. doi: 10.1097/01.AOG.0000183597.31630.db
4. Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. (2010) 116:1064–70. doi: 10.1097/AOG.0b013e3181f60b0a
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association (2013).
6. Beck CT. Predictors of postpartum depression: an update. Nurs Res. (2001) 50:275–85. doi: 10.1097/00006199-200109000-00004
7. Drozd F, Haga SM, Valla L, Slinning K. Latent trajectory classes of postpartum depressive symptoms: a regional population-based longitudinal study. J Affect Disord. (2018) 241:29–36. doi: 10.1016/j.jad.2018.07.081
8. Kinser PA, Thacker LR, Lapato D, Wagner S, Roberson-Nay R, Jobe-Shields L, et al. Depressive symptom prevalence and predictors in the first half of pregnancy. J Womens Health. (2018) 27:369–76. doi: 10.1089/jwh.2017.6426
9. Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. (2004) 26:289–95. doi: 10.1016/j.genhosppsych.2004.02.006
10. World Health Organization. Improving Maternal Mental Health. Geneva: World Health Organization (2008).
11. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. (2006) 3:e442. doi: 10.1371/journal.pmed.0030442
12. Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. (2010) 67:1012–24. doi: 10.1001/archgenpsychiatry.2010.111
13. Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. (2007) 20:189–209. doi: 10.1080/14767050701209560
14. Goodman SH, Brogan D, Lynch ME, Fielding B. Social and emotional competence in children of depressed mothers. Child Dev. (1993) 64:516–31. doi: 10.2307/1131266
15. Junge C, Garthus-Niegel S, Slinning K, Polte C, Breines S, Eberhard-Gran M. The impact of perinatal depression on children's social-emotional development: a longitudinal study. Matern Child Health J. (2017) 21:607–15. doi: 10.1007/s10995-016-2146-2
16. Bridgett DJ, Burt NM, Edwards ES, Deater-Deckard K. Intergenerational transmission of self-regulation: a multidisciplinary review and integrative conceptual framework. Psychol Bull. (2015) 141:602–54. doi: 10.1037/a0038662
17. Bonari L, Bennett H, Einarson A, Koren G. Risks of untreated depression during pregnancy. Can Fam Physician. (2004) 50:37–9.
18. Cox J. Postnatal depression in fathers. Lancet. (2005) 366:982. doi: 10.1016/S0140-6736(05)67372-2
19. Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA. (2010) 303:1961–9. doi: 10.1001/jama.2010.605
20. Skjothaug T, Smith L, Wentzel-Larsen T, Moe V. Does fathers' prenatal mental health bear a relationship to parenting stress at 6 months? Infant Ment Health J. (2018) 39:537–51. doi: 10.1002/imhj.21739
21. Edmondson OJ, Psychogiou L, Vlachos H, Netsi E, Ramchandani PG. Depression in fathers in the postnatal period: assessment of the Edinburgh Postnatal Depression Scale as a screening measure. J Affect Disord. (2010) 125:365–8. doi: 10.1016/j.jad.2010.01.069
22. Escribà-Agüir V, González-Galarzo MC, Barona-Vilar C, Artazcoz L. Factors related to depression during pregnancy: are there gender differences? J Epidemiol Community Health. (2008) 62:410–4. doi: 10.1136/jech.2007.063016
23. van den Berg MP, van der Ende J, Crijnen AA, Jaddoe VW, Moll HA, Mackenbach JP, et al. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics. (2009) 124:e96–103. doi: 10.1542/peds.2008-3100
24. Goodman JH. Paternal postpartum depression, its relationship to maternal postpartum depression, and implications for family health. J Adv Nurs. (2004) 45:26–35. doi: 10.1046/j.1365-2648.2003.02857.x
25. Condon JT, Boyce P, Corkindale CJ. The first-time fathers study: a prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust N Z J Psychiatry. (2004) 38:56–64. doi: 10.1111/j.1440-1614.2004.01298.x
26. Ayers S, Joseph S, McKenzie-McHarg K, Slade P, Wijma K. Post-traumatic stress disorder following childbirth: current issues and recommendations for future research. J Psychosom Obstet Gynecol. (2008) 29:240–50. doi: 10.1080/01674820802034631
27. Kessler RC, Berglund P, Demler O. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. (2003) 289:3095–105. doi: 10.1001/jama.289.23.3095
28. Wilson S. Durbin CE. Effects of paternal depression on fathers' parenting behaviors: a meta-analytic review. Clin Psychol Rev. (2010) 30:167–80. doi: 10.1016/j.cpr.2009.10.007
29. Ramchandani PG, O'Connor TG, Heron J, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: a population cohort study. J Am Acad Child Psychiatry. (2008) 47:390–8. doi: 10.1097/CHI.0b013e31816429c2
30. Paulson JF, Keefe HA, Leiferman JA. Early parental depression and child language development. J Child Psychol Psychiatry. (2009) 50:254–62. doi: 10.1111/j.1469-7610.2008.01973.x
31. Fredriksen E, von Soest T, Smith L, Moe V. Parenting stress plays a mediating role in the prediction of early child development from both parents' perinatal depressive symptoms. J Abnorm Child Psychol. (2019) 47:149–64. doi: 10.1007/s10802-018-0428-4
32. Ramchandani P, Stein A, Evans J, O'Connor TG. Paternal depression in the postnatal period and child development: a prospective population study. Lancet. (2005) 365:2201–5. doi: 10.1016/S0140-6736(05)66778-5
33. Massoudi P, Hwang CP, Wickberg B. Fathers' depressive symptoms in the postnatal period: Prevalence and correlates in a population-based Swedish study. Scand J Public Health. (2016) 44:688–94. doi: 10.1177/1403494816661652
34. Massoudi P, Hwang CP, Wickberg B. How well does the Edinburgh Postnatal Depression Scale identify depression and anxiety in fathers? A validation study in a population based Swedish sample. J Affect Disord. (2013) 149:67–74. doi: 10.1016/j.jad.2013.01.005
35. Kress V, Steudte-Schmiedgen S, Kopp M, Förster A, Altus C, Schier C, et al. The impact of parental role distributions, work participation, and stress factors on family health-related outcomes: study protocol of the prospective multi-method cohort “Dresden Study on Parenting, Work, and Mental Health” (DREAM). Front Psychol. (2019) 10:1273. doi: 10.3389/fpsyg.2019.01273
36. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
37. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
38. Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O. Deutschsprachige fassung und validierung der “Edinburgh Postnatal Depression Scale” [German version and validation of the “Edinburgh Postnatal Depression Scale”]. Dtsch Med Wochenschr. (1998) 123:35–40. doi: 10.1055/s-2007-1023895
39. Hewitt CE, Gilbody SM, Mann R, Brealey S. Instruments to identify post-natal depression: which methods have been the most extensively validated, in what setting and in which language? Int J Psychiatry Clin Pract. (2010) 14:72–6. doi: 10.3109/13651500903198020
40. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry J Ment Sci. (1987) 150:782–6. doi: 10.1037/t01756-000
41. Fydrich T, Sommer G, Tydecks S, Brähler E. Fragebogen zur sozialen Unterstützung (F-SozU): Normierung der Kurzform (K-14). [Social Support Questionnaire (F-SozU): Standardization of short form (K-14).]. Z Med Psychol. (2009) 18:43–8. Available online at: https://psycnet.apa.org/record/2008-19370-004
42. Kliem S, Job AK, Kröger C, Bodenmann G, Stöbel-Richter Y, Hahlweg K, et al. Entwicklung und Normierung einer Kurzform des Partnerschaftsfragebogens (PFB-K) an einer repräsentativen deutschen Stichprobe. Z Klin Psychol Psychother. (2012) 41:81–9. doi: 10.1026/1616-3443/a000135
45. Ryoo JH, Wang C, Swearer SM, Hull M, Shi D. Longitudinal model building using latent transition analysis: an example using school bullying data. Front Psychol. (2018) 9:675. doi: 10.3389/fpsyg.2018.00675
46. Schwarz G. Estimating dimension of a model. Ann Stat. (1978) 6:461–4. doi: 10.1214/aos/1176344136
47. Akaike H. Information theory an extension of the maximum likelihood principle. In: Parzen E, Tanabe K, Kitagawa G, editors. Selected Papers of Hirotugu Akaike. New York, NY: Springer (1998). p. 199–213.
49. Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif . (1996) 13:195–212. doi: 10.1007/BF01246098
50. Wang J, Wang X. Structural Equation Modeling: Applications Using Mplus. West Sussex: John Wiley & Sons (2012).
51. Cameron EE, Sedov ID, Tomfohr-Madsen LM. Prevalence of paternal depression in pregnancy and the postpartum: an updated meta-analysis. J Affect Disord. (2016) 206:189–203. doi: 10.1016/j.jad.2016.07.044
52. Molgora S, Fenaroli V, Malgaroli M, Saita E. Trajectories of postpartum depression in Italian first-time fathers. Am J Mens Health. (2017) 11:880–7. doi: 10.1177/1557988316677692
53. Tuohy A, McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. Br J Clin Psychol. (2008) 47:153–69. doi: 10.1111/j.2044-8260.2008.tb00463.x
Keywords: paternal perinatal depression, depression profiles, latent class analysis, latent transition analysis, DREAM study
Citation: Garthus-Niegel S, Staudt A, Kinser P, Haga SM, Drozd F and Baumann S (2020) Predictors and Changes in Paternal Perinatal Depression Profiles—Insights From the DREAM Study. Front. Psychiatry 11:563761. doi: 10.3389/fpsyt.2020.563761
Received: 19 May 2020; Accepted: 28 September 2020;
Published: 29 October 2020.
Edited by:
Paul Stokes, King's College London, United KingdomReviewed by:
Sarah Kittel-Schneider, University Hospital Würzburg, GermanyCopyright © 2020 Garthus-Niegel, Staudt, Kinser, Haga, Drozd and Baumann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susan Garthus-Niegel, c3VzYW4uZ2FydGh1cy1uaWVnZWxAdW5pa2xpbmlrdW0tZHJlc2Rlbi5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.