- 1URPP “Dynamics of Healthy Aging”, University of Zurich, Zurich, Switzerland
- 2Department of Anthropology, McGill University, Montréal, QC, Canada
- 3Department of Geriatric Psychiatry, Psychiatric University Hospital Zurich, Zurich, Switzerland
The concept of severe and persistent mental illness (SPMI) lacks a consensual definition. Variations in definitions stem above all from different meanings about the constituent features of the concept and how to operationalize them. Our objective was to clarify the concept of SPMI and to explore the level of concept maturity through pragmatic utility (PU) concept analysis. Our findings suggest that SPMI is a partially mature concept that needs further clarification. We argue that the lack of a uniform definition is inherent to the problem: SPMI refers to a patient population rather than a disease entity, and the term has to be useful for different stakeholder purposes. Therefore, while an agreement on the principle three dimensions included in a definition may be possible (diagnosis, disability, and duration), their operationalization will have to be context-dependent and specific for the task at hand.
Introduction
Severe and persistent mental illness (SPMI) is associated with suffering in the affected persons and burden to their caregivers. To provide optimal healthcare for these patients is a challenge. To advance service provision for this population, research is needed to guide treatments and resource allocation. However, several authors have highlighted that SPMI lacks a consensual definition (1–5). Variations in definitions stem above all from different meanings about the constituent features of the concept and how to operationalize them. Consequently, researchers, policymakers, and healthcare providers may have various understandings of SPMI, measure different phenomena, and deal with different patient groups. Therefore, an analysis of the definitional basis of SPMI is needed to advance the field.
The term SPMI was introduced by a workgroup convened by the NIMH in 1987 (6) and defined SPMI as a function of the three “Ds”, namely, diagnosis, disability, and duration. The workgroup aimed to improve service and policy planning in the United States (3, pp. 13–14, 6). In the following years, several authors developed definitions of SPMI to be used on the local level (1–4).
Recently, a debate has emerged that connects SPMI with palliative care (7–15). A paradigm shift to “palliative psychiatry” for SPMI has been proposed as this population is at risk of therapeutic neglect and/or overly aggressive care within the existing care paradigms (13). However, this ongoing debate has so far neglected to scrutinize the closely linked concept of SPMI. SPMI plays a crucial epistemic role in the formation of a palliative psychiatry paradigm as it refers to its target. The current debate about palliative psychiatry marks a “pre-paradigm” stage as the description lacks conceptual consensus (16, p. 47). The idea of palliative psychiatry itself may remain immature as long as the level of conceptual maturity of SPMI has not been assessed. Consequently, there is a need to evaluate the maturity of the concept of SPMI for palliative psychiatry to become “normal science”, i.e., the default state of mature science, which is characterized by a broad consensus of the practitioners of a scientific field on fundamental questions (16, p. 10).
Hence, our objective was to clarify the concept of SPMI in the health sciences and to explore the level of concept maturity through a particular form of systematic literature review, Pragmatic Utility (PU) concept analysis (17–19). Specifically, our research questions were: How is SPMI defined and what are the features of the definition, i.e., is SPMI clearly and consensually defined, fully described, with clear characteristics, demonstrated preconditions and outcomes, and clearly delineated boundaries? The need for a consensus definition of SPMI has emerged in specific domains with particular ways of understanding and reasoning of the issue. Therefore, we also aimed to explore how the problem of defining SPMI was initially framed and followed up by various authors.
Methods
Literature Identification and Selection
Following a scoping search, a systematic search of the following databases was carried out to guarantee adequate and efficient identification of pertinent research related to the topic of interest and to minimize publication bias (20): EMBASE, SCOPUS, PsychINFO, MEDLINE, and Web of Science. Search tools such as medical subject headings (MeSH), Boolean operators, truncations, and positional operators were used. The search was limited to English-only literature, and no year limits were applied. The search strategy was developed in consultation with a research librarian, and the search strings adapted to suit the search style of specific databases used. In all databases, single and combined search terms included the terms “severe”, “serious”, “chronic”, “mental”, “illness”, “disorder”, “disease”, as well as “definition”, “concept”, “theory”, “model”, “method”, “concept model”, “concept framework”, and “approach”. The scoping search identified the article by Schinnar et al. (2) as a key article on the topic of definitions of SPMI. Subsequently, a forward search in Google Scholar was performed to identify further studies that may have been missed in the primary database searches for inclusion (21, p. 121).
Only publications that develop, propose, or describe a definition, theory, model, approach, or framework (theoretical or empirical) for defining, assessing, analyzing, and/or reporting SPMI were included for the concept analysis (inclusion criteria). The included studies could be both empirical (qualitative and/or quantitative methods and systematic reviews) or theoretical (theory formation/development based on literature reviews and/or experience). The studies which were identified through the database and citation searches were downloaded into a reference management database and deduplicated. All titles and abstracts were then screened against inclusion criteria. References not meeting the inclusion criteria were excluded. A random sample of 20 articles (10 classified as not relevant, 10 as relevant by the first reviewer, NZ) was drawn, and a blind classification was performed by the second reviewer, FR. Classification differed in only one case that was resolved by subsequent discussion between reviewers 1 and 2, with reviewer 1’s classification prevailing.
Organization and Structuring of the Literature
Articles were coded using MAXQDA 12 to chart the data. The organization and structuring of the literature were initially undertaken by NZ and then reviewed by FR. Relevant articles were first organized according to general features such as publication year, origin, the field of application, type of studies, and focus of the publication. A more in-depth structuring of the papers was guided by the following analytical questions: Which definitions were used in the literature? Is there a consensus within the literature about the definition? Was the lack of a consensus definition addressed and followed up in the literature? Which definitions of SPMI were used in relationship with the topic of palliative care? Was the lack of a consensus definition addressed and followed up in the literature about palliative care? The coding frame for this in-depth structuring was based on an iterative deductive and inductive category formation (22, p. 93).
Concept Analysis
We chose a particular variation of a systematic review, namely, PU concept analysis, as developed by Morse et al. (17–19). PU concept analysis explores the level of maturity of concepts by assessing their internal structure, use, representativeness, and/or relations to other concepts. It serves, among other things, to determine the need to refine or clarify a concept or to examine the congruence between the definition of the concept and the way it has been operationalized (17, pp. 75–79). The evaluation of maturity uses the following overlapping criteria: epistemological (clarity of definition, boundaries, attributes, preconditions, and outcomes), pragmatic (operationalization of the concept in research and practice), linguistic (use in various contexts), and logical (differentiation of the concept from other concepts when used in theory). A concept is “mature” when it is well-defined, has clearly described characteristics, delineates boundaries, and documented preconditions and outcomes (18). However, a concept is not required to meet all of these criteria. Between the two extremes of immature and mature concepts are concepts that are partially developed (17, p. 88), for instance, when distinguishing features are not yet fully articulated and need further clarification.
Rather than a series of steps, PU concept analysis is a non-linear, iterative process. It contains, apart from the initial clarification of the purpose of the analysis the following guiding principles (23): a) identification and selection of relevant literature to ensure validity of the concept analysis, b) organization of literature in a general way, c) structuring literature through decontextualization to reveal general features of the concept, and d) formulation of key analytical questions to derive consistent dimensions and boundaries of the concept. Also, we explored how the problem of defining the concept was framed and followed up by analyzing the underlying assumptions and premises.
Results
Identified Literature
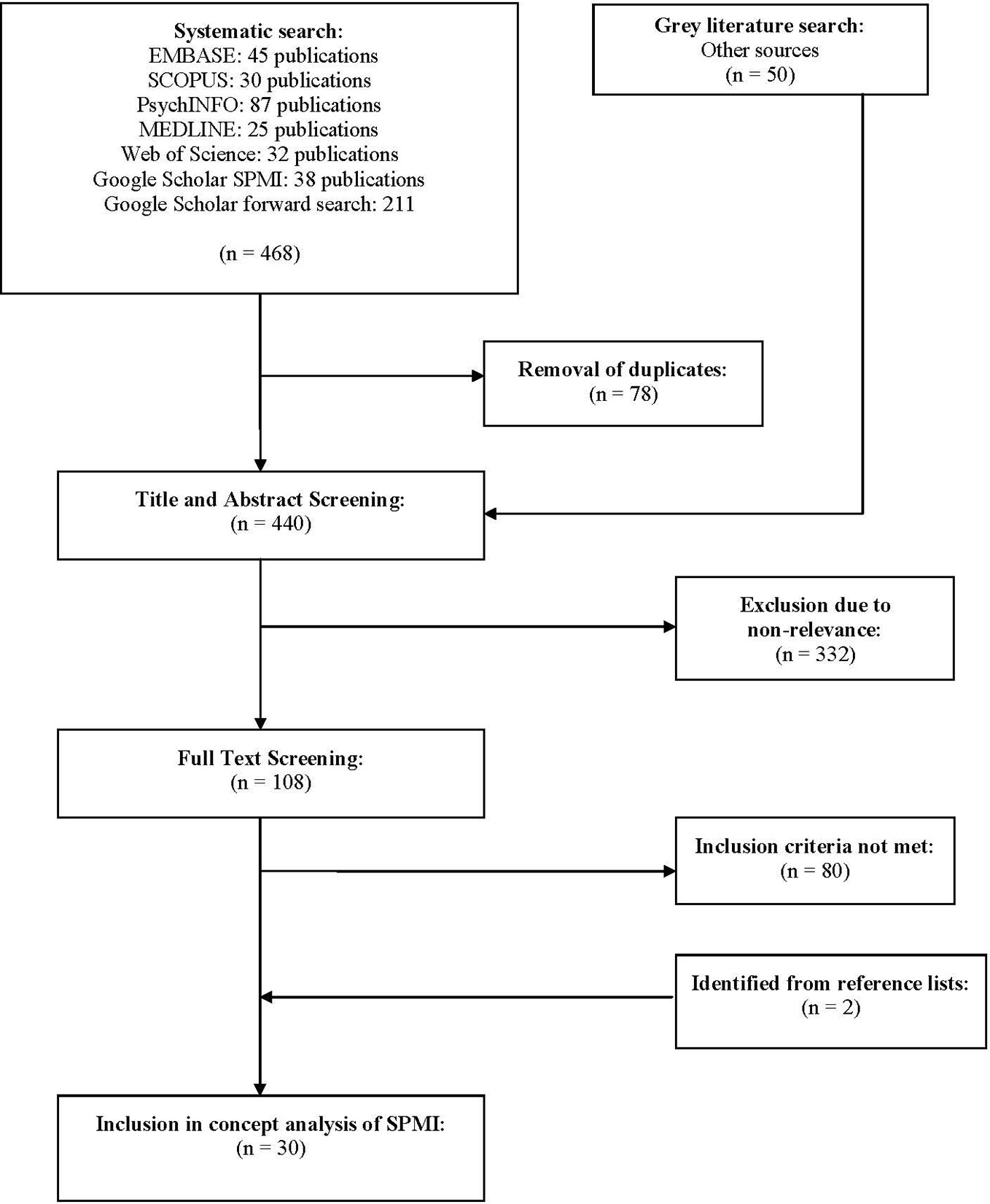
After removal of duplicates, the initial literature search identified 440 articles. After exclusion of articles based on title and abstract, 108 articles underwent full-text reading. Based on the full-text, 28 articles were identified as relevant for our analysis. The reference lists of these studies were checked for further resources, resulting in the inclusion of an additional two publications for a total of 30 articles. For a flow chart of the literature identification and selection process, see Figure 1.
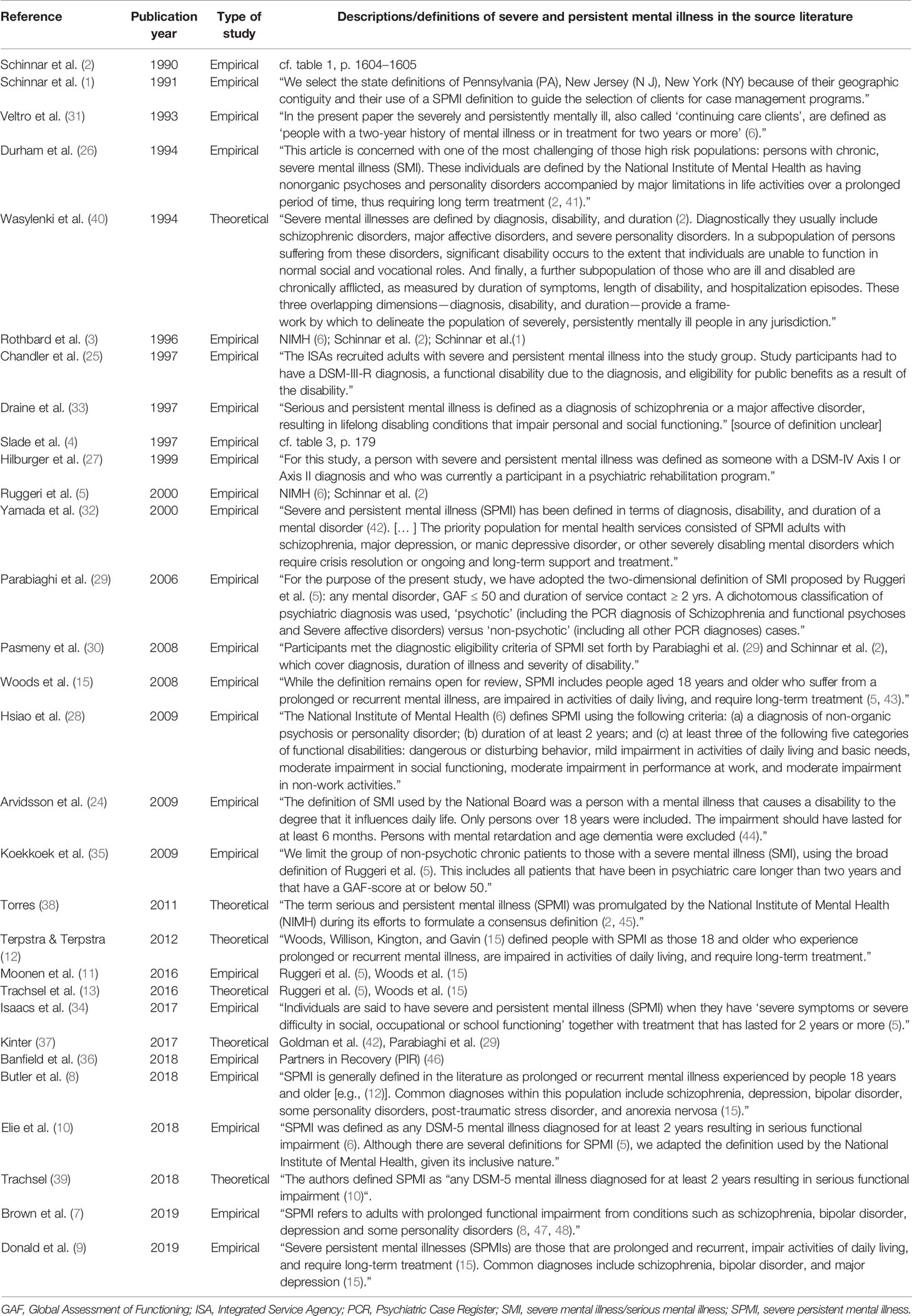
The articles in our final sample included descriptive studies (1, 3, 5, 8, 10, 24–32), systematic literature reviews (2, 4, 9, 15), a non-systematic literature review (33), qualitative case studies (11, 34, 35), a mixed-method approach (36), and theoretical papers (7, 12, 13, 37–40). Eleven articles originated in the United States, five in Canada, three each in Australia and Italy, two in Switzerland, one each in Sweden, Taiwan, Belgium, Netherlands, New Zealand, and the United Kingdom. Articles were distributed over time since the initial article in 1990 (2) (see Table 1). Definitions and concepts of SPMI in included studies were based on psychiatry (eleven), nursing (six), psychology (three), social science (three), rural, public, population health (three), social work (three), and ethics (one). Findings from our review drawn from the collected articles resulted in the following themes in relation to which SPMI is discussed: health services, care practices, palliative care, recovery, rehabilitation, social support, rehospitalization, and family adaptation. For characteristics of the included articles and the descriptions and definitions used, see Table 1.
Definitions of Severe and Persistent Mental Illness
The analysis of the descriptions and definitions used across the studies reveals an abundance and inconsistent use of different expressions, phrases, and initialisms. For instance, the initialism SMI was not just used for “severe mental illness” but also for “severe and persistent mental illness” instead of SPMI [e.g., (5, 24, 29)]. The initialism SPMI was used for “severe and persistent mental illness” as well as “serious and persistent mental illness” (7). Half of the papers addressed the lack of a consensus definition (1–5, 10, 13, 15, 24, 29–31, 35, 37, 38). Nine articles of those which addressed the lack of a consensus definition also discussed which dimension to include and how to operationalize them (1–5, 24, 29, 31, 38). Initially, the phrase “lack of consensus” referred to a lack of consensus among researchers, mental health planners, and policymakers on the local and national level in the United States (1–3). In subsequent papers, the authors highlighted the lack of consensus on the international level [e.g., (4, 5, 13, 31)]. Hence, the problem of “consensus definition” was reframed in a far-reaching way. Shifting the meaning of the notion “consensus” implies a different approach to find a consensus definition.
Variations in definitions appeared to mainly originate from different meanings of the constituent features of the concept, i.e., which dimensions to include. Associations and forms of the dimensions varied according to the different situations or conditions in which the concept was being used. Commonly, the definitions consisted of three dimensions, namely diagnosis, duration, and disability. “Diagnosis” included a variety of illnesses, “duration” referred either to the duration of symptoms, treatment or disability and “disability” was used for functional impairment or quality of life. Slade et al. (4) proposed a five-dimensional framework for developing definitions at a local level. Ruggeri et al. (5) tested two operationalized definitions in two different settings, a narrow one (the “three-dimensional definition”) based on the National Institute of Mental Health definition (6) and a broad one (the “two-dimensional definition”).
Nine articles discussed SPMI in connection with palliative care (7–13, 15, 39). Four out of the nine papers were theoretical (7, 12, 13, 39) and five empirical (8–11, 15). The definitions of SPMI used in these papers were those from the National Institute of Mental Health (6), Schinnar et al. (2), Ruggeri et al. (5), and Woods et al. (15). Woods et al. refer to Ruggeri et al. (5) and the state definition of serious mental illness of Virginia (USA) (43). Among the palliative care-related articles, only three address the lack of a consensus definition of SPMI (10, 13, 15). However, none of them discussed and followed up on this issue in detail.
Milestone Publications
We identified the definitions in the papers by the NIMH (6), Schinnar et al. (2), Slade et al. (4), and Ruggeri et al. (5) as the most impactful on subsequent publications and therefore present them in more detail here.
The phrase “severe and persistent mental illness” was introduced by the NIMH in 1987 (6) to replace “chronic mental illness” (CMI) because of the association chronicity has had with continuous or incurable illness (3, p. 10). The task of the workgroup convened by the NIMH in 1987 was to develop a national definition of “severe and persistent mental illness” and builds on the work of Goldman et al. (42), who discussed how to define and count the “chronically mentally ill” (CMI). The objective of the NIMH workgroup was to reduce the variance in counts of persons affected by SPMI to improve service and policy planning and to increase the congruence between federal and state guidelines for beneficiaries of federal and state economic and social support programs (3, pp. 13–14). Also, the workgroup proposed to operationalize the definition using measures of disability or dysfunction that are congruent with the Social Security Administration’s approach to defining disability. However, the workgroup also suggested that specific thresholds on the measures could vary for state and local purposes.
The original NIMH definition (6) comprised the three dimensions diagnosis, disability and duration operationalized as follows: “Diagnosis: A major mental disorder according to DSM-III-R: a major affective, non-organic psychotic disorder or a disorder that may lead to a chronic disability such as a borderline personality disorder. Disability: Severe recurrent disability resulting from mental illness. The disability results in functional limitations in major life activities. Individuals must meet at least two of the following criteria on a continuing or intermittent basis: (1) Is unemployed, is employed in a sheltered setting or supportive work situation, or has markedly limited skills and a poor work history (2) Requires public financial assistance from out-of-hospital maintenance and may be unable to procure such assistance without help (3) Has difficulty in establishing or maintaining a personal social support system (4) Requires help in basic livings skills such as hygiene, food preparation, or money management (5) Exhibits inappropriate social behavior which results in intervention by the mental and/or judicial system; Duration: Treatment history meets one or both of the following criteria: (1) Has undergone psychiatric treatment more intensive than outpatient care more than once in a lifetime (e.g., crisis response services, alternative home care, partial hospitalization, or inpatient hospitalization) (2) Has experienced an episode of continuous, supportive residential care, other than hospitalization, for a period long enough to have significantly disrupted the normal living situation.”
Schinnar and his colleagues (2) used the NIMH definition as a reference point because it reflects a national perspective on SPMI. The authors aimed to define and operationalize “severe and persistent mental illness” to obtain better national and local prevalence rates of SPMI and to assess program effectiveness for recovery from SPMI. Seventeen definitions of the severe and persistent mentally ill, which have been developed in the context of mental health care in the United States were reviewed. Based on the narrative descriptions of SPMI, each criterion was operationalized. The operationalized definitions were applied to a stratified sample of 222 adult patients who were admitted to an inner-city community mental health center in the city of Philadelphia to estimate the prevalence of SPMI in this sample. Their findings suggest that there is general agreement in the literature that diagnosis, disability, and duration criteria in some form are necessary to define serious mental illness. The authors state that there is uncertainty about the relevant diagnostic categories, the nature and degree of disability, the length of illness, and the relative importance of each. According to the authors, there is a general consensus that the duration criterion should reflect the persistence of disability and not the duration of illness or treatment time. The authors posit that departures from the consensus definition, which uses persistence of disability as a criterion for the duration, will and should occur within specific communities with special needs.
In a subsequent study (1), the authors highlight that mental health care needs are too heterogeneous across the United States, and resources available to meet such needs are too unevenly distributed to make a consensus definition of SPMI a practical tool. Hence, federal agencies should promote the development of a consistent framework for counting and reporting services for persons affected by SPMI. The authors underline that states should remain free to develop definitions that suit their local needs best. However, they should be encouraged to develop definitions in a manner that is consistent with the components of the framework.
Slade et al. (4) address the problem of prioritization in mental health care and surveyed current practice in England by obtaining written documentation from 20 agencies on the eligibility criteria they use for deciding whether someone should receive mental health care. The study also included surveys of government departments, user groups, and professional bodies. The authors propose to include a “top-down” and “bottom-up” process in formulating a definition. “Top-down” includes consultation of managers specifying principles for identifying priority groups, by applying official guidelines to the local level. “Bottom-up” entails staff working together to amend these principles in the light of their experience with individual clients. The findings indicate that definitions of severe mental illness are based on the SIDDD dimensions, i.e., safety, informal and formal support, diagnosis, disability, and duration. This particular set of components can be used as a framework for definitions at a local level.
Ruggeri and her colleagues (5) tested two operationalized definitions of “severe mental illness” (SMI) to calculate prevalence rates of SMI in two catchment areas in Europe (South London and South Verona). The prevalence rates were calculated according to a narrow (three-dimensional), and broad (two-dimensional) operationalized definition of SMI, which were derived from the NIMH (6) definition. The “three-dimensional definition” uses three criteria: diagnosis of psychosis, duration of service contact ≥ 2 years, and GAF ≤ 50. The “two-dimensional definition” uses only the last two criteria, i.e., duration and dysfunction. Describing the definition as either “two-dimensional” or “three-dimensional” is, however, imprecise. “Dimension” refers to diagnosis, duration, and disability or, in this case, dysfunction. According to the authors, the two-dimensional definition is based on duration and dysfunction only and applied to patients with and without psychotic disorders. Hence, the dimension “diagnosis” has actually not been excluded but rather operationalized differently.
Concept Maturity
A concept is “mature” when it is well-defined, has clearly described characteristics, delineates boundaries, and documented preconditions and outcomes (18). The heterogeneity of dimensions included in the definitions did not allow us to assess the preconditions, outcomes, and boundaries of the concept in a structured way. Therefore, we conclude that SPMI is a concept that is only partially mature because definitions and terminology vary widely across the literature and because the constituent features are—as of yet—not fully articulated and need further clarification.
Discussion
Research and improvement of service provision for SPMI are hampered by a lack of a clear theoretical framework and, consequently, consensus what SPMI actually is. Our aim was, therefore, to systematically review the existing literature on SPMI for its definitions and to perform a PU concept analysis to examine the concept’s maturity. We found inconsistent use of terminology and perpetual confusion about the constituent features of the concept and, consequently, different operationalizations of the dimensions. We conclude that SPMI is—as of yet—a partially mature concept that requires further theoretical development to become useful. Following Brigandt (49), we believe that an essential function of concepts is to set a problem agenda. Also, partial maturity is not a hindrance to practical research. According to MacLeod (50), the open-endedness (or partial maturity) of a concept refers to an as of yet not well-known aspect of reality. However, a concept is not required to give a correct representation of it to be scientifically useful.
The Lack of a Consensus Definition
Several studies have addressed the problem of how to define and operationalize the concept (1–5, 29, 38). Since the seminal studies of Schinnar and his colleagues (1–3), only Slade at al. (4) as well as Ruggeri and her colleagues suggested how to operationalize the concept (5, 29). Definitions used in articles about palliative care and SPMI refer to four sources (2, 5, 6, 15), and the lack of a consensus definition of SPMI is left commonly unaddressed.
Initially, the phrase “lack of consensus” referred to a lack of consensus among researchers, mental health planners, and policymakers on the local and national level in the United States (1–3). The main goal of finding a consensus definition of SPMI was to increase the congruence between federal and state guidelines for beneficiaries of federal and state economic and social support programs. For instance, the dimension “disability” was formulated in congruence with the Social Security Administration’s approach to defining disability. The Social Security Administration is a national agency of the U.S., and its regulations on disability may not be suitable as a reference point to develop a definition that will be applied in other contexts. Moreover, definitions developed by institutions are commonly not based on empirical findings and not intended for scientific use but for management issues.
Interestingly, these statements about the scale of the definition have been ignored in subsequent studies as the problem of defining “severe and persistent mental illness” (SPMI) or “severe mental illness” (SMI) has been mainly framed as the lack of an international consensus definition. Hence, the problem of consensus definition was reframed in a far-reaching way as it implies a different approach to solving the problem of lack of consensus. The lack of an international consensus definition seems to have become a commonsense idea, a “thought style” (51), which remained unquestioned and carried on from one paper to the other. The underlying assumption of this kind of problematization is that there should be a general theory of SPMI.
We argue that the search for a grand theory of SPMI is misdirected because it ignores that the aim of every individual research project informs the choice of theoretical frameworks and the context-dependence of the operationalization. SPMI is not a disease entity but rather refers to a particular population. Also, the claim for a consensus definition implies a homogeneity of the target population, but all descriptions of the target population are, of necessity, combinations of medical (e.g., diagnostic assessment) and social (e.g., community functioning assessment) (52) as well legal criteria. Hence, the call for a standardized international definition of SPMI is based on an incomplete understanding of the requirements that such a uniform definition would have to fulfill. Moreover, the call for a consensus definition of SPMI follows a kind of reverse epistemology as the elaboration of the concept stands at the beginning of the explanation chain; it precedes the accumulation of empirical evidence.
Finally, while an international consensus definition may facilitate large scale epidemiological research, it may create a clinically irrelevant category on the local level as the definition neglects local conditions, specificities, and nuances and has, therefore, no practical use. SPMI affects people who differ considerably with regards to their diagnoses, treatment histories, functional levels, and needs. Thus, a consensus definition might even be potentially detrimental to the target population, as it may lead to a “one size fits all” approach. This argument has already been put forward by Bachrach (53) but seemingly ignored in subsequent studies. Although she refers to CMI, we believe that her argument also applies to “severe and persistent mental illness”.
Reaching a Useful Definition
Instead of rebutting the concept of SPMI as a whole due to the alleged problem of lack of consensus definition, we propose to keep it as a heuristic device. Still, we argue against a consensus definition for use on the international level. We argue that the search for a consensus definition of SPMI based on a single general theory is misguided as it ignores the context-dependence of health and healthcare. Future research on SPMI ought to focus first on reducing ambiguity in the terminology and achieving context-dependent clarity about the meaning of the concept (54, p. 10). Hence, to clarify the connection between the concept of SPMI and its theoretical or empirical statements, there is a need to develop a specific context-dependent theoretical framework and to formulate a definition of SPMI for use on the local level and to operationalize the constituent dimensions according to specificities and needs in a given context.
As a starting point for such locally useful definitions, we propose the original NIMH definition of SPMI (see results section) (6). According to van der Steen (54, p. 18), a useful definition in the life sciences must be clear, not circular, neither too broad nor too narrow, should not include accompanying features, and should refer to the features present (rather than referring to features that are absent). Accordingly, we suggest the definition of SPMI to be based on the three Ds, i.e., diagnosis, duration, and disability. As constituent characteristics, they are abstract enough to define the concept regardless of the context in which it appears, yet unique enough to define and differentiate it from other concepts [cf. (18, p. 388)]. Also, this allows a notion of SPMI that is wide enough for quite different further developments. Given the context-dependence of the different constituent features of the definition, we argue that the constituent dimensions then have to be further operationalized according to the priorities, needs, and subtleties prevailing in a given context. Local operationalizations would undoubtedly require an update of the diagnostic system in use (i.e., DSM 5 or ICD-11 instead of DSM-III-R) and would likely involve more subjective parameters in the disability and duration dimensions (emphasizing SPMI as illness concept rather than as healthcare planning construct).
SPMI and Palliative Psychiatry
It has been postulated that a palliative approach in psychiatry has the potential to improve the quality of care, person-centeredness, and autonomy for patients affected by SPMI (13). In other words, SPMI is considered the target population of palliative psychiatry, and palliative psychiatry attempts to promote person-centeredness and patient autonomy. As to be expected from our concept analysis, a recent article on a novel therapeutic approach to SPMI had to further specify its intended target population as “most serious forms of SPMI, for instance, when the quality of life is seriously compromised” (55). We ultimately believe that a definition of SPMI true to a palliative ethos of care will necessarily have to take the perspectives of the affected persons into account. Thus, a definition of SPMI for use in the field of palliative psychiatry should be negotiated among user groups and their caregivers, government agencies, insurers, and treatment teams who establish a set of principles to help guide the development of a definition. To a certain extent, this may allow for the self-assignment of persons affected by SPMI to receive palliative care in psychiatry based on patients’ needs, goals, and preferences. However, the theoretical framework, as well as the empirical evidence for palliative psychiatry, have to be developed further to be able to define its target population.
Hence, we propose a participatory/collaborative approach as a research strategy which combines theoretical and practical knowledge to generate new knowledge about a phenomenon. The underlying ethos of such a research strategy has been formulated by Burns (56). The work of Vreman et al. (57) illustrates how semi-structured group discussions and open session workshops among various stakeholders provided insights about the concept of unmet medical need (UMN).
Strengths and Limitations
This is the first PU concept analysis to evaluate the maturity of the concept of SPMI. Important strengths of our systematic review include a well-defined research question, an exhaustive search strategy, well-defined inclusion and exclusion criteria, and comprehensive data coding. A significant limitation was that the iterative coding process was mainly performed by NZ. However, the analysis of the coded data was conducted in close cooperation with both authors.
Conclusions
A systematic concept evaluation is a fundamental step in the research process that should precede more formal research procedures such as operationalization or identification of the variables (18). It allowed us to identify ambiguities and inconsistency of constituent features of the concept of SPMI. According to our PU concept analysis, SPMI refers to a partially mature concept that lacks a standard definition. We argue that this lack of a uniform definition is inherent to the problem: SPMI refers to a patient population rather than a disease entity, and the term has to be useful for different stakeholder purposes. Hence, the next step toward concept clarification and development consists of an assessment of the different perceptions of various stakeholders through a participatory oriented approach between researchers, persons affected by SPMI, and multiple practitioners. Insights gained from semi-structured group discussions and open session workshops among these different stakeholders have then to be incorporated in a modified definition of SPMI.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Author Contributions
All authors contributed to the article and approved the submitted version.
Funding
Open access publication was funded by the University of Zurich.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Jill Boruff, MLIS, Liaison Librarian to the School of Physical and Occupational Therapy, the School of Communication Sciences and Disorders, and the Department of Psychiatry, McGill University, Montreal, Canada
References
1. Schinnar AP, Rothbard AB, Kanter R. Adding state counts of the severely and persistently mentally ill. Adm Policy Ment Hlth (1991) 19(1):3–12. doi: 10.1007/BF00710514
2. Schinnar AP, Rothbard AB, Kanter R, Jung YS. An empirical literature review of definitions of severe and persistent mental illness. Am J Psychiat (1990) 147(12):1602–8. doi: 10.1176/ajp.147.12.1602
3. Rothbard AB, Schinnar AP, Goldman H. The Pursuit of a Definition for Severe and Persistent Mental Illness. In: Soreff SM, editor. Handbook for the Treatment of the Seriously Mentally Ill. Ashland, OH: Hogrefe & Huber Publishers (1996). p. 9–26.
4. Slade M, Powell R, Strathdee G. Current approaches to identifying the severely mentally ill. Soc Psych Psych Epid (1997) 32(4):177–84. doi: 10.1007/BF00788236
5. Ruggeri M, Leese M, Thornicroft G, Bisoffi G, Tansella M. Definition and prevalence of severe and persistent mental illness. Brit J Psychiat (2000) 177:149–55. doi: 10.1192/bjp.177.2.149
6. National Institute of Mental Health. Towards a Model for a Comprehensive Community-Base Mental Health System. Washington DC: NIMH (1987).
7. Brown R, Chambers S, Rosenberg J. Exploring palliative care nursing of patients with pre-existing serious persistent mental illness. Prog Palliat Care (2019) 27(3):117–21. doi: 10.1080/09699260.2019.1619964
8. Butler H, O’Brien AJ. Access to specialist palliative care services by people with severe and persistent mental illness: A retrospective cohort study. Int J Ment Health Nu (2018) 27(2):737–46. doi: 10.1111/inm.12360
9. Donald EE, Stajduhar KI. A scoping review of palliative care for persons with severe persistent mental illness. Palliat Support Care (2019) 17(4):479–87. doi: 10.1017/S1478951519000087
10. Elie D, Marino A, Torres-Platas SG, Noohi S, Semeniuk T, Segal M, et al. End-of-life care preferences in patients with severe and persistent mental illness and chronic medical conditions: a comparative cross-sectional study. Am J Geriat Psychiat (2018) 26(1):89–97. doi: 10.1016/j.jagp.2017.09.018
11. Moonen C, Lemiengre J, Gastmans C. Dealing with existential suffering of patients with severe persistent mental illness: Experiences of psychiatric nurses in Flanders (Belgium). Arch Psychiat Nurs (2016) 30(2):219–25. doi: 10.1016/j.apnu.2015.10.005
12. Terpstra TL, Terpstra TL. Hospice and palliative care for terminally ill individuals with serious and persistent mental illness: widening the horizons. J Psychosoc Nurs Men (2012) 50(9):28–34. doi: 10.3928/02793695-20120807-02
13. Trachsel M, Irwin SA, Biller-Andorno N, Hoff P, Riese F. Palliative psychiatry for severe persistent mental illness as a new approach to psychiatry? Definition, scope, benefits, and risks. BMC Psychiatry (2016) 16:260. doi: 10.1186/s12888-016-0970-y
14. Trachsel M, Irwin SA, Biller-Andorno N, Hoff P, Riese F. Palliative psychiatry for severe and persistent mental illness. Lancet Psychiatry (2016) 3:1–2. doi: 10.1016/S2215-0366(16)00005-5
15. Woods A, Willison K, Kington C, Gavin A. Palliative care for people with severe persistent mental illness: A review of the literature. Can J Psychiat (2008) 53(11):725–36. doi: 10.1177/070674370805301104
16. Kuhn TS. The Structure of Scientific Revolutions. Chicago London: University of Chicago Press (1962).
17. Morse JM, Hupcey JF, Mitcham C, Lenz ER. Choosing a Strategy for Concept Analysis in Nursing Research: Moving Beyond Wilson. In: Gift AG, editor. Clarifying Concepts in Nursing Research. New York: Springer (1997). p. 73–96.
18. Morse JM, Mitcham C, Hupcey JF, Tasón Cerdas M. Criteria for concept evaluation. J Adv Nurs (1996) 24(2):385–90. doi: 10.1046/j.1365-2648.1996.18022.x
19. Morse JM. Exploring Pragmatic Utility: Concept Analysis by Critically Appraising the Literature. In: Rodgers BL, KA K, editors. Concept Development in Nursing: Foundations, Techniques, and Applications. Philadelphia: W.B. Saunders (2000). p. 333–52.
20. Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst Rev (2017) 6:245. doi: 10.1186/s13643-017-0644-y
21. Booth A, Sutton A, Papaioannou D. Systematic Approaches to a Successful Literature Review. 2nd ed. Los Angeles: Sage (2016).
22. Kuckartz U, Rädiker S. Analyzing Qualitative Data with MAXQDA. Text, Audio, and Video. Wiesbaden: Springer (2019).
23. Weaver K, Mitcham C. Nursing concept analysis in North America: state of the art. Nurs Philos (2008) 9(3):180–94. doi: 10.1111/j.1466-769X.2008.00359.x
24. Arvidsson H. Severely and persistently mentally ill—a changing group. Ten years after the 1995 Swedish mental health care reform. Nord J Psychiat (2009) 63(5):355–60. doi: 10.1080/08039480903093922
25. Chandler D, Hu T-W, Meisel J, McGowen M, Madison K. Mental health costs, other public costs, and family burden among mental health clients in capitated integrated service agencies. J Ment Health Admin (1997) 24(2):178–88. doi: 10.1007/BF02898512
26. Durham ML. Healthcare’s greatest challenge: Providing services for people with severe mental illness in managed care. Behav Sci Law (1994) 12(4):331–49. doi: 10.1002/bsl.2370120404
27. Hilburger JJ. Readiness for change among people with severe and persistent mental illness in a rehabilitation program. Rehabil Couns Bull (1999) 41(1):12–9. doi: 10.1177/003435529904300104
28. Hsiao C-Y. Individual and family adaptation to severe and persistent mental illness (SPMI) in Taiwanese families. Res Nurs Health (2009) 32:307–20. doi: 10.1002/nur.20322
29. Parabiaghi A, Bonetto C, Ruggeri M, Lasalvia A, Leese M. Severe and persistent mental illness: a useful definition for prioritizing community-based mental health service interventions. Soc Psych Psych Epid (2006) 41(6):457–63. doi: 10.1007/s00127-006-0048-0
30. Pasmeny GA. Social support and quality of life in adults with severe and persistent mental illness [master’s thesis]. Lethbridge (AB): University of Lethbridge (2008).
31. Veltro F, Magliano L, Lobrace S, Morosini P. Severely and persistently mentally ill patients in Italy: an overview of epidemiological and psychosocial findings. Int J Soc Psychiatr (1993) 39(4):285–302. doi: 10.1177/002076409303900405
32. Yamada MM, Korman M, Hughes CW. Predicting rehospitalization of persons with severe mental illness. J Rehabil (2000) 66(2):32–9.
33. Draine J. A critical review of randomized field trials of case management for individuals with serious and persistent mental illness. Re Soc Work Prac (1997) 7(1):32–52. doi: 10.1177/104973159700700102
34. Isaacs AN, Sutton K, Dalziel K, Maybery D. Outcomes of a care coordinated service model for persons with severe and persistent mental illness: A qualitative study. Int J Soc Psychiatr (2017) 63(1):40–7. doi: 10.1177/0020764016678014
35. Koekkoek B, Van Meijel B, Schene A, Hutschemaekers G. Problems in psychiatric care of ‘difficult patients’: a Delphi-study. Epidemiol Psych Sci (2009) 18(4):323–30. doi: 10.1017/S1121189X00000294
36. Banfield M, Forbes O. Health and social care coordination for severe and persistent mental illness in Australia: a mixed methods evaluation of experiences with the Partners in Recovery Program. Int J Ment Health Sy (2018) 12:13. doi: 10.1186/s13033-018-0194-2
37. Kinter KT. What’s in a Name: “Serious”, “Severe”, and “Severe and Persistent”. Int J Psychosoc Rehabil (2017) 21(1):52–4.
38. Torres D. Defining Severe Persistent Mental Illness: Implications for Knowledge, Needs, and Services. In: Estrine SA, Hettenbach R, Arthur H, Messina M, editors. Service Delivery for Vulnerable Populations: New Directions in Behavioral Health. New York, NY: Springer Publishing Company (2011). p. 1–38.
39. Trachsel M. The ethical importance of assessing end-of-life care preferences in patients with severe and persistent mental illness. Am J Geriat Psychiat (2018) 26(1):98–9. doi: 10.1016/j.jagp.2017.09.026
40. Wasylenki D, Goering P, Macnaughton E. Planning mental health services: background and key issues. New Dir Ment Health Serv (1994) (61):21–9. doi: 10.1002/yd.23319946105
41. Skartvedt E. Definitions of chronic mental illness (CMI): A literature review: A technical report. Denver: National Institute of Mental Health Contract 86M5T067090D (1987).
42. Goldman HH, Gattozzi AH, Taube CA. Defining and Counting the Chronically Mentally Ill. Hosp Community Psych (1981) 32(1):21–7. doi: 10.1176/ps.32.1.21
43. State Board Policy 1029. Definition of serious mental illness. Richmond (VA): Department of Mental Health, Mental Retardation and Substance Abuse Services (1990).
44. National Board of Health and Welfare. The First Thousand Days of the Swedish Mental Health Care Reform. Stockholm: National Board on Health and Welfare (1998).
45. Grob GIJO. Mental health policy in the United States. Int J Law Psychiat (2008) 31:89–100. doi: 10.1016/j.ijlp.2008.02.003
46. Australian Government. Partners in Recovery (PIR): Coordinated support and flexible funding for people with severe, persistent mental illness and complex needs intiative. Program guidelines for the engagement of PIR Organisations 2012-2013 to 2015-2016. Canberra: Department of Health and Ageing (2011).
47. Clark D, Graham F, Centeno C. Changes in the world of palliative care. Medicine (2015) 43(12):696–8. doi: 10.1016/j.mpmed.2015.09.012
48. World Health Organization. Integrating palliative care and symptom relief into primary health care: a WHO guide for planners, implementers and managers. (2018). Available from: http://apps.who.int/iris/bitstream/handle/10665/274559/9789241514477-eng.pdf?ua.
49. Brigandt I. The dynamics of scientific concepts: The relevance of epistemic aims and values. In: Steinle F, Feest U, editors. Scientific concepts and investigative practice. Berlin: De Gruyter (2012). p. 75–103.
50. MacLeod M. Rethinking scientific concepts for research contexts: The case of the classical gene. In: Steinle F, Feest U, editors. Scientific concepts and investigative practice. Berlin: De Gruyter (2012). p. 47–74.
51. Fleck L. Entstehung und Entwicklung einer wissenschaftlichen Tatsache. Einführung in die Lehre vom Denkstil und Denkkollektiv. Frankfurt am Main: Suhrkamp (1980 [1935]).
52. Milazzo-Sayre LJ, Henderson MJ, Manderscheid RW. Serious and Severe Mental lllness and Work: What Do We Know? In: Bonnie RJ, Monahan J, editors. Mental Disorder, Work Disability, and the Law. Chicago London: University of Chicago Press (1997).
53. Bachrach LL. Defining Chronic Mental Illness: A Concept Paper. Hosp Community Psych (1988) 39(4):383–8. doi: 10.1176/ps.39.4.383
54. van der Steen WJ. A Practical philosophy for the life sciences. Albany: University of New York Press (1993).
55. Decorte I, Verfaillie F, Moureau L, Meynendonckx S, Van Ballaer K, De Geest I, et al. Oyster care: An innovative palliative approach towards SPMI patients. Front Psychiatry (2020) 11:509. doi: 10.3389/fpsyt.2020.00509
56. Burns D. Systemic action research: A strategy for whole system change. Bristol: The Policy Press (2007).
Keywords: severe and persistent mental illness, SPMI, palliative psychiatry, pragmatic utility concept analysis, systematic review
Citation: Zumstein N and Riese F (2020) Defining Severe and Persistent Mental Illness—A Pragmatic Utility Concept Analysis. Front. Psychiatry 11:648. doi: 10.3389/fpsyt.2020.00648
Received: 29 January 2020; Accepted: 22 June 2020;
Published: 06 July 2020.
Edited by:
Anna Lisa Westermair, University of Lübeck, GermanyCopyright © 2020 Zumstein and Riese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Naomi Zumstein, bmFvbWkuenVtc3RlaW5AdXpoLmNo
 Naomi Zumstein
Naomi Zumstein Florian Riese
Florian Riese