- 1Humanism and Social Resilience, University of Humanistic Studies, Utrecht, Netherlands
- 2Care Ethics, University of Humanistic Studies, Utrecht, Netherlands
- 3Department of Psychiatry, Leiden University Medical Center, Leiden, Netherlands
- 4Ministry of Defense, Military Mental Health Research Center, Utrecht, Netherlands
- 5ARQ National Psychotrauma Center, Diemen, Netherlands
Background: Firefighters, paramedics, specialized nurses working in Intensive Care Units (ICUs), Operating Rooms (OR), and Emergency Rooms (ER), police officers and military personnel are more frequently exposed to potentially traumatic events than the general population; they are considered high-risk professionals. To reduce the risk of traumatization it is of great importance to be embedded in a social environment with supportive relationships.
Methods: We performed a systematic review (based on the PRISMA-Guidelines) looking for social connections within the environment in which high-risk professionals are embedded (work, home, community), to obtain evidence on the impact of these connections on the risk of traumatization. Additionally, we aim to identify relevant supportive relationships in the professionals' environments. We identified the relevant scientific literature by searching, without time, and language restriction, five electronic bibliographic databases: MEDLINE, PsycINFO, Sociological Abstracts, CINAHL, and Web of Science. These databases were last searched in January 2019.
Results: A qualitative analysis of the 89 eligible (out of 9,047 screened) studies shows that for firefighters, paramedics, and emergency nurses social connections in their work environment are predominantly supportive relationships and may protect them against traumatization. In other occupations (OR-nurses, ICU-nurses, police officers), however, social connections at work are not only a source of support but are also a source of stress. For military personnel study results are inconclusive as to whether their social connections at work or at home support them against traumatization. In so far as connections are supportive, their sources vary greatly from one occupational group to another; they differ between work vs. home as well as within work between peers vs. supervisor.
Conclusions: Being embedded in a social environment, i.e., having social connections, is important but not always sufficient to protect high-risk professionals against traumatization. For, while these connections may be the antecedents of supportive relationships, they can also be the antecedents of damaging relationships. Additionally, the sources of supportive relationships differ among groups. This suggests that knowledge of how the social structures of the occupational groups differ may increase our understanding of the impact of social connections and relationships, including socialization, on the risk of traumatization of high-risk professionals.
Introduction
Firefighters, ambulance paramedics, police officers, and military personnel are more frequently exposed to potentially traumatic events than the general population (1–3). Their involvement in critical incidents, which are often a matter of life and death of others and sometimes of their own, may go along with high arousal or dissociative states and feelings of powerlessness. They risk the development of posttraumatic stress disorder (PTSD) (1, 4–6), or other mental health problems related (comorbidity) to traumatization (7, 8). Exposure to human suffering and indirect exposure to extreme stressful events can also result in secondary traumatic stress disorder, compassion fatigue, or burnout (9–11). Any lower level of mental health can compromise the mental capacity to integrate stressful events and thus increases the risk of traumatization (12, 13). That is why they are considered to be a high-risk category. Exposure to critical and potentially traumatic events not only concerns the aforementioned occupations, but also professionals working intramurally. Emergency and operating room nurses are also exposed to the severely injured patient. Although gruesome wounds are often physically covered by the time a patient arrives at the intensive care unit, the nurses are still exposed to the underlying stories of pain and suffering. Reviews confirm that specialized nurses working in intensive care units, emergency, and operating rooms also report significant mental health problems (14–24). It would be incorrect to assume however, that exposure to these events inevitably leads to dysfunctional or pathological reactions (25). Most high-risk professionals are not affected by traumatic stress and stay on the job (26), and numerous studies even report positive and salutary outcomes as a result of the experience of occupational trauma, i.e., posttraumatic growth (27–29). What may account for these different outcomes?
High-risk professionals were “all too often expected to be invulnerable to emotions” [(30), p. 4] in the presence of the distress of others, and therefore sometimes viewed as super-human with exceptional emotional strength or even, by the general population, as “heroes” (31, 32). Meta-analytic reviews of studies conducted across a wide range of general adult populations did indeed reveal several clear predictive personal variables with respect to PTSD risk, such as pretraumatic experiences, peritraumatic distress or peritraumatic dissociation, and the experience of subsequent stressful life events (5, 33).
Expectations about special, personal qualities to overcome stressful events may be the result of early research efforts that focused on “resilient children” (34–36). This changed when it became clear that resilience often derives from environmental resources. This can be seen as a reflection of the established structure-agency debate in sociology in that early researchers of development and resilience were later criticized of having been too agency centered, while ignoring any “structural forces” (37). We wonder whether this neglect of the social environment might still be present in studies on high-risk professionals. When resilience is taken as a personal trait (38) we may inadvertently pave the way for perceptions that some individuals simply do not “have what it takes” (34, 35). This is an individual-focused perspective that can easily lead to blaming the person (38).
Conceptual Clarification
When focusing on available environmental resources in adult populations, meta-analytic reviews found social support to be the single most protective factor (5, 33). Significant others can protect people who deal with stressful and potential traumatic events against traumatization. Their responding and offering of support may diminish the impact of these events. The perception that one can rely on the social connections in the environment to provide the necessary support may redefine a difficult situation as being less threatening, as well as enhance a person's sense of control, self-esteem, optimism and reinforce one's coping efforts, and/or regulation of emotions (39–43). Although at first glance the construct social support may seem to measure an environmental resource, the way social support is conceptualized (40, 44, 45) reveals that personal variables play a large role as well.
Next to this, we noticed that different high-risk occupations are often lumped together in one study, thereby ignoring differences in the environment of the distinct professions. Both concepts will be clarified underneath and will restrict the focus of this review.
Social Support: Offered vs. Perceived
Social-emotional support is a multidimensional concept. It is commonly conceptualized by three constructs; social embeddedness, enacted social support, and perceived social support (46, 47). Social embeddedness refers to the connections that individuals have with others in their social environment. Being socially connected is a central element in one's psychological sense of community. This sense of community (48–50) is associated with a wide range of positive psychological outcomes (51–53). It generally refers to a geographically defined group and to the ties that link people to their place of residence. Some researchers also applied this concept to organizations and work settings (54–57) and a few specifically to high-risk professionals (58). A function of social embeddedness is enacted support, which is conceptualized as actions that significant others perform when they offer assistance, i.e., actual social support (40, 46, 59) or supportive relationships. These naturally occuring supportive relationships are not the same as a top-down policy driven procedure such as professional support or formal peer support, which is therefore not taken into account.
Perceived social support refers to how individuals perceive and appraise enacted or actual social support (60). It is, crucially for this review, not an environmental factor as it is influenced by how the relationships, through which it is offered, are perceived (60). When two or more people interact in support, there are by default two perspectives involved: providing and receiving support (45, 46, 61). Whether or not people accept or make use of actually offered support depends upon their personal capacity to perceive it.
Different Occupations
The literature on high-risk professionals consists primarily of studies of comparable but undistinguished occupational groups, and researchers have made few attempts to distinguish subgroups within this broad category. Firefighters, police officers, emergency service, and ambulance personnel are often lumped together in one single category such as “first responders” (64, 65) or “critical occupations” (30).
The background may be that some highly influential researches, among which those of Beaton and Murphy (66) and Beaton et al. (10), took place in the United States (U.S.). In the U.S. firefighters are also trained as Emergency Medical Technicians (EMTs) or some as paramedics. As EMTs they are also called upon to render emergency medical treatments, such as cardiac arrests and other first medical aid; in one study (66) a firefighter/EMT group reported that over 60% of their “runs” were of such an emergency medical nature. In some rural (remote) areas of the U.S. firefighters are even trained as paramedics, which increased the percentage to over 80% (66). Not surprisingly, researchers found comparable outcomes among firefighters and paramedics concerning operational stressors, such as gruesome victim incidents (10), and organizational stressors, such as conflict with administration (66). Therefor they concluded that their occupational duties as well as their training and work “cultures” are comparable. To use these outcomes to group these two occupations together, however, does not seem justified as not all paramedics are also firefighters nor are all firefighter also paramedics.
We do not take into account professionals who experience incidents infrequently. For, while dealing with natural disasters and terrorist attacks, individuals and organizations may temporarily replace their traditional social structures and functions with temporary ones so that social relationships in the environment may change temporarily too (62, 63). To summarize, high-risk professionals cannot be taken as one single category, as specific environmental factors have to be taken into account. Additionally, if we intend to explore the influence of the social environment on traumatization of high-risk professionals, we should exclude studies that solely measured perceived social support.
Objectives
This systematic literature review aims to enhance insight into the social connections within the environment in which high-risk professionals are embedded (work, home, community), and the influence of these connections on the risk of traumatization. Additionally, we aim to identify supportive relationships in the professionals' environments.
Methods
Selection Criteria
Included in this review are published studies that focused on the mental health of professionals in relation to social connections or relationships at home, in their communities or their work in military, police, ambulance, and fire departments, as well as in intensive care units, operating rooms, and emergency rooms. While mainly focusing on studies about traumatization we decided to broaden our search to studies that included other mental health constructs.
Excluded from this review are studies in which samples of different occupations are grouped together, e.g., medical specialists with specialized nurses, or in which the occupational group was not specified by the researchers. Studies on professionals involved in rescue and disaster operations, and studies that focused on the effect of formal social support (e.g., debriefing or mental health treatment) are also excluded from this review. Generally, the following exclusion criteria are also applied: discussion and opinion papers; studies available merely in the form of abstracts or presentations; duplicates or papers not written in the Latin alphabet.
To improve the likelihood of identifying all relevant papers we decided not to restrict this systematic review to quantitative research only. Qualitative research may be important in identifying the role of social connections or relationships in the environment as well, as it may provide important information about phenomena such as the feeling of belonging, emotional connection, or qualitative aspects of relationships.
This review was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (67) (see Supplementary Material 1). However, this review has not been subjected to meta-analysis due to the heterogeneity of the constructs and their assessments.
Search Strategy
The research group identified the relevant scientific literature by searching, without time and without language restriction, five electronic bibliographic databases including: MEDLINE, PsycINFO, Sociological Abstracts, CINAHL, and the citation indexing service of Web of Science. These databases were last searched in January 2019.
Within each professional domain (P), papers were searched for containing at least one term or synonym from the block “mental health” (O). In the MEDLINE, PsycINFO, and Sociological Abstracts databases was the search narrowed for some professional domains (police officers and military personnel), by adding the block “social environment” (I). Major terms and their synonyms, or related terms, were derived from keywords of papers during a pilot search (see Supplementary Material 2 Major Search Terms). For an example of the used search strings for all professional domains in two of the databases, see Supplementary Material 3. (An outline of the full used search terms and search strings for all occupational groups and all five databases is available on request).
Study Selection
The flow charts documenting the selection process for each professional group can be viewed in Figure 1. After duplicates were removed, titles and abstracts were screened for this first selection process by two reviewers (RG and MV). Disagreements between them were resolved by a third reviewer (EV). In the second selection process full texts of all potential relevant studies were read by RG, MV, and EV. Doubts between these authors regarding article eligibility, or key criteria during extraction were resolved through discussion with the remaining author (JD).
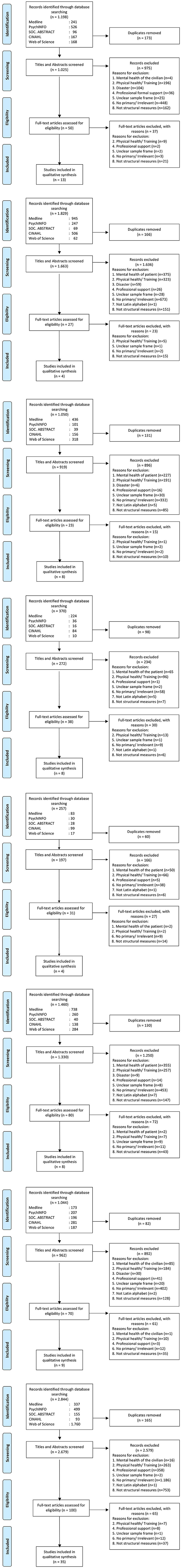
Figure 1. PRISMA-based Flow-Charts of each occupational group. From Moher et al. (67).
During the second selection process we decided to sharpen the selection by excluding all studies which did not measure or address the outcome of any mental health constructs of the professional but focused on job satisfaction or commitment toward the organization's mission, “end-product” or service. Though job satisfaction might be expected to correlate positively with, for example, a sense of community in the workplace, job satisfaction is not a necessary, nor a sufficient condition for the experience of a sense of belonging or community at work (56).
Data Extraction and Synthesis
For each included study we extracted the following data: authors, year of publication, country, journal, study design, professional group (sample characteristics, context), measured constructs and measurements. Risk of bias (RoB) of individual studies is assessed with a tool for cross-sectional studies and surveys (68). For a full list of eligible articles of each professional group, see Supplementary Table 1.
To give an overall impression of the studies included in this review, eligible articles for each professional group are summarized in the following results section.
Results
In total, 89 studies were eligible for inclusion in this review. Except seven, all were published after 2000. This section first provides an overview of the results from studies that focused on occupations in emergency services organizations starting with firefighters and ambulance paramedics, to be followed by specialist areas of nursing. Nurses in emergency rooms, operating rooms and intensive care units are discussed separately. Next, the results from studies that focused on armed services organizations are discussed, namely police officers and military personnel. Every section of an occupational group begins with a summary of quantitative findings.
In synthesizing the qualitative results per group, we first summarize studies on general embeddedness, i.e., the connections to potential supportive others in the professionals' social environment (at work, at home, or in their communities, respectively). Under this heading we also include outcomes on a sense of community and organizational belongingness, the last refers to the extent employees feel valued and respected by their organizations (69) or administrators. This section is followed by studies that focused on relevant supportive relationships in which the professional is embedded; at work with peers and supervisors, to be followed at home with family members and friends.
Firefighters
Study Characteristics
The search identified 196 articles on the mental health of firefighters, of which 13 addressed social connections in the environment (7%). All studies were quantitative, of which two included a longitudinal design. Eleven studies focused on general embeddedness under the following constructs: a sense of organizational membership, belongingness, social bonding and connection, camaraderie, organizational connectedness or disconnectedness, harassment, and workplace discrimination. Four studies (also) focused on relevant supportive relationships within the organization, i.e., supervisors/coworkers (70), relationships between employees, supervisory relations; two of these also expanded their focus to the relationships of the professional outside the fire department, i.e., family and friends.
General Embeddedness
Professional firefighters engage not only in work-related tasks but also live together for extended periods of time, usually 3-day, 24-h shifts (71, 72). A study among U.S. firefighters in six different firehouses investigating quality of life and social bonding showed that those with a low level of social bonding and connection, although low prevalent, are also more likely to report poor mental health. The instrument developed for this study was not subjected to psychometric testing. Nevertheless, it allowed the researchers to assess how frequently these firefighters engaged in activities related to social bonding. Out of these 112 firefighters 96% had a high score on these activities (73). One study (74) found that firefighters' psychological sense of (work-) community was positively impacted by their satisfaction with social support from other coworkers. Firefighters that were satisfied with the support experienced less stress with providing care to victims than those who experience low levels of support satisfaction. A lower report of thwarted belongingness (cf. disconnectedness) was associated with lower levels of PTSD symptoms (75, 76). In a small subgroup sample of wildland firefighters this feeling of disconnectedness was associated with higher suicide risk (76).
A cross-sectional study among Australian volunteer firefighters found that camaraderie—defined as a feeling of belonging, a sense of shared identity, reciprocal trust, and the strong positive bonds that exist within cohesive work groups—is a protective factor against posttraumatic stress (77). However, in a study among professional Australian firefighters organizational belongingness was not a predictor of reduction in PTSD symptoms (78) but might play a mediating role in the development of Post Traumatic Growth (PTG) (79).
Results from a study among Finnish firefighters indicated that positive interaction with coworkers may have long-term effects on work engagement and self-esteem, and consequently on (future) work ability (80).
Korean firefighters who experienced workplace discrimination had a higher likelihood of depressive symptoms (81). Among female U.S. firefighters who reported having a history of (sexual) harassment while on the job, significant higher levels of PTSD symptoms were found (82).
Relevant Supportive Relationships
Supervisors
The study among Finnish firefighters found the same results for support and positive feedback from one's supervisor (80). Spanish firefighters' emotional social support from supervisors and coworkers is positively related with the ability to face up to adversities in life (resilience), but actions from people in leadership positions denoting support, recognition, and social companionship are especially important to these firefighters (83).
Home
Huynh et al. (84) showed through a longitudinal design that support from family and friends not only protects Australian volunteer firefighters from burnout (cynicsm), but it also helps them to stay connected to volunteering.
Paramedics
Study Characteristics
Of all the identified articles on the mental health of ambulance paramedics (170), four addressed social connections in the environment (2%). All studies were quantitative studies, of which one included a longitudinal design. Two studies focused on general embeddedness, i.e., workplace belongingness and connectedness. One study focused specifically on potential supportive relationships outside the organization, i.e., with a spouse. Two studies (also) focused on relevant supportive relationships, i.e., peer and supervisor.
General Embeddedness
Workplace belongingness (i.e., a sense of organizational membership) showed to have impact on the mental health of Australian ambulance officers who experienced a traumatic event. It reduced their distress levels and enhances their ability to bounce back or recover from stress (85).
Another study amongst Canadian couples, of which one is a paramedic, investigated the social environment at home (marital interaction and coping strategies) in relation to occupational stress and burnout (emotional exhaustion and depersonalization). Significant associations were observed between paramedics' work stress, the subsequent increased rumination and interpersonal withdrawal at home. Not only the paramedics withdrew from interactions but their spouses too, which can be considered an impairment of the social resource (potential support) for the paramedic (86).
Relevant Supportive Relationships
Peers
Lewig et al. (69) used a sample of 487 rural volunteer ambulance officers in Australia to develop a better understanding of the relationship between connectedness, and mental health problems and turnover. Results showed that when volunteers feel supported by their peers they were less likely to become overly exhausted or cynical about their volunteering obligations and more likely to continue.
Supervisors
A large sample size study in Australia demonstrated the important role of support from supervisors on symptoms of common mental disorder and psychological well-being of ambulance personnel (87).
Emergency Room Nurses
Study Characteristics
The search identified 103 articles on the mental health of emergency room nurses of which eight addressed social connections in the environment (8%). All eight studies were quantitative and included a cross-sectional design, of which one longitudinal. Three of these studies focused on general embeddedness i.e., feeling supported by the hospital administration after potentially traumatic incidents or the relations with physicians. Six studies (also) focused on relevant supportive relationships within the organization i.e., supervisors and colleagues and one study included the social relationships outside the organization (i.e., family, peers and religious groups).
General Embeddedness
Two small sample size studies conducted in Ireland and Canada examined the effects of stress-related incidents in the emergency department (88, 89). The Canadian study found that interpersonal conflict with coworkers is significantly associated with PTSD symptoms (89). Both studies found that the majority of respondents reported they had received no (74%) or inadequate (20%) support from their hospital employer to help them deal with acute stress (88) or traumatic incidents (67%) (89). Considering the relatively small samples of these two studies (90 and 51), and their unclear sampling frames (as other professionals working in the emergency department were included) we should refrain from drawing specific conclusions about emergency room nurses.
Similar to other specialized nurses (90) emergency room nurses collaborate closely with physicians. In a small sample size study among 64 Irish emergency room nurses, those who perceive their relationships with physicians to be collegial (i.e., having a good relationship) feel significantly less emotionally exhausted and less depersonalized (91).
Relevant Supportive Relationships
Peers
In a large sample size study in Belgium emergency room nurses reported higher social support from colleagues than from their nurse supervisor. However, when they received support from the supervisor, nurses indicated less psychosomatic distress (92, 93). A large sample size study examined the social network integration in relation to resilience of Taiwanese emergency room nurses who had experienced verbal or physical violence by patients or their families. In this research resilience is regarded as a process of adapatation to adverisity or stressful events, and it helps individuals cope with challenges in life and recover from trauma. The results showed that among all measured forms of social network (i.e., family, peers, and religious groups) only peer support enhanced resilience among abused nurses (94).
In contrast, another large sample size study among emergency department personnel, compared 356 doctors with 279 nurses, and showed that low social support among coworkers was associated with poor mental health only among doctors, but not among nurses (95). However, the sample frames of the two Belgian studies are unclear since 50–58% of these emergency room nurses also functioned as paramedics in ambulance care.
Supervisors
In the Belgian study mentioned above, lack of social support from the nurse supervisor for emergency room nurses was referenced as an important predictor of psychosomatic distress (92, 93). In Spain, low social support from nurse supervisors for emergency room nurses was associated with high scores of emotional exhaustion (95).
In a study among 11 emergency departments in Belgium, 292 emergency room nurses were studied on the association between social support from supervisors and nurses' turnover intention. This association was only significant among female nurses whose turnover was higher due to emotional exhaustion (96).
Operating Room Nurses: Perioperative Nurses and Nurse Anesthetists
Work in operating rooms differs from other clinical areas. While nurses in other settings focus their attention on direct patient care and planning, operating room nurses provide direct patient care only briefly prior to anesthesia. Frequently, sometimes up to 8 or 12 continuous hours, time is spent one-to-one with a physician while performing a surgery. Compared to nurses on medical wards, operating room nurses do not experience stress as much from involvement with patients and their families, but mostly from interacting with physicians (97). In fact, here interpersonal relationships are the most frequent source of stress (97, 98).
In operating rooms two nurse specialties are distinguished: a perioperative nurse in surgical teams, and a nurse supporting the anesthesia team. In a study among Finnish operating room nurses, workplace culture was investigated through the constructs of job stress, job satisfaction, and practice environment in the operating room. The demands and content of the work of anesthesia or perioperative specialties seem to determine differences in workplace cultures and in particular the experience of job stress (99).
Study results for perioperative nurses and anesthesia nurses will be summarized separately below.
Perioperative Nurses
Study Characteristics
Of all the identified articles on the mental health of nurses working in surgical teams (21), eight addressed social connections in the environment (38%). Five studies were quantitative, two qualitative, and one was mixed. Six studies focused on general embeddedness, i.e., social networks, relationship with the surgeon, workplace violence, and bullying. Two studies focused on relevant supportive relationships within the organization, i.e., coworkers, supervisors, or nursing manager.
General Embeddedness
Social connections may not only diminish the impact of job-related stress but could also be a source of stress. The operating room is a unit in the hospital where bullying seems to be common practice (100, 101), though it does not automatically lead to low job satisfaction (102, 103). A study among perioperative personnel in two different hospitals in the U.S. indicated that personnel did not perceive this disruptive behavior as problematic, yet the results do show a positive correlation with emotional exhaustion (102). In this study, however, there may be a potential source of non-response bias (29% response rate) and unclear sampling (53% surgical technologists, 45% nurse). In a large sample size study among different nursing units in Korea, physicians in the operating rooms were reported as the most frequent perpetrators of verbal abuse and sexual harassment (104). A qualitative study in Canada focused on the contribution of specific factors, such as an aura of seclusion, an inability to leave and hierarchy, to physician-perpetrated abuse in the operating room. All of these factors fostered a setting conducive to abuse without consequences. The (10) interviewed operating room nurses experienced negative psychological and social health effects from the abuse (105).
A qualitative study from the U.K. found that (predominantly female) nurses perceive “looking after surgeons” to be one of their stressful responsibilities. This “hostess” role is a kind of emotional labor but performed with coworkers rather than patients. Seventeen interviewed operating room nurses felt this emotional labor was necessary to minimize emotional disturbances of the surgeons (106).
Relevant Supportive Relationships
Peers
Members of surgical teams depend on each other for the performance of their functions. In a large sample size Australian study, Gillespie (107) measured the degree of collaboration and support among nurses in the operating room in relation to their resilience, and found it to be limited and not to be a statistically significant explanatory variable of self-reported “resilient qualities” of operating room nurses. However, the total sample of 772 respondents in this study included 415 perioperative nurses, 69 nurse anesthetists and the rest were other professionals working in the operating room. We should refrain from conclusions about perioperative nurses in this study due to this unclear sampling frame.
In another Australian study, Michael (108) examined social support within the operating room following a traumatic event. The amount of social support from perioperative coworkers was higher than the amount from supervisors. Coworkers also dealt more effectively with the problem and the respondents' feelings.
Supervisors
In the same study perioperative nurses reported a low level of support from supervisors (i.e., nursing manager) following a traumatic event (108).
Nurse Anesthetists
Study Characteristics
Of all the identified articles on the mental health of nurses working in anesthesia teams (24), four addressed social connections in the environment (17%). Two studies were quantitative, one qualitative and one is mixed. All four studies focused on general embeddedness, i.e., social networks, interpersonal relations or conflicts, workplace aggression, and incivility. No research is found on relevant supportive relationships in the environment in which the nurse anesthetist is embedded.
General Embeddedness
The direct supervisor of the nurse anesthetists in the operating room is not the surgeon but the anesthesiologist. Nurse anesthetists and anesthesiologists have many overlapping skills. Therefore, the allocation of work tasks can be a source of conflict and interpersonal stress (98, 109, 110).
Among U.S. nurse anesthetists, interpersonal work relationships caused more stress than any of the other perceived job stressors, such as workload or production pressure (111). Nurse anesthetists' workplace stress was significantly correlated with experiences of aggression (80%) by physician supervisors (58.4%) and coworkers (36.6%) (112). For Dutch nurse anesthetists, conflicts with coworkers were strongly related to job stress and the intention to leave (109).
Elmblad et al. (113) focused their research on the effects of incivility, i.e., rude or disruptive behaviors, as well as on distress and burnout. They define burnout as a state of prolonged physical and psychological exhaustion, which is perceived as related to the person's work. The researchers found a direct and statistically significant relationship between workplace incivility and burnout. The sources of incivility affecting nurse anesthetists in the U.S. are general hospital employees, patients, visitors, and physicians; a lesser prevalent source of incivility were other nurse anesthetists. The least prevalent source of incivility were direct supervisors (i.e., the person she reports to most frequently) of nurse anesthetists. It is unclear from the used questionnaire in this study if the physician mentioned was the surgeon or the anesthetist (or both), and if the direct supervisor was the nurse manager or anesthetist. A direct and statistically significant, relationship existed between workplace incivility and burnout.
Intensive Care Nurses
Study Characteristics
The search identified 199 articles on the mental health of intensive care nurses, of which eight addressed social connections in the environment (4%). Six studies were quantitative and two were qualitative. Six out of these eight studies focused on general embeddedness, i.e., social work environment, communication (114) cultural context and the relationship with physicians. Three studies focused on relevant supportive relationships within the organization, i.e., supervisors (115, 116) and peers (115). One study also expanded its focus on supportive relationships at home (115).
General Embeddedness
A small sample size study in the U.S. compared nurses in two general medical units with those in two ICUs. The study showed that psychological symptoms were not affected by the major patient-care activity of a given unit, but rather by social system variables, including peer cohesion and staff support (117). Mrayyan (118) conducted a larger sample size comparative study on job stressors in ICUs and wards. ICU nurses reported higher numbers of conflicts with physicians than the general wards nurses. Mahon (119) examined through a critical ethnography the cultural context of a Canadian Pediatric Intensive Care Unit (PICU). The lack of respect shown to nurses by hospital administrators appears to be one of the major sources of stress. Many actions or demands, such as “floating” nurses to other units while the PICU was quiet, appeared to undermine the sense of team and belonging, which is fundamental to PICU nurses' retention. An institutional ethnography, also conducted in a Canadian PICU, showed that negotiating patient care within the hierarchy (from a lower position than the physicians) was a consistent source of stress for the nurses (120). Brazilian nurses who have poor relationships with physicians, experienced higher levels of emotional exhaustion. This negatively influences their perception of quality of care, job satisfaction and intention to stay in their jobs (121).
Relevant Supportive Relationships
Peers
Mrayyan (118) found that ICU nurses score higher on social emotional support behaviors toward others nurses experiencing stressful situations than nurses working at wards.
Police Officers
Study Characteristics
Of all the identified articles on the mental health of police officers (172), nine addressed social connections in the environment (5%). Eight studies were quantitative, of which one included a longitudinal design, and one study was qualitative. Eight of the nine studies focused on general embeddedness, i.e., relationships with coworkers (122) social capital at work and at home, social network, marital functioning (123) workplace incivility, bullying (124) and social undermining. Two studies (also) focused on relevant supportive relationships whitin the organization, i.e., peers and supervisors.
General Embeddedness
A study among U.S. police officers showed that good and effective cooperation between units as well as trust in work partners (i.e., “social capital within a work environment”) can lower the negative aspects of stress. Even when officers reported high levels of potentially traumatic events, strain levels did not increase if there was a certain degree of social capital within the police unit. The latter was the most significant factor in reducing the negative effect of stress, closely followed by “stability at home” (i.e., support from family or friends and talking about problems with spouse, relatives or friends) (125). Among Nigerian police officers, lower scores on “workplace social capital” were related to anxiety and depression symptoms (126).
Adams and Buck (127) compared the stressfulness of interactions with civilians and suspects (both outsiders), with workplace incivility from coworkers and supervisors (both insiders) among US police officers. It turned out that the average stress arising from insiders was similar to those from outsiders. Both stressors were positively related to psychological distress, emotional exhaustion, and turnover intention. A study among Slovenian police officers focused on behavior intended to hinder, over time, the ability to establish and maintain positive interpersonal relationships, work-related success, and favorable reputation. This social undermining by coworkers and/or supervisors was significantly, negatively, linked with employee mental health (128).
A large network (at work, home and/or community), in terms of frequency of contact and level of satisfaction, was not sufficient to prevent the development of burnout (emotional exhaustion, depersonalization and lack of accomplishment) among Mexican traffic police officers (129).
Relevant Supportive Relationships
Supervisors
The researchers of the previously mentioned study among Slovenian police officers found that the negative effects from social undermining by coworkers could only modestly be compensated by social support from supervisors. When supervisors were the source of undermining, as well as the source of social support, police officers report significantly more psychosomatic symptoms (128).
Buunk and Verhoeven (130) conducted a fine-grained analysis of stress-reducing features of daily social interactions, over 1 week, among Dutch police personnel. They found the degree of intimate support provided by supervisors closely related to less stress at the end of the workday.
Peers
Buunk and Verhoeven also found that a higher frequency in social interactions with peers (labeled as “intimate support”) was linked with more reported negative affect at the end of the day (130).
Military Personnel
Study Characteristics
Of all the articles found on the mental health of military personnel (825), 35 addressed social connections in the environment (4%). All studies were quantitative, except for two qualitative studies. The majority (33) of these studies focused on general embeddedness under the following construct; unit cohesion (131) or group (132) cohesion (133) camaraderie (134) family cohesion or family conflict, a sense of community or belongingness (135–137) social connectedness (138) community integration or social network (139). Three studies focused on relevant supportive relationships, two inside the organization (i.e., from the supervisor) and one included non-military relationships (friends and family).
General Embeddedness
A sense of belonging may protect service members from depression and posttraumatic stress, starting from pre-deployment preparations through deployment and post-deployment adjustment (140). The term deployment is used by the military to describe sending troops to carry out a combat, peacekeeping, or humanitarian mission. Among Air Force men above the age of 29 years, who have been exposed to high levels of combat, a strong sense of belonging protected against suicidal ideation (141).
In military studies, unit or group cohesion was a topic of considerable interest and often used interchangeably with social support. However, unit cohesion is a multidimensional construct. It may include not only interpersonal aspects, such as emotional bonds among unit members (i.e., social cohesion), but also task-oriented aspects, such as shared commitment to a goal or mission (i.e., task cohesion) (142). Research results among personnel of the Canadian Army and Navy Forces highlighted the importance of this distinction. Where task cohesion seems to be critical to the operational effectiveness, social cohesion was related to reduced psychological symptomatology (143).
This finding was confirmed in a study among Australian military personnel deployed in the Middle East. Respondents with low unit (social) cohesion had higher odds of PTSD symptoms compared with those reporting high unit cohesion (144). Among U.S. Army soldiers, the confirmed link between exposure to stressors before deployment and PTSD symptoms after deployment (33) appears to be weaker when unit support was high (145). In contrast, another study found unit cohesion not to be related to post-deployment mental health outcomes. However, when an individual perceived their unit cohesion as lower compared to other members of the same unit, there was a significant association with post-deployment PTSD and depression symptoms (146).
Contrary to these findings, a study among Vietnam combat veterans found that low to moderate unit cohesion is related to lower reported rates of PTSD symptoms. Very high levels of unit cohesion was associated with higher than expected levels of PTSD symptoms (147).
Among regular U.K. military personnel, comradeship (i.e., “I felt a sense of comradeship between myself and other people in my unit”) was associated with greater alcohol abuse (148). Comparable results were found among U.S. Marines where higher unit cohesion was associated with a higher likelihood of alcohol misuse (146). Problematic alcohol use is well-known to be linked to posttraumatic stress reactions (149).
Among female service members and veterans, sexual harassment (by unit leaders or other unit members) during deployment was more highly associated with post-deployment PTSD symptoms (150) than combat exposure (151). One study concluded that it is not the culture or unit cohesion but the tolerance of sexism in the organization that accounts for the levels of harassment (152).
The following studies focused on the mental health of military personnel post-deployment (i.e., veterans). In most U.S. studies the status of “veteran” includes personnel who returned from deployment, who still serve and may be deployed again. However, in Europe the status of “veteran” is defined as former defense personnel (153).
U.S. army soldiers with higher than average unit cohesion during deployment and with post-deployment community support, had significantly lower post-deployment PTSD scores (154) and fewer suicidal thoughts (155). Formerly deployed U.S. veterans with low postemployment support scored high on PTSD and suicidality (156). A study among U.S. veterans returning from Middle East underscores this effect of post-deployment social support and reintegration on mental health symptoms (150).
In a qualitative study in Britain, 25 World War II veterans were interviewed about their social support experiences both during the war as well as during the years afterwards. There was a clear distinction: Wives and families generally provided practical and emotional help that is not associated directly with the traumatic memories, whereas comradeship (with fellow soldiers of the same generation) and veterans' associations provided the means to process traumatic experiences (157).
Among U.S. female active duty members who experienced social conflict during post-deployment, some of the benefits that social support might provide, were canceled out. Instead, more symptoms of PTSD and anxiety were reported (158). A lack of family cohesion, the degree to which family members are helpful and supportive, emerged as a consistent predictor of PTSD diagnosis for U.S. troops who served in the Persian Gulf War (159). Israeli soldiers who returned after war, and who were diagnosed with delayed PTSD, are less socially integrated in their community. That is, they regard their ties to their families as weak or non-existent (160). Later studies confirmed this notion and found that their family environment was less cohesive than those of the control groups (161, 162).
When service leavers of the U.K. military maintain a social network in which most members are still in the military, or if they belong to fewer social organizations outside the military and participate in fewer social activities outside work, higher levels of mental problems were found (163). Among United Nation soldiers who served in former Yugoslavia, the only statistically significant moderator between trauma exposure and trauma symptoms is the available support from a social network of friends and colleagues. Family and neighbors, on the contrary, seemed to be relatively unimportant as buffers (164). Unfortunately, the instrument in this study does not distinguish between friends at home vs. friends among colleagues. A large sample size study among U.S. Air Force personnel showed that PTSD symptoms were less likely when service members experienced support from family, neighbors as well as their community (165).
In contrast to these research findings, a study among U.S. millennial veterans who were transitioned back to their communities, found that a high sense of community is not a protective factor for mental health or reintegration. In fact, to the surprise of the researchers, results suggest that veterans who are connected to their local communities may be more at risk for reintegration difficulties and depression (166).
A qualitative study among Dutch combat veterans indicated that societal misrecognition may directly or indirectly contribute to moral injury (167).
Relevant Supportive Relationships
Supervisors
The association between stress exposure in prior life and PTSD symptoms after deployment (33) appeared to be weaker when U.S. Army soldiers' satisfaction with leadership is high (145). Among U.K. troops who were deployed in Iraq, perceived interest from seniors was associated with a lower probability for PTSD and other mental disorders (148).
Home
Deployed U.S. military personnel reported similar levels of support from military and non-military sources. However, only the social support from non-military friends and family had a positive influence on overall mental health (168).
Synthesized Findings
Quantitative
Of all screened studies which focused on mental health of high-risk professionals, only 2–7 percent address social connections and relationships in the environment, with the exception of the nurses in operating rooms. In the studies of operating room nurses, a higher percentage focused on social connections and relationships (nurse anesthetists 17%; perioperative nurses 38%), though the total number of studies is considerable lower (45 studies) in comparison to other high-risk professionals (i.e., from 103 studies of emergency room nurses to 825 studies of military personnel).
The eligible studies can be distinguished as follows: The majority focused on the connections in the environment, i.e., general embeddedness, whereas a minority (0–36%) focused on relevant supportive relationships among these connections.
Studies on general embeddedness focused primarily on the organization. Only a minority of studies focused on social connections outside the organization (i.e., only one study of police officers, paramedics and intensive care nurses and two studies of firefighters). In contrast, 23 out of 35 studies among soldiers and other military personnel focused on social connections (general embeddedness) outside the military organization, i.e., friends, family, and their civilian community.
Qualitative
The included studies of firefighters, paramedics, and emergency room nurses showed that being embedded in their social environment can be a protective factor against mental health problems. Peers can be an important source of support for these professionals, but relationships with supervisors seem to be more important, especially for firefighters and emergency room nurses. Studies of perioperative nurses and intensive care nurses are inconclusive as to which supportive relationships in their environment are relevant to help them deal with potentially traumatic events. However, study results show that their connections with others in their work environment can also have a negative influence on their mental health. Nurse anesthetists' connections at work can be source of stress. We found no research addressing supportive relationships in their environment. Study results for police officers are inconclusive and show that social connections in their work environment can have positive as well as negative effects on their mental health. Supervisors seem to offer relevant supportive relationships.
Lastly, military personnel studies show that being embedded in their work environment may be a protective factor against mental health disorders. Despite the general positive overtones, in some studies these connections with others are also associated with heightened PTSD levels and alcohol misuse. A supportive relationship with their supervisor can protect against PTSD. While, the study results are inconclusive about the protective effect of being embedded at home and in their community, one study also showed that supportive relationships with friends or family members have a positive effect on their overall mental health.
On a general note, several methodological challenges, such as small or unclear samples, limit the interpretation of some studies. Considerable diversity exists in the conceptualization and measurement of, for example, social support by different researchers. Unfortunately, many researchers used scales that were created post-hoc from large data sets or created their own scales without psychometric testing or development. Other researchers used single-item measures. Although most of these scales have some face validity, they almost certainly have low reliability.
Summary of Main Findings
Of the 9,047 screened studies 1,705 focused on the professionals' mental health, a minority (89) of which addressed social connections or relationships in the environment. In studies to date on high-risk professionals, the role of the social environment in relation to traumatization and lower level of mental health is still relatively neglected. A qualitative analysis of the eligible studies shows that in most occupational groups being embedded in a social environment may protect professionals against mental health problems. However, in some occupations, study results are inconclusive, and in some occupations social connections may be additional stressors or even damaging to mental health. Additionally, the source of relevant supportive relationships (peer, supervisor or friend, family member) shows great variety across and even inconsistencies within occupational groups.
Discussion
The past few decades witnessed a growing concern about professionals who are called to help and save others on a daily basis, while risking their own (mental) life. This may result in trauma-related mental health problems and ultimately in the intention to leave their profession. Trauma researchers and theorists have extensively studied independent, intervening, and moderating variables that may affect the risk of traumatization. Consequently, an enormous amount of studies resulted in considerable insight in personal factors. However, traumatization is also related to peoples' social environments. More importantly, what happens after a potentially traumatic event may have stronger impact on mental health than the experience itself, as is well-known and documented by trauma therapists (33, 169–171). Traumatized individuals often speak of the devastation caused by “secondary wounding” when they perceive that others (in their social environment) blame them, withhold validation, denigrate the severity of their experience, or otherwise contribute to the shaming of their symptoms (172, 173). Nevertheless, the majority of research still tends to limit analysis of the risk of traumatization to the individual, while largely neglecting the social context of the person, i.e., the social environment in which he is embedded.
Being socially embedded provides a lens through which people interpret daily incidents (45), and may therefore influence how potential traumatic incidents are interpreted and processed, or not. Different occupational groups may have different sources of supportive relationships, which may all in different contexts and stages be more or less effective in ameliorating stress. These sources may indeed shift over time. For example, among military personnel it can shift from work-based support (e.g., from fellow military personnel and supervisors) to post-deployment support (e.g., from family and friends) once individuals return home.
Generally, the sense of connection and belonging to an organization, home or the community, satisfies basic needs for affiliation, security and identity (174). However, social relationships are only supportive in as far as they are non-conflictual, imply care for the well-being of those involved and facilitate trust. It is of great importance for high-risk professionals, to work with the conviction that others “have your back”; to be confident of the availability and help of others, to feel assured of emotional support, especially in their most vulnerable moments.
This support is not a given in every professional group. As this review demonstrated, interpersonal relationships can be a double-edge sword, with aspects of support as well as conflict. Work relationships that generate stress are most prevalent among specialized (OR and ICU) nurses and amongst police officers as well. We might suppose that in specialized and “enclosed” hospital wards, such as ORs and ICUs, coworkers are physically in close contact to offer emotional support when they experience stressful situations. However, interpersonal conflict, disruptive behaviors and bullying seem to be common practice among these professional groups, and also create hostile work settings (100, 101). This may continue for a long time, without consequences, due to the hierarchical nature of the work setting and the (physical) inability to leave the setting. Among police officers social undermining, another negative workplace behavior, was prevalent. Among military personnel sexual harassment was found.
Negative interpersonal experiences are a considerable source of stress (61). They disrupt social networks (175) and cancel out the positive effect of social support (170). This finding can be especially detrimental for high-risk professionals, given that they often have to rely on each other and that they are an important source of social support for one another (14, 69, 80, 83, 92, 108, 145, 148, 176). A meta-analysis shows that social support deficiencies in military samples are associated with more psychological effects than among civilian samples (33).
In addition, the experience of inconsistent responses, i.e., support from as well as conflict with the same person, leads to feelings of insecurity, and lack of control, trust, and predictability in the relationship. This is also associated with higher levels of personal distress (128, 177) and might increase the risk of traumatization (178). While studying persons who frequently face potential traumatic situations, or when treating high-risks professionals with trauma-related disorders, we should not overlook these “dark sides” of social relationships (61) (p. 147).
Embeddedness, whether with supportive or damaging relationships, may be particularly salient during the organizational or professional socialization process, which in many high-risk occupations takes place during the formative late adolescent years. In emergency organizations knowledge and practices are mainly experience-based and “on-the-job training” in the existing culture is prominent. More importantly, mentors (senior colleagues and supervisors) not only teach novices professional norms, but also teach coping (or survival) strategies (179, 180) when dealing with potential traumatic events. Coping often occurs in response to stressors that arise in situations where other people are also affected and attempt to cope with them. This means that the coping actions of one person may be constrained, encouraged, or channeled by the expectations and actions of others (181). Young professionals may be particularly prone to incorporating others' coping strategy, adaptive or not, when they enter a novel environment, as they are highly motivated to belong in order to develop a social (and professional) identity. This may make them vulnerable in the long run, as adaptation is always a product of complex interactions between an individual and his social environment. A certain coping response of an individual may be considered adaptive or helpful in one environment or situation, but may be maladaptive or inappropriate in another (181). A certain social environment may promote an individual's willingness to talk about a traumatic event or, on the contrary, it may inhibit the expression of emotional problems (182–185). Likewise, people may receive social support when the social environment acknowledges a crisis, but support may be withheld in situations which are considered to be shameful (186–188). In short, even though supportive relationships are vehicles for psychological development and essential for sustaining mental health (34), they are highly dependent upon and tailored to the social environment in which a young professional is formed.
Limitations of this Review
Several limitations of our systematic literature review may provide additional research opportunities. First, stressors among high-risk professionals may involve a wide variety of factors such as conflicts between work and home, role conflicts or spill-over effects. These conflicts are typically called “inter domain” conflicts, and consequently in our study we struggled in the selection process with the question to which domain stressors should be attributed. Any comprehensive inquiry into the social context must map the professionals' larger social field to ensure that all potential relevant environmental factors are taken into account.
Second, the “sense of community” construct is often compared to constructs found in industrial-organizational psychology, e.g., organizational commitment and job satisfaction (74). Although we decided to exclude studies that solely focused on the construct “job satisfaction,” we are aware that it might be (indirectly) related to retention. Lastly, we excluded studies that solely focused on perceived social support. We maintain that perceived social support is primarily to be seen as a personal factor. However, indirectly environmental factors play a role as well as perceived social support is influenced by personal generalized assumptions that emerge from numerous previous experiences with help offered by others (61, 189, 190).
Further Research
The initial aim of this review was to explore the influence of social connections and relationships in the professionals' environment on traumatization. However, excluding studies focusing on other mental health issues while only including studies on traumatization, yielded considerably fewer eligible studies (i.e., 27 military-studies, 5 firefighters studies, 1 each for police, ICU, perioperative nurses, ER-nurses, and zero for nurse anesthetist and paramedics). An explanation may be that the construct “trauma,” or even the use of the very word “trauma,” may be stigmatized (191–195), which may direct research away from PTSD toward other mental health problems such as substance abuse, burnout, depression, or moral injury (4, 196). Some of those mental disorders have comorbidity with PTSD (7, 8). All mental health problems, however, have in common that the mental capacity to integrate stressfull events is compromised (12, 13). Being aware of the broad range of trauma-related mental health problems (7, 8) can assure that we, researchers and clinicians, do not lose sight of the fact that these professionals are frequently exposed to potentially traumatic events.
The findings and implications from studies among one specific occupational group have often been applied to other professions, such as the findings among firefighters to paramedics or other “emergency services personnel.” Take for example Australian “ambulance officers”: it is not clear whether they resemble paramedics, or whether they more closely resemble EMTs and ambulance drivers who each have different skills and training backgrounds. Variables such as the type of training received, the nature of the traumatic exposures, and the probability of repeated exposures, as well as contextual variables, especially their primary sources of support, might differ from one profession to the other. It may require careful ethnographic research to judge to what extent different high-risk professions may be comparable in terms of traumatization.
Most studies in this review have used quantitative self-report measures to investigate embeddedness, enacted social support and their related constructs. Although a perception most likely reflects reality, self-report measures are subject to a variety of biases (44, 197). The diversity of social relationships suggests that much could be gained from using diverse research methods, including qualitative approaches (198). This type of research can provide critical directions for future quantitative studies, for it may result in more meaningful hypothesis about the influence of social relationships on the risk of traumatization.
Author Contributions
RG and MV contributed conceptualization, formal analysis, and methodology and of the review. RG wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.496663/full#supplementary-material
References
1. Berger W, Coutinho ESF, Figueira I, Marques-Portella C, Luz MP, Neylan TC, et al. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1001–11. doi: 10.1007/s00127-011-0408-2
2. McFarlane AC, Williamson P, Barton CA. The impact of traumatic stressors in civilian occupational settings. J Public Health Policy. (2009) 30:311–27. doi: 10.1057/jphp.2009.21
3. Skogstad M, Skorstad M, Lie A, Conradi HS, Heir T, Weisaeth L. Work-related post-traumatic stress disorder. Occupat Med Oxford. (2013) 63:175–82. doi: 10.1093/occmed/kqt003
4. Jones S. Describing the mental health profile of first responders: a systematic review [formula: see text. J Am Psychiatr Nurses Assoc. (2017) 23:200–14. doi: 10.1177/1078390317695266
5. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. (2003) 129:52–73. doi: 10.1037/0033-2909.129.1.52
6. Sterud T, Ekeberg O, Hem E. Health status in the ambulance services: a systematic review. BMC Health Serv Res. (2006) 6:82. doi: 10.1186/1472-6963-6-82
7. American Psychological Association A Diagnostic and Statistical Manual of Mental Disorders : DSM-5. Arlington, VA: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
8. Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health. (2008) 29:115–29. doi: 10.1146/annurev.publhealth.29.020907.090847
9. Alexander D, Klein S. Ambulance personnel and critical incidents - impact of accident and emergency work on mental health and emotional well-being. Br J Psychiatry. (2001) 178:76–81. doi: 10.1192/bjp.178.1.76
10. Beaton R, Murphy S, Johnson C, Pike K, Corneil W. Exposure to duty-related incident stressors in urban firefighters and paramedics. J Trauma Stress. (1998) 11:821–8. doi: 10.1023/A:1024461920456
11. Figley CR. Compassion fatigue as secondary traumatic stress disorder. In: Figley CR, editor. An Overwies. Compassion Fatigue. New York, NY: Brunner Mazel (1995).
13. Hart O, Nijenhuis ERS, Steele K. The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization. New York, NY: WW Norton (2006).
14. Adriaenssens J, de Gucht V, Maes S. The impact of traumatic events on emergency room nurses: findings from a questionnaire survey. Int J Nurs Stud. (2012) 49:1411–22. doi: 10.1016/j.ijnurstu.2012.07.003
15. Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. (2015) 52:649–61. doi: 10.1016/j.ijnurstu.2014.11.004
16. de Boer J, van Rikxoort S, Bakker AB, Smit BJ. Critical incidents among intensive care unit nurses and their need for support: explorative interviews. Nurs Crit Care. (2014) 19:166–74. doi: 10.1111/nicc.12020
17. Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. (2007) 13:482–8. doi: 10.1097/MCC.0b013e3282efd28a
18. Gomez-Urquiza JL, De la Fuente-Solana EI, Albendin-Garcia L, Vargas-Pecino C, Ortega-Campos EM, Canadas-De la Fuente GA. Prevalence of burnout syndrome in emergency nurses: a meta-analysis. Crit Care Nurse. (2017) 37:e1–9. doi: 10.4037/ccn2017508
19. Hyman SA, Michaels DR, Berry JM, Schildcrout JS, Mercaldo ND, Weinger MB. Risk of burnout in perioperative clinicians: a survey study and literature review. Anesthesiology. (2011) 114:194–204. doi: 10.1097/ALN.0b013e318201ce9a
20. McVicar A. Workplace stress in nursing: a literature review. J Adv Nurs. (2003) 44:633–42. doi: 10.1046/j.0309-2402.2003.02853.x
21. Meeusen V, van Dam K, van Zundert A, Knape J. Job satisfaction amongst Dutch nurse anaesthetists: the influence of emotions on events. Int Nurs Rev. (2010) 57:85–91. doi: 10.1111/j.1466-7657.2009.00763.x
22. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement-burnout syndrome in critical care health-care professionals: a call for action. Chest. (2016) 150:17–26. doi: 10.1016/j.chest.2016.02.649
23. Li H, Cheng B, Zhu XP. Quantification of burnout in emergency nurses: a systematic review and meta-analysis. Int Emerg Nurs. (2018) 39:46–54. doi: 10.1016/j.ienj.2017.12.005
24. Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. (2007) 175:698–704. doi: 10.1164/rccm.200606-806OC
25. Yehuda R, Hoge CW, McFarlane AC, Vermetten E, Lanius RA, Nievergelt CM, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. (2015) 1:15057. doi: 10.1038/nrdp.2015.57
27. Linley PA, Joseph S. The positive and negative effects of disaster work: a preliminary investigation. J Loss Trauma. (2006) 11:229–45. doi: 10.1080/15325020500494186
28. Shakespeare-Finch JE, Smith SG, Gow KM, Embelton G, Baird L. The prevalence of post-traumatic growth in emergency ambulance personnel. Traumatology. (2003) 9:58–71. doi: 10.1177/153476560300900104
29. Tedeschi RG. Posttraumatic growth in combat veterans. J Clin Psychol Med Settings. (2011) 18:137–44. doi: 10.1007/s10880-011-9255-2
30. Paton D, Smith LM. Psychological trauma in critical occupations: methodological and assessment strategies. In: Traumatic Stress in Critical Occupations: Recognition, Consequences and Treatment. Springfield, IL: Charles C Thomas, Publisher (1996). p. 15–57.
31. Cooper R. The fireman: immaculate manhood. J Popular Cult. (1995) 28:139–70. doi: 10.1111/j.0022-3840.1995.1395768.x
32. Maglio MA, Scott C, Davis AL, Allen J, Taylor JA. Situational pressures that influence firefighters' decision making about personal protective equipment: a qualitative analysis. Am J Health Behav. (2016) 40:555–67. doi: 10.5993/AJHB.40.5.2
33. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. (2000) 68:748–66. doi: 10.1037/0022-006X.68.5.748
34. Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. (2000) 71:543–62. doi: 10.1111/1467-8624.00164
35. Masten AS. Ordinary magic. resilience processes in development. Am Psychol. (2001) 56:227–38. doi: 10.1037/0003-066X.56.3.227
36. Rutter M. Resilience as a dynamic concept. Dev Psychopathol. (2012) 24:335–44. doi: 10.1017/S0954579412000028
37. Mohaupt S. Review article: resilience and social exclusion. Soc Policy Soc. (2009) 8:63–71. doi: 10.1017/S1474746408004594
38. Luthar SS, Zelazo LB. Research on resilience: an integative review. In: Luthar SS, editor. Resilience and Vulnerability: Adaptation in the Context of Childhood Adversities. Cambridge/New York, NY: Cambridge University Press (2003). p. 510–49. doi: 10.1017/CBO9780511615788.023
39. Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: durkheim in the new millennium. Soc Sci Med. (2000) 51:843–57. doi: 10.1016/S0277-9536(00)00065-4
40. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
41. Hobfoll SE. Conservation of resources. a new attempt at conceptualizing stress. Am Psychol. (1989) 44:513–24. doi: 10.1037/0003-066X.44.3.513
42. Hobfoll SE. Social and psychological resources and adaptation. Rev Gen Psychol. (2002) 6:307–24. doi: 10.1037/1089-2680.6.4.307
43. Sippel LM, Pietrzak RH, Charney DS, Mayes LC, Southwick SM. How does social support enhance resilience in the trauma-exposed individual? Ecol Soc. (2015) 20:10. doi: 10.5751/ES-07832-200410
44. Flannery RB. Social support and psychological trauma: a methodological review. J Trauma Stress. (1990) 3:593–611. doi: 10.1002/jts.2490030409
45. Thoits PA. Conceptual, methodological, and theoretical problems in studying social support as a buffer against life stress. J Health Soc Behav. (1982) 23:145–59. doi: 10.2307/2136511
46. Barrera M. Distinctions between social support concepts, measures, and models. Am J Community Psychol. (1986) 14:413–45. doi: 10.1007/BF00922627
47. Gottlieb BH, Bergen AE. Social support concepts and measures. J Psychosom Res. (2010) 69:511–20. doi: 10.1016/j.jpsychores.2009.10.001
48. Hill JL. Psychological sense of community: suggestions for future research. J Community Psychol. (1996) 24:431–8. doi: 10.1002/(SICI)1520-6629(199610)24:4<431::AID-JCOP10>3.0.CO;2-T
49. McMillan DW, Chavis DM. Sense of community: a definition and theory. J Community Psychol. (1986) 14:6–23. doi: 10.1002/1520-6629(198601)14:1<6::AID-JCOP2290140103>3.0.CO;2-I
50. McMillan DW. Sense of community. J Commun Psychol. (1996) 24:315–25. doi: 10.1002/(SICI)1520-6629(199610)24:4<315::AID-JCOP2>3.0.CO;2-T
51. Davidson WB, Cotter PR. The relationship between sense of community and subjective well-being: a first look. J Commun Psychol. (1991) 19:246–53. doi: 10.1002/1520-6629(199107)19:3<246::AID-JCOP2290190308>3.0.CO;2-L
52. Peterson NA, Speer PW, McMillan DW. Validation of A brief sense of community scale: confirmation of the principal theory of sense of community. J Commun Psychol. (2008) 36:61–73. doi: 10.1002/jcop.20217
53. Prezza M, Amici M, Roberti T, Tedeschi G. Sense of community referred to the whole town: its relations with neighboring, loneliness, life satisfaction, and area of residence. J Commun Psychol. (2001) 29:29–52. doi: 10.1002/1520-6629(200101)29:1<29::AID-JCOP3>3.0.CO;2-C
54. Cockshaw WD, Shochet IM. The link between belongingness and depressive symptoms: an exploration in the workplace interpersonal context. Austr Psychol. (2010) 45:283–9. doi: 10.1080/00050061003752418
55. Cockshaw WD, Shochet IM, Obst PL. General belongingness, workplace belongingness, and depressive symptoms. J Commun Appl Soc Psychol. (2013) 23:240–51. doi: 10.1002/casp.2121
56. Klein KJ, D'Aunno TA. Psychological sense of community in the workplace. J Commun Psychol. (1986) 14:365–77. doi: 10.1002/1520-6629(198610)14:4<365::AID-JCOP2290140405>3.0.CO;2-H
57. Pretty GMH, McCarthy ME, Catano VM. Psychological environments and burnout: gender considerations within the corporation. J Organiz Behav. (1992) 13:701–11. doi: 10.1002/job.4030130706
59. Thoits PA. Stress, coping, and social support processes: where are we? What next? J Health Soc Behav. (1995) Spec No:53–79. doi: 10.2307/2626957
60. Sarason IG, Sarason BR, Pierce GR. Social support: the search for theory. J Soc Clin Psychol. (1990) 9:133–47. doi: 10.1521/jscp.1990.9.1.133
61. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–61. doi: 10.1177/0022146510395592
62. Drabek TE, McEntire DA. Emergent phenomena and the sociology of disaster: lessons, trends and opportunities from the research literature. Disaster Prev Manag. (2003) 12:97–112. doi: 10.1108/09653560310474214
63. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service workers. Sex Relat Ther. (2001) 16:261–7. doi: 10.1080/14681990124457
64. Benedek DM, Fullerton C, Ursano RJ. First responders: mental health consequences of natural and human-made disasters for public health and public safety workers. Annu Rev Public Health. (2007) 28:55–68. doi: 10.1146/annurev.publhealth.28.021406.144037
65. Marmar CR, McCaslin SE, Metzler TJ, Best S, Weiss DS, Fagan J, et al. Predictors of posttraumatic stress in police and other first responders. In: The Psychobiology of Post-Traumatic Stress Disorder Malden. Malden: Blackwell Publishing. (2006). p. 1–18. doi: 10.1196/annals.1364.001
66. Beaton RD, Murphy SA. Sources of occupational stress among firefighter/EMTs and firefighter/paramedics and correlations with job-related outcomes. Prehosp Disaster Med. (1993) 8:140–50.
67. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
68. Moore S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute (2017).
69. Lewig KA, Xanthopoulou D, Bakker AB, Dollard MF, Metzer JC. Burnout and connectedness among Australian volunteers: a test of the job demands-resources model. J Vocat Behav. (2007) 71:429–45. doi: 10.1016/j.jvb.2007.07.003
70. Wong J, Lin J, Liu S, Wan T. Fireman's job stress: Integrating work/non-work conflict with job demand-control-support model. Eur Rev Appl Psychol Revue Eur Psychol Appl. (2014) 64:83–91. doi: 10.1016/j.erap.2013.12.002
71. Beaton RD, Murphy SA, Pike KC, Corneil W. Social support and network conflict in firefighters and paramedics. West J Nurs Res. (1997) 19:297–313. doi: 10.1177/019394599701900303
72. Landen SM, Wang CDC. Adult attachment, work cohesion, coping, and psychological well-being of firefighters. Counsel Psychol Q. (2010) 23:143–62. doi: 10.1080/09515071003776028
73. Carey MG, Al-Zaiti SS, Dean GE, Sessanna L, Finnell DS. Sleep problems, depression, substance use, social bonding, and quality of life in professional firefighters. J Occupat Environ Med. (2011) 53:928–33. doi: 10.1097/JOM.0b013e318225898f
74. Cowman SE, Ferrari JR, Liao-Troth M. Mediating effects of social support on firefighters' sense of community and perceptions of care. J Commun Psychol. (2004) 32:121–6. doi: 10.1002/jcop.10089
75. Stanley IH, Hom MA, Chu C, Dougherty SP, Gallyer AJ, Spencer-Thomas S, et al. Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: a multistudy investigation. Psychol Serv. (2018) 16:543–55. doi: 10.1037/ser0000240
76. Stanley IH, Hom MA, Gai AR, Joiner TE. Wildland firefighters and suicide risk: examining the role of social disconnectedness. Psychiatry Res. (2018) 266:269–74. doi: 10.1016/j.psychres.2018.03.017
77. Tuckey MR, Hayward R. Global and occupation-specific emotional resources as buffers against the emotional demands of fire-fighting. Appl Psychol. (2011) 60:1–23. doi: 10.1111/j.1464-0597.2010.00424.x
78. Armstrong D, Shakespeare-Finch J, Shochet I. Predicting post-traumatic growth and post-traumatic stress in firefighters. Aust J Psychol. (2014) 66:38–46. doi: 10.1111/ajpy.12032
79. Armstrong D, Shakespeare-Finch J, Shochet I. Organizational belongingness mediates the relationship between sources of stress and posttrauma outcomes in firefighters. Psychol Trauma. (2015) 8:343–7. doi: 10.1037/tra0000083
80. Airila A, Hakanen JJ, Schaufeli WB, Luukkonen R, Punakallio A, Lusa S. Are job and personal resources associated with work ability 10 years later? The mediating role of work engagement. Work Stress. (2014) 28:87–105. doi: 10.1080/02678373.2013.872208
81. Lee N, Kim J, Kim JY, Kim S. Association between workplace discrimination and depressive symptoms among firefighters in South Korea. Am J Ind Med. (2018) 61:741–50. doi: 10.1002/ajim.22876
82. Hom MA, Stanley IH, Spencer-Thomas S, Joiner TE. Women firefighters and workplace harassment: associated suicidality and mental health sequelae. J Nerv Ment Dis. (2017) 205:910–17. doi: 10.1097/NMD.0000000000000759
83. Bernabé M, Botia JM. Resilience as a mediator in emotional social support's relationship with occupational psychology health in firefighters. J Health Psychol. (2016) 21:1778–86. doi: 10.1177/1359105314566258
84. Huynh JY, Xanthopoulou D, Winefield AH. Social support moderates the impact of demands on burnout and organizational connectedness: a two-wave study of volunteer firefighters. J Occup Health Psychol. (2013) 18:9–15. doi: 10.1037/a0030804
85. Shakespeare-Finch J, Daley E. Workplace belongingness, distress, and resilience in emergency service workers. Psychol Trauma Theory Res Pract Policy. (2017) 9:32–35. doi: 10.1037/tra0000108
86. King DB, DeLongis A. When couples disconnect: rumination and withdrawal as maladaptive responses to everyday stress. J Fam Psychol. (2014) 28:460–9. doi: 10.1037/a0037160
87. Petrie K, Gayed A, Bryan BT, Deady M, Madan I, Savic A, et al. The importance of manager support for the mental health and well-being of ambulance personnel. PLoS ONE. (2018) 13:e0197802. doi: 10.1371/journal.pone.0197802
88. Healy S, Tyrrell M. Stress in emergency departments: experiences of nurses and doctors. Emerg Nurse. (2011) 19:31–7. doi: 10.7748/en2011.07.19.4.31.c8611
89. Laposa JM, Alden LE, Fullerton LM. Work stress and posttraumatic stress disorder in ED nurses/personnel. J Emerg Nurs. (2003) 29:23–8. doi: 10.1067/men.2003.7
90. Chaboyer WP, Patterson E. Australian hospital generalist and critical care nurses' perceptions of doctor-nurse collaboration. Nurs Health Sci. (2001) 3:73–9. doi: 10.1046/j.1442-2018.2001.00075.x
91. O'Mahony N. Nurse burnout and the working environment. Emerg Nurse. (2011) 19:30–7. doi: 10.7748/en2011.09.19.5.30.c8704
92. Adriaenssens J, De Gucht V, Van Der Doef M, Maes S. Exploring the burden of emergency care: predictors of stress-health outcomes in emergency nurses. J Adv Nurs. (2011) 67:1317–28. doi: 10.1111/j.1365-2648.2010.05599.x
93. Adriaenssens J, De Gucht V, Maes S. Causes and consequences of occupational stress in emergency nurses, a longitudinal study. J Nurs Manag. (2015) 23:346–58. doi: 10.1111/jonm.12138
94. Hsieh HF, Hung YT, Wang HH, Ma SC, Chang SC. Factors of resilience in emergency department nurses who have experienced workplace violence in Taiwan. J Nurs Scholarsh. (2015) 48:23–30. doi: 10.1111/jnu.12177
95. Escribà-Agüir V, Pérez-Hoyos S. Psychological well-being and psychosocial work environment characteristics among emergency medical and nursing staff. Stress Health. (2007) 23:153–60. doi: 10.1002/smi.1131
96. Bruyneel L, Thoelen T, Adriaenssens J, Sermeus W. Emergency room nurses' pathway to turnover intention: a moderated serial mediation analysis. J Adv Nurs. (2017) 73:930–42. doi: 10.1111/jan.13188
97. Cronin-Stubbs D, Brophy EB. Burnout: can social support save the psych nurse? J Psychosoc Nurs Ment Health Serv. (1985) 23:8–13.
98. Cavagnaro MA. A comparison study of stress factors as they affect CRNAs. AANA J. (1983) 51:290–4.
99. Eskola S, Roos M, McCormack B, Slater P, Hahtela N, Suominen T. Workplace culture among operating room nurses. J Nurs Manag. (2016) 24:725–34. doi: 10.1111/jonm.12376
100. Lee YJ, Bernstein K, Lee M, Nokes KM. Bullying in the nursing workplace: applying evidence using a conceptual framework. Nurs Econ. (2014) 32:255–67.
101. Salin D. Ways of explaining workplace bullying: a review of enabling, motivating and precipitating structures and processes in the work environment. Hum Relat. (2003) 56:1213–32. doi: 10.1177/00187267035610003
102. Chipps E, Stelmaschuk S, Albert NM, Bernhard L, Holloman C. Workplace bullying in the OR: results of a descriptive study. AORN J. (2013) 98:479–93. doi: 10.1016/j.aorn.2013.08.015
103. Dunn H. Horizontal violence among nurses in the operating room. AORN J. (2003) 78:977–88. doi: 10.1016/S0001-2092(06)60588-7
104. Park M, Cho S, Hong H. Prevalence and perpetrators of workplace violence by nursing unit and the relationship between violence and the perceived work environment. J Nurs Scholarship. (2015) 47:87–95. doi: 10.1111/jnu.12112
105. Higgins BL, MacIntosh J. Operating room nurses' perceptions of the effects of physician-perpetrated abuse. Int Nurs Rev. (2010) 57:321–7. doi: 10.1111/j.1466-7657.2009.00767.x
106. Timmons S, Tanner J. Operating theatre nurses: emotional labour and the hostess role. Int J Nurs Pract. (2005) 11:85–91. doi: 10.1111/j.1440-172X.2005.00507.x
107. Gillespie BM, Chaboyer W, Wallis M, Grimbeek P. Resilience in the operating room: developing and testing of a resilience model. J Adv Nurs. (2007) 59:427–38. doi: 10.1111/j.1365-2648.2007.04340.x
108. Michael R. Caring for the carers – myth or reality? Social and personal resources amongst perioperative nurses following work related trauma. ACORN. (2002) 15:14–19.
109. van Beuzekom M, Akerboom S, Boer F, Dahan A. Influence of latent risk factors on job satisfaction, job stress and intention to leave in anaesthesia teams: a cross-sectional survey. Eur J Anaesthesiol. (2013) 30:222–8. doi: 10.1097/EJA.0b013e32835d2db2
110. Kendrick P. Comparing the effects of stress and relationship style on student and practicing nurse anesthetists. AANA J. (2000) 68:115–22.
111. Perry TR. The certified registered nurse anesthetist: occupational responsibilities, perceived stressors, coping strategies, and work relationships. AANA J. (2005) 73:351–6.
112. Sakellaropoulos A, Pires J, Estes D, Jasinski D. Workplace aggression: assessment of prevalence in the field of nurse anesthesia. AANA J. (2011) 79(4 Suppl):S51–7.
113. Elmblad R, Kodjebacheva G, Lebeck L. Workplace incivility affecting CRNAs: a study of prevalence, severity, and consequences with proposed interventions. AANA J. (2014) 82:437–45.
114. Vermeir P, Blot S, Degroote S, Vandijck D, Mariman A, Vanacker T, et al. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: a questionnaire study. Intensive Crit Care Nurs. (2018) 48:21–7. doi: 10.1016/j.iccn.2018.07.001
115. Norbeck JS. Types and sources of social support for managing job stress in critical care nursing. Nurs Res. (1985) 34:225–30. doi: 10.1097/00006199-198507000-00011
116. Klopper HC, Coetzee SK, Pretorius R, Bester P. Practice environment, job satisfaction and burnout of critical care nurses in South Africa. J Nurs Manag. (2012) 20:685–95. doi: 10.1111/j.1365-2834.2011.01350.x
117. Mohl PC, Denny NR, Mote TA, Coldwater C. Hospital unit stressors that affect nurses: primary task vs social factors. Psychosomatics. (1982) 23:366–74. doi: 10.1016/S0033-3182(82)73399-7
118. Mrayyan MT. Job stressors and social support behaviors: comparing intensive care units to wards in Jordan. Contemp Nurse. (2009) 31:163–75. doi: 10.5172/conu.673.31.2.163
119. Mahon PR. A critical ethnographic look at paediatric intensive care nurses and the determinants of nurses' job satisfaction. Intensive Crit Care Nurs. (2014) 30:45–53. doi: 10.1016/j.iccn.2013.08.002
120. McGibbon E, Peter E, Gallop R. An institutional ethnography of nurses' stress. Qual Health Res. (2010) 20:1353–78. doi: 10.1177/1049732310375435
121. Panunto MR, Guirardello Ede B. Professional nursing practice: environment and emotional exhaustion among intensive care nurses. Rev Lat Am Enfermagem. (2013) 21:765–72. doi: 10.1590/S0104-11692013000300016
122. Pelegrini A, Cardoso TE, Claumann GS, Pinto AdA, Gomes Felden EP. Perception of work conditions and occupational stress among civil and military police officers of special operations units. Cadernos brasileiros de terapia ocupacional-Brazilian. J Occupat Ther. (2018) 26:423–30. doi: 10.4322/2526-8910.ctoAO1160
123. Tuttle BM, Giano Z, Merten MJ. Stress spillover in policing and negative relationship functioning for law enforcement marriages. Fam J. (2018) 26:246–52. doi: 10.1177/1066480718775739
124. Brunetto Y, Xerri M, Shacklock K, Farr-Wharton B, Farr-Wharton R. Management, bullying and the work outcomes of Australian paramilitary. Aust N Z J Criminol. (2017) 50:341–59. doi: 10.1177/0004865816647429
125. Gachter M, Savage DA, Torgler B. The relationship between stress, strain and social capital. Policing. (2011) 34:515–40. doi: 10.1108/13639511111157546
126. Ojedokun O, Balogun SK. The costs of policing: psychosocial capital and mental health outcomes in a Nigeria police sample. Span J Psychol. (2015) 18:E78. doi: 10.1017/sjp.2015.76
127. Adams GA, Buck J. Social stressors and strain among police officers: it's not just the bad guys. Crim Justice Behav. (2010) 37:1030–40. doi: 10.1177/0093854810374282
128. Duffy MK, Ganster D, Pagon M. Social undermining in the workplace. Acad Manag J. (2002) 45:331–51. doi: 10.5465/3069350
129. Beltrán CA, Moreno MP, Estrada JGS, López TMT, Rodríguez MGA. Social support, burnout syndrome and occupational exhaustion among Mexican traffic police agents. Spanish J Psychol. (2009) 12:585–92. doi: 10.1017/S1138741600001955
130. Buunk BP, Verhoeven K. Companionship and support at work: a microanalysis of the stress-reducing features of social interaction. Basic Appl Soc Psychol. (1991) 12:243–58. doi: 10.1207/s15324834basp1203_1
131. Luciano MT, McDevitt-Murphy ME. Posttraumatic stress and physical health functioning: moderating effects of deployment and postdeployment social support in OEF/OIF/OND veterans. J Nerv Ment Dis. (2017) 205:93–98. doi: 10.1097/NMD.0000000000000571
132. Milgram NA, Orenstein R, Zafrir E. Stressors, personal resources, and social supports in military performance during wartime. Mil Psychol. (1989) 1:185–99. doi: 10.1207/s15327876mp0104_1
133. Williams J, Brown JM, Bray RM, Goodell EMA, Olmsted KR, Adler AB. Unit cohesion, resilience, and mental health of soldiers in basic combat training. Mil Psychol. (2016) 28:241–50. doi: 10.1037/mil0000120
134. Nevarez MD, Yee HM, Waldinger RJ. Friendship in war: camaraderie and prevention of posttraumatic stress disorder prevention. J Trauma Stress. (2017) 30:512–20. doi: 10.1002/jts.22224
135. Huang K, Tzeng D, Lin C, Chung W. Interpersonal–psychological theory, alexithymia, and personality predict suicide ideation among maladjusted soldiers in Taiwan. Suicide Life Threat Behav. (2017) 47:603–11. doi: 10.1111/sltb.12315
136. Monteith LL, Bahraini NH, Menefee DS. Perceived burdensomeness, thwarted belongingness, and fearlessness about death: associations with suicidal ideation among female veterans exposed to military sexual trauma. J Clin Psychol. (2017) 73:1655–69. doi: 10.1002/jclp.22462
137. Wesselmann ED, Ispas D, Olson MD, Swerdlik ME, Caudle NM. Does perceived ostracism contribute to mental health concerns among veterans who have been deployed? PLoS ONE. (2018) 13:e0208438. doi: 10.1371/journal.pone.0208438
138. Kintzle S, Barr N, Corletto G, Castro CA. PTSD in US veterans: the role of social connectedness, combat experience and discharge. Healthcare. (2018) 6:102. doi: 10.3390/healthcare6030102
139. Teo AR, Chan BK, Saha S, Nicolaidis C. Frequency of social contact in-person vs. on Facebook: an examination of associations with psychiatric symptoms in military veterans. J Affect Disord. (2019) 243:375–80. doi: 10.1016/j.jad.2018.09.043
140. Bryan CJ, Heron EA. Belonging protects against postdeployment depression in military personnel. Depress Anxiety. (2015) 32:349–55. doi: 10.1002/da.22372
141. Bryan CJ, McNaughton-Cassill M, Osman A. Age and belongingness moderate the effects of combat exposure on suicidal ideation among active duty air force personnel. J Affect Disord. (2013) 150:1226–9. doi: 10.1016/j.jad.2013.05.087
142. Oliver LW, Harman J, Hoover E, Hayes SM, Pandhi NA. A quantitative integration of the military cohesion literature. Mil Psychol. (1999) 11:57–83. doi: 10.1207/s15327876mp1101_4
143. Ahronson A, Cameron JE. The nature and consequences of group cohesion in a military sample. Mil Psychol. (2007) 19:9–25. doi: 10.1080/08995600701323277
144. Kanesarajah J, Waller M, Zheng WY, Dobson AJ. Unit cohesion, traumatic exposure and mental health of military personnel. Occupat Med Oxford. (2016) 66:308–15. doi: 10.1093/occmed/kqw009
145. Brailey K, Vasterling JJ, Proctor SP, Constans JI, Friedman MJ. PTSD symptoms, life events, and unit cohesion in US soldiers: baseline findings from the neurocognition deployment health study. J Trauma Stress. (2007) 20:495–503. doi: 10.1002/jts.20234
146. Breslau J, Setodji CM, Vaughan CA. Is cohesion within military units associated with post-deployment behavioral and mental health outcomes? J Affect Disord. (2016) 198:102–7. doi: 10.1016/j.jad.2016.03.053
147. Fontana A, Rosenheck R, Horvath T. Social support and psychopathology in the war zone. J Nerv Ment Dis. (1997) 185:675–81. doi: 10.1097/00005053-199711000-00004
148. Du Preez J, Sundin J, Wessely S, Fear NT. Unit cohesion and mental health in the UK armed forces. Occupat Med. (2012) 62:47–53. doi: 10.1093/occmed/kqr151
149. Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, et al. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. (2008) 300:663–75. doi: 10.1001/jama.300.6.663
150. Smith BN, Wang JM, Vaughn-Coaxum RA, Di Leone BAL, Vogt D. The role of postdeployment social factors in linking deployment experiences and current posttraumatic stress disorder symptomatology among male and female veterans. Anxiety Stress Coping. (2017) 30:39–51. doi: 10.1080/10615806.2016.1188201
151. Dutra L, Grubbs K, Greene C, Trego LL, McCartin TL, Kloezeman K. Women at war: implications for mental health. J Trauma Dissoc. (2011) 12:25–37. doi: 10.1080/15299732.2010.496141
152. Harris RJ, McDonald DP, Sparks CS. Sexual harassment in the military. Armed Forces Soc. (2018) 44:25–43. doi: 10.1177/0095327X16687069
153. Dandeker C, Wessely S, Iversen A, Ross J. What's in a name? Defining and caring for “Veterans”: the united kingdom in international perspective. Armed Forces Soc. (2006) 32:161–77. doi: 10.1177/0095327X05279177
154. Han SC, Castro F, Lee LO, Charney ME, Marx BP, Brailey K, et al. Military unit support, postdeployment social support, and PTSD symptoms among active duty and national guard soldiers deployed to Iraq. J Anxiety Disord. (2014) 28:446–53. doi: 10.1016/j.janxdis.2014.04.004
155. Griffith J. Cross (unit)-level effects of cohesion on relationships of suicide thoughts to combat exposure, postdeployment stressors, and postdeployment social support. Behav Med. (2015) 41:98–106. doi: 10.1080/08964289.2014.987719
156. Boscarino JA, Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Boscarino JJ, et al. Mental health impact of homecoming experience among 1730 formerly deployed veterans from the vietnam war to current conflicts: results from the veterans' health study. J Nerv Ment Dis. (2018) 206:757–64. doi: 10.1097/NMD.0000000000000879
157. Hunt N, Robbins I. World war II veterans, social support, and veterans' associations. Aging Ment Health. (2001) 5:175–82. doi: 10.1080/13607860120038384
158. Nayback-Beebe AM, Yoder LH. Social conflict versus social support: what is more influential in mental health symptom severity for female service members? Arch Psychiatr Nurs. (2011) 25:469–78. doi: 10.1016/j.apnu.2011.02.005
159. Sutker PB, Davis JM, Uddo M, Ditta SR. War zone stress, personal resources, and PTSD in persian gulf war returnees. J Abnorm Psychol. (1995) 104:444–52. doi: 10.1037/0021-843X.104.3.444
160. Solomon Z, Oppenheimer B. Social network variables and stress reaction-lessons from the 1973 Yom-Kippur War. Mil Med. (1986) 151:12–15. doi: 10.1093/milmed/151.1.12
161. Karstoft K, Armour C, Elklit A, Solomon Z. Long-term trajectories of posttraumatic stress disorder in veterans: the role of social resources. J Clin Psychiatry. (2013) 74:e1163–8. doi: 10.4088/JCP.13.m08482
162. Solomon Z, Mikulincer M, Waysman M. Delayed and immediate onset posttraumatic stress disorder: the role of life events and social resources. J Commun Psychol. (1991) 19:231–36. doi: 10.1002/1520-6629(199107)19:3<231::AID-JCOP2290190304>3.0.CO;2-C
163. Hatch SL, Harvey SB, Dandeker C, Burdett H, Greenberg N, Fear NT, et al. Life in and after the armed forces: social networks and mental health in the UK military. Soc Health Illn. (2013) 35:1045–64. doi: 10.1111/1467-9566.12022
164. Kaspersen M, Matthiesen SB, Götestam KG. Social network as a moderator in the relation between trauma exposure and trauma reaction: A survey among UN soldiers and relief workers. Scand J Psychol. (2003) 44:415–23. doi: 10.1046/j.1467-9450.2003.00362.x
165. Olson MD. Exploring military social work from a social justice perspective. Int Soc Work. (2018) 61:119–29. doi: 10.1177/0020872815606792
166. Thomas VJ, Bowie SL. Sense of community: is it a protective factor for military veterans? J Soc Serv Res. (2016) 42:313–31. doi: 10.1080/01488376.2015.1109575
167. Molendijk T. Moral injury in relation to public debates: the role of societal misrecognition in moral conflict-colored trauma among soldiers. Soc Sci Med. (2018) 211:314–20. doi: 10.1016/j.socscimed.2018.06.042
168. Cederbaum JA, Wilcox SL, Sullivan K, Lucas C, Schuyler A. The influence of social support on dyadic functioning and mental health among military personnel during postdeployment reintegration. Public Health Rep. (2017) 132:85–92. doi: 10.1177/0033354916679984
169. Burger N. Guidelines for Psychosocial Support for Uniformed Workers. Extensive Summary and Recommendations. Amsterdam; Utrecht: Impact/Trimbos Instituut (2012). Available online at: www.eutopa-info.eu
170. Guay S, Billette V, Marchand A. Exploring the links between posttraumatic stress disorder and social support: processes and potential research avenues. J Trauma Stress. (2006) 19:327–38. doi: 10.1002/jts.20124
171. Olff M. Bonding after trauma: on the role of social support and the oxytocin system in traumatic stress. Eur J Psychotraumatol. (2012) 3:18597. doi: 10.3402/ejpt.v3i0.18597
173. McFarlane AC, Van der Kolk BA. Trauma and its Challenge to Society. New York, NY: Guilford Press (1996). p. 24–46.
174. Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. (1995) 117:497–529. doi: 10.1037/0033-2909.117.3.497
175. Potter C. To what extent do nurses and physicians working within the emergency department experience burnout: a review of the literature. Australas Emerg Nurs J. (2006) 9:57–64. doi: 10.1016/j.aenj.2006.03.006
176. He N, Zhao J, Ren L. Do race and gender matter in police stress? A preliminary assessment of the interactive effects. J Crim Justice. (2005) 33:535–47. doi: 10.1016/j.jcrimjus.2005.08.003
177. Major B, Zubek JM, Cooper ML, Cozzarelli C, Richards C. Mixed messages: implications of social conflict and social support within close relationships for adjustment to a stressful life event. J Pers Soc Psychol. (1997) 72:1349–63. doi: 10.1037/0022-3514.72.6.1349
178. Lyons JA. Strategies for assessing the potential for positive adjustment following trauma. J Traum Stress. (1991) 4:93–111. doi: 10.1002/jts.2490040108
179. Loriol M. Collective forms of coping and the social construction of work stress among industrial workers and police officers in France. Theory Psychol. (2016) 26:112. doi: 10.1177/0959354315616877
180. Sommer M, Njå O. Learning amongst Norwegian fire-fighters. J Workplace Learn. (2011) 23:435–55. doi: 10.1108/13665621111162963
181. Pearlin LI. The sociological study of stress. J Health Soc Behav. (1989) 30:241–56. doi: 10.2307/2136956
182. Dick P. The social construction of the meaning of acute stressors: a qualitative study of the personal accounts of police officers using a stress counselling service. Work Stress. (2000) 14:226–44. doi: 10.1080/02678370010026422
183. Evans R, Pistrang N, Billings J. Police officers' experiences of supportive and unsupportive social interactions following traumatic incidents. Eur J Psychotraumatol. (2013) 4. doi: 10.3402/ejpt.v4i0.19696
184. Lowery K, Stokes MA. Role of peer support and emotional expression on posttraumatic stress disorder in student paramedics. J Trauma Stress. (2005) 18:171–9. doi: 10.1002/jts.20016
185. Steen E, Naess AC, Steen PA. Paramedics organizational culture and their care for relatives of cardiac arrest victims. Resuscitation. (1997) 34:57–63. doi: 10.1016/S0300-9572(96)01045-3
186. McFarlane AC. The phenomenology of posttraumatic stress disorders following a natural disaster. J Nerv Ment Dis. (1988) 176:22–29. doi: 10.1097/00005053-198801000-00003
187. Pogrebin MR, Poole ED. Police and tragic events: the management of emotions. J Crim Justice. (1991) 19:395–403. doi: 10.1016/0047-2352(91)90036-U
188. Stephens C, Long N, Miller I. The impact of trauma and social support on posttraumatic stress disorder: a study of New Zealand police officers. J Crim Justice. (1997) 25:303–14. doi: 10.1016/S0047-2352(97)00015-9
189. Hobfoll SE. Social support: the movie. J Soc Pers Relat. (2009) 26:93–101. doi: 10.1177/0265407509105524
190. Wethington E, Kessler RC. Perceived support, received support, and adjustment to stressful life events. J Health Soc Behav. (1986) 27:78–89. doi: 10.2307/2136504
191. Britt TW. The stigma of psychological problems in a work environment: evidence from the screening of service members returning from bosnia1. J Appl Soc Psychol. (2000) 30:1599–618. doi: 10.1111/j.1559-1816.2000.tb02457.x
192. Halpern J, Gurevich M, Schwartz B, Brazeau P. What makes an incident critical for ambulance workers? Emotional outcomes and implications for intervention. Work Stress. (2009) 23:173–89. doi: 10.1080/02678370903057317
193. Jones N, Keeling M, Thandi G, Greenberg N. Stigmatisation, perceived barriers to care, help seeking and the mental health of British military personnel. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:1873–83. doi: 10.1007/s00127-015-1118-y
194. Kim PY, Thomas JL, Wilk JE, Castro CA, Hoge CW. Stigma, barriers to care, and use of mental health services among active duty and national guard soldiers after combat. Psychiatr Serv. (2010) 61:582–8. doi: 10.1176/ps.2010.61.6.582
195. Molendijk T, Kramer E, Verweij D. Conflicting notions on violence and PTSD in the military: institutional and personal narratives of combat-related illness. Cult Med Psychiatry. (2016) 40:338–60. doi: 10.1007/s11013-015-9469-0
196. Vermetten E, Jetly R. A critical outlook on combat-related PTSD: review and case reports of guilt and shame as drivers for moral injury. Military Behavioral Health. (2018) 6:156–64. doi: 10.1080/21635781.2018.1459973
197. Schwarz N. Self-reports: how the questions shape the answers. Am Psychol. (1999) 54:93–105. doi: 10.1037/0003-066X.54.2.93
Keywords: trauma, high-risk professionals, social embeddedness, environment, relationships
Citation: Geuzinge R, Visse M, Duyndam J and Vermetten E (2020) Social Embeddedness of Firefighters, Paramedics, Specialized Nurses, Police Officers, and Military Personnel: Systematic Review in Relation to the Risk of Traumatization. Front. Psychiatry 11:496663. doi: 10.3389/fpsyt.2020.496663
Received: 08 September 2019; Accepted: 20 November 2020;
Published: 21 December 2020.
Edited by:
Wulf Rössler, Charité – Universitätsmedizin Berlin, GermanyReviewed by:
Michaela Pascoe, Victoria University, AustraliaKonstantinos Papazoglou, Yale University, United States
Copyright © 2020 Geuzinge, Visse, Duyndam and Vermetten. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renate Geuzinge, cmVuYXRlLmdldXppbmdlQHBoZC51dmgubmw=
 Renate Geuzinge
Renate Geuzinge Merel Visse
Merel Visse Joachim Duyndam
Joachim Duyndam Eric Vermetten
Eric Vermetten